Abstract
Aim
This paper proposes a novel, trauma‐informed, conceptual model of care for Post‐Acute Sequelae of COVID‐19 illness (PASC).
Design
This paper describes essential elements, linkages and dimensions of the model that affect PASC patient experiences and the potential impact of trauma‐informed care on outcomes.
Data sources
PASC is a consequence of the global pandemic, and a new disease of which little is known. Our model was derived from the limited available studies, expert clinical experience specific to PASC survivors and publicly available social media narratives authored by PASC survivors.
Implications for nursing
The model provides a critical and novel framework for the understanding and care of persons affected by PASC. This model is aimed at the provision of nursing care, with the intention of reducing the traumatic impacts of the uncertain course of this disease, a lack of defined treatment options and difficulties in seeking care. The use of a trauma‐informed care approach to PASC patients can enhance nurses' ability to remediate and ameliorate both the traumatic burden of and the symptoms and experience of the illness.
Conclusion
Applying a trauma‐informed perspective to care of PASC patients can help to reduce the overall burden of this complex condition. Owing to the fundamentally holistic perspective of the nursing profession, nurses are best positioned to implement care that addresses multiple facets of the PASC experience.
Impact
The proposed model specifically addresses the myriad ways in which PASC may affect physical as well as mental and psychosocial dimensions of health. The model particularly seeks to suggest means of supporting patients who have already experienced a life‐threatening illness and are now coping with its long‐term impact. Since the scope of this impact is not yet defined, trauma‐informed care for PASC patients is likely to reduce the overall health and systems burdens of this complex condition.
Keywords: COVID‐19, long‐haul COVID, nursing care, trauma‐informed care, traumatic stress
1. INTRODUCTION
Post‐acute sequelae of SARS‐CoV‐2 infection (PASC) is the persistence of COVID‐19 symptoms extending beyond expected resolution of the disease. Over 313 million people worldwide, and over 62 million in the United States, have survived infection with SARS‐CoV‐2 virus (New York Times, 2022). It is estimated that 10%–80% of these survivors will develop Post‐Acute Sequelae of SARS‐CoV‐2 illness, or PASC (Carfì et al., 2020; Davis et al., 2021; Yong, 2021). As a relatively new condition, PASC is not yet fully clinically characterized, but was recently defined by the World Health Organization (WHO, 2021a) as occurring:
in individuals with a history of probable or confirmed SARS‐CoV‐2 infection, usually 3 months from the onset of COVID‐19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others and generally have an impact on everyday functioning. Symptoms may be new onset, following initial recovery from an acute COVID‐19 episode, or persist from the initial illness. Symptoms may also fluctuate or relapse over time.
Given its potential prevalence, PASC has been called the next ‘national health disaster’ (Phillips & Williams, 2021, p. 577). This paper proposes a model that establishes contextual factors, patient experiences and potential patient outcomes which may contribute to recovery among PASC survivors.
2. BACKGROUND
The pathology of PASC is not fully elucidated, although emerging evidence suggests persistent activation of the immune system and endothelium as key contributors (Proal & VanElzakker, 2021). Patient reports demonstrate that PASC symptoms vary in type and duration; however, multiple studies suggest that symptoms affecting cognition and ability to complete activities of daily living have a significant impact (Davis et al., 2021). This has great import for care of affected individuals, as these symptoms are likely to prompt care‐seeking. It is, therefore, crucial to consider how nurses can best support patients with the symptom, social and system effects of PASC.
2.1. Trauma and the need for trauma‐informed care for PASC
According to SAMHSA's Trauma and Justice Strategic Initiative (2014), ‘trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual's functioning and physical, social, emotional, or spiritual well‐being’ (p. 7). This is the ‘three E's’ definition of trauma, and it should be noted that these can be cyclical if circumstances recur or have multiple antecedents. Traumatic impact thus derives less from the kind of event than from how a person experiences it, based on interplay among biopsychosocial and cultural factors. Ultimately, the impact of a traumatic experience is unique to the individual, but a considerable body of research has demonstrated that trauma contributes to a variety of poor health outcomes (Humphreys et al., 2016; O'Neill et al., 2018).
Owing to the novelty and complexity of PASC, affected individuals may experience distressing symptoms, only to have these dismissed or downplayed by friends, family and healthcare providers. In the latter case, patients may be left feeling betrayed by the very system from which they sought help—a phenomenon known as betrayal trauma. Betrayal trauma results from being injured or wronged by an entity upon which one depends for support or survival (Smith, 2017; Smith & Freyd, 2017). In addition to betrayal trauma, PASC survivors have often experienced the trauma of a life‐threatening illness followed by persistent, challenging symptoms and sequelae—warranting a trauma‐informed approach to care. Such an approach involves a ‘universal precautions’ perspective, which assumes that most people have experienced trauma; that trauma affects everyone differently and that trauma can affect all aspects of well‐being—physical, emotional, cognitive, behavioural, social, economic and spiritual (SAMHSA, 2014). Using a trauma‐informed lens when providing care to PASC patients can promote recovery across dimensions and increase potential for patient re‐engagement with healthcare.
3. CONCEPTUAL MODEL OF TRAUMA‐INFORMED CARE FOR PATIENTS WITH PASC
Our model (see Figure 1) conceptualizes how a trauma‐informed approach can improve care for PASC patients. Underlying assumptions include that: the PASC patient is experiencing unpleasant symptoms, based on individual perception and self‐report; the patient is actively seeking to minimize or resolve the impact of the symptom(s) and trauma‐informed care has the potential to improve patient engagement and health outcomes, and to decrease unnecessary systems utilization. The first and second assumptions are grounded in the Theory of Unpleasant Symptoms (Lenz et al., 1997), which suggests that symptoms can occur simultaneously and interact multiplicatively, that they reflect changes in usual function, and that help‐seeking is often a consequence. The third assumption is based on theories of trauma, including betrayal trauma (Smith & Freyd, 2014; Tebes et al., 2019).
FIGURE 1.
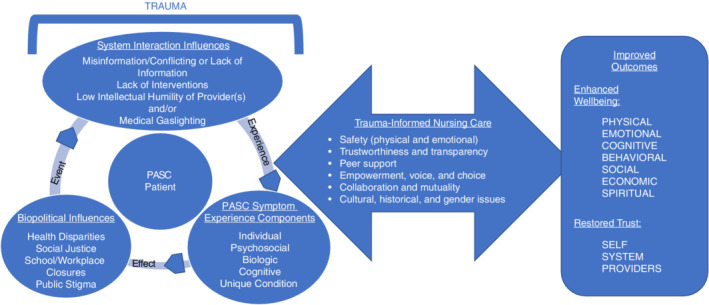
Conceptual model of trauma‐informed care for patients with PASC
3.1. Elements of the model
Elements of the proposed model include the traumatic arc of event‐experience‐effect (three E's), contextual factors, PASC symptom experience, trauma‐informed nursing care and outcomes. The model is specifically context‐bound: the model's temporal context is after the emergence of the SARS‐CoV‐2 virus and following the WHO's definition of PASC. There are several aspects of this context that influence other elements of the model, and factors listed are not exhaustive.
