Abstract
Introduction
In early 2020, the Japanese government declared a nationwide state of emergency for the COVID‐19 pandemic. We investigated the impact of the emergency declaration on endoscopy adherence and conducted a follow‐up study of patients with canceled examinations at a tertiary endoscopy facility in Japan in 2020.
Methods
We compared the number of endoscopies performed, and cancelations at the endoscopy unit between 2019 and 2020 and used the Bayesian structural time series (BSTS) model to estimate the decrease in the number of endoscopies in 2020. We administered a questionnaire to those who had not undergone a scheduled endoscopy.
Results
Of 14 146 and 13 338 scheduled examinations, 1233 (8.7%) and 1403 (10.5%) were canceled in 2019 and 2020, respectively. During both years, age < 50 years, age > 80 years, upper endoscopy, and experience of endoscopy in the past 5 years were significantly associated with cancelations. In 2020, cancelations in the 14th–26th week of the year, including the period of state of emergency, increased significantly, and more women canceled. Of the 409 questionnaire‐respondents, 174 (42.5%) indicated that COVID‐19 had influenced their cancelation, and 315 (77.0%) had not undergone similar endoscopic examinations since then. The BSTS model predicted a decrease of 957 (95% CI −1213 to −708, P = .003) examinations.
Conclusion
In 2020, despite low numbers of COVID‐19 cases in the study site, the number of endoscopies decreased, and cancelation increased. Further research is needed on the future impact of a decrease in the number of endoscopies during a COVID‐19 pandemic.
Keywords: assessment of adherence, COVID‐19, endoscopy
1. INTRODUCTION
Endoscopic screening and surveillance contribute to early detection and treatment of diseases, which is especially useful in high‐risk gastrointestinal cancer patients. In areas where gastric cancer is endemic, such as in Asia1, 2 upper endoscopy screening is recommended every 2–3 years, and annual surveillance is recommended for patients with Helicobacter pylori infection or a history of gastric cancer treatment. 3 , 4 Colonoscopy in patients at risk of colorectal cancer is also useful for detecting early‐stage cancer and precancerous polyps. 5 Furthermore, periodic screening for intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas by endoscopic examination along with other modalities is recommended. 6 , 7 In such endoscopic practice, no‐shows and cancelations of scheduled endoscopic examinations hamper timely examinations, and reducing these behaviors is challenging. 8 , 9
The coronavirus disease (COVID‐19) pandemic hinders gastrointestinal cancer detection. COVID‐19 has exhausted medical resources and delayed regular work. The number of endoscopic examinations has decreased in areas where the pandemic is severe, 10 raising concerns on disease progression, increase in mortality, and additional deaths. This is attributed to provider factors, such as the allocation of resources for COVID‐19 response and restricting regular work for infection control, and patient factors, such as avoiding hospital visits for fear of infection and decreased screening priorities. The patient factors are difficult to investigate and are less reported.
In this context, evaluating endoscopic practices in Japan during the early phases of COVID‐19 pandemic can reveal patient factors. In Japan, the number of COVID‐19 infections in 2020 was approximately 240 000, fewer than the 2.44 million in the UK and 19.9 million in the US. 11 Although the actual number of COVID‐19 infections was relatively controlled, there are concerns regarding their impact on the gastrointestinal cancer healthcare system in Japan. A multicenter study from Osaka, Japan, found that the number of endoscopies performed had decreased due to provider reasons, following the recommendation of the Japan Gastroenterological Endoscopy Society. 12 , 13 The number of endoscopic examinations decreased not only in cities with high COVID‐19 infection rates, but throughout Japan. In addition to the provider factors, patient behavior may have affected the number of endoscopic examinations, although there is limited information on these factors.
Herein, we investigated the real‐world practices of a tertiary endoscopy center in Miyagi, Japan, which reported few COVID‐19 cases in 2020, to estimate the impact of the pandemic on patients' endoscopic visits. Miyagi Prefecture is a regional hub in the Tohoku region in Japan, and the cumulative number of COVID‐19 infections was 78 cases by the time the nationwide state of emergency was declared in April 2020. We aimed to evaluate the impact of the COVID‐19 pandemic on the behavior of patients by investigating the status of endoscopic care and reasons for patients' non‐attendance.
2. PATIENTS AND METHODS
2.1. Study population and the situation of COVID‐19 pandemic
Eligible patients were those scheduled for endoscopy between 2017 and 2020 at the outpatient department of Sendai Kousei Hospital, which is a large tertiary endoscopy center in Miyagi, Japan, and receives many referrals from hospitals and clinics in the prefecture. The endoscopy center provides endoscopic examinations mainly for pre‐treatment scrutiny of referred patients, and surveillance and screening for various cancers of the gastrointestinal tract, biliary system, and pancreas. On April 16, 2020 (the 16th week), a state of emergency was declared throughout Japan; however, because the number of COVID‐19 cases was fewer in Miyagi, the endoscopy center continued to provide scheduled endoscopic examinations with appropriate infection control measures in accordance with the Japanese endoscopic guidelines. The trend of new COVID‐19 cases in both Miyagi Prefecture and throughout Japan in 2020 is shown in Figure 1. 14
FIGURE 1.
