Abstract
Understanding predictors of parents' willingness to vaccinate their children appears fundamental to promote vaccine acceptability, especially in a pandemic scenario. The present study aimed to investigate the role of conspiracy beliefs and absolutist thinking in parental attitude toward COVID‐19 vaccine, and the predictive role of parents' individual differences on decisions against children's vaccination. An online survey was administered to 415 parents of children aged 5–11, at the very beginning of the vaccination targeting this population in Italy. Results showed that absolutism predicted the tendency to believe in conspiracies, associated with a negative attitude toward the COVID‐19 vaccine administration to children. Moreover, mothers were less willing to vaccinate children and parents of children aged 5–7 were more hesitant, or even against vaccination, than parents of older children. Finally, the worry about consequences of COVID‐19 infection on children's health facilitated vaccine adherence. These findings contribute to deepening mechanisms regarding the vaccine acceptability.
Keywords: absolutist thinking, conspiracy theories, COVID‐19 pediatric vaccine, decision making, individual differences, parental attitude
1. INTRODUCTION
Starting from February 2020, when patient 1 was detected in Lombardy, the outbreak of Coronavirus disease 2019 (COVID‐19) has caused severe health, social, and economic consequences in Italy (Golinelli et al., 2021; Sanmarchi et al., 2021). The first initial phase of the pandemic has displayed an exponential and uncontrolled growth of infection and death throughout the country (Berardi et al., 2020). With no vaccine available, to respond to the rapid spread of the virus, the Italian government has implemented a number of non‐pharmaceutical containment measures, including social distancing, school closures, and national lockdown.
Even though these non‐pharmaceutical interventions have been initially effective in controlling the spread of the virus, they have been found to be associated with considerable economic, social, and psychological harm (Petrocchi et al., 2022), which made them difficult to sustain for a long time, and highlighted that the full control of the pandemic cannot be achieved solely by using non‐pharmaceutical measures alone. Hence, after the first epidemic wave in the spring 2020, Italy has experienced another three epidemic waves in a period of time of two years, with the virus and its new genetic variants that has continued to circulate.
Vaccinating the entire population seemed the only way to try to get out of the pandemic. As of December 2020, the first COVID‐19 vaccine has been approved (Governo Italiano, 2022) and mass vaccination strategies worldwide have been implemented. In Italy the immunization campaign started during the first months of 2021. Due to the shortage of vaccines, the Italian government has first been oriented to the protection of groups at the highest risk of COVID‐19 exposure and severe clinical consequences, such as elderly, healthcare workers, and subjects with underlying medical conditions. Children and teenagers, who have reported mild (or even no) symptoms over the pandemic were not considered as a priority within the vaccination campaign. Young people aged 12–18 years have been offered the opportunity to receive vaccination starting from June 2021 and since December 2021 also children aged 5–11 years have been given this possibility (European Medicines Agency, 2021).
At the time of writing this article (March 2022), in Italy 33.5% of the population aged 5–11 years has completed the COVID‐19 vaccination schedule (Governo Italiano, 2022). The percentage rate of children vaccinated against COVID‐19 is in line with the level of general vaccination adherence which, in Italy has been decreasing in the latest years, leading the Government to introduce mandatory school‐entry vaccination to contrast the re‐emergence of infectious diseases (Siani, 2019; Bertoncello et al., 2020). Even if the clinical picture of COVID‐19 in pediatric population is usually mild, with a 1% to 8% incidence of severe cases (Castagnoli et al., 2020; Bhuiyan et al., 2021; Osorio & Vaca, 2021), COVID‐19 in children presents some conditions that still deserve attention and for which it is worthwhile to extend the vaccination audience. First of all, there are children belonging to high‐risk pediatric subpopulations. Moreover, there is the possible risk of viral transmission, also to other family members who may present fragile conditions, and coinfections from COVID‐19 (Cruz & Zeichner, 2020). Further, it is worth mentioning that at this critical stage of development it is necessary to ensure as far as possible the continuity of both in‐presence school activities and extracurricular ones, and the possibility of attending both educational and workplaces, and leisure activities (Loades et al., 2020; Klass & Ratner, 2021; Haleemunnissa et al., 2021). Thus, in this current scenario, it seems crucial to investigate willingness and hesitancy related to pediatric COVID‐19 vaccine, in order to understand the possible reasons for non‐vaccination, and investigate those factors that may affect vaccine acceptability. In Italy, the willingness to accept COVID‐19 vaccination in the general population ranged from 65% to 84%, whereas the intention to get their children vaccinated is between 60% and 74.5% in parents of children aged 12–18 years (di Giuseppe et al., 2022; Montalti et al., 2021) and 65.5% in parents of 5–11 aged children (di Giuseppe et al., 2022). However, it is worth mentioning that such willingness rates were collected before vaccination for children under 12 was possible in Italy.
A number of factors have been found to correlate with parents' vaccine acceptability. Literature has recognized parental attitude and decision‐making toward vaccination as a crucial issue even long before pandemics (Pearce et al., 2008; Samad et al., 2006), however, the management of the COVID‐19 crisis made the point any more relevant and topical.
Recent studies highlighted that parents' sociodemographic characteristics influence the parental attitude toward COVID‐19 vaccines. In particular, hesitant parents are more likely to be younger (Goldman et al., 2022; Montalti et al., 2021), belonging to Black, Asian, or minority ethnic groups (Bell et al., 2020; Kelly et al., 2021), and with low educational levels (Montalti et al., 2021; Bianco et al., 2022; Rhodes et al., 2020; Goldman et al., 2022). Regarding parental roles (mother vs. father), results are mixed: some studies highlighted that mothers show greater levels of vaccine hesitancy compared to fathers (Goldman et al., 2020; Montalti et al., 2021; Xu et al., 2021; Zhang et al., 2021), whereas other studies found the opposite (Russo et al., 2021). As for children's age, parents who show a greater vaccine hesitancy have generally younger children (di Giuseppe et al., 2022; Goldman et al., 2020; Montalti et al., 2021; Musa et al., 2021; Russo et al., 2021; Zhang et al., 2021) or children with chronic illnesses (Musa et al., 2021). Moreover, individual differences in parents' beliefs, attitudes, and personality characteristics might also affect the attitude toward vaccination. Overall parental confidence in vaccines (Ruggiero et al., 2021) and, specifically, in COVID‐19 vaccine (Humble et al., 2021) have been found to be highly correlated with the intention to vaccinate their children against COVID‐19. Parents with a personal history of previous vaccinations against other diseases (i.e., influenza) turned out to be more prone to get their children vaccinated, even against COVID‐19 (Kelly et al., 2021), whereas overall concerns for both effectiveness and serious side effects of COVID‐19 vaccination decreased parents' intention to vaccinate their children (Ruggiero et al., 2021). A number of studies investigated the crucial role played by personal beliefs in COVID‐19 conspiracy theories (see Colautti et al., 2022; Đorđević et al., 2021; Howard & Davis, 2022; Pivetti et al., 2021) in undermining the COVID‐19 vaccination adherence. Accordingly, parents who are more prone to embrace conspiracy theories show greater levels of hesitation in having their children immunized (Cookson et al., 2021; Pisl et al., 2021; Zhang et al., 2021). Another individual characteristic, that might influence vaccine attitude and has been little investigated so far, is the ability to tolerate ambiguous situations, that is, the level of tolerance for unstructured, ambiguous events (Colautti et al., 2022; White, 2022). In detail, individuals with a low tolerance for ambiguity perceive unstructured situations as a source of discomfort and threat (Furnham & Ribchester, 1995; Iannello et al., 2017; Petrocchi et al., 2022), which is often associated with the experience of a lack of perceived control (Endler et al., 2000).
