Abstract
Objective
To define the conversion risk to open procedure during robot‐assisted thyroid surgery (RATS) identifying potential specific subclasses of procedures or accesses at higher conversion risk.
Methods
In a PRISMA‐compliant framework, all original prospective studies providing RATS conversion rates from multiple databases were pooled in a random‐effects meta‐analysis. Conversion rates were compared between different typologies of thyroid surgery and robotic access.
Results
13 studies were deemed eligible. Four conversions from two studies were reported out of 398 procedures. No significant heterogeneity was observed (Cochran's Q p = 0.932; I2 = 0%). The pooled conversion rate was 1% (95% confidence interval, 0.1%–2%). The ANOVA‐Q test failed to show significant differences when comparing type of thyroid surgery or robotic access (respectively p = 0.766 and p = 0.457).
Conclusion
While the conversion rate appears consistently low across studies, prospective data collection and systematic reporting of procedural complications are required for framing high‐risk procedures and accesses.
Keywords: adverse events, complications, hemithyroidectomy, minimally invasive surgery, robotic surgery, thyroidectomy
1. INTRODUCTION
Minimally invasive surgical techniques, whether robot‐ or endoscope‐assisted, have a known risk of conversion to open irrespectively of the surgical area of application. 1 , 2 , 3
While robotic assistance has been first employed for thyroid surgery later than in other anatomical compartments, 4 its use soon became widespread. Reports of conversions, therefore, grew in numbers also for thyroid surgery. In robotic‐assisted thyroid surgery (robot‐assisted thyroid surgery (RATS), known conversion had been required, among other causes, for excessive bleeding, previously undetected neoplastic infiltration or unexpected disease extension, or technical issues. 5 , 6 , 7
Despite the potential need for conversion being recognized in most case series, conversion rates are reported inconsistently in the literature and span from large case series with no conversion 8 to significantly preliminary smaller series with rates higher than 15%. 9
To the authors' knowledge, no study has systematically explored the risk of conversion in RATS or addressed whether different RATS procedures (e.g. Total thyroidectomy ,TT, hemithyroidectomy (HT), or radicalisation thyroidectomy) or approaches (e.g. transoral, facelift, gasless transaxillary, retroauricolar, robotic‐assisted breast‐axillo insufflation thyroidectomy) hold significantly different conversion rates. Defining such risk of conversion appears pivotal, as the need for a neck incision for controlling the surgical field, despite not hindering the procedure outcomes, nullifies the major advantage of RATS, that is, the scarless or near‐scarless approach. 10
This systematic review and meta‐analysis aims at delineating the risk of conversion in RATS and assessing whether specific subclasses of procedures or accesses should be regarded at higher risk.
2. METHODS
This review was registered in the International Prospective Register of Systematic Reviews under the number CRD42021277928.
2.1. Search strategy
A systematic review and meta‐analysis was conducted between 12 September 2021, and 20 January 2022, according to the Preferred Reporting Items for Systematic Reviews and Meta‐analyses reporting guidelines. 11 We completed systematic electronic searches for studies written in English, Italian, German, French, or Spanish published until the search date that reported original data obtained from humans and focussed entirely or partly on RATS in humans.
On 23 September 2021, we searched MEDLINE, Embase, Web of Science, Scopus, Cochrane Library, and http://ClinicalTrials.gov databases using wide search strategies for thyroid‐, thyroid surgery‐, and robot‐related terms. The detailed search strategy with the number of unique items retrieved from each database is available in Table 1.
TABLE 1.
Databases, keys, and number of unique results for the initial search
| Database | Key | Results |
|---|---|---|
| Cochrane library | (Thyroid OR thyroidectomy OR hemithyroidectomy) AND (robot OR robotic OR robot‐assisted OR ‘robot assisted’) in all text ‐ (word variations have been searched) | 69 |
| Medline | (Thyroid OR thyroidectomy OR hemithyroidectomy) AND (robot OR robotic OR robot‐assisted OR ‘robot assisted’) | 720 |
| Clinicaltrials.gov | (Thyroid OR thyroidectomy OR hemithyroidectomy) AND (robot OR robotic OR robot‐assisted OR ‘robot assisted’) | 20 |
| Scopus | TITLE‐ABS‐KEY ((thyroid OR thyroidectomy OR hemithyroidectomy) AND (robot OR robotic OR ‘robot AND assisted’)) | 540 |
| Embase | (thyroid:ti,ab, kw OR thyroidectomy:ti,ab, kw OR hemithyroidectomy:ti,ab,kw) AND (robot:ti,ab, kw OR robotic:ti,ab, kw OR ‘robot assisted’:ti,ab,kw) | 826 |
| Web of science | (Thyroid OR thyroidectomy OR hemithyroidectomy) AND (robot OR robotic OR robot‐assisted OR ‘robot assisted’) (topic) | 782 |
We included any study dealing with RATS in humans. We excluded cadaver studies, meta‐analyses, systematic and narrative reviews, and case reports, though references from review articles were hand‐checked for additional potentially relevant studies. No minimum study population was required. We included only prospective studies that explicitly reported conversion rates (even if nil) and specified the robotic technique of choice and the type of thyroid surgeries that had been performed.
