Abstract
Introduction
In China, recurrent pandemics require frequent city‐wide lockdowns and quarantine actions to contain the impact of COVID‐19, exposing college students to psychological problems, including hopelessness. Hence, the purpose of helping problematic college students alleviate hopelessness symptoms motivates us to carry out the present study to explore their interrelationship.
Methods
Hopelessness (i.e., a complex phenomenon with important clinical consequences, such as depression and suicidality) was investigated in a large longitudinal sample of college students (N = 2787; 58.59% female; age mean ± SD = 18.34 ± 0.92) who were recruited during and after the COVID‐19 lockdown using the Beck Hopelessness Scale (BHS).
Results
Applying the novel approach (i.e., symptom network analysis), the results indicated that the edge of #BHS1 (i.e., [NOT] hope‐enthusiasm)–#BHS15 (i.e., [NOT] faith‐in‐the‐future) showed the strongest association both in Wave 1 and Wave 2. Similarly, #BHS20 (i.e., not‐trying) had the highest node expectedinfluence (centrality) in the hopelessness symptoms network both among Wave 1 and Wave 2. The Network Comparison Test indicated that the global network strength significantly differed between the two time points. As expected, college students' hopelessness will gradually dissipate with the end of segregation control. The stability and accuracy indicated that the network analysis results were trustworthy.
Conclusions
The study findings provide evidence that central nodes and edges connecting symptoms should be addressed. Further interventions and treatments that may target these symptoms are essential to effectively alleviate the overall hopelessness level among college students. Theoretical and clinical potential consequences were discussed in detail.
Keywords: child and adolescent mental health, depression, depressive symptoms, measurement, psychiatry
1. INTRODUCTION
Since the breakout of the new coronavirus SARS‐CoV‐2 (COVID‐19) pandemic in late 2019, policy‐makers have taken strong measures, such as city‐wide lockdowns and quarantines, to control the further spread of the pandemic, notably in China (Saricali et al., 2020; Tanne et al., 2020). Pfefferbaum and North (2020) emphasized that these public health policies had a huge psychological cost, including loneliness, boredom, and anxiety (Brooks et al., 2020; Mertens et al., 2020; Rubin & Wessely, 2020). Although effective methods to prevent COVID‐19 spread are needed, the emotional health of individuals in quarantine cannot be overlooked.
The proportion of a country's population enrolled in higher education is vital in evaluating that nation's potential for economic development and achievement. However, given that the group is most prone to mental health problems (Auerbach et al., 2018), college students have been proven to experience more anxiety, fear, and worry when public health emergencies occur (Feng et al., 2021). Moreover, the COVID‐19 resurgence made college students uncertain of their future (Duplaga & Grysztar, 2021). An earlier study indicated that worsening financial circumstances was the main risk factor for prolonged hopelessness (Haatainen et al., 2003b). For college students, worsening financial circumstances and strict isolation policies made getting an internship or job difficult. As a result, suffering from negative emotions (Brooks et al., 2020) coupled with concerns about future career development (Wang et al., 2020) has caused many psychological problems (e.g., hopelessness) among college students during the pandemic, which must be taken seriously.
Hopelessness is defined as the expectation that negative events will occur and/or positive events will not occur, accompanied by the belief that the person cannot change this gloomy situation (Abramson et al., 1989). Hopelessness is often reported in major psychopathological conditions, such as depression and schizophrenia (Cole, 1988; Lysaker et al., 2004). Additionally, hopelessness has been shown to be a key component of depressive symptoms and present at clinical levels in the general population (i.e., ∼10%; Haatainen et al., 2003b), strongly linked to anxiety (Kocalevent et al., 2017). Initially, hopelessness developed from learned helplessness theory, which posits that repeated exposure to uncontrollable and aversive environmental stimuli gradually leads the individual to believe that the aversive situation is inescapable and that a sense of helplessness ensues regarding the situation (Seligman & Maier, 1967). Nevertheless, the components of hopelessness are more than helplessness (Ratcliffe, 2015), biased future thinking (Roepke & Seligman, 2016), and blocked goal processing (Hadley & MacLeod, 2010). During adolescent individuation, negative early life experiences may be too severe, causing the frustration of hope and hopelessness to develop (Liu et al., 2015). For youth, hopelessness (i.e., losing curiosity, dreams, and aspiration) is a state that cannot be tolerated for more than a short time, which is characterized by a void and a sense that they do not know anything. The youth may choose to rebel against authority, participate in gangs and illegal activities, or even use drugs for temporary gratification (Akhtar et al., 2018). Hopelessness is even associated with early suicide attempts and suicidal thoughts in early adulthood (Troister et al., 2015). Hence, such a pessimistic attitude toward life (e.g., from college students) warrants considerable therapeutic and research attention among adolescents (Marchetti, 2018).
As a traditional and standard statistical method, the latent factor approach assumes that observable psychological components independently generate unobservable factors. On the other hand, this traditional approach reveals no causality effect on each observable component but simply reflects the underlying latent factor. As a result, this approach cannot fully capture and elucidate the interactive process among the different components of complex psychological structures such as hopelessness (Dalege et al., 2016; Schmittmann et al., 2013).