As parents are responsible for deciding about their children's vaccination, it seems crucial to investigate those factors (i.e., personal attitudes, beliefs, and personality characteristics) that might affect the decision to have their children immunized in order to increase vaccine acceptance and achieve population immunity within the shortest time possible.
2. AIMS
The present study aimed (a) to investigate the role of conspiracy beliefs and absolutistic thinking in the parental negative attitude toward COVID‐19 vaccine for their children; (b) to measure the predictive role of parents' individual differences on their decision against their children's vaccination; (c) to describe the characteristics of parents based on their intention to not vaccinate their children. As reviewed in Introduction, to date, no study analyzed parents' vaccine acceptance since the opening of the 5–11 years old vaccination campaign in Italy. Therefore, our study intended to further the knowledge on vaccine attitudes and acceptance at an incumbent phase of parents' decision‐making process. Furthermore, other than investigating attitudes as predictors of the intention to vaccinate children, as often studied in previous research, we were interested in exploring the role of cognitive and individual differences on the modulation of parents' vaccine attitudes. As such, we broadened the focus of the investigation by studying both distal (e.g., traits and individual differences) and proximal (e.g., attitudes and beliefs) predictors of parents' vaccine acceptance.
3. METHODS
3.1. Participants
Participants were recruited in Italy based on the following inclusion criteria: (a) being the parent (mother or father) of at least one child aged 5–11 at the time of recruitment; (b) having a 5/11‐year‐old child who was eligible to get the COVID‐19 vaccine, namely, not having any medical conditions for which the COVID‐19 shot was not recommended. A 50–50 gender quota was set during the recruitment process. An initial sample of 511 respondents who completed every section of the survey was screened for inclusion criteria, based on the responses to the corresponding survey questions (i.e., (a) child's age outside the 5–11 range and (b) “Cannot do so for medical or clinical reasons” response to the “Will your child have the COVID‐19 vaccine?” question). A final sample of 415 respondents (208 fathers and 207 mothers; Mage = 42.5 years; SDage = 6.73) was considered in the analyzes. Participants were distributed as follows: 27.71% from north‐west regions (Liguria, Lombardia, Piemonte), 20.72% from north‐east regions (Trentino‐Alto Adige, Veneto, Emilia‐Romagna); 17.59% from central regions (Toscana, Umbria, Marche, Lazio); 33.98% from southern regions and islands (Abruzzo, Molise, Campania, Puglia, Basilicata, Calabria, Sicilia, Sardegna).
3.2. Procedure
Data collection started in Italy when vaccination had just been opened to children aged 5–11 and continued for 7 days (3rd–10th December 2021). The survey was hosted and distributed using the Qualtrics online survey platform (www.qualtrics.com). Respondents were recruited via e‐mail invitations (response rate: 31%) and they received credits to complete the survey, which can be accumulated to receive an annual monetary compensation. Survey completion required approximately 45 min. Written informed consent was collected from all respondents. The study was approved by the Ethics Review Board of the Catholic University of the Sacred Heart of Milan (protocol code: 37–21; date of approval: 30 April 2021) and was conducted according to the guidelines of the Declaration of Helsinki.
3.3. Measures
Socio‐demographics and child's health status: An ad‐hoc questionnaire exploring demographic variables of age, gender, residence, marital status, educational level, COVID‐19 vaccination status, and child's age was devised.
Information sources: A multiple‐answer question was used to explore the number and type of information sources respondents usually employ to gather information about vaccines (“What are the main sources of information you consult?”). The options were categorized based on their reliability (level 1 = TV talks, political debates, social media, friends, relatives; level 2 = online news, newspapers, TV news reports; level 3 = physicians, medical professionals, scientific articles). An information source index was calculated by adding up the reliability scores of each selected option and dividing it by the number of the selected options. For example, if a person selected social media, friends, and relatives as their information sources, they would score 1, whereas if a person selected newspapers, physicians and scientific articles they would score 2.67. Scores ranged from 1, representing the average lowest level of reliability of sources, to 3, representing the highest level of reliability.
3.3.1. Decision to vaccinate children against COVID‐19
One question measuring the parental decision on their children's vaccination (“Will your child have the COVID‐19 vaccine?”; Yes/No/I do not know/cannot do so for medical or clinical reasons) was formulated.
3.3.2. Parental novax COVID‐19 attitude
An ad‐hoc questionnaire that delves into the negative attitude toward the COVID‐19 vaccines was administered. It is composed of six statements to be endorsed on a scale ranging from 1 = completely disagree to 5 = completely agree. The statements are: “Not knowing what's inside vaccines stops me from vaccinating my child”; “I am very concerned about possible serious and/or irreversible side effects that the vaccine may have on my child”; “Compared to before the start of the vaccination campaign, to date, I am very concerned about the side effects that the vaccine may have”; “I feel that I have no control over the choice to vaccinate my child”; “Most people close to me are against getting my child vaccinated”; “Taking appropriate precautions is already an adequate measure against COVID‐19.” Item construction was inspired by previous studies which had shown that similar beliefs (i.e., knowledge about vaccine; worries about unforeseen future side effects; mistrust of vaccine benefit; perceived lack of control over the vaccination choice; social pressure; preference for alternative protective measures) were linked to a negative attitude toward the decision to vaccinate themselves and their children (e.g., Colautti et al., 2022; Cookson et al., 2021; Facciolà et al., 2019; Fedele et al., 2021; Goldman et al., 2020; Martin & Petrie, 2017; Ruggiero et al., 2021). To confirm the construct validity a confirmatory factor analysis was conducted (for more details, see the results section).
3.3.3. Worry about Covid‐19
The COVID‐19 worry scale (CWS, Faisal et al., 2022) is composed of seven items on a 4‐point Likert scale (ranging from 1 = not at all, to 4 = very much). This instrument assesses participants' worry about the spread of COVID‐19 and its consequences. The scale was translated into Italian from the original version according to a method of inter‐judge agreement based on two native Italians' independent translations and was subsequently translated by a third fellow expert in the original language to verify possible discrepancies with the original version.
3.3.4. Attitude toward ambiguity
The subscale moral absolutism/splitting from the multidimensional attitude toward ambiguity scale (MAAS, Lauriola et al., 2016) was used to measure respondents' tendency to show a rigid and absolutist thinking. The subscale is composed of 10 items on a 7‐point Likert scale (ranging from 1 = strongly disagree to 7 = strongly agree).
Conspiracy beliefs: The generic conspiracist beliefs scale (GCB, Brotherton et al., 2013) consists of 15 items on a 5‐point Likert scale (ranging from 1 = definitely not true 5 = definitely true). It explores five dimensions: government malfeasance, malevolent global conspiracy, extraterrestrial cover‐up, personal well‐being, and control of information. The tool was translated into Italian through a method of inter‐judge agreement based on two native Italians' independent translations and subsequently translated by a third fellow expert in the original language.
