Summary
Background
Information is limited for the benefits of physical activity (PA) in preschoolers. Previous research using accelerometer‐assessed PA may be affected for multicollinearity issues.
Objectives
This study investigated the cross‐sectional and prospective associations of sedentary behaviour (SB) and PA with body composition and physical fitness using compositional data analysis.
Methods
Baseline PA and SB were collected in 4‐year‐old (n = 315) using wrist‐worn GT3X+ during seven 24 h‐periods. Body composition (air‐displacement plethysmography) and physical fitness (PREFIT test battery) were assessed at baseline and at the 12‐month follow‐up.
Results
Increasing vigorous PA at expenses of lower‐intensity behaviours for 4‐year‐old was associated with body composition and physical fitness at cross‐sectional and longitudinal levels. For example, reallocating 15 min/day from lower intensities to vigorous PA at baseline was associated with higher fat‐free mass index (+0.45 kg/m2, 95% confidence intervals [CI]: 0.18–0.72 kg/m2), higher upper‐body strength (+0.6 kg, 95% CI: 0.1–1.19 kg), higher lower‐body strength (+8 cm, 95% CI: 3–13 cm), and shorter time in completing the motor fitness test (−0.4 s, 95% CI: −0.82 to [−0.01] s) at the 12‐month follow‐up. Pairwise reallocations of time indicated that the behaviour replaced was not relevant, as long as vigorous PA was increased.
Conclusions
More time in vigorous PA may imply short‐ and long‐term benefits on body composition and physical fitness in preschoolers. These findings using compositional data analysis corroborate our previously published results using isotemporal substitution models.
Keywords: fitness tracker, movement behaviour, movement sensor, sedentary time, youth
1. INTRODUCTION
Physical activity (PA) is widely known to produce health benefits across the lifespan. 1 However, information is limited in several populations, including preschoolers (i.e., 3–5 years old). 2 , 3 In this population, body composition and physical fitness (hereinafter fitness) are markers of current and future health, 4 , 5 but the role of PA in promoting healthy body composition and fitness is still unclear.
Accelerometers are valid and feasible to monitor PA in 3–5‐year‐old children. 6 , 7 Previous studies described cross‐sectional 8 , 9 , 10 , 11 , 12 and longitudinal 13 , 14 , 15 , 16 associations of device‐measured PA with body composition and fitness in preschoolers. For example, from MINISTOP (a population‐based randomized controlled trial to promote PA and diet among 315 Swedish preschoolers), we demonstrated cross‐sectional and longitudinal positive associations of vigorous PA with fat‐free mass index (FFMI), cardiorespiratory, muscular and motor fitness in preschoolers. 12 , 16 However, there has been a concern that multicollinearity issues may bias previous findings, 3 , 17 which were obtained from linear regression and isotemporal substitution models. Accelerometer‐assessed sedentary behaviour (SB), light, moderate and vigorous PA share the awake time of the day, which increases the multicollinearity risk in regression models. 18 Isotemporal substitution models have traditionally been used to investigate time reallocations across behaviours, 19 yet these models may be also affected by multicollinearity.
Compositional data analysis has been proposed instead to properly investigate the reallocation of time across behaviours while lowering risk of multicollinearity. 20 , 21 Therefore, this study aimed to re‐analyse the MINISTOP data to investigate whether the previously described associations of PA with body composition and fitness in preschoolers are corroborated by compositional models.
2. MATERIAL AND METHODS
2.1. Study design and participants
This study includes baseline and 12‐month follow‐up data from the MINISTOP trial. 22 , 23 Children were ~4 years old (4.48 ± 0.15 years) at baseline. For this study, we analysed the baseline data of all participants for the cross‐sectional associations (n = 315), and only the control group data for the longitudinal associations (n = 159) to eliminate any possible confounding introduced by the intervention. Children without sufficient accelerometer data (n = 8), or without complete follow‐up data (n = 13), were excluded from analyses. Informed consents from parents were obtained. The trial was registered at clinicaltrials.gov (NCT02021786) and approved by the Research Ethics Committee, Stockholm, Sweden (2013/1607–31/5; 2013/2250–32).
