ABSTRACT
The spread of coronavirus disease 2019 posed a public health crisis beginning in January 2020, affecting hospitals and health care personnel worldwide and disrupting perioperative services. Organization leaders at Xijing Hospital, Xi’an, China, developed a mitigation system for the OR that involved creating a pandemic response team to identify and implement appropriate infection control practices to prevent virus transmission. The leaders addressed managing the daily surgery schedule through patient screening and a focus on the urgency and volume of procedures. They required increased use of personal protective equipment and more stringent cleaning and disinfection protocols and ensured that the physical and mental health of staff members were monitored and prioritized. This article describes how leaders implemented these enhanced processes to protect personnel from infection as they continued to provide patient care. It also describes how high‐risk procedures involving patients with confirmed or suspected infections were managed and discusses lessons learned.
Keywords: coronavirus disease 2019 (COVID‐19), pandemic response team, patient screening, personal protective equipment (PPE), infection prevention and control
The coronavirus disease 2019 (COVID‐19) pandemic has caused more than 531 million confirmed infections and more than 6.3 million deaths worldwide. 1 In consideration of the high risk for disease transmission, the World Health Organization (WHO) Emergency Committee agreed that the outbreak met the criteria for a Public Health Emergency of International Concern on January 30, 2020, 2 and the WHO Director‐General declared this health emergency the same day. 3 On March 11, 2020, the WHO Director‐General officially characterized COVID‐19 as a pandemic. 4 This article describes how leaders at a hospital in China reacted and adapted to the emerging threat, took measures to protect personnel, managed patients infected with COVID‐19 during high‐risk procedures, and ensured quality patient care.
PANDEMIC RESPONSE
Between February 1 and March 31, 2020, surgeons at Xijing Hospital, Xi’an, China, performed 3,398 surgical procedures, 1,047 of which required general anesthesia and lasted several hours (eg, aortic dissection repair, exploratory laparotomy for acute abdomen, orthopedic trauma procedures, craniocerebral procedures). A total of 324 perioperative personnel (ie, 130 surgeons and anesthesiologists, 158 nurses, and 36 health care attendants) made direct contact with these patients. Perioperative leaders (ie, we) used national regulations 5 , 6 and guidelines 7 to develop a response system for the OR that outlined the implementation of new infection control measures during the pandemic and addressed daily schedule, surgical team, and personnel management. At the time of this writing, no perioperative personnel have experienced a COVID‐19 infection or any COVID‐19–related complications as a result of patient exposure.
Key Takeaways.
The coronavirus disease 2019 (COVID‐19) pandemic challenged health care leaders to develop a response plan that would allow personnel to provide high‐quality patient care safely while minimizing the risk of COVID‐19 transmission.
At one hospital in China, perioperative leaders convened a pandemic response team to determine updated requirements for perioperative patients and personnel. Perioperative leaders adjusted the daily schedule as needed according to the urgency and volume of procedures.
The pandemic response team implemented increased precautions to prevent disease transmission, including multiple layers of personal protective equipment, either a negative‐pressure OR or an OR with separate air‐purification processes for patients with suspected or confirmed infection, thorough environmental cleaning, and monitoring and quarantining personnel after any possible exposure.
As the intensity of the pandemic lessened, it became clear that some of the measures taken may have increased costs and not been as effective as originally planned (eg, frequent cleaning of areas that did not involve patient care). Overall, the COVID‐19 pandemic served to increase the awareness of infection prevention and control practices in perioperative areas, and no personnel at the hospital contracted COVID‐19 or experienced COVID‐19–related complications from patient exposure.
Perioperative administrators (eg, OR head nurse) created inpatient reception plans according to the Chinese Center for Disease Control and Prevention guidelines 8 and revised surgery regulations for each perioperative department. Leaders evaluated surgical tasks and schedules and allocated human resources accordingly. To ensure safety and efficiency in the OR and protect staff members from infection, leaders implemented an improved response system that focused on personnel and perioperative processes.