3.4. Statistical plan
Internal consistency of each scale included in the survey was assessed by means of reliability analysis (Cronbach's α). Additionally, a confirmatory factor analysis (CFA) was conducted to analyze the construct validity of the parental novax COVID‐19 attitude scale. Then, a mediation analysis was performed to assess the mediating role of conspiracy beliefs on the association between absolutism and parental novax attitude. Subsequently, to test the predictive role of a set of individual differences on the parents' decision not to vaccinate their children, a multinomial logistic regression was performed. More precisely, the answer to the question “Will your child have the COVID‐19 vaccine?” was considered as the outcome variable with three categories (yes, I do not know, no), while parental role (mother, father), age group (5–7, 8–11 years), the worry about COVID‐19, and the parental novax attitude were selected as predictors. The propensity to vaccinate their own children (i.e., “yes” response) was selected as the baseline category in the multinomial logistic regression. Collinearity diagnostics confirmed the assumption of no multicollinearity in the linear regression model (VIF values ranged between 1.01 and 1.05; tolerance ranging between .955 and .989). Finally, to further explore the characteristics of parents based on their intention to not vaccinate their children, we investigated the differences between the three groups (i.e., yes, no, I do not know) in socio‐demographics. Differences were tested using Chi‐squared test for categorical variables and univariate ANOVA for continuous variables; When Levene's test was significant, detecting a violation in the homogeneity of variance, we reported Welch's test results. Post‐hoc pairwise comparisons (Tukey test) were tested for significant results. Effect sizes were reported as Cramer's V and Eta‐squared.
The complete dataset analyzed in the present study is available on OSF (https://osf.io/s9zq4/?view_only=a7d28ed44c9949c8bfee22ddf75710a3).
4. RESULTS
4.1. Reliability and validity of survey scales
The theoretical model of the parental novax COVID‐19 attitude scale showed a good fit (χ2 = 10.6, df = 9, p = .302; RMSEA = .020 [.00, .06]; CFI = .998), therefore confirming the construct validity of the scale. Reliability analyzes revealed an acceptable internal consistency of all survey measures (Table 1).
TABLE 1.
Internal consistency (i.e., Cronbach's α) of all survey measures
4.2. The role of conspiracy beliefs and absolutist thinking in the novax attitude: Mediation analysis
The mediation analysis revealed that the association between absolutism and noxav attitude is fully mediated by conspiracy beliefs (Figure 1). The total effect of absolutism on novax attitude was significant (c: b = .222; 95% CI [.091, .355]; Z = 3.299; p < .001). When accounting for conspiracy beliefs, the effect of absolutism on novax attitude was found to be nonsignificant (c′: b = .050; 95% CI [−.076, .176]; Z = .776; p = .438). Finally, the indirect effect of absolutism on novax attitude through conspiracy was found significant (ab: b = .172; 95% CI [.107, .238]; Z = 5.162; p < .001).
FIGURE 1.
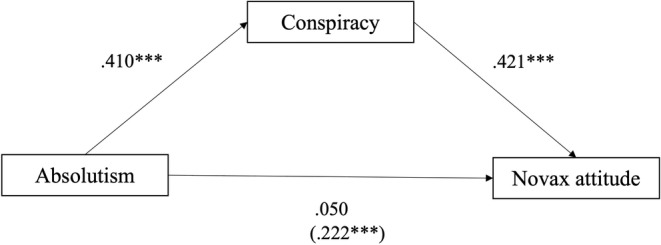
Mediation model with novax attitude as dependent variable, absolutism as independent variable, and conspiracy beliefs as mediator (*** p < .001)
4.3. Predictors of the decision not to vaccinate children: Multinomial logistic regression
The selected predictors significantly predicted the likelihood of the membership to the options about the decision to vaccinate their own children (Nagelkerke's R2 = .22; χ2[8] = 147.0, p < .001). Table 2 reports the individual parameter estimates for the comparison between the “yes” and “no” groups (based on their decision to vaccinate their children), and between the “I don't know” and “yes” groups. The parental role (i.e., mother or father) significantly predicted whether the parent decided against vaccinating their children or they claimed they would vaccinate them. The odds ratio revealed that mothers were slightly less likely to vaccinate their children than fathers. However, the parental role did not significantly predict whether the parent was hesitant (i.e., “I do not know” response) or convinced (i.e., “yes” response) to vaccinate their children. Whether the child was younger (i.e., 5–7 vs. 8–11 years old) significantly predicted whether parents decided to not vaccinate them or to vaccinate them, as well as whether parents did not decide yet rather than being already convinced. More precisely, the odds of a younger child to be vaccinated compared to not being vaccinated were 2.6 times less likely than for an older one. Additionally, the odds of a younger child to have a parent who is convinced about vaccinating them, compared to a parent who is hesitant, were 1.73 less likely than for a 8–11 child. Probability means for parental role and child's age predictions are reported in Figure 2. The level of worry about COVID‐19 infection predicted if the parent was already convinced to vaccinate their children or was already convinced against vaccinating them. The odds ratio showed that parents who were more worried about the infection were 1.25 times more likely to answer “yes” than to answer “no” when asked about their decision to vaccinate their children. Finally, a stronger attitude against the COVID‐19 vaccine significantly predicted whether the parent would or would not vaccinate their children, and whether they were hesitant or already convinced to do that, by making the ‘no’ and ‘I do not know’ responses more likely.
TABLE 2.
Multinomial logistic regression parameter estimates for the “no” compared to “yes” category (referring to the decision to vaccinate their children) and for the “I don't know” compared to “yes” category
| B | SE | p | Odds ratio | |
|---|---|---|---|---|
| No versus Yes | ||||
| Parental role (mother vs. father) | .669 | .332 | .044 | 1.952 |
| Child's age range (8–11 vs. 5–7) | −.952 | .336 | .005 | .386 |
| Worry covid | −1.052 | .233 | < .001 | .349 |
| Novax attitude | 1.927 | .240 | < .001 | 6.871 |
| I do not know versus Yes | ||||
| Parental role (mother vs. father) | .388 | .254 | .126 | 14.740 |
| Child's age range (8–11 vs. 5–7) | −.568 | .252 | .024 | .567 |
| Worry Covid | −.227 | .185 | .219 | .797 |
| Novax attitude | 1.114 | .165 | < .001 | 3.045 |
Significant parameters (p < .05) are marked in bold.
FIGURE 2.
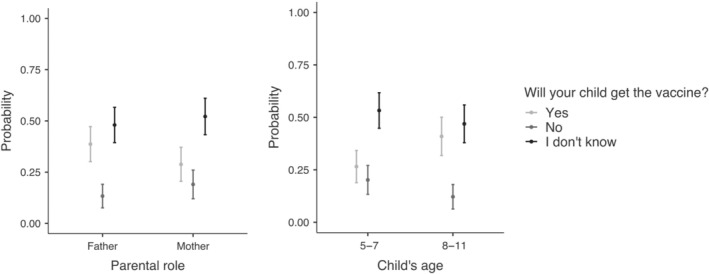
Probability means for parental role and child's age predictions of the parents' responses to the “Will your child have the COVID‐19 vaccine?” question
4.4. Characterization of parents' decision not to vaccinate their children
Considering the whole sample (n = 415), the distribution of responses to the statement “Will your child get the COVID‐19 vaccine” revealed that 35.9% of respondents said “yes,” 20.7% said “no,” and the remaining 43.4% said they did not know. Descriptive statistics of all survey measures and their comparison between decision groups (i.e., yes, no, I do not know) are reported in Table 3 and visually plotted in Figure 3. Parental role was found to be significantly associated with the decision to vaccinate (V = .16); 60.4% of parents who claimed to have decided to vaccinate their children were fathers, whereas 60.5% of parents who decided against the vaccine were mothers. A significant association was also found between the decision to vaccinate children and the child's age range (V = .13); larger ratios of hesitant or opposite decisions were measured for 5–7 years old children compared to 8–11 years old. As expected, whether the parent was vaccinated was significantly associated with the decision to vaccinate their child (V = .59), with the vast majority (92.1%) of unvaccinated parents deciding not to vaccinate their children. Furthermore, parents' education level was associated with the decision to vaccinate their child (V = .17): Parents with higher education were less likely to decide to not vaccinate their children. Interestingly, the type of information sources consulted by parents did not affect their decision.
