Abstract
Trauma‐exposed veterans receiving mental health care may have an elevated risk of experiencing COVID‐19–related difficulties. Using data from several ongoing clinical trials (N = 458), this study examined exposure to COVID‐19–related stressors and their associations with key sociodemographic factors and mental health outcomes. The results showed that exposure to COVID‐19–related stressors was common, higher among veterans who were racial/ethnic minorities d = 0.32, and associated with elevated posttraumatic stress disorder (PTSD), r = .288, and depressive symptom severity, r = .246. Women veterans experienced more difficulty accessing social support, d = 0.31, and higher levels of COVID‐19–related distress, d = 0.31, than men. Qualitative data were consistent with survey findings and highlighted the broader societal context in veterans’ experience of COVID‐19–related distress. These findings may inform future research on the impact of the pandemic on veterans, particularly those who are women and members of minoritized racial/ethnic groups, as well as mental health treatment planning for this population.
The COVID‐19 pandemic has had a profound negative impact on mental health within the general population (Robinson et al., 2022), including among veterans (Murphy et al., 2022; Richardson et al., 2022). Widespread exposure to stressors related to COVID‐19, such as experiencing COVID‐19 illness (e.g., Lei et al., 2020), social disruptions (e.g., Venkatesh et al., 2020), and economic hardships (e.g., Nicola et al., 2020) have been documented along with increased rates of mental health problems, including symptoms of posttraumatic stress and depression. Sociodemographic factors associated with the negative mental health impact of COVID‐19 include female gender, younger age (e.g., Xiong et al. 2020), and being part of a minoritized ethnic/racial group (e.g., Wirkner et al., 2022).
Veterans may have an elevated risk for COVID‐19–related mental health problems given their high rate of preexisting trauma exposure (e.g., Fein‐Schaffer et al., 2021; Murphy et al., 2022; Na et al., 2021), which may sensitize these individuals to the negative impact of future stressors (e.g., Nichter et al., 2020). COVID‐19–related stressors may also exacerbate existing mental health disorders, which veterans experience at a higher rate compared with the general public (e.g., Trivedi et al., 2015; Wild et al., 2016). One study found that veterans who endorsed more COVID‐19–related stressors reported that the pandemic had a more negative impact on their PTSD symptoms (Hendrikx et al., 2022). Identifying the strength and nature of the association between COVID‐19–related stressors and mental health symptoms, such as those related to PTSD and depression, could have implications for treatment planning, including determining the focus and duration of therapy.
The goal of this study was to understand the impact of COVID‐19–related stressors among trauma‐exposed treatment‐seeking veterans. We examined the (a) prevalence of COVID‐19–related stressors, (b) associations between COVID‐19–related stressors and select sociodemographic variables, and (c) the associations between COVID‐19–related stressors and symptoms of PTSD and depression. In line with prior work, we hypothesized that female gender, younger age, and having a minoritized racial and/or ethnic identity would be associated with more COVID‐19–related stressors and that COVID‐19–related stressors would be associated with higher levels of PTSD and depressive symptom severity.
METHOD
Participants
Participants were 458 trauma‐exposed, treatment‐seeking veterans enrolled in 1 of 6 treatment trials. Data for this study were collected from April 2020 to September 2021. Specific inclusion criteria for the parent trials varied. All participants had clinically significant symptoms of PTSD (n = 362) or had been diagnosed with PTSD (n = 84); among those with diagnosed PTSD, 69 individuals had also been diagnosed with alcohol use disorder. In addition, 12 participants were recruited based on reporting trauma‐related guilt. All participants had experienced a Criterion A traumatic event and were enrolled in a clinical trial focused on evaluating a psychotherapy for trauma‐related mental health problems. Trauma exposure included military sexual trauma (MST; n = 278), any (i.e., mixed) trauma exposure (n = 168), or deployment‐related trauma exposure (n = 12). Exclusion criteria varied across trials, but active psychosis and suicidal ideation warranting crisis intervention were exclusion criteria for all trials. Sample demographic characteristics can be found in Table 1.
TABLE 1.