3.1.1. Traumatic arc
In the proposed model, the arc of the three E's permeates the contextual factors (described below) that are part of the patient experience of PASC. This illustrates the potential for ongoing, overlapping, interacting traumas in this experience. For example traumatic events could include loss of job and related healthcare access, having PASC symptoms dismissed by an uninformed provider, or the symptom experience itself. The experience of such events can influence how the patient interacts with or experiences other factors and may increase likelihood of further traumatic experiences. Some PASC patients describe a cascading effect where symptoms were disregarded by providers, but clearly affected their daily personal and professional lives, causing them to experience stigma from those around them when they were unable to function as they had previously (Callan et al., 2021). In some cases this led to unemployment or underemployment, prompting healthcare changes and the cycle repeating itself (Davis et al., 2021).
3.1.2. Contextual factors
Contextual factors shape how the individual understands and experiences PASC, and what sources of trauma may affect them. Importantly, some patients are unaware of their COVID‐19 status until the onset of PASC symptoms. Therefore, this element of the model encompasses both Biopolitical Influences and System Interactions that may contribute to traumatization of PASC patients.
Biopolitical influences
Biopolitical influences are those which, as described by Foucault (1978), ‘ensure, sustain, and multiply life, to put this life in order’ (p. 138) Within these processes, however, is embedded the contrasting action of not doing so—in effect, allowing encroachment of dysfunction and/or death. Critically, Georges (2014) addresses how the creation and sustenance of biopolitical spaces within healthcare may diminish or even eliminate compassion for patient suffering. In the proposed model, influences including absent social justice, disparities in health and healthcare and the public stigma associated with COVID‐19 contribute to the incapacitation of a system that ostensibly relieves suffering. Those suffering the loss of capacity or function associated with PASC are thus ejected from the systems that define what it is to live in society. This is intensified for those holding reduced biopolitical power, for whom disparities in health and healthcare access are also a critical consideration, as are other social justice and resource issues.
Health disparities
Health disparities are a function of biopolitical power, proceeding from the impact of social structures that skew towards particular groups—a phenomenon known as structural violence (Burton et al., 2020). Under COVID‐19 pandemic conditions, health disparities in the United States have intensified as many vulnerable populations eschewed care due to changed circumstances, fear of discrimination and economic pressures (Mein, 2020). For those rendered socially and structurally vulnerable, decreased access to or contact with healthcare can increase risk of poor outcomes or even death—furthering potential for traumatic experiences and intensifying the impact of PASC‐associated traumas.
Social justice
A further aspect of the temporal context for this model, movements to counter systemic patterns of racial injustice and violence against people of colour gained momentum in the wake of the violent deaths of Breonna Taylor, Ahmaud Arbery, George Floyd and other people of colour. This is an important consideration insofar as both the murders themselves and the images of violence directed at those protesting were ubiquitous in the media and therefore potentially vehicles of indirect traumatization for many (Thompson et al., 2020). With such issues so visible, patients of colour struggling with PASC prior to its formal identification may have felt doubly betrayed by both their communities and healthcare institutions.
School and workplace closures
Although intended to reduce potential for transmission of COVID‐19, school and workplace closures upended the lives of many families. In addition to isolation and impacts on psychosocial development, many safety nets for food security and social services became unavailable even as families simultaneously experienced job losses or decreases in working hours. As a result, many lost access to health insurance and care systems while under the strain of maintaining financial stability. Combined, school and industry closures created increased risks for traumatic experiences with significant negative long‐term potential. These may have reduced access to care for PASC‐related symptoms as well as increasing stress and trauma burdens for families already facing structurally violent circumstances.
Public stigma
Finally, for many PASC patients, there is an attached experience of stigma related to both having COVID‐19 and subsequently suffering the symptoms of PASC. Given the high public threat and contagion perceptions associated with COVID‐19, those who contracted the illness were automatically forced into isolation or quarantine conditions—invoking fear and suspicion from others (Bagcchi, 2020). For those who developed PASC, the disabling symptoms and the somewhat ‘invisible’ nature of the condition—often initially diagnosed as something else or dismissed by providers—further stigmatized patients who found themselves feeling misaligned with personal as well as social norms (Callan et al., 2021; Ysasi et al., 2018).
System interaction influences
Healthcare in the United States requires the individual to interact directly with systems that provide access to and delivery of care. The systems depend on engagement of individuals as providers and patients, and the system controls these individuals by directing engagement through regulations, requirements, diagnostic pathways and practice guidelines. PASC presents a significant challenge to this system, due to both its novelty and significant associated morbidity. In the absence of clear pathways for the treatment of PASC survivors, interactions with healthcare may be at best challenging and at worst betraying for an already distressed population.
Misinformation, conflicting and/or lack of information
Conflicting information and misinformation about SARS‐CoV‐2, COVID‐19 and PASC illnesses have spread rapidly. Conflicting information occurs when two or more discordant assertions are presented as true (e.g. wearing a mask is not vs. is necessary to reduce viral spread), while misinformation is inaccurate information knowingly or unknowingly presented as fact (e.g. the COVID‐19 vaccine makes people magnetic) (Nagler et al., 2020). Both conflicting information and misinformation ‘create a breeding ground for uncertainty. Uncertainty in turn fuels skepticism and distrust, which is the perfect environment to foster fear, anxiety, blame, stigma, [and] violent aggression’ (World Health Organization, 2021b).
Lack of interventions
Many healthcare providers have had little exposure to those with PASC and may not readily include it in a differential diagnosis, seeking instead to fit its symptoms into known diagnoses such as post‐viral fatigue or undiagnosed mental health problems (Callard & Perego, 2021). Subsuming PASC within other, more familiar paradigms fails to appreciate the unique disease pathophysiology, presentation and trajectory—risking further patient distress as well as inadequate treatment. Due to its novelty, even those suffering with PASC may not recognize the illness. This creates isolation, related to stigma issues as described above, and this combined with frightening and unexplained symptoms is distressing—particularly for those 40%–45% of individuals whose initial infection was asymptomatic and/or undiagnosed (Oran & Topol, 2020). Even if aware of PASC, these individuals may not consider their symptoms related if unaware that they had COVID‐19 (Rushforth et al., 2021). Moreover, even if symptoms are treated they may be addressed individually, and such strategies fail to address the cumulative symptom burden of PASC (Lambert et al., 2021).
