Abstract
Aim
Sweden initially chose a different disease prevention and control path during the pandemic than many other European countries. In June 2020, the Swedish Government established a National Commission to examine the management of COVID‐19 in Sweden. This paper summarises, and discusses, its findings.
Methods
Three reports published by the Commission were analysed. The first focused on the care of older people during the pandemic. The second examined disease and infection transmission and control and health care and public health. The third updated the first two reports and also covered economic aspects, crisis management and public communication.
Results
By 25 February 2022, when the final report was published, 15 800 individuals, 1.5 per 1000 Swedish inhabitants, had died after COVID‐19. The death rates were high in spring 2020, but overall excess mortality in 2020–2021 was +0.79%, which was lower than in many other European countries. The Commission suggested that the voluntary measures that were adopted were appropriate and maintained Swedes' personal freedom during the pandemic. However, more extensive and earlier measures should have been taken, especially during the first wave.
Conclusion
The Swedish COVID‐19 Commission felt that earlier and more extensive pandemic action should have been taken, particularly during the first wave.
Keywords: COVID‐19, Government inquiry, Pandemic, Schools, Strategy, Sweden
Abbreviations
- ICU
intensive care unit
- NBHW
National Board of Health and Welfare
- PHA
Public Health Agency
- SARS‐CoV‐2
severe acute respiratory syndrome coronavirus 2
Key notes.
Swedish society has been under severe stress from the COVID‐19 pandemic, and the Swedish Government appointed a Commission to examine how the country has handled the crisis.
The Commission suggested that voluntary measures had allowed Swedish people to keep their personal freedom during the pandemic.
However, the Commission also suggested that earlier and more extensive measures should have been taken against the virus, especially during the first wave of the pandemic.
1. INTRODUCTION
Sweden has faced severe issues as a result of the COVID‐19 pandemic. Although Swedish authorities initially followed a disease control path that differed from many other countries, extensive restrictions were implemented at a later date. The pandemic has affected many aspects of daily life in Sweden and has led to a dramatic loss of human life, especially among older and poorer residents. It has also caused unprecedented disruption to family life, work, schooling, the care continuum and society, and no one has escaped its impact.
In late June 2020, the Swedish Government established a national COVID‐19 Commission to examine how Sweden handled the pandemic. Interim reports were published in 2020 1 and 2021, 2 and the final report 3 was published on 25 February 2022. By the time all three reports had been published, 15 800 people in Sweden had died after being diagnosed with COVID‐19, which was 1.5 per 1000 inhabitants, 4 according to the National Board for Health and Welfare (NBHW). The Commission stated in its report that it preferred the organisation's definition of COVID‐19 deaths to the definition of the Swedish Public Health Agency (PHA). 2 The NBHW only included deaths if a physician had indicated that COVID‐19 was the underlying cause of death. The PHA, which also included deaths ≤30 days after someone had tested positive for COVID‐19, 5 had reported 17 497 deaths during the same period. This was 1.7 per 1000 inhabitants (Figure 1). 7
FIGURE 1.
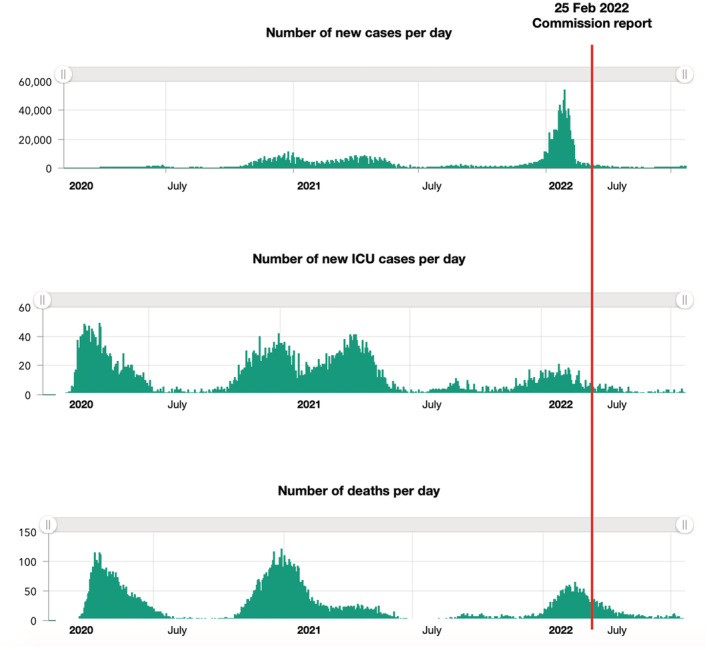
Daily number of new Swedish COVID‐19 cases, cases in intensive care units (ICUs) and deaths after COVID‐19 (according to the Swedish Public Health Agency). 6 In February 2022, public testing for the SARS‐COV‐2 virus, which causes COVID‐19, was no longer encouraged and data on the number of new cases are uncertain after this point. ICU cases and deaths should however still be reliable after February 2022. The number of deaths is discussed in more detail in the main text. The number of cases during the first wave was greatly underestimated because of a lack of testing in spring 2020
During spring 2020, COVID‐19 death rates in Sweden were among the highest in Europe. Overall, excess mortality in Sweden in 2020–2021 was 0.79 per 100 inhabitants, compared with 2015–2019, 8 which was lower than in many other European countries.
This paper summarises the main findings of the three Swedish COVID‐19 Commission reports, by focusing on health‐related aspects and how COVID‐19 was handled in Sweden. 1 , 2 , 3 It complements earlier papers on Sweden's early COVID‐19 strategy 2 , 5 and discusses the Commission's suggestions for strengthening pandemic preparedness.
2. METHODS
On 30 June 2020, the Swedish Government established a national COVID‐19 Commission. The Commission was asked to review the actions taken by the Government, and its agencies, regions and municipalities, to limit viral transmission and the effects of COVID‐19.
The COVID‐19 Commission published three reports on 7 December 2020, 1 18 October 2021 2 and 25 February 2022. 3 The first focused on the care of older people during the pandemic. The second covered disease and infection transmission and control and health care and public health. The third report updated the first two reports and focused on special aspects of the economy, crisis management, communication with the public and the need for more and better quality, data to improve decision‐making.
These reports were read by the author and have been put into a national and international context.
Members of the Commission represented different aspects of society, including health, justice, defence, economic and social sciences. The Commission was chaired by Mats Melin, former President of the Supreme Administrative Court (2011–2018) and Chief Parliamentary Ombudsman (2004–2011). The other members were as follows: Shirin Ahlbäck Öberg (Docent, political science), Ann Enander (Professor, leadership science), Vesna Jovic (Head of social policy at the Swedish Union for Society Academic Professionals; previously CEO of the Swedish Association of Local Authorities and Regions), Camilla Lif (Priest), Torsten Persson (Professor, economics), Göran Stiernstedt (Docent and infectious disease physician) and Mats Thorslund (Professor, social gerontology). External experts helped prepare parts of the reports, Swedish embassies supplied certain information from abroad, for comparative purposes and interviews were conducted with healthcare professionals and other key personnel. On 1 July 2021, the Swedish Government directed all Swedish authorities to cooperate with the Commission and stated that ordinary confidentiality rules were temporarily suspended during the Commission's work. This followed a request from the Commission.