Participant demographic characteristics
| Variable | M | SD | n | % |
|---|---|---|---|---|
| Age (years) | 44.6 | 12.1 | ||
| Gender | ||||
| Cisgender men | 222 | 48.5 | ||
| Cisgender women | 228 | 49.8 | ||
| Transgender women | 1 | 0.2 | ||
| Transgender men | 1 | 0.2 | ||
| Gender nonconforming | 1 | 0.2 | ||
| Other | 2 | 0.4 | ||
| Race/ethnicity | ||||
| White | 276 | 60.3 | ||
| Black or African American | 60 | 13.1 | ||
| Asian, Native Hawaiian, or Pacific Islander | 20 | 3.3 | ||
| American Indian or Alaska Native | 8 | 1.7 | ||
| Hispanic, Latino(a), or Mexican‐American | 52 | 11.4 | ||
| Other | 8 | 1.7 | ||
| Multiple racial identities | 29 | 6.3 | ||
| Middle Eastern or North African | 3 | 0.7 | ||
| Employment status | ||||
| Full‐time | 173 | 37.8 | ||
| Part‐time | 39 | 8.7 | ||
| Not currently working for pay | 177 | 38.6 | ||
| Retired | 65 | 14.2 | ||
| Educational attainment | ||||
| 4‐year college degree | 116 | 26.3 | ||
| H igh school degree or GED | 41 | 9.0 | ||
| Postgraduate | 71 | 15.0 | ||
| Some college or 2‐year degree | 228 | 49.8 | ||
| Some high school | 1 | 0.2 | ||
| Relationship status | ||||
| Married | 220 | 48.0 | ||
| Separated/divorced | 116 | 25.3 | ||
| Single | 111 | 24.2 | ||
| Widowed | 8 | 1.7 | ||
| Childrena | ||||
| 0 | 104 | 22.7 | ||
| 2–3 | 157 | 34.3 | ||
| ≥ 4 | 41 | 9.0 | ||
| Number of deploymentsb | 1.7 | 1.41 | ||
| Military branchc | ||||
| Army | 107 | 37.4 | ||
| Air Force | 33 | 11.5 | ||
| Navy | 89 | 31.0 | ||
| Marines | 49 | 16.9 | ||
| Coast Guard/National Guard | 8 | 3.0 |
Note: N = 458. Due to missing data, percentages may not add to 100.0.
Four of the six studies (n = 377) assessed number of children.
Three of the six studies (n = 96) assessed number of deployments.
Five of the six studies (n = 287) assessed military branch.
The treatment trials included those examining (a) MST‐related web‐based therapy (n = 171), (b) home‐based psychotherapy for women with MST in rural areas (n = 107; https://clinicaltrials.gov/ct2/show/NCT03429166), (c) written versus verbal brief exposure therapy (n = 84; https://clinicaltrials.gov/ct2/show/NCT04000217, (d) topiramate and prolonged exposure (n = 69; https://clinicaltrials.gov/ct2/show/NCT03176953, (e) an integrative technology approach to home‐based conjoint therapy for PTSD (n = 15; https://clinicaltrials.gov/ct2/show/NCT02720016), and (f) trauma‐informed guilt reduction therapy (n = 12; https://clinicaltrials.gov/ct2/show/NCT02512445).
Procedure
Participants completed the Coronavirus Stressor Survey (McLean & Cloitre, 2020) during a regularly scheduled assessment, which varied across studies. PTSD and depressive symptoms were assessed at the same time point. This study was designated as exempt from the Stanford University institutional review board.
Measures
Sociodemographic characteristics
Sociodemographic data, including age, race, and other relevant information, were collected in each trial.
COVID‐19 stressors
The Coronavirus Stressor Survey (McLean & Cloitre, 2020) is a 10‐item self‐report measure of COVID‐19–related stressors and the respondent's perceived impact of the pandemic. Six items aimed at assessing COVID‐19–related stressors, with response options of “happened to me,” “happened to someone close to me,” and “doesn't apply.” Additional items, rated on a 5‐point scale, assessed past‐week difficulty getting social support (rated from 0 = no difficulty at all to 4 = extreme difficulty), COVID‐19 media exposure (rated from 0 = none at all to 4 = more than two hours), and overall distress related to the pandemic (rated from 0 = no distress to 4 = extreme distress). One open‐ended item invited respondents to share additional concerns related to the impact of the pandemic. The measure was developed iteratively in consultation with National Center for PTSD experts in trauma, PTSD, and scale development.
