Abstract
The aim of the study was to determine intention to receive Coronavirus disease‐19 (COVID‐19) vaccination in India. An integrated model of Theory of Planned behaviour (TPB) and Health Belief Model (HBM) was used. Online survey was conducted in Delhi NCR region to find out the intention to receive vaccination. Data was collected from 845 respondents during 15 February 2021–15 March 2021, just after COVID‐19 vaccination became available in the India. Partial Least Square‐Structural Equation Modelling was used to establish the relationships. The results of the analysis show that proposed framework is significant and explained 71% variance in intentions. Attitude, subjective norm, perceived behaviour control and self‐efficacy from the TPB had direct (or significant independent) effects on intention and perceived benefits, perceived susceptibility from the HBM have indirect effect on the intentions through attitude. The present study can be used to maximise the uptake of vaccination in any future pandemic. This theoretically‐driven model can be used to guide health policy makers and health care providers to increase the uptake of vaccination.
Keywords: HBM, intention to have COVID‐19 vaccination, PLS‐SEM, TPB
Highlights
An Integration of TPB and Health Belief Model (HBM) was used to find out the vaccine intention.
The proposed model explained 71% variance in intentions to have COVID‐19 vaccination.
A significant variation in vaccine intentions is noticed from the self‐efficacy, subjective norms, perceived behaviour control and attitude.
Perceived benefits and perceived susceptibility have indirect impact on intentions through attitude.
1. INTRODUCTION
In late December 2019, a new strain of COVID‐19 virus, was reported in Wuhan city of China, and very soon it spread in many countries. 1 World Health Organisation (WHO) declared COVID‐19 as a pandemic on 11 March 2020, by which time only 60 cases were reported across various states of India. Kerala, southern state of India was the state where first case of COVID‐19 was confirmed on 30 January 2020. 2 In Asia, India has reported the highest number of confirmed cases 3 and, as of 8 May 2021, worldwide, India has the second position in reported cases of COVID‐19 after USA. 4 India has detected more than 20.65 million cases in the first half of April itself. 5 On 15 April 2021, more than 2 hundred thousand cases were recorded in India and there was a significant increment in the numbers of confirmed cases with 217,353 cases on 16 April 2021. Cases of COVID‐19 were increasing significantly in first half of the month of May 2021. Slightly positive cases were going to decrease after 15 May 2021. Worldwide, the COVID‐19 illness spectrum is broad, ranging from asymptomatic infection to acute respiratory distress syndrome, culminating death. Now, in August 2021, the confirmed cases of COVID‐19 have gone decreased. COVID‐19 has significant effect on the lives of human being by effecting various sectors such as hospitality, 6 supply chain of fruits, 7 agriculture, 8 education sector 9 and mass media. 10
Now scenario has changed. According to Kaur and Gupta, 11 number of vaccine development programs had been initiated to control the spread of pandemic. As a result of these programs, a vaccination for COVID‐19 was developed and it is available for controlling the spread of pandemic. It was launched on 16 January 2021 by the Honourable Prime Minister (MOH) in India. In the first phase, the vaccination was received by the healthcare workers and frontline workers. As per the announcement of the Ministry of Health and Family Welfare that vaccination is given to the persons over 60 years and the persons between the age group 45 to 59 having comorbid conditions from 1 March 2021. Government, Medical agencies, Pharmacists etc. are continuously watching the response of vaccination. Therefore, this study focuses on the attitude and behaviour towards COVID‐19 vaccination in general.
Numerous studies 12 , 13 , 14 , 15 , 16 have been conducted on the misinformation and attitude towards the COVID‐19 vaccination. These studies were conducted in UK, China etc. Only few studies have conducted in India 14 , 15 , 17 and focussed on the willingness, acceptance to pay, benefits and threats. Earlier in the current COVID‐19 alert, study was conducted in Israel to identify the intention to receive COVID‐19 vaccination. 18 This research was related to find out the intention for COVID‐19 vaccination or influenza for all the persons including priority group and when this research was conducted, vaccine was not available.
As per the knowledge of author, limited studies have investigated the intentions of the non‐priority groups (like excluded health care workers, administrative staff (e.g., police etc.), old age persons above 60 years old) regarding the vaccination when COVID‐19 vaccination will be available for these groups. Phase II of the COVID‐19 has been started and the new strain is more powerful than the previous one. The current study was conducted with a view that COVID‐19 is a life‐threateningly serious health issue to all. Therefore, it is important to investigate predictors of intention that influence the decision to have a vaccine or not among the general population during the COVID‐19 pandemic. Thus, the current study identified the intention of non‐priority population in India to have vaccination.
In order to predict the intentions, social cognition models have been extensively used. 19 Theory of Planned Behaviour (TPB) 20 have been used to predict intention and health‐related behaviour. 19 In order to explain and predict the health behaviour, TPB is a most robust and influential social cognition. 21 , 22 , 23 HBM is also an extensively researched model of health behaviour. The assumption of HBM was belief system of a person that leads a particular behaviour. Accordingly, health actions are motivated from the degree of fear and expected reduction of fear. Health Belief Model is used with TPB to predict the intentions to receive vaccination by researchers. 18 , 24 , 25 , 26
1.1. Purpose of the study
The main objective of the present study was to investigate the intention of an individual to receive COVID‐19 vaccination. This study also aimed to find out the attitudes and beliefs of the general public (including all who have not received vaccination) towards COVID‐19 vaccination and determine the factors that affect the decision to have vaccination or not by integrating the variables of HBM and TPB.
2. THEORETICAL FRAMEWORK AND HYPOTHESES DEVELOPMENT
2.1. Theory of planned behaviour
Theory of Planned Behaviour (TPB) 20 have been extensively used to predict intention and health related behaviour. 19 It is a most robust and influential social cognition model to predict and explain the health behaviour. 21 , 22 , 23 The Theory of Planned Behaviour suggests that the behaviour of an individual can be predicted by his or her behavioural intention. There are three antecedents of the behaviour intentions to receive COVID‐19 vaccination: (a) attitude towards performing the act (such as favourable and unfavourable attitude), (b) subjective norm (perceived social pressure to perform or not to perform the act), and (c) perceived behavioural control (capacity to perform the act 20 and more variable are added continually in this model time to time as per the study requirement such as self‐efficacy. These three variables (attitude, subjective norms and perceived control) are correlated with a wide range of behavioural intentions. 27 However, under the investigation on different populations, the perceived behavioural control, subjective norms and relative effect of attitude on intention and behaviour can vary as a function of the behaviour. 19 , 20 Many studies on health‐related behaviours explained the engagement of people in certain behaviours has been guided by TPB. 27 , 28 TPB is also helpful to guide for designing of influential communications and interferences that could effectively stimulate behavioural changes. 29 , 30 Explanatory power of the TPB has exemplified to predict behavioural intention. 21 , 31 Formation of attitude, perceived behavioural control and subjective norms were fundamentally depend on the control beliefs, normative beliefs, and behavioural beliefs. 20 Beliefs of an individual about the possibility to perform the behaviour that would lead to certain results is known as behavioural control. Then, the probability that these outcomes would occur and evaluations of these outcomes (individual's favourable and unfavourable behaviour) form attitude. 32 Likewise, two aspects compose normative beliefs: (a) perceived behavioural expectations such as the expectation of a person in his or her social environment from the friends, family and other important reference groups of an individual and (b) motivation of an individual to follow these expectations. Whereas facilitating factors or obstructing factors for the behavioural performance of an individual are involved in control beliefs. Self‐efficacy (perceived difficulty and perceived confidence of a person to perform a certain behaviour) 33 and perceived control (belief of an individual about their ability to control the behaviour) are two separate factors which comprises perceived behavioural control.
2.2. Health belief model
For measuring the health behaviour, the HBM was one of the first models which was based on the health problems. It remains one of the most widely recognized conceptual frameworks of health behaviour. Health Belief Model was emerged in the 1950s. At that time modest number of medical facilities were available. 34 The assumption of HBM was belief system of a person that leads a particular behaviour. Accordingly, health actions are motivated from the degree of fear and expected reduction of fear. However, original HBM was used by the early researchers to predict the intention and behaviour towards vaccination in the USA. 24 , 25 Four variables from the HBM as perceived benefits (positive aspects related to vaccination), perceived susceptibility (threats or risk related to the vaccination), perceived barriers and perceived severity (seriousness of the condition) were included in the study. Perceived susceptibility can be defined as the subjective risk to a person from contracting a disease or a health condition. 34 The feeling of a person towards the vulnerability to a condition widely vary from each other 35 and has significant effect on the behavioural intentions. 26 Perceived severity is the degree of seriousness of the health condition. It is also the degree of emotions arise when person thinks about the disease and the type of difficulties a person believes will occur because of the given health condition. 34 The possible social consequences and medical consequences (e.g., death) both are the part of perceived severity 35 and has impact on the attitude and behaviour.