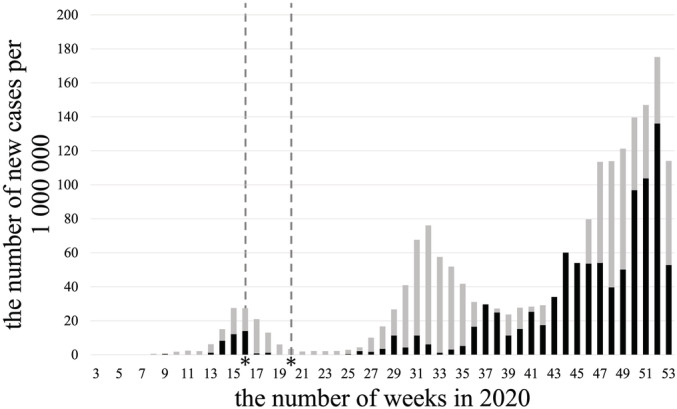
The number of new coronavirus disease (COVID‐19) infections per million population in Miyagi prefecture and throughout Japan in 2020. The asterisks show the start and end of the state of emergency declared by the central government. The light gray bars represent the number of newly diagnosed COVID‐19 cases per week for Japan as a whole and the dark black bars represent Miyagi Prefecture
2.2. Review of medical records and endoscopy charts
We targeted patient's cancelations or no‐shows for endoscopies for 2019 and 2020 (Figure 2). Once an examination appointment was registered in the endoscopy system, we defined a cancelation as a case in which the examination was not performed by the scheduled date for some reason, such as the patient not showing up for the examination on the scheduled date or notifying us in advance that the examination was canceled. We reviewed the medical records of all patients scheduled for outpatient endoscopy (January 2019–December 2020), with reference to the endoscopic findings, including patient age, gender, and type of scheduled endoscopy (upper endoscopy, colonoscopy, endoscopic ultrasound for pancreas). We also cross‐referenced each patient's endoscopic record to determine whether the patient had undergone an endoscopic procedure in the past 5 years, and in case of which, whether the patient had undergone an endoscopic treatment and gastrointestinal surgery.
FIGURE 2.
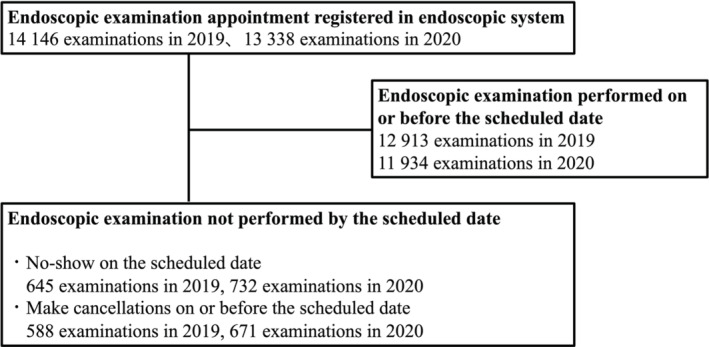
Flowchart for collecting status of endoscopic examinations performed or canceled
2.3. Statistical analysis and estimation of the impact by the Bayesian structural time series model (BSTS)
We analyzed the relationship between gender, age, examination type, past 5 years of endoscopic experience, and scheduled period (Q1: weeks 1–13, Q2: weeks 14–26, Q3: weeks 27–39, and Q4: weeks 40–52) to cancelation by multivariable logistic regression analysis. In addition, the BSTS model was used to estimate the impact of the COVID‐19 pandemic on endoscopic practice. 15 The R package Causal Impact was used in this study. We estimated the increase or decrease in the number of outpatient endoscopies performed after the declaration of a state of emergency in Japan (week 16). The number of endoscopies performed in the outpatient department between January 2017 and December 2020 was used to estimate the seasonal variations. Odds ratios were reported with 95% confidence intervals, and all statistical tests were considered significant if P < .05. All analyses were conducted using statistical package R (Version 3.6.3) and Stata Version 15.1 (Stata Corporation, College Station, TX, USA) software.