TABLE 3.
Descriptive statistics and comparisons of individual characteristics of parents based on their decision to vaccinate their child for COVID‐19. Significant differences (p < .05) are marked in bold
| Child vaccine decision | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | I do not know | No | Comparison | ||||||
| M (SD) | n (%) | M (SD) | n (%) | M (SD) | n (%) | F | χ2 | p | |
| Parental role | ‐ | 11.0 | .004 | ||||||
| Mother | ‐ | 59 (14.2) | ‐ | 96 (23.1) | ‐ | 52 (12.5) | |||
| Father | ‐ | 90 (21.7) | ‐ | 84 (20.2) | ‐ | 34 (8.2) | |||
| Child's age range | ‐ | 7.07 | .029 | ||||||
| 5–7 | ‐ | 64 (15.4) | ‐ | 98 (23.6) | ‐ | 51 (12.3) | |||
| 8–11 | ‐ | 85 (20.5) | ‐ | 82 (19.8) | ‐ | 35 (8.4) | |||
| Parent vaccine record | ‐ | 141 | <.001 | ||||||
| Vaccinated | ‐ | 148 (36.5) | ‐ | 175 (43.2) | ‐ | 44 (10.9) | |||
| Unvaccinated | ‐ | 1 (.2) | ‐ | 2 (.5) | ‐ | 35 (8.6) | |||
| Education level | ‐ | 24.4 | .002 | ||||||
| Middle school | ‐ | 11 (2.7) | ‐ | 8 (1.9) | ‐ | 6 (1.4) | |||
| High school | ‐ | 66 (15.9) | ‐ | 105 (25.3) | ‐ | 54 (13.0) | |||
| Bachelor's degree | ‐ | 14 (3.4) | ‐ | 23 (5.5) | ‐ | 14 (3.4) | |||
| Graduate/Master | ‐ | 48 (11.6) | ‐ | 41 (9.9) | ‐ | 11 (2.7) | |||
| MD/PhD | ‐ | 10 (2.4) | ‐ | 3 (.7) | ‐ | 1 (.2) | |||
| Info sources index | 2.37 (.51) | ‐ | 2.37 (.58) | ‐ | 2.22 (.64) | ‐ | 2.07 a | ‐ | .13 |
Welch's F.
FIGURE 3.
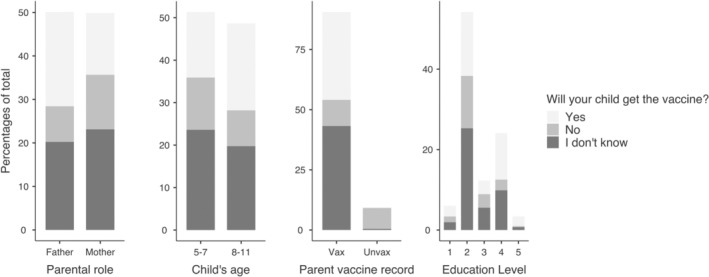
Bar plots of individual characteristics of parents based on their decision to vaccinate their child for COVID‐19. The parents' responses to the “Will your child have the COVID‐19 vaccine?” question
5. DISCUSSION
The main objective of the present research was to investigate, among Italian parents of children aged 5–11, the role of specific parental characteristics in influencing both the development of a negative attitude toward COVD‐19 vaccine and the decision of getting their children vaccinated. The questionnaire covered a range of issues related to COVID‐19, including attitudes, concerns, and practices toward COVID‐19 vaccines, and some variables concerning parental characteristics, namely, the individual tendency to believe in conspiracy theories and think in an absolutist and dichotomous way. Studying the relationship between parental characteristics and both attitude and decision toward pediatric vaccination seems crucial to tailor communication strategies and to prevent low immunization coverage.
The first step of our investigation was understanding how specific thinking styles of parents explained a negative attitude toward the COVID‐19 immunization of their children. Specifically, we focused on dichotomic and rigid thinking, as a cognitive reaction to perceived ambiguous stimuli (Furnham & Marks, 2013). Such an absolutist reaction toward ambiguity stems from an intolerance toward the coexistence of positive and negative features in the same situation (Lauriola et al., 2016), and ultimately leads to the tendency to oversimplify reality. When evaluating complex situations, individuals who show absolutist thinking may be more prone to use heuristics and mental shortcuts (Stanovich & West, 1999) to arrive at quick closure. The preference to resort to dichotomic solutions to problems makes individuals more susceptible to belief in untrustworthy information sources (Salvi et al., 2021), which further leads to the adherence to conspiracy theories (Mosleh et al., 2021; Pisl et al., 2021; Stoica & Umbreș, 2021). Our results confirmed this prediction: parents' tendency to absolutist thinking predicted their beliefs in conspiracy theories, as attempts to explain significant events through secret plots orchestrated by powerful and malevolent actors (Douglas et al., 2019). Conspiratorial narratives offer a readily available explanation of complex and ambiguous events by means of simple cause‐effect associations (e.g., “Groups of scientists manipulate, fabricate, or suppress evidence in order to deceive the public”). Our findings suggest that attitude toward health policies, such as the vaccination of young children against COVID‐19 is influenced by absolutist thinking only through the adherence to conspiracy theories. More precisely, although absolutism did not directly influence parents' attitude toward vaccines, it predicted the tendency to believe in conspiracies, which, in turns, was associated with a negative attitude toward the COVID‐19 vaccine administration to 5–11 years old children. We suggest that conspiracies were used by “rigid” parents to navigate the vaccine information overload (e.g., potential adverse effects, long‐term outcomes, efficacy against infection, cost–benefit ratio in children), and ultimately directed them toward a negative attitude toward vaccination. After describing the cognitive process leading to developing negative attitudes toward the vaccine, we aimed to deepen the understanding of what keeps parents from vaccinating 5/11‐year‐old children against COVID‐19, focusing on the predictors of the decision. Besides identifying the individual factors which predicted parents' decision‐making outcome, we were specifically interested in differentiating the variables which explained hesitancy from those explaining aversion toward vaccinating young children. In literature, vaccine hesitancy has been described as a complex, context‐specific phenomenon that is influenced by a plethora of variables (MacDonald, 2015) and therefore, it is worth analyzing separately. In the decision‐making process, attitudes influence the final decision by guiding the evaluation of choice options (Ajzen, 1996; Sanbonmatsu et al., 2014). Consistently, our results showed that the negative attitude toward the COVID‐19 vaccine was the strongest predictor of both hesitancy and rejection of the vaccine to children. Parental role significantly predicted whether the parent was willing to vaccinate their child, with mothers being less likely to vaccinate, compared to fathers. Previous surveys conducted in Italy reported contrasting results about the willingness of mothers versus fathers to get their children vaccinated against COVID‐19 (Montalti et al., 2021; Russo et al., 2021). In addition to being generally more apprehensive about their child's health and safety (Taubman‐Ben‐Ari & Ben‐Yaakov, 2020), mothers, as females, tend to experience more adverse effects after vaccination (Flanagan et al., 2017). Therefore, safety concerns could have affected mothers' appraisal of the cost‐benefit ratio associated with the immunization of their young children, and ultimately lead to decisions against it. Interestingly, parental role polarized the parents' decision into definite choices and did not influence hesitancy. In line with previous studies (di Giuseppe et al., 2022; Goldman et al., 2020; Montalti et al., 2021; Musa et al., 2021; Russo et al., 2021; Zhang et al., 2021), parents of children younger than 8 (5–7) years old were more frequently undecided or against the vaccination, compared to parents of older children (8–11 years old). This tendency can be interpreted in light of the lack of real‐world data on the effectiveness and safety of COVID‐19 vaccine in children under 8 years old at the time of launching the survey (December 2021). Contrary to safety concerns associated with the vaccine, the worry about the consequences of COVID‐19 infection on young children's health would facilitate vaccine adherence. Indeed, parental perception of the seriousness of COVID‐19 was a significant predictor of the decision to have their children vaccinated. This was expected as the perceived seriousness of COVID‐19 has been found to play a crucial role in vaccine acceptance (Karlsson et al., 2021).