2.3. Integrated model
Health Belief Model is also used with TPB to predict the intentions to receive vaccination by researchers. 18 , 24 , 25 , 26 Although the HBM and TPB focuses on the different areas of behavioural formation but they are also related to each other. To determine the adoption of a health behaviour, the importance of self‐efficacy is recognized in both models. Both models assumes that personal control is an important factor which initiate a particular behaviour. Subjective norms of TPB might influence HBM which is responsible for health behavioural change. The current study examined the effect of subjective norms on the behavioural intentions. Another linkage between TPB and HBM is also exist on the basis of cost and benefit analysis. The conceptualisation and evaluation of attitude from the TPB is based on cost and benefit. 36 Behavioural belief is the most important factor which influence the decision of an individual to perform a particular behaviour. Thus, perceived barriers could be a part of behavioural belief that may be a factor which affect the attitude in the TPB. Therefore, the current study examines the effect of perceived barriers on attitude directly and on intentions indirectly through attitude. Behavioural prediction is reflected in this integrated model 37 However, specific skills are not required to get the COVID‐19 vaccination. Thus, more variables are not the part of this study. TPB is represented as a superior model over HBM to predict the behavioural intention in previous studies. 25 , 38 TPB and HBM are integrated by Reid and Aiken 39 along with three more models to predict the behavioural intention, on the basis of key concepts. Integrated model was also used by the Yang 26 to predict the intention to receive H1N1 vaccination. Therefore, the current study examines the applicability of TPB and HBM to predict the intention of non‐priority group to receive COVID‐19 vaccination. Figure 1 shows the conceptual relationship between variables.
FIGURE 1.
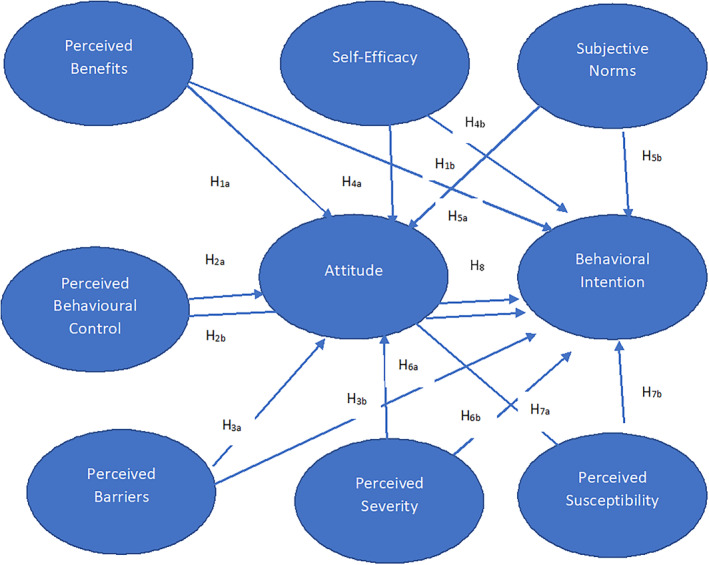
Conceptual framework
2.4. Hypotheses development
Thus, on the basis of above discussion the following hypotheses are formulated to investigate the intention to receive the COVID‐19 vaccination.
H 1a
Perceived benefits have positive effect on the attitude towards vaccination.
H 1b
Perceived benefits have positive effect on the behavioural intentions to receive vaccination.
H 2a
Perceived behaviour control have positive effect on the attitude towards vaccination.
H 2b
Perceived behaviour control have positive effect on the behavioural intentions to receive vaccination.
H 3a
Perceived barriers have positive effect on the attitude towards vaccination.
H 3b
Perceived barriers have positive effect on the behavioural intentions to receive vaccination.
H 4a
Self‐efficacy has positive effect on the attitude towards vaccination.
H 4b
Self‐efficacy has positive effect on the behavioural intentions to receive vaccination.
H 5a
Subjective norms have positive effect on the attitude towards vaccination.
H 5b
Subjective norms have positive effect on the behavioural intentions to receive vaccination.
H 6a
Perceived severity has positive effect on the attitude towards vaccination.
H 6b
Perceived severity has positive effect on the behavioural intentions to receive vaccination.
H 7a
Perceived susceptibility has positive effect on the attitude towards vaccination.
H 7b
Perceived susceptibility has positive effect on the behavioural intentions to receive vaccination.
H 8
Attitude has positive effect on the behavioural intentions to receive vaccination.
3. CONCEPTUAL FRAMEWORK
3.1. Methods
3.1.1. Participants
This study investigated intention towards the COVID‐19 vaccination in India which is a part of the international study. This research excluded the responses of vaccination priority groups such as health care workers and the persons who have taken their first dose of COVID‐19 vaccine.
3.1.2. Procedure
This is an empirical study identifies the behavioural intentions of the non‐vaccinated persons towards the intake of COVID‐19 vaccine. Survey questionnaire was prepared in this regard to collect the data. Survey instrument was prepared by using the Google forms and paper version were also prepared. Convenience sampling method was used to collect the data. Link of the Google form was sent to the respondents by using the social networking sites (e.g., Facebook, WhatsApp group). Survey link was also sent to the friends, colleagues, neighbours and relatives by using WhatsApp or e‐mail and they were also asked to send the link in their contacts to fill the form. Data collection was started from 15 February 2021, just after the availability of the COVID‐19 vaccination for health care workers and after that, MOH announced the vaccination for old age persons. Data was collected to till 15 March 2021.
3.2. Ethical considerations
In the beginning of the questionnaire, a cover page was attached. In which whole information about the purpose of survey were written. Assurance for maintaining the confidentiality of the respondent's identity were given. After reading the whole information, respondents were asked to participate in the survey. First question was related to the willingness (are you willing to participate in this survey?). if they select ‘yes’ as the response for the first question, were included in the study. Monetary incentive was not provided to the respondents, and anonymity was maintained to ensure the reliability and confidentiality of data. All the minors were not the part of the study.
4. MEASURES
Measures were drawn from the extended Theory of Planned Behaviour as self‐efficacy, perceived behavioural control, attitude, intention and subjective norms and also from the HBM as perceived barriers, perceived benefits, perceived severity and perceived susceptibility. These measures are adopted from the previous researches on HBM and TPB. 26 , 27 , 34 , 35 Demographic variables were also included in the questionnaire related to education, gender, income, age and information about the COVID‐19 vaccination.
4.1. Extended theory of planned behaviour components
All items were measured on a 5‐point rating Likert scale, unless otherwise stated. All items used to collect data are shown in Table 1.
TABLE 1.
Assessing measures with items and sources of TPB and Health Belief Model (HBM)
| Model | Measures | Items | No. of items | Source |
|---|---|---|---|---|
| TPB | Behavioural intention to receive COVID‐19 | I am planning to get the COVID‐19 vaccine this year. | 3 | Yang (2015) |
| If I will get an opportunity to get the COVID‐19 vaccine, I will try to get vaccination. | ||||
| I will put my sincere efforts to get Covid‐19 vaccine. | ||||
| Attitude towards vaccination | I feel that getting the COVID‐19 vaccine is good. | 3 | Yang (2015) | |
| I feel that getting the COVID‐19 vaccine is beneficial. | ||||
| I feel that getting the COVID‐19 vaccine is wise decision. | ||||
| Subjective norm | My family members think I should get the COVID‐19 vaccine. | 4 | Ajzen (1988) | |
| Generally speaking, I want to do what my family members think I should do. | ||||
| My close friends think I should get the COVID‐19 vaccine. | ||||
| Generally speaking, I want to do what my close friends think I should do. | ||||
| Self‐efficacy | I know just what to do to get the COVID‐19 vaccine., | 3 | Ajzen and fishbein (2005) | |
| I know how to get the COVID‐19 vaccine. It is easy for me to get the COVID‐19 vaccine if I wanted to. | ||||
| Perceived behavioural control | If I am offered a vaccine against COVID‐19, I am sure I will be vaccinated, and this decision is entirely up to me. | 1 | Shmueli (2021) | |
| Health belief model components | Perceived susceptibility: | The COVID‐19 can happen to many people, including my family, loved ones and friends. | 4 | Rosenstock (1966) |
| I Am at risk of suffering from the COVID‐19. | ||||
| The COVID‐19 can happen anytime to anyone, such as a healthy individual. | ||||
| The chance of me contracting the COVID‐19 is high. | ||||
| Perceived severity: | The COVID‐19 causes death quickly. | 4 | Becker (1984) | |
| Many people can die from the COVID‐19. | ||||
| A person who contracts the COVID‐19 will die if not treated. | ||||
| The COVID‐19 is a fatal virus. | ||||
| Perceived benefits | Taking the COVID‐19 vaccine will be effective in preventing me from contracting the virus. | 3 | Yang (2015) | |
| Taking the COVID‐19 vaccine will help to boost my body immunity in battling the virus. | ||||
| Taking the COVID‐19 vaccine will help me to save my family from infection. | ||||
| Perceived barrier | Taking the COVID‐19 vaccine will result in certain side effects to my body. | 3 | Yang (2015) | |
| My body may react adversely to the COVID‐19 vaccine. | ||||
| It is risky to take the COVID‐19 vaccine because there is high risk of side‐effects from COVID‐19 vaccination. |
Behavioural Intention to receive COVID‐19 was measured with three items. These items are used by the Yang 26 to predict the intention to get the H1N1 vaccine. These items are modified according to the current study. Five‐point rating scale is used for measuring the intention (5) anchored at ‘definitely will’ and (1) anchored at ‘definitely will not. A high score indicated a more positive intention to have a vaccination. Attitude towards Vaccination was measured using three statements. These statements are based on the behavioural beliefs which represent both experimental and instrumental attitudes suggested by Ajzen. 40 It was measured on a likert scale ranges from strongly disagree to strongly agree. Subjective norm was measured by 4 items. These items were based on the normative belief strength and motivation. 40 Self‐efficacy: Control beliefs and capacity should be used to assess self‐efficacy. 27 Thus, self‐efficacy was measured by three items. First two items were used to assess the capacity beliefs and the third item was used to assess control beliefs. Perceived Behavioural Control was measured by one item. This item was adopted from the study of Shmueli 18 on COVID‐19. Item was rated on the five‐point rating scale.