Low intellectual humility among provider(s)
Given the uncertainties in identifying and treating PASC, some providers may incorrectly assume that patients are incorrectly or even deceptively reporting symptoms. This form of attribution error can be compounded if the provider lacks intellectual humility: the capacity to revise an opinion when information conflicts with one's own views and to accept some degree of uncertainty (Grunberg et al., 2021; Schei et al., 2019). Low intellectual humility, especially coupled with attribution error, may lead to increased presumption that individuals with less biopolitical power by virtue of race, gender, educational level, ability or socioeconomic status have less capacity as patient informants both because the provider is assumed to be correct and because the sociohistorical context of medicine and medical practice categorizes individuals outside ‘the wealthy, white, able‐bodied, heterosexual, cissex, endosex and cisgender male subject’ as ‘other’ (Sebring, 2021, p. 1954). Worse, patients with PASC have reported ‘medical gaslighting’—a term that refers to having one's symptoms dismissed or rejected, often as psychogenic rather than physiological (Fetters, 2018; Sebring, 2021)—or not being believed when they report symptoms (Rushforth et al., 2021). LIH can thus contribute to traumatic burden and to increased health risk among PASC patients.
3.1.3. The PASC symptom experience
The PASC symptom experience is a dynamic, multidimensional interaction of individual, psychosocial, biologic, cognitive and PASC‐condition components unique to the affected individual. It is important to recognize that this experience can represent both event and experience pieces of trauma, in that for some patients PASC is the first inkling of illness. Understanding various components of PASC can thus assist providers in identifying sources of trauma and caring for those affected.
Individual component
The individual component of PASC symptomology describes the lived experiences and characteristics a person carries into living with PASC. These include disposition, coping skills, developmental stage and perceived self‐efficacy—qualities that affect how an individual perceives, responds to, manages and evaluates the experiences of COVID‐19 illness and PASC (Dodd et al., 2001; Millroth & Frey, 2021). Also in this domain are stigmatizing effects, such as those associated with having a communicable disease (COVID‐19) and its visible or invisible sequelae (PASC); and structural stressors, the social and political structures that cause distress by devaluing or excluding those with certain characteristics (Burton et al., 2020; DeWilde et al., 2019). Both stigma and structural stressors can negatively impact health‐seeking behaviours; access to resources and physical, psychological and behavioural responses to health challenges (DeWilde et al., 2019; DeWilde & Burton, 2016).
Psychosocial component
This refers to the intersection of an individual's social context, identity and behaviour. A person's identity may reflect qualities or actions attributed to or expected of self—for example being thought of as generous or as a good friend—while role performance is tied to social structures. By locating the self in a social context such as work or community, the individual is identified socially. This phenomenon has been described as sociolocation (Burton et al., 2013). For those affected by PASC, sociolocation processes may be disrupted when chronic illness symptoms alter role performance and/or self‐efficacy.
Biologic component
Viral infections can cause significant morbidity and potentially lifelong illness. In the case of PASC, the syndrome experience has crucial biologic components that may proceed from infection with SARS‐CoV‐2 and contribute to the overall experience of PASC.
Chronic inflammation
Among persons with PASC, evidence suggests a persistent and aberrant inflammatory response. In survivors of severe COVID‐19 disease, data show an increase in inflammatory markers such as procalcitonin, C‐reactive protein, ferritin, interleukin (IL)‐2R, IL‐6, IL‐8 and tumour necrosis factor (TNF)‐a (Qin et al., 2020). Many of these biomarkers, as well as changes in the composition of immune cells, have been documented in persons with PASC independent of the initial severity of COVID‐19 illness.
Activation of the hypothalamus–pituitary–adrenal (HPA) axis
Activation of the hypothalamus–pituitary–adrenal (HPA) axis has been associated with stress and with chronic illnesses including anxiety, post‐traumatic stress disorder (PTSD), major depressive disorder and occupational burnout (Labonte et al., 2014; Lee et al., 2021; McKay & Zakzanis, 2010). Emerging data suggest that persons with PASC experience significant stress which can lead to an alteration in HPA axis activity that also influences symptom experience (e.g. increase in symptom number or severity). SARS‐CoV‐2 may lead to direct activation of the HPA axis, and other systems involved in maintaining homeostasis through the production of cytokines in response to infection (Goldstein, 2020). Coupled with ongoing contextual factor‐based stressors as described above, such activations may be intensified (Perlmutter, 2021).
Sympathetic nervous system (SNS) activation
Increased or enhanced activation of the sympathetic nervous system (SNS), such as may be manifest via cardiac conduction and rhythm abnormalities, has been observed in individuals with COVID‐19 disease (Babapoor‐Farrokhran et al., 2020). Indeed, studies show that SARS‐CoV‐2 infection has led to the development of postural tachycardia syndrome (POTS) (Miglis et al., 2020). This may be because SARS‐CoV‐2 infects the brainstem and changes function of some medullary centers, causing increased central sympathetic outflow similar to takotsubo cardiomyopathy. Such a pathway could also explain changes to mental health such as new‐onset anxiety and depression, and to cerebral blood flow resulting in the common PASC complaint of ‘brain fog’ (Goldstein, 2021). Further, in the acute infection phase, an overwhelming immune response can impair capacity to re‐establish homeostasis—a phenomenon that may be related to the stress‐induced allostatic loading process (Al‐kuraishy et al., 2021; Goldstein, 2020).
Vascular instability
In combination with other inflammatory, stress‐related and reactive processes, endothelial cells abundantly express the ACE‐2 receptor which allows for binding of SARS‐CoV‐2 and facilitates endothelial activation. The response promotes thrombus formation, inflammation and vascular permeability. The activated endothelium can also release cytokines that further exacerbate inflammation and express adhesion molecules that allow migration of leukocytes into interstitial spaces. COVID‐19 infection may thus result in vascular events such as transient ischemic attack (TIA), cerebral vascular accident (CVA), pulmonary embolism (PE), or deep vein thrombosis (DVT)—which have been shown to be common in affected patients, independent of illness severity (Tiwari et al., 2020). For PASC patients, this may mean managing the sequelae of vascular events, risk for additional such events and weakened overall vasculature.
Cognitive component
The toll of PASC‐related cognitive impairments has been profound. Survivors report feelings of guilt, shame, and/or internalized stigma related to inability to fulfil role responsibilities as well as a lack of understanding from others—including some healthcare providers—about these impairments (Callan et al., 2021; Rushforth et al., 2021). Many suffering with PASC report cognitive impairments such as inability to concentrate; short‐ and long‐term memory problems; aphasic episodes; decision‐making difficulties and ‘brain fog’—a state which may include all of these as well as generalized disorientation or confusion (Callan et al., 2021; Callard & Perego, 2021; Huang et al., 2021). These symptoms can affect ability to work or attend school, manage daily responsibilities and participate in social activities (Callan et al., 2021; Lambert et al., 2021). At the same time, cognitive impairments are often not recognized by others—sufferers do not ‘look sick’ and may be faced with having to either demonstrably substantiate or conceal impairment (Ysasi et al., 2018).
Unique condition component
The novel, unique nature of PASC itself is also a critical function of the patient experience. Changing, remitting and relapsing symptoms and multiple concurrent symptoms contribute to the cumulative symptom burden reported by PASC sufferers (Lambert et al., 2021). Coupled with the uncertain course of PASC, this burden can be so distressing and debilitating that patients cannot fulfil work, household or social obligations.