PTSD symptoms
To assess symptoms of PTSD per the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; American Psychiatric Association, 2013), respondents completed the 20‐item PTSD Checklist for DSM‐5 (PCL‐5; Weathers et al., 2013). The PCL‐5 has demonstrated excellent reliability (e.g., Bovin et al., 2016). Items are rated on a Likert scale ranging from 0 to 4, with total scores ranging from 0 to 80 and higher scores indicating higher levels of symptom severity. Because we did not have access to item‐level data for all of the included trials, we were unable to calculate internal reliability for this measure.
Depressive symptoms
Four trials used the nine‐item Patient Health Questionnaire (PHQ‐9; Kroenke et al., 2001), a self‐report scale used to assess affective and somatic symptoms of depression over the past 2 weeks that has demonstrated excellent reliability (Kroenke et al., 2001). Items are rated on a 4‐point Likert scale ranging from 0 to 3, with higher scores indicating more severe depressive symptoms.
Two trials used the Beck Depression Inventory–II (BDI‐II; Beck et al., 1996), a 21‐item self‐report measure of the affective and somatic symptoms related to depression that has also demonstrated excellent reliability (Beck et al., 1996). Items are scored on a 4‐point Likert ranging scale from 0 to 3, with higher scores indicating higher levels of depressive symptom severity. Because we did not have access to item‐level data for all of the included trials, we were unable to calculate internal reliability for the PHQ‐9 or the BDI‐II.
Data analysis
Descriptive analyses were used to characterize the sample and represent frequencies from the survey. One‐way analyses of variance (ANOVAs), t tests, and correlations were used to examine associations between sociodemographic variables (i.e., gender, racial and ethnic identity, and number of children), COVID‐19–related stressors, and mental health symptoms. Effect sizes were calculated as Cohen's d, with values of 0.2, 0.5, and 0.8 interpreted as small, medium, and large, respectively (Cohen, 1988). Gender was coded as cisgender women, cisgender men, or gender minority. Racial and ethnic identity was dummy‐coded as White or racial and ethnic minority. Exploratory analyses examined PTSD and depressive symptoms across each COVID‐19 stressor that was directly or indirectly experienced. Cases with missing data (n = 5, 1.1%) or those for which Coronavirus Stressor Survey items were not implemented (i.e., items on social support, distress, and media exposure: n = 12, 2.6%; open‐ended item: n = 84, 18.3%) were excluded from the analyses. Two authors (Carmen P. McLean, Vaughn Hooper) reviewed qualitative data to inductively identify themes; repeated themes were coded and grouped together, and the number of participants who reported each theme was noted.
RESULTS
COVID‐19–related stressor exposure
On average, participants reported experiencing 2.6 (SD = 2.16) COVID‐19 stressors (Mdn = 2). The percentage of participants who reported each COVID‐19–related stressor is reported in Table 2.
TABLE 2.
COVID‐19–related stressor exposure
| Experience | Happened to me (%) | Happened to someone close to me (%) |
|---|---|---|
| Become ill from possible or certain exposure to the coronavirus | 13.8 | 28.6 |
| Hospitalized from exposure to the coronavirus | 3.1 | 19.9 |
| Job requires possible exposure to coronavirus | 31.4 | 21.3 |
| Lost job or lost income due to the coronavirus pandemic | 21.8 | 15.7 |
| Increased responsibilities at home due to the coronavirus pandemic | 40.6 | 15.5 |
| Difficulty getting food, medication, important medical procedures, or other necessities due to the coronavirus pandemic | 32.5 | 15.3 |
Note: N = 458.
Figure 1 depicts the additional survey results. The mean response for COVID‐19–related media exposure corresponded with the response option “about an hour,” and 46.5% of participants reported experiencing more than 1 hour of exposure per day (Figure 1a). In addition, 28.0% of participants reported at least some difficulty getting the social support they needed due to the COVID‐19 pandemic (Figure 1b), and 41.3% of participants reported at least some distress related to the pandemic (Figure 1c). Qualitative themes identified in the open‐response item are reported in Table 3. In total, 186 participants (40.6%) elected to share additional concerns.
FIGURE 1.
