Abstract
To describe hearing‐health service use, especially use of telehealth, during the early stages of the COVID‐19 pandemic in deaf/hard‐of‐hearing children. In 2020, the Victorian Childhood Hearing Longitudinal Databank surveyed 497 (61.6%) families of deaf/hard‐of‐hearing children aged 0.4–19.6 years, with 449 (90.3%) providing quantitative data and 336 (67.6%) providing free‐text comments about COVID‐19's impact on service use and access. We summarised quantitative data using descriptive statistics and analysed free‐text responses using inductive and deductive reasoning. Of the 1152 services families used during the pandemic, 711 (62%) were accessed via telehealth. Parents reported several challenges and facilitators of service access during the pandemic, particularly regarding telehealth. Parents reported that their child found telehealth appointments more difficult (347/665, 52.1%) and of worse quality (363/649, 55.9%) compared to in‐person. These difficulties were more evident in pre‐school than school‐age children. Consideration of these factors when implementing telehealth practice beyond the pandemic would improve family experiences, ensuring quality of care.
Keywords: COVID‐19, deaf, hard‐of‐hearing, mixed methods, telehealth
1. INTRODUCTION
The declaration of the coronavirus disease 2019 (COVID‐19) pandemic created large and grave implications for healthcare systems and governments around the world. Healthcare organisations had to rapidly acclimatise as demand for remote consultations increased following COVID‐19 restrictions and public health measures (Núñez et al., 2021). An explosion in the uptake of telehealth services in Australia followed COVID‐19, rising from <1% of all consultations prior to the pandemic to 28% of all federally funded consultations by the second half of 2020 (Taylor et al., 2021). Whilst telehealth is beneficial in minimising the risk of COVID‐19 transmission for both patients and health providers (Monaghesh & Hajizadeh, 2020), it is important to consider what role telehealth can play for different clinical groups and whether it can deliver the same level of care as in‐person services.
Children who are deaf and/or hard‐of‐hearing (DHH) are known to experience greater difficulties in accessing healthcare services when compared to children with typical hearing (Bush et al., 2017). Low rates of utilisation of healthcare services have also been described in families of children who are DHH from low socio‐economic backgrounds (Boss et al., 2011). Timely access to early intervention, including audiology, allied health and medical services is crucial in optimising language development and quality‐of‐life for children who are DHH. A study by Ching et al. (2017) demonstrated that when compared to children who received a cochlear implant at 6 months, children who received a cochlear implant at 24 months had lower language scores at 5 years of age. Another study by Roland et al. (2016) demonstrated that children who are DHH had lower quality‐of‐life scores across multiple domains (social and school) when compared to children with typical hearing. Furthermore, the same study highlighted an improvement in the quality‐of‐life scores following intervention thereby demonstrating the importance of timely access to audiology, early intervention services and medical care.
Telehealth has played an increasingly important role in the paediatric setting, with its applications extending beyond speech‐language pathology to physical therapy and psychology services (Havenga et al., 2015). Two studies conducted throughout the early stages of the pandemic that explored the role that telehealth services had in facilitating physiotherapy assessments and the provision of psychological services for children indicated that telehealth services played a vital role in facilitating access during the pandemic, especially when in‐person services were unavailable (Payne et al., 2020; Zischke et al., 2021). However, both studies referenced above left the impression that whilst telehealth services certainly provided access for children and their families, it was dangerous to assume that telehealth services were likely to overtake or replace in‐person services in the future. In fact, as both studies have noted, further research is needed to explore the validity and applicability of telehealth services, and the continuing role that telehealth services are to play in the provision of quality healthcare.
Indeed, whilst the value of telehealth cannot be understated, it is important to also consider how accessible and appropriate telehealth services are for children who are DHH and their families, given the unique challenges that COVID‐19 created for families and health providers. Furthermore, finding ways to optimise telehealth services for children who are DHH and their families is vital, especially beyond the pandemic where there will be a likely trend in continuing telehealth practice.
The aim of this study was to describe hearing‐health service use during the early stages of the COVID‐19 pandemic for children who are DHH. We also aimed to describe the perspectives and experiences of parents and children in accessing hearing‐health services during the pandemic, in particular in relation to telehealth, to better understand the challenges and facilitators of service provision in this population.
2. METHODS
2.1. Participants and setting
Data were collected and synthesised from a survey sent out to families enrolled in the Victorian Childhood Hearing Longitudinal Databank (VicCHILD) in May 2020.
VicCHILD is a population‐based longitudinal databank of children with permanent hearing loss, living in the state of Victoria, Australia (detailed information on methodology and population coverage described elsewhere; Sung et al., 2019). Recruitment of eligible participants has been ongoing through (A) the Victorian Infant Hearing Screening Program (VIHSP) since 2012: VIHSP screens >98% of newborns born in the state of Victoria, Australia; VIHSP, on behalf of VicCHILD, approaches and invites families of children diagnosed with permanent hearing loss to participate in the databank; and (B) the Caring for Hearing In Children Clinic (CHIC) at the Royal Children's Hospital, since 2016, a tertiary clinical service offering medical and developmental care for children who are DHH. As of the end of 2021, VicCHILD has more than 1150 participants, with an estimated annual uptake rate of 53.6%. Additionally, approximately 94% of VicCHILD families have consented to be contacted about future hearing‐related research (Sung et al., 2019).
2.2. Procedure
In May 2020, a survey was sent to VicCHILD families who had consented to be contacted, aiming to explore the impact of the COVID‐19 pandemic on children who are DHH and their families. Surveys were completed over a 4‐month period, during which Victoria was heavily impacted by COVID‐19 restrictions, border closures and state‐wide lockdowns. The survey collected demographic data (child age, education level, the degree and type of hearing loss), access/use of hearing‐health services in the last 12 months, and how access/use of services may have changed since the pandemic (e.g. frequency, mode: in‐person/telehealth, ease and quality of access). Families were asked to respond to an open‐ended question: ‘Please add comments about impact on your child's use and access to services’.
We used descriptive statistics to summarise the quantitative data, including type, frequency and mode of service access, parent and child ease in accessing the service, and quality of the service provided. Services were grouped into three categories: (i) audiology (diagnostic or rehabilitation audiology or cochlear implant services), (ii) allied health (early intervention, psychology and speech therapy) and (iii) medical (general practitioners, Ear Nose Throat [ENT], genetics and other specialists). We also summarised data by child education level (pre‐school vs. school‐aged children).
Qualitative data analysis was embedded within an interpretive phenomenological research approach (Matua & Van Der Wal, 2015), using a hybrid approach to thematic analysis, informed by both inductive codes (letting the data speak for itself) and deductive codes (derived from previous theory or research) (Fereday & Muir‐Cochrane, 2006). This provided a basic framework of codes to initially guide the analysis, whilst permitting enough flexibility for themes to emerge organically from the data. The steps outlined by DeCuir‐Gunby et al. (2011) were used as a guide to develop a codebook. Inductive codes were derived from the data, whilst deductive codes were generated using key domains from the survey. Services were grouped into the three categories above (audiology, allied health and medical) for analysis. A general node was created to cater for those who did not refer to any specific services. After initial coding, 10% of the sample was randomly selected to be coded by a senior researcher to establish inter‐rater reliability (DeCuir‐Gunby et al., 2011). Coding differences were noted and discussed to reach consensus. Finally, the collected data were organised into cases using NVivo software, with each case representing an individual participant. A series of nodes were used to represent the different themes and sub‐themes that emerged.
The VicCHILD study has approval from the Royal Children’s Hospital Human Research and Ethics Committee (HREC 31081).
3. RESULTS
Of the 806 VicCHILD families who were sent the survey, 497 (61.6%) families of children aged 0.4–19.6 years completed some or all of the survey. Of note, 449/497 (90.3%) provided quantitative data on health service access and use, and 336/497 (67.6%) provided qualitative data in response to the question regarding the impact of COVID‐19 on their access to services. For the qualitative analysis, a sample of 40 cases (~10%) were randomly selected for independent coding to establish inter‐rater reliability. Table 1 illustrates the participant characteristics, comparing VicCHILD participants who completed the COVID‐19 survey (responders) to those who did not (non‐responders) across a range of demographic and hearing loss information.
TABLE 1.