Abstracts and full texts were reviewed in duplicate by different authors (B.M. and L.N.). To maximise the rate of inclusivity in the early stages of the review, at the abstract stage, we included all studies deemed eligible by at least one rater. Then, during the full‐text review stage, disagreements were resolved by consensus between raters.
2.2. Patient/population, intervention, comparison, outcomes, timing, studies (PICOTS) criteria
The Patient/population, intervention, comparison, outcomes, timing, studies (PICOTS) criteria for the present review were as follows:
- P
patients with thyroid disease candidate to RATS
- I
RATS
- C
comparison between different typologies of available robot‐assisted approaches and thyroid surgeries (total thyroidectomy, subtotal thyroidectomy, hemithyroidectomy, completion thyroidectomy)
- O
RATS conversion rate into open surgery
- T
intraoperative events only
- S
all prospective original studies except case reports
3.
For each included article, we recorded study type, country of origin, number of RATS cases, overall number of patients included in the study, RATS patients' female to male ratio and age, thyroid and nodule size, and body mass index ,BMI criteria for eligibility to RATS, final histology, number of RATS procedure according to typology of thyroid surgery, number and type of neck dissections during RATS, number of procedures according to RATS access type, number of conversion and details on converted procedures, and conversion rate with other closed techniques (where available).
Selected studies were assessed for both quality and methodological bias according to the National Heart, Lung, and Blood Institute Study Quality Assessment Tools (NHI‐SQAT). 12 Articles were rated in duplicate by two authors (B.M. and L.N), with disagreements resolved by consensus. Items were rated as good if they fulfiled at least 80% of the items required by the NHI‐SQAT, fair if they fulfiled between 50% and 80% of the items, and poor if they fulfiled less than 50% of the items, respectively.
Also, the level of evidence was scored according to the Oxford Centre for Evidence‐based Medicine (OCEBM) level of evidence guide. 13 For clinical trials, bias was assessed with the revised Cochrane risk of bias tool for randomized trials. 14
Articles rated as being of fair or good quality according to the NHI‐SQAT were selected for meta‐analysis. The pooled frequency of conversion to open surgery with 95% confidence intervals was assessed using a Der Simonian ‐ Laird random‐effects model. Conversion rates were also compared according to the robotic access used and the type of thyroid surgery being performed via the ANOVA‐Q test, again in a random‐effects model. The between‐study heterogeneity was assessed by Cochran's Q and I2 statistics. Publication bias was assessed graphically via the funnel plot method and Egger's and Begg's test.
All search results, abstract and article selection, data extraction, and descriptive statistics were performed with the Google Sheets web application (Google LLC, Mountain View, CA, USA). The meta‐analysis was performed using the freeware software Openmeta [Analyst] (built 12/3/2013; Brown University, Providence, RI, USA) and Prometa (version 3.0; IDoStatistics, Italy).
4. RESULTS
4.1. Search results
Among the 1356 unique research items initially identified, a total of 184 articles were selected to undergo full‐text evaluation. Ultimately, 13 studies published between 2010 and 2019 were retained for further analysis (see Figure 1).
FIGURE 1.
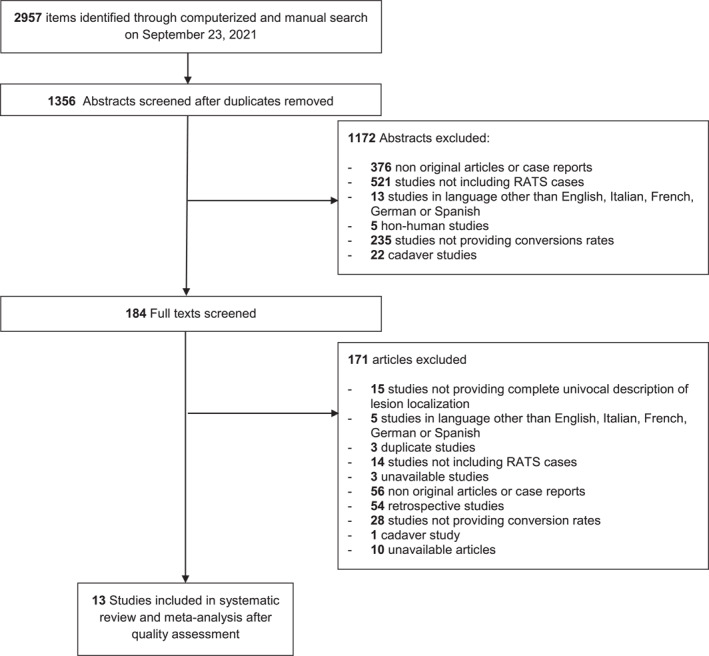
PRISMA‐style flow chart of selection of studies throughout the systematic review and meta‐analysis
Table 2 reports the characteristics and demographics of the included studies. 11 articles were prospective cohort studies, 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 one was a prospective case‐control study 26 and one was a randomized controlled trial, RCT. 27 Four studies were performed in Europe (Great Britain, Greece, Italy, and Romania), four in the United States of America, and five in Asia (China, n = 2, and South Korea, n = 3). All studies were rated as level 2 studies according to the OCEBM scale. According to the NHI‐SQAT, seven articles were rated as good‐quality studies, six articles were rated as fair‐quality studies, and no articles were rated as poor‐quality studies. Most articles lacked ample information to support the comparability of patients. No other significant biases were identified. For the single randomized trial, analysis via the Cochrane tool suggested a high risk of bias in the randomisation process and some concerns in deviation from intended interventions and low risk of bias in all other domains, with some concerns in the overall risk of bias of the study.