Finally, parents who would not vaccinate their children were more frequently mothers, parents of children under 8 years old, unvaccinated individuals and individuals with lower education, consistently with previous findings (Montalti et al., 2021; Bianco et al., 2022; Rhodes et al., 2020; Goldman et al., 2022).
Concerning the overall vaccination acceptance rate in our study, over 64% of our sample of parents was not yet convinced to vaccinate their children at the very beginning of the 5–11 years old children vaccination campaign in Italy. Specifically, 20.7% of respondents fully rejected the possibility of vaccinating their children. In addition, our results revealed a greater number of parents who were hesitant to vaccinate their young children (43.3% of the total sample). These results are partly inconsistent with previous surveys conducted in Italy, which reported a higher parental willingness to vaccinate their children (Montalti et al., 2021: Only 10% of the parents were against children's vaccination). However, it should be acknowledged that, in studies that have been conducted before vaccines became available, willingness to vaccinate was generally higher than in studies conducted after the introduction of the vaccination. Our results are in line with more recent surveys reporting lower vaccination willingness in parents after the immunization campaign has begun (Russo et al., 2021). This finding suggests that, after the vaccination campaign began and information on possible vaccine's side effects became available, parents have shown a more critical attitude toward pediatric vaccination, which resulted in a reduced parental intention to have their children vaccinated.
Rather than mapping all potential individual predictors of pediatric vaccine adherence, we focused our investigation on cognitive characteristics which undermined vaccine acceptance through modulating parental attitude toward the immunization of their children. Consequently, other potential factors (e.g., perceived effectiveness and safety of the vaccine Haydarov & Gordon, 2015; Nan et al., 2012; anticipated regret, Penţa et al., 2020; Caso et al., 2019; religiosity, Shelton et al., 2013; trust in science and healthcare institutions, Dubé & Gagnon, 2018), which were already analyzed by previous studies on the same topic, were not considered in our investigation. Although our participants belonged to a non‐probability panel sample, the distribution of respondents across Italian regions was homogeneous and the measured rate of unvaccinated parents (9.4%) was consistent with national statistics (15.4% of Italian population over 12, as of 1st December 2021; Istituto Superiore di Sanità, 2021). Therefore, the representativeness of our sample can be considered acceptable. The present study, however, shows some limitations. First, the design of the study involves only indirect measures about the attitude toward vaccines. So, further studies should also include implicit measures to investigate the impact of the automatic cognitive processes and psychological attributes (e.g., stereotypes, attitudes) which could contribute to understanding the decision process to get children vaccinated. Second, responses to questionnaires could be subjected to participants' social desirability, and also confounding variables (i.e., concerning the reliability of participants in their home environment) have to be considered. Finally, the quantitative tools revealed some interesting and little explored aspects, which did not allow the phenomenon to be explored in depth. Thus, further studies should deepen the issue also with qualitative methods, to delve into participants' emotional experiences underlying attitudes toward vaccines and fully understand possible causes why some parents show vaccine hesitancy or refusal and, more in general, the cultural meaning of what it means “being vaccinated.”
We believe that some interesting implications may derive from the findings of the present study to ensure vaccination adherence, especially in view of the future seasonal booster shots. We found a difference in COVID‐19 vaccine attitude depending on the parental role, with mothers being less likely to vaccinate their children. On the grounds that mothers generally have a greater impact concerning children's healthcare decisions in the family―at least in part because fathers may perceive less confidence in taking primary health care of children (Garfield & Isacco III, 2012; Lee et al., 2020)―and given that mothers showed a greater vaccine aversion, it may be crucial for healthcare providers to promote fathers' involvement in the child vaccine decision‐taking and childcare process.
Focusing both on conspiracy theories that bias the vaccine attitude and on the models of attitude structure, specific cognitive, and affectively‐based educational interventions addressed to modify personal beliefs can be designed. Hence, we believe that this point needs to be seriously addressed, provided that the impact of conspiracy beliefs goes much further than COVID‐19 vaccine and the current pandemic. Conspiracy beliefs relate to a broader range of detrimental health outcomes that may affect the overall individual well‐being and, which, consequently, should be firmly countered.
Vaccine hesitancy, intended as a delay in the decision of (accepting or refusing) vaccination (MacDonald, 2015) can also be seen as a preference to choose in the short term a well‐known status rather than a not familiar one, that is deciding not to decide. In this way, it would be interesting to investigate in further research the role that individual differences in susceptibility to cognitive biases may have on parents' decision to vaccinate their children. Specifically, it would be interesting to investigate both the status quo bias, which consists in choosing, among conflicting options, the one that allows maintaining the current condition (Samuelson & Zeckhauser, 1988)―and the omission bias―which implies that a negative consequence from inaction, not getting a vaccine, is weighted less heavily than a negative outcome from an action (getting the vaccine) (Baron & Ritov, 1994). Acquiring knowledge about parents' susceptibility to cognitive biases when deciding about their children's vaccines could help policymakers to develop more effective and not coercive solutions to increase acceptance, for example, integrating the use of nudges (see for instance: Giubilini et al., (2019)).
Finally, future studies should investigate the role of parental style on the decision to vaccinate their children. More precisely, parental style is a psychological construct that represents strategies and patterns used by parents in childcare growing. This is consistent with previous findings on HPV vaccination: Mothers who provided more direct monitoring of children were found to be more prone to vaccinate them (Rosenthal et al., 2008). Consequently, it could be interesting to deepen and explore the possible role of parental style in the COVID‐19 attitude toward children vaccination.
6. CONCLUSIONS
Experts have indicated vaccination as one of the most important achievements in public health, positioning immunization as a key contributor to people's physical and mental health (as reported in the global guidance file Immunization Agenda 2030, IA2030; World Health Organization, 2020). Vaccines (pediatric vaccinations in particular) are critical for controlling “well‐known” diseases, combating the spread of “novel” emerging infectious diseases, such as the outbreak of COVID‐19 pandemic, and addressing possible threat of future pandemics. Despite their relevance, parents' hesitancy toward pediatric vaccinations is still strong. Therefore, understanding factors associated with pediatric vaccine acceptability is fundamental to assure the efficacy of the vaccination campaign and orient/guide policy makers in promoting it. Few studies have yet deepened into the role of individual differences specifically addressed to parents' attitude toward the vaccination against COVID‐19. A strength of the present study is the specific focus on psychological measures, such as personal attitudes, beliefs, and personality characteristics as predictors of vaccine attitude and willingness to vaccinate their children. Findings from this study contribute to a better understanding of vaccine acceptability among parents of children aged 5–11, through the identification of individual factors that may promote and support the decision to get their children vaccinated. Based on our findings, it could be possible to design communication campaigns, specifically addressed to parents and targeted on specific individual characteristics, so as to enhance child vaccine adherence.
AUTHOR CONTRIBUTIONS
All authors have:(1) made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; (2) been involved in drafting the manuscript or revising it critically for important intellectual content; (3) given final approval of the version to be published; (4) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST
The authors have no relevant financial or non‐financial interests to disclose.
