Abstract
Background
Prior to the COVID‐19 pandemic there were many barriers to telemedicine primary care for adults ≥65 years including insurance coverage restrictions and having lower digital access and literacy. With the pandemic, insurance coverage broadened and many older adults utilized telemedicine creating an opportunity to learn from their experiences to inform future policy.
Methods
Between April 2020 and June 2021, we conducted a cross‐sectional multimethod study of English‐speaking, cognitively‐intact, adults ≥65, who had a phone‐only and/or video telemedicine visit with their primary care physician within one large Massachusetts health system (10 different practices) since March 2020. The study questionnaire asked participants their overall satisfaction with telemedicine (7‐point scale) and to compare telemedicine with in‐person care. We used linear regression to examine the association between participants' demographics, Charlson comorbidity score, and survey completion date with their satisfaction score. The questionnaire also included open‐ended questions on perceptions of telemedicine; which were analyzed using qualitative methods.
Results
Of 278 eligible patients reached, 208 completed the questionnaire; mean age was 74.4 years (±4.4), 61.5% were female, 91.4% were non‐Hispanic White, 64.4% had ≥1 comorbidity, and 47.2% had a phone‐only visit. Regardless of their age, participants reported being satisfied with telemedicine; median score was 6.0 on the 7‐point scale (25th percentile = 5.0 and 75th percentile = 7.0). Non‐Whites satisfaction scores were on average 1 point lower than those of non‐Hispanic Whites (p = 0.02). Those with comorbidity reported scores that on average were 0.5 points lower than those without comorbidity (p = 0.07). Overall, 39.5% felt their telemedicine visit was worse than in‐person care; 4.9% thought it was better. Participants appreciated telemedicine's convenience but described frustrating technical challenges. While participants preferred in‐person care, most wanted telemedicine to remain available.
Conclusions
Adults ≥65 reported being satisfied with primary care telemedicine during the pandemic's first 14 months and wanted telemedicine to remain available.
Keywords: older adults, primary care, telemedicine
Key points
Regardless of their age, most of the 208 adults ≥65 years that participated in this multimethod study about telemedicine primary care were satisfied with their telemedicine visit; however, non‐Whites and those with comorbidity reported being less satisfied.
In total, 39.5% of participants felt telemedicine was worse than a traditional in‐person visit (only 4.9% said it was better than an in‐person visit) and 22.2% reported that they would be less likely to ask about multiple health problems during a telemedicine visit (4.8% said they would be more likely).
In open‐ended comments, participants described being satisfied with telemedicine and appreciating its convenience but also described technical difficulties and a preference for in‐person care. Despite this, most participants wanted telemedicine to remain an option.
Why does this paper matter?
As policy makers are debating the future coverage of telemedicine, there is great and immediate need to understand older adults' experience with telemedicine. In a multimethod study of 208 adults ≥65 from one large health system in Boston, we found that most older adults were satisfied with their telemedicine visits, especially Whites and those in good health, and wanted telemedicine to remain available after the pandemic. However, many older adults still preferred in‐person care particularly for annual wellness visits and for complex care.
INTRODUCTION
Prior to the COVID‐19 pandemic, provision of primary care via telemedicine (care delivered remotely through telephone and/or video technology) was generally limited to rural settings or within specific health systems, such as the Veteran's Administration, due to insurance coverage restrictions. 1 , 2 Pre‐pandemic, telemedicine was found to be effective for monitoring chronic conditions such as hypertension, 2 , 3 , 4 , 5 , 6 but not a substitute for in‐person care of older adults with complex health issues. 7 Patients reported being satisfied with telemedicine 8 and appreciated its convenience 9 ; but in a 2010 randomized trial preferred in‐person care. 10
Pre‐pandemic, studies also found that older adults were the least likely to use telemedicine due to lower broadband internet access, lower digital literacy, Medicare coverage restrictions, and greater prevalence of sensory impairments making telemedicine more challenging. 11 , 12 In February 2020, only 0.1% of Fee‐For‐Service Medicare primary care visits occurred via telemedicine. 13 Due to stay‐at‐home orders to reduce COVID‐19 transmission; the inclusion of telehealth provisions in the Coronavirus Aid, Relief, and Economic Security (CARES) Act; and Medicare lifting restrictions on telehealth‐eligible services, technologies, and geographic and site service requirements; by April 2020, 43.5% of Fee‐For‐Service Medicare primary care visits occurred via telemedicine (73.1% in Boston, MA). 13
Current law mandates that telehealth flexibilities (e.g., continued coverage of audio‐only visits or telemedicine from home) continue for 151 days after the end of the public health emergency (currently slated for October 13, 2022) and policy‐makers are debating telemedicine's future. Several telehealth bills have been introduced to extend Medicare telehealth flexibilities to allow more time for data collection. To inform future policy, we interviewed adults ≥65 years to learn about their experience with telemedicine since the pandemic. We used both quantitative and qualitative methods since patients tend to rate their satisfaction with telemedicine highly but in open‐ended comments share more challenges. 14 We hypothesized that adults ≥75 years would find telemedicine less satisfactory than adults 65–74 due to lower digital access and literacy with increasing age. 15
METHODS
Between April 2020 and June 2021, we surveyed adults ≥65 years who had completed a phone‐only and/or video telemedicine primary care visit with their primary care physician (PCP) within one large health system in Massachusetts since March 2020. Within the health system, we recruited patients from one large academic internal medicine practice, one academic geriatrics practice, and eight community primary care practices (see TableS1 for practice descriptions). When the pandemic began, PCPs in these practices were encouraged to use StarLeaf.com or Google Meet for HIPAA compliant video visits. By April 2020, PCPs were encouraged to sign‐up for Virtual Visits which utilized the SnapMD platform; Doximity video caller was recommended as a back‐up option. By March, 2021, Virtual Visits were incorporated into the health system's electronic medical records (EMR). Beth Israel Deaconess Medical Center's (BIDMC's) IRB deemed this study exempt from further review.
Eligibility and consent
Adults ≥65 years were eligible if they were English‐speaking, received in‐person primary care within the health system in the 12 months prior to March 2020, had ≥1 telemedicine primary care visit (video or phone‐only) since March 16, 2020, and were able to provide consent. We excluded patients on hospice, with severe psychological illness/or cognitive impairment (based on chart review or primary care physician [PCP] report), and/or those who scored ≥9 (indicative of dementia) on the orientation‐memory‐concentration test 16 before telephone interviews.