TABLE 2.
Characteristics and demographics of the included Studies
| Study | Article‐type | Country of origin | OCEBM rating | NHI‐SQAT rating | No. Of procedures | Female to male ratio for RATS group | Age for RATS group (years) | Eligibility criteria for RATS | ||
|---|---|---|---|---|---|---|---|---|---|---|
| RATS procedures | Total procedures | Nodule/gland characteristics | BMI (kg/m2) | |||||||
| Arora et al, 2016 26 | PCCS | GB | 2 | G | 16 | 32 | 15:1 | 42 ± 10.8 | Solitary nodule< 6 cm | n/a |
| Axente et al, 2013 15 | PCS | Romania | 2 | F | 50 | 50 | 49:1 | 47.5 ± 15.24 | Uni‐ or bilateral nodules <6 cm and no suspicion of malignancy | n/a |
| Chai et al, 2016 16 | PCS | South Korea | 2 | F | 27 | 54 | 27:1 | 36.0 ± 8.3 | n/a | n/a |
| Duke et al, 2016 17 | PCS | USA | 2 | G | 90 | 102 | 89:1 | 41.9 ± 13.1 | Largest nodule ≤4 cm. | <30 |
| He et al, 2016 27 | RCT | China | 2 | F | 50 | 100 | 41:9 | 40.9 ± 9.8 | Intrathyroidal papillary carcinoma <10 mm, lobe volume <40 ml | <30 |
| Kandil et al, 2011> 18 | PCS | USA | 2 | F | 5 | 5 | 3:2 | 36.2 ± 5.56 | n/a | n/a |
| Kandil et al, 2014 19 | PCS | USA | 2 | G | 12 | 12 | 12:0 | 45 ± 4.43 | Nodule <4 cm | <30 |
| Kim et al, 2015 20 | PCS | South Korea | 2 | G | 10 | 10 | 10:0 | 35.1 ± 9.6 | n/a | n/a |
| Kiriakopoulos and linos, 2012 21 | PCS | Greece | 2 | F | 8 | 12 | 6:2 | 38.8 ± 8.9 | Nodules <5 cm | <30 |
| Lang and chow, 2010 22 | PCS | China | 2 | G | 7 | 46 | 7:0 | Median 43.4, range 20.2–54.7 | Dominant nodule <4 cm in benign cases and <2 cm in potentially malignant cases | n/a |
| Lee et al, 2015 23 | PCS | South Korea | 2 | G | 76 | 280 | 62:14 | 43.6 ± 11.8 | n/a | n/a |
| Prete et al, 2019 24 | PCS | Italy | 2 | G | 12 | 12 | 12:0 | Mean 44.9, range 31–63 | Nodules <5 cm (<1 cm if suspect for differentiated ca), lobe <7 cm | <30 |
| Rodriguez et al, 2011 25 | PCS | USA | 2 | F | 35 | 35 | 30:5 | Mean 42.15, range 3–79, median 37 | n/a | n/a |
Note: Age is reported as mean ± standard deviation unless otherwise stated.
Abbreviations: BMI, body mass index.; F, fair; G, good; lung, and blood institute study quality assessment tools; NHI‐SQAT, national heart; OCEBM, Oxford centre for evidence‐based medicine; PCCS, prospective case‐control study; PCS, prospective cohort study; RATS, robot‐assisted thyroid surgery; RCT, randomized controlled trial; SD, standard deviation.
The 13 included studies reported 398 RATS procedures on individual patients out of a total of 750 procedures. There was a clear female prevalence across studies (363 female patients and 35 male patients were included in the studies), with female sex being an explicit inclusion criterion in 2 studies. RATS patients were on average in their third or fourth decade in all studies. Nine studies provided variable nodular or glandular dimensional criteria for eligibility to RATS, while a BMI lower than 30 kg/m2 was an eligibility criterion for RATS in 5 studies.
