Abstract
There is a deep interrelation between the thyroid gland and the kidney parenchyma, with dysfunction of the first leading to significant changes in renal metabolism and vice versa. Given the recognition of cancer as a systemic disease, the raise of thyroid tumors and the common association of several malignancies, such as breast cancer, prostate cancer, colorectal cancer, and other, with an increased risk of kidney disease, public health alert for these conditions is warranted. A systematic review of the current evidence on the bidirectional relationship between thyroid and renal cancers was conducted including 18 studies, highlighting patient’s characteristics, histology, time for secondary malignancy to develop from the first diagnosis, treatment, and follow-up. A total of 776 patients were identified; median age was 64 years (range: 7–76 years). Obesity and family history were identified as the most common risk factors, and genetic susceptibility was suggested with a potential strong association with Cowden syndrome. Controversy on chemo and radiotherapy effects was found, as not all patients were previously exposed to these treatments. Men were more likely to develop kidney cancer after a primary thyroid malignancy, with 423/776 (54%) experiencing renal disease secondarily. Median time after the first malignancy was 5.2 years (range: 0–20 years). With the advancement of current oncological therapy, the prognosis for thyroid cancer patients has improved, although there has been a corresponding rise in the incidence of multiple secondary malignancy within the same population, particularly concerning the kidney. Surgery can achieve disease-free survival, if surveillance follow-up allows for an early localized form, where radical treatment is recommended.
Keywords: thyroid cancer, renal cancer, multiple cancer, cancer surveillance and screening, cancer risk
Introduction
Thyroid cancer (TC) is one of the most rapidly increasing malignancies in Western countries, with an annual incidence rate of 5.4% in men and 6.5% in women (1). Much of this rise is largely due to early detection using more sensitive diagnostic procedures, including Artificial Intelligence, performed for other medical reasons and able to identify incidental small thyroid nodules, otherwise missed (2–4). Certain risk factors for TC are female sex, family history of TC, radiation exposure, lymphocytic thyroiditis, and reduced iodine intake (5, 6). On the basis of the histological and the clinical behavior, TCs are divided into well differentiated and poorly differentiated; well-differentiated TCs include the papillary and follicular histotypes (7). Surgery, either lobectomy or total thyroidectomy, represents the standard therapeutic approach for well-differentiated TC; radioactive iodine therapy is recommended for high-risk patients (5). Ablation and active surveillance are of increasing importance in patients who refuse surgery or are unfit for.
Improvements in the detection of TC and therapeutic strategies have likewise resulted in a more favorable course for this disease. Because the mortality rates for TC remained stable at around 0.5 deaths per 100,000, the number of patients surviving is on the rise (8, 9).
On the other hand, renal cancer, or renal cell carcinoma (RCC), is the 9th common cancer in men and the 14th one in women. RCC frequently presents incidentally; in fact, it is asymptomatic in most cases. Therefore, the diagnosis of patients with localized renal cancer, which is potentially treatable only with surgery or ablation, is almost always accidental (10). Identified risk factors include male sex, smoking tobacco, obesity, and hypertension (10, 11). RCC comprises an heterogeneous group of histological subtypes: Clear cell renal cell carcinoma (ccRCC), papillary, and chromophobe are the most common solid RCC (11). Nephron-sparing surgery or partial nephrectomy has evolved as the standard of care in patients with localized RCC; ablation and active surveillance are traditionally alternatives for patients who are unfit for surgery (11).
Thyroid interrelation with the kidney is well known (12); on the one hand, this gland is necessary for renal cells growth and for the maintenance of hydro-electrolyte homeostasis; on the other hand, the kidney eliminates thyroid hormones and regulates their serum level. There is therefore a deep interrelation among the two organs, with thyroid dysfunction causing significant changes to renal metabolism and vice versa ( 13).
Cancer is a systemic disease, and many common cancers, such as breast cancer, prostate cancer, colorectal cancer, and other, are associated with an increased risk of kidney cancer development, especially within the first 5 years after their diagnosis (14). Because the risk of second cancers after the diagnosis of primary TC is elevated (15), too, the aim of this manuscript is to review the current state of knowledge on the interrelationship between thyroid and renal cancers.