4.2. Health belief model components
Perceived Susceptibility: Rosenstock 34 suggested that susceptibility referred to one's subjective risks of contracting a disease or a health condition. Janz and Becker 35 also argued that people varied widely in their feelings of personal vulnerability to a condition. Thus, perceived susceptibility was measured by four items with one end of the scale, ‘strongly disagree’ anchored at (1) and the other end of the scale ‘strongly agree’ anchored at (5). Perceived Severity: possible social consequences and medical consequences (e.g., death) should be included to evaluate the perceived severity. 35 Therefore, it was measured with four items with (1) anchored at ‘strongly agree’ and (5) anchored at ‘strongly disagree’. Perceived Benefits: Future perceived benefits from the COVID‐19 vaccine were measured by four items. Yang 26 used these items to find out the benefits from H1N1 vaccine. These items were modified to measure the benefits from COVID‐19 vaccine. Perceived Barrier consisted of three questions for measuring the perceived barriers. These items were related to the side effects and adverse reaction from the vaccine. Yang 26 used these items to investigate the barriers in H1N1 flu vaccination. These items were modified in case of COVID‐19.
4.3. Demographic details
Participants were asked their age, gender (coded as: 1 = female, 2 = male), education status (coded as: 1 = High School, 2 = Intermediate, 3 = Diploma, 4 = Graduation, 5 = Post Graduation), family income (1 = below 250,000, 2 = 250,000–500,000, 3 = 500,000–10,00,000 and 4 = above 10,00,000). Respondents were also asked about the vaccine uptake by using the question: ‘Did you get COVID‐19 vaccine?’ This question was rated as ‘yes,’ ‘no’.’ If the respondent answered ‘yes’, they were excluded from the study. High priority groups for vaccination are excluded from the study. Initially, vaccination was offered to the health care personnel and frontline workers. Persons over 60 years of age of 1 January 2021 are included in the second group to receive COVID‐19 vaccine. Persons between 45 and 59 with comorbid conditions are also included under the second group to receive vaccination (MOH). All the persons who have taken vaccination were excluded from this study.
4.4. Data analysis
Present study was a cross‐sectional survey and data was collected through the electronic form of the questionnaire. Electronic questionnaires were imported into SPSS 23. Data processing was done through SPSS. Partial Least Square‐Structural Equation Modelling (PLS‐SEM) was used over the Covariance‐Based‐SEM (CB‐SEM) because PLS‐SEM is used to predict the key target constructs and it is not possible by using CB‐SEM. The current study's aim is to predict the attitude and behaviour towards the COVID‐19 vaccination. Hence, in this case PLS‐SEM is useful. CB‐SEM is useful in theory confirmation and theory testing but not useful in extension and exploration the existing structural theory. TPB and HBM are existing models and integration of these are examined in this study. Thus, PLS‐SEM is best method to analyse the data. PLS‐SEM can provide best results on small sample size and CB‐SEM requires large sample. One construct in the current study has only one item and CB‐SEM cannot be applied in this case. Therefore, finally, the analyses of the data were performed using Smart‐PLS. First, measurement model was analysed. After that the structural model was analysed.
4.5. Participants characteristics
Total 845 responses collected from the respondents. Among them only 818 responses were used in the present study. Remaining were not matching with the aims of the study. Demographic description of these respondents was as follows: on the basis of age groups; 304 (37.3%) respondents were below 20 years, 320 (39.3%) respondents were in the age group 20–30, 145 (17.8%) respondents were 41–50 years old, 51–60 years old persons were only 4 (0.5%) and above 60 years were only 8 (1%) respondents. The classification on the basis of gender was as 484 (59.4%) male and 331 (40.6%) female participants. Area wise classification were as follows: 131 (15.8%) respondents from the rural area, 213 (26.1%) respondents from the semi urban area and 474 (58.2%) respondents from the urban area participated in the study. On the basis of their education status; 37 (4.6%) respondents have completed high school, 101 (12.4%) have completed intermediate, 13 (1.6%) have done diploma, 440 (54.2) respondents have done graduation, 221 (27%) participants have completed post‐graduation. On the basis of income groups 404 (49.6%) respondents were having up to 250,000 Rupees per annum income, 254 (31.2%) participants have 250,000–500,000 per annum income, 92 (11.2%) respondents fall under the category 500,000–10,00,000 Rupees per annum income and 65 (8%) have more than 10,00,000 Rupees income per year.
Correlation between the variables of TPB and HBM were calculated by using SPSS and it is clear from the Table 2 correlation between these variables were significant.
TABLE 2.
Correlation between the items
| Int1 | Int2 | Int3 | Att1 | Att2 | Att3 | SN1 | SN2 | SN3 | SN4 | SE1 | SE2 | SE3 | PS1 | PS2 | PS3 | PS4 | PSEV1 | PSEV2 | PSEV3 | PSEV4 | PBN1 | PBN2 | PBN3 | PBR1 | PBR3 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Int1 | 1 | 0.781* | 0.700* | 0.631* | 0.648* | 0.583* | 0.688* | 0.590* | 0.533* | 0.518* | 0.442* | 0.285* | 0.249* | 0.284* | 0.354* | 0.533* | 0.251* | 0.264* | 0.245* | 0.329* | 0.266* | 0.462* | 0.481* | 0.580* | 0.253* | 0.270* |
| Int2 | 1 | 0.770* | 0.667* | 0.678* | 0.630* | 0.689* | 0.629* | 0.535* | 0.500* | 0.450* | 0.269* | 0.259* | 0.320* | 0.421* | 0.535* | 0.275* | 0.290* | 0.299* | 0.329* | 0.296* | 0.456* | 0.556* | 0.558* | 0.318* | 0.278* | |
| Int3 | 1 | 0.725* | 0.740* | 0.674* | 0.660* | 0.618* | 0.484* | 0.431* | 0.405* | 0.251* | 0.206* | 0.249* | 0.395* | 0.484* | 0.300* | 0.159* | 0.294* | 0.314* | 0.297* | 0.467* | 0.533* | 0.575* | 0.332* | 0.186* | ||
| Att1 | 1 | 0.810* | 0.703* | 0.645* | 0.569* | 0.502* | 0.459* | 0.425* | 0.275* | 0.244* | 0.313* | 0.369* | 0.502* | 0.361* | 0.127* | 0.292* | 0.241* | 0.303* | 0.501* | 0.599* | 0.597* | 0.329* | 0.224* | |||
| Att2 | 1 | 0.764* | 0.677* | 0.569* | 0.487* | 0.477* | 0.427* | 0.300* | 0.205* | 0.297* | 0.431* | 0.487* | 0.403* | 0.160* | 0.349* | 0.350* | 0.318* | 0.522* | 0.649* | 0.652* | 0.322* | 0.202* | ||||
| Att3 | 1 | 0.623* | 0.567* | 0.552* | 0.489* | 0.471* | 0.361* | 0.317* | 0.344* | 0.416* | 0.552* | 0.372* | 0.151* | 0.334* | 0.364* | 0.335* | 0.519* | 0.604* | 0.627* | 0.384* | 0.244* | |||||
| SN1 | 1 | 0.688* | 0.686* | 0.600* | 0.487* | 0.403* | 0.342* | 0.290* | 0.377* | 0.686* | 0.278* | 0.261* | 0.287* | 0.305* | 0.358* | 0.490* | 0.496* | 0.568* | 0.339* | 0.312* | ||||||
| SN2 | 1 | 0.614* | 0.667* | 0.499* | 0.372* | 0.410* | 0.290* | 0.412* | 0.614* | 0.444* | 0.197* | 0.265* | 0.306* | 0.345* | 0.452* | 0.460* | 0.520* | 0.230* | 0.312* | |||||||
| SN3 | 1 | 0.672* | 0.412* | 0.278* | 0.368* | 0.271* | 0.315* | 0.431* | 0.285* | 0.257* | 0.276* | 0.245* | 0.336* | 0.465* | 0.354* | 0.454* | 0.294* | 0.271* | ||||||||
| SN4 | 1 | 0.558* | 0.444* | 0.476* | 0.268* | 0.332* | 0.416* | 0.269* | 0.285* | 0.235* | 0.310* | 0.293* | 0.368* | 0.312* | 0.442* | 0.170* | 0.419* | |||||||||
| SE1 | 1 | 0.676* | 0.525* | 0.266* | 0.263* | 0.377* | 0.251* | 0.230* | 0.186* | 0.285* | 0.328* | 0.345* | 0.276* | 0.339* | 0.391* | 0.441* | ||||||||||
| SE2 | 1 | 0.652* | 0.255* | 0.266* | 0.412* | 0.275* | 0.157* | 0.236* | 0.240* | 0.292* | 0.256* | 0.209* | 0.255* | 0.361* | 0.500* | |||||||||||
| SE3 | 1 | 0.281* | 0.194* | 0.315* | 0.300* | 0.233* | 0.245* | 0.217* | 0.313* | 0.259* | 0.225* | 0.237* | 0.305* | 0.636* | ||||||||||||
| PS1 | 1 | 0.408* | 0.332* | 0.361* | 0.299* | 0.269* | 0.218* | 0.251* | 0.393* | 0.310* | 0.329* | 0.318* | 0.255* | |||||||||||||
| PS2 | 1 | 0.263* | 0.403* | 0.196* | 0.338* | 0.298* | 0.326* | 0.375* | 0.320* | 0.404* | 0.313* | 0.260* | ||||||||||||||
| PS3 | 1 | 0.401* | 0.218* | 0.381* | 0.261* | 0.334* | 0.467* | 0.289* | 0.245* | 0.262* | 0.521* | |||||||||||||||
| PS4 | 1 | 0.412* | 0.248* | 0.327* | 0.223* | 0.334* | 0.467* | 0.221* | 0.256* | 0.273* | ||||||||||||||||
| PSEV1 | 1 | 0.371* | 0.424* | 0.230* | 0.257* | 0.216* | 0.295* | 0.224* | 0.266* | |||||||||||||||||
| PSEV2 | 1 | 0.444* | 0.541* | 0.393* | 0.376* | 0.394* | 0.299* | 0.168* | ||||||||||||||||||
| PSEV3 | 1 | 0.513* | 0.392* | 0.354* | 0.454* | 0.169* | 0.211* | |||||||||||||||||||
| PSEV4 | 1 | 0.384* | 0.352* | 0.376* | 0.286* | 0.211* | ||||||||||||||||||||
| PBN1 | 1 | 0.531* | 0.632* | 0.451* | 0.190* | |||||||||||||||||||||
| PBN2 | 1 | 0.706* | 0.359* | 0.191* | ||||||||||||||||||||||
| PBN3 | 1 | 0.351* | 0.220* | |||||||||||||||||||||||
| PBR1 | 1 | 0.476* | ||||||||||||||||||||||||
| PBR2 | 1 |
* significant at 5% level of significance (p < 0.05).