Two hundred 45 RATS procedures were total thyroidectomies, 138 were hemithyroidectomies and 15 were subtotal thyroidectomies. 89 patients underwent concomitant robot‐assisted central compartment neck dissection (ND), while no lateral compartment dissection was performed. In 87 patients a bilateral axillo‐breast access (BABA) was used, in 102 patients a retroauricular facelift approach (RFA) was used and in 209 a transaxillary gasless approach (TGA) was used. Each study employed a specific RATS approach and no intra‐study comparison for RATS approaches was available. Two studies 15 , 25 reported a total of 4 conversions into open procedures, all occurring during TGA total thyroidectomies. One conversion was due to excessive bleeding in a female patient, another one was due to unexpected high glandular volume (multinodular goitre) and two were due to previously undetected significant tumour extension (specifically, a papillary cancer invading the cricothyroid area and a follicular carcinoma with cranial extension). All converted procedures were completed via a midline neck incision and without any further complication. Data on procedures, approaches, and conversion rates are reported in Table 3.
TABLE 3.
Data on procedures, approaches, and conversion rates of the included studies
| Study | RATS procedure by type (n) | Associated robot‐assisted ND | RATS procedures by access | Conversion rate | |||||
|---|---|---|---|---|---|---|---|---|---|
| TT | HT | ST | CND | LND | BABA | RFA | TGA | ||
| Arora et al, 2016 26 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 0:16 |
| Axente et al, 2013 15 | 9 | 33 | 8 | 0 | 0 | 0 | 0 | 50 | 1:50 |
| Chai et al, 2016 16 | 27 | 0 | 0 | 27 | 0 | 27 | 0 | 0 | 0:27 |
| Duke et al, 2016 17 | 12 | 78 | 0 | 1 | 0 | 0 | 90 | 0 | 0:90 |
| He et al, 2016 27 | 50 | 0 | 0 | 50 | 0 | 50 | 0 | 0 | 0:50 |
| Kandil et al, 2011 18 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 5 | 0:5 |
| Kandil et al, 2014 19 | 2 | 10 | 0 | 0 | 0 | 0 | 12 | 0 | 0:12 |
| Kim et al, 2015 20 | 9 | 1 | 0 | 9 | 0 | 10 | 0 | 0 | 0:10 |
| Kiriakopoulos and linos, 2012 21 | 3 | 3 | 2 | 1 | 0 | 0 | 0 | 8 | 0:8 |
| Lang and chow, 2010 22 | 4 | 3 | 0 | 1 | 0 | 0 | 0 | 7 | 0:7 |
| Lee et al, 2015 23 | 76 | 0 | 0 | 0 | 0 | 0 | 0 | 76 | 0:76 |
| Prete et al, 2019 24 | 2 | 10 | 0 | 0 | 0 | 0 | 0 | 12 | 0:12 |
| Rodriguez et al, 2011 25 | 35 | 0 | 0 | 0 | 0 | 0 | 0 | 35 | 3:35 |
Abbreviations: BABA, bilateral axillo‐breast approach; CND, central ND; HT, hemithyroidectomy; LND, lateral ND; ND, neck dissection; RATS, robot‐assisted thyroid surgery; RFA, retroauricolar facelift approach; ST, subtotal thyroidectomy; TGA, transaxillary gasless approach; TT, total thyroidectomy.
RATS was compared with open approaches in 4 studies and with endoscopic thyroidectomy in two studies. A single conversion from endoscopic to open was reported over 43 overall endoscopic procedures.
Final histology reports for included patients are reported in Table 4.
TABLE 4.