3.1.4. Trauma‐informed nursing interventions
The complexities of the social contextual and experiential components that surround and influence patients' trajectories of SARS‐CoV‐2 infection and PASC have the potential to generate significant traumatic impacts. This is the effect element of trauma. Our proposed model thus incorporates the principles of trauma‐informed care practice with cyclic processes of assessment, intervention and reappraisal to plan and implement care for the PASC patient. Applying trauma‐informed care strategies has potential to reduce emotional and psychological effects of PASC, as well as to help restore patient confidence and self‐efficacy in care. The following sections explore how the principles of a trauma‐informed approach (SAMHSA, 2014) can be applied in care of PASC patients.
Physical and emotional safety
Safety is a cornerstone of nursing practice and is defined as freedom from accidental injury (Kohn et al., 2000). It is important to consider that such injuries need not be physical and can be inflicted by almost anyone with whom a patient has contact—the present pandemic has illuminated the perils of the healthcare system in terms of maintaining effective and adequate care (Dean et al., 2019). For example people of colour, those affected by chronic conditions, and those residing in nursing homes or rehabilitation facilities have increased morbidity and mortality from COVID‐19 (Berkowitz et al., 2020; Sabatello et al., 2020). Particularly in the care of PASC patients, it is thus critical that nurses establish a sense of safety with and for patients as the novelty of this condition brings with it uncertainty which can in turn provoke fear and frustration (Lancet, 2021). PASC patients report feeling misunderstood, having symptoms dismissed as self‐injury or anxiety and experiencing fear or mistrust of providers as a result (Callard & Perego, 2021; Paredes et al., 2021; Pinto et al., 2022).
Trustworthiness and transparency
Safety is related to trustworthiness insofar as trust in each interaction requires a sense of safety. Further, transparency is also related to both safety and trustworthiness as transparency helps to facilitate trust and ultimately safety. Trust requires that individuals have a specific need that cannot be met without the assistance of another, because it places the individual conferring trust in a ‘dependent and vulnerable situation’ (Hupcey et al., 2001, p. 286). Dinç and Gastmans (2012) tie this to nursing, in that patients cannot meet their own care needs and therefore rely on and trust nurses to do so. Prior research has indicated that factors such as trustor's beliefs about trustee's intentions towards goodwill and not malevolent action (Bell & Duffy, 2009), consistency in words and action (Carter, 2009) and evaluation of moral character and perception of sufficient knowledge to fulfil a need (Hupcey et al., 2001) all inform perception of trustworthiness. Hupcey et al. (2001) also note that while trust is formed in the present, the ability to trust is also situated in the past and future based on prior experiences, which impute to what degree an individual may be trusted. For instance in situations where PASC patients experienced medical gaslighting, many felt betrayed and unable to trust in provider professionalism (Rushforth et al., 2021).
Peer support
Peer support, originally described by Gartner and Riessman (1982), is a type of social support usually provided by individuals with a particular health condition to others with a similar condition, with the end goal of producing social or personal change. Later, this definition was clarified to add ‘a system of giving and receiving help founded on key principles of respect, shared responsibility and mutual agreement of what is helpful’ (Mead et al., 2001, p. 6). This reflects the importance of trust and safety in peer support. Peer support has been a prominent aspect of the developing understanding of PASC, with many patients seeking support via social media and other online forums (Callard & Perego, 2021). In fact, some peer support forums include affected healthcare providers who are well‐positioned to advocate for patients with provider colleagues (Rushforth et al., 2021).
Empowerment, voice and choice
The act of assisting—without judgement—a patient in seeking peer support is also a reflection of the value of empowerment, voice and choice in trauma‐informed care. Engaging in patient‐related advocacy has been identified as a critical function of nursing care during acute COVID‐19 illness and is almost certainly to be equally valuable to PASC patients (Abuhammad et al., 2021; Arcadi et al., 2021). Especially where patients have experienced betrayal, either through some form of medical gaslighting or another contextual or experiential pathway, advocating for patient empowerment and supporting voice and choice in care planning can support reengagement with the healthcare system and increase perceived self‐efficacy (Smith & Freyd, 2017).
Collaboration and mutuality
As with the reengagement of patients through empowerment, voice and choice, it is critical that PASC patients perceive that they are collaborative partners in their care. The novelty of PASC has caused patients to have difficulty obtaining diagnoses and treatment, and many report feeling ignored, dismissed or even shamed for seeking medical intervention during a pandemic (Roth & Gadebusch‐Bondio, 2022). Nurses and other providers can help ameliorate this trauma by acknowledging the value of patient input in treatment, and by demonstrating awareness of the vital roles that patient narratives have had in identifying and characterizing PASC (Roth & Gadebusch‐Bondio, 2022).
Cultural, historical and gender issues
The last principal of trauma‐informed approaches involves attending to and seeking to limit the impact of cultural, racial, gender or other biases. Actual or perceived biases profoundly impact a patient's approach to, trust in and comfort with the healthcare system and providers. Even small indicators of bias—often called microaggressions or microinsults—can lead to mistrust and disengagement by patients (Orphanidys et al., 2022) Examples of care practices that consider these issues include providing care in a patient's preferred language; using preferred gender pronouns and acknowledging and addressing the effects of racism on social determinants of health such as housing and safe living environment, education, employment and access to healthcare (Burton et al., 2020). Given the extensive history of dismissing or invalidating as psychosomatic the health concerns of women, people of colour, members of the LGBTQIA+ community and other groups lacking in biopolitical power, it is vital that these groups receive culturally safe nursing and other healthcare (Sebring, 2021; Ziauddeen et al., 2021).
3.2. Application of a trauma‐informed process to care of PASC patients
Trauma‐informed nursing interventions are implemented using an iterative process adapted from the nursing process. The centring of the PASC patient in this process is a fundamental element of the proposed model, as many of the principles of trauma‐informed care rely on effective and therapeutic interaction between patient and nurse. In this model, relevant Contextual Factors and components of the PASC Symptom Experience may affect the patient before the clinical nursing encounter. This means that the nurse (or indeed any provider) must recognize and consider these in the patient interaction, to provide fully trauma‐informed care. Similar engagement processes have demonstrated effective responses with vulnerable groups, such as in nursing research that employs a community‐based participatory methodology and in cross‐cultural efforts to develop ethical, respectful research engagement with vulnerable populations (Lucero et al., 2020; Mathew et al., 2017). These represent cases in which a ‘trustor’—in this model, a PASC patient—must become confident that the ‘trustee’—here, a nurse—will both acknowledge situational trauma burdens and provide care in a trauma‐informed manner. The practice of trauma‐informed care allows for appropriate leeway in clinical judgement and in the interactions of nurse and patient in developing care and treatment plans, and as such lends itself well to care of PASC patients.