An alternative approach named network analysis, a novel way to conceptualize psychological phenomena, has been proposed and widely used to study mental disorders (Afzali et al., 2016; Robinaugh et al., 2020). Compared to the traditional statistical method, network analysis is a symptom‐oriented method that argues that the mental structure (e.g., hopelessness) is likely to arise from the interaction among observable indicators (e.g., questionnaire items) (Borsboom & Cramer, 2013). In this way, researchers can clearly find the extent to which variables belonging to the same construct are interconnected and how different constructs mutually interact with each other (Blasi et al., 2021). Additionally, network analysis allows for identifying which nodes are the most central in the network structure and which edges between nodes function as the main pathways of the network (Marchetti, 2018). In sum, the network approach offers a different and effective perspective to shed light on complex psychological structures.
Given the potential psychological problems (e.g., hopelessness) that college students experience under lockdown conditions, it is necessary to explore hopelessness symptoms during and after the lockdown and to clarify the specific impact of quarantine on college students' hopelessness. To the best of our knowledge, no longitudinal studies have compared hopelessness symptoms among Chinese college students using network analysis, which provides the impetus to carry out this study. Therefore, this longitudinal study investigated the inner structure of hopelessness and the interactions among its constituent elements among Chinese college students utilizing network analysis and compared the differences in hopelessness symptoms among college students during and after the COVID‐19 lockdown. The hypotheses are that (1) the association of the symptom‐to‐symptom relationship during the lockdown is stronger than that after the lockdown, and (2) the feeling of hopelessness will decrease after the lockdown.
2. METHODS
2.1. Participants
Participants were recruited through online advertisements using a social media platform (i.e., WeChat). Before collecting the baseline data sets, all of them met the criteria of living in school accommodations and getting at least 1 month in a mandatory school lockdown. Hence, we obtained the first wave of data from 6710 college students during the COVID‐19 pandemic lockdown from September 26 to September 30, 2021. The second wave of data from 3731 college students was collected at the same university from December 23 to December 27, 2021, after the closure management was lifted. The total valid data size was 2787 (male, N = 1154; female, N = 1633; age mean ± SD = 18.34 ± 0.92) after matching the two waves of data. All subjects were informed of the study's purpose and signed an electronic informed consent form before participation. The research was examined and approved by the ethics committee of Beijing Normal University (Reference number: 202112220084).
3. MEASURES
3.1. Beck Hopelessness Scale (BHS)
The BHS consists of 20 items (Beck et al., 1974), 11 of which are negative (e.g., “My future seems dark to me”) and 9 of which are positive (e.g., “I look forward to the future with hope and enthusiasm”). All items are rated as 1 or 0, indicating “yes” and “no” statements, respectively. The total scale score varies from 0 to 20, with higher values suggesting a stronger sense of hopelessness. We did not reverse items to guarantee access to the network's core symptoms in the present study.
Excellent reliability has been reported for the BHS in Chinese studies (Ma et al., 2020; Zhang et al., 2015). In this study, Cronbach's α coefficients for Wave 1 and Wave 2 were 0.81 and 0.84, respectively.
3.2. STATISTICAL ANALYSIS
3.2.1. Item check
First, all BHS items were analyzed for mean, standard deviation (SD), kurtosis, skewness, and polychoric correlations. The informativeness of each item was evaluated by means of the SD (Mullarkey et al., 2019). According to the manual, if the polychoric correlation between “A” and other items differed statistically in 25% of the cases, we judged that the two items measured the same feature/symptom (i.e., redundancy) (Jones, 2021). The item redundancy test was performed with the R package “networktools 1.3.0” (Jones, 2021).
3.2.2. Network estimation
Second, we used the Ising model to estimate the network following current guidelines (van Borkulo et al., 2014). The Ising model evaluated network structures based on binary data, which can be considered a sequence of pairwise associations among binary variables after taking the confounding effects of all other associations into account. This method used logistic regression in combination with model selection based on a goodness‐of‐fit index to detect associations between nodes. The network models were regularized using enhanced least absolute shrinkage and selection operation to reduce the number of spurious edges and increase network comprehensibility (eLASSO) (Ravikumar et al., 2010). This approach yielded a sparse network model that was more intelligible than the original. The extended Bayesian information criterion was used to identify a model (Foygel & Drton, 2010). We used the package “bootnet” to fit the binary network (Epskamp et al., 2018).
Nodes represent symptoms in network analysis, whereas edges represent connections between nodes. Partial correlation analysis was used to determine the relationship between two nodes while controlling the interference of other nodes. Green edges indicate positive correlations, whereas red edges suggest negative correlations. Three major centrality indices (i.e., betweenness, closeness, and strength) need to be reported in network analysis. Previous research has shown that assessments of closeness and betweenness are unreliable in determining nodes' importance (Bringmann et al., 2019). Hence, strength was chosen as the metric in the current study. Moreover, traditional indices such as strength centrality may not accurately predict node influence on a network containing both positive and negative edges. Robinaugh et al. (2016) demonstrated that expectedInfluence is a more appropriate index in such cases.
3.2.3. Estimation of network accuracy and stability
To assess the robustness of the results, three procedures were adopted to examine the accuracy and stability of the network model (Epskamp et al., 2018). First, the accuracy of edge weights was estimated by computing confidence intervals (CIs) using the nonparametric bootstrapping method. The observations in the data were then randomly resampled to create new data sets from which the 95% CIs were calculated. Larger CIs indicated less precise estimations of the edges, whereas smaller CIs indicated more trustworthy networks (Epskamp et al., 2018).
Second, with subset bootstraps, the correlation stability coefficient (CS‐C) was used to assess the stability of the centrality indices (i.e., strength and expectedInfluence) (Costenbader & Valente, 2003). If the centrality indices of the nodes did not change significantly after excluding a portion of the sample in the data set, the network structure could be considered stable.