The current paper focuses on the health‐related aspects of the Commission reports, but does not discuss vaccinations and vaccination strategy, as that was not part of the Commission's remit. Finally, the Commission only commented marginally on the Omicron variant of the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), which had higher transmission rates, but was deemed milder than earlier variants. 9 As a result, the conclusions of the Commission reports may not apply to the Omicron or later variants of the severe acute respiratory syndrome coronavirus 2 (SARS‐COV‐2). That is why most of the health‐related information in this review relates to the first, second and third waves of COVID‐19, up to spring 2021.
3. RESULTS
The results are based on the reports and recommendations of the Swedish COVID‐19 Commission. 1 , 2 , 3
3.1. Care for older people
Approximately 20% of the Swedish population are at least 65 years of age, 10 and elderly care consists of social care, residential facilities and other types of support (Table 1).
TABLE 1.
Characteristics of people receiving social care a in Sweden
| Any social care receiver a | The typical social care receiver is an 87‐year‐old woman living alone, with 15 h of external home support per week |
| During a 14‐day period, an average of 16 different care providers (people) will visit a home support beneficiary with ≥2 visits per day | |
| Long‐term residential care facilities for older people b (specifically) | Average age on moving to residential care: 85 years for men and 87 years for women |
| Median duration in residential care: 2.0 years (usually until death) | |
Comorbidity in people living in these facilities:
|
The four most common forms of social care in order of frequency were security alarm, home support, residential care facility for older people and food deliveries.
In Swedish ‘SÄBO’.
In March 2020, the NBHW urged people aged 70 plus to limit personal contacts to avoid COVID‐19. Citizens of all ages were also asked to observe social distancing, wash their hands regularly with soap and water for at least 20 s, avoid non‐essential travel and work from home if possible. The Commission concluded that Sweden's overall strategy to protect older people and other risk groups failed.
A large proportion of individuals who died after COVID‐19 were ≥70 years of age, and many lived in long‐term residential care facilities. Table 1 describes the typical recipients of such care, based on the Commission reports.
3.1.1. Flaws in elderly care
The Commission concluded that the high number of deaths among older people in Sweden, especially during the first wave, was probably due to high overall viral transmission in society. However, other contributory factors included structural deficiencies in residential care and lack of pandemic support for staff. While the Government and its agencies launched several measures in spring 2020 to protect older people, these were often too little and too late. Early reports stated that older people were particularly susceptible to the SARS‐CoV‐2 virus and severe COVID‐19 disease. COVID‐19 guidelines for municipal residential care and for people with dementia were both issued in April 2020, but the NBHW did not recommend extensive testing for people living in residential care facilities until May 2020.
Sweden's elderly care had a number of flaws, including fragmented organisation due to a large number of actors with unclear responsibilities, a lack of common information technology systems and no standard electronic health records. There was also a lack of communication channels, for example between the NBHW and the municipalities that were responsible for elderly care. In addition, residential care facilities often had poor access to medical equipment, were short staffed, had low levels of competence and lacked decent and reasonable working conditions for the staff. The regulatory framework for such care was insufficient, and the municipalities were not allowed to employ physicians.
Elderly care had been neglected and under‐resourced in Sweden until the pandemic, but this also applied to many other countries. In addition, working in elderly care was not seen as an attractive occupation.
3.1.2. Cohort care for the elderly
Many measures undertaken to limit viral transmission did not agree with the values of, and regulations for, Swedish elderly care. One example was cohort care, where staff only cared for patients with COVID‐19, including those who had been moved from elsewhere. While the Commission accepted that extreme measures may be needed in a crisis, it pointed out that such measures must agree with existing laws, which may not have been the case. For example, individuals with dementia may not be legally competent to provide the necessary consent for cohort care outside hospitals.
3.1.3. Access to physicians and medical equipment
Municipalities were responsible for elderly care, but could not employ physicians, as these are employed by healthcare regions or by private healthcare companies. Swedish regions are legally obliged to provide municipalities with medical care for the elderly.
This meant that physicians were less involved in planning elderly care and that municipalities were more dependent on the healthcare regions' priorities. The other Nordic countries did not have similar divisions between regions and municipalities. The Commission suggested that municipalities should be allowed to employ physicians in the future. It also stated that all residential care facilities must have access to the medical equipment needed for good palliative care, including oxygen and intravenous nutrition. Local access to such treatment decreases the need to transport older people to hospital for palliative care.
The Commission agreed that the Government agencies made sure that Swedish health care had sufficient capacity to manage patients with severe COVID‐19 during the first pandemic wave. However, more emphasis should have been put on residential care for older people and the conditions in such facilities that made its residents vulnerable to COVID‐19. It was clear at the beginning of the pandemic that older people faced a high risk of severe COVID‐19.
3.1.4. Visit ban
A national ban on visiting elderly people in residential care facilities was implemented on 1 April 2020, following existing bans in the Stockholm and the Västra Götaland regions, and lasted until 1 October 2020. However, studies have not demonstrated that these bans had a significant effect on viral transmission in such facilities. Despite this, the Commission felt that a national ban should have been instituted earlier, followed by regular re‐assessments. However, the Commission suggested that terminally ill individuals should have been exempt from any visiting bans to allow families to visit.
3.1.5. Healthcare priorities and lack of individual assessments
Before the pandemic, the NBHW had stipulated that priorities for inpatient care use should not be based on chronological age, socioeconomic status, bodily function and whether a condition was self‐inflicted.
Several healthcare regions issued regulatory frameworks on healthcare priorities during the pandemic. Between March and May 2020, the Stockholm region recommended that individuals with a clinical frailty score of 1–4 should be prioritised. Later research found that frailty was an important risk factor for deaths after COVID‐19. 11 Very few care residents would have achieved this score and would have been prioritised for care. From February to June 2020, the number of older people referred from residential care to specialised care decreased in Sweden. However, the Swedish Palliative Care quality register showed that palliative care was better in residential care than hospitals. The Commission suggested that the Stockholm region priority recommendations, combined with a lack of equipment and personnel in residential care, may have led to decisions to opt for palliative care rather than hospital care more often than was reasonable.
While the Commission emphasised that guidelines for COVID‐19 management were clear that an individual‐based perspective should be applied in health care, it stated that such policies must always be constructed with care, emphasise individual assessments and avoid simple categorisations.
The Swedish Health and Social Care Inspectorate reviewed the patient charts of 847 individuals in 98 residential care facilities with at least 1 case of COVID‐19. It found that 20% had not been assessed by a physician: 40% of those patients had not been assessed individually by a nurse either. It should be pointed out that, on 7 April 2020, the NBHW had advised physicians to avoid visiting elderly residential care patients when possible. However, the Commission felt that distance visits were inappropriate if the physicians had not dealt with patients before.
3.1.6. How to improve elderly care to withstand the next pandemic
On 30 March 2020, the Government asked the PHA to formulate a national strategy for COVID‐19 testing and this was published on 17 April 2020. Despite a shortage of testing equipment, the Commission believed that more, and faster, testing should have been carried out among elderly people moving into residential care and individuals who were discharged from hospital to residential care. Their first report on older people during the pandemic recommended improving elderly care and its resilience (Table 2). 1
TABLE 2.