Methods
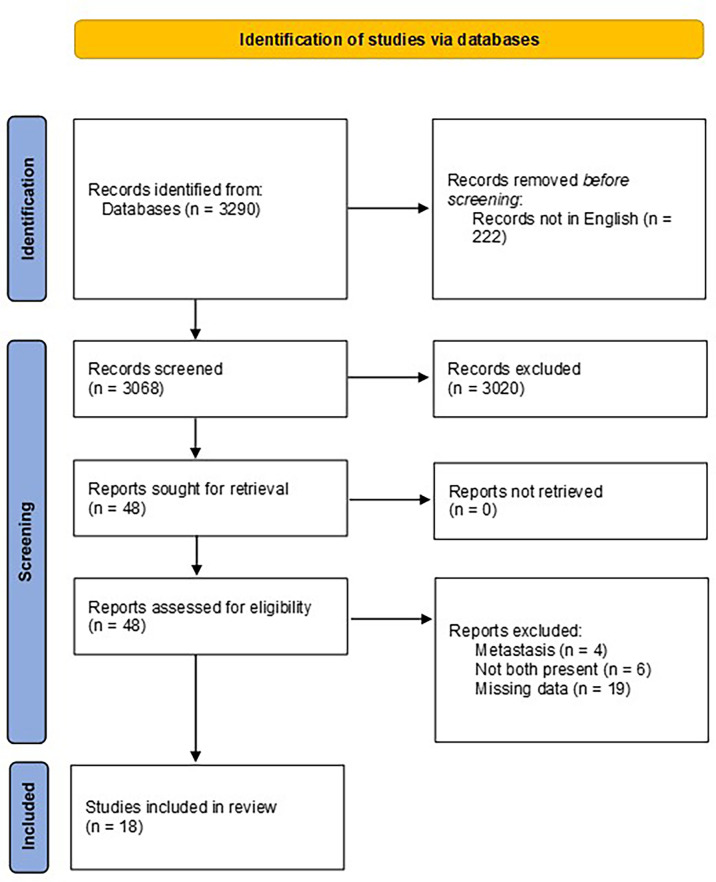
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA) (16). The search was run in February 2022 across PubMed, Web of Science, and Scopus databases and was restricted to articles written in English only. References were cross-checked for additional relevant studies. The retrieved lists were exported to a reference manager (EndNote™) to eliminate duplicates, as shown in Figure 1 .
Figure 1.
PRISMA diagram.
Keywords “thyroid cancer” and “renal cancer” were used to include studies evaluating TC characteristics in patients previously affected by kidney cancer or kidney cancer characteristics in patients previously affected by TC. Reports of metastases were excluded from the analysis.
The research was performed by two independent investigators; subsequently, the results were compared and combined; in case of disagreement on the value of the selected papers, an additional comparison was crucial in the decision-making process. Only published literature was included, and no date limits have been set. Only English language articles were included; reviews, editorials, and repeated or redundant manuscripts were excluded. Only registry analyses and retrospective studies, mostly case reports, were found and included in the present review.
Data extraction was performed thereafter, including the details of title, authors, date of publication, country, research design, patients’ characteristics, and outcomes.
A risk of bias assessment was performed using the Newcastle–Ottawa Scale quality assessment star system ( Table 1 ), in which a paper is judged on the selection of the study groups, the comparability of the groups, and the ascertainment of either the exposure or the outcome of interest for case control or cohort studies, respectively (24).
Table 1.
Newcastle–Ottawa Scale (NOS) quality assessment star system.
| NOS17 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| COHORT STUDY | ||||||||||
| Article | Selection | Comparability | Outcomes | Total | ||||||
| Selection of nonexposed cohort | Representativeness of exposed cohort | Ascertainment of exposure | Outcome not present at the start of the study | Assessment of outcomes | Length of follow-up | Adequacy of follow-up | ||||
| Canchola et al. (17) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9/9 | |
| CASE CONTROL | ||||||||||
| Article | Selection | Comparability | Outcomes | Total | ||||||
| Case Definition | Representativeness of the Cases | Selection of Controls | Definition of Controls | Ascertainment of Exposure | Non-Response Rate |
Same methods of
Ascertainment for cases and control |
||||
| Abdel-Rahman, et al. (14) | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8/9 | |
| Antonelli, et al. (18) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9/9 | |
| Carhill et al. (19) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9/9 | |
| Murray, et al. (20) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9/9 | |
| Murray S, et al. (21) | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8/9 | |
| Ngeow, et al. (22) | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ | 9/9 | |
| Van Fossen, et al. (23) | ☆ | – | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7/9 | |
The stars mean the grading according to the Newcastle-Ottawa scale.
Results
A total of 3,290 manuscripts were retrieved from the search; following exclusion based on title and abstract screening (n = 3,020) and after full text read (n = 48), the remaining studies included in the review were 18 ( Table 2 ). The majority (11/18) were case reports. A total of 776/64,187 patients were identified.
Table 2.
Results.
