Summary
Shift work, defined as work occurring outside typical daytime working hours, is associated with an increased risk for metabolic syndrome (MetS) due to several biological and environmental changes. The MetS refers to the clustering of several known cardiovascular risk factors, including insulin resistance, obesity, dyslipidemia, and hypertension. This systematic review aims to evaluate the literature on the association between shift work and the risk of MetS in employees of the health sector. A systematic search was conducted in PubMed, Web of Science, and Scopus databases using appropriate keywords for studies published before September 1, 2021. Eligible studies were those that compared the prevalence of MetS between day and shift healthcare workers; had a cross‐sectional, case–control, or cohort study design; provided sufficient data for calculating odds ratios or relative risks with 95% confidence intervals; and articles in English. The Joanna Briggs Institute prevalence critical appraisal tool was used for quality analysis. Risk for MetS and related measures of effect size were retrieved from studies for meta‐analysis. Twelve studies met the criteria for inclusion in the review and meta‐analysis. Sample sizes ranged from 42 to 738, and the age range of subjects was between 18 and 65 years. Ten studies demonstrated high methodological quality, while two studies were of average quality. Ten out of 12 studies in the review demonstrated a higher risk in shift workers for developing MetS than day workers. The pooled OR of MetS in shift workers based on 12 studies was 2.17 (95% CI = 1.31–3.60, P = 0.003; I 2 = 82%, P < 0.001). Shift workers exhibited more than a twofold increase in the chance of developing MetS in comparison with day workers.
Keywords: day work, healthcare workers, metabolic syndrome, shift work
1. INTRODUCTION
Shift work is referred to as any schedule that is irregular or outside the normal daytime hours (7/8 a.m.–5/6 p.m.). Shift workers account for nearly 20% of the global workforce. 1 Shift work is considered indispensable in hospitals, industries, and many other essential services to maintain the continuation of services. Although shift work benefits the community, it can be hazardous both for workers and the community, if the workers' alertness and performance are impaired. 2 Shift work harms the physical, mental, and social well‐being of employees. 3 Further, it is associated with several chronic diseases, including obesity, 4 diabetes, 5 cardiovascular diseases (CVD), 6 and metabolic syndrome (MetS). 7
The MetS is a multiplex risk factor that comprises several risks correlates of metabolic origin. 8 The key components of MetS are dyslipidemia, raised arterial blood pressure, and dysglycemia, with abdominal obesity becoming more prominent as one of the syndrome's key characteristics. 9 MetS is related to an elevated risk for type 2 diabetes mellitus (T2DM) and CVD. 10 Moreover, people with MetS have a 46% higher risk of all‐cause mortality, compared with those without. 11 Several environmental and socio‐economic factors including age, physical inactivity, rapid nutritional changes, lifestyle, and socioeconomic transitions have been recognized as potential risk elements for MetS. 12 , 13
Previous research shows that occupational factors such as shift work, 14 , 15 excessive sitting‐time, and sedentary occupations significantly increase the risk for MetS. 16 Several systematic reviews have discovered a positive relationship between shift work and MetS 7 , 17 and a positive dose–response relationship with duration of exposure. 18 However, all these analyses included employees from different industries, and no study has been conducted up to date to investigate the risk among shift workers in the health sector.
Healthcare workers face a variety of occupational hazards at their workplace which increases the incidences of work‐related disease. 19 These include physical, chemical, biological, radiation, reproductive health, psychiatric disorders, the effects of shift work, and violence. 20 Moreover, the shift work disorder was found to be the most frequent work‐related disturbance in these employees working on shift schedules. 21 It has also been noted that the number of continuous duty hours that health care personnel are permitted to work is much higher than in other professions making them more susceptible to diseases like MetS. 22
The prevalence of hypertension among hospital staff was found to be 26%, which was higher than the 22% found among other occupational groups. 23 A study in the United States reported that physicians were 9% more likely to die from cerebrovascular disorders than other occupations. 24 Another large cohort study in the United States that followed shift working nurses over 22–24 years found that unhealthy lifestyles combined with a 5‐year increment of night shifts predicted a higher risk of diabetes. 25 Moreover, health care workers seem to be at greater risk of burnout than others due to a range of occupational stresses, such as emotionally difficult patient encounters, exposure to death and dying, time pressure and work overload. 26
Shift work is considered essential in the health sector to maintain continuity of service, as many patients require constant medical attention and monitoring. Therefore, an increasing number of healthcare employees are being forced to work irregular hours. However, the results of prior studies comparing the risk of MetS among different occupational groups, have produced mixed results. 27 , 28 Hence, it is of utmost importance to examine whether shift work and its associated lifestyle could accentuate the disease risk in healthcare workers who is already vulnerable due to the occupational hazards. The current review aims to summarize evidence on the association between the risk of developing MetS and shift work among employees of healthcare services.