Commission's recommendations for elderly care a
| Staffing levels | The status and appeal of elderly care work must increase. Sweden must clarify what an appropriate staffing level is for residential care and caring for patients with dementia b |
| Employers must facilitate true leadership in residential care and ensure that middle managers are not responsible for excessively large workforces | |
| Employment security and employees paid by the hour | Employment security should increase |
| The proportion of the workforce made up of employees paid by the hour should decrease | |
| Contact between care providers and people receiving care | People receiving care should see the same healthcare staff over time |
| All residential care should have access to a nurse 24/7 to guarantee high medical expertise when residents need intravenous hydration and oxygen and when staff with lower medical competence need supervision and guidance | |
| Competence | The (Swedish) language skills of healthcare staff involved in caring for older people c should improve |
Mostly based on the first wave of the pandemic (spring 2020).
Low staffing levels caused problems such as difficulties to follow COVID‐19 hygiene recommendations because of high workload. Low staffing levels also hindered staff from informing themselves about the pandemic and relevant measures, such as time to read relevant emails.
In the three largest cities in Sweden (Stockholm. Gothenburg, Malmö), 56% of the staff in elderly care did not have Swedish as their primary language. In the rest of the country, the corresponding percentage was 19%.
3.2. Viral transmission and infection control
In spring 2020, Sweden chose a different path from other countries, by mainly focusing on voluntary measures and personal responsibility for COVID‐19, rather than a stricter lockdown. However, there were early compulsory measures that limited the size of public gatherings, banned people from visiting most elderly care residents and introduced distance learning for those aged 17 years or more. Most other countries imposed stricter lockdown measures.
Compared with other European countries, Sweden had a high number of deaths per 1000 population after people developed COVID‐19 during the first wave. COVID‐19 mortality rates were slightly below average during the second wave, and Sweden fared better than most other European countries during the third wave (Figures 1 and 2).
FIGURE 2.
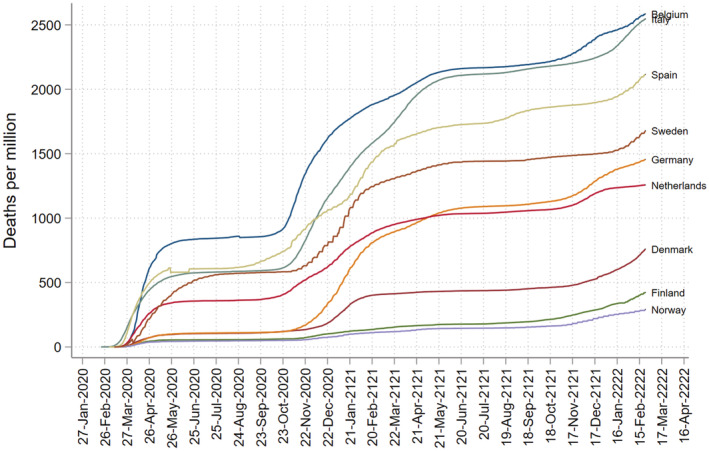
Cumulative mortality per million inhabitants following COVID‐19 in selected European countries up to 25 February 2022. Data in the figure are based on Arnarson (Sci Rep. 2021)
3.2.1. How the virus entered Sweden
The Commission suggested that SARS‐CoV‐2 probably entered Sweden through travellers from Italy and Austria in late February 2020. During Week 9, Stockholm and some other regions had a sports holiday and many Swedes travelled to the Alps for skiing. 12 Deaths during Weeks 14–23 were substantially higher in regions with sports holidays during Week 9 than in other Swedish regions. 12 It was notable that the capitals of Denmark, Finland and Norway had their sports holidays during Week 8, when the viral transmission was substantially lower in the Alps. One study has suggested that 38% of the excess mortality during the first wave could be explained by the sports holiday, 12 and this partly explains the sizable differences in COVID‐19 mortality during the first wave in Sweden.
Before Week 9 in 2020, there was little SARS‐CoV‐2 in Sweden, but after Weeks 10–11, most new cases had contracted the virus within Sweden.
The Commission suggested that proactive and stricter measures should have been applied earlier, in February and March 2020, to limit transmission. They argued that people returning from the Alps should have been recommended to quarantine at home for 7 days and sought testing if they developed a fever or upper respiratory tract symptoms. The Commission also said Sweden should have banned entry to the country in spring 2020. This would have given the Government and its agencies valuable time to make better, and more informed, decisions. The actual measures that were put in place were inadequate to protect high‐risk groups, including older people.
3.2.2. Swedish risk groups for COVID‐19
The risk of infection during the first wave was highest in people with many interpersonal contacts such as those working in large workplaces or with large families. Larger residential care facilities and those with high staff turnover were also more affected, and these had higher mortality.
Individuals with low education or income, immigrants, males and individuals without a partner were at increased risk of needing hospital admissions and intensive care unit (ICU) care for COVID‐19. Sweden had a higher proportion of immigrants (19.1%) and those living in crowded conditions (15.6%) than neighbouring Denmark, Finland and Norway.
The Swedish recommendations to mitigate transmission included working at home when possible. However, this guidance was more suitable for people whose work was computer based, than those who could not work at home.
Elderly people and people living in residential care were in the high‐risk groups, especially during the first and second waves, and the Commission suggested that viral transmission in residential care homes was linked to the high overall viral transmission in society. Furthermore, the viral variants seen in residential care during the first wave were similar to those in people travelling to Italy and Austria during Week 9. There is some evidence that the virus was mainly introduced to residential care through social care providers, rather than through family members. Whether the residential care home was operated privately or directly by the municipality does not seem to have influenced morbidity or mortality risks.
3.2.3. Voluntary measures and laws
The Commission suggested that voluntary, rather than mandatory, measures were suitable, because they gave Swedish people more personal freedom than many other countries. The Swedish approach assumed individual responsibility and mobile phone data did show a substantial decrease in mobility in Swedish society in early March 2020. This would probably have reduced viral transmission. This reduced mobility occurred even before the PHA issued recommendations to limit travel and to work from home.
Pandemic measures were too few and too late and the Commission concluded that these should have been more extensive, particularly during the first wave and considering the limited knowledge about COVID‐19. This delay included the late use of legal measures to allow for more decisive actions. The Commission concluded that changes in the Communicable Disease Act allowed certain activities and operations to be shut down, but decisions should have been made earlier. The Act stipulates that measures should be proportionate and evidence‐based or empirically proven. The PHA also argued that measures should be sustainable over time and acceptable to the population. Quarantine measures can be recommended in Sweden, but it is challenging to carry them out in residential care. The only legal action that could be taken against someone with the virus who broke the quarantine rules was isolation in hospital. However, hospitals were already crowded with patients with severe COVID‐19.
Work on a temporary Pandemic Act only began in August 2020 and was valid from 10 January 2021 to 31 March 2022. The aim was to allow the Government, its agencies, and, to some extent, municipalities to initiate and adapt restrictions quickly. Another aim was to better control viral transmission by restricting public gatherings, venues for cultural events and leisure, shops and malls, public transport and domestic flights and venues for private gatherings. The Pandemic Act complemented the Swedish Communicable Disease Act and the Authorisation Act. It was broader than existing laws that were considered insufficient to tackle the pandemic.
3.2.4. Insufficient preparedness for the pandemic and stressed healthcare staff
The Swedish infection control framework was decentralised and fragmented, so it was unclear who had the overall responsibility when COVID‐19 hit Sweden.