3.3. Outcomes
Studies suggest that survivors of COVID‐19 report persistent and elevated stress levels well beyond resolution of the acute illness (Chrousos & Kaltsas, 2005). Owing to the biological and psychological effects of infection with the SARS‐CoV‐2 virus and the additional stresses imposed by the pandemic, a critical outcome of the proposed model is an improved sense of wellbeing across multiple domains. Measurements of this outcome could take the form of mental and physical health assessments, as well as physiological measures of exercise and activity tolerance, and psychosocial inventories of social supports and overall quality of life.
A secondary, though equally important, outcome of the proposed model is restoration of trust and self‐efficacy for the PASC patient. While self‐efficacy may be assessed via psychosocial or psychological inventory, trust in the healthcare system and in healthcare providers is a more complex consideration. Assessment of this outcome may require some combination of patient satisfaction measures with qualitative data collection on what meaning trust has in such relationships, particularly for PASC survivors.
4. DISCUSSION AND IMPLICATIONS FOR NURSING RESEARCH AND PRACTICE
The proposed model specifically seeks to elucidate how PASC, both novel and understudied but potentially affecting large populations, can engender traumatic experiences. The possible population burden of PASC may create significant demand for nursing care, and it is thus critical to identify models and strategies readily applicable to such care. Nursing science and practice are well‐situated to facilitate integration of symptom management with the developing understanding of PASC, and indeed COVID‐19 itself (Pinto et al., 2021, 2022). For example Perazzo et al. (2017) detailed strategies used by palliative care nurses for fatigue management in individuals with human immunodeficiency virus (HIV). The approach incorporated awareness of the multidimensional experiences of fatigue in the context of HIV, and sought to address fatigue across physiological, psychological and behavioural domains. In a similar manner, nurses can integrate knowledge of how PASC patients are affected by trauma and seek to remediate that trauma while providing appropriate supports and care across symptom and contextual domains. Further, the complexities of pandemic care in current conditions are necessarily tied to the context in which the pandemic occurs: one in which there are significant sources of trauma even for those not directly affected by COVID‐19 illness or PASC. This means that trauma‐informed care may be as fundamental to patient well‐being as other types of interventions and treatment protocols.
One of the most challenging elements of diagnosis and treatment of PASC is the variability with which symptoms are experienced, documented and remediated—particularly because PASC is multisystemic in manifestation. In addition, the interaction between the symptom experiences of PASC and relevant contextual factors can intensify traumatic burden. It is therefore critical that approaches to the study of and care for PASC‐affected persons take a trauma‐informed approach. This is in line with nursing's disciplinary focus on holistic research and practice, in that it considers a wide array of influences and experiences involved in the PASC experience. In the broadest sense, nursing care is generally focused on the restoration of health and wellbeing to the highest possible level in a patient (Benner, 1994). In the proposed model, the application of a trauma‐informed approach augments such restoration by creating more holistically complete strategies for care of PASC patients. The trauma‐informed care approach proposed here combines expected overall improvements in health and well‐being that should follow any healthcare intervention with a larger remediation in the traumatic stress sequelae that may accompany the PASC experience. Further, this model proposes a conceptualization of PASC‐related care that seeks disruption of the ongoing stressful processes in which illness experience is combined with external contextual and system‐based stressors. This is similar to the cyclic process described by DeWilde and Burton (2016) in their framework for cultural distress, wherein a lack of culturally congruent care contributes to worsening patient outcomes.
In addition, PASC management is likely to require the direct engagement of patients in handling symptoms and self‐managing some aspects of treatment—areas in which nursing science has established significant expertise (Brown et al., 2020; Pinto et al., 2021). Individualized approaches to patient care and symptom management, particularly when trauma‐informed, can thus help frightened and otherwise traumatized patients re‐establish their trust in and relationship with healthcare systems.
5. CONCLUSION
Nurses represent approximately 60% of the healthcare workforce, and there are nearly 28 million nurses globally (World Health Organization, 2020). In rural and other locations where access to a physician is not always feasible, a nurse may be the only point of contact between an individual and the healthcare system. This, along with nursing's consistent recognition by the Gallup organization as the most‐trusted profession (Advisory Board, 2020), imbues nurses with immense potential for meaningful changes in the lives of patients. Those suffering with PASC have been exposed to a plethora of potential traumas: from conflicting information and misinformation spread about the virus, the disease and the vaccine to health disparities and medical gaslighting. Added to these traumas is the distress of having a poorly understood novel illness with an unidentified aetiology, no known cure and an unknown trajectory.
Nursing has an established history in symptom science and our collective expertise is badly needed to address the unprecedented global health crisis. In addition to advancing the biological and molecular underpinnings of symptoms, nursing is poised to rapidly re‐tool and repurpose symptom management interventions to care for individuals with PASC. As the science develops around PASC, it may be possible to implement pharmacological and non‐pharmacological interventions early in SARS‐CoV‐2 infection to mitigate long‐term sequelae. An effective response to this global health crisis will require clinical and research collaboration among nurses to manage symptom burden among persons with PASC. Our model provides a conceptual framework for such management utilizing principles of and evidence base for trauma‐informed care.
AUTHOR CONTRIBUTIONS
Conceptualization: H.A., C.B., T.H., C.D., N.L., M.P., A.R., M.H.; Writing—original draft preparation: H.A., C.B., T.H., C.D., M.P.; Writing—Review & Editing: H.A., C.B., C.D., M.H., Y.H., A.R., J.L, R.C.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the thousands of survivors who have shared their stories to help develop understanding of the profound effects of PASC. The answers we need to effectively manage and cure PASC will come from listening and learning from those who suffer from the disease.
Burton, C. W. , Downs, C. A. , Hughes, T. , Lambert, N. , Abrahim, H. L. , Herrera, M. G. , Huang, Y. , Rahmani, A. , Lee, J.‐A. , Chakraborty, R. , & Pinto, M. D. (2022). A novel conceptual model of trauma‐informed care for patients with post‐acute sequelae of SARS‐CoV‐2 illness (PASC ) . Journal of Advanced Nursing, 00, 1–11. 10.1111/jan.15426
Contributor Information
Candace W. Burton, Email: cwburton@uci.edu, @DrCBurton.
Charles A. Downs, @PhysioChuck
Natalie Lambert, @NatalieJLambert.
Melissa D. Pinto, @md_pinto
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during development of the current work.