2. METHODS
The PRISMA (Preferred Reporting Items for Systematic reviews and Meta‐Analyses) statement guidelines 29 were followed in reporting this systematic review and meta‐analysis.
2.1. Literature search strategy
The literature search was carried out in five stages in PubMed® (U.S. National Library of Medicine, USA), Web of Science [v.5.4] (Thomson Reuters, USA), and SciVerse Scopus (Elsevier Properties S. A, USA) databases for articles published before September 1, 2021. We searched databases using Medical Subject Headings (MeSH) terms when possible or keywords when otherwise appropriate and included (“shift work” OR “Shift Work Schedule” OR “Work Schedule Tolerance” OR “Night Shift” OR “night work” OR “irregular working hours” OR “night duty” AND “Metabolic Syndrome” OR “Dysmetabolic Syndrome” OR “Cardiometabolic Syndrome” OR “Metabolic X Syndrome” OR “Syndrome X" OR “deadly quartet” OR “insulin resistance syndrome” OR “Reaven's Syndrome” AND “health personnel” OR “health care worker” OR “health worker” OR “caregiver” OR “physician” OR “medical staff” OR “nurses” OR “hospital employees” OR “hospital staff”). In the PubMed database, an “advanced” search was conducted utilizing the above MeSH terms and keywords in the article title and abstract. The Web of Science® database was searched with the advanced search operator TS (Title, Abstract, Author Keywords, Keywords Plus) for the above search terms in the article topic. The Scopus® database was searched for the aforementioned terms in article title, abstract, or keywords (Data S1).
The total citations gathered from three databases were pooled in the second step and removed the duplicates. The remaining articles were examined to see if they were eligible, by reading article “title,” “abstract,” and “full‐text” in the third, fourth, and fifth stages, respectively, using the inclusion and exclusion criteria mentioned below. A manual search was conducted to obtain additional articles from reference lists of included articles. The literature search was conducted independently by two authors (PS and RJ) separately to identify the studies, and any discrepancies were resolved by discussion.
2.2. Inclusion and exclusion criteria
The inclusion criteria of relevant articles were (1) articles published in English; (2) research comparing a shift worker group to a standard day worker group employed in the healthcare sector; (3) studies reporting the prevalence of MetS in both day and shift workgroups (night work or rotating work covering the period between 12:00 a.m.–5:00 a.m. or reporting as shift work); (4) with cross‐sectional, case–control or cohort study designs, and (5) studies that provide adequate information to calculate odds ratios (ORs) or relative risks (RRs) with 95% confidence interval (CI). Furthermore, conference proceedings, commentaries, editorials, and book chapters/book reviews were excluded. Here the healthcare worker was referred to as someone who provides direct or indirect care and services to the sick and injured, whether as doctors or nurses, aides, helpers, laboratory technicians, or even medical waste handlers. 30
In addition, individual studies were only eligible if the prevalence of MetS was determined according to one of the following acceptable criteria: (a) American Heart Association/National Heart, Lung and Blood Institute (AHA/NHLBI) criteria, 31 (b) National Cholesterol Education Programme's Adult Treatment Panel III criteria (NCEP/ATP III), 32 (c) International Diabetes Federation (IDF) criteria, 33 or (d) modified IDF and modified NCEP/ATP III criteria. 34 When studies estimated the prevalence of MetS using two different criteria, prevalence values based on the most recent criteria were taken into analysis.
2.3. Data extraction
The following variables were extracted and tabulated by an author (PS): first author, publication year, country, study design, gender and age of the study population, sample size, the definition of the night shift, MetS criteria, number of MetS cases, RR or OR values and covariates used in the adjustment. A second author (RJ) double‐checked the accuracy of extracted data, and discrepancies were resolved by discussion. Data not presented in the original manuscript (ORs), where possible were calculated using available data.