4.6. Smart‐PLS
PLS‐SEM produces a precise and significant relationship between the variables. 41 The path models of the PLS are generally defined by two sets of the linear equations. The first set is known as the measurement model and the second set is known as a structural model. 42
4.7. Measurement model analysis
A measurement model analysis determines these relationships, and this condition is required to obtain the rewarding results from PLS‐SEM. According to Hair et al., 41 the validity and reliability of the constructs depend on the measurement models.
4.8. Common method bias and multicollinearity
Common method bias is well known problem specially occur in survey research and because of the many reasons like: when estimates are measured with same method, 43 cross sectional data, response tendencies, dispositional mood states, socially desirable tendencies and so on. 44 , 45 In this study, the problem of common method bias was treated by using both procedural and statistical approaches. 44 Research purpose was clearly mentioned in the beginning of the questionnaire, proper numbering and levels were assigned to the scale items. Questions were very concise and simple and double meaning questions were avoided. Statistically, after collection of the data, Harman's single factor test was applied by using SPSS to check the common method bias. 46 Result of which showed that total variance explained value is 37.7% which means there is no problem of common method bias for this study. The problem of multicollinearity was another issue. The value of VIF (Variance Inflationary Factor) should be less than 5. 47 In current study all values of VIF were less than 3.3 48 except second item of attitude. For attitude two, it was 3.7 which is acceptable. 47
4.9. Internal consistency reliability
Scale reliability is considered as internal consistency reliability. Inter‐correlation's degree between the scale items is referred to internal consistency. 49 Cronbach's alpha was used to check the reliability. The value of which should be greater than 0.6. 41 , 49 From the Table 3 all constructs are reliable, having cronbach's alpha value more than 0.7 except perceived barriers. It is 0.684 and it is acceptable. 50 SEM based composite reliability is another measure to check the reliability of the scale. 51 Interpretation of these measures are same. The value of composite reliability should be more than 0.6 and less than 0.9. 41 Table 3 shows the results of composite reliability. All values of composite reliability are more than 0.6 and less than 0.9. It means scale was reliable. Figure 2 shows the results of outer loadings which are acceptable.
TABLE 3.
Results of cronbach's alpha and composite reliability
| Constructs | Cronbach's alpha | Composite reliability |
|---|---|---|
| Perceived barriers | 0.657 | 0.849 |
| Perceived benefits | 0.841 | 0.868 |
| Perceived susceptibility | 0.816 | 0.896 |
| Attitude | 0.913 | 0.898 |
| Self‐efficacy | 0.834 | 0.897 |
| Subjective norms | 0.884 | 0.882 |
| Perceived severity | 0.747 | 0.840 |
| Behavioural intention | 0.897 | 0.898 |
FIGURE 2.
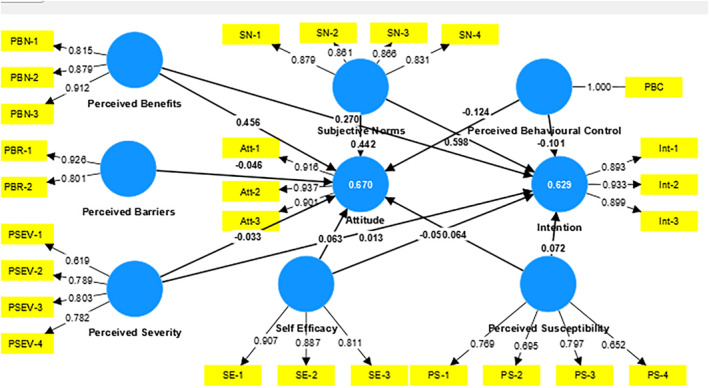
Model showing the values of outer loadings and R 2
4.10. Validity analysis
Validity was measured in the forms of convergent validity and discriminant validity.
4.10.1. Convergent validity
Average Variance Extracted (AVE), outer loadings and indicator reliability of the indicators were used to check the convergent validity. 41 According to Fornell and Larcker, 52 average variance is obtained by a construct from its indicators relative to the amount due to measurement errors. The threshold value of AVE is 0.5. 41 Thus, it should be more than 0.5, which means on an average more than half of the construct's variance is explained by the indicators of that construct. Table 4 showed the results of indicator reliability, outer loadings and AVE. Outer loadings of the all items are more than the threshold value 0.7. Indicator reliability for all items were more than 0.5. Thus, it showed all indicators were reliable. The values of AVE were also more than 0.5. It is also satisfying the threshold requirement.
TABLE 4.
Results of outer loadings, indicator reliability and average variance extracted (AVE)
| Latent variable | Indicators | Loadings | Indicator reliability | AVE |
|---|---|---|---|---|
| >0.70 | >0.50 | >0.50 | ||
| Perceived barriers | PBR1 | 0.915 | 0.83 | 0.738 |
| PBR2 | 0.800 | 0.64 | ||
| Perceived benefits | PBN1 | 0.815 | 0.65 | 0.759 |
| PBN2 | 0.880 | 0.77 | ||
| PBN3 | 0.915 | 0.83 | ||
| Perceived susceptibility | PSUS1 | 0.955 | 0.90 | 0.837 |
| PSUS2 | 0.873 | 0.75 | ||
| Attitude | Attitude1 | 0.922 | 0.64 | 0.852 |
| Attitude2 | 0.942 | 0.88 | ||
| Attitude3 | 0.904 | 0.81 | ||
| Self‐efficacy | SE1 | 0.907 | 0.81 | 0.744 |
| SE2 | 0.879 | 0.75 | ||
| SE3 | 0.798 | 0.62 | ||
| Subjective norms | SN1 | 0.882 | 0.77 | 0.741 |
| SN2 | 0.865 | 0.73 | ||
| SN3 | 0.864 | 0.73 | ||
| SN4 | 0.832 | 0.68 | ||
| Perceived severity | PSEV1 | 0.712 | 0.50 | 0.569 |
| PSEV2 | 0.772 | 0.59 | ||
| PSEV3 | 0.815 | 0.65 | ||
| PSEV4 | 0.778 | 0.59 | ||
| Behavioural intention | Int1 | 0.893 | 0.79 | 0.829 |
| Int2 | 0.931 | 0.86 | ||
| Int3 | 0.907 | 0.81 |
4.10.2. Discriminant validity
Hulland 53 states that the degree to which a construct is different from the other constructs is known as discriminant validity. It was assessed by Fornell‐Larcker criterion, cross‐loading and HTMT ratio.
4.11. Cross loadings
The correlation of indicator with other constructs is known as cross‐loadings. According to Hair et al., 41 the value of indicators outer loading with their constructs should be greater than any of its cross loadings. The highlighted value of indicator in Table 5 with their constructs were greater than other of its cross loadings.
TABLE 5.