2.2. Data collection
PA and SB were monitored with non‐dominant wrist‐worn accelerometers (ActiGraph GT3X+, Pensacola, FL, US) for 7 days (24 h/day). Devices recorded accelerations at 50 Hz, and participants were instructed to only remove accelerometers for water‐based activities. Children wearing accelerometer ≥3 days for ≥10 h/day were considered. Non‐wear time was determined from the raw acceleration; awake and sleep time were detected with an automated algorithm, 24 and then, awake time was classified as SB, light, moderate or vigorous PA. 25 Detailed methods can be found elsewhere. 12
Body composition was assessed using air‐displacement plethysmography (BOD POD GS, Cosmed Company, Italy, www.cosmed.com). 26 Fat mass percentage was calculated using the Lohman's equation (i.e., , where D is density, D fat is assumed to be 0.9000). 27 Absolute fat mass (kg) was obtained from fat mass percentage, and fat‐free mass was the difference between body weight (kg) and fat mass (kg). Body composition outcomes included body mass index (BMI, kg/m2), FFMI (kg/m2), fat mass percentage (%) and fat mass index (kg/m2).
Cardiorespiratory, muscular and motor fitness were assessed with the PREFIT fitness test battery for preschoolers. 28 The 20‐m shuttle run test was used for cardiorespiratory fitness, the handgrip strength test for upper‐body strength, the standing long jump test for lower‐body strength and the 4 × 10‐m shuttle run test for motor fitness. Two attempts were recorded and the best attempt was used, except for the 20‐m shuttle run test that was performed once. 12 , 16
2.3. Statistical methods
Descriptive characteristics of participants regarding sociodemographic and anthropometric values, PA levels, body composition and fitness can be found elsewhere. 12 , 16 Multiple regression models over compositional data were used to study the cross‐sectional and longitudinal associations of PA with body composition and fitness. 20 , 21 Compositional data analysis accounts for the relative nature of accelerometer‐assessed PA by quantifying the effect of increasing a specific behaviour while reducing at least one of the others. Two different time‐use compositions were defined: composition 1 included: SB, light, moderate and vigorous PA; composition 2 included: SB, light and moderate‐to‐vigorous PA. Isometric log‐ratios were calculated as previously proposed 20 and included as explanatory variables. Gamma (γ) coefficients inform of the strength and direction of the association of each behaviour relative to the others with a certain outcome. To estimate the effect size, dose–response curves were drawn by reversing the isometric log ratios. These curves represent the effect of increasing one behaviour while reducing others on the outcome. Model 1 was unadjusted; model 2 was adjusted for sex, age and awake wear time; and model 3 was additionally adjusted for maternal and paternal BMI and as well as their educational attainment (i.e., university degree or not). Analyses were performed in R (v.4.0.3), and statistical significance was set at p < 0.05.
3. RESULTS
3.1. Cross‐sectional associations
Tables S1 and S2 show the models using composition 1 (i.e., SB, light, moderate and vigorous PA) and composition 2 (i.e., SB, light and moderate‐to‐vigorous PA), respectively. Vigorous PA relative to SB and lower PA intensities was associated with FFMI (γ's ≥ 0.275, p's ≤ 0.020), cardiorespiratory fitness (γ's ≥ 1.515, p's < 0.001), lower‐body strength (γ's ≥ 4.502, p's ≤ 0.017) and motor fitness (γ's ≤ −1.238, p's < 0.001) (Table S1). Increasing moderate‐to‐vigorous PA while reducing SB and light PA was associated with FFMI (γ's ≥ 0.850, p's ≤ 0.010), fat mass percentage (γ's ≥ −3.522, p's ≤ 0.026) and all fitness components (cardiorespiratory fitness: γ's ≥ 3.658, p's < 0.001; upper‐body strength: γ's ≥ 1.187, p's ≤ 0.031; lower‐body strength: γ's ≥ 19.718, p's ≤ 0.001; and motor fitness: γ's ≤ −2.528, p's < 0.001) in all models (Table S2). Figure S1 shows the dose–response curves relative to increasing vigorous PA while proportionally decreasing the other behaviours (model 2 was used for illustrative purposes). Figure S2 shows the pairwise reallocations from other behaviours to vigorous PA.