Recruitment
Using billing records, a BIDMC data manager provided the research team with lists of all potentially eligible patients quarterly during the study. After confirming eligibility via the EMR and obtaining PCP approval, research assistants (RAs) sequentially attempted to reach patients. If the RAs (EG, GA, MK) were unable to reach a patient by telephone and the patient's email was in the EMR then RAs emailed the patient information about the study and a survey‐link. For patients reached by telephone, RAs offered to administer the survey or to send a secure web‐based survey‐link for patients to self‐administer. Over the telephone, RAs assessed patient capacity to participate (see capacity questionnaire, Text S1) and obtained verbal consent. Participants who completed the survey electronically were required to affirm their consent before viewing survey questions. The study was voluntary, no incentive was provided.
Study questionnaire
The questionnaire (see Text S2) included both close‐ended and open‐ended questions. It asked participants their overall satisfaction with telemedicine from very dissatisfied to very satisfied (7‐point scale), to rate their confidence (5‐point scale) on using a landline or cell‐phone for telephone visits or a computer/tablet for video visits, and about the length and type of telemedicine (phone, video, both) they experienced. The questionnaire also asked participants to compare telemedicine to in‐person visits (better, just as good, worse); to compare their likelihood to ask questions about their health, medicines, or to share concerns during telemedicine versus in‐person visits; and to complete a 10‐item satisfaction with telemedicine index (included questions on the quality, duration, comfort, convenience, of the telemedicine visit). 8 , 17 Participants were also asked to complete the 3‐item validated collaboRATE scale (highest [27] vs. lower scores) to understand their perceptions of shared decision‐making during telemedicine. 18 In addition, the survey included questions to estimate participant 10‐year life expectancy, 19 Charlson comorbidity, 20 physical function, 21 health and computer literacy, and about their sociodemographics (e.g., age, race/ethnicity). 22 In open‐ended questions, participants were asked to share their thoughts on (1) how telemedicine compared to in‐person care (and to compare telephone‐only to video visits if they experienced both); (2) how to improve telemedicine; and (3) when telemedicine may be most useful. Participants were additionally asked to share three words to describe telemedicine which we used to develop a word cloud. At the end of the survey, participants were asked to share any additional thoughts on telemedicine. We pilot tested the survey with five older adults before study initiation.
Statistical methods
Statistical analyses were completed using SAS statistical software, version 9.4. While the study was designed to be descriptive, we aimed to recruit 200 patients (at least 75 adults ≥75 years) to have 0.86 power to detect a one point difference in satisfaction with telemedicine between adults 65–74 and ≥75 years assuming a standard deviation of two on the scale. We used the Wilcoxon rank sum test to examine the association between measures of satisfaction with telemedicine and age (65–74, ≥75). We used chi‐square tests to examine differences in categorical outcomes by age. We used the paired t‐test to compare participant confidence in using landline or cell‐phones for phone visits versus their confidence in using computers/tablets for video visits. We used multivariable linear regression to examine the association between higher telemedicine satisfaction scores and participant age, race/ethnicity, educational attainment, survey completion year, and comorbidity; we considered these variables because telemedicine use has been shown to vary by these factors. 23 , 24
Qualitative methods
We used Braun and Clarke's methods for thematic analyses to identify themes in participants' open‐ended comments about telemedicine. 25 Three investigators (RB, EG, MAS) reviewed the first 20 participants' open‐ended comments to identify themes that emerged and to develop a codebook (Text S3). Once a codebook was agreed upon, all participants' open‐ended comments were coded by at least two investigators. Discrepancies in themes identified by investigators were resolved by consensus. As new themes emerged, new codes were developed and previously coded interviews were recoded. Although thematic saturation was achieved by the 30th participant survey all participants' open‐ended comments were coded. Direct quotes and participants' study identification numbers were used to illustrate themes. Nvivo 11 qualitative software was used for analyses.
RESULTS
Figure S1 demonstrates participant recruitment flow. Of 278 eligible patients reached, 230 agreed to participate, of which 208 completed the survey (84.6% self‐administered the survey) and 94.2% answered ≥1 open‐ended question (89.9% answered all 3 of the core open‐ended questions). Median time for survey completion was 31.5 min (IQR 23.0, 52.5). Participants were similar to those who declined participation based on age and sex. Participant mean age was 74.4 years (±4.4); 47.6% were ≥75 years; 91.4% were non‐Hispanic White, 26.9% had less than a college education; and 38.5% had a community PCP (participants were seen by 63 different PCPs), Table 1. Nearly half (47.2%) of participants had a phone‐only visit, 23.1% had a video visit only, and 29.7% experienced both visit types; 44.7% reported that their telemedicine visit was ≤15 min. Participants ≥75 were similar to those 65–74 years but had shorter estimated life expectancies.
TABLE 1.