Results of cross loadings
| Attitude | Behavioural intention | Perceived barriers | Perceived benefits | Perceived severity | Perceived behavioural control | Perceived susceptibility | Self‐efficacy | Subjective norms | |
|---|---|---|---|---|---|---|---|---|---|
| Att1 | 0.922 | 0.759 | 0.339 | 0.645 | 0.325 | 0.402 | 0.100 | 0.415 | 0.661 |
| Att2 | 0.942 | 0.767 | 0.328 | 0.668 | 0.386 | 0.434 | 0.126 | 0.417 | 0.671 |
| Att3 | 0.904 | 0.713 | 0.389 | 0.660 | 0.396 | 0.470 | 0.126 | 0.483 | 0.674 |
| Int1 | 0.673 | 0.893 | 0.303 | 0.526 | 0.361 | 0.439 | 0.135 | 0.412 | 0.675 |
| Int2 | 0.740 | 0.932 | 0.351 | 0.590 | 0.405 | 0.470 | 0.082 | 0.435 | 0.715 |
| Int3 | 0.792 | 0.906 | 0.334 | 0.609 | 0.369 | 0.382 | 0.059 | 0.379 | 0.671 |
| PBN1 | 0.526 | 0.469 | 0.347 | 0.815 | 0.424 | 0.406 | 0.085 | 0.297 | 0.474 |
| PBN2 | 0.660 | 0.572 | 0.311 | 0.880 | 0.440 | 0.359 | 0.152 | 0.286 | 0.495 |
| PBN3 | 0.663 | 0.602 | 0.341 | 0.915 | 0.499 | 0.429 | 0.179 | 0.327 | 0.566 |
| PBR1 | 0.390 | 0.354 | 0.915 | 0.398 | 0.294 | 0.375 | 0.084 | 0.421 | 0.331 |
| PBR2 | 0.244 | 0.257 | 0.800 | 0.230 | 0.240 | 0.377 | 0.278 | 0.577 | 0.369 |
| PSUS1 | 0.135 | 0.111 | 0.198 | 0.171 | 0.285 | 0.349 | 0.955 | 0.270 | 0.189 |
| PSUS2 | 0.089 | 0.060 | 0.130 | 0.118 | 0.278 | 0.283 | 0.873 | 0.218 | 0.168 |
| PCB | 0.366 | 0.345 | 0.357 | 0.350 | 0.317 | 0.760 | 0.184 | 0.359 | 0.366 |
| PSEV1 | 0.148 | 0.249 | 0.212 | 0.290 | 0.647 | 0.392 | 0.211 | 0.220 | 0.283 |
| PSEV2 | 0.334 | 0.292 | 0.257 | 0.398 | 0.778 | 0.329 | 0.223 | 0.221 | 0.287 |
| PSEV3 | 0.313 | 0.335 | 0.178 | 0.434 | 0.815 | 0.279 | 0.204 | 0.247 | 0.317 |
| PSEV4 | 0.377 | 0.362 | 0.296 | 0.435 | 0.768 | 0.362 | 0.279 | 0.367 | 0.420 |
| SE1 | 0.510 | 0.497 | 0.473 | 0.367 | 0.327 | 0.380 | 0.207 | 0.907 | 0.599 |
| SE2 | 0.361 | 0.318 | 0.470 | 0.247 | 0.282 | 0.352 | 0.247 | 0.879 | 0.463 |
| SE3 | 0.302 | 0.287 | 0.521 | 0.255 | 0.313 | 0.366 | 0.273 | 0.798 | 0.475 |
| SN1 | 0.722 | 0.750 | 0.369 | 0.575 | 0.398 | 0.447 | 0.129 | 0.511 | 0.882 |
| SN2 | 0.617 | 0.669 | 0.335 | 0.526 | 0.374 | 0.430 | 0.155 | 0.542 | 0.865 |
| SN3 | 0.603 | 0.608 | 0.335 | 0.500 | 0.383 | 0.447 | 0.158 | 0.450 | 0.864 |
| SN4 | 0.523 | 0.539 | 0.328 | 0.401 | 0.354 | 0.434 | 0.253 | 0.599 | 0.832 |
Note: The bold values are greater than the values of other constructs’ outer loading.
4.12. Fornell and Larcker criterion
According to Fornell and Larcker, 52 the square root of the AVE values with the correlations of the latent variable is compared under the Fornell‐Larcker. From the Table 6, it is clear that the square root of the diagonal value is higher than from the other off‐diagonal values of the constructs.
TABLE 6.
Results of Fornell‐Larcker criterion
| Attitude | Behavioural intention | Perceived barriers | Perceived benefits | Perceived severity | Perceived behaviour control | Perceived susceptibility | Self‐efficacy | Subjective norms | |
|---|---|---|---|---|---|---|---|---|---|
| Attitude | 0.923 | ||||||||
| Behavioural intention | 0.809 | 0.911 | |||||||
| Perceived barriers | 0.381 | 0.363 | 0.859 | ||||||
| Perceived benefits | 0.712 | 0.633 | 0.380 | 0.871 | |||||
| Perceived severity | 0.400 | 0.416 | 0.314 | 0.523 | 0.755 | ||||
| Perceived behaviour control | 0.472 | 0.472 | 0.432 | 0.455 | 0.445 | 1.00 | |||
| Perceived susceptibility | 0.127 | 0.099 | 0.187 | 0.163 | 0.306 | 0.350 | 0.915 | ||
| Self‐efficacy | 0.474 | 0.449 | 0.557 | 0.348 | 0.357 | 0.423 | 0.271 | 0.863 | |
| Subjective norms | 0.724 | 0.754 | 0.398 | 0.589 | 0.439 | 0.510 | 0.196 | 0.606 | 0.861 |
Note: The bold values are higher than from the other off‐diagonal values.
4.13. HTMT ratio
Henseler et al. 54 defined HTMT as it is the ratio between trait correlations to the within trait correlations. The results of the HTMT ratio are shown in Table 7. The threshold value for the HTMT ratio is 0.85 54 and if the construct is conceptually very similar in the path model than 0.90 threshold value is suggested by the Henseler et al. 54 Table 7 show that HTMT ratio for all constructs are less than 0.9.
TABLE 7.
Results of HTMT ratio
| Attitude | Behavioural intention | Perceived barriers | Perceived benefits | Perceived severity | Perceived behaviour control | Perceived susceptibility | Self‐efficacy | Subjective norms | |
|---|---|---|---|---|---|---|---|---|---|
| Attitude | |||||||||
| Behavioural intention | 0.892 | ||||||||
| Perceived barriers | 0.475 | 0.460 | |||||||
| Perceived benefits | 0.808 | 0.722 | 0.492 | ||||||
| Perceived severity | 0.470 | 0.501 | 0.441 | 0.649 | |||||
| Perceived behaviour control | 0.527 | 0.542 | 0.605 | 0.549 | 0.164 | ||||
| Perceived susceptibility | 0.141 | 0.111 | 0.275 | 0.185 | 0.390 | 0.454 | |||
| Self‐efficacy | 0.518 | 0.491 | 0.794 | 0.400 | 0.441 | 0.532 | 0.332 | ||
| Subjective norms | 0.797 | 0.836 | 0.531 | 0.672 | 0.532 | 0.611 | 0.236 | 0.694 | |
Note: The bold values are showing the result. All values are lesser than 0.9.
4.14. Structural equation modelling
To examine the predictive capability of the model and research constructs relations, structural model is evaluated. The results of the structural model are shown in Figure 3. The structural model is assessed using the significance of the path coefficients (β), the level of R 2 (coefficient of determination), f 2 (Effect size), Q 2 (Predictive relevance of the model). 5000‐sample bootstrapping is used to analyse the model. 55 Table 8 shows the results of R 2, f 2 and Q 2. The R 2 values 0.25, 0.50 and 0.75 are interpreted as low, moderate and high respectively. 57 The values of R 2 for attitude and intention to receive vaccination were 0.67 and 0.71 respectively (Figure 2). The values of R 2 were greater than 0.5 which showed integrated model has moderate predicting power. Integrated model was fit as model fit indices showed the model fitness. The value of Chi‐square was more than 0.5 (1321.29), the value of Normative Fit Index was 0.75 and the square root mean residual was less than 0.08 (0.07). These values showed the fitness of integrated model. The effect size of each exogenous latent construct on the endogenous latent construct was measured through f 2. Large, medium and small effect sizes were termed when the values of f 2 were 0.35, 0.15 and 0.02 respectively. Perceived benefits have large effect on the attitude and perceived barriers has medium effect and remaining variables have small effect on the attitude. Subjective norms have large effect on the intention to receive vaccination and others have small effect on the intention to receive vaccination. Predictive relevance of the model is measured through Q 2. The values of Q 2 for attitude and intention are shown in Figure 4 which are more than zero which shows the predictive relevance of the model. 41
FIGURE 3.
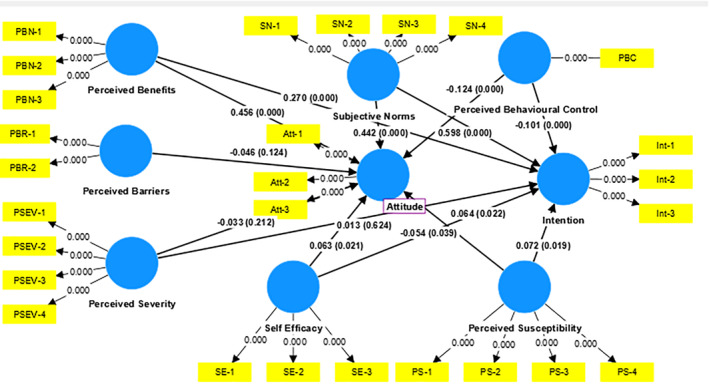
Structural model analysis
TABLE 8.