The Swedish healthcare system was able to scale up COVID‐19 care, largely thanks to healthcare staff. However, the re‐adjustments that were required put considerable strain on staff and postponed ordinary healthcare activities. Staff felt tense and stressed by the excessive workload and persistent concerns about getting the virus. These concerns may have been exacerbated by the lack of protective equipment and the fear that recommendations on protective equipment by the authorities were based on the availability of equipment rather than best evidence. There were also contrasting recommendations by different government agencies. Staff also experienced mental stress due to the large number of severely sick patients and high mortality rates. Their concerns could also have been related to ethical stress, resulting from feelings of personal inadequacy.
The Commission concluded that excessive workloads, harsh working conditions and postponing regular health care would have long‐term adverse effects.
3.2.5. Measures during the second and third waves
During the second and third waves, the Government and its agencies launched several new and robust measures (which they had previously rejected or refrained from using), to reduce the transmission of the virus. These included restrictions in restaurants and commercial areas, household quarantine if a family member had COVID‐19 and wearing facemasks on public transport during the rush hour. The latter applied between 7 January and 28 June 2021 for individuals aged 17 years or more. The changes between the first and second waves were not based on any new knowledge. Some measures in late autumn 2020 were initiated by the Government rather than requested by the PHA. These included no alcohol in restaurants and limits on the number of people allowed at public gatherings.
The Commission said the new measures were reasonable, but suggested that introducing them late during the second wave, without motivation, may have created confusion and lowered compliance. They said that using facemasks on public transport and indoors (but outside peoples' homes) should have been recommended earlier. Of note, none of the Nordic countries encouraged the public use of facemasks during the first wave.
Sweden's measures were not as strict as comparable countries in late March to May 2020, but did not differ after that period (Figure 3).
FIGURE 3.
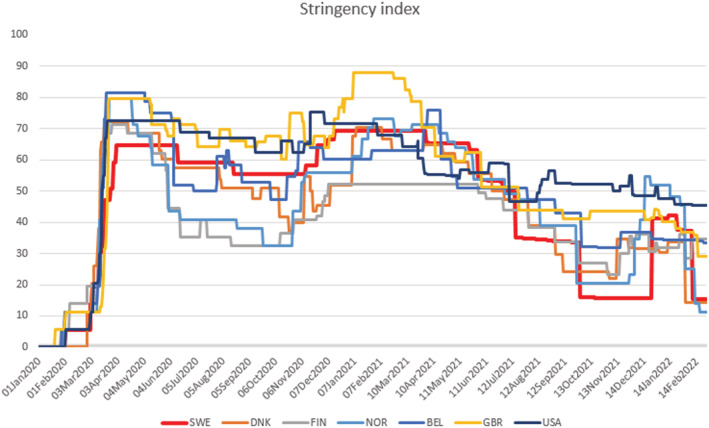
COVID‐19 government response (Stringency Index)* in Sweden and selected countries, according to the Blavatnik School of Government, University of Oxford, 1 January 2020 until 25 February 2022. Swe, Sweden (red line). DNK, Denmark. Fin, Finland. Nor, Norway. Bel, Belgium. GBR, Great Britain. USA, United States. A high index equals a more stringent lockdown (with the highest numbers for Great Britain (yellow) in early 2021. *The Stringency Index is a composite measure based on nine response indicators including school closures, workplace closures and travel bans
3.2.6. SARS‐CoV‐2 testing
The scope and need for virus testing were enormous, not least because the virus needed to be diagnosed to trace and report an infectious disease. That required a systematic testing approach. Effective testing requires personnel, equipment, funding and protective equipment, and this coincided with the need for resources to care for patients with COVID‐19. Scaling up testing in Sweden was slow, and this may partly have been because the country's pandemic preparedness had focused on influenza rather than a coronavirus.
In April 2020, the Government aimed to carry out 100 000 COVID‐19 tests per week, but that goal was only reached in September 2020. The scale‐up of testing was substantially slower in Sweden than in Norway, Denmark and Finland. The first guidelines for COVID‐19 tracing were published on 22 July 2020.
Tracing was initially restricted to contacts in the last 24 h prior to symptoms, despite the 48 h recommended by the World Health Organization. This was only extended to contacts 24–48 h before the onset of symptoms in February 2021. Mobile phone apps were never used for tracing in Sweden, but 13 million text messages were sent to all Swedish mobile phones on 14 December 2020 to emphasise the new stricter COVID‐19 recommendations.
Close contacts were tested as part of disease tracing: asymptomatic adults from March 2021 and asymptomatic children from April 2021.
The Commission believed that one reason for the relatively slow build‐up of testing capacity was the PHA's early guidelines that prioritised testing for four groups. The first two groups were tested on 12 March 2020, and these were very sick people who needed to be admitted to hospital because of potential COVID‐19 and personnel in health care and residential care with known exposure or symptoms. The third and fourth groups were tested on 17 April 2020, and these were individuals who were vital to society, such as key workers working outside health care. Certain healthcare regions thought testing the third and fourth groups was outside their responsibility and demanded extra funding for this.
The Commission felt that the PHA's decision to prioritise the first two groups was reasonable given the initial lack of testing capacity, but suggested that the PHA should have clarified that any prioritisation was only temporary until the regions had attained full testing capacity. The Government allocated 1 billion Swedish Krona, about 100 million United States dollars, for testing. However, it was unclear who was responsible for testing the third and fourth groups and who would provide the funding that was needed. This may have led to further delays in large‐scale testing.
Most of the testing in Sweden used the polymerase chain reaction (PCR) technique, but in April 2021, the PHA allowed the use of antigen tests to increase testing capacity, speed up disease tracing and test patients admitted to hospital.
3.2.7. Protective equipment
The need for protective equipment and garments increased dramatically during the early pandemic and countries competed for the limited supplies held by manufacturers.
During the first wave, personnel had to work without appropriate protection, especially in elderly care and municipal care facilities. The Commission said that the Swedish Kommunal union reported that the residential facilities that lacked protective equipment had more COVID‐19 cases than the facilities with such equipment.
The risk of a shortage of protective equipment was pointed out both by the Swedish Civil Contingency Agency and the NBHW in early February 2020, but the Board did not control the equipment supplies in the municipalities until April 2020.
The Government and the NBHW were clear that they needed to purchase items for regions and municipalities to cover initial shortages, but there were several complications. The NBHW was given the responsibility for securing protective equipment, but had little experience of large‐scale procurement. It made limited purchases of protective equipment in February 2020, but government agencies did little to prevent shortages until mid‐March. In addition, some suppliers were unsure about whether they could sell directly to regions and municipalities.
The Commission pointed out that, over time, regions and municipalities secured large amounts of protective equipment for healthcare organisations and elderly care, supplemented by private businesses and civil society. However, some companies had trouble communicating with the responsible agencies. The Commission concluded that communication must improve, including public agencies' willingness to accept contributions from the private sector and civil society. In addition, national preparedness, such as supplies of protective equipment, must improve. The Commission also stated that the NBHW lacked the experience to procure large supplies of protective equipment and should not have been asked to do this.
The shortage of protective equipment shortage eased during late spring 2020, and there were only selected shortages in certain regions during the third wave in spring 2021.
There were several examples of successful collaboration between regions and municipalities and the private sector to supply protective equipment, but the Commission argued that the regions should have stockpiled more equipment and medication to handle a catastrophe more efficiently.
The Commission said there was a lack of explicit instructions on what protective equipment should be used when working with individuals with suspected versus confirmed COVID‐19. That confusion may have contributed to the increased transmission of COVID‐19 in residential care facilities for older people.