REFERENCES
- Abuhammad, S. , AlAzzam, M. , & Mukattash, T. (2021). The perception of nurses towards their roles during the COVID‐19 pandemic. International Journal of Clinical Practice, 75(4), e13919. 10.1111/ijcp.13919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Advisory Board . (2020). For the 18th year in a row, nurses are the most‐trusted profession, according to Gallup. Advisory Board. Retrieved January 6 from. https://www.advisory.com/daily‐briefing/2020/01/10/nurse‐trusted [Google Scholar]
- Al‐kuraishy, H. M. , Al‐Gareeb, A. I. , Qusti, S. , Alshammari, E. M. , Gyebi, G. A. , & Batiha, G. E.‐S. (2021). Covid‐19‐induced dysautonomia: A menace of sympathetic storm. ASN Neuro, 13, 17590914211057635. 10.1177/17590914211057635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcadi, P. , Simonetti, V. , Ambrosca, R. , Cicolini, G. , Simeone, S. , Pucciarelli, G. , Alvaro, R. , Vellone, E. , & Durante, A. (2021). Nursing during the COVID‐19 outbreak: A phenomenological study. Journal of Nursing Management, 29(5), 1111–1119. 10.1111/jonm.13249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babapoor‐Farrokhran, S. , Rasekhi, R. T. , Gill, D. , Babapoor, S. , & Amanullah, A. (2020). Arrhythmia in COVID‐19. SN Comprehensive Clinical Medicine, 2(9), 1430–1435. 10.1007/s42399-020-00454-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagcchi, S. (2020). Stigma during the COVID‐19 pandemic. The Lancet Infectious Diseases, 20(7), 782. 10.1016/S1473-3099(20)30498-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell, L. , & Duffy, A. (2009). A concept analysis of nurse–patient trust. British Journal of Nursing, 18(1), 46–51. 10.12968/bjon.2009.18.1.32091 [DOI] [PubMed] [Google Scholar]
- Benner, P. (1994). Introduction. In Benner P. (Ed.), Interpretive phenomenology: Embodiment, caring, and ethics in health and illness (pp. xiii–xxvii). Sage. [Google Scholar]
- Berkowitz, R. L. , Gao, X. , Michaels, E. K. , & Mujahid, M. S. (2020). Structurally vulnerable neighbourhood environments and racial/ethnic COVID‐19 inequities. Cities & Health, 1‐4, S59–S62. 10.1080/23748834.2020.1792069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, C. , Peck, S. , Humphreys, J. , Schoenherr, L. , Saks, N. T. , Sumser, B. , & Elia, G. (2020). COVID‐19 lessons: The alignment of palliative medicine and trauma‐informed care. Journal of Pain and Symptom Management, 60(2), e26–e30. 10.1016/j.jpainsymman.2020.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton, C. W. , Gilpin, C. E. , & Draughon Moret, J. (2020). Structural violence: A concept analysis to inform nursing science and practice. Nursing Forum, 1‐7, 382–388. Retrieved December 29, from. https://onlinelibrary.wiley.com/doi/abs/10.1111/nuf.12535 [DOI] [PubMed] [Google Scholar]
- Burton, C. W. , Halpern‐Felsher, B. , Rehm, R. S. , Rankin, S. , & Humphreys, J. C. (2013). "it was pretty scary": The theme of fear in young adult women's descriptions of a history of adolescent dating abuse. Issues in Mental Health Nursing, 34(11), 803–813. 10.3109/01612840.2013.827286 [DOI] [PubMed] [Google Scholar]
- Callan, C. , Ladds, E. , Husain, L. , Pattinson, K. , & Greenhalgh, T. (2021). I can't cope with multiple inputs. Qualitative study of the lived experience of ‘brain fog’ after Covid‐19. medRxiv. 10.1101/2021.08.07.21261740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callard, F. , & Perego, E. (2021). How and why patients made long Covid. Social Science and Medicine, 268, 113426. 10.1016/j.socscimed.2020.113426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carfì, A. , Bernabei, R. , Landi, F. , & for the Gemelli Against COVID‐19 Post‐Acute Care Study Group . (2020). Persistent symptoms in patients after acute COVID‐19. JAMA, 324(6), 603–605. 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter, M. A. (2009). Trust, power, and vulnerability: A discourse on helping in nursing. Nursing Clinics of North America, 44(4), 393–405. 10.1016/j.cnur.2009.07.012 [DOI] [PubMed] [Google Scholar]
- Chrousos, G. P. , & Kaltsas, G. (2005). Post‐SARS sickness syndrome manifestations and endocrinopathy: How, why, and so what?*. Clinical Endocrinology, 63(4), 363–365. 10.1111/j.1365-2265.2005.02361.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, H. E. , Assaf, G. S. , McCorkell, L. , Wei, H. , Low, R. J. , Re'em, Y. , Redfield, S. , Austin, J. P. , & Akrami, A. (2021). Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine, 38, 101019. 10.1016/j.eclinm.2021.101019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean, W. , Talbot, S. , & Dean, A. (2019). Reframing clinician distress: Moral injury not burnout. Federal Practitioner, 36(9), 400–402. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6752815/ [PMC free article] [PubMed] [Google Scholar]
- DeWilde, C. , & Burton, C. W. (2016). Cultural distress: An emerging paradigm. Journal of Transcultural Nursing, 28(4), 334–341. 10.1177/1043659616682594 [DOI] [PubMed] [Google Scholar]
- DeWilde, C. , Carrington, J. , Abbate, A. , Burton, C. W. , Bearman, G. , & Salyer, J. (2019). Structural stress and otherness: How do they influence psychological stress? Journal of Transcultural Nursing, 1043659618823915 478–491. 10.1177/1043659618823915 [DOI] [PubMed] [Google Scholar]
- Dinç, L. , & Gastmans, C. (2012). Trust and trustworthiness in nursing: An argument‐based literature review. Nursing Inquiry, 19(3), 223–237. 10.1111/j.1440-1800.2011.00582.x [DOI] [PubMed] [Google Scholar]
- Dodd, M. , Janson, S. , Facione, N. , Faucett, J. , Froelicher, E. S. , Humphreys, J. , Lee, K. , Miaskowski, C. , Puntillo, K. , Rankin, S. , & Taylor, D. (2001). Advancing the science of symptom management. Journal of Advanced Nursing, 33(5), 668–676. 10.1046/j.1365-2648.2001.01697.x [DOI] [PubMed] [Google Scholar]
- Fetters, A. (2018). The doctor doesn't listen to her. But the media is starting to. The Atlantic. https://www.theatlantic.com/family/archive/2018/08/womens‐health‐care‐gaslighting/567149/ [Google Scholar]
- Foucault, M. (1978). The history of sexuality, volume 1: An introduction (R. Hurley, Trans.). Vintage. [Google Scholar]
- Gartner, A. J. , & Riessman, F. (1982). Self‐help and mental health. Psychiatric Services, 33(8), 631–635. 10.1176/ps.33.8.631 [DOI] [PubMed] [Google Scholar]
- Georges, J. M. (2014). Compassion, biopower, and nursing. In Kagan P. N., Smith M. C., & Chinn P. L. (Eds.), Philosophies and practices of emancipatory nursing: Social justice as praxis (pp. 51–63). Routledge. [Google Scholar]