| Article | Year | Type of study | Case | Sex | Age | Histology | Genetic syndrome | Risk factors | Thyroid cancer | Interval to second cancer | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Abdel-Rahman (14) | 2017, Egypt |
Case control | 341/9861 | N/A | N/A | N/A | N/A | Treatment factors (radiation) Common etiology factors (smoking) Rare hereditary cancer syndromes |
Primary | 5 years | Beyond 5 years, patients with primary thyroid cancer have an enhanced risk to develop a second primary kidney cancer. This link may be an expression of a particular genetic makeup determining patients’ susceptibility to both cancers. |
| Albores-Saavedra, et al. (25) | 2014, Mexico |
Case report | 2/2 | F | 72 54 |
Papillary urothelial carcinoma and PTC | N/A | No specific risk factors were identified. | Second Second |
14 years 1,5 years |
These malignant neoplasms do not apparently share similar risk factors. |
| Antonelli, et al. (18) | 2012, Italy | Case control | 15/285 | N/A | N/A | N/A | N/A | No specific risk factors were identified. | Second | N/A | The risk of development of a second neoplasia in patients with RCC increases with aging. |
| Canchola et al. (17) | 2005, USA |
Cohort study | 16/10932 | F | 55 | PTC and RCC not otherwise specified | N/A | Obesity increases the risk of both thyroid and kidney cancer | Primary | 3 years | Increased surveillance is warranted for kidney cancer among women with thyroid cancer. |
| Carhill et al. (19) | 2014, USA | Case control | 117/23514 | N/A | N/A | Papillary thyroid carcinoma (85%) and ccRCC (79%) | N/A | Genetic susceptibility, implication of clinical therapy | N/A | 6 years | The association between thyroid and kidney cancer needs further investigation. |
| Oh, et al. (26) | 2015, Korea |
Case report | 1/1 | M | 50 | ccRCC and PTC | N/A | Family history of thyroid cancer | Synchronous | 0 | No specific risk factor or genetic syndrome were identified. |
| Atta, et al. (27) | 2016, Egypt |
Case report | 1/1 | F | 76 | ccRCC and PTC | No mutations were detected | Family history of colon, lung, kidney and thyroid cancer. | Primary | 14 years | No genetic mutation was detected, despite the family history. |
| Kim, et al. (15) | 2020, Canada |
Case report | 1/2 | M | 22 | Chromophobe RCC and PTC | Cowden syndrome (CS) | Family history of kidney and thyroid cancer. | Primary | 12 years | Thyroid neoplasia and RCC are minor diagnostic criteria for CS. |
| Klain, et al. (28) | 2021, Italy |
Case report | 1/2 | M | 64 | ccRCC and PTC (tall-cell variant) |
N/A | No specific risk factors were identified | Second | 20 years | No specific risk factor or genetic syndrome were identified. |
| Ma, et al. (29) | 2014, China |
Case report | 1/1 | F | 35 | ccRCC+ SFT and PTC + follicular thyroid carcinoma | N/A | Negative family history of neoplasia | Synchronous | 0 | No specific risk factor or genetic syndrome were identified. |
| Malchoff et al. (30) | 1999, USA | Family report | 31/31 | N/A | N/A | Papillary renal carcinoma and PTC | Mutation of a gene that maps to 1q21 | No specific risk factors, except for genetics, were identified | N/A | N/A | Familial association of PTC with papillary renal neoplasia defines a distinct familial tumor syndrome. |
| Murray, et al. (20) | 2016, USA |
Case control | 12/3066 | 6 F 6 M |
53 64 |
PTC and RCC not otherwise specified | N/A | No specific risk factors were identified | Second | N/A 7 years |
The rate of thyroid cancer in both women and men surgically treated for RCC was significantly higher. Observed association is unlikely due to treatments effects because primary treatment in renal cancer is surgical. |
| Murray S, et al. (21) | 2013, USA |
Case control | 3/433 | N/A | N/A | N/A | N/A | Older and radiation exposure | Synchronous | 0 | Papillary thyroid cancer is the most frequent histologic type associated to RCC. |
| Ngeow, et al. (22) | 2014, USA |
Case control | 2/114 | M F |
7 36 |
N/A | PHTS | PTEN mutation | Primary | 14 8 |
A bidirectional association between thyroid and renal cancers suggests shared genetic and environmental risk factors. |
| Peng, et al. (31) | 2019, China |
Case report | 1/1 | M | 58 | ccRCC and micro-papillary thyroid carcinoma | N/A | No specific risk factors were identified | Primary | 1 years | Integrin ανβ6 is positively expressed in multiple primary cancer, also in patients with RCC and thyroid cancer. |
| Samarasinghe, et al. (32) | 2020, USA |
Case report | 1/1 | F | 56 | ccRCC and PTC + medullary thyroid cancer | RET mutational analysis was negative | Family history of breast cancer and RCC | Primary | 2 years | RET mutational analysis was negative. |
| Song, et al. (33) | 2017, Canada |
Case report | 1/1 | M | 72 | ccRCC and PTC | N/A | N/A | Synchronous | 0 | Tumour-to-tumour metastasis of a thyroid cancer into a primary renal neoplasm is extremely rare and maybe resulting from rich vascularity and perfusion to enable successful delivery and deposition of metastatic tumour cells. |
| Van Fossen, et al. (23) | 2013, USA |
Case control | 230/15940 | 90 M 60 F |
N/A | N/A | N/A | N/A | 60 primary 80 second |
N/A | This study demonstrated a bidirectional association between thyroid and renal cancers. This association is more likely explained by shared genetic and environmental factors. |
ccRCC, clear cell renal cell carcinoma; PTC, papillary thyroid carcinoma; N/A, not available; F, female; M, male.
Patients’ characteristics
Median age was 64 years (range: 7–76 years). The association of thyroid and renal malignancies was more often observed in the male population. After evaluating the time between the two malignancies for all the studies included in the review, in no case, a significant difference was detected: The median interval between first and second cancer was 5.2 years (range: 0–20 years).
Most patients presented a TC as first primary malignancy (423 out of 776; 54%), and 110 patients (14%) developed a TC as second primary malignancy; a renal tumor was synchronous in only six patients out of 776 (0.78%).
Histopathological characteristics
With regards to histology, the papillary phenotype of TC was found in all patients. Sporadic cases of follicular carcinoma (29) and medullary (32) thyroid carcinoma have also been identified; however, both of them were also associated with a papillary thyroid carcinoma. On the contrary, with regards to renal carcinoma, a greater variety was observed concerning histology. In the series evaluated, the most represented type was ccRCC; however, sporadic cases of other renal malignancy cases were also reported, namely, urothelial (25), chromophobic (34), and papillary renal carcinoma (30).