Demographics of study participants (n = 208)
| Characteristic | Overall (n = 208) % | Age 65–74 (n = 109; 52.4%) % | Age ≥ 75 (N = 99; 47.6%) % | p value |
|---|---|---|---|---|
| Female | 61.5 | 58.7 | 64.7 | 0.38 |
| Race b | 0.23 | |||
| White non‐Hispanic | 91.4 | 89.9 | 92.9 | |
| Black non‐Hispanic | 5.3 | 6.4 | 4.0 | |
| Hispanic | 0 | 0 | 0 | |
| Other race | 3.4 | 3.7 | 3.0 | |
| Education | 0.61 | |||
| High school or less | 10.1 | 9.2 | 11.1 | |
| Some college | 16.8 | 15.7 | 19.2 | |
| College graduate | 29.3 | 33.0 | 25.3 | |
| Master's/professional degree | 43.8 | 43.1 | 44.4 | |
| Annual household income (n = 201, 103 65–74) | 0.93 | |||
| ≤$65,000 | 21.4 | 21.4 | 21.4 | |
| $66,000‐100,000 | 19.9 | 21.4 | 18.4 | |
| >$100,000 | 29.9 | 28.2 | 31.6 | |
| Prefers not to answer/do not know | 28.9 | 29.1 | 28.6 | |
| Insurance | 0.19 | |||
| Medicaid + Medicare | 7.7 | 8.3 | 7.1 | |
| Medicare + private or Medicare HMO | 82.2 | 81.7 | 82.8 | |
| Medicare + state/federal | 6.7 | 4.6 | 9.1 | |
| Private only | 3.4 | 5.5 | 1.0 | |
| PCP setting | 0.76 | |||
| Academic | 61.5 | 60.6 | 62.6 | |
| Community | 38.5 | 39.5 | 37.4 | |
| Type of telemedicine | 0.87 | |||
| Visit phone only | 47.2 | 47.7 | 46.5 | |
| Video only | 23.1 | 23.9 | 22.2 | |
| Both | 29.8 | 28.4 | 31.3 | |
| Length of telemedicine visit on average | 0.89 | |||
| 15 min or less | 44.7 | 43.1 | 46.5 | |
| 20–<30 min | 30.3 | 32.1 | 28.3 | |
| 30 min or longer | 19.2 | 18.4 | 20.2 | |
| Unsure | 5.8 | 6.4 | 5.1 | |
| Time period of participation | 0.61 | |||
| April 2020 to December 2020 | 43.3 | 45.0 | 41.4 | |
| January 2021 to August 2021 | 56.7 | 55.1 | 58.6 | |
| Marital status married/significant other | 63.5 | 67.0 | 59.6 | 0.27 |
| Other | 36.5 | 33.0 | 40.4 | |
| Charlson Comorbidity Index | 0.74 | |||
| 0 | 35.6 | 35.8 | 35.4 | |
| 1 | 20.7 | 18.4 | 23.2 | |
| 2+ | 43.8 | 45.9 | 41.4 | |
| Life expectancy score on Schonberg index (n = 204) a | 5.4 (±3.2) | 3.7 (±2.6) | 7.3 (±2.7) | <0.0001 |
| Needs help with routine needs (n = 205) | 5.4 | 4.7 | 6.1 | 0.65 |
| Needs help with bathing (n = 206) | 2.4 | 1.9 | 3.2 | 0.58 |
| Lives alone | 28.4 | 27.5 | 29.3 | 0.78 |
| How often do you have someone help you read hospital materials? (n = 203) Sometimes to always | 7.2 | 4.6 | 10.1 | 0.12 |
| Access to computer or cell‐phone with internet | 93.8 | 93.6 | 93.9 | 0.91 |
| Survey completed | 0.29 | |||
| By phone | 15.4 | 12.8 | 18.2 | |
| Web‐link | 84.6 | 87.2 | 81.8 | |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
| Survey completion time, min | 31.5 (23.0, 52.5) | 30.0 (23.0, 47.0) | 32.0 (34.0, 57.0) | 0.38 |
| By phone | 32.0 (25.0, 44.5) | 35.5 (25.0, 50.0) | 28.5(25.0, 42.0) | 0.44 |
| Web‐link | 31.0 (23.0, 55.6) | 30.0(23.0, 47.0) | 33.0(23.0, 63.0) | 0.25 |
| Days from telemedicine visit to survey completion | 101.5 (59.5, 204.0) | 98.0 (60.0–173.0) | 118.0 (59.0, 228.0) | 0.39 |
Abbreviations: PCP, primary care physician; IQR, interquartile range.
Schonberg index: Scores ≥10 are associated with ≥50% chance of 10 year mortality. 19
For race/ethnicity, 195 participants self‐reported their race/ethnicity and for 13 information was obtained from the demographics sheet in the online medical record.
Regardless of their age, participants reported being satisfied with their telemedicine visit; their median score was 6.0 (25th percentile = 5.0 and 75th percentile = 7.0) on the 7‐point satisfaction scale, Table 2. Similarly, in multivariable linear regression satisfaction scores did not vary by participant age. However, non‐Whites reported satisfaction scores that on average were one point lower than non‐Hispanic Whites (p = 0.02, Table 3) and participants with comorbidity (Charlson ≥1) reported scores that on average were 0.5 points lower than those without comorbidity (p = 0.07). Participants interviewed in 2021 reported satisfaction scores that were on average 0.3 points higher than those interviewed in 2020; however, this difference was not statistically significant (p = 0.16). In total, 39.5% of participants felt telemedicine was worse than an in‐person visit (only 4.9% felt it was better than an in‐person visit) and 22.2% reported that they would be less likely to ask about multiple health problems during a telemedicine visit (4.8% said they would be more likely); 45.9% gave the top collaboRATE score for their telemedicine visit, Table 2. Participants reported being satisfied with the convenience of telemedicine, the ability to connect, the effort made to help them understand their health issues, the quality of the video, the privacy, and the duration of their visit. Adults ≥75 had similar perceptions of telemedicine as adults 65–74 years.
TABLE 2.