- Goldstein, D. S. (2020). The extended autonomic system, dyshomeostasis, and COVID‐19. Clinical Autonomic Research, 30(4), 299–315. 10.1007/s10286-020-00714-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein, D. S. (2021). The possible association between COVID‐19 and postural tachycardia syndrome. Heart Rhythm, 18(4), 508–509. 10.1016/j.hrthm.2020.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunberg, N. , McManigle, J. , & Barry, E. (2021). Applying classic social psychology principles to improve healthcare teams [version 2]. MedEdPublish, 9(251). 10.15694/mep.2020.000251.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. , Pinto, M. D. , Borelli, J. L. , Mehrabadi, M. A. , Abrihim, H. , Dutt, N. , Lambert, N. , Nurmi, E. L. , Chakraborty, R. , Rahmani, A. M. , & Downs, C. A. (2021). COVID symptoms, symptom clusters, and predictors for becoming a long‐hauler: Looking for clarity in the haze of the pandemic. medRxiv, 2021.2003.2003.21252086. 10.1101/2021.03.03.21252086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys, K. L. , Esteves, K. , Zeanah, C. H. , Fox, N. A. , Nelson, C. A. , & Drury, S. S. (2016). Accelerated telomere shortening: Tracking the lasting impact of early institutional care at the cellular level. Psychiatry Research, 246, 95–100. 10.1016/j.psychres.2016.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hupcey, J. E. , Penrod, J. , Morse, J. M. , & Mitcham, C. (2001). An exploration and advancement of the concept of trust. Journal of Advanced Nursing, 36(2), 282–293. 10.1046/j.1365-2648.2001.01970.x [DOI] [PubMed] [Google Scholar]
- Kohn, L. T. , Corrigan, J. M. , & Donaldson, M. S. (Eds.). (2000). To err is human: Building a safer health system. The National Academies Press. 10.17226/9728 [DOI] [PubMed] [Google Scholar]
- Labonte, B. , Azoulay, N. , Yerko, V. , Turecki, G. , & Brunet, A. (2014). Epigenetic modulation of glucocorticoid receptors in posttraumatic stress disorder. Translational Psychiatry, 4, e368. 10.1038/tp.2014.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert, N. , Survivor Corps , El‐Azab, S. A. , Ramrakhiani, N. S. , Barisano, A. , Yu, L. , Taylor, K. , Esperanca, A. , Downs, C. A. , Abrahim, H. L. , Rahmani, A. M. , Borelli, J. L. , Chakraborty, R. , & Pinto, M. D. (2021). COVID‐19 Survivors' reports of the timing, duration, and health impacts of post‐acute sequelae of SARS‐CoV‐2 (PASC) infection. medRxiv, 2021.2003.2022.21254026. 10.1101/2021.03.22.21254026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, M. J. , Rittschof, C. C. , Greenlee, A. J. , Turi, K. N. , Rodriguez‐Zas, S. L. , Robinson, G. E. , Cole, S. W. , & Mendenhall, R. (2021). Transcriptomic analyses of black women in neighborhoods with high levels of violence. Psychoneuroendocrinology, 127, 105174. 10.1016/j.psyneuen.2021.105174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenz, E. R. , Pugh, L. C. , Milligan, R. A. , Gift, A. , & Suppe, F. (1997). The middle‐range theory of unpleasant symptoms: An update. Advances in Nursing Science, 19(3), 14–27. https://journals.lww.com/advancesinnursingscience/Fulltext/1997/03000/The_Middle_Range_Theory_of_Unpleasant_Symptoms__An.3.aspx [DOI] [PubMed] [Google Scholar]
- Lucero, J. E. , Emerson, A. D. , Beurle, D. , & Roubideaux, Y. (2020). The holding space: A guide for partners in tribal research. Progress in Community Health Partnerships: Research, Education, and Action, 14(1), 101–107. 10.1353/cpr.2020.0012 [DOI] [PubMed] [Google Scholar]
- Mathew, L. , Brewer, B. B. , Crist, J. D. , & Poedel, R. J. (2017). Designing a virtual simulation case for cultural competence using a community‐based participatory research approach: A Puerto Rican case. Nurse Educator, 42(4), 191–194. 10.1097/nne.0000000000000338 [DOI] [PubMed] [Google Scholar]
- McKay, M. S. , & Zakzanis, K. K. (2010). The impact of treatment on HPA axis activity in unipolar major depression. Journal of Psychiatric Research, 44(2010), 183–192. [DOI] [PubMed] [Google Scholar]
- Mead, S. , Hilton, D. , & Curtis, L. (2001). Peer support: A theoretical perspective. Psychiatric Rehabilitation Journal, 25(2), 134–141. 10.1037/h0095032 [DOI] [PubMed] [Google Scholar]
- Mein, S. A. (2020). COVID‐19 and health disparities: The reality of “the great equalizer”. Journal of General Internal Medicine, 35(8), 2439–2440. 10.1007/s11606-020-05880-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miglis, M. G. , Prieto, T. , Shaik, R. , Muppidi, S. , Sinn, D.‐I. , & Jaradeh, S. (2020). A case report of postural tachycardia syndrome after COVID‐19. Clinical Autonomic Research, 30(5), 449–451. 10.1007/s10286-020-00727-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millroth, P. , & Frey, R. (2021). Fear and anxiety in the face of COVID‐19: Negative dispositions towards risk and uncertainty as vulnerability factors. Journal of Anxiety Disorders, 83, 102454. 10.1016/j.janxdis.2021.102454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler, R. H. , Vogel, R. I. , Gollust, S. E. , Rothman, A. J. , Fowler, E. F. , & Yzer, M. C. (2020). Public perceptions of conflicting information surrounding COVID‐19: Results from a nationally representative survey of U.S. adults. PLoS One, 15(10), e0240776. 10.1371/journal.pone.0240776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York Times . (2022). Coronavirus world map: Tracking the global outbreak. The New York Times Company. Retrieved January 6 from. https://www.nytimes.com/interactive/2021/world/covid‐cases.html [Google Scholar]
- O'Neill, L. , Fraser, T. , Kitchenham, A. , & McDonald, V. (2018). Hidden burdens: A review of intergenerational, historical and complex trauma, implications for indigenous families. Journal of Child & Adolescent Trauma, 11(2), 173–186. 10.1007/s40653-016-0117-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oran, D. P. , & Topol, E. J. (2020). Prevalence of asymptomatic SARS‐CoV‐2 infection. Annals of Internal Medicine, 173(5), 362–367. 10.7326/M20-3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orphanidys, J. C. , Singer, R. , & Mukerjee, R. (2022). Racial and LGBTQIA+ microaggressions. In Mukerjee R., Wesp L., Singer R., & Menkin D. (Eds.), Clinician's guide to LGBTQIA+ care (pp. 53–68). Springer. [Google Scholar]