The CS‐C represented the maximum proportion of samples that could be removed so that the correlation between the original centrality indices could be at least 0.7 with a 95% probability (Epskamp et al., 2018). In general, the CS‐C should be greater than 0.25 and preferably greater than 0.5. The difference between the two strength indices was then considered significant if the 1000‐bootstrap 95% nonparametric CIs did not include zero. Furthermore, predictability was calculated using the R package mgm (version 1.2–12) (Haslbeck & Waldorp, 2020), reflecting how well all of a node's neighbors predict a specific node.
3.2.4. Comparison of the network structure across two waves
The Network Comparison Test (NCT) was used, a permutation test that evaluates the difference between two networks (i.e., during the COVID‐19 pandemic lockdown vs. after the COVID‐19 pandemic lockdown). As previously recommended (Wang et al., 2020), the NCT was conducted with 1000 permutations. This procedure assessed the global network strength by comparing the absolute sum of all edge weights between the networks. Next, the edge weight distributions within each network were compared to characterize the network's structure. After controlling for multiple tests (Holm–Bonferroni correction of p values), the differences in strength for each edge were compared between the two networks. The R package “NetworkComparisonTest” 2.2.1 was used to run all of the tests (van Borkulo et al., 2022).
4. RESULTS
4.1. Descriptive statistics and item check
First, item informativeness (i.e., the item's SD) and item redundancy were assessed. No items were found to be poorly informative (i.e., 2.5 SD below the mean level of informativeness) or redundant with other items (i.e., fewer than 25% of statistically different correlations). Supporting Information: Tables S1 and S2 show the mean, SD, skewness, and kurtosis of hopelessness symptoms measured by the BHS in Waves 1 and 2, respectively.
4.2. Network structure and centrality measures analysis
The networks of the symptoms of hopelessness during and after the lockdown are shown in Figure 1 and Supporting Information: Figure S1, and the corresponding partial correlation matrix is presented in Supporting Information: Tables S3 and S4.
Figure 1.

Network structures for the 20 items of the Beck Hopelessness Scale. (a) Wave 1. (b) Wave 2.
Across Wave 1, the edge of #BHS1 (i.e., [NOT] hope‐enthusiasm)–#BHS15 (i.e., [NOT] faith‐in‐the‐future) showed the strongest association, followed by the edge of #BHS6 (i.e., [NOT] expect‐to‐succeed)–#BHS19 (i.e., [NOT] better‐future) and the edge of #BHS11 (i.e., unpleasantness‐ahead)–#BHS12 (i.e., not‐getting). Similarly, the edge of #BHS1 (i.e., [NOT] hope‐and‐enthusiasm)–#BHS15 (i.e., [NOT] faith‐in‐the‐future) revealed the strongest association across Wave 2, followed by the edge of #BHS11 (i.e., unpleasantness‐ahead)–#BHS12 (i.e., not getting) and #BHS16 (i.e., giving‐up‐on‐wanting)–#BHS20 (i.e., not‐trying).
In Supporting Information: Tables S1 and S2, Figure S1, Figures 1 and 2, #BHS20 (i.e., not‐trying) had the highest node expectedInfluence (centrality) in the hopelessness symptoms network among Wave 1 college students, followed by #BHS11 (i.e., unpleasantness‐ahead), #BHS12 (i.e., not‐getting), and an average of 85.69% of the variance could be potentially accounted for by each node's neighbors (M predictability = 0.857 ± 0.092). Similar to Wave 1, #BHS20 (i.e., not‐trying) had the highest node expectedInfluence (centrality) in the hopelessness symptoms network among Wave 2 college students, followed by #BHS11 (i.e., unpleasantness‐ahead), #BHS12 (i.e., not‐getting), and an average of 85.84% of the variance could be potentially accounted for by each node's neighbors (M predictability = 0.858 ± 0.088).
Figure 2.
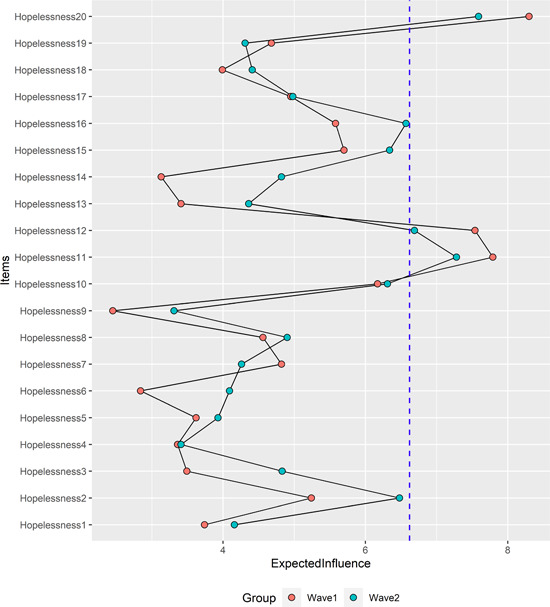
The strength and expectedInfluence (centrality) value (raw scores) of the hopelessness symptoms among Wave 1 and Wave 2. The core symptoms identified in this study are indicated by a blue dashed line (top three). The case‐dropping bootstrap procedure showed that the CS‐C of the centrality indices (i.e., strength and expectedInfluence) was 0.67 and 0.75 both in wave 1 (Part A of Figure 3) and wave 2 (Part B of Figure 3).
In addition, #BHS18 (i.e., uncertain‐future) had the highest node strength (centrality) in the hopelessness symptoms network among Wave 1 college students, whereas #BHS15 (i.e., [NOT] faith‐in‐the‐future) had the highest node strength (centrality) in the hopelessness symptoms network among Wave 2 college students.