2.4. Assessment of quality
The study quality assessment was done by two independent investigators using the Joanna Briggs Institute (JBI) prevalence critical appraisal tool. 35 The JBI quality assessment tool has nine components to assess the overall quality of prevalence studies, including sampling procedure, research subjects, data collection, and classification. The presence of these components can be answered either with a yes, no, unclear, or not applicable. The total number of “yes” responses was counted for each study. A higher number of “yes” responses indicated a lower risk of bias.
2.5. Data analysis
The meta‐analysis comprised the studies that matched the eligibility criteria and reported unadjusted/adjusted ORs or RR values with 95% CIs or provided enough data to calculate unadjusted ORs at 95% CIs. The most adjusted model value was used in our meta‐analyses if a publication reported the results of many adjusted ORs or RRs. In addition, we pooled the effect estimates separately, for unadjusted and adjusted ORs. A subgroup analysis was performed according to the occupation.
The I 2 statistical test was used to examine the heterogeneity among studies. Initially, we performed a fixed‐effects meta‐analysis, but if I 2 was large (>60%), which suggests substantial heterogeneity between studies, a random‐effect model was used. 36 A P value of 0.05 or lower was considered statistically significant. The between‐study variance was represented by Tau. 2 A funnel plot was constructed to evaluate publication bias by visual assessment. The analysis was performed with Rev Man version 5.3 statistical software package using the generic inverse variance method.
3. RESULTS
The literature search was performed according to the aforementioned search criteria and the search strategy is summarized in Figure 1. The search resulted in 82 citations (PubMed: 19; Web of Science: 36; SciVerse Scopus: 27), while two additional articles were identified from search of references. The database search resulted in 55 articles after removing duplicates. After initial screening, based on titles and abstracts, 21 articles were selected for further full‐text review. After screening for inclusion and exclusion criteria, 12 studies were included.
FIGURE 1.
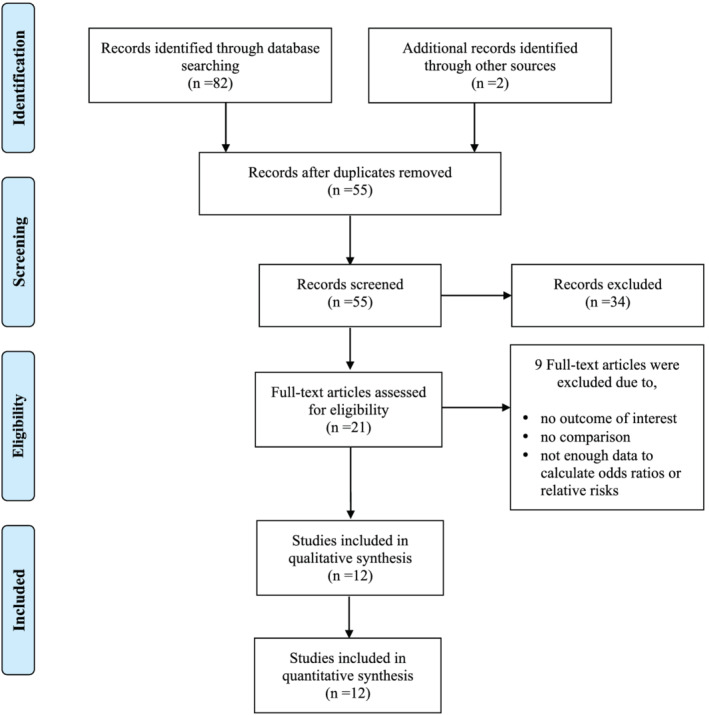
Preferred reporting items for systematic reviews and meta‐analyses flow diagram for study selection
A summary of the included articles is presented in Table 1. Out of the 12 eligible articles identified, six studies were conducted in North and South America, 37 , 40 , 42 , 49 , 50 , 51 two in the Middle East, 43 , 45 two in Europe, 39 , 48 and two in Asian countries. 38 , 46 The review included 11 cross‐sectional studies and one cohort study. 39 The sample sizes ranged between 42 and 738 workers, while the age range of the participants was between 18 and 65 years. Only female workers were involved in five studies, 37 , 40 , 46 , 50 , 51 whereas the others included both males and females. Night shift work was defined in five studies in terms of frequency and time range, 39 , 43 , 48 , 49 , 50 while one study simply reported only the time range. 46 Other studies did not give a clear definition. All the night shift definitions covered the time period from 11:00 p.m. to 5:00 am.