ACKNOWLEDGMENT
Authors would like to thank Giulia Capobianco for her technical support in implementing the questionnaire online. Open Access Funding provided by Universita Cattolica del Sacro Cuore within the CRUI‐CARE Agreement.
Iannello, P. , Colautti, L. , Magenes, S. , Antonietti, A. , & Cancer, A. (2022). Black‐and‐white thinking and conspiracy beliefs prevent parents from vaccinating their children against COVID‐19. Applied Cognitive Psychology, 1–11. 10.1002/acp.3999
DATA AVAILABILITY STATEMENT
Data presented in this study are available on OSF.
REFERENCES
- Ajzen, I. (1996). The social psychology of decision making. In Social psychology: Handbook of basic principles (pp. 297–325). Guilford. [Google Scholar]
- Baron, J. , & Ritov, I. (1994). Reference points and omission bias. Organizational Behavior and Human Decision Processes, 59(3), 475–498. 10.1006/obhd.1994.1070 [DOI] [PubMed] [Google Scholar]
- Bell, S. , Clarke, R. , Mounier‐Jack, S. , Walker, J. L. , & Paterson, P. (2020). Parents' and guardians' views on the acceptability of a future COVID‐19 vaccine: A multi‐methods study in England. Vaccine, 38(49), 7789–7798. 10.1016/j.vaccine.2020.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berardi, C. , Antonini, M. , Genie, M. G. , Cotugno, G. , Lanteri, A. , Melia, A. , & Paolucci, F. (2020). The COVID‐19 pandemic in Italy: Policy and technology impact on health and non‐health outcomes. Health Policy and Technology, 9(4), 454–487. 10.1016/j.hlpt.2020.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertoncello, C. , Ferro, A. , Fonzo, M. , Zanovello, S. , Napoletano, G. , Russo, F. , Baldo, V. , & Cocchio, S. (2020). Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccine, 8(2), 276. 10.3390/vaccines8020276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhuiyan, M. U. , Stiboy, E. , Hassan, M. Z. , Chan, M. , Islam, M. S. , Haider, N. , Jaffe, A. , & Homaira, N. (2021). Epidemiology of COVID‐19 infection in young children under five years: A systematic review and meta‐analysis. Vaccine, 39(4), 667–677. 10.1016/j.vaccine.2020.11.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianco, A. , Della Polla, G. , Angelillo, S. , Pelullo, C. P. , Licata, F. , & Angelillo, I. F. (2022). Parental COVID‐19 vaccine hesitancy: A cross‐sectional survey in Italy. Expert Review of Vaccines, 21(4), 541–547. 10.1080/14760584.2022.2023013 [DOI] [PubMed] [Google Scholar]
- Brotherton, R. , French, C. C. , & Pickering, A. D. (2013). Measuring belief in conspiracy theories: The generic conspiracist beliefs scale. Frontiers in Psychology, 4, 279. 10.3389/fpsyg.2013.00279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caso, D. , Carfora, V. , Starace, C. , & Conner, M. (2019). Key factors influencing Italian mothers' intention to vaccinate sons against HPV: The influence of trust in health authorities, anticipated regret and past behaviour. Sustainability, 11(23), 6879. 10.3390/su11236879 [DOI] [Google Scholar]
- Castagnoli, R. , Votto, M. , Licari, A. , Brambilla, I. , Bruno, R. , Perlini, S. , Rovida, F. , Baldanti, F. , & Marseglia, G. L. (2020). Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection in children and adolescents: A systematic review. JAMA Pediatrics, 174(9), 882–889. 10.1001/jamapediatrics.2020.1467 [DOI] [PubMed] [Google Scholar]
- Colautti, L. , Cancer, A. , Magenes, S. , Antonietti, A. , & Iannello, P. (2022). Risk‐perception change associated with COVID‐19 Vaccine's side effects: The role of individual differences. International Journal of Environmental Research and Public Health, 19(3), 1189. 10.3390/ijerph19031189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cookson, D. , Jolley, D. , Dempsey, R. C. , & Povey, R. (2021). A social norms approach intervention to address misperceptions of anti‐vaccine conspiracy beliefs amongst UK parents. PLoS One, 16(11), e0258985. 10.1371/journal.pone.0258985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz, A. T. , & Zeichner, S. L. (2020). COVID‐19 in children: Initial characterization of the pediatric disease. Pediatrics, 145(6), e20200834. 10.1542/peds.2020-0834 [DOI] [PubMed] [Google Scholar]
- di Giuseppe, G. , Pelullo, C. P. , Volgare, A. S. , Napolitano, F. , & Pavia, M. (2022). Parents' willingness to vaccinate their children with COVID‐19 vaccine: Results of a survey in Italy. The Journal of Adolescent Health, 70(4), 550–558. 10.1016/j.jadohealth.2022.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Đorđević, J. M. , Mari, S. , Vdović, M. , & Milošević, A. (2021). Links between conspiracy beliefs, vaccine knowledge, and trust: Anti‐vaccine behavior of Serbian adults. Social Science & Medicine, 277, 113930. 10.1016/j.socscimed.2021.113930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas, K. M. , Uscinski, J. E. , Sutton, R. M. , Cichocka, A. , Nefes, T. , Ang, C. S. , & Deravi, F. (2019). Understanding conspiracy theories. Political Psychology, 40, 3–35. 10.1111/pops.12568 [DOI] [Google Scholar]
- Dubé, È. , & Gagnon, D. (2018). Trust, information sources and the impact on decision‐making: The example of vaccination. In Paganelli C. (Ed.), Confidence and legitimacy in health information and communication (Vol. 1, pp. 43–65). John Wiley & Sons. 10.1002/9781119549741.ch3 [DOI] [Google Scholar]
- Endler, N. S. , Speer, R. L. , Johnson, J. M. , & Flett, G. L. (2000). Controllability, coping, efficacy, and distress. European Journal of Personality, 14(3), 245–264. [DOI] [Google Scholar]
- European Medicines Agency . (2021). Comirnaty COVID‐19 vaccine: EMA recommends approval for children aged 5 to 11. Retrieved from https://www.ema.europa.eu/en/news/comirnaty-covid-19-vaccine-ema-recommends-approval-children-aged-5-11
- Facciolà, A. , Visalli, G. , Orlando, A. , Bertuccio, M. P. , Spataro, P. , Squeri, R. , Picerno, I. , & Pietro, A. D. (2019). Vaccine hesitancy: An overview on parents' opinions about vaccination and possible reasons of vaccine refusal. Journal of Public Health Research, 8(1), 1436. 10.4081/jphr.2019.1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faisal, R. A. , Jobe, M. C. , Ahmed, O. , & Sharker, T. (2022). Replication analysis of the COVID‐19 worry scale. Death Studies, 46(3), 574–580. 10.1080/07481187.2020.1815104 [DOI] [PubMed] [Google Scholar]
- Fedele, F. , Aria, M. , Esposito, V. , Micillo, M. , Cecere, G. , Spano, M. , & De Marco, G. (2021). COVID‐19 vaccine hesitancy: A survey in a population highly compliant to common vaccinations. Human Vaccines & Immunotherapeutics, 17(10), 3348–3354. 10.1080/21645515.2021.1928460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan, K. L. , Fink, A. L. , Plebanski, M. , & Klein, S. L. (2017). Sex and gender differences in the outcomes of vaccination over the life course. Annual Review of Cell and Developmental Biology, 33, 577–599. 10.1146/annurev-cellbio-100616-060718 [DOI] [PubMed] [Google Scholar]