Results of R 2, f 2 and Q 2
| Construct | R 2 | f 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Attitude | Perceived barriers | Perceived benefits | Perceived behavioural control | Perceived severity | Perceived susceptibility | Subjective norms | Self‐efficacy | Q 2 | ||
| Attitude | 0.67 | 0.004 | 0.338 | 0.038 | 0.002 | 0.008 | 0.261 | 0.006 | 0.560 | |
| Intention to receive vaccination | 0.715 | 0.299 | 0.001 | 0.003 | 0.006 | 0.002 | 0.004 | 0.169 | 0.010 | 0.583 |
Note: The bold values are showing the results.
FIGURE 4.
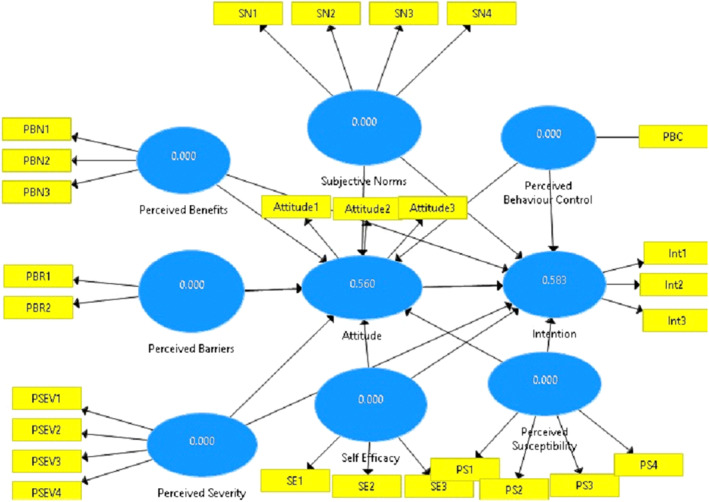
Results of Q2 (Predictive relevance)
4.15. Results of hypotheses testing
Results of the Integrated model show that perceived benefits have positive effect on the attitude towards vaccination (β = 0.46, p < 0.01). Thus, hypothesis 1a was accepted. As if people feel that the intake of vaccination is useful in curbing and controlling the spread of COVID‐19, this concept changes the attitude towards vaccination. Simultaneously, perceived benefits do not have direct effect on the intention to receive vaccination. The relationship between these two variables was insignificant (β = 0.043, ns). Thus, hypothesis 1b was not supported. Second hypothesis 2a investigated the relationship between perceived behaviour control and attitude. The relationship between theses variables were not significant (β = −0.124, p < 0.01) but the relationship between perceived behavioural control and intention to receive vaccination was significant (β = −0.045, p < 0.05). Thus, self‐decision to be vaccinated has significant impact on the intention to receive COVID‐19 vaccination. Third hypothesis investigated the relationship between perceived barriers and attitude. The relationship was insignificant (β = −0.045, ns). Therefore, hypothesis 3a was not accepted. The relationship between perceived barriers and intention to have COVID‐19 vaccination was not significant (β = 0.003, ns). Thus, hypothesis 3b was not supported. Forth hypothesis investigated the relationship between self‐efficacy and attitude. The relationship was significant (β = 0.077, p < 0.01) at 5% level of significance. Self‐efficacy also has significant effect on the intention to receive vaccination. Therefore, Hypotheses 4a and 4b accepted. The relationship of subjective norms with attitude (β = 0.442, p < 0.01) and intention to receive vaccination (β = 0.372, p < 0.01) were significant. Thus, hypothesis five was accepted. Subjective norms play a significant role in behavioural intentions. Sixth hypothesis examined the relationship of perceived severity with attitude and intention to have COVID‐19 vaccination. Perceived severity has not significant relationship with attitude and intention to receive vaccination. Thus, hypotheses were not significant (β = 0.05, ns). The relationship between perceived susceptibility and attitude examined in hypothesis 7a. The relationship was significant (β = 0.064, p < 0.05). perceived susceptibility has not significant impact on intentions to have COVID‐19 vaccination (β = 0.044, p < 0.05). Therefore, the perceived susceptibility and intention to have COVID‐19 vaccination was not significantly related. Last hypothesis (H8) investigated the relationship between attitude and intention to have COVID‐19 vaccination and it is found that relationship was significant (β = 0.512, p < 0.01). Therefore, hypothesis eight accepted. Results of the hypotheses are shown in Table 9.
TABLE 9.
Results of hypotheses testing
| Hypotheses | Path coefficients | p ‐value | T ‐statistics | Supported/Not supported |
|---|---|---|---|---|
| H1a:: Perceived benefits→ | 0.456** | 0.000 | 13.00 | Supported |
| Attitude towards vaccination | ||||
| H1b: Perceived benefits→ | 0.043 | 0.168 | 1.37 | Not supported |
| Intention to receive vaccination | ||||
| H2a: Perceived behavioural control→ | −0.124** | 0.000 | 4.83 | Supported |
| Attitude towards vaccination | ||||
| H2b: Perceived behavioural control→ | −0.045* | 0.03 | 2.176 | Supported |
| Intention to receive vaccination | ||||
| H3a: Perceived barriers→ | −0.048 | 0.168 | 0.108 | Not supported |
| Attitude towards vaccination | ||||
| H3b: Perceived barriers→ | 0.003 | 0.887 | 0.142 | Not supported |
| Intention to receive vaccination | ||||
| H4a: Self‐efficacy→ | 0.063* | 0.02 | 2.32 | Supported |
| Attitude towards vaccination | ||||
| H4b: Self‐efficacy→ | 0.077** | 0.003 | 2.97 | Supported |
| Intention to receive vaccination | ||||
| H65a: Subjective norms→ | 0.442** | 0.000 | 11.7 | Supported |
| Attitude towards vaccination | ||||
| H5b: Subjective norms→ | 0.372** | 0.000 | 8.43 | Supported |
| Intention to receive vaccination | ||||
| H6a: Perceived severity→ | −0.034 | 0.197 | 1.29 | Not supported |
| Attitude towards vaccination | ||||
| H6b: Perceived severity→ | 0.032 | 0.178 | 1.34 | Not supported |
| Intentions to receive vaccination | ||||
| H7a: Perceived susceptibility→ | 0.064* | 0.025 | 2.248 | Supported |
| Attitude towards vaccination | ||||
| H7b: Perceived susceptibility→ | 0.044 | 0.136 | 1.49 | Not supported |
| Intentions to receive vaccination | ||||
| H8: Attitude→ | 0.512** | 0.000 | 12.74 | Supported |
| Intention to receive vaccination |
* Significant at 5% level of significance (p < 0.05) and ** significant at 1% level of significance (p < 0.01).
4.16. Mediation analysis
Perceived benefits and the intention to have COVID‐19 vaccination were not directly related but the indirect effect of perceived benefits on intention to receive vaccination through attitude is significant (β = 0.232, p < 0.01) at 1% significant level. Thus, mediation exists between perceived benefits and intention to have COVID‐19 vaccination. Mediation effect also exists between perceived behavioural control and intention to have COVID‐19 vaccination. Perceived behavioural control and the intention to receive vaccination were not directly related but the indirect effect of perceived behavioural control on intention to have COVID‐19 vaccination though attitude was significant (p = 0.000) at 1% level of significance. Mediation effect between susceptibility and intention to receive vaccination was also significant (β = 0.032, p < 0.05). Perceived susceptibility does not have direct impact on intentions but indirectly through attitude perceived susceptibility has significant on intentions to receive vaccination. Self‐efficacy is also had significant (β = 0.032, p < 0.01) indirect effect on the intention through attitude. Mediation also exists between subjective norms and intention through attitude (β = 0.225, p < 0.01).
5. DISCUSSION
The present research was carried out to find out the factors that affect the intentions to receive vaccination. During the COVID‐19 pandemic, encouraging the uptake of COVID‐19 vaccination is necessary. This is similar to interventions for improving intake of ordinary vaccination of influenza 56 and other vaccinations. This study is a combination of an extended Theory of planned Behaviour and HBM to predict the behavioural intentions of the non‐priority groups to receive COVID‐19 vaccination which explained 71% variation in the behavioural intention. Sharun et al. 57 conducted a study on COVID‐19 vaccination acceptance rate in India and reported that the COVID‐19 vaccination acceptance rate is 86.3% and the factors which affect the Covid‐19 vaccination intensions among the college students were identified. 15 Dror et al. 58 reported the vaccination acceptance rate in Israel and it was 75% which was lesser than India. Reiter et al. 59 also demonstrated the same results in United States. Accordingly, in United States 69% participants were willing to take COVID‐19 vaccination whereas the findings of Wong et al. 60 showed that 48% participants will definitely get COVID‐19 Vaccination. Thus, the current research is fruitful to analyse the predictors of the vaccination uptake during COVID‐19 pandemic and current framework provide a base to increase the uptake of vaccination in future interventions.
In this study, many variables are examined to predict the intention to receive the COVID‐19 vaccination. Some of the variables from the present study were not previously used by the researchers to predict the behavioural intentions towards vaccination. These include demographic variables and health related variables. The majority of sample was collected from the adult population from the Delhi NCR and UP west region because it consists many good educational institutions and corporates. Thus, people come from different places to get job and education in Delhi NCR. The educated population are first adopter of the vaccination. Therefore, educated population were the main target for the study because their intention to receive vaccination is also very important.
The theoretical model of the present study was to use TPB model which is a widely used model to predict the intentions to perform a certain behaviour. Simultaneously, this research also used the HBM. Results showed that the integrated model was significant to predict the intentions. Perceived benefits and perceived severity were the most important variable drawn from the HBM to identify the behavioural intentions.