3.2. Prospective associations
The prospective associations of SB and PA (at 4‐year‐old) with body composition and fitness outcomes (at 5‐year‐old) are presented in Tables S3 and S4. Vigorous PA relative to SB and lower PA intensities was associated with BMI (γ's ≥ 0.663, p's ≤ 0.013), FFMI (γ's ≥ 0.588, p's ≤ 0.002), upper‐body strength (γ's ≥ 0.759, p's ≤ 0.050) and lower‐body strength (γ's ≥ 10.940, p's ≤ 0.002) in all models (Table S3). Vigorous PA was associated with motor fitness only in models 1 and 2 (γ's ≤ −0.596, p's ≤ 0.038). Table S4 shows that increasing moderate‐to‐vigorous PA at expenses of SB and light PA was associated with FFMI (γ's ≥ 1.038, p's ≤ 0.040), cardiorespiratory fitness (γ's ≥ 5.195, p's < 0.019), lower‐body strength (γ's ≥ 23.187, p's ≤ 0.013) and motor fitness (γ's ≤ −1.997, p's < 0.012) in all models. Furthermore, Figure 1 shows the dose–response curves relative to increasing vigorous PA while proportionally decreasing SB, light and moderate PA. For example, reallocating 15 min/day from SB, light and moderate PA to vigorous PA was associated with higher FFMI (+0.45 kg/m2, 95% confidence intervals [CI]: 0.18–0.72 kg/m2), upper‐body strength (+0.6, 95% CI: 0.1–1.19 kg), lower‐body strength (+8 cm, 95% CI: 3–13 cm) and motor fitness (−0.4 s, 95% CI: −0.82 to [−0.01] s). Figure S3 shows the prospective associations of pairwise reallocations from lower‐intensity behaviours to vigorous PA.
FIGURE 1.
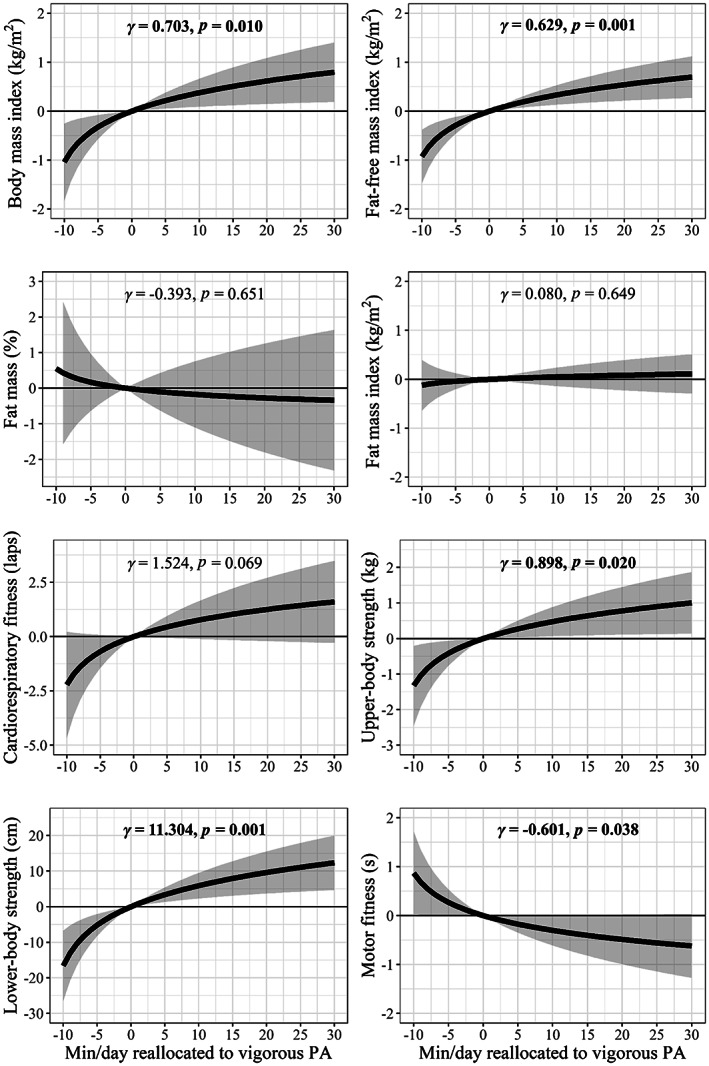
Prospective associations of vigorous physical activity (PA) relative to sedentary behaviour (SB) and lower PA intensities at 4 years with body composition and physical fitness at the 12‐month follow‐up. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light and moderate PA. Models are adjusted for sex, age and awake wear time
4. DISCUSSION
Our findings showed that more time in vigorous PA at expenses of lower intensities (SB, light and moderate PA) were associated with cross‐sectional and prospective benefits on body composition and fitness in preschoolers. This study corroborates our previous observations using linear regression and isotemporal substitution models. Also, interestingly, our time‐use reallocation analyses indicate that it is not relevant which behaviour is replaced, as long as vigorous PA is increased for most of the outcomes studied.