Participant characteristics
| Responders (n = 497) | Non‐responders (n = 309) | |
|---|---|---|
| Demographics: Child | ||
| Age, years – mean (SD) | 6.6 (4.0) | 7.0 (3.7) |
| Sex: male – n (%) | 298 (60.0%) | 161 (52.1%) |
| SEIFA disadvantage index† − mean (SD) | 1014.5 (69.6) | 1006.0 (68.5) |
| Remoteness area: regional – n (%) | 96 (19.3%) | 55 (17.8%) |
| Hearing loss information | ||
| Hearing laterality – n (%) | ||
| Unilateral | 143 (28.8%) | 84 (27.2%) |
| Bilateral | 320 (64.4%) | 204 (66.0%) |
| Unknown | 34 (6.8%) | 21 (6.8%) |
| Hearing loss type – n (%) | ||
| Sensorineural | 339 (68.2%) | 215 (69.6%) |
| Conductive | 14 (2.8%) | 11 (3.6%) |
| Mixed | 49 (9.9%) | 30 (9.7%) |
| Auditory Neuropathy Spectrum Disorder | 39 (7.8%) | 27 (8.7%) |
| Atresia | 19 (3.8%) | 4 (1.3%) |
| Unknown | 37 (7.4%) | 22 (7.1%) |
| Degree of hearing loss – n (%) | ||
| Mild | 117 (23.5%) | 74 (23.9%) |
| Moderate | 145 (29.2%) | 83 (26.9%) |
| Severe | 84 (16.9%) | 55 (17.8%) |
| Profound | 109 (21.9%) | 76 (24.6%) |
| Unknown | 42 (8.5%) | 21 (6.8%) |
SEIFA = Socioeconomic Indexes for Areas Index of Disadvantage– an index developed by the Australian Bureau of Statistics which ranks areas in Australia according to the relative socioeconomic disadvantage. The higher the number, the more advantaged an area is (national mean 1000, SD 100) (ABS, 2016).
As indicated in Table 1, only 96 (19.3%) of the 497 responders were from inner/outer regional or remote areas, with the rest of the responders being from major cities or metropolitan areas. On average, metropolitan responders had higher SEIFA scores (mean 1023.1, SD 64.8) when compared to regional responders (mean 971.7, SD 47.8).
Table S1 indicates the frequency of visits for each service used by participants during the 12 months prior to completing the survey.
Figures 1 and 2 and Table S2 summarise the parent‐reported data from questions about the frequency, type, ease and quality of health service use during the COVID‐19 pandemic.
FIGURE 1.
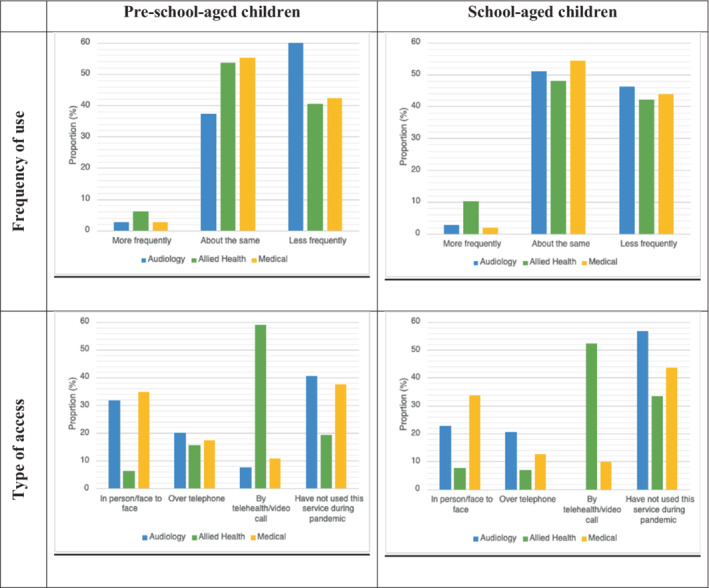
Frequency and type of appointments accessed during the COVID‐19 pandemic by child age‐group. The full questions, responses and proportions are available in Table S2
FIGURE 2.
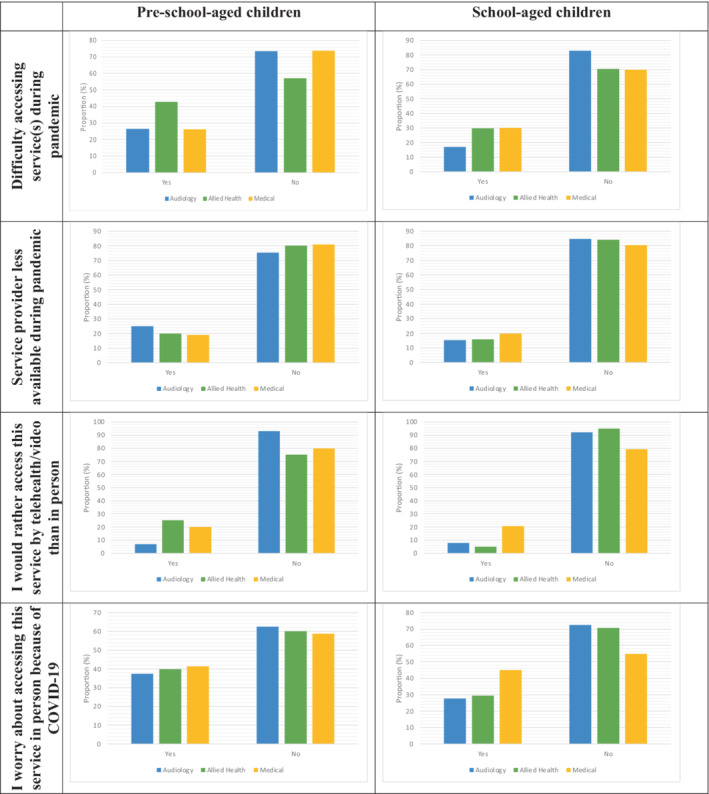
Parent responses about difficulty in accessing services, service provider availability, parent preference for telehealth and worry about accessing services due to COVID‐19. The full questions, responses and proportions are available in Table S2
Figure 1 shows very few children (<10% across all ages and services) utilised services more frequently during the pandemic than they had previously. Around half utilised services about the same and approximately 40% utilised them less frequently than they previously had. Of note, ~60% of pre‐school‐aged children used audiology services less frequently during the pandemic, with <40% using them about the same as usual.
Out of the 1152 reported service access by families throughout the pandemic, 711 (61.7%) were conducted via telephone or telehealth/video call.
Audiology services were poorly utilised during the pandemic, with 40.5% of all pre‐school and 56.7% of all school‐aged children not attending audiology during the pandemic. Those who completed appointments mostly did so either in person or over the telephone.
In comparison, allied health services were mostly accessed via telehealth video for both pre‐school (58.9%) and school‐aged (52.2%) children. A smaller proportion of pre‐school (19.3%) and school‐aged children (33.3%) did not access allied health services at all during the pandemic. The rest accessed allied health services in person or over the telephone.
Medical services (general practitioner, genetics, ENT) appointments were rarely utilised via telehealth (telephone/video) during the pandemic. Most appointments were accessed in person for both pre‐school (34.6%) and school‐aged (33.7%) children. Of note, many pre‐school (37.4%) and school‐aged children (43.6%) did not access medical services during the pandemic.
Figure 2 summarises parent responses about the difficulty in accessing services, service provider availability, parent preference for telehealth and worry about accessing the service due to COVID‐19.
Across all three categories of services, most parents of both pre‐school and school‐aged children reported no difficulty in accessing services during the pandemic. Furthermore, very few parents indicated that service providers were ‘less available’ during the pandemic.
Moreover, across all three categories of services, most parents of both pre‐school and school‐aged children reported a preference for accessing the service in‐person rather than accessing services via telehealth/video. In keeping with this, most parents indicated that they were not worried about accessing services in‐person due to COVID‐19.
Figure 3 describes parent and child ease of telehealth appointments as well as the quality of telehealth appointments compared to in‐person appointments for those who attended a telehealth appointment during the COVID‐19 pandemic.
FIGURE 3.
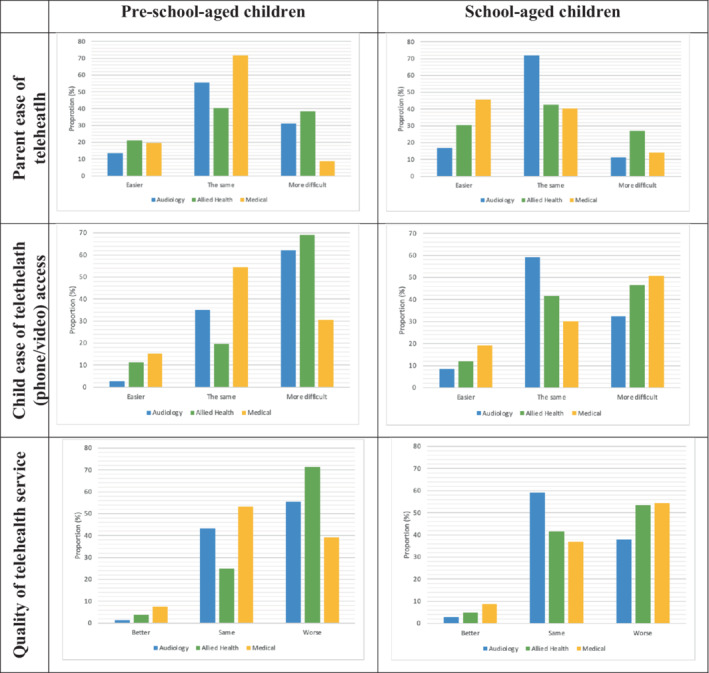
Parent and child ease of service access and quality of telehealth service use during COVID‐19 pandemic by child age. The full questions, responses and proportions are available in Table S2
3.1. Parent ease of service access and use with telehealth
For most services reported to have been accessed by telehealth (327/648, 50.5%), parents reported that using telehealth was about the same for them in terms of ease of accessing or using the service. For about a quarter of the time, parents reported telehealth made it more difficult (167/648, 25.8%) or easier for them (154/648, 23.8%) to access or use the services.