- Paredes, M. R. , Apaolaza, V. , Fernandez‐Robin, C. , Hartmann, P. , & Yañez‐Martinez, D. (2021). The impact of the COVID‐19 pandemic on subjective mental well‐being: The interplay of perceived threat, future anxiety and resilience. Personality and Individual Differences, 170, 110455. 10.1016/j.paid.2020.110455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perazzo, J. D. , Webel, A. R. , Voss, J. G. , & Prince‐Paul, M. (2017). Fatigue symptom management in people living with human immunodeficiency virus. Journal of Hospice and Palliative Nursing, 19(2), 127. https://journals.lww.com/jhpn/Fulltext/2017/04000/Fatigue_Symptom_Management_in_People_Living_With.5.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlmutter, A. (2021). Immunological interfaces: The COVID‐19 pandemic and depression. Frontiers in Neurology, 12, 657004. 10.3389/fneur.2021.657004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips, S. , & Williams, M. A. (2021). Confronting our next National Health Disaster—Long‐haul Covid. New England Journal of Medicine, 385(7), 577–579. 10.1056/NEJMp2109285 [DOI] [PubMed] [Google Scholar]
- Pinto, M. D. , Downs, C. A. , Lambert, N. , & Burton, C. W. (2021). How an effective response to post‐acute sequelae of SARS‐CoV‐2 infection (PASC) relies on nursing research. Research in Nursing and Health, 44(5), 743–745. 10.1002/nur.22176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto, M. D. , Downs, C. A. , Lambert, N. , & Burton, C. W. (2022). Case report: Antihistamines for post‐acute sequelae of SARS‐CoV‐2 (PASC) infection. The Journal for Nurse Practitioners, 18, 335–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proal, A. D. , & VanElzakker, M. B. (2021). Long COVID or post‐acute sequelae of COVID‐19 (PASC): An overview of biological factors that may contribute to persistent symptoms. Frontiers in Microbiology, 12, 1494. https://www.frontiersin.org/article/10.3389/fmicb.2021.698169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin, C. , Zhou, L. , Hu, Z. , Zhang, S. , Yang, S. , Tao, Y. , Xie, C. , Ma, K. , Shang, K. , Wang, W. , & Tian, D.‐S. (2020). Dysregulation of immune response in patients with coronavirus 2019 (COVID‐19) in Wuhan, China. Clinical Infectious Diseases, 71(15), 762–768. 10.1093/cid/ciaa248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth, P. H. , & Gadebusch‐Bondio, M. (2022). The contested meaning of “long COVID”—Patients, doctors, and the politics of subjective evidence. Social Science and Medicine, 292, 114619. 10.1016/j.socscimed.2021.114619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushforth, A. , Ladds, E. , Wieringa, S. , Taylor, S. , Husain, L. , & Greenhalgh, T. (2021). Long Covid—The illness narratives. Social Science and Medicine, 286, 114326. 10.1016/j.socscimed.2021.114326 [DOI] [PubMed] [Google Scholar]
- Sabatello, M. , Landes, S. D. , & McDonald, K. E. (2020). People with disabilities in COVID‐19: Fixing our priorities. The American Journal of Bioethics, 20(7), 187–190. 10.1080/15265161.2020.1779396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schei, E. , Fuks, A. , & Boudreau, J. D. (2019). Reflection in medical education: Intellectual humility, discovery, and know‐how. Medicine, Health Care and Philosophy, 22(2), 167–178. 10.1007/s11019-018-9878-2 [DOI] [PubMed] [Google Scholar]
- Sebring, J. C. H. (2021). Towards a sociological understanding of medical gaslighting in western health care. Sociology of Health and Illness, 43(9), 1951–1964. 10.1111/1467-9566.13367 [DOI] [PubMed] [Google Scholar]
- Smith, C. P. (2017). First, do no harm: Institutional betrayal and trust in health care organizations. Journal of Multidisciplinary Healthcare, 2017(10), 133–144. 10.2147/JMDH.S125885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, C. P. , & Freyd, J. J. (2014). Institutional betrayal. American Psychologist, 69(6), 575–587. [DOI] [PubMed] [Google Scholar]
- Smith, C. P. , & Freyd, J. J. (2017). Insult, then injury: Interpersonal and institutional betrayal linked to health and dissociation. Journal of Aggression, Maltreatment & Trauma, 1‐15, 1117–1131. 10.1080/10926771.2017.1322654 [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . (2014). SAMHSA's concept of trauma and guidance for a trauma‐informed approach. ([SMA] 14‐4884). Substance Abuse and Mental Health Services Administration. Retrieved from. https://store.samhsa.gov/system/files/sma14‐4884.pdf [Google Scholar]
- Tebes, J. K. , Champine, R. B. , Matlin, S. L. , & Strambler, M. J. (2019). Population health and trauma‐informed practice: Implications for programs, systems, and policies. American Journal of Community Psychology, 64(3–4), 494–508. 10.1002/ajcp.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet . (2021). Understanding long COVID: A modern medical challenge. The Lancet, 398(10302), 725. 10.1016/S0140-6736(21)01900-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, R. R. , Holman, E. A. , & Silver, R. C. (2020). Worst life events and media exposure to terrorism in a nationally representative U.S. sample. Journal of Traumatic Stress, 33(6), 984–993. 10.1002/jts.22534 [DOI] [PubMed] [Google Scholar]
- Tiwari, A. , Berekashvili, K. , Vulkanov, V. , Agarwal, S. , Khaneja, A. , Turkel‐Parella, D. , Liff, J. , Farkas, J. , Nandakumar, T. , Zhou, T. , Frontera, J. , Kahn, D. E. , Kim, S. , Humbert, K. A. , Sanger, M. D. , Yaghi, S. , Lord, A. , Arcot, K. , & Dmytriw, A. A. (2020). Etiologic subtypes of ischemic stroke in SARS‐CoV‐2 patients in a cohort of new York City hospitals. Frontiers in Neurology, 11, 1004. https://www.frontiersin.org/article/10.3389/fneur.2020.01004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). State of the world's nursing 2020: Investing in education, jobs and leadership. World Health Organization. [Google Scholar]
- World Health Organization . (2021a). https://www.who.int/publications/i/item/WHO‐2019‐nCoV‐Post_COVID‐19_condition‐Clinical_case_definition‐2021.1
- World Health Organization . (2021b). Fighting misinformation in the time of COVID‐19, one click at a time. World Health Organization. Retrieved January 6 from. https://www.who.int/news‐room/feature‐stories/detail/fighting‐misinformation‐in‐the‐time‐of‐covid‐19‐one‐click‐at‐a‐time [Google Scholar]
- Yong, S. J. (2021). Long COVID or post‐COVID‐19 syndrome: Putative pathophysiology, risk factors, and treatments. Infectious Diseases, 53(10), 737–754. 10.1080/23744235.2021.1924397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ysasi, N. , Becton, A. , & Chen, R. (2018). Stigmatizing effects of visible versus invisible disabilities. Journal of Disability Studies, 4(1), 2018. http://pubs.iscience.in/journal/index.php/jds/article/view/779 [Google Scholar]
- Ziauddeen, N. , Gurdasani, D. , O'Hara, M. E. , Hastie, C. , Roderick, P. , Yao, G. , & Alwan, N. A. (2021). Characteristics of long Covid: Findings from a social media survey. medRxiv, 2021.2003.2021.21253968. 10.1101/2021.03.21.21253968 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during development of the current work.