Vigorous PA was cross‐sectionally associated with FFMI and fitness components in the previous study, 12 which is consistent in these analyses. Both studies show that the time in vigorous PA is the main driver of the associations. Increasing vigorous PA at expenses of others may benefit body composition and fitness, independently of which behaviour is replaced. Similar findings were obtained in the prospective associations, that is, consistent findings across multiple regression, 16 isotemporal substitution 16 and compositional data analysis (present study). Previous studies have also found consistent findings across isotemporal substitution models and compositional data analysis, 29 and we hypothesize that this occurs when the associations are mainly driven by one of the behaviours (in this case, vigorous PA). The findings were also robust across models, indicating that the associations are independent of potential confounders.
Altogether, previous literature and this study suggest that increasing vigorous PA is associated with body composition and physical fitness in preschoolers, while the SB‐related findings are inconsistent. 13 , 14 , 30 A potential explanation is that engaging in vigorous PA could be more effective than reducing SB to increase energy expenditure in preschoolers and, subsequently, to improve body composition and physical fitness. Furthermore, the variability of SB, light and moderate PA is rather low in our participants (coefficients of variation of ~0.10, ~0.12 and 0.22, respectively), while the variability of vigorous PA is higher (i.e., ~0.60), suggesting that there is more room to change vigorous PA than the other behaviours. The current World Health Organization PA guidelines recommend 4‐year‐old to perform at least 180 min/day of PA, of which at least 60 minutes should be of moderate‐to‐vigorous intensity. 3 Our findings support such a recommendation and initiate a debate on whether vigorous PA should be specifically encouraged rather than moderate‐to‐vigorous PA in this age group. In this respect, it is relevant to note that our previous qualitative work has shown that preschool teachers and parents perceived that preschoolers engage in too little vigorous PA. 31 Previous research did not utilize a compositional data approach, 13 , 14 , 30 which makes it difficult to isolate the associations of the different intensities with the outcome (i.e., those children engaging in more moderate PA are likely to also engage in more vigorous PA, and this not adjusted for in standard linear regression models). The guidelines also recommend limiting sedentary screen time to no more than 60 min/day. Unfortunately, we do not have an estimate of the specific screen time in our participants. However, our results do support not limiting the total sedentary time for the body composition and the physical fitness in this early stage of life.
These findings are of relevance for public health strategies to prevent childhood obesity and its comorbidities. This study corroborates that spending more time in vigorous PA may imply short‐ and long‐term health benefits already early in life (i.e., preschoolers). Furthermore, we can now conclude that vigorous PA, and not lower intensities, is the main driver of the associations. This implies that it is more relevant to focus on increasing vigorous PA than on reducing SB in this age group. This study has several limitations to acknowledge such the relatively small sample size for the prospective analyses as we excluded participants from the intervention group. Furthermore, this is an observational analysis and causation cannot be concluded. Strengths of this study are the accurate methods used to measure PA, body composition and fitness; the combination of the cross‐sectional and longitudinal design and the use of compositional data analysis to appropriately account for the multicollinearity of accelerometer‐determined PA data.