However, these results varied when broken down by service type. Most parents reported that using telehealth during the pandemic made accessing or using audiology services about the same for them in terms of ease of access (55.4% pre‐school, 71.8% school‐aged). In some cases, parents found using telehealth made it easier to access audiology services (13.5% pre‐school, 16.9% school‐aged), while others found it more difficult (31.1% pre‐school, 11.3% school‐aged).
Many parents reported that using telehealth made accessing allied health services about the same for them in terms of ease of access (40.4% pre‐school, 42.6% school‐aged). Some parents reported telehealth made access to allied health services easier for them (21.1% pre‐school, 30.5% school‐aged), whilst others found telehealth made it more difficult to access or use allied health services during the pandemic (38.5% pre‐school, 27.0% school‐aged).
In most cases (71.7%), parents of pre‐school‐aged children reported using telehealth did not change the ease of access and use of medical services during the pandemic, with parents reporting easier access in 19.6% of cases, and more difficult in only 8.7% of cases. On the other hand, parents of school‐aged children reported that telehealth made access to medical services easier during the pandemic in 45.6% of cases, with parents reporting that access was the same for them in 40.4% of cases, and parents reporting that access was more difficult in only 14.0% of cases.
3.2. Child ease of service access or use with telehealth
In most cases (347/665, 52.2%), parents reported using telehealth to access or use the service was more difficult for their child. In about a third of cases (241/665, 36.2%), using telehealth to access or use the service during the pandemic was about the same in terms of ease for their child while in the remaining cases (77/665, 11.6%) parents reported telehealth made it easier for their child to access and use the service.
Responses varied by service type. In most cases (62.2%), parents of pre‐school‐aged children reported telehealth made access and use of audiology services more difficult for their child, with 35.1% reporting that their child's ease of access to audiology remained unchanged, and only 2.7% reporting that access was easier during the pandemic. In contrast, in 32.4% of cases, parents of school‐aged children found telehealth made access to audiology services more difficult, in the majority of cases (59.2%), ease of access was unchanged and in only 8.5% of cases access was easier during the pandemic.
Parents reported that telehealth made access and use of allied health services more difficult for their child in the majority of cases (69% pre‐school‐aged and 46.5% of school‐aged). In a smaller number of cases (11.3% pre‐school‐aged, 12% of school‐aged), parents reported that using telehealth made access easier for their child, and in 19.7% of cases for pre‐school‐aged and 41.6% of cases for school‐aged children access was the same during the pandemic.
Likewise, in the majority of cases (54.4%), parents of pre‐school‐aged children reported that ease of access and use of medical services via telehealth was the same for their children during the pandemic. Interestingly, in the majority of cases (50.7%), parents of school‐aged children reported that telehealth made access to medical services more difficult for their child during the pandemic. In a minority of cases (30.4%), parents of pre‐school‐aged children reported that telehealth made access to medical services more difficult for their child, with parents reporting that telehealth made access easier for their pre‐school‐aged child in only 15.2% of cases. In contrast, school‐aged parents reported it was easier for their child to access medical services in 19.2% of cases, and that ease of access to medical services using telehealth remained the same in 30.1% of cases.
3.3. Quality of telehealth service compared to in‐person services
For approximately half of those services accessed by telehealth during the pandemic (336/649, 55.9%), parents reported that the quality of telehealth services was worse when compared to in‐person.
Parents of pre‐school children more often reported poorer quality of services delivered via telehealth compared to in‐person, and indicated a preference for in‐person appointments (audiology: 55.4%, allied health: 71.4%, medical services: 39.1%). Meanwhile, in a large proportion of cases, parents of school‐aged children reported no change in the quality of services delivered via telehealth as compared to in‐person (audiology: 59.2%, allied health: 41.6%, medical: 36.8%). Furthermore, consistently across all services for all children (both pre‐school and school‐aged), in a small minority of cases, parents reported better quality of service and preference for telehealth over in‐person (<9%).
Figure 4 describes how well telehealth services met the needs of the parent and child, according to education level.
FIGURE 4.
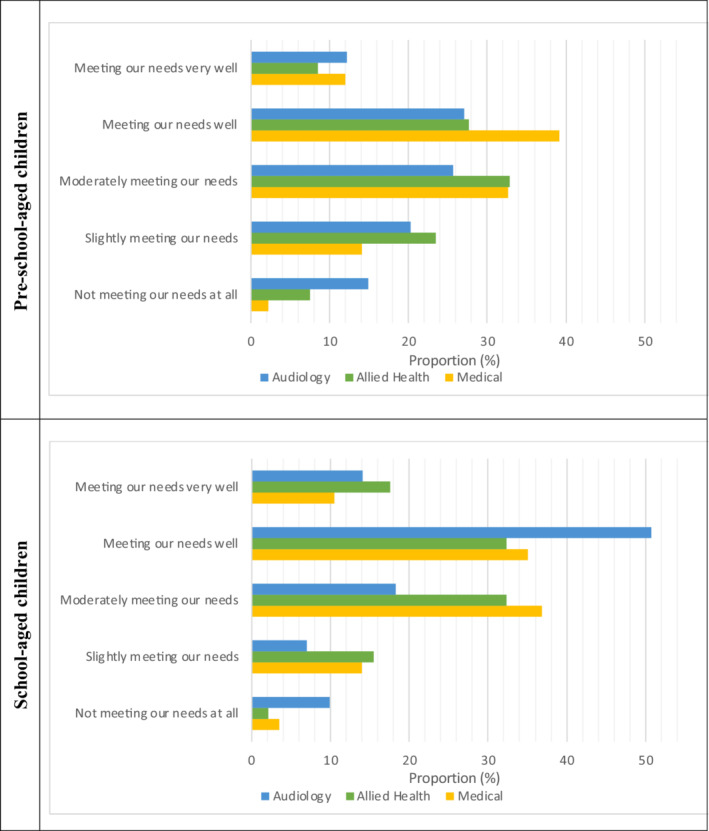
How well telehealth services met the needs of the parent and child. The full questions, responses and proportions are available in Table S2
Overall, in most cases (~75%–85% of those services accessed using telehealth during COVID‐19), parents reported that telehealth was meeting their needs at least moderately. However, some parents reported that the care they were receiving from their service/health professional via telehealth was not or only slightly meeting their needs. In a third of cases (~35%), preschool children's parents reported their audiology service did not or only slightly met their needs. Allied health services were also often (~30%) not/slightly meeting needs. Medical services were more likely to meet needs with only ~16% reporting their service not meeting/slightly meeting needs.
Comparatively, school‐aged children were more likely to have their needs met at least moderately. In most cases (~83%), parents of school‐aged children reported that their audiology service was at least moderately meeting their needs. Most allied health services (~82%) were at least moderately meeting their needs. Similarly, most medical services (~83%) were at least moderately meeting their needs.
The impact of the pandemic on hearing‐health service access and use were examined in more depth using qualitative analysis. Themes and sub‐themes were identified and categorised under two main headings: the challenges and facilitators of hearing‐health access and use. Figures 5, 6, 7, 8, 9, 10, 11 include quotes that illustrate the different themes regarding the challenges of hearing‐health access, categorised into one of four headings to demonstrate the relevant service (i.e. G – general, AU – audiology, AH – allied health, M – medical). Figures 12, 13, 14, 15 include quotes that illustrate the different themes regarding the facilitators of hearing‐health access.
FIGURE 5.

Parent comments describing delay or difficulty accessing services
FIGURE 6.
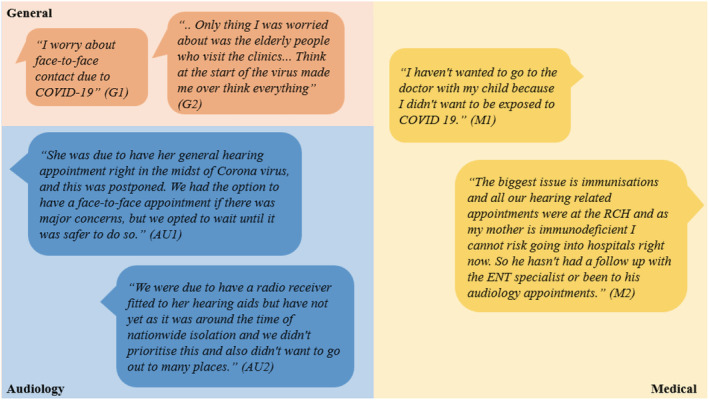
Parent comments describing anxiety related to COVID‐19
FIGURE 7.
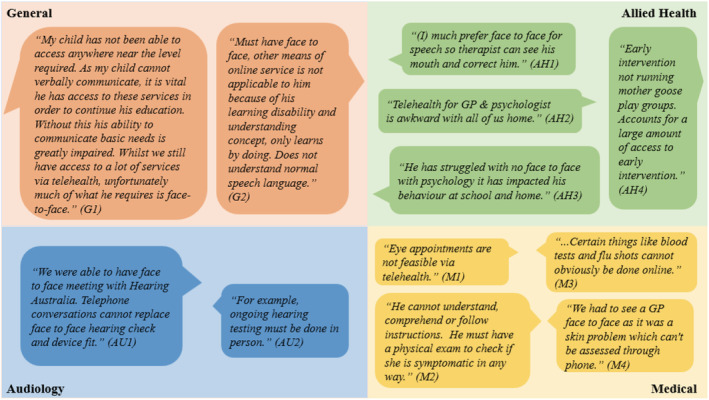
Parent comments describing preference or requirement for in‐person services
FIGURE 8.