Sex
With regard to TC, female sex was universally identified as a risk factor (17, 20); on the contrary, male sex is associated to the development of RCC (17). From the report by Van Fossen et al. (23), female TC patients had a twofold increase in the prevalence of a subsequent renal cell cancer (23), and female renal cell cancer patients had a 1.5-fold increase in the prevalence of TC; male patients with TC had 4.5-fold prevalence increase of subsequent RCC, and male patients with RCC had an increased threefold prevalence of subsequent TC. Male sex emerged as a risk factor of association between thyroid and kidney cancers (18).
Common identified risk factors
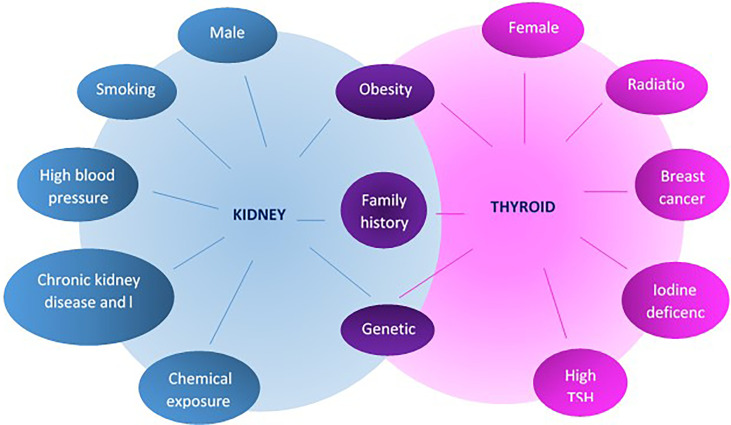
Identified common risk factors between thyroid and kidney cancers are few (19, 25), with obesity remaining a unique denominator to develop malignancy in general and in particular for these two; see Figure 2 . Family history (29) of both cancers is also well recognized, and as previously mentioned, male sex as well as aging increased the risk to develop both cancers and, in particular, RCC (18).
Figure 2.
Risk factors for the development of thyroid and kidney cancer.
Although radiation exposure is a known risk factor for the development of neoplasms and, in particular, for TC, no correlation between radiotherapy and the development of both TC and renal cancer was identified in any of the studies included in the review. Murray et al. (21) observed, in fact, that only 35% of patients with TC and an additional primary cancer, whether it is RCC or not, reported radiation exposure in their medical history. Given the recognized increased risk of TC following other primary malignancies, particularly RCC, it seems unlikely that the increased incidence could be due to the carcinogenic effect of radiations (14).
Although many chemotherapeutic agents are known to be carcinogenic, the patients have not undergone chemotherapy, and it is therefore not possible to evaluate the carcinogenic effects of these drugs.
Genetic syndrome
TC is associated with a heterogeneous pattern of genetic mutations involving the mitogen-activated protein kinase (MAPK) pathway (6). The main genetic mutations are represented by the oncogenes RAS and BRAF; in particular, BRAFV660E is present in about half of the PTCs (35).
Excluding the familial forms of medullary thyroid carcinoma, such as familial medullary thyroid carcinomas and multiple endocrine neoplasia (MEN), the familial forms of thyroid carcinoma are numerous and can be divided into syndromes with a prevalence of non-thyroid neoplasms and syndromes with a prevalence of TC. The first group includes also familial adenomatous polyposis, Cowden syndrome (CS), Werner syndrome, Carney complex, and Pendred syndrome; the second group includes pure familial papillary thyroid carcinoma with or without oxyphilia and familial papillary thyroid carcinoma with papillary RCC or with multinodular goiter (36).
There are also numerous genetic alterations involved in the development of RCC, in particular, the most important mutations involving the tumor-suppressor Von Hippel-Lindau (VHL), observed in about 80% of ccRCC (9). Hereditary forms of RCC include von Hippel-Lindau syndrome, hereditary papillary RCC, Birt-Hogg-Dubé syndrome, hereditary leiomyomatosis, and tuberous sclerosis (11).
The link between thyroid and kidney cancer may be an expression of genetic makeup that increases patients’ susceptibility to both malignancies (26, 27). Although this condition seems the most likely to occur, few studies have identified genetic syndromes or specific mutations, which are associated with the increased susceptibility to these two tumors, highlighting a familiar link (23, 32).
In the present review, CS (15, 22) was confirmed a risk factor leading to thyroid and renal cancers. CS is part of the Phosphatase and tensin homolog (PTEN)-hamartoma tumor syndrome, a disorder caused by a germline mutation of PTEN, a tumor suppressor gene. This syndrome is associated with the development of a variety of tumors, both benign and malignant (11): Thyroid carcinoma is one of major diagnostic criteria for CS, whereas RCC is part of the minor criteria.
PTEN mutation, even in the absence of the CS, was identified as risk factor (22), with Integrin ανβ6 positively expressed in multiple primary cancer, among which TC and RCC (31). The genetic mutation 1q21 (30) was identified in forms where PTC was associated to papillary renal neoplasia tumors, highlighting in this way a peculiar familial tumor syndrome ( Table 2 ).