2.4. Questionnaire for non‐attendees in 2020
We conducted a survey among those scheduled for the procedure in 2020 who had canceled and did not undergo another endoscopy at the time of the survey (April 2021), excluding those with obvious reasons such as death. An invitation letter was sent by mail, and responses by mail, telephone, or web form were accepted. The response period was from May 25 to June 25, 2021. The content of the questionnaire was prepared based on previous studies 16 and in consultation with gastrointestinal endoscopists (HS, TM, and DH) (Supplementary File 1). The outline of the study was described beforehand in the questionnaire, and the response to the questionnaire was regarded as consent. In addition, regarding the analysis of other data, this study used anonymized data, which was collected by the opt‐out method of our hospital website. This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of the Sendai Kousei Hospital (No. 3–2, 2021).
3. RESULTS
A total of 14 146 examinations (9420 upper endoscopy, 4036 colonoscopy, and 690 endoscopic ultrasounds of pancreas) were scheduled in 2019, while 13 338 endoscopies were scheduled in 2020 (9022 upper endoscopy, 3651 colonoscopy, and 665 endoscopic ultrasounds for pancreas) (Table 1). Of these, 1233 (8.7%) were canceled in 2019 (961 [10.2%] upper endoscopy, 230 [5.7%] colonoscopy, and 42 [6.1%] endoscopic ultrasound of pancreas), while 1403 (10.5%) were canceled in 2020 (1114 [12.4%] upper endoscopy, 244 [6.7%] colonoscopy, and 45 [6.8%] endoscopic ultrasound of pancreas). Of those who did not arrive as planned, few scheduled other appointments and in the end 50.0% (616/1233) and 60.5% (849/1403) were not tested in 2019 and 2020, respectively. As a result, a total of 11 992 endoscopic examinations were performed in 2020, which is 6.7% less than that in 2019 when 12 856 examinations were performed.
TABLE 1.
Comparison of characteristics of patients scheduled for endoscopy in 2019 and 2020
| Variable | Scheduled in 2019 (N = 14 146) | Scheduled in 2020 (N = 13 338) | P value |
|---|---|---|---|
| Age, mean, SD | 70.3 (12.0) | 69.5 (12.1) | * |
| Female | 6144 (43.4) | 5653 (42.4) | .08 |
| Scheduled week | * | ||
| Q1 (1st – 13th week of the year) | 3272 (23.1) | 3297 (24.7) | – |
| Q2 (14th – 26th week of the year) | 3333 (23.6) | 3010 (22.6) | – |
| Q3 (27th – 39th week of the year) | 3617 (25.6) | 3236 (24.3) | – |
| Q4 (40th – 52nd week of the year) | 3924 (27.7) | 3795 (28.5) | – |
| Type of endoscopy | .10 | ||
| Upper endoscopy | 9420 (66.6) | 9022 (67.6) | – |
| Colonoscopy | 4036 (28.5) | 3651 (27.4) | – |
| Endoscopic ultrasound for pancreas | 690 (4.9) | 665 (5.0) | – |
| Endoscopic experience in the past 5 years | 10136 (71.7) | 9751 (73.1) | * |
| The history of ESD or EMR | 2391 (23.6) | 2371 (24.3) | .23 |
| The history of surgery for gastrointestinal diseases | 1234 (12.2) | 1243 (12.7) | .23 |
Note: Values are n (%). P value <.05 is indicated as *.
Q, quarter of the year, Q1 represents the 1st quarter of the year, corresponding to the 1st to 13th weeks of the year.
ESD, endoscopic submucosal dissection.
EMR, endoscopic mucosal resection. Endoscopic experience was based on the last 5 years of endoscopy performed at Sendai Kousei Hospital. Gastrointestinal diseases includes esophageal, gastric, intestinal, colonic, pancreatic, biliary cancer and gastroduodenal ulcers.
3.1. Medical records from 2019 and 2020
The reasons for cancelation in 2019 and 2020 were no‐shows/unknown (52.3% vs 52.2%), inconvenient time of appointment (20.4% vs 15.0%), priority given to other health issues (7.9% vs 5.4%), and perception of no need to undergo the examination (5.1% vs 7.2%), whereas the fear of COVID‐19 (7.6%) was reported in 2020 (Table 2). The logistic regression analysis of each factor associated with no‐shows/cancelation is shown in Table 3. In both 2019 and 2020, age < 50 years, age > 80 years, upper endoscopy, and experience of endoscopy in the past 5 years were significantly associated with cancelation. In 2020, cancelations in Q2 (14th–26th week of the year), which included the period of the state of emergency, increased significantly compared to those in Q1 (adjusted odds ratio [aOR] 1.88, 95% CI 1.61–2.20, P < .05). Women were significantly more likely to cancel appointments than men (aOR 1.19; 95% CI 1.06–1.33; P < .05).
TABLE 2.