Daily Schedule Management
Perioperative leaders adjusted the daily schedule according to the urgency and volume of procedures. Leaders and surgeons prioritized emergent procedures and, when possible, postponed elective procedures for patients with a confirmed or suspected COVID‐19 infection. When the procedure volume was too high, leaders and surgeons canceled elective procedures. For example, perioperative leaders adjusted procedure volume and reduced the number of procedures (ie, from 12,506 from February 1 to March 31, 2019, to 3,398 from February 1 to March 31, 2020); they also prioritized procedures according to the patient’s needs and medical urgency.
Leaders and surgeons prioritized emergent procedures and, when possible, postponed elective procedures for patients with a confirmed or suspected COVID‐19 infection.
Patient Screening
Patients requiring emergent surgery underwent testing for COVID‐19 before procedures. If the patient’s condition was too critical to wait for the test results, at least two members of the hospital’s expert evaluation team weighed the necessity of the procedure before surgery. Patients who were scheduled for elective surgery underwent COVID‐19 screening according to the facility guideline, and the surgeon and anesthesiologist confirmed the results. If the patient’s test result was negative, the team proceeded with performing the elective procedure.
Perioperative Processes
Perioperative leaders strictly limited access to the OR and did not allow visitors (eg, the patient’s family members or friends) to enter. Personnel involved in a particular procedure could enter and leave the designated OR. Organization leaders required all health care workers (HCWs) to adhere to the facility’s perioperative dress code and strictly prohibited personnel from leaving the OR while wearing the surgical gowns and gloves that they had worn during a procedure. To prevent cross infection when there were two consecutive procedures in the same OR, the surgeons, anesthesia professionals, and nurses who were involved in the first procedure were not allowed to transfer patients out of the OR. Perioperative leaders assigned designated personnel groups comprising one perioperative nurse and one attending medical staff member who were not associated with the procedure to transfer patients in and out of the OR.
Facility leaders increased occupational protection of personnel (ie, use of personal protective equipment [PPE]) and facilities management personnel placed hand sanitation stations containing fast‐acting disinfectants (eg, 75% alcohol, hydrogen peroxide) at all OR entrances and in corridors and office areas. Personnel disinfected their hands after each patient contact and wore gloves whenever they anticipated contact with a patient’s blood or other body fluids. The leaders required personnel to replace their gloves, masks, and goggles when the items became damaged or contaminated with blood or other body fluids.
Perioperative leaders also strengthened the cleaning and disinfection protocol in the perioperative environment. In addition to the strict cleaning and disinfection of the ORs (eg, at least once for each scheduled procedure), environmental services (EVS) personnel cleaned and disinfected all corridors and other rooms (eg, staff member lounge, OR control desk) at least four times each day. They specifically used 75% alcohol‐ or chlorine‐containing wipes to carefully clean public areas and high‐contact surfaces in the ORs (eg, doorknobs, light switches, phones, computers) before and after each procedure. They conducted air sterilization with ultraviolet light and a high‐filtration system at least once a day. The EVS personnel also cleaned and disinfected the floors at least twice a day. The effective concentration of chlorine‐containing disinfectant was increased from 1,000 to 2,000 mg/L for disinfection of surfaces. Perioperative personnel left all items that directly or indirectly contacted patients in the OR. During the postprocedure turnover process, EVS personnel cleaned reusable items and disposed of single‐use items without contaminating areas outside the OR. All cleaning and disinfection procedures complied with relevant national standards 8 , 9 and regulations 5 , 6 and practice guidelines. 7
To conserve OR supplies and PPE, perioperative leaders ensured these items were managed with precision and care. Assigned personnel prepared the items and checked expiration dates on a daily basis for planned and possible emergent procedures.
Perioperative Team Management
Researchers have identified a relationship between perioperative team management and the team’s performance. 10 They determined that there are seven core values that contribute to optimal team performance:
a common goal,
knowledge of individual roles,
mutual respect and support,
open communication,
high morale,
a positive work ethic, and
effective leadership.