- Furnham, A. , & Marks, J. (2013). Tolerance of ambiguity: A review of the recent literature. Psychology, 4, 717–728. 10.4236/psych.2013.49102 [DOI] [Google Scholar]
- Furnham, A. , & Ribchester, T. (1995). Tolerance of ambiguity: A review of the concept, its measurement and applications. Current Psychology, 14(3), 179–199. [Google Scholar]
- Garfield, C. F. , & Isacco, A. J., III . (2012). Urban fathers' involvement in their child's health and healthcare. Psychology of Men & Masculinity, 13(1), 32–48. 10.1037/a0025696 [DOI] [Google Scholar]
- Giubilini, A. , Caviola, L. , Maslen, H. , Douglas, T. , Nussberger, A. M. , Faber, N. , Vanderslott, S. , Loving, S. , Harrison, M. , & Savulescu, J. (2019). Nudging immunity: The case for vaccinating children in school and day care by default. Hec Forum, 31(4), 325–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. D. , Ceballo, R. , & International COVID‐19 Parental Attitude Study (COVIPAS) Group . (2022). Parental gender differences in attitudes and willingness to vaccinate against COVID‐19. Journal of Paediatrics and Child Health., 58, 1016–1021. 10.1111/jpc.15892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, R. D. , Yan, T. D. , Seiler, M. , Cotanda, C. P. , Brown, J. C. , Klein, E. J. , Hoeffe, J. , Gelernter, R. , Hall, J. E. , Davis, A. L. , Griffiths, M. A. , Mater, A. , Manzano, S. , Gualco, G. , Shimizu, N. , Hurt, T. L. , Ahmed, S. , Hansen, M. , Sheridan, D. , … International COVID‐19 Parental Attitude Study (COVIPAS) Group . (2020). Caregiver willingness to vaccinate their children against COVID‐19: Cross sectional survey. Vaccine, 38(48), 7668–7673. 10.1016/j.vaccine.2020.09.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golinelli, D. , Campinoti, F. , Sanmarchi, F. , Rosa, S. , Beleffi, M. , Farina, G. , Tampieri, A. , Fantini, M. P. , Giostra, F. , & Santi, L. (2021). Patterns of emergency department visits for acute and chronic diseases during the two pandemic waves in Italy. The American Journal of Emergency Medicine, 50, 22–26. 10.1016/j.ajem.2021.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Governo Italiano . (2022). Report Vaccini Anti‐COVID 19. Retrieved from https://www.governo.it/it/cscovid19/report-vaccini/
- Haleemunnissa, S. , Didel, S. , Swami, M. K. , Singh, K. , & Vyas, V. (2021). Children and COVID19: Understanding impact on the growth trajectory of an evolving generation. Children and Youth Services Review, 120, 105754. 10.1016/j.childyouth.2020.105754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydarov, R. , & Gordon, J. C. (2015). Effect of combining attribute and goal framing within messages to change vaccination behavior. Journal of Communication in Healthcare, 8(1), 45–54. 10.1179/1753807615y.0000000005 [DOI] [Google Scholar]
- Howard, M. C. , & Davis, M. M. (2022). The mediating role of vaccine hesitancy in the relations of COVID‐19 conspiracy beliefs and vaccination outcomes: Which dimensions matter? Journal of Health Psychology. 10.1177/13591053221096013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humble, R. M. , Sell, H. , Dubé, E. , MacDonald, N. E. , Robinson, J. , Driedger, S. M. , Sadarangani, M. , Meyer, S. B. , Wilson, S. , Benzies, K. M. , Lemaire‐Paquette, S. , & MacDonald, S. E. (2021). Canadian parents' perceptions of COVID‐19 vaccination and intention to vaccinate their children: Results from a cross‐sectional national survey. Vaccine, 39(52), 7669–7676. 10.1016/j.vaccine.2021.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannello, P. , Mottini, A. , Tirelli, S. , Riva, S. , & Antonietti, A. (2017). Ambiguity and uncertainty tolerance, need for cognition, and their association with stress. A study among Italian practicing physicians. Medical Education, 22(1), 1270009. 10.1080/10872981.2016.1270009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istituto Superiore di Sanità . (2021). Epidemia COVID‐19. Retrieved from https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_1-dicembre-2021.pdf
- Karlsson, L. C. , Soveri, A. , Lewandowsky, S. , Karlsson, L. , Karlsson, H. , Nolvi, S. , Karukivi, M. , Lindfelt, M. , & Antfolk, J. (2021). Fearing the disease or the vaccine: The case of COVID‐19. Personality and Individual Differences, 172, 110590. 10.1016/J.PAID.2020.110590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, B. J. , Southwell, B. G. , McCormack, L. A. , Bann, C. M. , MacDonald, P. D. , Frasier, A. M. , Bevc, C. A. , Brewer, N. T. , & Squiers, L. B. (2021). Predictors of willingness to get a COVID‐19 vaccine in the US. BMC Infectious Diseases, 21(1), 1–7. 10.1186/s12879-021-06023-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klass, P. , & Ratner, A. J. (2021). Vaccinating children against Covid‐19—The lessons of measles. New England Journal of Medicine, 384(7), 589–591. 10.1056/NEJMp2034765 [DOI] [PubMed] [Google Scholar]
- Lauriola, M. , Foschi, R. , Mosca, O. , & Weller, J. (2016). Attitude toward ambiguity: Empirically robust factors in self‐report personality scales. Assessment, 23(3), 353–373. 10.1177/1073191115577188 [DOI] [PubMed] [Google Scholar]
- Lee, C. H. , Overall, N. C. , & Sibley, C. G. (2020). Maternal and paternal confidence in vaccine safety: Whose attitudes are predictive of children's vaccination? Vaccine, 38(45), 7057–7062. 10.1016/j.vaccine.2020.09.020 [DOI] [PubMed] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , Linney, C. , McManus, M. N. , Borwick, C. , & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1218–1239. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald, N. E. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. 10.1111/pops.12568 [DOI] [PubMed] [Google Scholar]
- Martin, L. R. , & Petrie, K. J. (2017). Understanding the dimensions of anti‐vaccination attitudes: The vaccination attitudes examination (VAX) scale. Annals of Behavioral Medicine, 51(5), 652–660. 10.1007/s12160-017-9888-y [DOI] [PubMed] [Google Scholar]
- Montalti, M. , Rallo, F. , Guaraldi, F. , Bartoli, L. , Po, G. , Stillo, M. , Perrone, P. , Squillace, L. , Dallolio, L. , Pandolfi, P. , Resi, D. , Fantini, M. P. , Reno, C. , & Gori, D. (2021). Would parents get their children vaccinated against SARS‐CoV‐2? Rate and predictors of vaccine hesitancy according to a survey over 5000 families from Bologna, Italy. Vaccines, 9(4), 366. 10.3390/vaccines9040366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosleh, M. , Pennycook, G. , & Rand, D. G. (2021). Field experiments on social media. Current Directions in Psychological Science, 31(1), 69–75. 10.1177/09637214211054761 [DOI] [Google Scholar]
- Musa, S. , Dergaa, I. , Abdulmalik, M. A. , Ammar, A. , Chamari, K. , & Saad, H. B. (2021). BNT162b2 COVID‐19 vaccine hesitancy among parents of 4023 young adolescents (12–15 years) in Qatar. Vaccine, 9(9), 981. 10.3390/vaccines9090981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nan, X. , Xie, B. , & Madden, K. (2012). Acceptability of the H1N1 vaccine among older adults: The interplay of message framing and perceived vaccine safety and efficacy. Health Communication, 27(6), 559–568. 10.1080/10410236.2011.617243 [DOI] [PubMed] [Google Scholar]