The need for medication increased during spring 2020, but most demands were met. Certain drugs were in short supply, such as propofol shortage for ICUs in April 2020.
3.3. The Swedish healthcare system
3.3.1. Pre‐pandemic situation
The Swedish healthcare system had several deficiencies before the pandemic, including limited continuity and access and numerous incompatible IT systems and the lack of data. Data that could have facilitated decision‐making during the pandemic were lacking. In addition, regions and municipalities were short of healthcare staff.
The strengths of the Swedish healthcare system are high‐quality medical care, highly developed specialised care, increasing digitalisation and services that are well received and accessed because they are free or affordable.
3.3.2. Increasing pressure on the healthcare system
From March to April 2020, hospital admissions for COVID‐19 increased, particularly in the Stockholm region. 2 Sweden had the fewest hospital beds per 1000 residents in the European Union in 2017: 2.2 versus the European Union average of 5.5. The growing number of COVID‐19 patients put enormous pressure on the Swedish healthcare system and required immediate changes and resource re‐allocations. It was only able to meet the exceptionally high demands for care because of its healthcare staff, who endured difficult working conditions. All patients who needed inpatient or ICU care received it.
Mobile healthcare teams became more common during the pandemic, but development work was suspended. Digital care increased, but it became clear that better communication between different computer systems was needed. The Commission also believed that more knowledge was required about long COVID/post‐COVID and such knowledge should be shared with primary care and other healthcare suppliers.
Local infectious disease departments usually led and supervised clinical care in each region and issued local COVID‐19 guidelines. The number of COVID‐19 patients greatly exceeded bed capacity in the infectious disease departments and ICUs and patients needed to be cared for in other departments during the pandemic waves.
During the peaks of waves 1–3, some 50–60 new patients with COVID‐19 were admitted to Swedish ICUs each day. In 2019, the median ICU duration for pre‐pandemic patients was 1.1 days, but it was 6.1 days for COVID‐19 patients in 2020. This increased the ICU burden, especially because many patients required mechanical ventilation and chronic renal replacement treatment. The bed shortage led to frequent transfers between ICUs and between regions. Various aspects of ICU health care were tracked daily by the Swedish Intensive Care Register, 13 which became a major source of information on severe COVID‐19. The PHA had previously used this quality register for influenza surveillance.
Meanwhile, primary care focused on testing, contact tracing, lending personnel to hospitals and later vaccinating the public.
3.3.3. Private healthcare suppliers
Private healthcare suppliers contributed to the pandemic efforts by lending staff, caring for COVID‐19 patients and carrying out surgery that would otherwise have been delayed. However, the Commission suggested that binding agreements with private healthcare suppliers should be considered in the future, which would require them to support public health care in times of national crisis. This is most pertinent in regions where private care is common.
3.3.4. Postponed and delayed health care
The care of COVID‐19 patients delayed or made some other health care impossible, and this is likely to have had an impact on the incidence of several diagnoses. Physical visits to primary care facilities and hospitals decreased and digital visits increased. The reduction in physical visits also affected planned surgery and procedures. For example, inpatient episodes of myocardial infarction decreased by 10% in 2020 (Table 3).
TABLE 3.
Postponed and delayed health care in 2020
| Child health |
Obesity probably increased in children aged 3–5 years of age and this increase could have been higher in groups with low socioeconomic status. In a report from the Swedish opinion poll institute in May 2020, a quarter of children aged 8–18 years reported having exercised less in 2020. The proportion was even higher in children aged 16–18 years, at almost a half. Childhood vaccination rates were not affected and remained high throughout the pandemic |
| Prescriptions/dispensed medication |
Increased dispensing of antihypertensives a and asthma a medication in spring 2020. Decreased dispensing of antibiotics in spring 2020, mostly in children |
| Inpatient episodes decreased (hospital‐based admissions and visits) |
Cardiovascular disease (−9%) Myocardial infarction (−10%) Respiratory disease (−31%) Cancer (−9%) Musculoskeletal disease (−18%) Number of rheumatoid arthritis visits to departments of medicine/rheumatology (−20%) Gastrointestinal disease (−5%) Psychiatric care (−4%) Neurological disease (−8%) Visits for certain immune‐mediated diseases decreased, including eye disease examinations for patients with diabetes |
| Visits to health care |
20% of all adults reported abstaining from seeking health care during the pandemic. 39% of all adults said they had avoided or delayed seeking health care |
| Cancer screening |
Breast cancer screening was paused in certain regions Cervical cancer screening (−5%) |
| Surgery |
Planned surgery (−11%) Emergency surgery (−3%) |
| Other | Follow‐ups for certain major cancers were affected |
Note: Data from the Commission reports and personal communication with Professor Anders Ekbom (Karolinska Institutet, 31 July 2022).
During the first wave, some thought that these drugs would protect people against COVID‐19.
Many people also stayed away from healthcare facilities, unless they had COVID‐19, to avoid catching or transmitting the virus.
Overall, child health and maternal health care were less affected by pandemic prioritisation, but there were indications that groups with low socioeconomic status fared worse than other groups. In 2020, cancer diagnoses in Sweden decreased more in people born outside Europe than those from Europe. They also decreased more in individuals with low education than in those with high education.
Table 3 outlines various areas where the pandemic affected diseases, conditions and procedures.
3.3.5. The Communicable Disease Act and the role of infection control physicians
The Communicable Disease Act is based on free will and personal responsibility, but it stipulates the use of specified measures to counter the transmission of communicable diseases. These include testing, tracing and quarantine. The Commission believed that some measures were never appropriately applied and that the individual nature of the Act failed to protect the population. For instance, the Act stipulates that disease isolation should occur at hospitals, which was practically impossible when there were thousands of cases, especially if hospitals were already caring for large numbers of sick people. Other measures, such as banning visits to residential care facilities for older people or restaurant restrictions, were not covered by the Act. The limits of the Act complicated efforts to stop viral transmission in Sweden.
The Commission suggested that the PHA should have temporarily paused their evidence‐based approach when an unknown virus hit society and taken precautions instead. Not doing so contributed to the initial failure to limit viral transmission.
The Commission also believed that the relationships between regional infection control physicians and healthcare regions were unclear. These physicians should have acted independently of the regions' economic and organisational capabilities, but the independence and influence of individual physicians varied dramatically. The Commission recommended that the role of these physicians be strengthened.
3.3.6. Poor mental preparedness and fragmented crisis management
Despite an earlier evaluation that showed that Sweden was poorly prepared for H1N1 influenza, commonly known as swine flu, in 2009–10, preparedness was still low when COVID‐19 struck. Many municipalities and larger county administrative boards were not formally prepared for a pandemic. Large‐scale pandemic exercises had been rare and targeted influenza. All these factors may have contributed to delays in important decisions. However, the Commission also underlined that the mere existence of pandemic preparedness plans does not effectively cope with a pandemic. Mental preparedness is also needed to act on weak evidence. Furthermore, the Commission suggested that the Government seek help from external experts, outside its agencies, in such a situation. The Government consulted external experts to some extent, but these were almost exclusively medical experts. They did not include experts in the social and behavioural sciences, which would have been relevant to the pandemic.