Organization leaders at our facility convened a special pandemic response team to foster optimal functioning among perioperative teams and formulate and implement management processes for the OR during the pandemic. This response team comprised medical staff members from the Departments of Surgery and Anesthesiology, perioperative personnel, and members of the infection control and prevention team that existed before the pandemic.
Perioperative staff members collected preoperative COVID‐19 test results and verified that patients underwent all the necessary preoperative examinations. The pandemic response team members conducted preoperative surgical risk assessments, evaluated the risk of occupational exposure for personnel, and determined the level of protection and specific measures necessary for each member of the team.
Before each procedure, a designated perioperative nurse checked each team member to ensure proper use of required PPE, including surgical scrubs, a disposable hair cover, two surgical masks, latex gloves, a medical protective mask, a fluid‐resistant gown, protective coveralls, goggles, disposable shoe covers, powered air‐purifying respirator headgear, and additional equipment as needed (eg, protective head lamp holder), to prevent direct contact with the patient’s blood or other body fluids (Figure 1). The physical encumbrance of wearing PPE was associated with reduced peripheral vision and auditory acuity, thereby impairing communication among perioperative team members. During procedures, team members used special microphones and simplified processes to facilitate communication and avoid the risk of infection or cross‐contamination related to unnecessary manipulation of potentially contaminated items. Perioperative nurses were fully responsible for implementing these infection prevention and control measures to protect the occupational safety of all surgical team members.
Figure 1.

Scrubbed team members wearing required personal protective equipment perform surgery in the OR at Xijing Hospital, Air Force Medical University, Xi’an, China, during the coronavirus disease 2019 pandemic.
Personnel Management
The head nurse monitored and supervised personnel who implemented the perioperative infection prevention and control processes. All medical staff members, nurses, EVS personnel, and security personnel who might possibly contact patients with a confirmed or suspected COVID‐19 infection participated in just‐in‐time education sessions on the specific processes related to COVID‐19 infection prevention and control. In addition, facility leaders required all personnel to complete and pass online tests related to the changed processes.
Perioperative leaders closely monitored the health status of all personnel (eg, temperature) and recorded any respiratory symptoms. Leaders immediately reported any identified abnormalities and sent the affected staff members to quarantine for additional examination. The leaders scheduled personnel according to the number of elective and anticipated emergent procedures. Organization leaders restricted in‐person staff meetings and gatherings and held online meetings if necessary. Because surgical volume was reduced, leaders also minimized the workload to ensure adequate rest for personnel.
Some personnel showed signs of anxiety and depression associated with the working hours and the strain of coping during this immensely difficult time; therefore, mental health was a priority. After completing the required just‐in‐time training, all staff members were able to better understand the situation and assess risks. Organization leaders provided timely mental health support and psychological treatment when needed to ensure that morale and quality of work remained high.
CARE OF PATIENTS INFECTED WITH COVID‐19
Generally, patients diagnosed with or suspected of being infected with COVID‐19 underwent procedures in a separate OR with a pressure differential of −5 Pascals (ie, a negative‐pressure OR). If such an OR was not available, personnel performed procedures in an available OR with separate air purification processes and special signage. Because all ORs shared the same air purification system, personnel in the designated OR maintained the system in a closed status until the end of the procedure to prevent transmission of potentially contaminated air to other ORs, at which time they disinfected the OR.
Leaders assigned a minimal number of personnel in the OR to decrease the possibility of staff member exposure to COVID‐19 (Figure 2). The perioperative team usually included
three nurses (ie, two inside the OR, one outside),
two anesthesia professionals (ie, one inside the OR, one outside), and
at least one surgeon.
Figure 2.