Satisfaction with Telemedicine (shared decision making, connectivity, logistics, and overall satisfaction)
| Overall (n = 208) | Age 65–74 (n = 109) | Age ≥75 (n = 99) | ||
|---|---|---|---|---|
| Median (25th, 75th percentile) | Median (25th, 75th percentile) | Median (25th, 75th percentile) | p value | |
| Overall satisfied with the visit (7‐point, Likert scale, 1 [very dissatisfied]‐7 [very satisfied]) | 6 (5,7) | 6 (5,7) | 6 (5,7) | 0.79 |
| Satisfaction with telemedicine index (each scored on a 11‐point Likert scale, 0 [very dissatisfied]–10 [very satisfied]): | ||||
| Satisfied with visit quality (n = 188) | 10 (8,10) | 10 (8,10) | 10 (8,10) | 0.90 |
| Satisfied with treatment plan (n = 176) | 10 (8,10) | 10 (9,10) | 10 (8,10) | 0.30 |
| Satisfied with ability to get connected (n = 190) | 10 (8,10) | 10 (9,10) | 10 (8,10) | 0.96 |
| Satisfaction with the convenience (n = 182) | 10 (8,10) | 10 (8,10) | 10 (8,10) | 0.74 |
| Satisfaction with privacy (171) | 10 (10,10) | 10 (10,10) | 10 10,10) | 0.70 |
| Satisfied with duration of the visit (n = 185) | 10 (8,10) | 10 (8,10) | 10 (8,10) | 0.92 |
| Satisfied with ability to hear (n = 191) | 10 (9,10) | 10 (9,10) | 10 (9,10) | 0.48 |
| Satisfied with comfort using telemedicine (n = 183) | 10 (7,10) | 10 (7,10) | 10 (6,10) | 0.32 |
| Satisfied with how staff answered questions about the process (n = 148, 50 did not ask staff any questions) | 10 (8,10) | 10 (8,10) | 10 (8,10) | 0.60 |
| Satisfaction with the quality of the video (n = 101) | 10 (9,10) | 10 (8,10) | 10 (9,10) | 0.80 |
| Confidence in using each of the following for telemedicine (5‐point scale, not at all confident to very confident | ||||
| Landline for telephone visit (n = 198) | 5 (5,5) | 5 (5,5) | 5 (5,5) | 0.10 |
| Cell‐phone for telephone visit (n = 202) | 5 (5,5) | 5 (5,5) | 5 (5,5) | 0.57 |
| Computer/tablet/cell‐phone for video visit (n = 198) | 5 (4,5) | 5 (4,5) | 5 (3,5) | 0.04 |
| % | % | % | ||
| How did virtual visit compare with a traditional in‐person visit? (n = 203) | ||||
| Better than traditional visit | 4.9 | 4.6 | 5.2 | 0.99 |
| Same | 35.1 | 36.1 | 34.0 | |
| Worse than a traditional visit | 39.5 | 38.9 | 40.2 | |
| Not sure | 20.5 | 20.4 | 20.6 | |
| Likelihood of asking PCP about multiple health problems (n = 207) | 0.93 | |||
| More likely than a traditional visit | 4.8 | 4.6 | 5.1 | |
| Just as likely | 73.0 | 74.1 | 71.7 | |
| Less likely than a traditional visit | 22.2 | 21.3 | 23.2 | |
| Likelihood of asking PCP about medicines (n = 205) | 0.44 | |||
| More likely than a traditional visit | 4.9 | 5.7 | 4.0 | |
| Just as likely | 86.8 | 84.0 | 89.9 | |
| Less likely than a traditional visit | 8.3 | 10.4 | 6.1 | |
| Likelihood of sharing worries/concerns (n = 205) | 0.56 | |||
| More likely than a traditional visit | 4.4 | 5.6 | 3.1 | |
| Just as likely | 83.8 | 84.1 | 83.5 | |
| Less likely than a traditional visit | 11.8 | 10.3 | 13.4 | |
| Top collaboRATE score a | 45.9 | 45.5 | 46.2 | 0.92 |
| Among those who have both a telephone‐only and video visit their preferred visit type: (n = 58) | 0.32 | |||
| Telephone‐only | 10.3 | 6.7 | 14.3 | |
| Video | 63.8 | 60.0 | 67.9 | |
| No preference | 28.9 | 33.3 | 17.9 | |
| Had to convert video to phone visit because of technical difficulties (n = 111) | 27.0 | 29.2 | 25.4 | 0.66 |
CollaboRATE index: 3 items (scored from 0 [no effort] to 9 [maximal effort]): how much effort was made to (1) help your understand your health issues; (2) listen to things that matter most to you about your health issues; and (3) include what matters most to you in choosing how to manage your health issues. 18
TABLE 3.
Correlates of overall satisfaction with telemedicine among adults ≥65 years in multivariable linear regression model (n = 207) a
| Characteristic | Beta estimate (standard error) | p value from regression model |
|---|---|---|
| Sex: Male | ||
| Female | −0.028 (0.241) | 0.91 |
| Race/ethnicity: Non‐Hispanic White | ||
| Black, Hispanic, or other race | −1.023 (0.432) | 0.02 |
| Age: 65–74 years | ||
| 75 years or older | −0.149 (0.231) | 0.52 |
| Education: <college | ||
| College graduate or beyond | 0.106 (0.272) | 0.70 |
| Charlson Comorbidity Index: None | ||
| 1 or more comorbidity | −0.446 (0.245) | 0.07 |
| Date of survey completion: April 2020 to December 2020 | ||
| January 2021 to August 2021 | 0.330 (0.235) | 0.16 |
Overall satisfaction was measured on a 7‐point Likert scale from very dissatisfied (1) to very satisfied (7).
Participants reported being confident using either a landline or cell‐phone for phone visits (median = 5 on 5‐point confidence scale [5, 5] for both). However, they reported significantly less confidence with video visits than with either form of phone visits (median 5 [4, 5], p < 0.001 for both comparisons). Adults ≥75 were significantly less confident about using computers/cell‐phones for video visits than adults 65–74, Table 2. Among 58 patients who had both a phone‐only and a video visit, 63.8% reported that they preferred video visits. Of 111 participants scheduled for a video visit, 27.0% had to convert to audio‐only due to technical difficulties.
Qualitative themes
Participants' open‐ended comments about telemedicine were congruous with their quantitative responses. The main themes identified were that despite being satisfied with telemedicine most participants preferred in‐person care. Yet, most wanted telemedicine to remain available after the pandemic despite experiencing challenges with video technology. A minority felt that telemedicine provided lower quality of care and should not be continued (Table 4). Figure 1 presents a word cloud of participants' generally positive one‐word descriptions of telemedicine, highlighting participants' appreciation of telemedicine's convenience.
TABLE 4.