4.3. Network accuracy and stability
In Figure 3, the case‐dropping bootstrap procedure showed that the CS coefficients ranged from 0.67 to 0.75 across the four groups. The results of the nonparametric bootstrap procedure revealed that most comparisons among edge weights, node strength, and node expectedInfluence were statistically significant (Supporting Information: Figures S2–S4). Additionally, bootstrapped 95% CIs were narrow, representing edges that were trustworthy.
Figure 3.
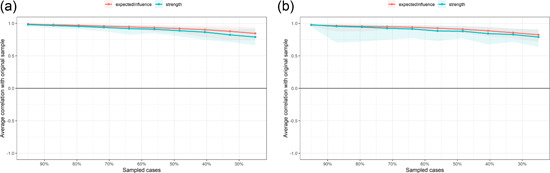
The x‐axis indicates the percentage of cases of the original sample included at each step. The y‐axis indicates the average of correlations between the centrality indices from the original network and the centrality indices from the networks that were re‐estimated after excluding increasing percentages of cases. (a) Wave 1. (b) Wave 2.
Moreover, we checked the variability by correlating this sample's strength, expectedInfluence, and predictability. First, strength (r s = 0.83 [0.62; 0.93]), expectedInfluence (r s = 0.91 [0.77; 0.96]) and predictability (r s = 0.97 [0.92; 0.99]) were highly correlated across the two waves of data sets. In Wave 1, strength (r s = 0.47 [0.04; 0.76]) and expectedInfluence (r s = 0.48 [0.05; 0.76]) were positively correlated with predictability. However, strength (r s = 0.39 [−0.07; 0.71]) and expectedInfluence (r s = 0.30 [−0.17; 0.65]) were not correlated with predictability in Wave 2.
4.4. Network and symptom mean level comparisons across sex and two waves
The NCT is a permutation test to investigate invariance in different network characteristics. First, we compared the network models and network centrality indices between male (N = 1154) and female (N = 1633) participants at two time points. There were no significant sex differences in network global strength (males: 46.86 vs. females: 52.61; global strength difference (S)= 5.75, p = 0.42) or distribution of edge weights (M = 1.07, p = 0.74) at Wave 1 (all p> 0.05 after Holm–Bonferroni corrections) (Supporting Information: Figure S6). Similarly, there were no significant sex differences in network global strength (males: 454.13 vs. females: 56.38; global strength difference (S)= 2.25, p = 0.79) or distribution of edge weights (M = 1.34, p = 0.32) at Wave 2 (Supporting Information: Figure S7). Second, we compared the network models and network centrality indices between the two waves. As shown in Figure 4 (left panel), the bootstrap value of the maximum difference in any edge weight (1000 permutations) was not significantly different (M = 1.17, p = 0.24). The right panel in Figure 4 indicates the bootstrap value of the difference in global network strength, with a significant difference (network strength among Wave 1 participants: 62.9; among Wave 2 participants: 77.3; S= 14.4, p = 0.000). The Holm–Bonferroni corrected p values were all >0.05, indicating the absence of significant differences, except for #BHS14 (i.e., not‐working‐out) (p < 0.000).
Figure 4.
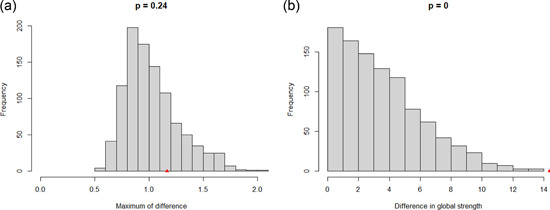
Comparison of network properties between Wave 1 and Wave 2 participants
4.5. Covariate (age and sex) network structures across two waves
Previous studies found that age and sex were associated with the clinical features of hopelessness (Haatainen et al., 2003a). Hence, after controlling for the basic sociodemographic characteristics (i.e., sex and age), the network model and local structure indices were re‐estimated (Supporting Information: Figure S5). Compared with the original network in Wave 1, an almost identical network was obtained with respect to edge magnitude (r = 0.66 [0.56; 0.76]), strength (r = 0.93 [0.83; 0.97]) and expectedInfluence (r = 0.57 [0.17; 0.81]) for the hopelessness network structure. Similarly, an almost identical network was obtained with respect to edge magnitude (r = 0.62 [0.52; 0.72]), strength (r = 0.62 [0.25; 0.83]), and expectedInfluence (r = 0.30 [−0.16; 0.66]) for the hopelessness network structure in Wave 2.
5. DISCUSSION
The results of this study involved 2787 participants who provided complete responses both during and after the COVID‐19 epidemic lockdown in China. Network analysis was used to understand the structure of hopelessness and how it was altered in two different situations, complementing prior studies that used the latent factor approach. Several findings are noteworthy.
First, the results of this study showed that #BHS1 (i.e., [NOT] hope‐enthusiasm) was most strongly associated with #BHS15 (i.e., [NOT] faith‐in‐the‐future) in both Wave 1 and Wave 2, and the strength of the association increased following the quarantine measures. According to the developmental trajectory (Mac Giollabhui et al., 2018), negative life events throughout adolescence are associated with increased hopelessness and a decrease in future orientation. This implies that whether in quarantine or not, once college students feel hopeless about the future, they will lose their vision for it, and vice versa. That is, the negative impact of this epidemic on college students is profound and lasting (Li et al., 2021), leading them to lose the confidence to imagine the future as they did previously. Thus, mindfulness can be used to alleviate negative psychological effects (Saricali et al., 2020), as mindful awareness could help reduce rumination among college students, regardless of whether they are in lockdown.