Final histological diagnoses in the reviewed articles
| Study | Final histologic diagnoses | |
|---|---|---|
| Benign | Malignant | |
| Arora et al, 2016 26 | Multinodular goitre (n = 3), follicular adenoma within multinodular goitre (n = 2), thyroid cyst (n = 1), dominant nodule in goitre (n = 1), colloid nodule (n = 2) | Papillary cancer (n = 2), papillary microcarcinoma (n = 1), papillary carcinoma within goitre (n = 1) |
| Axente et al, 2013 15 | Multinodular goitre (n = 25), follicular adenoma (n = 13), toxic adenoma (n = 2), hurtle cell adenoma (n = 2), graves' disease (n = 2), papillary adenoma (n = 2), nodular autoimmune thyroiditis (n = 3), diffuse goitre (n = 1) | Papillary cancer (n = 2) |
| Chai et al, 2016 16 | None | Malignant (papillary) n = 27 |
| Duke et al, 2016 17 | Adenoma (n = 29), multi‐nodular goitre (n = 39), toxic adenoma (n = 1), thyroid cyst (n = 1), no pathologic findings (n = 3) | Papillary carcinoma (n = 21) papillary microcarcinoma (n = 5), follicular carcinoma (n = 4), sclerosing mucoepidermoid carcinoma (n = 1). |
| He et al, 2016 27 | None | Papillary microcarcinoma (n = 50) |
| Kandil et al, 2011 18 | Graves' disease (n = 5) | None |
| Kandil et al, 2014 19 | Hyperplasia (n = 7), hashimoto thyroiditis (n = 2) | Follicular carcinoma (n = 2), papillary carcinoma (n = 1) |
| Kim et al, 2015 20 | Nodular hyperplasia (n = 1) | Papillary carcinoma (n = 9) |
| Kiriakopoulos and linos, 2012 21 | Toxic adenoma (n = 3), multinodular goitre (n = 2) | Papillary carcinoma (n = 3) |
| Lang and chow, 2010 22 | Nodular hyperplasia (n = 6) | Papillary carcinoma (n = 1) |
| Lee et al, 2015 23 | None | Unspecified malignant histology (n = 76) |
| Prete et al, 2019 24 | Unspecified benign histology (n = 7) | Papillary microcarcinoma (n = 5) |
| Rodriguez et al, 2011 25 | Unspecified benign histology (n = 12) | Follicular carcinoma (n = 19), hurtle cell carcinoma (n = 1), papillary carcinoma (n = 3) |
All articles of fair or good quality according to the NHI‐SQAT were included as no significant methodological bias emerged, therefore all 13 articles were included in the final meta‐analysis.
The funnel plot method and Begg's test suggested the presence of some degree of publication bias in the published literature (p = 0.458), while no significant heterogeneity was observed between studies (Cochran's Q p = 0.932; I2 = 0%). The pooled conversion rate for patients undergoing RATS was 1% (95% confidence interval, 0.1%–2%) (see Figure 2), with an effect size of 0.06 (95% confidence interval, 0.03–0.1). As the ANOVA‐Q test failed to show significant differences when comparing patients for the type of thyroid surgery performed or robotic access used (respectively p = 0.766 and p = 0.457), no subgroup analyses were performed.
FIGURE 2.
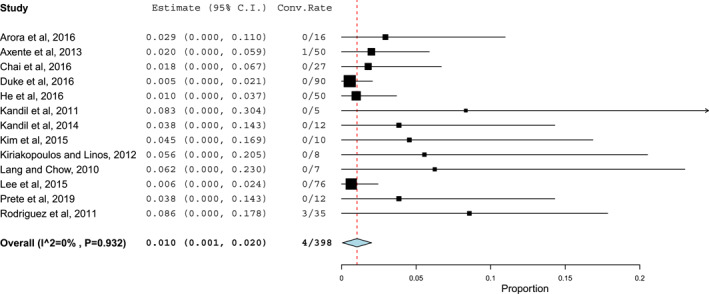
The pooled conversion rate in patients undergoing robot‐assisted thyroid surgery (RATS). Effects and summaries were calculated using a random‐effect model weighted by the study population
Due to the low numbers of endoscopic procedures provided as a comparison in the reviewed articles, a meta‐analytic comparison between different minimally invasive thyroidectomies choices was deemed too biased to provide adequate supporting clinical evidence. Analogously, the heterogeneity and reporting inconsistency in patient selection criteria prevented a targeted meta‐analytic subgroup comparison.
5. DISCUSSION
To the authors' knowledge, this is the first systematic review to address specifically the risk of RATS conversion into open‐neck procedures. Despite the small effect size, we found that the conversion rate is consistent between different studies and with the 1% pooled rate emerging from our meta‐analysis. This issue, intrinsic to all minimally invasive procedures irrespective of the surgical site, has not been addressed by already published review works, either because they were focussed on other safety features 28 or because they simply explored the differences between robotic and open procedures, the latter being unaffected per se by conversions. 29 , 30 Analogously, the same risk has not been specifically assessed also for endoscopic thyroidectomies procedures, with review works and meta‐analytic comparison focussing again on different aspects of the surgical procedures and other patient outcomes. 31 , 32
The 1% conversion rate stemmed from four different events during TGA total thyroidectomies reported in two studies from different groups. 15 , 25 These data were recovered from a set of 398 robot‐assisted procedures in 13 average‐to‐good methodological quality small‐scale prospective studies. Despite the good evidence level and methodological consistency, the relatively small scale of studies determined a moderate degree of publication bias, which should be hopefully covered by future larger‐scale studies. The procedures taken into account cover most types of thyroid surgery types (ST, HT, and TT, with a clear predominance of the last, accounting for 62% of procedures), with or without ND, performed with three distinct access types (BABA, RFA, and TGA, the last accounting alone for 53% of procedures). If we examine the four conversion events, it's interesting to observe that a more thorough preoperative planning potentially could avoid the three events due to unexpectedly relevant tumour extension or goitre volume, while the bleeding event remains unforeseeable. Though these data are still scarce, careful preoperative imaging, especially in case of malignancy or high volume goitres, might be beneficial on the conversion rates.