Participant themes regarding telemedicine primary care a
| PCP themes | Example quotes |
|---|---|
| Prefer in person visits | |
| Physical exam necessary | “I also have several issues that I have put off until I can be seen as a virtual visit will not be of any help‐ are you going to get undressed and show a body part to the screen.” (Patient 51) |
| In‐person interaction helpful | “At my age there's a certain positivity when seeing my PCP, which I did not get from the virtual visit. Comfort factor, I guess. I'm old … it's nice to be seen.” (Patient 29) |
| One‐stop (vitals, blood work, testing can be done) | “My preference is an in‐person visit because there is always blood work. The virtual visit is not a time and/or trip saver. It is an interim solution to in‐person visits during the COVID 19 Pandemic.” (Patient 47) |
| Higher quality |
“Virtual visit cannot possibly offer the same high level of care as a traditional visit. Many details and questions are missed or forgotten because of contending with technical issues concurrently.” (Patient 134) “Face to face visits are necessary so that the provider can examine or observe the patient and maybe detect a problem of which the patient is unaware or had forgotten.” (Patient 25) |
| Annual Wellness Exams should be in person | “The virtual visit was completely satisfactory for an interim visit but not for an annual visit where the physician needs to examine the patient.” (Patient 159) |
| Prefer telemedicine to remain an option | |
| Hybrid model | “I'm happy to do some virtual and then alternate with in person visits.” (Patient 37) |
| Ease of scheduling | “I am able to get an appointment faster than if it was for an in person visit.” (Patient 122) |
| Useful for follow‐up care, minor issues | “Virtual visits are quite satisfactory for routine matters. For non‐routine matters I would prefer a traditional visit.” (Patient 64) |
| Better with good doctor‐patient relationship | “Since I have had this PCP for a while, I am comfortable enough raising issues/asking questions in person or virtually. If she was new, I might feel a little less likely to do so virtually.” (Patient 145) |
| Prefer video to phone‐only | “Video based is the closest thing to being there in person.” (Patient 85) |
| Accessible | “I think it could be very useful if a patient has difficulty getting to the office ‐ bad weather, mobility or illness problems, etc.” (Patient 112) |
| Convenient | “Virtual visit will save a lot of time in terms of travel and waiting in the waiting room.” (Patient 118) |
| Safer during a pandemic | “Maybe in an emergency, where somebody's health would be compromised by going out.” (Patient 93) |
| More focus/less interruption | “Quicker, easier and specific info given and received because there are no other interruptions. Recommend them for most of my problems, I am an old man with an ailing body …” (Patient 189) |
| Easier to involve family | “My daughter attended a couple of appointments to take notes which was very useful.” (Patient 143) |
| Briefer visit | “Feels there is more time pressure for calls; that doctor is more willing to spend extra time when in person.” (Patient 96) |
| Technical challenges with telemedicine | |
| Needs better processes |
“A virtual reception room, to reassure the patient they have made the correct connections, would be reassuring.” (Patient 126) “In the future I should have had my blood drawn a week or two before so that we can discuss the findings.” (Patient 112) “If needed, send the pdf link to the Health Risk Assessment, prior to meeting.” (Patient 84) |
| More training needed | “We believe that more care can be provided in this manner with appropriate planning and education.” (Patient 33) |
| Need better technology |
“Video for one is not good enough—we all know how hard it is to take a picture that looks like life.” (Patient 165) “It's harder to hear the doctor.” (Patient 115) |
| Too technologically challenging | “I'm not a computer person. The tech needed to use this virtual visit is beyond me.” (Patient 133) |
| Too many different platforms | “Unfortunately I found that every practice uses a different program. It was very difficult to clarify what program I was supposed to use with each appointment.” (Patient 174) |
| Plans not to use telemedicine | |
| Not patient‐centered | “There are times when I MUST have to see him face to face and a virtual visit would be totally unacceptable. I would change providers if it came to that.” (Patient 43) |
| Perceives financial benefit to doctors/hospital | “I am very suspicious that the long term motivation to (get away with) virtual/phone doctor “visits” is driven by health care entities bottom line and am very concerned about that!” (Patient 74) |
| Lower quality | “Do away with them. It is a ridiculous way to offer healthcare. An email would result in the same outcome.” (Patient 38) |
Codes were grouped into major themes which are highlighted in bold.
FIGURE 1.
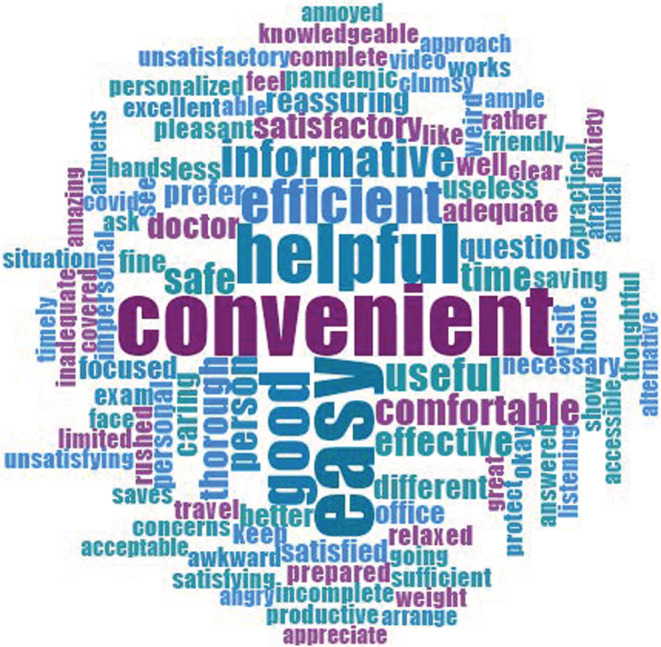
Word‐cloud of participants' one‐word descriptions of telemedicine primary care
Preference for in‐person visits
Many participants felt that in‐person visits were higher quality than telemedicine visits because of the ability of the PCP to observe them, to identify problems patients were unaware of, and to complete a physical examination. Participants worried that without in‐person observation PCPs would miss a diagnosis or not properly address a health issue. “I prefer not to have a virtual visit. I like the touch and feel and talking in person to my doctor. I like my doctor to see me during an examination. It allows for more of an interchange” (Patient 18). Participants also felt that in‐person visits allowed for relationship building, particularly during annual wellness visits, and they appreciated that they could get laboratory testing or imaging done concurrently. “I prefer in person visits. Virtual is not intimate and body language is important. Virtual is too impersonal” (Patient 156). A few noted that they did not choose telemedicine, it was the only visit‐type offered. “It didn't make me feel happy knowing that they didn't want to see me personally. It wasn't the same” (Patient 7).
Prefer telemedicine to remain available
Despite preferences for in‐person care, many participants envisioned utilizing a hybrid of telemedicine and in‐person care in the future. Participants suggested that telemedicine may be useful for follow‐up appointments and straight‐forward issues. “I think both traditional and virtual visits should be offered. I would like an in‐person visit for my physical, but would be happy to do virtual for follow‐ups or for minor health issues that do not require a physical exam” (Patient 191). For telemedicine, most participants preferred video over phone‐only visits because they felt communication was better and more effective with video. “Video gave me more of a sense of human interaction because I could see facial expressions” (Patient 43).