The Commission said that the PHA should have an official mandate to coordinate the work of different actors regarding pandemic preparedness and infection control. It did not believe that actors who have operative responsibility under usual circumstances should necessarily have the same responsibility during a crisis. This is because during a crisis, the fragmentation of such a system may lead to unclear boundaries of responsibility and a failure to apply a national perspective. During the Swedish pandemic, the PHA led the pandemic response but the fact that it both evaluated the risks and suggested the crisis management had weaknesses. Still, the Commission suggested it may be helpful for one Government agency to have broader responsibility for handling national crises. Furthermore, any central agency, in this case the PHA, should be prepared to request input from external sources.
The PHA appointed an advisory board on 17 April 2020, and the Commission believes this was too late as the main strategy was already in place by then. Furthermore, the skills and competencies of the advisory board were not used optimally, and meetings were irregular. The Commission suggested that the PHA should have asked for more input from additional external actors, including those with a more critical view of the Swedish strategy.
Much of the communication between the government and the 21 regions and 290 municipalities was handled by the Swedish Association of Local Authorities and Regions, which played a crucial role during the pandemic. The Association is an employer organisation that covers all regions and municipalities in Sweden. It supports its members and aims to improve regional and local autonomy. However, the organisation lacked absolute authority over regions and municipalities and did not have to adhere to the usual transparency rules that were mandatory for all Swedish government agencies. The Commission argued that the regions, and in particular this central Association, should have launched more extensive testing and tracing during the first wave.
Pandemic responsibilities were scattered and the response to COVID‐19 was fragmented. The responsibilities tended to be geographical, but pandemics do not normally respect administrative boundaries. More action by the Government, and possibly larger regional bodies, would have been desirable and the Commission recommended that administrative healthcare reforms should be considered.
3.4. Measures related to work and education
3.4.1. Social isolation and home working
The Commission indicated that the pandemic had substantial indirect health effects. Distance working and learning and social isolation negatively affected people's physical and mental health, but these effects were skewed. Socioeconomically deprived groups suffered more from postponed health care, loss of income and unemployment due to the pandemic. Some people had occupations that made home working impossible and some did not have, or could not afford, cars that enabled them to avoid them being exposed to the virus on public transport.
Older people were often affected by long‐term social isolation, were fearful of COVID‐19 and sometimes did not receiving appropriate health care if they became ill. Disabled people also suffered from isolation, particularly those with neurocognitive and functional impairments.
The Commission cited social workers who suggested that there had been more violence, drug abuse and poorer psychiatric health during the pandemic, especially in those with low socioeconomic status. Several regions stated that the number of reports of suspected child abuse and maltreatment to social services had increased, although the NBHW has suggested that this increase may not have been related to COVID‐19.
There was no increase in diagnosed psychiatric diseases in 2020, but these may develop over time and access to psychiatric care may have been limited in 2020 (Table 3).
There has been no clear evidence of increased violence during the pandemic, although the Commission acknowledged that there could be a lack of high‐quality data to form a complete picture. Although digitalisation eased social isolation for many people, not everyone had access to, or could benefit, from it. The long‐term consequences of the dramatic increase in youth unemployment are yet to be determined.
Civil society played an important role in countering the harmful effects of social isolation during 2020–21, and the Government allocated extra funding, especially for sports associations and clubs.
3.4.2. Open schools and distance learning
During spring 2020, and to some extent until spring 2021, distance teaching was used for high school students aged 17 years or more. Elementary schools and kindergartens remained open, with minor exceptions for some upper secondary school students aged 14–16 years. Distance learning was mandatory for universities. Overall, access to teaching was good in Sweden during the pandemic, but it was difficult to perform certain practical teaching tasks. Some between‐group and between‐school differences in teaching quality and learning results worsened during the pandemic. Students with neurocognitive and functional impairment probably suffered from the transition to distance learning in spring 2020. Data suggest that stress and anxiety increased in students, especially high school students, when distance learning was applied. However, data are inconsistent, as younger children's results and grades seemed to be unaffected during the pandemic. 14
The Commission agreed with the decision to keep schools open, but suggested that other venues with intense personal contact, such as restaurants and swimming pools, should have been closed during the early pandemic. It also felt that cultural and sports events should have been cancelled.
3.5. Overall recommendations from the Commission
The three Commission reports 1 , 2 , 3 contain hundreds of suggestions or reflections. Some merit particular mentions and are listed in Table 4.
TABLE 4.
Selected health and healthcare recommendations from the Swedish COVID‐19 Commission
| A precautionary principle |
While crisis management in Sweden should be based on principles of responsibility, similarity and subsidiarity, a precautionary principle or a principle of action should be added. The Commission defines the precautionary principle as ‘that it is better to act than to wait for better data for decision‐making, and then later modify one's actions as new knowledge becomes available’. (from the English‐language summary of the Commission reports). This means deploying ‘sufficient resources for a relatively major incident and subsequently stand some of them down if it turns out that they are not needed’ |
| Pandemic preparedness a | Sweden needs to strengthen its pandemic preparedness, at governmental, regional and municipal levels, including mental and legal preparedness and material and organisational preparedness |
| Government leadership | In a future crisis, the Government, rather than government agencies, should assume leadership of all aspects of crisis management. Furthermore, the Government should not rely solely on one agency for advice. A national crisis management group should be established that directly reports to the Government |
| Documentation | Crisis management decisions must be better documented |
| International collaboration | Sweden needs to improve international collaborations related to communicable diseases and build up emergency stockpiles, both nationally and within the European Union (EU). The EU collaboration to purchase vaccines was regarded as successful |
| Public communication |
Swedish authorities must improve infectious disease prevention and control communications to all parts of society and make sure they are clear. Statements such as ‘Do not participate in large gatherings such as weddings’ or ‘think about whether you could save a trip until next Easter’ should have been clarified and sometimes replaced by clearer and more concise language. Communication should have been more inclusive b |
| Communicable Disease Act | The Communicable Disease Act needs to focus more on health at the population level |
| Administrative reforms | Sweden needs to reform its administrative model, decrease the number of actors in health care and municipal care and increase regional, national and international cooperation |
| Care for older people | The staffing and quality of elderly care must increase |
| Information technology systems | The country needs more efficient information technology systems, including follow‐up testing and analysis |
| Need for data for improved decision‐making | Data are currently missing on primary care, residential care for older people, social care, municipal health and short‐term sick leave c . Such data must be available to researchers and decision‐makers to prepare for future pandemics |
Not all pandemics are due to influenza. Before COVID‐19, Sweden's pandemic preparedness targeted a relatively short influenza pandemic in which older adults were already expected to have some immunity through earlier influenza exposure. There was also an expectation that effective vaccines would be available within 4–5 months in the event of an influenza pandemic.
After the H1N1 influenza pandemic, young people and people who spoke other languages than Swedish as their native language were difficult to reach with recommendations and advice.
Primary care is often responsible for patients with chronic diseases such as type 2 diabetes and psychiatric disorders. Primary care data would also have been useful on the long‐term, follow‐up consequences of the pandemic on mental health. Data on short‐term sick leave would have helped monitor viral transmission in society and the pandemic's impact on society.
4. DISCUSSION
This review shows that the Swedish COVID‐19 Commission identified crucial weaknesses and failures in the country's response to the pandemic. However, it also showed several areas where Sweden may have stood out from other countries and yielded potentially long‐term benefits. The largest benefit was avoiding strict lockdowns and allowing Swedish residents to protect their natural freedom.