Given the huge impact of the scarless or near‐scarless approach of RATS on patients' surgical preferences, a clearer definition of conversion risks is of the utmost importance for informed consent purposes. This systematic review allows for a more data‐driven patient consent going beyond single‐study results, which show a significant variation in conversion rates, especially in retrospective case series. Even if we take into account that several high‐volume centres have considerable experience in RATS, it still comes as surprising to see conversions raising from 0% in three case series with n > 500 8 , 33 , 34 to 16.6–33.3% in small, either preliminary or non‐thyroid‐specific, case series with n < 10. 9 , 35
Even if we take into account the experience of high‐volume tertiary centres or the pilot experience on specific accesses or high‐risk patient classes, the mere existence of such a considerable gap in reported conversion rates claims the possibility of a reporting bias. On the basis of this potential bias, this meta‐analysis was based only on prospective studies, thus allowing for a higher level of evidence and also for avoiding duplicated results that may be generated by partially overlapping case series presented in different articles or multi‐centre studies.
On the other hand, the small number of prospective studies available in the literature and their relatively small sample sizes prevented us from drawing conclusions on the potential differential risk between different types of RATS procedures or accesses. Although TT might indeed hold a higher conversion risk than HT, being thyroidectomy and TGA respectively the most common procedure and access in this meta‐analysis, it's not surprising that all conversion cases belong to these groups. Analogously, the sample size is too small to draw any reliable comparison with the conversion rate for endoscopic procedures and the allocation bias to RATS versus endoscopy‐assisted procedures or open procedures might be considerable, as the single RCT included demonstrates. Furthermore, the relatively small size of included studies determines a more considerable publication bias. Nevertheless, these biases were considered too low to hinder the overall value of our conclusions. Another limitation of this meta‐analysis stems from the heterogeneity of RATS eligibility criteria in terms of nodule/thyroid volume and the inconstant reporting of BMI criteria, which do not allow to draw any conclusion on which thyroid‐ and patient‐specific characteristics determine a higher risk of conversion. Last, databases searches didn't locate any eligible stud reporting conversion rates for transoral robotic thyroidectomy (TORT), so this approach was not covered in our analysis or included in any subgroup evaluation. Nevertheless, a recent wide retrospective multicentric review suggested TORT has similar conversion rates as those emerging from our systematic review, around 0.7%. 36
6. CONCLUSION
By providing a novel insight on the conversion risk in RATS, this meta‐analysis calls nevertheless for greater attention to this often neglected surgical adverse event. Only routine implementation of a common and unbiased reporting system into prospective multicentric studies might allow for better defining patient groups, RATS procedures, and accesses at higher conversion risk, and providing a sounder risk assessment. Irrespective of future studies, the conversion risk should be adequately discussed with patients in everyday practice, given its impact on the secondary outcomes of RATS. Even if aggregate conversion rates are low, an average 1% risk of neck scar is worth exploring with patients who mostly see RATS as the scarless answer to their thyroid disease.
CONFLICT OF INTEREST
The authors have no potential conflict of interest or financial disclosures pertaining to this article.
ACKNOWLEDGMENTS
The authors received no financial support for the research, authorship, and/or publication of this article.
Open Access Funding provided by Universita degli Studi di Milano within the CRUI‐CARE Agreement.
Martino B, Nitro L, De Pasquale L, et al. Conversion rates in robotic thyroid surgery: A systematic review and meta‐analysis. Int J Med Robot. 2022;18(5):e2427. 10.1002/rcs.2427
Barbara Martino and Letizia Nitro contributed equally to this manuscript
Giovanni Felisati and Alberto Maria Saibene contributed equally to this manuscript
DATA AVAILABILITY STATEMENT
All data pertaining to this meta‐analysis are available from the authors upon reasonable request.