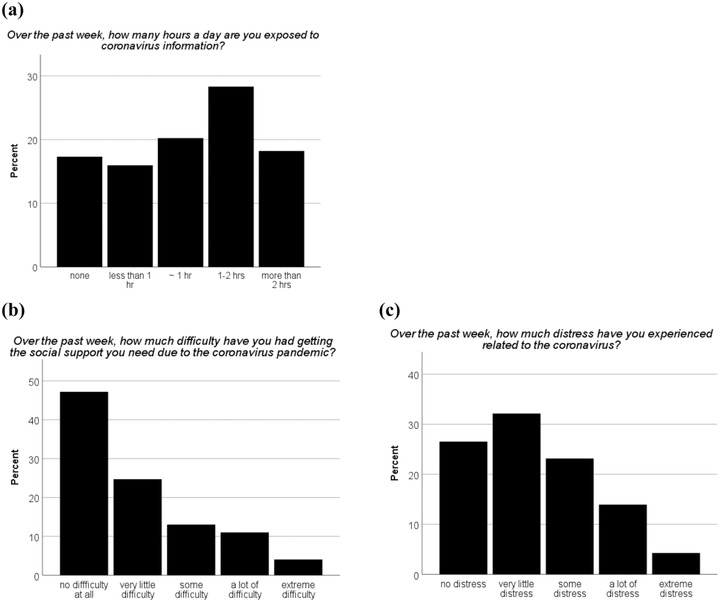
Descriptive data for Coronavirus Stress Survey items.
TABLE 3.
Qualitative themes and illustrative quotes for additional concerns about the impact of COVID‐19
| Qualitative theme | Theme description | Illustrative quotes |
|---|---|---|
| Health and safety concerns (n = 91) | Concerns about contracting COVID‐19 and the potential impact of the virus on the health of oneself and loved ones. |
“Afraid that the people I care about my get it because they are all high risk.” “Fearful of getting the virus and not recovering.” “I am worried that my husband and daughter will become sick, or if I become sick and cannot help them.” |
| Negative impact on life (n = 61) | Pandemic‐related loss of life and the negative impact of the pandemic on veterans’ work, mental health, and general functioning. |
“Loss of an aunt was devastating.” “Scared my son will miss key social experiences.” “Lay‐offs of coworkers who won't get their jobs back.” “My PTSD is highly triggered when I feel that I am in a medical or hostile environment against my will.” |
|
Added stress (n = 42) |
The pandemic has caused increased stress and worry directly and indirectly via the impact of movement restrictions and other COVID‐19 safety mandates on finances and childcare. |
“I am worried about loss of income for total household because of coronavirus.” “Having a child at home for months due to pandemic, my wife and I both were and continue to be under stress from this.” “I enjoy being at home but we are getting tired. My family fighting about it. People are upset because of financial issues.” |
|
Limited access to needs (n = 39) |
Difficulty accessing needed social connection, health care, and other necessities. |
“Accessibility to aging, impaired parents who live across country. How to create a new relationship with someone I'm just starting to date.” “Transgender transition process delayed due to COVID.” “Not being able to get an ID, haircut, go to the bank.” |
| Uncertainty about the future (n = 26) | Uncertainty about when the pandemic will end and what the scope of the impact will be. |
“When will it end? When will it get back to normal?” “It's mostly challenging trying to plan or be prepared when you have little to no control of what the future holds.” “Just job stability in the future and when can I leave my home.” |
|
Dissatisfaction with pandemic management (n = 20) |
Frustration and worry about how the pandemic has been managed by the government and media, as well as how individuals have responded to pandemic‐related mandates. |
“No one is actually reporting the facts. They are reporting what the different parties are doing and not doing.” “They are opening too soon and can lead to another large outbreak and I, who has been practicing social distancing, am at high risk to get it until they have a vaccine.” “Disparate impact on people of color and how this is not being addressed properly.” |
|
Interpersonal discord (n = 20) |
Feelings of anger, frustration, and disconnection from others, including loved ones, due to divergent responses to COVID‐19 and the safety‐related mandates as well as xenophobia and racial tension. |
“Angry at non–mask‐wearers.” “Differences in feelings about the vaccine.” “Frustration with disbelieving family.” “Xenophobia.” |
Note: n = 186. The number of participants who endorsed various themes is greater than the total number of participants who provided data because responses were multiply coded across themes. PTSD = posttraumatic stress disorder; ID = identification.