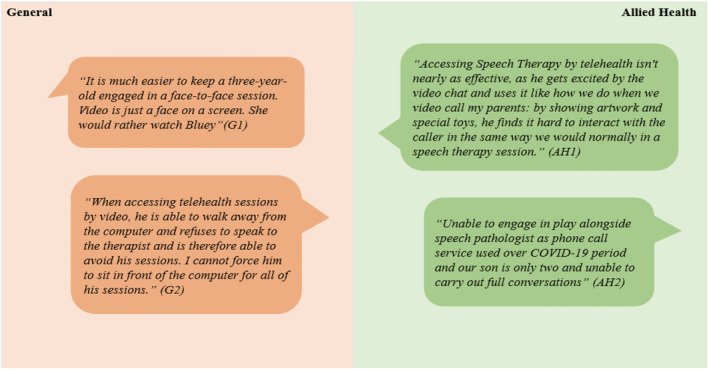
Parent comments describing their child's reduced attention span in telehealth sessions
FIGURE 9.

Parent comments describing the increased need for parental input or involvement with telehealth appointments
FIGURE 10.
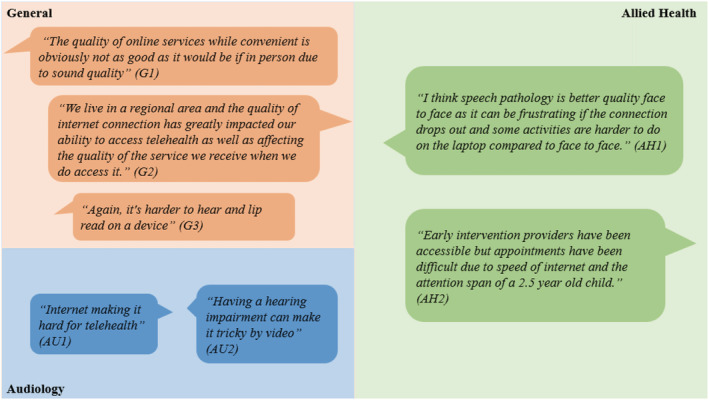
Parent comments describing technical issues with telehealth
FIGURE 11.
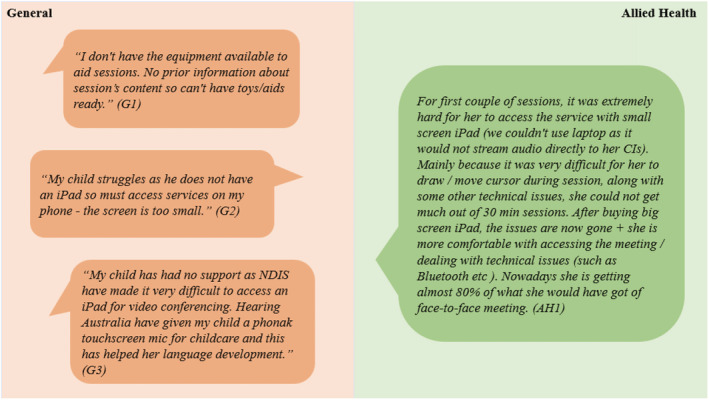
Parent comments describing lack of equipment or funding for telehealth
FIGURE 12.
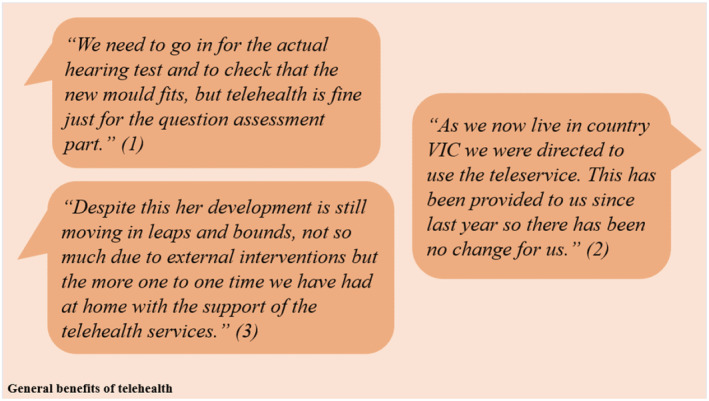
Parent comments describing the general benefits of telehealth
FIGURE 13.
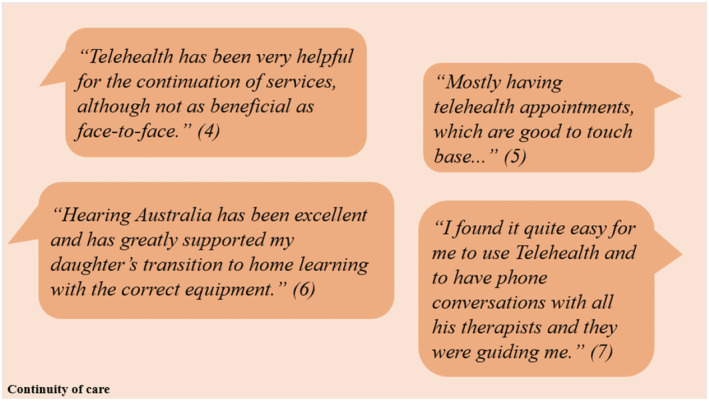
Parent comments describing the continuity of care provided via telehealth
FIGURE 14.

Parent comments describing the convenience of telehealth
FIGURE 15.
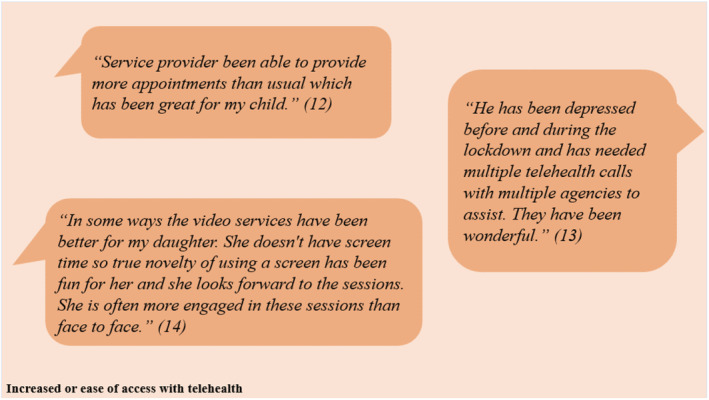
Parent comments describing the ease of access via telehealth
3.4. The challenges of hearing‐health service access and use
Four main themes were reported by participants regarding the challenges of accessing and using hearing‐health services throughout the COVID‐19 pandemic and are described below: (1) delay or difficulty in accessing services, (2) anxiety related to COVID‐19 exposure, (3) preference or requirement for in‐person services and (4) reduced quality of telehealth sessions. Themes and sub‐themes are discussed below.
3.4.1. Delay or difficulty in accessing services
Figure 5 summarises the key comments from parents describing delays or difficulty accessing health services throughout the COVID‐19 pandemic. Some parents experienced longer waiting times (G1), with not enough service providers or appointments available. Others expressed an inability to engage with online services as some providers only operated on an in‐person basis (G2).
Regarding audiology‐related services, some parents found it difficult to get their child's hearing devices fitted or fixed in time, with longer wait times and appointment cancellations due to restrictions (AU1, AU5). One parent reported a delay in accessing cochlear mapping appointments (AU2). Other parents expressed difficulties in being able to access audiology services on their own, especially for parents who are juggling multiple responsibilities including home‐schooling and caring for their other children (AU3). Temporary school closures also meant that some families were unable to receive assistance in their children's educational setting, from specialised teachers for the deaf (AU4).
Allied health services were also harder to access with longer waiting times (AH1) and insufficient providers or appointments (AH2). Access was further complicated for families residing in rural or remote areas (AH2). Medical services including routine check‐ups, specialist appointments and nonurgent surgeries were delayed following COVID restrictions (M1, M2).
3.4.2. Anxiety related to COVID‐19
Figure 6 summarises the key comments from parents describing a degree of anxiety surrounding COVID‐19 exposure. Some parents were concerned about their personal safety and their risk of exposure to the virus (G1, M1). Others were apprehensive of the risk that in‐person appointments had on high‐risk population groups, such as the elderly and immunocompromised individuals, especially when considering the odds of asymptomatic transmission of the virus (G2, M2).
As a result of this, several parents elected to postpone any in‐person appointments or appointments that they perceived to be unnecessary to minimise their exposure and transmission risk (AU1, AU2). This inevitably had an impact on timely access to medical and audiology services that required in‐person contact, preventing some children from accessing immunisation and device fitting appointments.