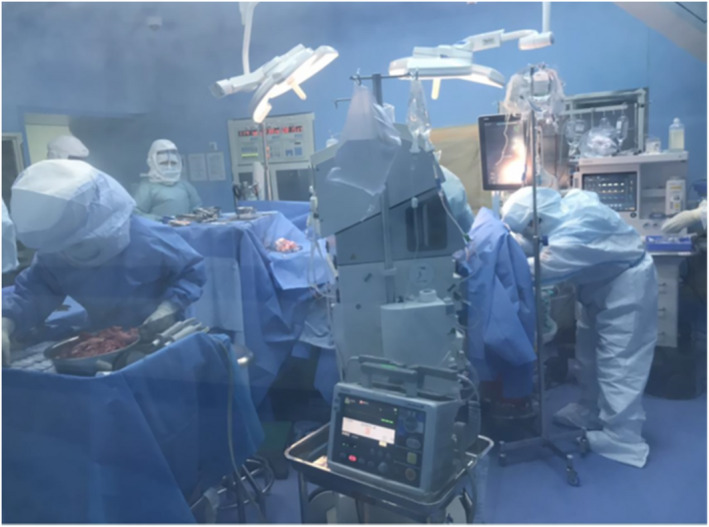
Perioperative team members wearing required personal protective equipment perform intraoperative tasks in the OR at Xijing Hospital, Air Force Medical University, Xi’an, China, during the coronavirus disease 2019 pandemic.
High‐level protection measures were taken and all team members inside the OR wore the required PPE as previously described. The nurses and anesthesia professionals outside the OR employed lower‐level protection measures (eg, gloves, masks, disposable hair covers, protective foot coverings) because they were not directly caring for the patient.
Perioperative Infection Control
To reduce the risk of contamination, personnel minimized the surgical items (eg, supplies, instruments, equipment) in the OR and only prepared the items that they knew were needed for a specific procedure. When possible, perioperative team members preferred to use disposable items. Personnel placed disposable plastic covers on all computer equipment (eg, keyboards, monitors) and medical device controls and then replaced the covers after each procedure. To avoid accidental injury and subsequent contamination, scrubbed personnel used a no‐touch technique to pass sharp instruments during procedures.
During transport, patients wore a medical protective mask if their condition allowed and staff members used a transport cart equipped with negative pressure (Figure 3) and entered the OR through a negative‐pressure corridor. All patients who did not receive general anesthesia wore a surgical mask during the procedure if their condition allowed. When intubation was required, the anesthesia professional placed a disposable filter between the endotracheal tube and the respiratory circuit to reduce the bioburden inside the general anesthesia devices. Personnel used wipes (eg, 75% alcohol, hydrogen peroxide) to disinfect patient care items and equipment after use (Figure 4).
Figure 3.

Perioperative personnel wearing required personal protective equipment use a transport cart equipped with negative pressure to transport a patient from the OR at Xijing Hospital, Air Force Medical University, Xi’an, China, during the coronavirus disease 2019 pandemic.
Figure 4.
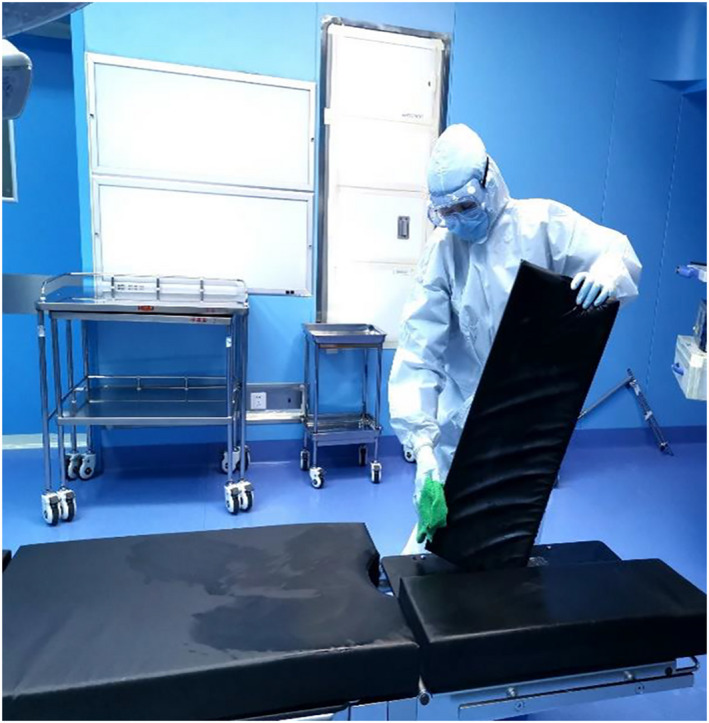
Personnel perform disinfection in the OR at Xijing Hospital, Air Force Medical University, Xi’an, China, during the coronavirus disease 2019 pandemic.