Overview of primary reasons for non‐participants from medical chart review
| Variable | 2019 (N = 14 146) | 2020 (N = 13 338) | P value |
|---|---|---|---|
| Cancel, no‐shows | 1233 (8.7) | 1403 (10.5) | * |
| Type of endoscopy | |||
| Upper endoscopy | 961 (10.2) | 1114 (12.4) | * |
| Colonoscopy | 230 (5.7) | 244 (6.7) | .07 |
| Endoscopic ultrasound for pancreas | 42 (6.1) | 45 (6.8) | .61 |
| Week of cancel | |||
| Q1 (1st – 13th week of the year) | 273 (8.3) | 295 (9.0) | .384 |
| Q2 (14th – 26th week of the year) | 307 (9.2) | 483 (16.1) | * |
| Q3 (27th – 39th week of the year) | 303 (8.4) | 280 (8.7) | .683 |
| Q4 (40th – 52nd week of the year) | 350 (8.9) | 345 (9.1) | .792 |
| Reason for cancel | ‐ | ||
| Unknown, no‐shows | 645 (52.3) | 732 (52.2) | |
| Inconvenient time of appointment | 251 (20.4) | 210 (15.0) | |
| Fear of COVID‐19 | – | 107 (7.6) | |
| Feeling no need to undergo the examination | 63 (5.1) | 101 (7.2) | |
| Priority given to other health issue | 97 (7.9) | 76 (5.4) | |
| Too sick on day of appointment | 75 (6.1) | 65 (4.6) | |
| Unaware of appointment | 25 (2.0) | 31 (2.2) | |
| Insufficient preparation | 35 (2.8) | 27 (1.9) | |
| Death | 10 (0.8) | 22 (1.6) | |
| Had procedure in other hospital | 19 (1.5) | 12 (0.9) | |
| Relocation | 0 | 4 (0.3) | |
| Bad weather | 2 (0.2) | 0 | |
| Others | 11 (0.9) | 16 (1.1) |
Note: Values are n (%). Chi‐square test was used for testing. P value <.05 is indicated as *.
Q, quarter of the year, Q1 represents the 1st quarter of the year, corresponding to the 1st to 13th week of the year.
TABLE 3.
Factors related to cancelation and no‐shows for scheduled endoscopies in 2019/2020
| 2019 | 2020 | |||||
|---|---|---|---|---|---|---|
| Variable | aOR | 95% CI | P value | aOR | 95% CI | P value |
| Age | ||||||
| <50 y | 1.45 | (1.14–1.84) | * | 1.47 | (1.17–1.84) | * |
| 50–80 y | Reference | Reference | ||||
| ≧ 80 y | 1.46 | (1.28–1.67) | * | 1.59 | (1.39–1.81) | * |
| Gender | ||||||
| Male | Reference | Reference | ||||
| Female | 1.11 | (0.99–1.25) | .09 | 1.19 | (1.06–1.33) | * |
| Scheduled week | ||||||
| Q1 (1st – 13th week of the y) | Reference | Reference | ||||
| Q2 (14th – 26th week of the y) | 1.09 | (0.91–1.29) | .35 | 1.88 | (1.61–2.20) | * |
| Q3 (27th – 39th week of the y) | 1.00 | (0.84–1.19) | .97 | 0.95 | (0.80–1.13) | .60 |
| Q4 (40th – 52nd week of the y) | 1.08 | (0.91–1.27) | .39 | 1.02 | (0.86–1.20) | .83 |
| Examination type | ||||||
| Upper endoscopy | 1.70 | (1.46–1.98) | * | 1.66 | (1.44–1.93) | * |
| Colonoscopy | Reference | Reference | ||||
| Endoscopic ultrasound for pancreas | 1.08 | (0.77–1.51) | .67 | 0.93 | (0.67–1.30) | .68 |
| Endoscopy experience before 5 y* | ||||||
| Absent | Reference | Reference | ||||
| Present | 1.64 | (1.41–1.91) | * | 2.08 | (1.77–2.43) | * |
aOR, adjusted odds ratio.
Q, quarter of the year, Q1 represents the 1st quarter of the year, corresponding to the 1st to 13th week of the year. P value <.05 is indicated as *.
3.2. Questionnaire for the non‐attendees
A questionnaire was sent to 780 patients, and 409 people responded (52.4%). Table 4 summarizes the reasons for non‐attendance. Of the 409 respondents, 174 (42.5%) indicated that the impact of COVID‐19 influenced their cancelation. Among them, 120 (69%) feared the possibility of infection with COVID‐19 by visiting the hospital, 73 (42%) were reluctant to go out, 65 (37.4%) feared the risk of infecting their family members with COVID‐19 by visiting the hospital, and 54 (31.0%) reported they did not visit the hospital because of the declarations by the prefecture or the government. Of the 409 respondents, 315 have not undergone similar examinations since then. Of the 315 respondents, 51 (16.2%) had already made plans to undergo the examination, 205 (65.1%) were considering having the examination eventually, and 58 (18.4%) were not considering it. Of those who were considering examinations, 14.4% were planning to undergo it in 2022.