3.4.3. Preference or requirement for in‐person services
Figure 7 summarises the significant number of parents' comments indicating a preference for in‐person appointments. Some parents voiced their concerns that telehealth was an inappropriate substitute for interactions that required in‐person contact. A variety of reasons underpinned this. Some children were non‐verbal (G1). Others had intellectual or learning disabilities (G2), which made communication with therapists complicated and difficult over telehealth. Furthermore, some parents reported the superiority of in‐person and its perceived benefits over telehealth. This was especially true for speech therapy as it allowed therapists to be more effective and encouraged children to apply the required motor techniques for proper speech and language development (AH1).
Additionally, some parents reported that telehealth appointments were inappropriate for specific medical and audiology‐related services. For instance, hearing tests and device fit checks had to be conducted via in‐person sessions (AU1, AU2). Furthermore, physical examinations including skin and eye checks, blood tests and vaccinations were all components of a consultation that had to be performed in‐person (M1, M2, M3, M4).
Psychology services were also generally deemed inappropriate over telehealth. One parent reported that attending psychology via telehealth with other family members present at home was awkward, implying privacy concerns for their child (AH2). Another parent reported the impact of the absence of in‐person psychology on their child's behaviour at school and home (AH3).
Furthermore, in‐person services also provided children with the opportunity to interact, play and socialise with each other, for instance through parent–child play groups. This was an element that was reported as missed by parents throughout the pandemic, and one that could not be accommodated for with telehealth and online learning (e.g. AH4).
3.4.4. Reduced quality of telehealth sessions
Many parents reported that telehealth sessions were of reduced quality and benefit when compared to in‐person consultations. Whilst a variety of reasons were reported, a few main sub‐themes were evident. These could be summarised into four main categories: (a) reduced attention span, (b) increased need for parental input or involvement throughout or following the consult, (c) technical issues associated with telehealth appointments and (d) lack of equipment or funding required for effective engagement.
Reduced attention span: In general, children were reported to have a shorter attention span when interacting with different healthcare providers over telehealth. Figure 8 provides examples of children losing interest (G1), being easily distracted (AH1), being too young to effectively engage or communicate (AH2), or being unable to sit still throughout their sessions (G2). Many parents implied or stated that these difficulties could have been avoided or at least reduced to a large extent with in‐person consultations.
-
B
Increased need for parental input or involvement: Figure 9 provides examples of comments suggesting that telehealth sessions create an extra layer of complexity for some parents. Telehealth meant that some parents had to prepare in advance for the session (G1). Others had to be present at the time of the consult to assist their children, with a greater emphasis on the parents to direct the sessions. Parents also had to be present to constantly ensure that their children remained engaged with the clinician or therapist (G2). Furthermore, some parents were tasked with additional homework or programmes to work on with their child following the session (AH1, AH2). This created a burden on some, especially for parents that were juggling other responsibilities at home, such as home‐schooling and work commitments.
-
C
Technical issues with telehealth: Figure 10 describes the technical challenges for some families. Video and sound quality and the quality of the Internet connection, especially in rural and regional areas, were low for some families. This impacted children's ability to interact and engage with therapists and other staff. Furthermore, children with a significant degree of hearing loss or those that relied on lip reading struggled to understand and communicate throughout their sessions. As one parent pointed out, ‘it is harder to hear and lip read on a device (G3)’.
-
D
Lack of equipment or funding: Figure 11 summarises parent concerns regarding a lack of equipment or aids necessary for telehealth sessions (G1, G3, AH1). Access to iPads or other devices that facilitated video conferencing was crucial for proper engagement (G2). Furthermore, as one parent pointed out, these devices had to be of an appropriate size to allow for children to engage effectively with their therapists – for instance, to be able to use functions that allowed the child to draw or move the cursors in response to the therapist's instructions (AH1).
3.5. The facilitators of hearing‐health service access and use: The benefits of telehealth
Whilst many parents voiced a preference for in‐person over telehealth, some acknowledged the value of telehealth in providing quality care and support to families and their children. Parents suggested telehealth was entirely appropriate for certain elements of a consult, even if an in‐person assessment is required for physical assessments (Figure 12, comment 1).
Some parents, especially those who were accustomed to attending appointments via telehealth, reported very little change with the pandemic, stating that it had little or no impact on their child's access to healthcare services or the quality of care that they received (Figure 12, comment 2).
Additionally, it is possible that in the absence of telehealth, childhood development could have been impacted. Telehealth has allowed for the provision of support and services that is crucial for the development of children's social, language and speech skills. In many ways, it bridged the gap that would have been felt if families were left unsupported throughout the pandemic with no in‐person contact (Figure 12, comment 3).
The benefits of telehealth can be divided into three major themes: (1) continuity of care, (2) convenience of telehealth and (3) increased/ease of access.
3.5.1. Continuity of care
Telehealth has allowed families to stay connected with healthcare providers. It provided parents the opportunity to raise any concerns or questions, and to ensure adequate follow‐up (Figure 13, comments 4 and 5).
Parents also reported that they felt especially supported and cared for when it came to telehealth services assisting them in their transition to attending therapy sessions and school from home (Figure 13, comments 6 and 7).
3.5.2. Convenience of telehealth
Many parents expressed that telehealth was incredibly convenient, as it allowed families to access vital health services from the comfort of their own homes. Families could easily avoid many of the difficulties associated with in‐person services – for instance, travel times and costs, taking time off work or school, childcare arrangements for other children. For these reasons, some expressed the view that they would continue accessing services via both modes (in‐person and telehealth), even after the pandemic (Figure 14, comments 8 and 9).
Interestingly, one parent mentioned that the home setting facilitated a more natural and organic environment for the child, allowing clinicians to observe different sets of behaviours that would have otherwise been missed in an in‐person clinical setting. Another parent also reported telehealth to be beneficial as it allowed them to be more involved with their child's therapy sessions, and to gain a more holistic view of what occurs during their sessions (Figure 14, comments 10 and 11).
3.5.3. Increased or ease of access with telehealth
Some parents reported an increased availability of appointments via telehealth, which was beneficial for their child's well‐being and allowed for constant follow‐up. Thus, parents were able to increase the number of therapy sessions that their child could attend from home. This was important for some families, especially when it came to accessing psychology services to assist children with anxiety and/or depression (Figure 15, comments 12 and 13).
Some parents also reported that their children enjoyed attending telehealth sessions, even if they were more distractable. One parent even reported that telehealth was superior to in‐person for their child, as the novelty of video services and screen time kept her engaged (Figure 15, comment 14).
4. DISCUSSION
Overall, this study provided valuable insights into the lived experiences of hearing‐health service access and use in families of children who are DHH throughout the early stages of the COVID‐19 pandemic in Victoria, Australia. Healthcare access for children who are DHH has been previously recognised as a complex issue, involving multiple patient and provider factors (Bush et al., 2017). Thus, it is no surprise that the pandemic added another layer of challenge for children who are DHH and their families, and further complicated their timely access to services (Taylor et al., 2021).
4.1. Key findings
Our findings demonstrated that most families accessed allied health and medical services as often and easily as they accessed services prior to the pandemic, with no obvious major differences between pre‐school and school‐aged children. The only exception to this was for audiology services, where a slight majority of families of both pre‐school and school‐aged children accessed services less frequently but with the same level of ease compared to prior to the pandemic.
This was made possible by the use of telehealth services during public health lockdown restrictions, with 711 (61.7%) of the 1152 services accessed by families throughout the pandemic reported to be conducted via telehealth/video call. Moreover, across all three categories of services, most parents of both pre‐school and school‐aged children reported no difficulty in accessing services during the pandemic and that access to service providers was not reduced during the pandemic. Interestingly, whilst this reflects the overall trend reported by parents that they found access to services via telehealth easy, the same could not be said for how easy it was for their children to access services via telehealth. Only a small number of parents (25.8%, 167 of 648) reported difficulty in accessing services via telehealth; however, almost half of parents (52.2%, 347 of 665) reported difficulties for their children in accessing services via telehealth.
Thus, despite the financial incentives and funding that were provided by the Australian government to support the implementation of telehealth services throughout the early stages of the COVID‐19 pandemic, access to healthcare services via telehealth was not feasible for some families, at least in the early stages of the pandemic (Fisk et al., 2020). Many parents reported a preference for in‐person services, and that care delivered by telehealth was of a lower quality. This was consistent across all categories of services accessed by participants, and applicable to both pre‐school and school‐aged children. Indeed, almost half (55.9%, 336 of 649) of the number of parents who reported they attended an appointment during the pandemic via telehealth and answered the question regarding the quality of service compared to in‐person indicated that telehealth services were of worse quality when compared to in‐person services. Moreover, parents of pre‐school children were less likely to report that telehealth services met their needs at least moderately when compared to parents of school‐aged children. Whilst multiple reasons are likely to underlie this disparity, as reported by Sezgin et al. (2021), engagement during telehealth appointments has been outlined as an important challenge for paediatric populations, with younger children potentially finding it harder to engage compared to older children.