Time of second cancer occurrence
According to the analysis of the data presented in Table 2 , the median interval between first and second cancer was 5.2 years (range: 0–20 years), with no substantial difference in the time interval considering one or the other cancer as the first presented.
Treatment and follow-up
For both thyroid and kidney cancers, treatment of choice was represented by surgical excision (28), with no differences if they were primary, synchronous, or second malignancies. In most cases, the selected patients were affected by localized neoplasms; thus, no need for systemic therapy was required. Furthermore, as they were detected at an early stage, surgery had a curative effect. In case of synchronous malignancy, radical nephrectomy first and then total thyroidectomy with lymphoadenectomy were carried out (33).
In general, management of PTC remained equivalent, regardless of whether or not the patient had a synchronous or antecedent non-thyroidal neoplasia (21).
In most of the reported cases, the second cancer was identified during follow-up, except for the few cases of synchronous tumors, for which the pre-operative investigations made it possible to identify the second neoplasm at an earlier stage (33). In consideration of the increased risk of developing a second tumor after the primary cancer, all the authors recommended to keep this risk in mind during the follow-up of thyroid and kidney malignancies.
Discussion
The present review evaluated the association between thyroid and renal cancers, regardless of which cancer occurred first, highlighting that each primary thyroid or renal malignancy increases the relative risk of subsequent malignancy in the remnant organ of the survived patients. This applies to both sexes, particularly relevant in men (23), even if other reports document an increase only in treated female TCs (37).
Although there is a risk of a second primary tumor following primary invasive neoplasms and, specifically, there is a reciprocal association between thyroid and renal cancers, the estimated risk for the development of both cancers is low, with an incidence of about 1% according to Van Fossen et al. (23) For this reason, it is not considered necessary to include diagnostic screening tests in the follow-up of these neoplasms, compared with what is already foreseen for general population. If a more targeted preventive screening is deemed appropriate (7, 38, 39) in the presence of additional risk factors, ultrasound scans of the neck and kidneys may be indicated.
A bidirectional association between thyroid and renal cancers can be explained by shared genetic and/or common environmental risk factors including recognized etiological factors (i.e., smoking and obesity), or rare genetic syndromes predisposing to both events and regardless of the use of any forms of radiation treatment (14). Furthermore, individuals who develop both thyroid and renal carcinomas may represent a unique subset of cancer patients (19).
TC is associated with a number of genetic mutations leading to a different aggressive behavior. BRAF and RAS rearrangements remain the principal oncogenes, although other mutations, namely, TERT promoter and in TP53, as well as PIK3CA–PTEN–AKT–mTOR pathway and SWI–SNG complex (40), synergistically concur to worse outcomes and can be used in tumor prognostication (41). In the case of medullary carcinoma, RET mutation is commonly identified, supporting a distinct clonal origin in the case of a coexisting papillary tumor, as different cellular types might be affected simultaneously (42, 43).
The majority of renal carcinomas are sporadic, and numerous are the genetic alterations involved; in particular, the most important mutations involve the tumor-suppressor VHL, observed in about 80% of ccRCC (9). A genetic predisposition accounts for around 4% of the incidence of this malignancy, namely, in people affected by von Hippel-Lindau disease, hereditary papillary renal cancer, hereditary leiomyomatosis and renal cancer, and Birt-Hogg-Dubé syndrome. Other studies have also proposed possible genetic correlations between thyroid and renal cancers; Malchoff et al. (30) identified a distinct familial tumor syndrome linked to a germline mutation in chromosome 1q21 and characterized by a familial association of papillary TC, nodular thyroid disease, and papillary renal neoplasia. TC of follicular origin and renal cancer have also been found with greater frequency in CS, a hereditary cancer syndrome associated with a germline mutation in PTEN (44) and characterized by the presence of multiple hamartoma and dermatologic manifestations such as acral keratosis and facial trichilemmomas. For CS, thyroid carcinoma is one of the major diagnostic criteria, whereas RCC is part of the minor criteria.
Interestingly, as our review reported, the phenomenon of increased genetic instability and reduction of tumor immunity in multiple cancer patients was confirmed by the case of the woman with medullary, papillary, and RCC (32), a very rare combination, where even if the patient had no previous endocrine history, her mother was affected by breast cancer, another disease deeply connected to TC (4, 45–47) and the brother presented with RCC, too. A triple malignant tumor was also reported in a male of the same age with thyroid, kidney, and colon being affected (31), demonstrating common expression paths with integrin avß6 in multiple primary cancer (29).
Treatment of choice is surgery, regardless of whether or not the patient had a synchronous or antecedent neoplasia (21). The prognosis is in relation to the biological characteristics of each cancer, with the extent of the surgical procedure aiming to radically excise the mass and potentially reduce the incidence of subsequent cancers (48), without additional chemo and/or radiotherapy. If the patient is unfit for surgery, ablation via interventional radiology might represent a valid alternative (14).
Although radiation exposure is a known risk factor for the development of neoplasms and in particular for TC, and many chemotherapeutic agents are known to be carcinogenic, no correlation between radiotherapy or chemotherapy and the development of both TC and renal cancer was identified in any of the studies included in the review. This is mainly because the treatment of localized kidney cancer is primarily surgical, such as the treatment of well-differentiated TC; in fact, the association between kidney and TC is probably not related to radio and chemotherapy treatments (22) but rather to a shared genetic makeup or other environmental factors.