Participants also described favoring telemedicine in bad weather or during pandemics, when they were not feeling well or had restricted mobility, and with doctors whom they knew well and/or had a good relationship. They appreciated the convenience and accessibility of telemedicine, noting that telemedicine eliminated the time, stress, and cost of commuting and parking at appointments or waiting in clinic rooms, and avoided difficulties with stairs or walking distances to reach offices. “I love virtual visits because of the ease and efficiency with which they are accomplished ‐ no driving, parking, waiting” (Patient 125) With telemedicine they felt that the doctor could focus more and there were fewer interruptions. “She seemed more focused on me and less on entering notes in the computer” (Patient 94). Participants perceived that telemedicine could be scheduled more quickly and that telemedicine made it easier to include family. However, a few described feeling rushed during telemedicine visits and did not feel as comfortable bringing up numerous health issues. “Felt like I was being rushed. Didn't feel comfortable to follow up with questions” (Patient 179).
Technical challenges
Many patients described technical challenges with telemedicine, especially using video, and felt that both doctors and patients needed more training. “I like the virtual visit options and if providers have been adequately trained on the technology” (Patient 151) They recommended that the health system choose one telemedicine platform and standardize processes to improve efficiency, such as standardized procedures for obtaining vitals, completing health forms, and for blood draws. Notably, a few participants described lacking the technological skills needed for video visits and some reported not having a computer. “Not everyone over 65 has an iPhone or computer and technological savvy to access a telemedicine visit” (Patient 176).
Plans not to use telemedicine
A few participants commented that they would not use telemedicine after the pandemic. “If you continue them after the pandemic is over, I will switch to care elsewhere” (Patient 89). Some wondered whether doctors were benefiting financially from telemedicine to the detriment of patient care. “I am concerned that there will be a cost‐cutting and income incentive to expand this option that is not for the benefit of the patient” (Patient 74).
DISCUSSION
In a multimethod study of adults ≥65 years who received primary care at one large Boston‐area health system, most older adults regardless of their age reported being satisfied with telemedicine. Despite this, participants tended to prefer in‐person care because of the greater potential for relationship building with their PCP; the opportunity for their PCP to observe them, to complete a physical examination, and to identify new problems that patients were unaware of; and because in‐person visits allowed for laboratory testing and imaging to occur at the time of a visit. Yet, older adults wanted telemedicine to remain an option for follow‐up visits and for minor health issues not requiring physical examination. They appreciated telemedicine for its convenience, ease of access, and because it reduced their exposure to infectious diseases. A minority of participants, especially those with greater comorbidity or of non‐White race were dissatisfied with telemedicine, and did not plan to use telemedicine after the pandemic.
As policy‐makers debate telemedicine's future, our findings highlight some key considerations to support continued coverage of telemedicine for older adults. First, adults ≥65 years, including those ≥75 and those living within or close to a large metropolitan city (i.e., Boston), wanted telemedicine to remain an option for care. Older adults described challenges obtaining transportation to get to in‐person visits and difficulties navigating long hallways to see their PCPs, and valued the time they saved with telemedicine. They also appreciated the ability to easily include family in these visits.
Second, while patients in this and other studies reported that they preferred video to audio‐only visits 26 ; nearly half (47%) of older adults in our study, and similar proportions in other studies, experienced telemedicine only through phone‐only visits. 27 , 28 These findings suggest that lack of coverage for audio‐only visits will reduce access to telemedicine for older adults. However, some policy‐makers contend that audio‐only visits are less effective and may be over‐utilized than in‐person visits because of the ease of access. 29 , 30 Others argue that audio‐only visits allow individuals who would otherwise not receive care a way to do so. 12 , 27 , 31 , 32 , 33 Importantly greater access to care has been associated with improved patient survival and outcomes. 34 While a study found that telemedicine was associated with a slight increase (<1.5% increase) in follow‐up office visits than in‐person care; there were fewer lab tests and prescriptions ordered after telemedicine and there were no differences in hospitalizations or emergency department visits compared to in‐person visits. 35 Another concern is that if coverage for audio‐only visits continues but at a substantially lower rate, few PCPs may be willing or able to continue offering audio‐only visits. This may be a particular issue for older adults because PCPs report that they find telemedicine with adults ≥65 years more challenging. 36
Third, 27% of study participants scheduled for a video visit reported that they had to convert to a phone‐only visit due to technical difficulties. This is greater than the 10% reported in a study of patients of all ages, 31 suggesting that there may be a longer learning curve for using video visits among older adults. This may be particularly true for adults ≥75 who we found to be less confident using video visit technology. To facilitate video visit utilization, study participants recommended that health systems choose one telemedicine platform so that older adults may become familiar with the technology and that patients and clinicians receive formal training. Others have recommended offering in‐home technical assistance and broadening access to low‐cost or free broadband internet, especially for those living in geographically deprived neighborhoods. 28 , 33 , 35 , 37
During our study telemedicine often replaced in‐person care; meaning that many patients did not get to choose how they saw their PCP since physical distancing mandates limited the number of in‐person visits available. This lack of choice may have affected older adults' perceptions of telemedicine. Others have reported that 27% of individuals would like in‐person visits only after the pandemic 38 and overtime telemedicine use has declined to around 20% of visits. 39 , 40 Going forward, older adults should be given a choice of whether they see their PCP in‐person or via telemedicine, especially since older adults with comorbidity and/or those who were non‐White tended to be less satisfied with telemedicine. 41 Others have found that non‐Whites may have heightened concerns about privacy and confidentiality associated with telehealth. 42 In addition, 22% of study participants reported feeling less comfortable bringing up multiple health issues during a telemedicine visit which is concerning for older adults with multimorbidity.
While 45.9% of study participants gave their telemedicine visit the highest CollaboRATE score for shared decision‐making; in prior studies 65%–72% of older adults have given the top CollaboRATE score for shared decision‐making during in‐person visits. 43 , 44 , 45 Experts purport that frameworks for shared decision‐making may need adapting for optimal use during telemedicine. 46 PCPs may also need time to develop best communication practices for these visits. 47
Our study has limitations. Our findings are limited to one geographic area and one health system. Our sample was English‐speaking and predominantly non‐Hispanic White (91.4%) limiting generalizability. Also, our population was highly educated (73.1% had a college degree or higher educational attainment) which may be representative of the population of older adults willing to utilize telemedicine primary care. In addition, we surveyed patients at one point in time and perceptions of telemedicine may be changing quickly; however, we did not find a significant increase in satisfaction with telemedicine between 2021 and 2020. While we asked patients to compare telemedicine to an in‐person visit, we did not assess participants' satisfaction with their most recent in‐person visit. However, older adults tend to rate satisfaction with primary care visits highly. 48 Furthermore, patients were interviewed on average about 3 months after their telemedicine visit which may have affected their recall.