4.2. The preference for in‐person care
Audiology and medical services were accessed more frequently in‐person than were allied health services, which were more commonly accessed via telehealth or over telephone for both pre‐school and school‐aged participants. This could indicate the need for the family and child to be physically present for many audiology and medical consults to achieve the goal of the consultation. For example, many parents suggested physical examinations and audiology assessments were harder to perform over telehealth, whereas allied health and early intervention services were more transferable and accessible via telehealth. One study of children with cystic fibrosis in the United States during COVID‐19 revealed comparable findings, with a majority of parents reporting poorer interactions and quality of care delivered via telehealth due to the lack of physical examinations and sputum or throat cultures (Solomon et al., 2021).
Thus, it is not surprising that in‐person services were perceived by many parents as more beneficial for their children. A study by Havenga et al. (2015) that compared parental perceptions on conventional intervention versus tele‐intervention for children with hearing loss also reported similar findings, with parents reporting that in‐person services were more beneficial, comfortable and familiar to them and their children. However, as all participants had participated in conventional intervention prior to partaking in tele‐intervention, familiarity with the use of conventional intervention could have influenced and caused this disparity in preference for in‐person services. Thus, the potential for preference bias merely due to familiarity with in‐person services may have influenced our findings, and can partially explain why the majority of participants preferred accessing healthcare services in‐person rather than via telehealth/video.
Whilst most families still accessed allied health and medical services as often as they did prior to the pandemic with a slight majority of parents accessing audiology services less frequently, it is important to note that our survey did not explore the mode in which participants accessed services prior to the pandemic. This creates difficulties on being able to assess the impact of our participants' prior experience with telehealth services on the quality and apparent effectiveness of telehealth intervention reported by families in this study. Of note, a study by Claridge and Kroll (2021) that examined the perspectives of families of children with hearing devices on their use of telehealth services during the COVID‐19 pandemic demonstrated their confidence in delivering intervention via telehealth was associated with previous experience and use of telehealth services. The same study, however, documented that a significant number of respondents were still sceptical of the outcomes and the quality of early intervention services that were delivered by telehealth (Claridge & Kroll, 2021), showcasing yet again how parental preferences and familiarity with attending services in‐person (Havenga et al., 2015) could contribute and explain the reduced apparent quality of telehealth services that some of our participants reported.
Another important factor to consider is the nature of how service providers and families interact during telehealth sessions. Numerous studies have shown that parents need to play an active role in telehealth sessions for them to be effective, where parents are required to work with service providers as they coach them on how to best interact with their child to aid their development and learning (Behl et al., 2017; Pollard & Hogan, 2021). At the same time, given that therapists cannot play and interact in the same way as they would with the child during an in‐person session, therapists need to be appropriately trained and flexible in their approach when coaching the caregiver and when interacting with the child (Pollard & Hogan, 2021). Indeed, as some parents had reported, telehealth sessions often required more preparation and imposed a greater burden on parents to direct the sessions. Additionally, for a variety of reasons that stretched across both providers and families, younger children were more commonly reported to have faced difficulties in engaging with therapists via telehealth. Thus, these are some factors that could potentially complicate the delivery of effective telehealth services, and could partly explain the reduced quality of telehealth services that were reported by some participants, especially if participants had never previously accessed services via telehealth and were unfamiliar with what arrangements or conditions are needed to run sessions efficiently.
4.3. The challenges of telehealth
In our study, parents reported telehealth as a challenge for their children who have short attention spans and were more likely to lose interest compared to in‐person appointments. Distractions in the home environment have been previously cited as a possible barrier in the provision of telehealth services for children with hearing loss (Havenga et al., 2015). One study that surveyed parents of children with cochlear implants in the United Arab Emirates (U.A.E) reported similar findings, and attributed the difficulties children faced in adapting to remote learning to boredom and due to spending extended periods of time isolated at home (Ayas et al., 2020).
Technical difficulties including poor Internet connection speeds, problems with video and sound quality, and the lack of proper video‐conferencing equipment (such as iPads) also caused further complications for some families. These issues are known to generally complicate access to healthcare services for children who are DHH (Constantinescu, 2012; Havenga et al., 2015). This is an important consideration, especially for families in remote and regional settings, as some participants reported an impact on the quality and their ability to engage in telehealth sessions due to poor broadband connection speeds.
According to Barr et al. (2018), children who are DHH in remote and regional areas of Australia are known to have reduced access to healthcare and disability services compared to those in urban areas. Travel costs, the lack of specialised services, poor access to information and lower socioeconomic status are some factors known to contribute towards this disparity (Barr et al., 2018). Indeed, survey responders in regional settings reported difficulties in booking appointments and accessing local providers, with some having to travel longer distances to access healthcare services required for their children. Whilst it is difficult to ascertain to what degree these difficulties in access can be attributed to COVID‐19 alone, it is important to acknowledge the role that increased rurality has on access to healthcare services for children who are DHH.
Indeed, as mentioned previously, of the 497 survey responders, 96 (19.3%) were from regional areas. Of note, responders from regional areas also on average had lower SEIFA scores (mean 971.1, SD 47.8) when compared to responders from metropolitan areas (mean 1023.1, SD 64.8), putting them under the national average (mean 1000, SD 100) (ABS, 2016). The relationship between socioeconomic status (SES) and access to healthcare is complex for many reasons (Barr et al., 2018). Low SES has been linked to a greater degree of expenses, even with free therapy and services given the significant accommodation and travel costs that families in regional and remote of children with disabilities face (Barr et al., 2018). Furthermore, families of low SES appear to have less access to information regarding what services are available when compared to parents from higher SES, with a strong association shown between parental education and the risk of having a child with disabilities (Barr et al., 2018). Thus, given the differences in SEIFA scores of regional survey responders vs. metropolitan survey responders, the disparity in SES might partially contribute to the increased difficulties in access that were reported by some families in remote and regional settings.
Many families also reported longer waiting times during the pandemic, and commonly experienced deferrals for non‐urgent medical, surgical and cochlear mapping appointments. One study involving children with cochlear implants in the United Arab Emirates throughout the COVID‐19 pandemic revealed that timely access to cochlear mapping appointments was delayed for these children, with most parents lacking access to adequate follow‐up (Ayas et al., 2020). Another study conducted in Saudi Arabia by Telmesani et al. (2021) following paediatric cochlear implant patients during COVID‐19 similarly reported difficulties for patients in obtaining follow‐up cochlear programming appointments, with access to surgery, audiology and speech and language pathology delayed especially during lockdown periods. These findings highlight the worldwide impact of COVID‐19 on healthcare service delivery.
Furthermore, family‐centred early intervention (FCEI) has widely been accepted as best practice for children who are DHH (McCarthy et al., 2020), a practice that is centred on the belief that ‘the child's well‐being and care needs are best supported within the family context through effective collaboration with professionals and services’ (Mccarthy & Guerin, 2022). This approach appears to be more common with younger children (i.e. pre‐school‐aged children, aged 0–6 years), whereas older children (i.e. school‐aged children, age 6+ years) can benefit from a more professional‐centred approach (Maluleke et al., 2021). Indeed, whilst telehealth has been shown to be an acceptable alternative to in‐person services for the delivery of FCEI (McCarthy et al., 2020) especially when barriers to in‐person services exist, telehealth might not deliver the level or quality of care that certain families require. This also suggests that the use of telehealth to deliver FCEI still requires optimisation.
Interestingly, whilst a majority of participants (72% of pre‐school children, ~54% of school‐aged children) reported that the quality of allied health services delivered via telehealth was worse when compared to in‐person, in most cases (~70% of pre‐school children, ~82% of school‐aged children) parents reported that telehealth services were still meeting their needs at least moderately. This suggests that despite the preference that many families had for in‐person services, many families can acknowledge the value that telehealth had in the provision of services that are necessary for their child's well‐being and needs. Additionally, the differences in quality of allied health services delivered via telehealth reported by parents of pre‐school and school‐aged children can reflect the different needs that children of different age groups might require, and what is developmentally appropriate for each age group.
For context, family‐centred practices include caregiver ‘coaching, the use of everyday routines and emphasising collaborative practices’, whereas practitioner‐led intervention strategies focus more on the professional ‘teaching the child directly, using practitioner‐provided materials and the reliance on practitioner‐determined activities’ (McCarthy et al., 2020). For an older child who might have the capacity to engage with the therapist for the duration of the session, telehealth might be an entirely suitable mode of service access. The same cannot necessarily be true for a younger child, especially when considering the well‐known associations between hearing loss and other disorders associated with cognitive delay including Down's syndrome, autism spectrum disorder, global developmental delay and cerebral palsy (Trudeau et al., 2021). Further research into how these two different approaches and how they can be best delivered for children who are DHH of different age groups via telehealth is needed. An emphasis should be made on exploring the perspectives of both families and health professionals, and what challenges or issues need to be addressed to optimise access via telehealth, especially if in‐person services are unavailable.
Additionally, another important factor that can influence the effectiveness and quality of telehealth sessions is the provider's skills, knowledge and training. There is limited evidence on what training and education healthcare providers might require to successfully engage in telehealth services catered for children who are DHH as indicated by McCarthy et al. (2018). A more recent study by Jiménez‐Rodríguez et al. (2020) that examined the perspectives of healthcare professionals throughout the COVID‐19 pandemic on the use telehealth services reported that further training was necessary in multiple domains including technological and other non‐technical or social–emotional skills (including communication, empathy and learning how to respond to verbal and nonverbal cues). These skills are arguably just as important for healthcare professionals who interact with children who are DHH. Further research that specifically examines the perspectives of healthcare providers on engaging telepractice with children who are DHH would provide invaluable insight into how telehealth services can be optimised for both healthcare providers and families of children who are DHH.