TABLE 1.
Characteristics of the included studies
| Author, published year, country | Study design | Gender; sample size; age | Occupation | Sample size | Definition of shift work | MetS criteria | MetS cases (%) | p value | OR/RR | Adjusted confounders | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day | Non‐day | Day | Night | Adjusted/crude | ||||||||
| Arias et al., 37 2021; Ecuador | CS |
M & F 300 18–60 years |
Volunteers worked in healthcare centers |
150 (M:6; F:90) |
150 (M:46; F:104) |
8 h or more at night, from 7:00 p.m. to 6:00 a.m. and ≥6 month | NCEP‐ATP III | 6 (4.0%) | 84 (56.0%) | <0.001 | 22.13 (8.68–66.07) c | Age, gender, physical activity and energy consumption. |
| Copertaro et al., 38 2008; Italy | CS |
M & F 147 (M:74, F:73) 35–65 years |
hospital staff (mostly nurses) |
77 (M:31; F:46) |
70 (M:43; F:27) |
10:00 p.m.–6:00 a.m. night shift and ≥1.5 nights/month | IDF | 16 (20.8%) | 26 (37.1%) | <0.05 | 2.25 (1.08–4.69) b | None |
|
Farha and Alefishat, 39 2018; Jordan |
CS |
M & F 140 (M:60; F:80) 20–59 years |
Hospital employees |
58 (M:13; F:45) |
82 (M:47; F:35) |
4:00 p.m. to 7:00 a.m. ≥4 night shifts/month for ≥3 years | AHA/NHLBI 2005 | 6 (10.3%) | 13 (15.9%) | 0.48 | 1.63 (0.58–4.58) b | None |
| Holanda et al., 40 2018; Brazil | CS |
F 42 26–40 years |
Nursing professionals | 12 | 30 | ≥3 h between 10:00 p.m. to 5:00 a.m. for ≥6 months. | IDF | 4 (33.3%) | 12 (40.0%) | 0.24 | 1.33 (0.33–5.43) b | None |
| Jung et al., 41 2020; Korea | CS |
F 403 20–45 years |
Nurses | 162 | 241 | 11:00 p.m. to 7:00 a.m. | NCEP‐ATP III | 40 (24.7%) | 47 (19.5.0%) | NR | 0.74 (0.46–1.19) b | None |
| Kirk et al., 42 2015; Canada | CS |
F 466 45.8 ± 9.4 years |
Hospital employees | 300 | 166 | NR | JIS | 60 (20.0%) | 38 (22.9%) | NR | 1.30 (0.78–2.12) c | Age, personal, and leisure time physical activity |
| Korsiak et al., 43 2018; Canada | CS |
F 294 |
Hospital employees. (mostly nurses—68%) | 152 | 142 | NR | JIS | 18 (11.8%) | 29 (20.4%) | 0.04 | 2.72 (1.38–5.36) c | Age |
| Kumar et al., 44 2021; India | CS |
M & F 160 (M:80; F:80) 25–50 years |
Hospital staff |
80 (M:46; F:34) |
80 (M:46; F:34) |
NR | IDF | 33 (41.3%) | 20 (25.0%) | 0.03 | 0.55 (0.24–1.29) c | Age, gender, diet, physical activity, sleep, stress, alcohol consumption |
| Lajoie, et al., 45 2015; Canada | CS |
F 271 |
Hospital employees | 150 | 121 | NR | JIS | 20 (13.3) | 27 (22.3) | 0.05 | 2.29 (1.12–4.70) c | Age, household income, menopausal status |
| Niazi et al., 46 2018; Iran | CS |
M & F 410 (M:124; F:286) 33.43 ± 8.51 years |
Nurse, emergency workers, office workers, and others | 56 | 352 | NR | NCEP‐ATP III | NR | NR | NR | 3.97 (1.67–9.45) | None |
| Pietroiusti et al., 47 2010; Italy | Cohort |
M & F 738 |
Nurses |
336 (M: 92; F:244) |
402 (M:124; F:278) |
Between 9:00 p.m. and 7:00 a.m. and 4 nights/month for ≥1 year | Updated NCEP‐ATP III | 6 (1.8%) | 36 (9.0%) | NR | 5.10 (2.15–12.11) a , c | Age, gender, smoking, alcohol intake, familiar history, physical activity |
| Ritonja et al., 48 2018; Canada | CS | M & F | Hospital employees | 160 | 166 | NR | JIS | 19 (11.9%) | 35 (21.0%) | <0.01 | 1.98 (1.08–3.64) b | |
Abbreviations: AHA/NHLBI, American Heart Association/National Heart, Lung and Blood Institute; CS, cross‐sectional; F, female; h, hours; IDF, International Diabetes Federation; JIS, joint interim statement; M, male; NCEP ATP III, National Cholesterol Education Program, Adult Treatment Panel III; NR, not reported; OR, odd ratio; RR, relative risk.