In summary, adults ≥65, regardless of their age, found telemedicine primary care visits satisfactory and saw a continued need for telemedicine. Future studies should examine outcomes of telemedicine visits, especially among older adults with multimorbidity and those who do not speak English. Prospective studies are needed to understand when and why older adults choose telemedicine over in‐person visits and to learn the effect of training older adults on video technology. While study participants reported that they preferred in‐person annual wellness exams (AWVs), all of the components of AWVs could be completed remotely with some innovation; therefore, satisfaction and outcomes of telemedicine AWVs should be studied. Our findings suggest that coverage of both audio‐only and video visits should continue for adults ≥65 years as we continue to learn best uses of this technology in this population.
AUTHOR CONTRIBUTIONS
All authors meet the criteria for authorship stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. Drs. Schonberg and Bhatia conceived of the study and acquiesced, analyzed, and interpreted the data. GA, MK, and LD conceived of the study, analyzed, and interpreted the data. EG conceived of the study, analyzed, and interpreted the data. Drs. Pinheiro and Davis analyzed and interpreted the data for this study. All authors drafted the work or revised it critically for important intellectual content and gave final approval of this manuscript.
FUNDING INFORMATION
This research was supported by Dr. Schonberg's NIA K24 AG071906. The Investigators retained full independence in the conduct of this research.
CONFLICT OF INTEREST
The authors declare that they do not have a conflict of interest. Roma Bhatia: None. Elizabeth Gilliam: None. Gianna Aliberti: None. Adlin Pinheiro: None. Maria Karamourtopoulos: None. Roger B. Davis: None. Laura DesRochers: None. Mara A. Schonberg: None.
SPONSOR'S ROLE
This research was supported by Dr. Schonberg's K24 AG071906. The Investigators retained full independence in the conduct of this research. The sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Supporting information
Table S1. Description of recruitment sites
Figure S1. Recruitment flow diagram
Text S1. Capacity questionnaire
Text S2. Patient telehealth survey
Text S3. Patient telehealth codebook
Bhatia R, Gilliam E, Aliberti G, et al. Older adults' perspectives on primary care telemedicine during the COVID‐19 pandemic. J Am Geriatr Soc. 2022;1‐13. doi: 10.1111/jgs.18035
Prior presentations: This research was presented in part at the 2021 annual meeting (virtual) of the Society of General Internal Medicine.
Funding information National Institute on Aging, Grant/Award Number: K24 AG071906
DATA AVAILABILITY STATEMENT
Data were entered into NVivo 11 (QSR international) qualitative software. The data are not publicly available to maintain participant confidentiality but are available from the corresponding author on reasonable request.
REFERENCES
- 1. Dang S, Ruiz DI, Klepac L, et al. Key characteristics for successful adoption and implementation of home telehealth technology in veterans affairs home‐based primary care: an exploratory study. Telemed J E Health. 2019;25(4):309‐318. [DOI] [PubMed] [Google Scholar]
- 2. Nesbitt TS, Marcin JP, Daschbach MM, Cole SL. Perceptions of local health care quality in 7 rural communities with telemedicine. J Rural Health. 2005;21(1):79‐85. [DOI] [PubMed] [Google Scholar]
- 3. van den Berg N, Schumann M, Kraft K, Hoffmann W. Telemedicine and telecare for older patients—a systematic review. Maturitas. 2012;73(2):94‐114. [DOI] [PubMed] [Google Scholar]
- 4. Levine DM, Dixon RF, Linder JA. Association of structured virtual visits for hypertension follow‐up in primary care with blood pressure control and use of clinical services. J Gen Intern Med. 2018;33(11):1862‐1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;2016(9):CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Batsis JA, DiMilia PR, Seo LM, et al. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019;67(8):1737‐1749. doi: 10.1111/jgs.15959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow‐up care. Am J Manag Care. 2019;25(1):40‐44. [PubMed] [Google Scholar]
- 8. Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients' satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31(3):269‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15(3):225‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stahl JE, Dixon RF. Acceptability and willingness to pay for primary care videoconferencing: a randomized controlled trial. J Telemed Telecare. 2010;16(3):147‐151. [DOI] [PubMed] [Google Scholar]
- 11. Foster MV, Sethares KA. Facilitators and barriers to the adoption of telehealth in older adults: an integrative review. Comput Inform Nurs. 2014;32(11):523‐533; quiz 534–525. [DOI] [PubMed] [Google Scholar]
- 12. Frydman JL, Gelfman LP, Goldstein NE, Kelley AS, Ankuda CK. The digital divide: do older adults with serious illness access telemedicine? J Gen Intern Med. 2022;37(4):984‐986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Assistant Secretary for Planning and Evaluation (ASPE) . Issue Brief. Medicare Beneficiary Use of Telehealth Visits: Early Data From the Start of the COVID‐19 Pandemic ; July 27, 2020. Accessed June 6, 2022. https://aspe.hhs.gov/reports/medicare-beneficiary-use-telehealth-visits-early-data-start-covid-19-pandemic
- 14. Young LB, Foster L, Silander A, Wakefield BJ. Home telehealth: patient satisfaction, program functions, and challenges for the care coordinator. J Gerontol Nurs. 2011;37(11):38‐46. [DOI] [PubMed] [Google Scholar]
- 15. Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;180(10):1386‐1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation‐memory‐concentration test of cognitive impairment. Am J Psychiatry. 1983;140(6):734‐739. [DOI] [PubMed] [Google Scholar]
- 17. Morgan DG, Kosteniuk J, Stewart N, O'Connell ME, Karunanayake C, Beever R. The telehealth satisfaction scale: reliability, validity, and satisfaction with telehealth in a rural memory clinic population. Telemed J E Health. 2014;20(11):997‐1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Barr PJ, Thompson R, Walsh T, Grande SW, Ozanne EM, Elwyn G. The psychometric properties of CollaboRATE: a fast and frugal patient‐reported measure of the shared decision‐making process. J Med Internet Res. 2014;16(1):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schonberg MA, Li V, Marcantonio ER, Davis RB, McCarthy EP. Predicting mortality up to 14 years among community‐dwelling adults aged 65 and older. J Am Geriatr Soc. 2017;65(6):1310‐1315. doi: 10.1111/jgs.14805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373‐383. [DOI] [PubMed] [Google Scholar]