TABLE 4.
Questionnaire for non‐attendees of scheduled endoscopies in 2020
| Characteristics of the respondent | Respondent N = 409 |
|---|---|
| Female, n % | 171 (41.8) |
| Age, median (interquartile range) | 76 (70–82) |
| Examination type | |
| Upper endoscopy | 361 (88.3) |
| Colonoscopy | 43 (10.5) |
| Endoscopic ultrasound for pancreas | 5 (1.2) |
| Questionnaire items | |
| Q1 Do you remember having an appointment for endoscopy in 2020? | |
| Yes | 338 (82.6) |
| No | 68 (16.6) |
| No answer | 3 (0.7) |
| Q2 What is the reason for non‐attendance? | |
| I had other appointments. | 50 (12.2) |
| Unaware of appointment | 63 (15.4) |
| I did not think I needed to be tested. | 29 (7.1) |
| I have already been tested at another medical institution. | 41 (10.0) |
| Priority given to other health issue | 50 (12.2) |
| Due to the spread of COVID‐19. | 166 (40.6) |
| Issue of transportation | 11 (2.7) |
| I did not want to be tested. | 11 (2.7) |
| Relocation | 2 (0.5) |
| Death | 5 (1.3) |
| Others | 97 (23.7) |
| Q3 Did the COVID‐19 pandemic associate with your cancelation of the examination? | |
| Yes | 174 (42.5) |
| No | 225 (55.0) |
| No answer | 10 (2.4) |
| Q3‐1 What kind of the impact did you feel? | |
| Feared that by going to the hospital, my family would be infected with COVID‐19 | 65 (37.4) |
| Feared that by going to the hospital, I would be infected with COVID‐19 | 120 (69.0) |
| Because of the declaration and request issued by the prefecture and the government | 54 (31.0) |
| Did not even want to go out | 73 (42.0) |
| Thought that endoscopy was considered a high risk for COVID‐19 infections | 13 (7.5) |
| Others | 34 (19.5) |
| Q4 Have you had the endoscopy examination at other clinics since then? | n = 409 |
| Yes | 58 (14.2) |
| No | 315 (77.0) |
| No answer | 36 |
| Q4‐1 Do you plan to undergo an endoscopic examination in the future? | n = 315 |
| I have already made appointments for the examination | 51 (16.2) |
| I am considering having the examination at some point | 205 (65.1) |
| I have no plans to have the examination in the future | 58 (18.4) |
| Q4‐2 At what time would you be likely to have the test? | n = 194 |
| In 2021 | 83 (42.8) |
| In 2022 | 28 (14.4) |
| Undecided | 83 (42.8) |
3.3. Causal impact simulation
The BSTS model predicted that 248.97 endoscopies per week would have been performed in the absence of the event (95% CI 242.41–255.70), compared to an average of 223.79 endoscopies per week after the declaration of a national state of emergency in 2020, an estimated decrease of −25.18 (95% CI ‐31.91–‐18.62). In total, 8504 endoscopies were performed, but 9461 (95% CI 8841–9611) would have been expected if no event had occurred, which is an estimated decrease of −957 (95% CI ‐1213 to ‐708). This result was statistically significant with the Bayesian one‐sided tail‐area probability (P = .003). Figure 3 shows the discrepancy between the number of tests predicted by the BSTS model and the actual number of examinations after the emergency was declared.
FIGURE 3.
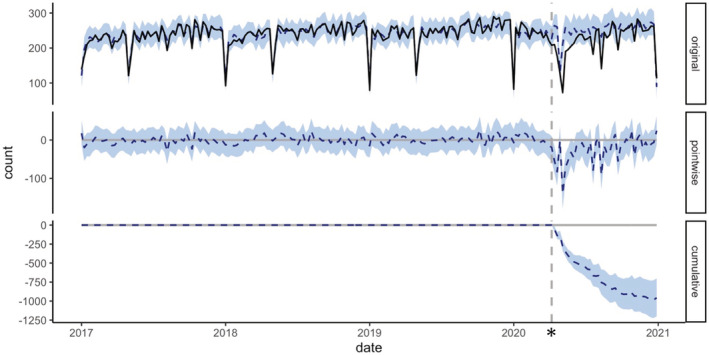
The causal impact model of the number of performed endoscopic examinations. The vertical dashed line represents the time in April 2020, when the state of emergency was declared. The graph in the upper “original” row shows the actual number of tests per week (solid line) and the number of tests estimated by the model (dashed line). The graph in the middle row shows the difference between the number of tests estimated by the model and the actual number of tests. The bottom row shows the change in the total number of tests since the event; the 95% confidence interval is shown in blue
4. DISCUSSION
In this study, we describe the actual clinical practice under the COVID‐19 pandemic at a large endoscopy facility in Japan. It is noteworthy that fewer endoscopic examinations were performed although it was in the early stage of the pandemic in the area, with the increase in cancelations after the state of emergency.