To minimize external contamination, personnel kept doors closed and opened them infrequently during procedures in both the negative‐pressure OR and the ORs with filtration units. The nurse outside the OR obtained additional items that were needed during the procedure.
Personnel used two sets of negative‐pressure suction devices during procedures. After transporting the patient to the OR, the anesthesia professional placed a mask over the patient’s face and connected it to a negative‐pressure suction device to minimize the diffusion of aerosolized particles. When using any device that produced surgical smoke, a scrubbed team member used the second suction device to collect the smoke plume and reduce diffusion of aerosolized particulate matter as much as possible.
The team members marked all clinical waste, disposal containers for reusable items, and waste bags to indicate possible COVID‐19 contamination. Personnel wrapped other items (eg, IV solution containers) in a double‐layer bag or a medical waste bag and then sealed and labeled the bag.
At the end of the procedure, a perioperative team member placed a clean sheet over the patient before the team moved the patient from the OR bed to the negative‐pressure transport cart. Two members of the team transported the patient to a single‐patient, negative‐pressure ventilation room located in the isolation unit. Personnel then used a 2,000‐mg/L chlorine‐containing solution to clean and disinfect the transport cart. During the disinfection process, personnel removed the mattress from the transport cart and placed it in the OR for cleaning and disinfection with hydrogen peroxide.
After transporting the patient from the OR and disinfecting the OR, including the transport cart mattress, the ventilation was kept closed (ie, not open to outside air) and no personnel were permitted to enter the OR for at least two hours. Personnel sent all waste from procedures involving a patient who may have been infected with COVID‐19 to the supply disinfection center for sterilization before disposal. Personnel then re‐entered the room, opened the ventilation system to outside air, and repeated the disinfection process with a 2,000‐mg/L chlorine‐containing disinfectant. Personnel used a 5,000‐mg/L chlorine‐containing solution to disinfect any surfaces that were visibly contaminated with blood or other body fluids. After 30 minutes, personnel wiped all surfaces with clean tap water.
At the completion of the cleaning and disinfection process, continuous negative‐pressure ventilation remained open for three hours and the OR was marked with a special sign indicating that it was not ready for use. The infection prevention personnel used a microbial air sampler to collect air samples that were cultured in a thermostatic incubator for 48 hours. The laboratory personnel calculated the colony‐forming units and identified samples that met designated criteria indicating that the OR could be used. All perioperative personnel who directly contacted the patient with confirmed or suspected COVID‐19 were quarantined with medical observation for no more than two weeks. When necessary, perioperative leaders addressed staff member assignments to meet the needs of patients.
DISCUSSION
As a result of the global pandemic, organization leaders at our facility closed many departments for the safety of patients and personnel. However, the intensive care units and perioperative, emergency, infectious disease, and pneumology departments remained open and personnel continued to provide essential and life‐saving services.
Unlike elective procedures, emergent procedures should be performed immediately without delay, even during a pandemic. When medical staff members determine that a condition is potentially fatal or likely to permanently impair function, they should make every effort to perform necessary treatment immediately to avoid risks to the patient’s health or life. 11 During the pandemic, personnel needed to take appropriate measures to balance life‐saving techniques with infection prevention and control.
Infection Prevention Practices
Perioperative infection prevention practices are very different from those in nonperioperative health care environments 12 , 13 because undergoing operative or other invasive procedures puts perioperative patients at risk for developing surgical site infections. 14 , 15 Further, aerosol‐generating procedures, such as the administration of general anesthesia, are a primary source of COVID‐19 infection. 16 Therefore, perioperative personnel used enhanced PPE and cleaning practices for each procedure to prevent disease transmission.