Relative risk.
Calculated odd ratios with MetS cases in day and night shift worker.
Adjusted odd ratios.
All the studies except the study by Niazi et al. 45 reported the prevalence of MetS among day and shift employees separately. In these studies, the prevalence or incidence of MetS among day workers ranged from 1.8% to 41.3%, whereas it ranged from 9.0% to 56.0% among shift workers when assessed using the aforementioned criteria. Out of the 12 studies, 10 studies reported a higher prevalence of MetS among shift employees compared with day employees, with the difference being statistically significant in five of them (P ≤ 0.05). Only the two studies by Kumar et al. 38 and Jung et al. 46 reported contradictory results.
Six studies reported adjusted OR or RR values for the effect of shift work on MetS, 37 , 38 , 39 , 40 , 49 , 51 while one study reported the crude value. 45 For the remaining five studies, crude OR values were manually calculated. 42 , 43 , 46 , 48 , 50 The study by Pietroiusti et al. 39 showed the highest OR value, while the lowest was reported by Kumar et al. 38 Age was the most commonly adjusted covariate in all of the aforementioned seven studies where effect size was adjusted for confounders. Three studies demonstrated OR adjustments for all three parameters of age, gender, and physical activity levels. 38 , 39 , 49
Results of the quality assessment process are presented in Table S1. The total number of “yes” responses varied from 6 to 9 between studies. Out of the 12 studies in the review, 10 studies appeared to be of high quality with the total number of “yes” scores varying between 7 and 9. Two studies received scores of 6 and seemed to be of average quality. Across all studies, the average number of “yes” responses was 7.42.
All 12 articles were included in the quantitative analysis. A random‐effects analysis was adopted because high I 2 values from fixed‐effects analysis suggested significant heterogeneity between studies. The meta‐analysis results revealed that the odds of developing MetS were significantly greater in shift employees than in day employees with a pooled OR value of 2.17 (95% CI = 1.31–3.60, P = 0.003; I 2 = 82%, P < 0.001) (Figure 2). Since the study by Arias et al. had a large OR and so acted as an outlier, the meta‐analysis was reconducted with the outlier removed, but the pooled effect size remained significant (OR 1.77; 95% CI = 1.19–2.64, P = 0.005; I 2 = 70%, P < 0.001) (Figure S1). The pooled estimate of unadjusted ORs based on six studies was 1.71 (95% CI = 0.98–2.97, P = 0.06; I 2 = 67%, P < 0.009) (Figure S2). When adjusted ORs were analyzed, the pooled estimate based on six studies was 2.74 (95% CI = 1.15–6.51, P = 0.02; I 2 = 88%, P < 0.001) (Figure S3). Based on the subgroup analysis for nurses, the pooled adjusted OR (95% CI) was estimated as 2.20 (95% CI = 1.11–4.38, P = 0.02; I 2 = 79%, P < 0.001) (Figure S4). The funnel plots revealed that the studies were distributed fairly symmetrically around the aggregate effect size, indicating that there was little publication bias (Figure S5).
FIGURE 2.