5. CONCLUSION
More time in vigorous PA was associated with short‐ and long‐term benefits on body composition and fitness in preschoolers, with vigorous PA being the main driver of these associations. Our findings using compositional data analysis corroborate our previously published results using linear regression and isotemporal substitution models.
CONFLICT OF INTEREST
No conflict of interest was declared.
AUTHOR CONTRIBUTIONS
Marie Löf is the Principal Investigator for the MINISTOP trial and designed this analysis together with all the co‐authors. Jairo H. Migueles was responsible for the data analysis and drafted the manuscript. Christine Delisle Nyström was responsible for data collection. Pontus Henriksson assisted on the data analysis and contributed to the manuscript preparation. The manuscript was reviewed by Christine Delisle Nyström, Marja H. Leppänen, Pontus Henriksson and Marie Löf. All the authors approved the final version.
Supporting information
Table S1. Cross‐sectional associations of physical activity (PA) intensities (light, moderate, and vigorous) and SB with body composition and physical fitness at 4 years with compositional data analysis.
Table S2. Cross‐sectional associations of physical activity (PA) intensities (light, and moderate‐to‐vigorous) and SB with body composition and physical fitness at 4 years with compositional data analysis.
Table S3. Prospective associations of associations of physical activity (PA) intensities (light, moderate, and vigorous) and SB at 4 years with body composition and physical fitness at the 12‐month follow up with compositional data analysis.
Table S4. Prospective associations of associations of physical activity (PA) intensities (light, and moderate‐to‐vigorous) and SB at 4 years with body composition and physical fitness at the 12‐month follow up with compositional data analysis.
Figure S1. Cross‐sectional associations of vigorous physical activity (PA) relative to sedentary behavior (SB) and lower PA intensities with body composition and physical fitness at 4 years. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light, and moderate PA. Models are adjusted for sex, age, and awake wear time. Lower values in motor fitness indicate higher performance.
Figure S2. Cross‐sectional effects of pairwise reallocations of time from sedentary behavior (SB), light and moderate physical activity (PA) to vigorous PA on body composition and physical fitness at 4 years. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light, and moderate PA. Models are adjusted for sex, age, and awake wear time. Lower values in motor fitness indicate higher performance.
Figure S3. Prospective effects of pairwise reallocations of time from sedentary behavior (SB), light and moderate physical activity (PA) to vigorous PA at 4 years with body composition and physical fitness at the 12‐month follow‐up. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light, and moderate PA. Models are adjusted for sex, age, and awake wear time. Lower values in motor fitness indicate higher performance.
ACKNOWLEDGEMENTS
The authors thank the participating families as well as Eva Flinke Carlsson, Gunilla Hennermark and Birgitta Jensen, for their help regarding recruitment and data collection. The MINISTOP project was funded by the Swedish Research Council (project no. 2012–2883, Marie Löf), the Swedish Research Council for Health, Working Life and Welfare (2012–0906, Marie Löf; 2021‐00036, Jairo H Migueles), Bo and Vera Axson Johnsons Foundation and Karolinska Institutet (Marie Löf).