The decrease in the number of endoscopies revealed in this study was small compared to that in other countries, and it was considered that endoscopic practice was largely maintained during the study period. This is probably since the actual number of COVID‐19 patients in Japan was lower than that in other countries, and the declaration of a state of emergency was not accompanied by penalties. However, it is important to note that endoscopic practice was affected even in areas with low levels of COVID‐19 infection. It has already been reported that endoscopic practice during the COVID‐19 pandemic is hampered in areas where infection is widespread. 17 , 18 , 19 , 20 Most facilities in North America provided endoscopic services at less than 10% of their usual volume in March and April 2020;19 in the Netherlands, 45% fewer colonoscopies and 57% fewer gastroscopy procedures were reported during the 2020 lockdown compared to the previous year, 21 and a national endoscopy database in the United Kingdom found that between March and May 2020, the number of endoscopies reduced to approximately 12% of the previous level. 18 All these studies in different countries reported a more severe COVID‐19 infection prevalence than the current study. On the other hand, few studies have examined changes in endoscopic practice in areas where COVID‐19 infections are less common, or the relationship between the prevalence of COVID‐19 and its impact on endoscopic practice. The decrease in the number of 2020 endoscopies seen in this survey is less than that reported in other countries or from cities in Japan with high COVID‐19 prevalence, 12 and may be because the endoscopy medical staff were not busy dealing with COVID‐19 and that medical resources were relatively secure. The prevalence of COVID‐19 varies according to country, region, and time of the year. There is a need to measure and analyze the impact of endoscopy practices at different times of the pandemic in many countries and regions with different COVID‐19 prevalence.
At the study site, there was a significant increase in the number of cancelations of scheduled examinations after the declaration of the state of emergency in April 2020, and the results showed that many cancelations were due to COVID‐19 pandemic‐related issues. In the multivariate analysis of the current study, the factors involved in cancelations were similar in 2019 and 2020, but being female was newly identified as a factor that was not found in 2019 and was more likely to cancel an endoscopy in 2020. In understanding this change, it is necessary to consider the possibility that factors such as employment status and psychological anxiety may be behind this trend. In the early stages of the COVID‐19 pandemic in 2020, there was a lack of information on COVID‐19 prevalence in Japan, its mortality rate, and the prospects for the spread and containment of the pandemic, all of which have caused anxiety and fear of COVID‐19. 22 The declaration of a state of emergency in Japan was a call for refraining from going out unnecessarily, but it had the effect of stopping the necessary examinations even in the present study area where there were almost no infected people during that time. In Japan, it has been shown that people who have a change in work style, change in daily life, decrease in income, and anxiety regarding COVID‐19, experienced more psychological distress in the early stages of the COVID‐19 pandemic, 23 which may also occur in people in areas with relatively low levels of COVID‐19 prevalence, thereby impacting medical visits. When assessing the impact of COVID‐19 on endoscopic practice in Japan, we should consider the changes that the pandemic has caused in medical resources, as well as the psychological fears of patients and their reluctance to seek medical care.
In this study, many patients who canceled appointments in 2020 did not receive subsequent testing, and many were planning to postpone it for a year or more. This may lead to delays in diagnosis. It has been shown that approximately 7% of early‐stage colorectal cancers (equivalent to clinical stages I and II) can progress to advanced stages (III and IV) if screening is delayed for 1 year. 24 Therefore, a prolonged delay in endoscopic screening during the COVID‐19 pandemic can delay the opportunity for appropriate treatment. In fact, the number of surgeries for gastrointestinal‐related malignancies in Japan in 2020 is reported to have decreased from the previous year. 25 It is speculated that a decrease in endoscopic screening may be a contributing factor to this decline. In Yokohama, which was one of the highest COVID‐19 prevalence areas in Japan, more advanced gastrointestinal cancers were diagnosed in late 2020. 26 This delay in diagnosis may occur in countries or regions with fewer COVID‐19 cases and needs to be further verified, as indicated by the increase in cancelations and decrease in the number of endoscopic examinations in this study.