During the pandemic, personnel needed to take appropriate measures to balance life‐saving techniques with infection prevention and control.
Cumbersome PPE and the limited field of vision caused by wearing goggles and face shields may increase the difficulty of surgical procedures. Use of PPE, especially powered air‐purifying respirators, can impair communication among perioperative team members; increased concentration and close cooperation among team members may be required. 17 Finally, the severity and infectious nature of COVID‐19 may cast a shadow on a patient’s care. For example, some infected patients experience airway compromise or dyspnea, which may increase the risks associated with a planned procedure. Therefore, collaboration and coordination is an essential part of ensuring a successful procedure and adequate protection of patients and HCWs.
Personnel Needs
In terms of personnel protection and training for infection prevention, all personnel should have knowledge of hospital regulations—for example, those related to PPE removal. This may be even more important than PPE protection, because failure to adhere to these rules may lead to infection transmission on a larger scale, despite the use of PPE. 18 Psychological support is also important for personnel who care for patients with a confirmed or suspected COVID‐19 infection in the OR. In general, there was an underlying sense of dread and fear among HCWs during the pandemic. 19 Studies suggest that psychological support helps individuals cope with their feelings and emotions during periods of uncertainty. 20 , 21 , 22 , 23
LESSONS LEARNED
More than a year after the beginning of the pandemic, the pressure to prevent the spread of COVID‐19 has lessened, and the availability of vaccinations has allowed HCWs in China to move forward. Patients continue to undergo nucleic acid testing for the virus before surgery; however, of the patients currently receiving care at our facility, very few have suspected or confirmed COVID‐19, and therefore some of the interventions we implemented no longer have clinical benefit and have been discontinued. Still, reviewing the lessons we learned during the initial stages of the pandemic should help us continue to improve our current infection control system and prepare for future infectious disease outbreaks.
The pandemic has been a test for our national public health system and hospital infection management protocols. After the outbreak of severe acute respiratory syndrome in 2002, the Chinese government established an online reporting system for infectious diseases; 24 this system was then used during the COVID‐19 pandemic. The aim of the reporting system is to control the source of infection in time to avoid the spread of disease. After local authorities reported the COVID‐19 outbreak to the Chinese Center for Disease Control and Prevention, health care leaders at our facility received instructions to implement the hospital’s infection control system and expected personnel in all departments to implement measures (eg, disinfect surfaces, quarantine after exposure to the virus) to prevent the transmission of COVID‐19. Considering their key role in preventing and controlling health care–associated infections, perioperative personnel should take responsibility for implementing the infection prevention measures that meet the specific needs of the OR. Examples of perioperative‐specific factors that may affect nursing practice during a disease outbreak include the
contained nature of the OR, which may limit staff member interaction with infected individuals;
use of reusable items that require effective disinfection rather than disposal; and
unique disinfection needs of OR equipment and furnishings.
We realized that a detailed plan based on specific criteria to determine patient status was needed (ie, to identify patients who tested positive for or were likely infected with COVID‐19) to implement subsequent work protocols to protect patients and personnel. The plan emphasized disinfection of environmental surfaces, postoperative treatment (eg, disposal) of patient care items, and occupational protection of personnel.
When a patient’s infection status is unknown, surgeons perform emergent surgery in the negative‐pressure OR; after the procedure, patients undergo nucleic‐acid testing for COVID‐19. Staff members also undergo nucleic‐acid testing once per month and adhere to the facility’s infection prevention medical observation protocols (eg, quarantining until the COVID‐19 test results are known) after caring for patients with a confirmed or suspected COVID‐19 infection who undergo surgery.