Migueles JH, Delisle Nyström C, Leppänen MH, Henriksson P, Löf M. Revisiting the cross‐sectional and prospective association of physical activity with body composition and physical fitness in preschoolers: A compositional data approach. Pediatric Obesity. 2022;17(8):e12909. doi: 10.1111/ijpo.12909
Funding information Bo and Vera Axson Johnsons Foundation; Forskningsrådet om Hälsa, Arbetsliv och Välfärd, Grant/Award Number: 2012‐0906; Karolinska Institutet; Vetenskapsrådet, Grant/Award Number: 2012‐2883
REFERENCES
- 1. Bull F, Saad Al‐Ansari S, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451‐1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carson V, Tremblay MS, Chastin SFM. Cross‐sectional associations between sleep duration, sedentary time, physical activity, and adiposity indicators among Canadian preschool‐aged children using compositional analyses. BMC Public Health. 2017;17:294‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. World Heal Organ. 2019;36:1‐36. https://apps.who.int/iris/handle/10665/311664 [PubMed] [Google Scholar]
- 4. Ayer J, Charakida M, Deanfield JE, Celermajer DS. Lifetime risk: childhood obesity and cardiovascular risk. Eur Heart J. 2015;36:1371‐1376. [DOI] [PubMed] [Google Scholar]
- 5. Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes. 2008;32:1‐11. [DOI] [PubMed] [Google Scholar]
- 6. Butte NF, Wong WW, Lee JS, Adolph AL, Puyau MR, Zakeri IF. Prediction of energy expenditure and physical activity in preschoolers. Med Sci Sports Exerc. 2014;46:1216‐1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roscoe CMP, James RS, Duncan MJ. Calibration of GENEActiv accelerometer wrist cut‐points for the assessment of physical activity intensity of preschool aged children. Eur J Pediatr. 2017;176:1093‐1098. [DOI] [PubMed] [Google Scholar]
- 8. Collings PJ, Brage S, Ridgway CL, et al. Physical activity intensity, sedentary time, and body composition in preschoolers. Am J Clin Nutr. 2013;97:1020‐1028. http://www.ncbi.nlm.nih.gov/pubmed/23553158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Metallinos‐Katsaras ES, Freedson PS, Fulton JE, Sherry B. The association between an objective measure of physical activity and weight status in preschoolers. Obesity. 2007;15:686‐694. http://www.ncbi.nlm.nih.gov/pubmed/17372319 [DOI] [PubMed] [Google Scholar]
- 10. Janz KF, Levy SM, Burns TL, Torner JC, Willing MC, Warren JJ. Fatness, physical activity, and television viewing in children during the adiposity rebound period: the Iowa bone development study. Prev Med. 2002;35:563‐571. [DOI] [PubMed] [Google Scholar]
- 11. Vale SMCG, Santos RMR, Soares‐Miranda LM, CMM M, Ruiz JR, JAS M. Objectively measured physical activity and body mass index in preschool children. Int J Pediatr. 2010;20(10):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leppänen MH, Nyström CD, Henriksson P, et al. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4‐year‐old children: results from the ministop trial. Int J Obes. 2016;40:1126‐1133. [DOI] [PubMed] [Google Scholar]
- 13. Bürgi F, Meyer U, Granacher U, et al. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross‐sectional and longitudinal study (Ballabeina). Int J Obes. 2011;35:937‐944. [DOI] [PubMed] [Google Scholar]
- 14. Metcalf BS, Voss LD, Hosking J, Jeffery AN, Wilkin TJ. Physical activity at the government‐recommended level and obesity‐related health outcomes: a longitudinal study (early bird 37). Arch Dis Child. 2008;93:772‐777. [DOI] [PubMed] [Google Scholar]
- 15. Moore LL, Nguyen US, Rothman KJ, Cupples LA, Ellison RC. Preschool physical activity level and change in body fatness in young children: the Framingham Children's Study. Am J Epidemiol. 1995;142:982‐988. http://www.ncbi.nlm.nih.gov/pubmed/7572980 [DOI] [PubMed] [Google Scholar]
- 16. Leppänen MH, Henriksson P, Delisle Nyström C, et al. Longitudinal physical activity, body composition, and physical fitness in preschoolers. Med Sci Sports Exerc. 2017;49:2078‐2085. [DOI] [PubMed] [Google Scholar]
- 17. Carson V, Lee EY, Hewitt L, et al. Systematic review of the relationships between physical activity and health indicators in the early years (0‐4years). BMC Public Health. 2017;17(Suppl 5):854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pedišić Ž. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research ‐ the focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology. 2014;46:135‐146. [Google Scholar]
- 19. Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170:519‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chastin SFM, Palarea‐Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio‐metabolic health markers: a novel compositional data analysis approach. PLoS One. 2015;10:e0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dumuid D, Stanford TE, Martin‐Fernández JA, et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2018;27:3726‐3738. [DOI] [PubMed] [Google Scholar]