4.4. The value of telehealth
Despite the difficulties reported above, the value of telehealth in providing access for families of children who are DHH during the COVID‐19 pandemic cannot be understated. Families were able to access telehealth services safely and remotely, with some reporting receiving great guidance from healthcare providers during their transition to telehealth and great satisfaction with the quality of care their children had received through telehealth. In fact, a high proportion of parents reported telehealth made no change in the ease of accessing services for their children during the pandemic. Interestingly, whilst parents reported that they found telehealth services quite easy to access, the same could not be said for their children, especially pre‐school‐aged children. These parents in particular reported that their children did not find audiology and allied health services easy to access. Thus, whilst age considerations may be important to ensure telehealth consultations are effective, it is equally important for service providers to be trained appropriately and flexible in their approach, especially with younger children.
Telehealth has also previously been shown to be the more convenient and efficient option as it allowed parents more flexibility when booking appointments but also cut travel times and costs associated with attending services in‐person (Govil et al., 2020). This was seen as highly desirable by some participants in our study, and a compelling reason for many to continue accessing healthcare services via telehealth, especially for those juggling multiple responsibilities.
Studies have also shown that telehealth is playing an increasingly important role for families of children who are DHH, with promising applications in paediatric hearing healthcare. For instance, infants who failed their newborn hearing screens were successfully evaluated, diagnosed and followed up purely via telehealth services in one study (Bush et al., 2017). Another study following children who are DHH who had already undergone hearing‐aid fitting indicated that telehealth provided a great platform for parents to troubleshoot devices, and ensured that parents and their children had timely access to the support and services that they required (Hoi et al., 2021).
Furthermore, whilst some families in this study questioned the feasibility of telehealth for physical examinations, some studies have reported that physical examinations were possible and potentially even more efficient for children over telehealth (Hoi et al., 2021). Parents could be remotely instructed on the best techniques, physical manoeuvres and accessories available at home (such as spoons as tongue depressors or phone flashlights) to aid them whilst examining their children (Hoi et al., 2021). Additionally, a study conducted in the United States in April 2020 found that school‐aged children were usually more relaxed in a home environment than in the clinical setting, making telehealth more efficient as children were much more likely to follow instructions set out by therapists (Govil et al., 2020). Whilst these findings were not necessarily relevant to our participants, they are important to consider especially given the increasing role that telehealth is likely to play during and even after the COVID‐19 pandemic.
4.5. Implications for future clinicians and policymakers
Thus, our findings described both the challenges and facilitators of health service access during the pandemic, with a particular focus on the role of telehealth in providing access to healthcare for children who are DHH and their families. Whilst telehealth allowed families to remotely access services throughout COVID‐19 and was frequently reported as more convenient, many improvements are still needed for optimal outcomes and access. Improvements in the delivery of telehealth services, including ensuring access to high quality Internet connections, video‐conferencing equipment, increasing the number of providers available to patients and the provision of proper training in the use of telehealth services for providers are some ways in which this can be achieved. Furthermore, whilst this study was focused on the perspectives of parents and children who are DHH, exploring the perspectives of clinicians who engaged in telehealth during COVID‐19 and what best worked for them could certainly yield findings that could inform future clinicians and service providers on how to best deliver telehealth services for children who are DHH.
4.6. Strengths and weaknesses
Our study had numerous strengths. The mixed methods approach of our study provided a rich and diverse array of perspectives on the experiences of a large cohort of families of 336 children who are DHH during the early stages of the COVID‐19 pandemic. Qualitative data were double coded to ensure inter‐rater reliability and rigour throughout the coding process. Importantly, this is one of the first qualitative studies conducted to explore the impact of COVID‐19 on access to healthcare services for children who are DHH. The insight gained on the experiences of children who are DHH and their families during COVID‐19 can help inform clinicians and healthcare providers on how to optimise care and access for this population of children in the future.
There were several limitations to this study. Not all families (68%) who filled in the survey provided qualitative data for analysis. Hence, there is potential for data to be skewed towards participants with particularly strong views or those who had negative experiences, especially when the option to comment in a non‐compulsory open text box is provided. Furthermore, whilst a comparison of responders to non‐responders (Table 1) indicated that there were no major differences in the demographics, it is important to consider the generalisability of the results. Whilst recruitment into VicCHILD is facilitated by the state's screening program and clinical services, only 53.6% of children with hearing loss in Victoria have been recruited into the databank. In addition, participants were more likely to be from higher socioeconomic status (SES), indicated by differences in their SEIFA disadvantage scores (Sung et al., 2019). Thus, our findings might not necessarily be applicable to families from lower SES.
Furthermore, there are many factors that complicate the distinctions between preference and quality for in‐person vs telehealth services. Whilst our survey was designed to explore these elements separately, as evidenced by Figures 2, 3 and Table S2, the nature of the survey limited the ability of responders to provide reasons for why they preferred or rated certain modes of service access as higher quality over others. However, systematic qualitative analysis of the open‐ended question has revealed key areas and themes that will guide future researchers in what is needed to optimise healthcare access for children who are DHH and their families, especially for telehealth services.
5. CONCLUSION
The COVID‐19 pandemic significantly impacted the way children who are DHH and their families accessed hearing health services. With the availability of telehealth, most families continued to access services during the COVID‐19 pandemic. Allied health services were more readily accessed via telehealth, whereas medical and audiology services often carried a need for an in‐person assessment. Whilst many families have identified challenges with using telehealth, telehealth has become increasingly important and will likely remain so even after the COVID‐19 pandemic has ended. As indicated by one participant, a hybrid model of telehealth and in‐person care will likely remain in use, given the convenience of telehealth:
Telehealth has worked well, it used to take about 3 1/2 hrs out of a day to attend the services in person (leave work, pick up from school, drive to service, undertake speech session, drive home), a lot more convenient, will likely look at a combination of face‐to‐face and telehealth once COVID restrictions ease.
Many families found telehealth appointments to be of worse quality than in‐person services. Improved Internet connection speeds, access to video‐conferencing equipment, addressing video and sound quality, creating engaging software to support the needs of children who are DHH and the provision of appropriate training and support to providers are ways in which the level and quality of care provided can be optimised. Future research is required to address how telehealth services can be optimised for families of children who are DHH, especially when in‐person services are unavailable. Exploring the experiences of clinicians who engaged in telehealth services alongside children who are DHH during COVID‐19 could yield valuable insights into what worked best, the common pitfalls of telehealth and how to increase virtual engagement with children. This information can be used to provide appropriate upskilling to all clinicians who deliver telehealth services to children and their families as we move forward with a new virtual way of accessing health services.
AUTHOR CONTRIBUTIONS
Ahmed Ibrahim Mardinli: Conceptualization; formal analysis; methodology; software; visualization; writing – original draft; writing – review and editing. Rona Weerasuriya: Conceptualization; formal analysis; methodology; supervision; validation; writing – review and editing. Alanna Gillespie: Data curation; formal analysis; investigation; visualization; writing – original draft; writing – review and editing. Libby Smith: Conceptualization; data curation; funding acquisition; investigation; methodology; project administration; software; supervision; writing – review and editing. Valerie Sung: Conceptualization; funding acquisition; methodology; project administration; supervision; visualization; writing – original draft; writing – review and editing.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Table S1 –S2
ACKNOWLEDGEMENTS
VicCHILD is funded by a Royal Children's Hospital Foundation Grant 2018 and the Murdoch Children's Research Institute (MCRI). The data collection for this study was supported by the Melbourne Children's Campus Lifecourse initiative for research into the impacts of COVID‐19 on children, funded by the Department of Health and Human Services, the Victor Chiodo Foundation and Morgan Stanley. V.S. is supported by a Melbourne Children's Campus Clinician‐Scientist Fellowship. Research at the Murdoch Children's Research Institute is supported by the Victorian Government's Operational Infrastructure Support Program. The authors thank families participating in VicCHILD as well as the VicCHILD research team members who assisted in collecting the data. Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
Biographies
Mr Ahmed Mardinli is a final year medical student at the University of Melbourne. He has a special interest in paediatric research and clinical practice.
Dr Rona Weerasuriya is a Senior Researcher at The Centre for Social Impact at the University of New South Wales and an Honorary Fellow at the Murdoch Children's Research Institute. She has methodological expertise and particular interest in phenomenological and participatory co‐design research approaches, healthcare services re‐design and social impact assessment.
Ms. Alanna Gillespie is a final year PhD student and research assistant at the Murdoch Children's Research Institute. Her current research focuses on improving outcomes for deaf and hard of hearing children and their families. She has a particular interest in early life disease prevention.
Ms. Libby Smith is a research assistant at the Murdoch Children's Research Institute. Her current research focuses on improving outcomes for deaf and hard of hearing children and their families. She has a particular interest in childhood speech and language development.