In addition, #BHS6 (i.e., [NOT] expect‐to‐succeed) was closely related to the thoughts of #BHS19 (i.e., [NOT] better‐future) in Wave 1. In Wave 2, #BHS11 (i.e., unpleasantness‐ahead) was more closely correlated with #BHS12 (i.e., not‐getting). Developing cognitive functions enhances adolescents' reasoning capability in analyzing the probable causes and implications of negative life experiences, while cognitive bias leads adolescents to biased attribution, resulting in a sense of hopelessness throughout their adolescence (Steinberg, 2005). Because college students do not know when the threat of COVID‐19 will remit even after the lockdown (Blasi et al., 2021), the conflict between their inner desire for freedom and peer interaction and the reality that they must obey the rules (e.g., quarantine, self‐isolation, switching to online teaching) makes them gradually think that their future is nothing more than this. Such negative future expectations may reduce the capability to imagine specific and detailed future scenarios (Marchetti, 2018). Hence, even when the lockdown was lifted, college students still lacked the capability to be ambitious about their future. Cognitive behavioral therapy may be a good choice (Stallard et al., 2010) because rectified cognitive reasoning may help adolescents prevent, potentially avoid, or solve stressful life events (Steinberg, 2005).
Moreover, as seen from the expectedInfluence index, the network structure analysis revealed that the top three central items of the network were #BHS20 (i.e., not‐trying), #BHS11 (i.e., unpleasantness‐ahead), and #BHS12 (i.e., not‐getting) (ordered by centrality) in both waves, indicating that the typical symptoms were superficially similar during and after the lockdown. Nevertheless, it is worth noting that the expectedInfluence value of nodes (top three) in Wave 2 was smaller than that in Wave 1, which means that individuals under lockdown conditions had a stronger sense of hopelessness than when they were not locked down. Taken together, the above findings suggest that despite a certain level of negative thoughts, the level of hopelessness among college students decreases once social restrictions are eased, possibly because they feel less fearful after the lockdown (Blasi et al., 2021). Additionally, the results implied that these three nodes constituted the “backbone” of the hopelessness network evidence, which was inconsistent with Marchetti's research on the general population in Germany (2018), suggesting that #BHS16 (i.e., giving‐up‐on‐wanting) and #BHS19 (i.e., [NOT] better‐future) were the two most central items in the hopelessness network. This difference may be caused by various factors, including culture, samples, and the outbreak of the COVID‐19 pandemic (Kazan Kızılkurt et al., 2021; Stewart et al., 2005). Overall, it is necessary to focus on the specific roles played by specific network components (Mullarkey et al., 2019).
In addition, this study also provides an analysis of the strength index, another common index used to identify the most central nodes, for reference. The results showed a completely different picture, which was reflected in that viewing the future as vague and uncertain (i.e., #BHS18) was the most central item in the network in Wave 1, while lacking faith and trust in the future (i.e., #BHS15) was the most central item in Wave 2. The fact that the central nodes are different due to the adoption of different indices suggests that the expectedInfluence index is more appropriate than the strength index for predicting node influence in a network containing both positive and negative edges (Robinaugh et al., 2016).
Finally, the analysis in this study pointed to no difference in the intensity between edges during and after the lockdown, while there were differences in the global network strength, with a higher global value in Wave 2 than in Wave 1. The increase in global values seems to underline more feelings of hopelessness after the lockdown. However, it is understandable that the present study did not reverse items to ensure the network's core symptoms when the expectedInfluence index was selected, and more than half of the nine positive items showed higher strength values in Wave 2, especially for #BHS15. Thus, the global value in Wave 2 may drop significantly if these items are reverse‐scored. It can be boldly assumed that the higher global strength value in Wave 2 than that in Wave 1 is probably caused by the unreversed #BHS15.
From this point of view, the increase in global value may indicate that college students felt less hopeless after the lockdown. Another change that should not be ignored is the difference in the values of the top central nodes in the two waves. As mentioned above, the strength value of #BHS15 increased in Wave 2, while the value of #BHS18 in Wave 2 decreased, suggesting less uncertainty about the future when college students are no longer quarantined. In line with this, a previous study showed that measures implemented to control the outbreak inevitably disrupted routine life and led to uncertainty (Tang et al., 2020). Such a sense of uncertainty could cause individuals to feel overwhelmed and impair their ability to manage negative emotions (Blasi et al., 2021). However, once the lockdown was lifted, college students could regain freedom and more interpersonal communication, which improved their mental states and caused less uncertainty (Xiao, 2020).
Several strengths characterize the current study. First, the first two‐wave analysis on COVID‐19‐related hopelessness among college students in China may add evidence to the multitude of previous cross‐sectional surveys. Second, a large sample was used to detect hopelessness's constituent components, and the reported findings are likely to be generalized to the adult student population. Third, by applying the network approach, this study helped to clarify the sense of hopelessness that occurs in the context of the pandemic lockdown and postlockdown.
In addition to these strengths, several limitations should be noted. First, although this study is highly informative on how hopelessness changed during the lockdown and postlockdown restrictive measures, it must be acknowledged that the network analyses do not define the causal associations between hopelessness and other factors. For instance, future research could further explore the relationship between depressive symptoms and hopelessness since the latter is an important precursor symptom of depression. The approach of cross‐lagged panel networks (Funkhouser et al., 2021), which conducts regularized regressions for each variable at Time 1 and Time 2 (autoregression) and for one variable at Time 1 predicts a different variable at Time 2 (cross‐lagged), could be used to examine the hopelessness transformation process deeply. Second, the study did not use a random population sample, and hence, the parameters may vary from one sample to another. Future studies on more extensive and representative samples across multiple time points are needed.