- 22. Nyström CD, Sandin S, Henriksson P, et al. Mobile‐based intervention intended to stop obesity in preschool‐aged children: the MINISTOP randomized controlled trial. Am J Clin Nutr. 2017;105:1327‐1335. [DOI] [PubMed] [Google Scholar]
- 23. Delisle Nyström C, Sandin S, Henriksson P, Henriksson H, Maddison R, Löf M. A 12‐month follow‐up of a mobile‐based (mHealth) obesity prevention intervention in pre‐school children: the MINISTOP randomized controlled trial. BMC Public Health. 2018;18:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sadeh A, Sharkey KM, Carskadon MA. Activity‐based sleep‐wake identification: an empirical test of methodological issues. Sleep. 1994;17:201‐207. [DOI] [PubMed] [Google Scholar]
- 25. Chandler JL, Brazendale K, Beets MW, Mealing BA. Classification of physical activity intensities using a wrist‐worn accelerometer in 8‐12‐year‐old children. Pediatr Obes. 2016;11:120‐127. [DOI] [PubMed] [Google Scholar]
- 26. Fields DA, Allison DB. Air‐displacement plethysmography pediatric option in 2‐6 years old using the four‐compartment model as a criterion method. Obesity. 2012;20:1732‐1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lohman TG. Assessment of body composition in children. Pediatr Exerc Sci [Internet]. 1989;1:19‐30. https://journals.humankinetics.com/view/journals/pes/1/1/article-p19.xml [DOI] [PubMed] [Google Scholar]
- 28. Ortega FB, Cadenas‐Sánchez C, Sánchez‐Delgado G, et al. Systematic review and proposal of a field‐based physical fitness‐test battery in preschool children: the PREFIT battery. Sport Med. 2015;45:533‐555. [DOI] [PubMed] [Google Scholar]
- 29. Biddle GJHH, Edwardson CL, Henson J, et al. Associations of physical behaviours and behavioural reallocations with markers of metabolic health: a compositional data analysis. Int J Environ Res Public Health. 2018;15:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jago R, Baranowski T, Baranowski JC, Thompson D, Greaves KA. BMI from 3‐6y of age is predicted by TV viewing and physical activity, not diet. Int J Obes. 2005;29:557‐564. [DOI] [PubMed] [Google Scholar]
- 31. Ek A, Sandborg J, Nyström CD, Lindqvist AK, Rutberg S, Löf M. Physical activity and mobile phone apps in the preschool age: perceptions of teachers and parents. JMIR Mhealth Uhealth. 2019;7:e12512. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Cross‐sectional associations of physical activity (PA) intensities (light, moderate, and vigorous) and SB with body composition and physical fitness at 4 years with compositional data analysis.
Table S2. Cross‐sectional associations of physical activity (PA) intensities (light, and moderate‐to‐vigorous) and SB with body composition and physical fitness at 4 years with compositional data analysis.
Table S3. Prospective associations of associations of physical activity (PA) intensities (light, moderate, and vigorous) and SB at 4 years with body composition and physical fitness at the 12‐month follow up with compositional data analysis.
Table S4. Prospective associations of associations of physical activity (PA) intensities (light, and moderate‐to‐vigorous) and SB at 4 years with body composition and physical fitness at the 12‐month follow up with compositional data analysis.
Figure S1. Cross‐sectional associations of vigorous physical activity (PA) relative to sedentary behavior (SB) and lower PA intensities with body composition and physical fitness at 4 years. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light, and moderate PA. Models are adjusted for sex, age, and awake wear time. Lower values in motor fitness indicate higher performance.
Figure S2. Cross‐sectional effects of pairwise reallocations of time from sedentary behavior (SB), light and moderate physical activity (PA) to vigorous PA on body composition and physical fitness at 4 years. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light, and moderate PA. Models are adjusted for sex, age, and awake wear time. Lower values in motor fitness indicate higher performance.
Figure S3. Prospective effects of pairwise reallocations of time from sedentary behavior (SB), light and moderate physical activity (PA) to vigorous PA at 4 years with body composition and physical fitness at the 12‐month follow‐up. Each line represents the effect of increasing vigorous PA while proportionally reducing SB, light, and moderate PA. Models are adjusted for sex, age, and awake wear time. Lower values in motor fitness indicate higher performance.