The Commission was not convinced of the benefits of lockdowns for future pandemics, as countries with lockdowns during the COVID‐19 pandemic rarely fared better than countries without lockdowns (Figures 2 and 3). Lockdowns exact a high price for self‐determination and subjective well‐being and public acceptance of long‐term lockdowns may be low, as evidenced by street protests in countries with recurrent lockdowns.
Sweden kept schools open for most children up to 16 years of age. Despite this, children also paid the price during the pandemic. According to the Commission, Swedish children indicated that cancelled leisure activities and not being able to play with their peers were major drawbacks of the pandemic. Several reports have shown that social isolation had a significant impact on the mental health of young people. 15
Much of the Commission's work focused on 2020 and particularly on the first wave, when many of the shortcomings and limitations of Sweden's pandemic preparedness became most apparent. However, although the overall excess mortality for 2020–2021 was lower than in many other countries, the Commission argued that more extensive and earlier action should have been undertaken during the first wave.
Many countries were surprised that Sweden chose a different strategy for COVID‐19 prevention during the first wave than most European countries, including its Nordic neighbours. A lot of older people died in Sweden after COVID‐19 during the first wave, probably as result of high viral transmission in the community. However, the Commission raised three other potential and contributory factors. The first was institutional factors, such as care fragmentation. The second was decisions taken by the Government and other actors, including prioritising health care rather than elderly care when responding to the pandemic. The third was random factors, such as a high proportion of vulnerable people in Sweden due to milder influenza in the preceding years. The Commission suggested that the proportion of deaths in elderly care, as a percentage of total deaths, may not have been higher in Sweden than in most other countries if the impact of previous milder influenza on vulnerability had been factored in. Overall, the excess mortality in Sweden in 2020–2021 was +0.79% compared with 2015–2019.
Until now, crisis management in Sweden has been based on three principles: responsibility, similarity and proximity. Responsibility refers to actors who have operative responsibility during usual circumstances and should have the same responsibility during a crisis. Similarity means that an organisation should be similar in peacetime, crisis and war. Proximity means that decisions during a crisis should be made at the lowest level possible. The COVID‐19 Commission agreed with the Swedish Catastrophe Commission in 2005, following the 2004 Tsunami, that a precautionary principle, or principle of action, should be applied when it is not possible to ascertain the facts, because information is absent or ambiguous. In other words, they argued that it is better to take action and change decisions as new information becomes available (Table 4). It was particularly noteworthy that Sweden seemed to have applied this precautionary principle to economic issues but not to the same extent in health care.
Applying a new principle for crisis management has enormous implications and some pre‐pandemic and pandemic approaches have attracted widespread criticism. From 2010 to 2011, a large proportion of the Swedish population was vaccinated against the H1N1 swine flu strain and this was followed by an increase in narcolepsy in children. 16 The Government's active, and precautionary, approach back then was subsequently criticised for being overly ambitious. Many countries have also been criticised for closing schools in 2020 and 2021 as a precaution. Sweden differed from its Nordic neighbours in keeping schools open and applying less strict measures (Figure 3). However, it is notable that the aims of the Nordic countries were similar. For instance, both the Danish and the Norwegian prime minister stated in March 2020 that they aimed to mitigate rather than suppress COVID‐19. Norway has published its COVID‐19 Commission report, 17 while Denmark has so far focused their assessment of the national COVID‐19 strategy on the culling of 17 million minks after a mutated SARS‐CoV‐2 virus was detected. 18
The Swedish Commission said that more data needed to be available to produce more effective policy decisions. It has called for better integration of information systems, including between regions and municipalities. However, the additional data gathering will come at a price, as it will further reduce the time spent on patients. In addition, it could cause a shift in resources from patient‐oriented health care to greater administration, which focuses more on data collection than patients. However, better data from the areas pinpointed by the Commission are needed and this should cover primary care, residential care for older people, social care, municipal health and short‐term sick leave. This should be as close to real time as possible if such data are to make a difference during a pandemic. The need for faster and more extensive data would challenge the current structure of Swedish health care and the medical quality registers that are run by healthcare professionals, not the Government. The daily updates from the Swedish ICU Register played an essential role during the COVID‐19 pandemic and was a key data source for decision‐making.
The final Commission report was published on 25 February 2022 and reviewed actions on COVID‐19 up to that point, 3 but much of the preparation for the reports was carried out in 2021 and focused on 2020. 1 , 2 , 3 Hence, the validity of the Commission report may be lower for 2021 than 2020. The Commission did not comment on the medical management of COVID‐19 in Sweden and for that reason I have also added a review of the critical features of the hospital‐based clinical management of COVID‐19 during the third wave in Sweden (Table 5).
TABLE 5.
Management of COVID‐19 in adults at one regional hospital in Sweden during the third wave in spring 2021
| Common indications for hospital admission in patients with COVID‐19 |
|
| Underlying comorbidity and implications for care |
|
| Laboratory data and their implications for care |
|
| Thorax CT scan | Perform in all patients needing high‐flow/airvo oxygen or mechanical ventilation. Look for pulmonary embolism, ground‐glass appearance (early disease) or consolidation (late disease) |
| Prone position | Preferred sleep position for patients with severe COVID‐19. It may cause pain in the neck (treat with paracetamol) |
| Dexamethasone use |
|
| Tocilizumab |
|
| Remdesivir |
|
| Thromboprophylaxis |
At hospital discharge: apixaban 2.5 mg*2 for 2 weeks (4 weeks if severe COVID‐19). Consider higher dosage if the patient had apixaban already before COVID‐19 disease |
| Bacterial infections |
|
| Other COVID‐19‐related health measures |
|
| Measures at discharge |
|
| Regarded as non‐contagious | Always required before declared non‐contagious: 2 days with normal temperature and general improvement, plus:
|
Note: Based on the personal experience of Jonas F Ludvigsson and local guidelines. The table refers to Örebro University Hospital principally serving the Örebro region.
The cut‐off for admission varied. In times of severe pressure in the wards, only COVID‐19 patients with a breathing frequency exceeding 35 were admitted to hospital.
Patients with cancer, neutropenia or certain immunosuppressive medications.
Overall, the Commission reports are well written and provide a comprehensive review of the largest health crisis in Sweden since the Spanish influenza pandemic after World War One. The Commission not only highlights structural deficiencies, but also shares some constructive guidelines for future pandemic management.
Despite this, some of the Commission's conclusions can be questioned.
The focus on the first three waves, until spring 2021, may have underestimated the benefits of a Swedish strategy that emphasised long‐term sustainability. While the excess mortality was high during the first wave, 5 the excess mortality in Sweden during the first two years of the pandemic was lower than in many other countries. The final Commission report 3 slightly modified the criticism in reports 1 and 2, 1 , 2 but some advantages of the Swedish approach to COVID‐19 could have received greater attention.
Also, the Commission's conclusion that government authorities should have been more cautious, but that it was appropriate not to close schools, shows some inconsistency. It may seem illogical that they urged caution but, in hindsight, did not support school closures. Throughout the reports, the Commission state that more robust measures should have been implemented during the first wave. However, it does not state that the viral transmission may have been so extensive in Sweden that more decisive steps may only have had a minimal impact on mortality rates.