Considering the low risk of developing kidney cancer after TC and vice versa, it does not seem necessary to change the follow-up of patients with one of the two cancers to monitor the onset of the other one; however, it is important to always keep in mind that there is an increased risk of developing a second malignancy. It is always necessary to remember that, in subjects with a genetic syndrome that increases the risk of developing tumors, the follow-up should be structured taking into account the underlying genetic pathology.
Limitations
In consideration of the practical difficulties associated with evaluating the research question in prospective settings, only registry analyses and retrospective studies, mostly case reports, were included in the present review, limiting the evidence achieved. High-quality population databases are recommended with prospective analysis to elucidate on the bidirectional association between thyroid and kidney cancers.
Conclusions
As for TC, the advancement of diagnostic methods has led to an early treatment and an improvement in prognosis; in the same way, for kidney cancer, the increase in the diagnosis of neoplasms in the early stages has led to an increased survival; therefore, there has been a corresponding rise in the incidence of multiple primary cancers. A bidirectional association between thyroid and renal cancers has been identified and can be explained by shared genetic and common environmental risk factors. Even if there is an association, the coexistence of primary thyroid and RCC is rare. The standard treatment for both thyroid and kidney cancers remains surgery, which does not need to be associated with adjuvant therapies in the early stages, and the follow-up does not require special attention from clinicians or screening tests, except in cases of known genetic syndromes.
Data availability statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Author contributions
Conceptualization: MB, EL, SS and DP. Methodology: MB, SS, FF, AL, DT, MA and MV. Investigation and Data curation: EL, DP, VC, VD, EB and SU. Writing—original draft preparation: MB and EL. Writing—review and editing: MB, EL, SS, DP, FF, AL, DT, MA, MV, VC, EB and SU. Supervision: SS, DP, FF, SU and AL. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ccRCC, clear cell renal cell carcinoma; CS, Cowden syndrome; PTC, papillary carcinoma of the thyroid; RCC, renal cell carcinoma; TC, thyroid cancer.
References
- 1. Miranda A, Lortet-Tieulent J, Bray F, Cao B, Franceschi S, Vaccarella S. Thyroid cancer incidence trends by histology in 25 countries: A population-based study. Article Lancet Diabetes Endocrinol (2021) 9(4):225–34. doi: 10.1016/s2213-8587(21)00027-9 [DOI] [PubMed] [Google Scholar]
- 2. Fresilli D, David E, Pacini P, Gaudio Del G, Dolcetti V, Lucarelli GT, et al. Thyroid nodule characterization: How to assess the malignancy risk. update of the literature. Diagn (Basel) (2021) 11(8). doi: 10.3390/diagnostics11081374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sorrenti S, Dolcetti V, Radzina M, Bellini MI, Frezza F, Munir K, et al. Artificial intelligence for thyroid nodule characterization: Where are we standing? Cancers (Basel) (2022) 14(14). doi: 10.3390/cancers14143357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Scerrino G, Cocorullo G, Mazzola S, Melfa G, Orlando G, Laise I, et al. Improving diagnostic performance for thyroid nodules classified as Bethesda category III or IV: How and by whom ultrasonography should be performed. J Surg Res (2021) 262:203–11. doi: 10.1016/j.jss.2020.12.009 [DOI] [PubMed] [Google Scholar]
- 5. Sorrenti S, Baldini E, Pironi D, Lauro A, D’Orazi V, Tartaglia F, et al. Iodine: Its role in thyroid hormone biosynthesis and beyond. Nutrients (2021) 13(12). doi: 10.3390/nu13124469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ulisse S, Baldini E, Lauro A, Pironi D, Tripodi D, Lori E, et al. Papillary thyroid cancer prognosis: An evolving field. Cancers (Basel) (2021) 13(21). doi: 10.3390/cancers13215567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baldini E, Presutti D, Favoriti P, Santini S, Papoff G, Tuccilli C, et al. In vitro and In vivo effects of the urokinase plasminogen activator inhibitor WX-340 on anaplastic thyroid cancer cell lines. Int J Mol Sci (2022) 23(7). doi: 10.3390/ijms23073724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Q, Zeng Z, Nan J, Zheng Y, Liu H. Cause of death among patients with thyroid cancer: A population-based study. Front Oncol (2022) 12:852347. doi: 10.3389/fonc.2022.852347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen J, Qi N, Wang H, Wang Z, He Y, Zhu S. Second primary renal cell carcinoma with nonrenal malignancies: An analysis of 118 cases and a review of literature. Front Oncol (2021) 11:780130. doi: 10.3389/fonc.2021.780130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stewart GD, Klatte T, Cosmai L, Bex A, Lamb BW, Moch H, et al. The multispeciality approach to the management of localised kidney cancer. Lancet (2022) 400(10351):P523–34. doi: 10.1016/s0140-6736(22)01059-5 [DOI] [PubMed] [Google Scholar]