- 21. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914‐919. [DOI] [PubMed] [Google Scholar]
- 22. Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self‐reported health literacy questions among diverse English and Spanish‐speaking populations. J Gen Intern Med. 2011;26(3):265‐271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hsiao V, Chandereng T, Lankton RL, et al. Disparities in telemedicine access: a cross‐sectional study of a newly established infrastructure during the COVID‐19 pandemic. Appl Clin Inform. 2021;12(3):445‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jaffe DH, Lee L, Huynh S, Haskell TP. Health inequalities in the use of telehealth in the United States in the lens of COVID‐19. Popul Health Manag. 2020;23(5):368‐377. [DOI] [PubMed] [Google Scholar]
- 25. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77‐101. [Google Scholar]
- 26. Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID‐19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9):e20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chen J, Li KY, Andino J, et al. Predictors of audio‐only versus video telehealth visits during the COVID‐19 pandemic. J Gen Intern Med. 2022;37(5):1138‐1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Karimi M, Lee EC, Couture SJ, et al. National Survey Trends in Telehealth Use in 2021: Disparities in Audio vs. Video Services ; February 1, 2022; Accessed June 6, 2022. https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
- 29. Mehrotra A, Bhatia RS, Snoswell CL. Paying for telemedicine after the pandemic. JAMA. 2021;325(5):431‐432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lion KC, Brown JC, Ebel BE, et al. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr. 2015;169(12):1117‐1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Crotty BH, Hyun N, Polovneff A, et al. Analysis of clinician and patient factors and completion of telemedicine appointments using video. JAMA Netw Open. 2021;4(11):e2132917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Khoong EC. Policy considerations to ensure telemedicine equity. Health Aff (Millwood). 2022;41(5):643‐646. [DOI] [PubMed] [Google Scholar]
- 33. Bose S, Dun C, Zhang GQ, Walsh C, Makary MA, Hicks CW. Medicare beneficiaries in disadvantaged neighborhoods increased telemedicine use during the COVID‐19 pandemic. Health Aff (Millwood). 2022;41(5):635‐642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025‐1034. [DOI] [PubMed] [Google Scholar]
- 35. Reed M, Huang J, Graetz I, Muelly E, Millman A, Lee C. Treatment and follow‐up care associated with patient‐scheduled primary care telemedicine and in‐person visits in a large integrated health system. JAMA Netw Open. 2021;4(11):e2132793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bhatia R, Aliberti G, Gilliam E, et al. A survey of Massachusetts primary care physicians' experience with telemedicine in older adults. J Am Geriatr Soc. 2021;70(3):683‐687. doi: 10.1111/jgs.17645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID‐19 pandemic in the United States. Health Aff (Millwood). 2021;40(2):349‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vosburg RW, Robinson KA. Telemedicine in primary care during the COVID‐19 pandemic: provider and patient satisfaction examined. Telemed J E Health. 2022;28(2):167‐175. [DOI] [PubMed] [Google Scholar]
- 39. Corez C, Mansour O, Qato DM, Stafford RS, Alexander GC. Changes in short‐term, long‐term, and preventive care delivery in US office‐based and telemedicine visits during the COVID‐19 pandemic. JAMA Health Forum. 2021;2(7):e211529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hays RD, Skootsky SA. Patient experience with in‐person and telehealth visits before and during the COVID‐19 pandemic at a large integrated health system in the United States. J Gen Intern Med. 2022;37(4):847‐852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ladin K, Porteny T, Perugini JM, et al. Perceptions of telehealth vs in‐person visits among older adults with advanced kidney disease, care partners, and clinicians. JAMA Netw Open. 2021;4(12):e2137193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Meno M, Abe J, Fukui J, Braun‐Inglis C, Pagano I, Acoba J. Telehealth amid the COVID‐19 pandemic: perception among Asian, native Hawaiian and Pacific islander cancer patients. Future Oncol. 2021;17(23):3077‐3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Forcino RC, Thygeson M, O'Malley AJ, Meinders MJ, Westert GP, Elwyn G. Do collaboRATE scores reflect differences in perceived shared decision‐making across diverse patient populations? Evidence from a large‐scale patient experience survey in the United States. J Patient Exp. 2020;7(5):778‐787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Barr PJ, Forcino RC, Thompson R, et al. Evaluating CollaboRATE in a clinical setting: analysis of mode effects on scores, response rates and costs of data collection. BMJ Open. 2017;7(3):e014681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tai‐Seale M, Elwyn G, Wilson CJ, et al. Enhancing shared decision making through carefully designed interventions that target patient and provider behavior. Health Aff (Millwood). 2016;35(4):605‐612. [DOI] [PubMed] [Google Scholar]
- 46. Hartasanchez SA, Heen AF, Kunneman M, et al. Remote shared decision making through telemedicine: a systematic review of the literature. Patient Educ Couns. 2022;105(2):356‐365. [DOI] [PubMed] [Google Scholar]
- 47. Aliberti GM, Bhatia R, Desrochers LB, Gilliam EA, Schonberg MA. Perspectives of primary care clinicians in Massachusetts on use of telemedicine with adults aged 65 and older during the COVID‐19 pandemic. Prev Med Rep. 2022;26:101729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. de Waard CS, Poot AJ, den Elzen WPJ, Wind AW, Caljouw MAA, Gussekloo J. Perceived doctor‐patient relationship and satisfaction with general practitioner care in older persons in residential homes. Scand J Prim Health Care. 2018;36(2):189‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Description of recruitment sites
Figure S1. Recruitment flow diagram
Text S1. Capacity questionnaire
Text S2. Patient telehealth survey
Text S3. Patient telehealth codebook
Data Availability Statement
Data were entered into NVivo 11 (QSR international) qualitative software. The data are not publicly available to maintain participant confidentiality but are available from the corresponding author on reasonable request.