- Osorio, M. F. , & Vaca, R. G. (2021). Coronavirus disease 2019 in children: Is it really mild? Infectious Diseases in Clinical Practice, 29(2), e78–e81. 10.1097/IPC.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce, A. , Law, C. , Elliman, D. , Cole, T. J. , & Bedford, H. (2008). Factors associated with uptake of measles, mumps, and rubella vaccine (MMR) and use of single antigen vaccines in a contemporary UK cohort: Prospective cohort study. BMJ, 336(7647), 754–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penţa, M. A. , Crăciun, I. C. , & Băban, A. (2020). The power of anticipated regret: Predictors of HPV vaccination and seasonal influenza vaccination acceptability among young Romanians. Vaccine, 38(6), 1572–1578. 10.1016/j.vaccine.2019.11.042 [DOI] [PubMed] [Google Scholar]
- Petrocchi, S. , Iannello, P. , Ongaro, G. , Antonietti, A. , & Pravettoni, G. (2022). The interplay between risk and protective factors during the initial height of the COVID‐19 crisis in Italy: The role of risk aversion and intolerance of ambiguity on distress. Current Psychology, 41(1), 437–448. 10.1007/s12144-021-01601-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisl, V. , Volavka, J. , Chvojkova, E. , Cechova, K. , Kavalirova, G. , & Vevera, J. (2021). Dissociation, cognitive reflection and health literacy have a modest effect on belief in conspiracy theories about Covid‐19. International Journal of Environmental Research and Public Health, 18(10), 5065. 10.3390/ijerph18105065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivetti, M. , Melotti, G. , Bonomo, M. , & Hakoköngäs, E. (2021). Conspiracy beliefs and acceptance of COVID‐vaccine: An exploratory study in Italy. Social Sciences, 10(3), 108. 10.3390/socsci10030108 [DOI] [Google Scholar]
- Rhodes, M. E. , Sundstrom, B. , Ritter, E. , McKeever, B. W. , & McKeever, R. (2020). Preparing for a COVID‐19 vaccine: A mixed methods study of vaccine hesitant parents. Journal of Health Communication, 25(10), 831–837. 10.1080/10810730.2021.1871986 [DOI] [PubMed] [Google Scholar]
- Rosenthal, S. L. , Rupp, R. , Zimet, G. D. , Meza, H. M. , Loza, M. L. , Short, M. B. , & Succop, P. A. (2008). Uptake of HPV vaccine: Demographics, sexual history and values, parenting style, and vaccine attitudes. Journal of Adolescent Health, 43(3), 239–245. 10.1016/j.jadohealth.2008.06.009 [DOI] [PubMed] [Google Scholar]
- Ruggiero, K. M. , Wong, J. , Sweeney, C. F. , Avola, A. , Auger, A. , Macaluso, M. , & Reidy, P. (2021). Parents' intentions to vaccinate their children against COVID‐19. Journal of Pediatric Health Care, 35(5), 509–517. 10.1016/j.pedhc.2021.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo, L. , Croci, I. , Campagna, I. , Pandolfi, E. , Villani, A. , Reale, A. , Barbieri, M. A. , Raponi, M. , Gesualdo, F. , & Tozzi, A. E. (2021). Intention of parents to immunize children against SARS‐CoV‐2 in Italy. Vaccine, 9(12), 1469. 10.3390/vaccines9121469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvi, C. , Iannello, P. , McClay, M. , Rago, S. , Dunsmoor, J. E. , & Antonietti, A. (2021). Going viral: How fear, socio‐cognitive polarization and problem‐solving influence fake news detection and proliferation during COVID‐19 pandemic. Frontiers in Communication, 5, 562588. 10.3389/fcomm.2020.562588 [DOI] [Google Scholar]
- Samad, L. , Butler, N. , Peckham, C. , Bedford, H. , & Millennium Cohort Study Child Health Group . (2006). Incomplete immunisation uptake in infancy: Maternal reasons. Vaccine, 24(47–48), 6823–6829. 10.1016/j.vaccine.2006.06.039 [DOI] [PubMed] [Google Scholar]
- Samuelson, W. , & Zeckhauser, R. (1988). Status quo bias in decision making. Journal of Risk and Uncertainty, 1(1), 7–59. 10.1007/BF00055564 [DOI] [Google Scholar]
- Sanbonmatsu, D. M. , Prince, K. C. , Vanous, S. , & Posavac, S. S. (2014). The multiple roles of attitudes in decision making. In Betsch T. & Haberstroh S. (Eds.), The routines of decision making (pp. 131–146). Psychology Press. 10.4324/9781410611826 [DOI] [Google Scholar]
- Sanmarchi, F. , Golinelli, D. , Lenzi, J. , Esposito, F. , Capodici, A. , Reno, C. , & Gibertoni, D. (2021). Exploring the gap between excess mortality and COVID‐19 deaths in 67 countries. JAMA Network Open, 4(7), e2117359. 10.1001/jamanetworkopen.2021.17359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton, R. C. , Snavely, A. C. , De Jesus, M. , Othus, M. D. , & Allen, J. D. (2013). HPV vaccine decision‐making and acceptance: Does religion play a role? Journal of Religion and Health, 52(4), 1120–1130. 10.1007/s10943-011-9553-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siani, A. (2019). Measles outbreaks in Italy: A paradigm of the re‐emergence of vaccine‐preventable diseases in developed countries. Preventive Medicine, 121, 99–104. 10.1016/j.ypmed.2019.02.011 [DOI] [PubMed] [Google Scholar]
- Stanovich, K. E. , & West, R. F. (1999). Individual differences in reasoning and the heuristics and biases debate. In Ackerman P. L., Kyllonen P. C., & Roberts R. D. (Eds.), Learning and individual differences: Process, trait, and content determinants (pp. 389–411). American Psychological Association. 10.1037/10315-017 [DOI] [Google Scholar]
- Stoica, C. A. , & Umbreș, R. (2021). Suspicious minds in times of crisis: Determinants of Romanians' beliefs in COVID‐19 conspiracy theories. European Societies, 23(sup1), S246–S261. 10.1080/14616696.2020.1823450 [DOI] [Google Scholar]
- Taubman‐Ben‐Ari, O. , & Ben‐Yaakov, O. (2020). Distress and apprehension among new parents during the COVID‐19 pandemic: The contribution of personal resources. American Journal of Orthopsychiatry, 90(6), 810–816. 10.1037/ort0000497 [DOI] [PubMed] [Google Scholar]
- White, H. A. (2022). Need for cognitive closure predicts stress and anxiety of college students during COVID‐19 pandemic. Personality and Individual Differences, 187, 111393. 10.1016/j.paid.2021.111393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). Immunization agenda 2030: A global strategy to leave no one behind. World Health Organization. https://www.who.int/docs/default-source/immunization/strategy/ia2030/ia2030-document-en.pdf [Google Scholar]
- Xu, Y. , Zhang, R. , Zhou, Z. , Fan, J. , Liang, J. , Cai, L. , Peng, L. , Ren, F. , & Lin, W. (2021). Parental psychological distress and attitudes towards COVID‐19 vaccination: A cross‐sectional survey in Shenzhen, China. Journal of Affective Disorders, 292, 552–558. 10.1016/j.jad.2021.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, M. X. , Lin, X. Q. , Chen, Y. , Tung, T. H. , & Zhu, J. S. (2021). Determinants of parental hesitancy to vaccinate their children against COVID‐19 in China. Expert Review of Vaccines, 20(10), 1339–1349. 10.1080/14760584.2021.1967147 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data presented in this study are available on OSF.