The Commission also failed to discuss the alternative costs of putting a massive number of international travellers in quarantine, in Week 9 and other weeks in 2020, when it was unclear whether COVID‐19 would develop into a pandemic. The Commission suggested that a ban on entering Sweden from abroad should have been applied in spring 2020, but all prohibitions, including disrupting travel between southern Sweden and Denmark, would have come at a price. Given Sweden's extensive viral transmission, it is logical to question whether any ban on foreign travel would have improved the situation.
The Commission states that the Swedish Government should have listened to external experts, but did not suggest who and how. Such clarification could help to anticipate other kinds of catastrophes, such as a new Chernobyl accident in Sweden or a climate disaster where expert knowledge would be needed to interpret information and make more informed, evidence‐based decisions. Throughout the report, the Commission argued that the Government should have listened less to its experts, namely the PHA, and taken the lead. However, examples from other countries, such as the mink culling in Denmark, have shown that politicians risk overstretching their mandates in a crisis.
My review had some limitations. It exclusively focused on the Commission reports and did not aim to review all the literature on COVID‐19 in Sweden. Up to 2 August 2022, some 4000 papers referred to Sweden and COVID‐19 in the PubMed database.
Another limitation was that my review has not detailed risk groups, as extensive research already covers this, and COVID‐19 risk factors are well‐known to the medical community. In addition, the current review does not focus on COVID‐19 aspects not directly linked to health care and health, such as employment and economic support. Lastly, my review does not cover COVID‐19‐related communication with the public, the interaction between authorities and government agencies, vaccinations against COVID‐19 and the later different PHA recommendations according to vaccination status.
5. CONCLUSION
This review of the National Commission reports on Sweden's COVID‐19 approach confirms that Sweden initially chose a different approach to COVID‐19 than many other European countries. The Commission suggests that voluntary measures, rather than mandatory measures and lockdowns, were suitable and safeguarded more personal freedom during the pandemic. However, the Commission has also indicated that more extensive and early measures against COVID‐19 should have been undertaken, primarily during the first wave of the pandemic.
FUNDING INFORMATION
No funding.
CONFLICT OF INTEREST
The author has worked on research projects with several people involved in the Commission and its expert groups, but they had no involvement in this completely independent review of the Commission's reports.
ACKNOWLEDGEMENTS
I am grateful to Björn Thor Arnarson for Figure 2 and Bjorn Roelstraete for Figure 3.
Ludvigsson JF. How Sweden approached the COVID‐19 pandemic: Summary and commentary on the National Commission Inquiry. Acta Paediatr. 2022;00:1–15. 10.1111/apa.16535
REFERENCES
- 1. Coronakommissionen . Delbetänkande 1: Äldreomsorgen under pandemin (Elderly care during the pandemic– SOU 2020:80) 2020. https://coronakommissionen.com
- 2. Coronakommissionen . Delbetänkande 2: Sverige under pandemin (Sweden during the pandemic)– SOU 2021:80 2021. https://coronakommissionen.com
- 3. Coronakommissionen . Slutbetänkande: Sverige under pandemin (Sweden during the pandemic) – SOU 2022:10 2022. https://coronakommissionen.com
- 4. Nise L. Personal communication, July 27.: Socialstyrelsen (Swedish national board of health and welfare), 2022.
- 5. Ludvigsson JF. The first eight months of Sweden's COVID‐19 strategy and the key actions and actors that were involved. Acta Paediatr 2020;109(12):2459–71. [published Online First: 2020/09/21]. 10.1111/apa.15582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Swedish Public Health Agency . Confirmed cases of COVID‐19 in Sweden 2022. Accessed 26 July, 2022. https://www.folkhalsomyndigheten.se/smittskydd‐beredskap/utbrott/aktuella‐utbrott/covid‐19/statistik‐och‐analyser/bekraftade‐fall‐i‐sverige/
- 7. Personal communication July 26, 2022: Folkhälsomyndigheten (Swedish Public Health Agency).
- 8. Johansson T. Personal communication August 2, 2022: Statistiska Centralbyrån (Statistics Sweden).
- 9. Wolter N, Jassat W, Walaza S, Welch R., Moultrie H., Groome M., Amoako D.G., Everatt J., Bhiman J.N., Scheepers C., Tebeila N., Chiwandire N., du Plessis M., Govender N., Ismail A., Glass A., Mlisana K., Stevens W., Treurnicht F.K., Makatini Z., Hsiao N.Y., Parboosing R., Wadula J., Hussey H., Davies M.A., Boulle A., Von Gottberg A., Cohen C. Early assessment of the clinical severity of the SARS‐CoV‐2 omicron variant in South Africa: a data linkage study. Lancet 2022;399(10323):437–46. [published Online First: 2022/01/23]. 10.1016/S0140-6736(22)00017-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ludvigsson JF, Almqvist C, Bonamy AE, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol 2016;31(2):125–36. [published Online First: 2016/01/16]. 10.1007/s10654-016-0117-y [DOI] [PubMed] [Google Scholar]
- 11. Hagg S, Jylhava J, Wang Y, et al. Age, frailty, and comorbidity as prognostic factors for short‐term outcomes in patients with coronavirus disease 2019 in geriatric care. J Am Med Dir Assoc 2020;21(11):1555‐59 e2. [published Online First: 2020/09/27]. 10.1016/j.jamda.2020.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bjork J, Mattisson K, Ahlbom A. Impact of winter holiday and government responses on mortality in Europe during the first wave of the COVID‐19 pandemic. Eur J Public Health 2021;31(2):272–77. [published Online First: 2021/02/25]. 10.1093/eurpub/ckab017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Emilsson L, Lindahl B, Koster M, et al. Review of 103 Swedish Healthcare Quality Registries. J Intern Med 2015;277(1):94–136. [published Online First: 2014/09/02]. 10.1111/joim.12303 [DOI] [PubMed] [Google Scholar]
- 14. Hallin AE, Danielsson H, Nordstrom T, et al. No learning loss in Sweden during the pandemic evidence from primary school reading assessments. Int J Educ Res 2022;114:102011. [published Online First: 2022/06/10]. 10.1016/j.ijer.2022.102011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McCracken LM, Badinlou F, Buhrman M, et al. Psychological impact of COVID‐19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur Psychiatry 2020;63(1):e81. [published Online First: 2020/08/28]. 10.1192/j.eurpsy.2020.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Persson I, Granath F, Askling J, Ludvigsson J.F., Olsson T., Feltelius N. Risks of neurological and immune‐related diseases, including narcolepsy, after vaccination with Pandemrix: a population‐ and registry‐based cohort study with over 2 years of follow‐up. J Intern Med 2014;275(2):172–90. [published Online First: 2013/10/19]. 10.1111/joim.12150 [DOI] [PubMed] [Google Scholar]
- 17. Koronakommisjonen . Myndighetenes håndtering av koronapandemien. (Norwegian COVID‐19 commission) (https://www.regjeringen.no/no/dokumentarkiv/regjeringen‐solberg/aktuelt‐regjeringen‐solberg/smk/nyheter/2021/koronakommisjonen‐overleverer‐kommisjonens‐sluttrapport‐til‐statsministeren/id2844008/). See also: https://www.regjeringen.no/contentassets/d0b61f6e1d1b40d1bb92ff9d9b60793d/no/pdfs/nou202220220005000dddpdfs.pdf, 2022.
- 18. Folketinget . Granskningskommissionens beretning om sagen om aflivning af mink. https://www.ft.dk/samling/20211/almdel/GRA/bilag/46/index.htm, 2022.