Associations with sociodemographic variables
Gender was unrelated to the number of reported COVID‐19 stressors, F(2, 452) = 1.892, p = .152, but was related to difficulty accessing social support, F(2, 439) = 5.095, p = .006. The results of follow‐up t tests showed more difficulty accessing social support among women (M = 1.16, SD = 1.28), than men (M = 0.82, SD = 1.05), t(435) = 3.10, p < .001, d = 0.31. Gender‐minority participants (n = 5) reported the greatest difficulty accessing social support (M = 1.4, SD = 1.31), but relative to men, the difference was not significant, d = 0.51. Gender was also related to overall COVID‐19–related distress, F(2, 439) = 6.21, p = .002, with higher levels of distress among women (M = 1.54, SD = 1.12), than men (M = 1.17 (SD = 1.14), t(435) = 3.42, p < .001, d = 0.31. Distress related to COVID‐19 was highest among gender minority participants (M = 1.8, SD = 1.1), but relative to men, this difference was not significant, d = 0.56. There were no gender differences with regard to COVID‐19–related media exposure.
Racial and ethnic minority participants reported more COVID‐19–related stressors (M = 3.02, SD = 2.21), than White participants (M = 2.34, SD = 2.08), t(454) = −3.317, p = .001, d = 0.32, and higher levels of COVID‐19–related media exposure (M = 2.32, SD = 1.39), than their White counterparts (M = 2.03, SD = 1.33), t(441) = −2.233, p = .026, d = 0.21. There were no differences between racial/ethnic groups with regard to accessing social support or COVID‐19–related distress. Participant age was unrelated to total stressors, media exposure, difficulty accessing social support, or COVID‐19–related distress, ps = .766–.963.
Associations between COVID‐19–related stressors and PTSD and depressive symptoms
The total number of COVID‐19–related stressors was related to PTSD, rs = .125, p = .008, and depressive symptoms, rs = .114, p = .015. Difficulty accessing social support was also associated with PTSD, rs = .288, p < .001, and depressive symptoms, rs = .246, p < .001. Participants reporting greater distress related to COVID‐19 reported higher PTSD, rs = .157, p = .001, and depressive symptoms, rs = .094, p = .049. COVID‐19 media exposure was unrelated to PTSD or depressive symptoms (ps ≥ .09).
PTSD symptoms were greater among those affected by COVID‐19 illness, m = 52.27 (SD = 16.12), versus m = 47.50 (SD = 17.95), t(453) = −2.84, p = .005, d = 0.28, COVID‐19 hospitalization, m = 55.14 (SD = 14.11), versus m = 47.53 (SD = 17.95), t(453) = −3.96, p < .001, d = 0.47, and difficulty accessing basic needs, m = 51.72 (SD = 16.09), versus m = 47.42 (SD = 18.18), t(453) = −2.62, p = .009, d = 0.25. Depressive symptoms were greater among those affected by COVID‐19 hospitalization, m = .20 (SD = .97), versus m = −.05 (SD = 1.01), t(453) = −2.26, p = .024, d = 0.25, and difficulty accessing basic needs, m = .15 (SD = .96), versus m = −.09 (SD = 1.02), t(454) = −2.64, p = .009, d = 0.24. There were no differences in PTSD or depressive symptoms across endorsement of other COVID‐19 stressors (ps ≥ .08).
DISCUSSION
Exposure to COVID‐19–related stressors was higher among veterans who are members of marginalized racial or ethnic groups than among those who identified as White, consistent with prior veteran (e.g., Fein‐Schaffer et al., 2021) and civilian research (e.g., Stockman et al., 2021). This small effect highlights the disproportionate impact of the pandemic on people from marginalized racial and ethnic groups.
Women veterans did not report more COVID‐19 stressors than men, which differs from findings among civilians (e.g., Ranji et al., 2021), but there was a small effect for women to report more difficulty accessing social support and higher levels of COVID‐19–related distress than men. Given civilian research showing higher levels of social support in women than men (e.g., Grey et al., 2020), it may be that social support access is more difficult for trauma‐exposed women veterans in particular and/or that women were able to successfully maintain social support but experienced more difficulty accessing this support than men. It may also be related to MST exposure, which was overrepresented in the combined sample and has been linked to lower perceived social support among veteran women (Suris & Lind, 2008). The finding of higher levels of pandemic‐related distress among women is consistent with longitudinal research (Breslau et al., 2021) and may suggest more reactivity to COVID‐19 stressors or could be related to exposure to other stressors not assessed by our survey.