In conclusion, by applying network analysis, this study was the first to explore the complicated structure of hopelessness symptoms on a large college student scale during the COVID‐19 pandemic. The results revealed that the thoughts of giving up on trying (#BHS20) and unpleasant expectations for the future (#BHS11), along with the belief that I cannot get what I want (#BHS12), are the top three central nodes both during and after the lockdown. Furthermore, edges connecting symptoms should also be addressed when central symptoms are identified. The findings suggested that targeting interventions to these symptoms is important to effectively alleviate the overall hopelessness level in college students.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENT PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/jclp.23439
ETHICS STATEMENT
The study was approved by the University of Beijing Normal University Institutional Review Board (202112220084).
Supporting information
Supporting information.
ACKNOWLEDGMENTS
Many thanks to the college students that participated in this study. May this distress‐inducing COVID‐19 pandemic end quickly, and may we achieve liberty sooner.
Tao, Y. , Niu, H. , Hou, W. , Zhang, L. , & Ying, R. (2022). Hopelessness during and after the COVID‐19 pandemic lockdown among Chinese college students: A longitudinal network analysis. Journal of Clinical Psychology, 1–14. 10.1002/jclp.23439
Yanqiang Tao and Haiqun Niu contributed equally to this study.
DATA AVAILABILITY STATEMENT
Data are available upon request from the first author.
REFERENCES
- Abramson, L. Y. , Metalsky, G. I. , & Alloy, L. B. (1989). Hopelessness depression: A theory‐based subtype of depression. Psychological Review, 96(2), 358–372. 10.1037/0033-295X.96.2.358 [DOI] [Google Scholar]
- Afzali, M. H. , Sunderland, M. , Teesson, M. , Carragher, N. , Mills, K. , & Slade, T. (2016). A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: The role of overlapping symptoms. Journal of Affective Disorders, 208, 490–496. 10.1016/j.jad.2016.10.037 [DOI] [PubMed] [Google Scholar]
- Akhtar, S. , & O'Neil, M. K. (2018). Hopelessness: Developmental, cultural, and clinical realms (2nd ed.). Routledge. [Google Scholar]
- Auerbach, R. P. , Mortier, P. , Bruffaerts, R. , Alonso, J. , Benjet, C. , Cuijpers, P. , Demyttenaere, K. , Ebert, D. D. , Green, J. G. , Hasking, P. , Murray, E. , Nock, M. K. , Pinder‐Amaker, S. , Sampson, N. A. , Stein, D. J. , Vilagut, G. , Zaslavsky, A. M. , & Kessler, R. C. (2018). WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. Journal of Abnormal Psychology, 127(7), 623–638. 10.1037/abn0000362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. , Weissman, A. , Lester, D. , & Trexler, L. (1974). The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology, 42(6), 861–865. 10.1037/h0037562 [DOI] [PubMed] [Google Scholar]
- Blasi, M. D. , Gullo, S. , Mancinelli, E. , Freda, M. F. , Esposito, G. , Gelo, O. C. G. , Lagetto, G. , Giordano, C. , Mazzeschi, C. , Pazzagli, C. , Salcuni, S. , & Lo Coco, G. (2021). Psychological distress associated with the COVID‐19 lockdown: A two‐wave network analysis. Journal of Affective Disorders, 284, 18–26. 10.1016/j.jad.2021.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo, C. D. , van Bork, R. , Boschloo, L. , Kossakowski, J. J. , Tio, P. , Schoevers, R. A. , Borsboom, D. , & Waldorp, L. J. (2022). Comparing network structures on three aspects: A permutation test. Psychological Methods , 1–12. Advance online publication. 10.1037/met0000476 [DOI] [PubMed]
- van Borkulo, C. D. , Borsboom, D. , Epskamp, S. , Blanken, T. F. , Boschloo, L. , Schoevers, R. A. , & Waldorp, L. J. (2014). A new method for constructing networks from binary data. Scientific Reports, 4(1), 5918. 10.1038/srep05918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. , & Cramer, A. O. J. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Bringmann, L. F. , Elmer, T. , Epskamp, S. , Krause, R. W. , Schoch, D. , Wichers, M. , Wigman, J. T. W. , & Snippe, E. (2019). What do centrality measures measure in psychological networks. Journal of Abnormal Psychology, 128(8), 892–903. 10.1037/abn0000446 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet (British Edition), 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole, D. A. (1988). Hopelessness, social desirability, depression, and parasuicide in two college student samples. Journal of Consulting and Clinical Psychology, 56(1), 131–136. 10.1037/0022-006X.56.1.131 [DOI] [PubMed] [Google Scholar]
- Costenbader, E. , & Valente, T. W. (2003). The stability of centrality measures when networks are sampled. Social Networks, 25(4), 283–307. 10.1016/S0378-8733(03)00012-1 [DOI] [Google Scholar]
- Dalege, J. , Borsboom, D. , van Harreveld, F. , van den Berg, H. , Conner, M. , & van der Maas, H. L. J. (2016). Toward a formalized account of attitudes: The Causal Attitude Network (CAN) model. Psychological Review, 123(1), 2–22. 10.1037/a0039802 [DOI] [PubMed] [Google Scholar]