A/Prof Valerie Sung is a paediatrician at the Royal Children's Hospital, Clinician Scientist Fellow at the Murdoch Children's Research Institute, and Honorary Clinical Associate Professor at the University of Melbourne. She leads a research programme on childhood hearing loss integrating state‐wide hearing screening, clinical service and genomics application with population‐based research, clinical trials and implementation science.
Mardinli, A. , Weerasuriya, R. , Gillespie, A. , Smith, L. & Sung, V. (2022) Accessing hearing‐health services for deaf and hard‐of‐hearing children during the COVID‐19 pandemic: Parent and child perspectives. Australian Journal of Social Issues, 00, 1–27. Available from: 10.1002/ajs4.231
REFERENCES
- Australian Bureau of Statistics (ABS), A. B. O. S . (2016) 2033.0.55.001 – census of population and housing: socio‐economic indexes for areas (SEIFA), Australia, 2016. Australia: Australian Bureau of Statistics. [Google Scholar]
- Ayas, M. , Ali Al Amadi, A.M.H. , Khaled, D. & Alwaa, A.M. (2020) Impact of COVID‐19 on the access to hearing health care services for children with cochlear implants: a survey of parents. F1000Research, 9, 690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr, M. , Duncan, J. & Dally, K. (2018) A systematic review of services to DHH children in rural and remote regions. The Journal of Deaf Studies and Deaf Education, 23, 118–130. [DOI] [PubMed] [Google Scholar]
- Behl, D.D. , Blaiser, K. , Cook, G. , Barrett, T. , Callow‐Heusser, C. , Brooks, B.M. et al. (2017) A multisite study evaluating the benefits of early intervention via Telepractice. Infants & Young Children, 30(2), 147–161. [Google Scholar]
- Boss, E.F. , Niparko, J.K. , Gaskin, D.J. & Levinson, K.L. (2011) Socioeconomic disparities for hearing‐impaired children in the United States. The Laryngoscope, 121, 860–866. [DOI] [PubMed] [Google Scholar]
- Bush, M.L. , Kaufman, M.R. & Mcnulty, B.N. (2017) Disparities in access to pediatric hearing health care. Current Opinion in Otolaryngology & Head and Neck Surgery, 25, 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching, T.Y.C. , Dillon, H. , Button, L. , Seeto, M. , Van Buynder, P. , Marnane, V. et al. (2017) Age at intervention for permanent hearing loss and 5‐year language outcomes. Pediatrics, 140, e20164274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claridge, R. & Kroll, N. (2021) Aural rehabilitation via Telepractice during COVID‐19: a global perspective on evolving early intervention practices. International journal of telerehabilitation, 13, e6362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantinescu, G. (2012) Satisfaction with telemedicine for teaching listening and spoken language to children with hearing loss. Journal of Telemedicine and Telecare, 18, 267–272. [DOI] [PubMed] [Google Scholar]
- Decuir‐Gunby, J.T. , Marshall, P.L. & Mcculloch, A.W. (2011) Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods, 23, 136–155. [Google Scholar]
- Fereday, J. & Muir‐Cochrane, E. (2006) Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods, 5, 80–92. [Google Scholar]
- Fisk, M. , Livingstone, A. & Pit, S.W. (2020) Telehealth in the context of COVID‐19: changing perspectives in Australia, the United Kingdom, and the United States. Journal of Medical Internet Research, 22, e19264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govil, N. , Raol, N. , Tey, C.S. , Goudy, S.L. & Alfonso, K.P. (2020) Rapid telemedicine implementation in the context of the COVID‐19 pandemic in an academic pediatric otolaryngology practice. International Journal of Pediatric Otorhinolaryngology, 139, 110447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havenga, E. , Swanepoel, D.W. , Le Roux, T. & Schmid, B. (2015) Tele‐intervention for children with hearing loss: a comparative pilot study. Journal of Telemedicine and Telecare, 23, 116–125. [DOI] [PubMed] [Google Scholar]
- Hoi, K.K. , Curtis, S.H. , Driver, L. , Wisnosky, E. , Zopf, D.A. & Bohm, L.A. (2021) Adoption of telemedicine for multidisciplinary Care in Pediatric Otolaryngology. The Annals of Otology, Rhinology, and Laryngology, 130, 1105–1111. [DOI] [PubMed] [Google Scholar]
- Jiménez‐Rodríguez, D. , Santillán García, A. , Montoro Robles, J. , Rodríguez Salvador, M.D.M. , Muñoz Ronda, F.J. & Arrogante, O. (2020) Increase in video consultations during the COVID‐19 pandemic: Healthcare Professionals' perceptions about their implementation and adequate management. International Journal of Environmental Research and Public Health, 17, 5112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maluleke, N.P. , Khoza‐Shangase, K. & Kanji, A. (2021) An integrative review of current practice models and/or process of family‐centered early intervention for children who are deaf or hard of hearing. Family & Community Health, 44, 59–71. [DOI] [PubMed] [Google Scholar]
- Matua, G.A. & Van Der Wal, D.M. (2015) Differentiating between descriptive and interpretive phenomenological research approaches. Nurse Researcher, 22, 22–27. [DOI] [PubMed] [Google Scholar]
- Mccarthy, E. & Guerin, S. (2022) Family‐centred care in early intervention: a systematic review of the processes and outcomes of family‐centred care and impacting factors. Child: Care, Health and Development, 48, 1–32. [DOI] [PubMed] [Google Scholar]
- Mccarthy, M. , Leigh, G. & Arthur‐Kelly, M. (2018) Telepractice delivery of family‐centred early intervention for children who are deaf or hard of hearing: a scoping review. Journal of Telemedicine and Telecare, 25, 249–260. [DOI] [PubMed] [Google Scholar]
- Mccarthy, M. , Leigh, G. & Arthur‐Kelly, M. (2020) Practitioners' self‐assessment of family‐centered practice in Telepractice versus in‐person early intervention. The Journal of Deaf Studies and Deaf Education, 26, 46–57. [DOI] [PubMed] [Google Scholar]
- Monaghesh, E. & Hajizadeh, A. (2020) The role of telehealth during COVID‐19 outbreak: a systematic review based on current evidence. BMC Public Health, 20, 1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Núñez, A. , Sreeganga, S.D. & Ramaprasad, A. (2021) Access to healthcare during COVID‐19. International Journal of Environmental Research and Public Health, 18, 2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne, L. , Flannery, H. , Kambakara Gedara, C. , Daniilidi, X. , Hitchcock, M. , Lambert, D. et al. (2020) Business as usual? Psychological support at a distance. Clinical Child Psychology and Psychiatry, 25, 672–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard, R. & Hogan, S. (2021) Parental and practitioner views of Telepractice for pediatric auditory verbal habilitation at a time of global pandemic. Perspectives of the ASHA Special Interest Groups, 6, 1832–1856. [Google Scholar]
- Roland, L. , Fischer, C. , Tran, K. , Rachakonda, T. , Kallogjeri, D. & Lieu, J.E.C. (2016) Quality of life in children with hearing impairment: systematic review and meta‐analysis. Otolaryngology–Head and Neck Surgery, 155, 208–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sezgin, E. , Huang, Y. , Lin, D. , Ramtekkar, U. , Pauline, L. & Lin, S. (2021) Documented reasons of cancellation and rescheduling of telehealth appointments during the pandemic. Telemedicine Journal and E‐Health, 27, 1143–1150. [DOI] [PubMed] [Google Scholar]
- Solomon, G.M. , Bailey, J. , Lawlor, J. , Scalia, P. , Sawicki, G.S. , Dowd, C. et al. (2021) Patient and family experience of telehealth care delivery as part of the CF chronic care model early in the COVID‐19 pandemic. Journal of Cystic Fibrosis, 20(Suppl 3), 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung, V. , Smith, L. , Poulakis, Z. , Burt, R.A. , Carew, P. , Tobin, S. & Wake, M. (2019) Data resource profile: The victorian childhood hearing impairment longitudinal databank (VicCHILD). International Journal of Epidemiology, 48(5), 1409–1410h. [DOI] [PubMed] [Google Scholar]
- Taylor, A. , Caffery, L.J. , Gesesew, H.A. , King, A. , Bassal, A.‐R. , Ford, K. et al. (2021) How Australian health care services adapted to telehealth during the COVID‐19 pandemic: a survey of telehealth professionals. Frontiers in Public Health, 9. 10.3389/fpubh.2021.648009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telmesani, L.M. , Said, N.M. , Mahrous, M.M. & Alrusayyis, D.F. (2021) The difficulties encountered by pediatric Cochlear implant patients and their parents during the COVID‐19 pandemic. Audiology & Neuro‐Otology, 27, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau, S. , Anne, S. , Otteson, T. , Hopkins, B. , Georgopoulos, R. & Wentland, C. (2021) Diagnosis and patterns of hearing loss in children with severe developmental delay. American Journal of Otolaryngology, 42, 102923. [DOI] [PubMed] [Google Scholar]
- Zischke, C. , Simas, V. , Hing, W. , Milne, N. , Spittle, A. & Pope, R. (2021) The utility of physiotherapy assessments delivered by telehealth: a systematic review. Journal of Global Health, 11, 4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 –S2