COVID‐19–related stressors, particularly exposure to illness, hospitalization, and difficulty accessing basic needs, and difficulty accessing social support were related to PTSD and depressive symptom severity. This is consistent with findings from cross‐sectional (Murphy et al., 2022) and longitudinal research in veteran samples (Hendrikx et al., 2021; Hill et al., 2021). Taken together with prior findings, this suggests a more substantial mental health impact of COVID‐19 among trauma‐exposed veterans who are women and/or members of minoritized racial and ethnic groups, which, in turn, may exacerbate existing mental health disparities in these communities. Distress related to the pandemic was also related to PTSD and depressive symptoms, suggesting that existing mental health symptoms may make veterans vulnerable to experiencing pandemic‐related distress or that pandemic distress exacerbates existing mental health symptoms. A portion of the sample also had an alcohol use disorder; some participants may have used alcohol to cope with pandemic stress, which also may have contributed to mental health problems. Due to the cross‐sectional design, the present findings cannot speak to whether existing mental health problems sensitize veterans to the negative impact of COVID‐19–related stressors or whether COVID‐19 stressors exacerbate existing mental health problems. However, the findings are consistent with data demonstrating less resilience in the face of COVID‐19–related stressors among veterans with mental health conditions (Kachadourian et al., 2021) and lower levels of social support (Hendrikx et al., 2021).
Qualitative data demonstrated that veterans experienced concerns about the impact of COVID‐19 on their physical health, safety, work, mental health, and general functioning as well as uncertainty about the future. Consistent with the quantitative findings, veterans reported distress related to the pandemic and challenges accessing necessities, including social connection. Not captured in our quantitative data, veterans described distress related to how the pandemic has been handled and how people have responded to the pandemic and associated safety mandates. This highlights the importance of considering broader familial and societal contexts when understanding veterans’ experience of pandemic stressors.
The cross‐sectional study design prohibits conclusions about the directionality of effects. Most women participants had experienced MST; therefore, findings related to gender may be confounded with trauma type. Moreover, the findings may not generalize to non–treatment‐seeking veterans or other populations, including civilians. In addition, the Coronavirus Stressor Survey is an unvalidated instrument. These limitations notwithstanding, the findings contribute to the field's understanding of the impact of the COVID‐19 pandemic on PTSD and depressive symptoms among treatment‐seeking, trauma‐exposed veterans. The finding that women and members of minoritized racial and ethnic groups are disproportionately affected by COVID‐19–related stressors highlights the need to understand potential pathways leading to disproportionate risk (e.g., economic oppression, structural racism, access to social support) and disseminate clinical interventions to mitigate this disproportionate impact. Interventions that aim to bolster social support (e.g., peer support groups) or, when feasible, mitigate the effect of COVID‐19–related stressors by providing resources (e.g., Department of Veterans Affairs [VA] mobile apps, such as Mindfulness Coach and PTSD Coach) or problem‐solving skills training (e.g., VA Moving Forward online training) could be considered.
OPEN PRACTICES STATEMENT
Requests for deidentified data and research materials should be made to the lead author at carmen.mclean4@va.gov.
AUTHOR NOTE
The authors receive royalties from Elsevier Press (Sonya B. Norman) and the American Psychological Association Press (Carmen P. McLean) and income from UptoDate and System Analytic (Sonya B. Norman). This work was supported by funding from the U.S. Department of Defense (W81XWH‐15‐1‐0330; PI: Sonya B. Norman), the U.S. Department of Veterans Affairs (I01RX002412‐01A1 to Sonya B. Norman; IIR 16–070 to Marylene Cloitre; I01RX002093‐01 to Leslie Morland). The grant sponsors played no role in the study design; the collection, analysis, and interpretation of the data; the writing of this manuscript; or the decision to submit this manuscript for publication. The views expressed herein are solely those of the authors and do not reflect an endorsement by or the official policy or position of the Department of Defense, Department of Veterans Affairs, or the U.S. Government. This material is the result of work supported, in part, by resources provided by and the use of facilities at the VA Palo Alto Health Care System.