4.1. Future implications
The prevalence of COVID‐19 varies greatly among countries and regions. This study revealed that even with a low prevalence of COVID‐19, patient visits were affected. Although it needs to be verified whether this result occurred in other regions and countries, local governments and healthcare providers should send messages to patients to consider the local situation when a state of emergency is declared. In addition, this study demonstrates that in the early stages of a pandemic, the impact on conventional medical care may be caused more by the regulations and tensions generated by the pandemic than by the actual spread of COVID‐19. Consequently, the lessons acquired from this study could be applied to any long‐term outbreak of other emerging infectious illnesses or comparable public health hazards with a major societal impact. As patients with canceled examinations are unlikely to be tested for some time, individual attention should be given to those at high risk of disease, where a 1‐year delay in diagnosis can affect subsequent treatment. Particularly, it may be important to thoroughly explain the need for endoscopic examination to people at high risk for cancer, or to educate on endoscopy based on the patient's risk. Appropriate methods of communicating information to those who should undergo endoscopy during the pandemic should continue to be studied. In addition, estimation based on modeling may also be necessary for determining the negative influences that real reduction in endoscopic examination has had on patients. Analyzing the characteristics of the patient population that did not undergo endoscopic examinations, modeling the risk of diseases such as cancer and the risk of disease progression due to not undergoing examinations, and the resulting impact on life expectancy would more effectively highlight the need for countermeasures.
The strengths of this study are the ability to track the detailed number of visits by number of weeks and the high response rate of questionnaires from those who canceled. This may be difficult to achieve with other sites. However, the present study has some limitations. The information on the number of days between the appointment date and the test or the distance of the hospital from the patient's address, which could affect the cancelation rate, were unavailable. In addition, we were not able to elaborate on symptomatic or asymptomatic test purposes. Nonetheless, this study clarifies endoscopic practices during the initial phases of the COVID‐19 outbreak in Japan. In the future, long‐term, multicenter studies are required to assess in depth the influence of the COVID‐19 pandemic on endoscopic practices, and to quantify the impact on the number of diseases detected and disease progression.
5. CONCLUSION
In this study, we found that in 2020, the number of endoscopic cancelations increased after the declaration of a state of emergency in a COVID‐19 low prevalence area of Japan. Further research is needed on the changes in endoscopic practice during the COVID‐19 pandemic and their future implications.
AUTHOR CONTRIBUTIONS
H.S. had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis. Study concept and design: H.S., K.I., and I.M. Acquisition of data: H.S. and I.M. Analysis and interpretation of data: H.S. Drafting of the manuscript: H.S. and K.I. Critical revision and supervision: I.T., Y.N., Y.T., T.O., M. T., D.H., N.M., and T.M. All authors discussed the results and commented on the manuscript. All authors approved the contents of the submitted manuscript.
FUNDING INFORMATION
The present study was not supported by any funding.
CONFLICT OF INTEREST
Dr Hiroaki Saito reports personal fees from TAIHO pharmaceutical company outside of the submitted work. Dr Tomoki Matsuda reports personal fees from Takeda pharmaceutical company, Astellas pharma Inc., FUJIFILM Medical CO. Ltd., and EA Pharma Co., Ltd outside of the submitted work. Other authors, Fumiya Murakami, Kimihiro Igarashi, Ippei Tanaka, Yoshitaka Nawata, Yukari Tanaka, Toru Okuzono, Masaharu Tsubokura, Masato Nakahori, and Dai Hirasawa have nothing to declare.
Supporting information
Supplementary file 1 The content of the questionnaire; the original document is in Japanese and has been translated into English.
ACKNOWLEDGMENTS
We would like to thank Dr. Yoshitaka Nishikawa for the support to build the BSTS model and all the medical staff of the endoscopic unit in Sendai Kousei Hospital for their involvement in the questionnaire surveys.
Saito H, Igarashi K, Murakami F, et al. Impact of COVID‐19 on the endoscopy department since the early phase of the pandemic in 2020: A questionnaire study among patients with canceled examinations at a single Japanese institution. Asian J Endosc Surg. 2022;1‐10. doi: 10.1111/ases.13123
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Park HA, Nam SY, Lee SK, et al. The Korean guideline for gastric cancer screening. J Korean Med Assoc. 2015;58(5):373‐384. [Google Scholar]
- 2. Hamashima C, Kato K, Miyashiro I, et al. Update version of the Japanese guidelines for gastric cancer screening. Jpn J Clin Oncol. 2018;48(7):673‐683. [DOI] [PubMed] [Google Scholar]
- 3. Nakajima T, Oda I, Gotoda T, et al. Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer. 2006;9(2):93‐98. [DOI] [PubMed] [Google Scholar]
- 4. Graham DY, Asaka M. Eradication of gastric cancer and more efficient gastric cancer surveillance in Japan: two peas in a pod. J Gastroenterol. 2010;45(1):1‐8. Available from. http://link.springer.com/10.1007/s00535‐009‐0117‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the U.S. multi‐society task force on colorectal cancer. Gastrointest Endosc. 2017;86(1):18‐33. [DOI] [PubMed] [Google Scholar]
- 6. Elta GH, Enestvedt BK, Sauer BG, Lennon AM. ACG clinical guideline: diagnosis and Management of Pancreatic Cysts. Am J Gastroenterol. 2018. Apr;113(4):464‐479. [DOI] [PubMed] [Google Scholar]
- 7. Tanaka M, Fernández‐del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017. Sep;17(5):738‐753. [DOI] [PubMed] [Google Scholar]
- 8. Adams LA, Pawlik J, Forbes GM. Nonattendance at outpatient endoscopy. Endoscopy. 2004;36:5‐404. [DOI] [PubMed] [Google Scholar]
- 9. Denberg TD, Melhado TV, Coombes JM, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20(11):989‐995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Belle A, Barret M, Bernardini D, et al. Impact of the COVID‐19 pandemic on gastrointestinal endoscopy activity in France. Endoscopy. 2020;52(12):1111‐1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ritchie H, Mathieu E, Rodés‐Guirao L, et al. “Coronavirus Pandemic (COVID‐19)”. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/coronavirus’ [Online Resource]. (2020).