- 11. Capitanio U, Montorsi F. Renal cancer. Lancet (2016) 387(10021):894–906. doi: 10.1016/s0140-6736(15)00046-x [DOI] [PubMed] [Google Scholar]
- 12. Iglesias P, Díez JJ. Thyroid dysfunction and kidney disease. Eur J Endocrinol (2009) 160(4):503–15. doi: 10.1530/eje-08-0837 [DOI] [PubMed] [Google Scholar]
- 13. Baldini E, Odorisio T, Sorrenti S, Catania A, Tartaglia F, Carbotta G, et al. Vitiligo and autoimmune thyroid disorders. Front Endocrinol (Lausanne) (2017) 8:290. doi: 10.3389/fendo.2017.00290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abdel-Rahman O. Risk of subsequent primary kidney cancer after another malignancy: A population-based study. Clin Genitourin Cancer (2017) 15(5):e747–54. doi: 10.1016/j.clgc.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 15. Kim C, Bi X, Pan D, Chen Y, Carling T, Ma S, et al. The risk of second cancers after diagnosis of primary thyroid cancer is elevated in thyroid microcarcinomas. Thyroid (2013) 23(5):575–82. doi: 10.1089/thy.2011.0406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann T C, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj (2021) 372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Canchola AJ, Horn-Ross PL, Purdie DM. Risk of second primary malignancies in women with papillary thyroid cancer. Am J Epidemiol (2006) 163(6):521–7. doi: 10.1093/aje/kwj072 [DOI] [PubMed] [Google Scholar]
- 18. Antonelli A, Calza S, Arrighi N, Zani D, Corti S, Cozzoli A, et al. Clinical features and prognosis of patients with renal cancer and a second malignancy. Urol Oncol (2012) 30(3):294–300. doi: 10.1016/j.urolonc.2010.04.013 [DOI] [PubMed] [Google Scholar]
- 19. Carhill AA, Litofsky DR, Sherman SI. Unique characteristics and outcomes of patients diagnosed with both primary thyroid and primary renal cell carcinoma. Endocr practice: Off J Am Coll Endocrinol Am Assoc Clin Endocrinol (2015) 21(5):461–7. doi: 10.4158/EP14411.OR [DOI] [PubMed] [Google Scholar]
- 20. Murray KS, Zabor EC, Spaliviero M, Russo P, Bazzi WM., Musser JE, et al. Second primary malignancies in renal cortical neoplasms: An updated evaluation from a single institution. World J Urol Dec (2016) 34(12):1667–72. doi: 10.1007/s00345-016-1832-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Murray SE, Schneider DF, Bauer PS, Sippel RS, Chen H. Synchronous and antecedent nonthyroidal malignancies in patients with papillary thyroid carcinoma. J Am Coll Surg (2013) 216(6):1174–80. doi: 10.1016/j.jamcollsurg.2013.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ngeow J, Stanuch K, Mester JL, Barnholtz-Sloan JS, Eng C. Second malignant neoplasms in patients with cowden syndrome with underlying germline PTEN mutations. J Clin Oncol (2014) 32(17):1818–24. doi: 10.1200/jco.2013.53.6656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Van Fossen VL, Wilhelm SM, Eaton JL, McHenry CR. Association of thyroid, breast and renal cell cancer: A population-based study of the prevalence of second malignancies. Ann Surg Oncol (2013) 20(4):1341–7. doi: 10.1245/s10434-012-2718-3 [DOI] [PubMed] [Google Scholar]
- 24. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 25. Albores-Saavedra J, Dorantes-Heredia R, Chablé-Montero F, Córdova-Ramón JC, Henson DE. Association of urothelial carcinoma of the renal pelvis with papillary and medullary thyroid carcinomas. A new sporadic neoplastic syndrome? Ann Diagn Pathol (2014) 18(5):286–90. doi: 10.1016/j.anndiagpath.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 26. Oh SJ, Bae DS, Suh BJ. Synchronous triple primary cancers occurring in the stomach, kidney, and thyroid. Ann Surg Treat Res (2015) 88(6):345–8. doi: 10.4174/astr.2015.88.6.345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Atta IS, Alqahtani FN. Thyroid, renal, and breast carcinomas, chondrosarcoma, colon adenomas, and ganglioneuroma: A new cancer syndrome, FAP, or just coincidence. Case Rep Med (2016) 2016:5. doi: 10.1155/2016/2928084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Klain M, Maurea S, Gaudieri V, Zampella E, Volpe F, Manganelli M, et al. The diagnostic role of total-body (18)F-FDG PET/CT in patients with multiple tumors: A report of the association of thyroid cancer with lung or renal tumors. Quant Imaging Med Surg (2021) 11(9):4211–5. doi: 10.21037/qims-21-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ma J, Du J, Zhang Z, Wang H, Wang J. Synchronous primary triple carcinoma of thyroid and kidney accompanied by solitary fibrous tumor of the kidney: A unique case report. Int J Clin Exp Pathol (2014) 7(7):4268–73. [PMC free article] [PubMed] [Google Scholar]
- 30. Malchoff CD, Sarfarazi M, Tendler B, Forouhar F, Whalen G, Joshi V, et al. Papillary thyroid carcinoma associated with papillary renal neoplasia: Genetic linkage analysis of a distinct heritable tumor syndrome. J Clin Endocrinol Metab (2000) 85(5):1758–64. doi: 10.1210/jcem.85.5.6557 [DOI] [PubMed] [Google Scholar]