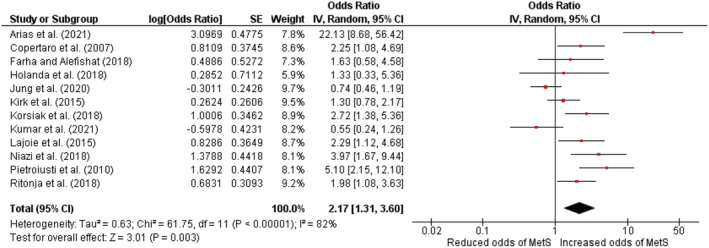
Association between metabolic syndrome and shift work among healthcare workers
4. DISCUSSION
Although earlier studies have examined the association between MetS and shift work, this is the first to quantify the risk for shift workers in the health sector. The results of the current study were consistent with the meta‐analyses done by Wang et al. and Yang et al., where both found significant positive associations between night shift work and MetS among workers from different industries. In Wang et al., the pooled RR for the association between night shift work and MetS risk was 1.57 (95% CI = 1.24–1.98), 18 while Yang et al. reported a RR of 1.30 (95% CI: 1.19–1.41). 47 A similar study among a group of Iranian drivers revealed that the risk of MetS is higher among shift working drivers (OR 1.495; 95% CI: 1.349–1.657). 41 Our study discovered a greater occurrence of MetS for employees working in the health care sector (OR 2.17; 95% CI = 1.31–3.60, P = 0.003). The pooled OR for the adjusted estimates was even higher when the analysis was adjusted for confounding factors 2.74 (95% CI = 1.15–6.51, P = 0.02). Therefore, it is evident that health sector workers have a pronounced risk of MetS.
According to recent research, circadian rhythm disruption (chronodisruption) may lead to manifestations of MetS. 44 The relationship between the circadian system and different MetS components such as impaired glucose and lipid metabolism, 52 , 53 adipose tissue function, and cardiac, 54 vascular, and hemostatic function 55 has been studied widely. The prevalence of adiposity and MetS is increased by shift employment, sleep deprivation, and exposure to bright light at night. 56 In line with these findings, a meta‐analysis has demonstrated a significant increase in the body fat percentage of shift employees when compared to the non‐shift group. 57 Further, among nurses, a correlation has been detected among the variables of anxiety and stress with MetS. 58
Health sector employees must work non‐traditional shifts which often result in sleep disruption, reduced sleep duration, or drowsiness due to misalignment of the circadian pacemaker with sleep–wake timing. 1 The progressive decrease in the amount of time spent sleeping, may disturb synchronization between sleep/activity and alternating periods of feeding/fasting and energy storage/usage. 59 Sleep deprivation is an individual risk factor for the development of MetS and an increased risk of obesity. 60 Leptin, which is primarily produced by adipose tissue and is the product of the obesity gene, controls food intake and energy expenditure, fatty acid metabolism of skeletal muscle, and hepatic glucose synthesis. 61 The structure of leptin is similar to that of pro‐inflammatory cytokines like interleukin (IL)‐6, which inhibits insulin activity. In addition, excessive fatty acid outflow from adipose tissue is a key factor in the onset of MetS. 62 Because insulin regulates this pathway, insulin resistance causes an increase in the free fatty acid release from adipose tissue and poor removal of triglyceride‐rich lipoproteins. 63 As a result, lipid accumulation in ectopic regions like the liver, skeletal muscle, and pancreatic islets can lead to the organ's functional impairment. 64
Out of the 12 studies included in the current review, 10 studies demonstrated a positive relationship between shift work and MetS, while the other two studies by Kumar et al. 38 and Jung et al. 46 resulted in contradictory outcomes. However, Kumar et al. reported that the OR for MetS among shift workers was not significant after adjusting for confounding variables including age, physical activity, sleep, and diet. 38 According to Jung et al., young nurses usually work shifts, and shift work nurses caring for patients will participate in more physical activities than non‐shift work nurses doing administrative tasks. 46
Several limitations are associated with this study. First, the diagnostic criteria for MetS differed between studies, limiting the study's comparability. Second, the inconsistency in the definition of night shift work. Because the night shift duration and frequency per week differed among studies, it could have led to a dilution of the pooled effect during the meta‐analysis. Third, there was considerable heterogeneity among the selected studies relative to sample sizes, primary objectives, and study designs. Finally, the OR values used for the meta‐analysis included both adjusted and unadjusted values. When studies reported adjusted values, we always used the best‐adjusted value for the highest number of covariates to minimize bias during the meta‐analysis. Furthermore, as to literature, the use of OR to compare effect sizes in meta‐analysis is not recommended as the magnitude of odds ratios is easy to misinterpret. 65 Also it has been reported that odds ratios cannot be interpreted as absolute effects, nor could be compared across different study samples. 66 The meta‐analysis indicated high heterogeneity which could be due to a variety of factors, including the differences in shift schedules among the workers. However, we could not conduct a subgroup analysis based on different shift schedules due to the lack of sufficient information. Therefore, to better understand these associations more future research is needed, such as appropriately powered cohort studies or interventional clinical trials. Furthermore, conducting subgroup analysis and adjusting for confounding variables, when possible, could reduce heterogeneity and increase precision in future research.