The results showed that intention to receive vaccination is significantly affected by the perceived benefits, self‐efficacy, perceived behavioural control, attitude, subjective norms and perceived susceptibility. Among them perceived benefits and perceived behavioural control are not directly related with intentions but indirectly these variables are having significant effect on the intentions through attitude. As Goruntla et al., 17 stated in their study that knowledge about perceived benefits can form positive attitude towards vaccination. Perceived behavioural control also forms the attitude towards vaccination. 14 Thus, these two variables (perceived benefits and perceived behavioural control) have indirect significant effect on the intentions to receive vaccination through attitude towards vaccination. Hence, these variables are important for forming the attitude and then effect the intentions towards vaccination. Perceived barriers do not have significant effect on the attitude and intention towards vaccination. This result is similar to the Malaysian study 60 where perceived barrier has lower impact on the intention to receive vaccination.
The variables like attitude and subjective norms from the original Theory of Planned Behaviour have significant effect on intentions. 14 Subjective norms play a great role in developing the intention. Respondent's intent to be vaccinated when they heard a positive word of mouth from the friends and family members and opinion of family and friends about the benefits of COVID‐19 vaccination affect the intention to receive vaccination. Similarly, the effect of self‐efficacy on the behavioural intentions was significant. It is similar to the previous studies. 61 , 62 The ability and understanding how to get vaccination has significant impact on of intention and mindfulness intervene the self‐efficacy. 63 Perceived behavioural control was associated with intention to receive vaccination indirectly through attitude. It is similar to the previous study conducted in Israel 18 where the relationship between perceived behavioural control and intention towards vaccination was significant. However, the effect of perceived control on the behavioural intention was also significant in case of the H1N1 flu. 26
Perceived severity was not significantly related with the intention to receive COVID‐19 vaccination but perceived susceptibility was significantly related to the intention to receive COVID‐19 vaccination through attitude. Perceived susceptibility refers to the perception of an individual to be infected by diseases whereas perceived severity refers to the perception of threat. Hence, if perceived threats and susceptibility increase like fear from the side effects of the vaccination than the intention to receive vaccination will decrease. Perceived threats will reduce the likelihood of getting the COVID‐19 vaccination and also stop the candidate to perform the desirable behaviour.
6. IMPLICATIONS OF THE STUDY
6.1. Managerial and academic implications
The current study provides a theoretical framework which is based on the extended TPB and HBM. This framework is useful to identify the determinants which influence the decision towards the vaccination uptake. Considering a large part of the world's population is non‐vaccinated and major thrust has been on providing vaccination to the entire population. Thus, the present theoretical driven model has been implication against this. The findings of the study are particularly useful for countries having similar socio‐economic, institutional and regulatory settings. The implications of this research are also useful in academics to determine the factors which can create an intention to receive vaccination. Academicians can utilise the same model for further research on the similar topics. Integration of two model (TPB and HBM) can provide the significant results and can be used as the benchmark for further studies.
6.1.1. Practical implications
This model can guide health policy makers and health care providers to increase the uptake of vaccination. This theoretical framework is also useful to determine the factors that influence decisions to receive vaccination to curb the spread of COVID‐19. This study can be applied to identify the intention towards booster dose of COVID‐19 Vaccination. Government can utilise this framework to enhance the uptake of booster dose. This study states that attitude has positive effect on the intentions. Attitude can be made by benefits, self‐efficacy, perceived susceptibility and subjective norms. Policy makers can focus on these variables to increase the intentions to receive vaccination like: awareness about the benefits and spread the knowledge about the centres and methods (where and how vaccination can take place) can be used to increase the uptake of vaccination. An opinion of the family and friends also have significant impact on the intentions. Perceived susceptibility also has impact on the intentions. Public awareness programs should take care of these factors. Thus, future pandemic vaccination uptake can be increase by theoretically‐driven applications.
6.2. Limitations
In this research intention of an individual was examined as a behaviour expectation, actual behaviour in the form of commitment to perform (or not perform) the behaviour was not a part of the study. 60 However, vaccine is available for priority groups or the persons above 60 years old or above. In this study behavioural aspects of the people have been taken. Model should be controlled by socio‐demographic variables. Religious belief about vaccination should be considered. Due to pandemic crisis, data was collected using convenience sampling mostly from personal contacts and social networking sites through online mode because there were movement restriction and social distancing issues. Hence, it may cause selection bias. Data was collected from NCR and western UP mainly. Therefore, findings of the research may not represent entire population.
7. CONCLUSIONS
Theoretical framework explained the factors which influence the decision of an individual to receive vaccination. This study is useful for the researchers, health policy makers and the persons who are involved in the planning for vaccination uptake. This study will help in increasing the uptake of the vaccination by considering this theoretically‐driven model.
Attitude towards the benefits of vaccination is crucial variable because perceived benefits are responsible for the formation of attitude. Therefore, it is the demand of current situation to create an awareness about the benefits of vaccination. Perceived behaviour control and subjective norms and self‐efficacy are the also responsible for forming an attitude. Perceived susceptibility and perceived benefits both these variables have indirect effect on the intentions to receive COVID‐19 vaccination. Subjective norms (the opinion of family and friends about the vaccination), perceived behavioural control (self‐control) and attitude are the important factors which also determine the intention to receive vaccination by influencing the behaviour.
Finally, this study provides a framework which can be used by the different entities like policy makers, health care providers and researchers to know about the predictors of COVID‐19 vaccination intentions.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
ETHICS STATEMENT
Ethic statement is not required in case of this research and ethical considerations which were taken for this research are mentioned in the manuscript under the heading of ethical considerations.
ACKNOWLEDGEMENTS
I would like to thank Dr. Waseem Khan (Jamia Hamdard University, Delhi) for his constant support throughout the preparation of my manuscript. I am also thankful to all the participants who participated in this survey selflessly. I would like to thank to the editor‐in‐chief of HPM Prof. Tiago Correia for considering this manuscript and gave second chance to resubmit the manuscript after incorporating revisions. There is no funding for this research.
Tarkar P. Predicting intentions to get the COVID‐19 vaccine in India: An integration of theory of planned behaviour and health belief model. Int J Health Plann Mgmt. 2022;1‐25. 10.1002/hpm.3582
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Poland GA. Tortoises, hares, and vaccines: a cautionary note for SARS‐CoV‐2 vaccine development. Vaccine. 2020;38(27):4219‐4220. 10.1016/j.vaccine.2020.04.073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Perappadan BS. India’s first coronavirus infection confirmed in Kerala. Hindu. 2020:1‐5. [Google Scholar]
- 3. WHO . Coronavirus Disease 2019 (COVID‐19): Situation Report. Vol 82; 2020. [Google Scholar]
- 4. India Fights Corona . COVID‐19. Accessed April 13 2021 #IndiaFightsCorona%20COVID‐19%20in%20India,%20Vaccination,%20Dashboard%20,%20Corona%20Virus%20Tracker%20mygov.in
- 5. Dutta PK. How Second Wave of COVID‐19 Is Different from First in Symptoms, Spread. Indiatoday.in April 16 2021. How%20second%20wave%20of%20COVID‐19%20is%20different%20from%20first%20in%20symptoms,%20spread%20Coronavirus%20Outbreak%20News%20(indiatoday.in)
- 6. Siddiquei MI, Khan W. Economic implications of coronavirus. J Public Aff. 2020;20(4):e2169. 10.1002/pa.2169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Khan W, Siddiquei MI. Covid 19: emerging challenges for the supply chain of fruits in India. Int J Agri Statis Sci. 2021:16. [Google Scholar]
- 8. Ali J, Khan W. Impact of COVID‐19 pandemic on agricultural wholesale prices in India: a comparative analysis across the phases of the lockdown. J Public Aff. 2020;20(4):e2402. 10.1002/pa.2402 [DOI] [Google Scholar]
- 9. Tarkar P. Impact of COVID‐19 pandemic on education system. Int J Adva Sci Technol. 2020;29(9 Special Issue):3812‐3814. [Google Scholar]
- 10. Pandoi D. Mass media: creating the image of COVID‐19. Emp Eco Lett. 2021;20:131‐137. [Google Scholar]
- 11. Kaur SP, Gupta V. COVID‐19 VacdEmp Eco Lettcine: a comprehensive status report. Virus Res. 2020;288:198114. 10.1016/j.virusres.2020.198114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chen M, Li Y, Chen J, et al. An online survey of the attitude and willingness of Chinese adults to receive COVID‐19 vaccination. Hum Vaccines Immunother. 2021;17(7):1‐10. 10.1080/21645515.2020.1853449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cordina M, Lauri MA, Lauri J. Attitudes towards COVID‐19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract. 2021;19(1):2317. 10.18549/pharmpract.2021.1.2317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Husain F, Shahnawaz MG, Khan NH, Parveen H, Savani K. Intention to get COVID‐19 vaccines: exploring the role of attitudes, subjective norms, perceived behavioral control, belief in COVID‐19 misinformation, and vaccine confidence in Northern India. Hum Vaccines Immunother. 2021;17(11):3941‐3953. 10.1080/21645515.2021.1967039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jain L, Vij J, Satapathy P, et al. Factors Influencing COVID‐19 vaccination intentions among college students: a cross‐sectional study in India. Front Public Health. 2021:9. 10.3389/fpubh.2021.735902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Loomba S, Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID‐19 vaccine misinformation on vaccination intent in the UK and USA. Nat Human Behav. 2021;5(3):337‐348. 10.1038/s41562-021-01056-1 [DOI] [PubMed] [Google Scholar]
- 17. Goruntla N, Chintamani SH, Bhanu P, et al. Predictors of acceptance and willingness to pay for the COVID‐19 vaccine in the general public of India: a health belief model approach. Asian Pacific J Tropical Med. 2021;14(4):165. 10.4103/1995-7645.312512 [DOI] [Google Scholar]
- 18. Shmueli L. Predicting intention to receive COVID‐19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Publ Health. 2021;21(1):1‐13. 10.1186/s12889-021-10816-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Conner M, Norman P. Predicting Health Behaviour. McGraw‐Hill Education; UK. [Google Scholar]
- 20. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179‐211. 10.1016/0749-5978(91)90020-t [DOI] [Google Scholar]
- 21. Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta‐analysis. Psychol Bull. 2001;127(1):142‐161. 10.1037/0033-2909.127.1.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Albarracín D, Kumkale GT, Johnson BT. Influences of social power and normative support on condom use decisions: a research synthesis. AIDS care. 2004;16(6):700‐723. 10.1080/09540120412331269558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta‐analytic review. Br J Soc Psychol. 2001;40(4):471‐499. 10.1348/014466601164939 [DOI] [PubMed] [Google Scholar]
- 24. Liao Q, Cowling BJ, Lam WWT, Fielding R. Factors affecting intention to receive and self‐reported receipt of 2009 pandemic (H1N1) vaccine in Hong Kong: a longitudinal study. PloS One. 2011;6(3):e17713. 10.1371/journal.pone.0017713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McClenahan C, Shevlin M, Adamson G, Bennett C, O'Neill B. Testicular self‐examination: a test of the health belief model and the theory of planned behaviour. Health Educ Res. 2007;22(2):272‐284. 10.1093/her/cyl076 [DOI] [PubMed] [Google Scholar]
- 26. Yang ZJ. Predicting young adults intentions to get the H1N1 vaccine: an integrated model. J Health Commun. 2015;20(1):69‐79. 10.1080/10810730.2014.904023 [DOI] [PubMed] [Google Scholar]
- 27. Ajzen I, Fishbein M. The Influence of Attitudes on Behavior; 2005.