McLean, C. P. , Wachsman, T. , Morland, L. , Norman, S. B. , Hooper, V. , & Cloitre, M. (2022). The mental health impact of COVID‐19–related stressors among treatment‐seeking trauma‐exposed veterans. Journal of Traumatic Stress, 00, 1–9. 10.1002/jts.22874
REFERENCES
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author. 10.1176/appi.books.9780890425596 [DOI]
- Beck, A. T. , Steer, R. A. , & Brown, G. K. (1996). Beck Depression Inventory: Second edition manual. The Psychological Corporation. [Google Scholar]
- Bovin, M. J. , Marx, B. P. , Weathers, F. W. , Gallagher, M. W. , Rodriguez, P. , Schnurr, P. P. , & Keane, T. M. (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders‐Fifth Edition (PCL‐5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Breslau, J. , Finucane, M. L. , Locker, A. R. , Baird, M. D. , Roth, E. A. , & Collins, R. L. (2021). A longitudinal study of psychological distress in the United States before and during the COVID‐19 pandemic. Preventive Medicine, 143, 106362. 10.1016/j.ypmed.2020.106362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Fein‐Schaffer, D. , Hawn, S. E. , Annunziata, A. J. , Ryabchenko, K. , Miller, M. W. , & Wolf, E. J. (2021). Premorbid traumatic stress and veteran responses to the COVID‐19 pandemic. Journal of Traumatic Stress, 35(2), 559–569. 10.1002/jts.22770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey, I. , Arora, T. , Thomas, J. , Saneh, A. , Tohme, P. , & Abi‐Habib, R. (2020). The role of perceived social support on depression and sleep during the COVID‐19 pandemic. Psychiatry Research, 293, 113452. 10.1016/j.psychres.2020.113452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrikx, L. J. , Williamson, C. , Baumann, J. , & Murphy, D. (2022). The impact of the COVID‐19 pandemic on treatment‐seeking veterans in the United Kingdom with preexisting mental health difficulties: A longitudinal study. Journal of Traumatic Stress, 35, 330–337. 10.1002/jts.22742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, M. , Nichter, B. , Na, P. , Norman, S. , Morland, L. , Krystal, J. , & Pietrzak, R. (2021). Mental health impact of the COVID‐19 pandemic in U.S. military veterans: A population‐based, prospective cohort study. Psychological Medicine . Advance online publication. 10.1017/S0033291721002361 [DOI] [PMC free article] [PubMed]
- Kachadourian, L. , Tsai, J. , Na, P. J. , Krystal, J. H. , Southwick, S. M. , & Pietrzak, R. H. (2021). Resilience in the face of the COVID‐19 pandemic: A national study of U.S. military veterans. The Primary Care Companion for CNS Disorders, 23(6), 21br03075. 10.4088/PCC.21br03075 [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei, L. , Huang, X. , Zhang, S. , Yang, J. , Yang, L. , & Xu, M. (2020). Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID‐19 epidemic in Southwestern China. Medical Science Monitor, 26, e924609. 10.12659/MSM.924609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean, C. P. , & Cloitre, M. (2020). Coronavirus Stressor Survey [Unpublished instrument].