- 12. Maruyama H, Hosomi S, Nebiki H, Fukuda T, Nakagawa K, Okazaki H. Gastrointestinal endoscopic practice during COVID‐19 pandemic: a multi‐institutional survey. Rom J Intern Med. 2021;59(2):166‐173. [DOI] [PubMed] [Google Scholar]
- 13. Irisawa A, Furuta T, Matsumoto T, et al. Gastrointestinal endoscopy in the era of the acute pandemic of coronavirus disease 2019: recommendations by Japan gastroenterological endoscopy society (issued on April 9th, 2020). Dig Endosc. 2020;32(5):650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Miyagi prefecture government. COVID‐19 Outbreaks in the Prefecture [Internet]. [cited 2021 Nov 13]. Available from: https://www.pref.miyagi.jp/site/covid-19/02.html
- 15. Brodersen KH, Gallusser F, Koehler J, Remy N, Scott SL. Inferring causal impact using bayesian structural time‐series models. Ann Appl Stat. 2015;9(1):247‐274. [Google Scholar]
- 16. Bhise V, Modi V, Kalavar A, et al. Patient‐reported attributions for missed colonoscopy appointments in two large healthcare systems. Dig Dis Sci. 2016;61(7):1853‐1861. [DOI] [PubMed] [Google Scholar]
- 17. Soetikno R, Teoh AYB, Kaltenbach T, et al. Considerations in performing endoscopy during the COVID‐19 pandemic. Gastrointest Endosc. 2020. Jul;92(1):176‐183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID‐19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021. Mar;70(3):537‐543. [DOI] [PubMed] [Google Scholar]
- 19. Forbes N, Smith ZL, Spitzer RL, et al. Changes in gastroenterology and endoscopy practices in response to the coronavirus disease 2019 pandemic: results from a north American survey. Gastroenterology. 2020. Aug;159(2):772‐774.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parasa S, Reddy N, Faigel DO, Repici A, Emura F, Sharma P. Global impact of the COVID‐19 pandemic on endoscopy: an international survey of 252 centers from 55 countries. Gastroenterology. 2020;159(4):1579‐1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lantinga MA, Theunissen F, ter Borg PCJ, Bruno MJ, Ouwendijk RJT, Siersema PD. Impact of the COVID‐19 pandemic on gastrointestinal endoscopy in The Netherlands: analysis of a prospective endoscopy database. Endoscopy. 2021;53:166‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kobayashi T, Maeda M, Takebayashi Y, Sato H. Traditional gender differences create gaps in the effect of COVID‐19 on psychological distress of Japanese workers. Int J Environ Res Public Health. 2021;18(16):8656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nagasu M, Muto K, Yamamoto I. Impacts of anxiety and socioeconomic factors on mental health in the early phases of the COVID‐19 pandemic in the general population in Japan: a web‐based survey. PLOS One. 2021. Mar 17;16(3);16:e0247705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ricciardiello L, Ferrari C, Cameletti M, et al. Impact of SARS‐CoV‐2 pandemic on colorectal cancer screening delay: effect on stage shift and increased mortality. Clin Gastroenterol Hepatol. 2021. Jul;19(7):1410‐1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ikeda N, Yamamoto H, Taketomi A, et al. The impact of COVID‐19 on surgical procedures in Japan: analysis of data from the National Clinical Database. Surg Today. 2022;52:22‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kuzuu K, Misawa N, Ashikari K, et al. Gastrointestinal cancer stage at diagnosis before and during the COVID‐19 pandemic in Japan. JAMA Netw Open. 2021;4:e2126334. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file 1 The content of the questionnaire; the original document is in Japanese and has been translated into English.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