- 28. Ajzen I, Manstead AS. Changing health‐related behaviours: an approach based on the theory of planned behaviour. Scope Soc Psychol. 2007;12:55‐76. [Google Scholar]
- 29. Andrews KR, Silk KS, Eneli IU. Parents as health promoters: a theory of planned behavior perspective on the prevention of childhood obesity. J Health Commun. 2010;15(1):95‐107. 10.1080/10810730903460567 [DOI] [PubMed] [Google Scholar]
- 30. Shemanski AR, Cerel J. The development of effective message content for suicide intervention: theory of planned behavior. Crisis. 2009;30(4):174‐179. 10.1027/0227-5910.30.4.174 [DOI] [PubMed] [Google Scholar]
- 31. Godin G, Kok G. The theory of planned behavior: a review of its applications to health‐related behaviors. Am J Health Promot. 1996;11(2):87‐98. 10.4278/0890-1171-11.2.87 [DOI] [PubMed] [Google Scholar]
- 32. Pandoi D, Gaur SS, Gupta AK. Role of virtues in the relationship between shame and tendency to plagiarise: study in the context of higher education. Int J Educ Manag. 2019;33(1):66‐85. 10.1108/ijem-02-2018-0074 [DOI] [Google Scholar]
- 33. Sharma HP, Chaturvedi A. Adoption of Smart technologies: an Indian perspective. In: 2021 5th International Conference on Information Systems and Computer Networks ISCON; 2021:1‐4.
- 34. Rosenstock IM. Why people use health services. Milbank Meml Fund Q. 1966;44(3):94‐127. 10.2307/3348967 [DOI] [PubMed] [Google Scholar]
- 35. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1‐47. 10.1177/109019818401100101 [DOI] [PubMed] [Google Scholar]
- 36. Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Commun Theor. 2003;13(2):164‐183. 10.1093/ct/13.2.164 [DOI] [Google Scholar]
- 37. Fishbein M. The role of theory in HIV prevention. AIDS Care. 2000;12(3):273‐278. 10.1080/09540120050042918 [DOI] [PubMed] [Google Scholar]
- 38. Bish A, Sutton S, Golombok S. Predicting uptake of a routine cervical smear test: a comparison of the health belief model and the theory of planned behaviour. Psychol Health. 2000;15(1):35‐50. 10.1080/08870440008400287 [DOI] [Google Scholar]
- 39. Reid AE, Aiken LS. Integration of five health behaviour models: common strengths and unique contributions to understanding condom use. Psychol Health. 2011;26(11):1499‐1520. 10.1080/08870446.2011.572259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ajzen I. Attitudes, Personality, and Behavior. Open University Press; 1988. [Google Scholar]
- 41. Hair JF, Hult GTM, Ringle CM, et al. A Primer on Partial Least Squares Structural Equation Modeling (PLS‐SEM). Sage publications; 2021. [Google Scholar]
- 42. Henseler J, Ringle CM, Sinkovics RR. The use of partial least squares path modeling in international marketing. In: New challenges to international marketing. Emerald Group Publishing Limited; 2009. [Google Scholar]
- 43. Podsakoff PM, Organ DW. Self‐reports in organizational research: problems and prospects. J Manag. 1986;12(4):531‐544. 10.1177/014920638601200408 [DOI] [Google Scholar]
- 44. Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annu Rev Psychol. 2012;63(1):539‐569. 10.1146/annurev-psych-120710-100452 [DOI] [PubMed] [Google Scholar]
- 45. Spector PE. Method variance in organizational research: truth or urban legend? Organ Res Methods. 2006;9(2):221‐232. 10.1177/1094428105284955 [DOI] [Google Scholar]
- 46. Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879‐903. 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 47. Hair JF, Ringle CM, Sarstedt MPLS.‐SEM. Indeed a silver bullet. J Market Theor Pract. 2011;19(2):139‐152. 10.2753/mtp1069-6679190202 [DOI] [Google Scholar]
- 48. Diamantopoulos A, Siguaw JA. Formative versus reflective indicators in organizational measure development: a comparison and empirical illustration. Br J Manag. 2006;17(4):263‐282. 10.1111/j.1467-8551.2006.00500.x [DOI] [Google Scholar]
- 49. Nunnally JC, Bernstein IH. Psychometric Theory (McGraw‐Hill Series in Psychology). McGraw‐Hill; 1994.3. [Google Scholar]
- 50. Nunnally JC. An overview of psychological measurement. Clin Diag Mental Disorders. 1978:97‐146. 10.1007/978-1-4684-2490-4_4 [DOI] [Google Scholar]
- 51. Garver MS, Mentzer JT. Logistics research methods: employing structural equation modeling to test for construct validity. J Bus Logist. 1999;20(1):33. [Google Scholar]
- 52. Fornell C, Larcker DF. Structural Equation Models with Unobservable Variables and Measurement Error: Algebra and Statistics; 1981:382‐388.
- 53. Hulland J. Use of partial least squares (PLS) in strategic management research: a review of four recent studies. Strategic Manag J. 1999;20(2):195‐204. [DOI] [Google Scholar]
- 54. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance‐based structural equation modeling. J Acad Market Sci. 2015;43(1):115‐135. 10.1007/s11747-014-0403-8 [DOI] [Google Scholar]
- 55. Ramayah TJFH, Cheah J, Chuah F, et al. Partial least squares structural equation modeling (PLS‐SEM) using smartPLS 3.0: An updated guide and practical guide to statistical analysis 2018.
- 56. Wang K, Wong ELY, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross‐sectional survey. Vaccine. 2020;38(45):7049‐7056. 10.1016/j.vaccine.2020.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sharun K, Rahman CF, Haritha CV, Jose B, Tiwari R, Dhama K. COVID‐19 vaccine acceptance: beliefs and barriers associated with vaccination among the general population in India. J Exp Bio Agri ScI. 2020;8(Special Issue 1):S210‐S218. 10.18006/2020.8(spl-1-sars-cov-2).s210.s218 [DOI] [Google Scholar]
- 58. Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID‐19. Eur J Epidemiol. 2020;35(8):775‐779. 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID‐19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500‐6507. 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID‐19 vaccine and willingness to pay. Hum Vaccines Immunother. 2020;16(9):2204‐2214. 10.1080/21645515.2020.1790279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Romate J, Rajkumar E, Greeshma R. Using the integrative model of behavioural prediction to understand COVID‐19 vaccine hesitancy behaviour. Sci Rep. 2022;12(1):1‐13. 10.1038/s41598-022-12466-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS‐CoV‐2 vaccine: a survey of US adults. Ann Intern Med. 2020;173(12):964‐973. 10.7326/m20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Jaenudin J, Komariah A, Chupradit S, et al. Study of the role of mindfulness intervention based on stress reduction in psychological distress and self‐efficacy among the health industry staff during COVID‐19 pandemic. Int J Work Organisat Emot. 2022;13(2):172‐185. 10.1504/ijwoe.2022.123512 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