- Duplaga, M. , & Grysztar, M. (2021). The association between future anxiety, health literacy and the perception of the COVID‐19 pandemic: A cross‐sectional study. Healthcare, 9(1), 1–18. 10.3390/healthcare9010043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp, S. , Borsboom, D. , & Fried, E. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng, S. Y. , Zhang, Q. C. , & Ho, S. M. Y. (2021). Fear and anxiety about COVID‐19 among local and overseas Chinese university students. Health and Social Care in the Community, 29(6), e249–e258. 10.1111/hsc.13347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foygel, R. , & Drton, M. (2010). Extended Bayesian information criteria for Gaussian graphical models. In Advances in neural information processing systems (Vol. 23. pp. 604–612). 10.48550/arXiv.1011.6640 [DOI] [Google Scholar]
- Funkhouser, C. J. , Chacko, A. A. , Correa, K. A. , Kaiser, A. J. E. , & Shankman, S. A. (2021). Unique longitudinal relationships between symptoms of psychopathology in youth: A cross‐lagged panel network analysis in the ABCD study. Journal of Child Psychology and Psychiatry, 62(2), 184–194. 10.1111/jcpp.13256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haatainen, K. M. , Tanskanen, A. , KylmÄ, J. , Honkalampi, K. , Koivumaa‐Honkanen, H. , Hintikka, J. , Antikainen, R. , & Viinamäki, H. (2003a). Gender differences in the association of adult hopelessness with adverse childhood experiences. Social Psychiatry and Psychiatric Epidemiology, 38(1), 12–17. 10.1007/s00127-003-0598-3 [DOI] [PubMed] [Google Scholar]
- Haatainen, K. M. , Tanskanen, A. , Kylmä, J. , Honkalampi, K. , Koivumaa‐Honkanen, H. , Hintikka, J. , Antikainen, R. , & Viinamäki, H. (2003b). Stable hopelessness and its predictors in a general population: A 2‐year follow‐up study. Suicide and Life‐Threatening Behavior, 33(4), 373–380. 10.1521/suli.33.4.373.25237 [DOI] [PubMed] [Google Scholar]
- Hadley, S. A. , & MacLeod, A. K. (2010). Conditional goal‐setting, personal goals and hopelessness about the future. Cognition and Emotion, 24(7), 1191–1198. 10.1080/02699930903122521 [DOI] [Google Scholar]
- Haslbeck, B. J. M. , & Waldorp, L. J. (2020). mgm: Estimating time‐varying mixed graphical models in high‐dimensional data. Journal of Statistical Software, 93(8), 1–46. 10.18637/jss.v093.i08 [DOI] [Google Scholar]
- Jones, P. (2021). networktools: Tools for identifying important nodes in networks. R package version 1.3.0. https://CRAN.R-project.org/package=networktools
- Kazan Kızılkurt, O. K. , Yılmaz, A. , Noyan, C. O. , & Dilbaz, N. (2021). Health anxiety during the early phases of COVID‐19 pandemic in Turkey and its relationship with postpandemic attitudes, hopelessness, and psychological resilience. Perspectives in Psychiatric Care, 57(1), 399–407. 10.1111/ppc.12646 [DOI] [PubMed] [Google Scholar]
- Kocalevent, R.‐D. , Finck, C. , Pérez‐Trujillo, M. , Sautier, L. , Zill, J. , & Hinz, A. (2017). Standardization of the Beck Hopelessness Scale in the general population. Journal of Mental Health, 26(6), 516–522. 10.1080/09638237.2016.1244717 [DOI] [PubMed] [Google Scholar]
- Li, Y. , Zhao, J. , Ma, Z. , McReynolds, L. S. , Lin, D. , Chen, Z. , Wang, T. , Wang, D. , Zhang, Y. , Zhang, J. , Fan, F. , & Liu, X. (2021). Mental health among college students during the COVID‐19 pandemic in China: A 2‐wave longitudinal survey. Journal of Affective Disorders, 281, 597–604. 10.1016/j.jad.2020.11.109 [DOI] [PubMed] [Google Scholar]
- Liu, R. T. , Kleiman, E. M. , Nestor, B. A. , & Cheek, S. M. (2015). The hopelessness theory of depression: A quarter‐century in review. Clinical Psychology, 22(4), 345–365. 10.1111/cpsp.12125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaker, P. H. , Davis, L. W. , & Hunter, N. L. (2004). Neurocognitive, social and clinical correlates of two domains of hopelessness in schizophrenia. Schizophrenia Research, 70(2), 277–285. 10.1016/j.schres.2004.01.007 [DOI] [PubMed] [Google Scholar]
- Ma, Z. , He, Q. , Nie, G. , Jia, C. , & Zhou, L. (2020). Reliability and validity of short Beck Hopelessness Scale in psychological autopsy study among Chinese rural elderly. International Psychogeriatrics, 32(4), 525–531. 10.1017/s1041610219001315 [DOI] [PubMed] [Google Scholar]
- Mac Giollabhui, N. , Nielsen, J. , Seidman, S. , Olino, T. M. , Abramson, L. Y. , & Alloy, L. B. (2018). The development of future orientation is associated with faster decline in hopelessness during adolescence. Journal of Youth and Adolescence, 47(10), 2129–2142. 10.1007/s10964-017-0803-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchetti, I. (2018). Hopelessness: A network analysis. Cognitive Therapy and Research, 43(3), 611–619. 10.1007/s10608-018-9981-y [DOI] [Google Scholar]