- 31. Peng C, Li Z, Gao H, Zou X, Wang X, Zhou C, et al. Synchronous primary sigmoid colon cancer and primary thyroid cancer followed by a malignant tumor of the kidney: Case report of multiple primary cancer and review of the literature. Oncol Lett (2019) 17(2):2479–84. doi: 10.3892/ol.2018.9867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Samarasinghe S, Yuksel S, Mehrotra S. Intermixed medullary and papillary thyroid cancer in a patient with renal cell carcinoma. Endocrinol Diabetes Metab Case Rep (2020) 2020(1):1–5. doi: 10.1530/EDM-20-0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Song JSA, Taylor SM, Trites J, Rigby MH, Bullock MJ, Merrimen J, et al. Tumor-to-tumor metastases: Papillary thyroid carcinoma into a clear cell renal cell carcinoma. J Otolaryngol - Head Neck Surg (2017) 46(1). doi: 10.1186/s40463-017-0193-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kim RH, Wang X, Evans AJ, Campbell SC, Nguyen JK, Farncombe KM, et al. Early-onset renal cell carcinoma in PTEN harmatoma tumour syndrome. Genomic Med (2020) 5(1). doi: 10.1038/s41525-020-00148-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Araque KA, Gubbi S, Klubo-Gwiezdzinska J. Updates on the management of thyroid cancer. Horm Metab Res (2020) 52(8):562–77. doi: 10.1055/a-1089-7870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Guilmette J, Nosé V. Hereditary and familial thyroid tumours. Histopathology (2018) 72(1):70–81. doi: 10.1111/his.13373 [DOI] [PubMed] [Google Scholar]
- 37. Berthe E, Henry-Amar M, Michels JJ, Rame JP, Berthet P, Babin E, et al. Risk of second primary cancer following differentiated thyroid cancer. Eur J Nucl Med Mol Imaging (2004) 31(5):685–91. doi: 10.1007/s00259-003-1448-y [DOI] [PubMed] [Google Scholar]
- 38. Baldini E, Tuccilli C, Prinzi N, Sorrenti S, Falvo L, De Vito C, et al. Deregulated expression of aurora kinases is not a prognostic biomarker in papillary thyroid cancer patients. PloS One (2015) 10(3):e0121514. doi: 10.1371/journal.pone.0121514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Baldini E, Tuccilli C, Prinzi N, Sorrenti S, Antonelli A, Gnessi L, et al. Effects of selective inhibitors of aurora kinases on anaplastic thyroid carcinoma cell lines. Endocr Relat Cancer (2014) 21(5):797–811. doi: 10.1530/ERC-14-0299 [DOI] [PubMed] [Google Scholar]
- 40. Xu B, Ghossein R. Genomic landscape of poorly differentiated and anaplastic thyroid carcinoma. Endocr Pathol (2016) 27(3):205–12. doi: 10.1007/s12022-016-9445-4 [DOI] [PubMed] [Google Scholar]
- 41. Bellini MI, Biffoni M, Patrone R, Borcea MC, Costanzo ML, Garritano T, et al. Poorly differentiated thyroid carcinoma: Single centre experience and review of the literature. J Clin Med (2021) 10(22). doi: 10.3390/jcm10225258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rossi S, Fugazzola L, De Pasquale L, Braidotti P, Cirello V, Beck-Peccoz P, et al. Medullary and papillary carcinoma of the thyroid gland occurring as a collision tumour: report of three cases with molecular analysis and review of the literature. Endocr Relat Cancer (2005) 12(2):281–9. doi: 10.1677/erc.1.00901 [DOI] [PubMed] [Google Scholar]
- 43. Baldini E, Tuccilli C, Pironi D, Catania A, Tartaglia F, Di Matteo F.M, et al. Expression and clinical utility of transcription factors involved in epithelial-mesenchymal transition during thyroid cancer progression. J Clin Med (2021) 10(18). doi: 10.3390/jcm10184076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. LLOYD KM, DENNIS M. Cowden’s disease. a possible new symptom complex with multiple system involvement. Ann Intern Med (1963) 58:136–42. doi: 10.7326/0003-4819-58-1-136 [DOI] [PubMed] [Google Scholar]
- 45. Baldini E, Lauro A, Tripodi D, Pironi D, Amabile MII, Catalina Ferent I, et al. Thyroid diseases and breast cancer. J Pers Med (2022) 12(2). doi: 10.3390/jpm12020156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Prinzi N, Baldini E, Sorrenti S, Vito De C, Tuccilli C, Catania A, et al. Prevalence of breast cancer in thyroid diseases: Results of a cross-sectional study of 3,921 patients. Breast Cancer Res Treat (2014) 144(3):683–8. doi: 10.1007/s10549-014-2893-y [DOI] [PubMed] [Google Scholar]
- 47. Graceffa G, Scerrino G, Militello G, Militello G, I, Randisi Laise B, et al. Breast cancer in previously thyroidectomized patients: Which thyroid disorders are a risk factor? Future Sci OA (2021) 7(5):Fso699. doi: 10.2144/fsoa-2021-0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Prinzi N, Sorrenti S, Baldini E, Vito De C, Tuccilli C, Catania A, et al. Association of thyroid diseases with primary extra-thyroidal malignancies in women: Results of a cross-sectional study of 6,386 patients. PloS One (2015) 10(3):e0122958. doi: 10.1371/journal.pone.0122958 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.