- Murphy, D. , Williamson, C. , Baumann, J. , Busuttil, W. , & Fear, N. T. (2022). Exploring the impact of COVID‐19 and restrictions to daily living as a result of social distancing within veterans with pre‐existing mental health difficulties. BMJ Military Health, 168(1), 29–33. 10.1136/bmjmilitary-2020-001622 [DOI] [PubMed] [Google Scholar]
- Na, P. J. , Tsai, J. , Hill, M. L. , Nichter, B. , Norman, S. B. , Southwick, S. M. , & Pietrzak, R. H. (2021). Prevalence, risk, and protective factors associated with suicidal ideation during the COVID‐19 pandemic in U.S. military veterans with pre‐existing psychiatric conditions. Journal of Psychiatric Research, 137, 351–359. 10.1016/j.jpsychires.2021.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola, M. , Alsafi, Z. , Sohrabi, C. , Kerwan, A. , Al‐Jabir, A. , Iosifidis, C. , Agha, M. , & Agha, R. (2020). The socio‐economic implications of the coronavirus pandemic (COVID‐19): A review. International Journal of Surgery, 78, 185–193. 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichter, B. , Hill, M. , Norman, S. , Haller, M. , & Pietrzak, R. H. (2020). Associations of childhood abuse and combat exposure with suicidal ideation and suicide attempt in U.S. military veterans: A nationally representative study. Journal of Affective Disorders, 276, 1102–1108. 10.1016/j.jad.2020.07.120 [DOI] [PubMed] [Google Scholar]
- Ranji, U. , Frederiksen, B. , Salganicoff, A. , & Long, M. (2021). Women, work and family during COVID‐19: Findings from the KFF Women's Health Survey. Kaiser Family Foundation. https://www.kff.org/womens‐health‐policy/issue‐brief/women‐work‐and‐family‐during‐covid‐19‐findings‐from‐the‐kff‐womens‐health‐survey/ [Google Scholar]
- Richardson, J. D. , St Cyr, K. , Forchuk, C. , Liu, J. , Plouffe, R. A. , Le, T. , Gargala, D. , Deda, E. , Soares, V. , Hosseiny, F. , Smith, P. , Dupuis, G. , Roth, M. , Bridgen, A. , Marlborough, M. , Jetly, R. , Heber, A. , Lanius, R. , & Nazarov, A. (2022). Well‐being of Canadian veterans during the COVID‐19 pandemic: Cross‐sectional results from the COVID‐19 veteran well‐being study. European Journal of Psychotraumatology, 13(1), 2012374. 10.1080/20008198.2021.2012374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, E. , Sutin, A. R. , Daly, M. , & Jones, A. (2022). A systematic review and meta‐analysis of longitudinal cohort studies comparing mental health before versus during the COVID‐19 pandemic in 2020. Journal of Affective Disorders, 296, 567–576. 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockman, J. K. , Wood, B. A. , & Anderson, K. M. (2021). Racial and ethnic differences in COVID‐19 outcomes, stressors, fear, and prevention behaviors among U.S. women: Web‐based cross‐sectional study. Journal of Medical Internet Research, 23(7), e26296. 10.2196/26296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suris, A. , & Lind, L. (2008). Military sexual trauma: A review of prevalence and associated health consequences in veterans. Trauma, Violence & Abuse, 9(4), 250–269. 10.1177/1524838008324419 [DOI] [PubMed] [Google Scholar]
- Trivedi, R. B. , Post, E. P. , Sun, H. , Pomerantz, A. , Saxon, A. J. , Piette, J. D. , Maynard, C. , Arnow, B. , Curtis, I. , Fihn, S. D. , & Nelson, K. (2015). Prevalence, comorbidity, and prognosis of mental health among U.S. veterans. American Journal of Public Health, 105(12), 2564–2569. 10.2105/AJPH.2015.302836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh, A. , & Edirappuli, S. (2020). Social distancing in COVID‐19: What are the mental health implications? BMJ, m1379. 10.1136/bmj.m1379 [DOI] [PubMed] [Google Scholar]
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmieri, P. A. , Marx, B. P. , & Schnurr, P. P. (2013). The PTSD Checklist for DSM‐5 (PCL‐5) . https://www.ptsd.va.gov/professional/assessment/adult‐sr/ptsd‐checklist.asp
- Wild, J. , Smith, K. V. , Thompson, E. , Béar, F. , Lommen, M. J. J. , & Ehlers, A. (2016). A prospective study of pre‐trauma risk factors for post‐traumatic stress disorder and depression. Psychological Medicine, 46(12), 2571–2582. 10.1017/S0033291716000532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirkner, J. , Christiansen, H. , Knaevelsrud, C. , Lüken, U. , Wurm, S. , Schneider, S. , & Brakemeier, E. ‐L. (2021). Mental health in times of the COVID‐19 pandemic: Current knowledge and implications from a European perspective. European Psychologist, 26(4), 310–322. 10.1027/1016-9040/a000465 [DOI] [Google Scholar]
- Xiong, J. , Lipsitz, O. , Nasri, F. , Lui, L. , Gill, H. , Phan, L. , Chen‐Li, D. , Iacobucci, M. , Ho, R. , Majeed, A. , & McIntyre, R. S. (2020). Impact of COVID‐19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]