As we reflected on the development and implementation of the response system, we found that the overarching goal of the measures used at our facility was to prevent COVID‐19 transmission at the lowest possible financial cost. Although none of the staff members have tested positive for COVID‐19 during the pandemic, some of the measures taken produced little effect and many of them required improvement. For example, we believe that frequent and thorough disinfection of all rooms in the perioperative suite may increase costs with no increase in preventive effect and that personnel should perform disinfection according to the risk of contamination. For areas in which personnel do not provide patient care (eg, library, conference room), the risk of contamination is low and one disinfection each day is adequate. Moreover, medical staff members and perioperative personnel without a history of close contact with patients with confirmed or suspected COVID‐19 can return to work after two consecutive negative nucleic acid tests.
CONCLUSION
The COVID‐19 outbreak caused health care leaders to identify and implement the most effective infection prevention and control measures for curbing highly infectious diseases. Successful implementation of measures designed to prevent disease transmission requires all HCWs to strictly adhere to relevant protocols—at our facility, our response system helped perioperative personnel avoid contracting COVID‐19 when caring for patients. Additionally, we found that forming a specialized interdisciplinary pandemic response team was useful in planning and implementing control measures in the OR during this unprecedented crisis.
Editor’s note: The processes described in this article may not conform to guidance from governmental agencies and professional organizations based in the United States and may not be generalizable to other settings.
Biographies
Dongmei Bian is the head nurse in the plastic surgery OR at Xijing Hospital, Air Force Medical University, Xi’an, China. Ms Bian has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.
Weina Jia is a nurse in the plastic surgery OR at Xijing Hospital, Air Force Medical University, Xi’an, China. Ms Jia has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.
Yana Wang is a nurse in the plastic surgery OR at Xijing Hospital, Air Force Medical University, Xi’an, China. Ms Wang has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.
Na Ma is a nurse in the plastic surgery OR at Xijing Hospital, Air Force Medical University, Xi’an, China. Ms Ma has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.
Yu Wang is a nurse in the OR at Xijing Hospital, Air Force Medical University, Xi’an, China. She was the head nurse in the OR at Xijing Hospital at the time this article was written. Ms Wang has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.
Qian Wang is the head nurse in the OR at Xijing Hospital, Air Force Medical University, Xi’an, China. Ms Wang has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.
REFERENCES
- 1. WHO coronavirus (COVID‐19) dashboard . World Health Organization. https://covid19.who.int/. Updated June 9, 2022. Accessed June 9, 2022.
- 2. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019‐nCoV) [press release]. Geneva, Switzerland: World Health Organization; January 30, 2020. https://www.who.int/news/item/30‐01‐2020‐statement‐on‐the‐second‐meeting‐of‐the‐international‐health‐regulations‐(2005)‐emergency‐committee‐regarding‐the‐outbreak‐of‐novel‐coronavirus‐(2019‐ncov). Accessed May 17, 2022.
- 3. COVID 19 Public Health Emergency of International Concern (PHEIC) . Global research and innovation forum: towards a research roadmap. World Health Organization. https://www.who.int/docs/default‐source/coronaviruse/global‐research‐and‐innovation‐forum‐towards‐a‐research‐roadmap.pdf. Published February 12, 2020. Accessed May 17, 2022.
- 4. WHO Director‐General’s opening remarks at the media briefing on COVID‐19 ‐ 11 March 2020. World Health Organization . https://www.who.int/director‐general/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19‐‐‐11‐march‐2020. Published March 11, 2020. Accessed May 5, 2022.
- 5. Ministry of Health of the PRC. Regulation of disinfection technique in healthcare settings (WS/T 367‐2012) . https://www.chinesestandard.net/PDF.aspx/WST367‐2012. Published April 5, 2012. Accessed May 17, 2022.
- 6. State Administration of Market Regulation; Standardization Administration of PRC . General requirements for ordinary objects surface disinfectant (GB 27952‐2020). https://www.gb‐gbt.cn/PDF/English.aspx/GB27952‐2020. Published April 9, 2020. Accessed May 17, 2022.