REFERENCES
- 1. Guerra F, Giuliani G, Coletta D. The risk of conversion in minimally invasive oncological abdominal surgery. Meta‐analysis of randomized evidence comparing traditional laparoscopic versus robot‐assisted techniques. Langenbecks Arch Surg. 2021;406(3):607‐612. 10.1007/s00423-021-02106-y [DOI] [PubMed] [Google Scholar]
- 2. Chen SH, Li ZA, Huang R, Xue HQ. Robot‐assisted versus conventional laparoscopic surgery for endometrial cancer staging: a meta‐analysis. Taiwan J Obstet Gynecol. 2016;55(4):488‐494. 10.1016/j.tjog.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 3. Hu J, Chen Y, Dai J, et al. Perioperative outcomes of robot‐assisted vs video‐assisted and traditional open thoracic surgery for lung cancer: a systematic review and network meta‐analysis. Int J Med Robot. 2020;16(5):1‐14. 10.1002/rcs.2123 [DOI] [PubMed] [Google Scholar]
- 4. Lobe TE, Wright SK, Irish MS. Novel uses of surgical robotics in head and neck surgery. J Laparoendosc Adv Surg Tech. 2005;15(6):647‐652. 10.1089/lap.2005.15.647 [DOI] [PubMed] [Google Scholar]
- 5. Piccoli M, Mullineris B, Gozzo D, et al. Evolution strategies in transaxillary robotic thyroidectomy: considerations on the first 449 cases performed. J Laparoendosc Adv Surg Tech. 2019;29(4):433‐440. 10.1089/lap.2019.0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Materazzi G, Fregoli L, Papini P, Bakkar S, Vasquez MC, Miccoli P. Robot‐assisted transaxillary thyroidectomy (RATT): a series appraisal of more than 250 cases from Europe. World J Surg. 2018;42(4):1018‐1023. 10.1007/s00268-017-4213-2 [DOI] [PubMed] [Google Scholar]
- 7. Kandil EH, Noureldine SI, Yao L, Slakey DP. Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg. 2012;214(4):558‐564. discussion 564‐66. [DOI] [PubMed] [Google Scholar]
- 8. Lee J, Yun JH, Nam KH, Choi UJ, Chung WY, Soh EY. Perioperative clinical outcomes after robotic thyroidectomy for thyroid carcinoma: a multicenter study. Surg Endosc. 2011;25(3):906‐912. 10.1007/s00464-010-1296-3 [DOI] [PubMed] [Google Scholar]
- 9. Tunca F, Dural AC, Sahbaz NA, et al. Pure transoral robotic thyroidectomy; institutional adaptation and early results from a tertiary endocrine surgery centre. Int J Med Robot. 2020;16(6):1‐8. 10.1002/rcs.2151 [DOI] [PubMed] [Google Scholar]
- 10. Qiu TY, Lau J, Wong O, et al. Preoperative scar perception study comparing “scarless” in the neck endoscopic thyroidectomy with open thyroidectomy: a cross‐sectional study. Ann R Coll Surg Engl. 2020;102(9):737‐743. 10.1308/rcsann.2020.0174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Heart, Lung, and Blood Institute (NHLBI) . Study Quality Assessment Tools. https://www.nhlbi.nih.gov/health‐topics/study‐quality‐assessment‐tools. accessed December 14, 2021. [Google Scholar]
- 13. Oxford Centre for Evidence‐Based Medicine. The Oxford Levels of Evidence 2. https://www.cebm.net/index.aspx?o=5653. accessed December 14, 2021. [Google Scholar]
- 14. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 15. Axente DD, Silaghi H, Silaghi CA, Major ZZ, Micu CM, Constantea NA. Operative outcomes of robot‐assisted transaxillary thyroid surgery for benign thyroid disease: early experience in 50 patients. Langenbecks Arch Surg. 2013;398(6):887‐894. 10.1007/s00423-013-1085-2 [DOI] [PubMed] [Google Scholar]
- 16. Chai YJ, Song J, Kang J, et al. A comparative study of postoperative pain for open thyroidectomy versus bilateral axillo‐breast approach robotic thyroidectomy using a self‐reporting application for iPad. Annals of Surgical Treatment and Research. 2016;90(5):239. 10.4174/astr.2016.90.5.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Duke WS, Holsinger FC, Kandil E, Richmon JD, Singer MC, Terris DJ. Remote access robotic facelift thyroidectomy: a multi‐institutional experience. World J Surg. 2017;41(1):116‐121. 10.1007/s00268-016-3738-0 [DOI] [PubMed] [Google Scholar]
- 18. Kandil E, Noureldine S, Abdel Khalek M, et al. Initial experience using robot‐ assisted transaxillary thyroidectomy for Graves’ disease. J Vis Surg. 2011;148(6):e447‐51. 10.1016/j.jviscsurg.2011.10.002 [DOI] [PubMed] [Google Scholar]
- 19. Kandil E, Saeed A, Mohamed SE, Alsaleh N, Aslam R, Moulthrop T. Modified robotic‐assisted thyroidectomy: an initial experience with the retroauricular approach. Laryngoscope. 2015;125(3):767‐771. 10.1002/lary.24786 [DOI] [PubMed] [Google Scholar]