- Mertens, G. , Gerritsen, L. , Duijndam, S. , Salemink, E. , & Engelhard, I. M. (2020). Fear of the coronavirus (COVID‐19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, 102258. 10.1016/j.janxdis.2020.102258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullarkey, M. C. , Marchetti, I. , & Beevers, C. G. (2019). Using network analysis to identify central symptoms of adolescent depression. Journal of Clinical Child and Adolescent Psychology, 48(4), 656–668. 10.1080/15374416.2018.1437735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum, B. , & North, C. S. (2020). Mental health and the Covid‐19 pandemic. The New England Journal of Medicine, 383(6), 510–512. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Ratcliffe, M. (2015). Experiences of depression: A study in phenomenology (1st ed.). Oxford University Press. [Google Scholar]
- Ravikumar, P. , Wainwright, M. J. , & Lafferty, J. D. (2010). High‐dimensional Ising model selction using ℓ 1‐regularized logistic regression. The Annals of Statistics, 38(3), 1287–1319. 10.1214/09-AOS691 [DOI] [Google Scholar]
- Robinaugh, D. J. , Hoekstra, R. H. , Toner, E. , & Borsboom, D. (2020). The network approach to psychopathology: A review of the literature 2008–2018 and an agenda for future research. Psychological Medicine, 50(3), 353–366. 10.1017/S0033291719003404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh, D. J. , Millner, A. J. , & McNally, R. J. (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757. 10.1037/abn0000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roepke, A. M. , & Seligman, M. E. (2016). Depression and prospection. British Journal of Clinical Psychology, 55(1), 23–48. 10.1111/bjc.12087 [DOI] [PubMed] [Google Scholar]
- Rubin, G. J. , & Wessely, S. (2020). The psychological effects of quarantining a city. British Medical Association, 368, m313. 10.1136/bmj.m313 [DOI] [PubMed] [Google Scholar]
- Saricali, M. , Satici, S. A. , Satici, B. , Gocet‐Tekin, E. , & Griffiths, M. D. (2020). Fear of COVID‐19, mindfulness, humor, and hopelessness: A multiple mediation analysis. International Journal of Mental Health and Addiction, 20, 1–14. 10.1007/s11469-020-00419-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittmann, V. D. , Cramer, A. O. , Waldorp, L. J. , Epskamp, S. , Kievit, R. A. , & Borsboom, D. (2013). Deconstructing the construct: A network perspective on psychological phenomena. New Ideas in Psychology, 31, 43–53. 10.1016/j.newideapsych.2011.02.007 [DOI] [Google Scholar]
- Seligman, M. E. , & Maier, S. F. (1967). Failure to escape traumatic shock. Journal of Experimental Psychology, 74(1), 1–9. 10.1037/h0024514 [DOI] [PubMed] [Google Scholar]
- Stallard, P. , Richardson, T. , & Velleman, S. (2010). Clinicians' attitudes towards the use of computerized cognitive behaviour therapy (cCBT) with children and adolescents. Behavioural and Cognitive Psychotherapy, 38(5), 545–560. 10.1017/S1352465810000421 [DOI] [PubMed] [Google Scholar]
- Steinberg, L. (2005). Cognitive and affective development in adolescence. Trends in Cognitive Sciences, 9(2), 69–74. 10.1016/j.tics.2004.12.005 [DOI] [PubMed] [Google Scholar]
- Stewart, S. M. , Kennard, B. D. , Lee, P. W. , Mayes, T. , Hughes, C. , & Emslie, G. (2005). Hopelessness and suicidal ideation among adolescents in two cultures. Journal of Child Psychology and Psychiatry, 46(4), 364–372. 10.1111/j.1469-7610.2004.00364.x [DOI] [PubMed] [Google Scholar]
- Tang, B. , Bragazzi, N. L. , Li, Q. , Tang, S. , Xiao, Y. , & Wu, J. (2020). An updated estimation of the risk of transmission of the novel coronavirus (2019‐nCov). Infectious Disease Modelling, 5, 248–255. 10.1016/j.idm.2020.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanne, J. H. , Hayasaki, E. , Zastrow, M. , Pulla, P. , Smith, P. , & Rada, A. G. (2020). Covid‐19: How doctors and healthcare systems are tackling coronavirus worldwide. British Medical Association, 368, m1090. 10.1136/bmj.m1090 [DOI] [PubMed] [Google Scholar]
- Troister, T. , D'Agata, M. T. , & Holden, R. R. (2015). Suicide risk screening: Comparing the Beck Depression Inventory‐II, Beck Hopelessness Scale, and Psychache Scale in undergraduates. Psychological Assessment, 27(4), 1500–1506. 10.1037/pas0000126 [DOI] [PubMed] [Google Scholar]
- Wang, Y. , Hu, Z. , Feng, Y. , Wilson, A. , & Chen, R. (2020). Changes in network centrality of psychopathology symptoms between the COVID‐19 outbreak and after peak. Molecular Psychiatry, 25(12), 3140–3149. 10.1038/s41380-020-00881-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, C. (2020). A novel approach of consultation on 2019 novel coronavirus (COVID‐19)‐related psychological and mental problems: Structured letter therapy. Psychiatry Investigation, 17(2), 175–176. 10.30773/pi.2020.0047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, W. C. , Jia, C. X. , Hu, X. , Qiu, H.‐M. , & Liu, X.‐C. (2015). Beck Hopelessness Scale: Psychometric properties among rural Chinese suicide attempters and non‐attempters. Death Studies, 39(7), 442–446. 10.1080/07481187.2014.970300 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
Data are available upon request from the first author.