- 7. Guyan W; Perioperative Infection Control Society of Chinese Society of Cardiothoracic and Vascular Anesthesiology Task Force on Disinfection and Sterilization of Breathing Circuit in Anesthesia Machine. Recommendations for disinfection and sterilization of breathing circuit in anesthesia machine. Article in Chinese. Chin J Anesthesiol. 2018;38(12):1417‐1420. [Google Scholar]
- 8. National Health Commission of the People’s Republic of China . Protocol for prevention and control of COVID‐19 (edition 6). China CDC Wkly. 2020;2(19):321‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Professional Committee for Infection Control . Standard for nosocomial infection control in operating department. Article in Chinese. Published 2019.
- 10. Kumar H, Morad R, Sonsati M. Surgical team: improving teamwork, a review. Postgrad Med J. 2019;95(1124):334‐339. [DOI] [PubMed] [Google Scholar]
- 11. Fahimi J, Goldfrank L. Principles of social emergency medicine. Ann Emerg Med. 2019;74(suppl 5):S6‐S10. [DOI] [PubMed] [Google Scholar]
- 12. Hambraeus A, Lytsy B. Infection control and what to wear in the operating room [letter to the editor]. Clin Infect Dis. 2018;67(1):159. [DOI] [PubMed] [Google Scholar]
- 13. Loftus RW. Infection control in the operating room: is it more than a clean dish? Curr Opin Anaesthesiol. 2016;29(2):192‐197. [DOI] [PubMed] [Google Scholar]
- 14. Ling ML, Apisarnthanarak A, Abbas A, et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob Resist Infect Control. 2019;8:174. 10.1186/s13756-019-0638-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Parizh D, Ascher E, Raza Rizvi SA, Hingorani A, Amaturo M, Johnson E. Quality improvement initiative: preventative surgical site infection protocol in vascular surgery. Vascular. 2018;26(1):47‐53. [DOI] [PubMed] [Google Scholar]
- 16. Tang LY, Wang J. Anesthesia and COVID‐10: what we should know and what we should do. Semin Cardiothorac Vasc Anesth. 2020;24(2):127‐137. [DOI] [PubMed] [Google Scholar]
- 17. Peng PWH, Wong DT, Bevan D, Gardam M. Infection control and anesthesia: lessons learned from the Toronto SARS outbreak. Can J Anaesth. 2003;50(10):989‐997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Honda H, Iwata K. Personal protective equipment and improving compliance among healthcare workers in high‐risk settings. Curr Opin Infect Dis. 2016;29(4):400‐406. [DOI] [PubMed] [Google Scholar]
- 19. Dong L, Bouey J. Public mental health crisis during COVID‐19 pandemic, China. Emerg Infect Dis. 2020;26(7):1616‐1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Petzold MB, Plag J, Ströhle A. Umgang mit psychischer belastung bei gesundheitsfachkräften im rahmen der COVID‐19‐pandemie [Dealing with psychological distress by healthcare professionals during the COVID‐19 pandemia]. Nervenarzt. 2020;91(5):417‐421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ćosić K, Popović S, Šarlija M, Kesedžić I. Impact of human disasters and COVID‐19 pandemic on mental health: potential of digital psychiatry. Psychiatr Danub. 2020;32(1):25‐31. [DOI] [PubMed] [Google Scholar]
- 22. Röhr S, Müller F, Jung F, Apfelbacher C, Seidler A, Riedel‐Heller SG. Psychosoziale folgen von quarantänemaßnahmen bei schwerwiegenden coronavirus‐ausbrüchen: ein rapid review [Psychosocial impact of quarantine measures during serious coronavirus outbreaks: a rapid review]. Psychiatr Prax. 2020;47(4):179‐189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Etkind SN, Bone AE, Lovell N, et al. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID‐19 pandemic. J Pain Symptom Manage. 2020;60(1):e31‐e40. 10.1016/j.jpainsymman.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hao P, Liu N, Li Z, Xi J, Tan F. Jiaqi Ma, China CDC’s Chief Expert of Health Information. China CDC Wkly. 2020;2(38):749‐750. [DOI] [PMC free article] [PubMed] [Google Scholar]