- 20. Kim SJ, Lee KE, Oh BM, et al. Intraoperative neuromonitoring of the external branch of the superior laryngeal nerve during robotic thyroid surgery: a preliminary prospective study. Ann Surg Treat Res. 2015;89(5):233‐239. 10.4174/astr.2015.89.5.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kiriakopoulos A, Linos D. Gasless transaxillary robotic versus endoscopic thyroidectomy: exploring the frontiers of scarless thyroidectomy through a preliminary comparison study. Surg Endosc. 2012;26(10):2797‐2801. 10.1007/s00464-012-2281-9 [DOI] [PubMed] [Google Scholar]
- 22. Lang BHH, Chow MP. A comparison of surgical outcomes between endoscopic and robotically assisted thyroidectomy: the authors’ initial experience. Surg Endosc. 2011;25(5):1617‐1623. 10.1007/s00464-010-1450-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee DY, Lim S, Kang SH, et al. A prospective 1‐year comparative study of transaxillary total thyroidectomy regarding functional outcomes: is it really promising? Surg Endosc. 2016;30(4):1599‐1606. 10.1007/s00464-015-4386-4 [DOI] [PubMed] [Google Scholar]
- 24. Prete FP, Marzaioli R, Lattarulo S, et al. Transaxillary robotic‐assisted thyroid surgery: technique and results of a preliminary experience on the Da Vinci Xi platform. BMC Surg. 2019;18(Suppl 1):19. 10.1186/s12893-019-0473-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodriguez FNS, Low RA, Singer JA, et al. A new technique for robotic thyroidectomy: “the daVinci gasless single‐incision axillary approach. J Robot Surg. 2011;5(3):157‐162. 10.1007/s11701-010-0220-0 [DOI] [PubMed] [Google Scholar]
- 26. Arora A, Garas G, Sharma S, et al. Comparing transaxillary robotic thyroidectomy with conventional surgery in a UK population: a case control study. Int J Surg. 2016;27:110‐117. 10.1016/j.ijsu.2016.01.071 [DOI] [PubMed] [Google Scholar]
- 27. He QQ, Zhu J, Zhuang DY, et al. Comparative study between robotic total thyroidectomy with central lymph node dissection via bilateral axillo‐breast approach and conventional open procedure for papillary thyroid microcarcinoma. Chin Med J. 2016;129(18):2160‐2166. 10.4103/0366-6999.189911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jackson NR, Yao L, Tufano RP, Kandil EH. Safety of robotic thyroidectomy approaches: meta‐analysis and systematic review. Head Neck. 2014;36(1):137‐143. 10.1002/hed.23223 [DOI] [PubMed] [Google Scholar]
- 29. Xing Z, Qiu Y, Abuduwaili M, et al. Surgical outcomes of different approaches in robotic assisted thyroidectomy for thyroid cancer: a systematic review and Bayesian network meta‐analysis. Int J Surg. 2021;89:105941. 10.1016/j.ijsu.2021.105941 [DOI] [PubMed] [Google Scholar]
- 30. Liu H, Wang Y, Wu C, Fei W, Luo E. Robotic surgery versus open surgery for thyroid neoplasms: a systematic review and meta‐analysis. J Cancer Res Clin Oncol. 2020;146(12):3297‐3312. 10.1007/s00432-020-03418-0 [DOI] [PubMed] [Google Scholar]
- 31. Wang Y, Zhou S, Liu X, et al. Transoral endoscopic thyroidectomy vestibular approach vs conventional open thyroidectomy: meta‐analysis. Head Neck. 2021;43(1):345‐353. 10.1002/hed.26486 [DOI] [PubMed] [Google Scholar]
- 32. Jiang WJ, Yan PJ, Zhao CL, et al. Comparison of total endoscopic thyroidectomy with conventional open thyroidectomy for treatment of papillary thyroid cancer: a systematic review and meta‐analysis. Surg Endosc. 2020;34(5):1891‐1903. 10.1007/s00464-019-07283-y [DOI] [PubMed] [Google Scholar]
- 33. Lee S, Ryu HR, Park JH, et al. Excellence in robotic thyroid surgery: a comparative study of robot‐assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg. 2011;253(6):1060‐1066. 10.1097/sla.0b013e3182138b54 [DOI] [PubMed] [Google Scholar]
- 34. Choi JY, Bae IE, Kim HS, et al. Comparative study of bilateral axillo‐breast approach endoscopic and robotic thyroidectomy: propensity score matching analysis of large multi‐institutional data. Annals of Surgical Treatment and Research. 2020;98(6):307. 10.4174/astr.2020.98.6.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Alimoglu O, Sagiroglu J, Atak I, et al. Robot‐assisted laparoscopic (RAL) procedures in general surgery. Int J Med Robot. 2016;12(3):427‐430. 10.1002/rcs.1706 [DOI] [PubMed] [Google Scholar]
- 36. Lira RB, De Cicco R, Rangel LG, et al. Transoral endoscopic thyroidectomy vestibular approach: experience from a multicenter national group with 412 patients. Head Neck. 2021;43(11):3468‐3475. 10.1002/hed.26846 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data pertaining to this meta‐analysis are available from the authors upon reasonable request.