Our results suggest that shift working employees in the healthcare sector are twice as likely to develop MetS compared with their day working counterparts. Although we could not inspect the relationship between years of shift employment and risk for MetS, prior shift work studies have shown a positive dose–response connection with exposure duration. 27 Therefore, future research should focus on creating intervention measures to reduce the incidence of MetS among shift workers. Research suggests that MetS is caused due to several underlying risk factors, including environmental, behavioral, genetic, 67 and hormonal variables. 68 Therefore, future policies and interventions should be planned to change these aspects (Table S2). As body composition and epigenetics are predictors of MetS, 69 it is recommended that employees be screened at the time of hiring based on their family disease history and BMI to determine their fit for shift work. Further, the physical environment at work plays a vital role in employees' health. 70 Especially for shift workers, the workplace meal environment, maybe uncomfortable, and canteens may have a limited supply of nutritious food late at night. 71 Therefore, the availability and accessibility of healthy foods at workplaces should be ensured. Also, the canteens that adhere to healthy dietary guidelines and promote healthy food habits among staff should be promoted. In addition, workplace health promotion programs could be set up to encourage employees to adopt healthy behavioral changes, 72 such as reducing obesity and increasing physical activity. 73 Different dietary intervention strategies such as portion control, meal replacements, and energy/calorie‐restricted diets should be introduced to shift working employees. Ultimately the employers and other policymakers should offer more flexible work schedules for shift working employees to ensure their work/life balance.
5. CONCLUSION
This is the first meta‐analysis to explore the association between shift employment and the possibility of developing MetS, particularly among the healthcare sector employees. In 10 of the 12 studies in the review, shift workers were shown to have a high prevalence of MetS in comparison to their non‐shift working counterparts. Outcomes of the meta‐analysis showed a twofold increased risk for the development of MetS in shift workers relative to the day group. Therefore, to safeguard shift workers from MetS, health promotion programs as well as other interventional strategies to adopt healthy environmental and behavioral changes should be introduced. In addition, organizations should streamline the shift work system with well‐designed rotational shift schedules to allow employees to maintain work/life balance.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
AUTHOR CONTRIBUTIONS
PS conceived and designed the study. PS and RJ were involved in data collection. PS analyzed data and drafted the manuscript. RJ, NK, and TP critically revised the manuscript. All authors read and approved the final manuscript.
Supporting information
Data S1: Search strategy
Figure S1. The pooled estimate of after removing the study Arias et al
Figure S2. The pooled estimate of unadjusted ORs
Figure S3. The pooled estimate of adjusted ORs
Figure S4. Pooled risk estimates of night shift work and metabolic syndrome for nurses
Figure S5. Funnel plots to assess publication bias
Table S1. Quality analysis
Table S2. Recommended policies and interventions to reduce the incidence of MetS among shift workers.
ACKNOWLEDGMENT
The authors would like to thank Professor Priyanga Ranasinghe for his assistance with the meta‐analysis. Open access publishing facilitated by Queensland University of Technology, as part of the Wiley ‐ Queensland University of Technology agreement via the Council of Australian University Librarians.
Sooriyaarachchi P, Jayawardena R, Pavey T, King NA. Shift work and the risk for metabolic syndrome among healthcare workers: A systematic review and meta‐analysis. Obesity Reviews. 2022;23(10):e13489. doi: 10.1111/obr.13489
REFERENCES
- 1. Wright KP, Bogan RK, Wyatt JK. Shift work and the assessment and management of shift work disorder (SWD). Sleep Med Rev. 2013;17:41‐54. doi: 10.1016/j.smrv.2012.02.002 [DOI] [PubMed] [Google Scholar]
- 2. Dhande KK, Sharma S. Influence of shift work in process industry on workers' occupational health, productivity, and family and social life: an ergonomic approach. Hum Factors Ergon Manuf. 2011;21(3):260‐268. doi: 10.1002/hfm.20231 [DOI] [Google Scholar]
- 3. Kim W, Kim TH, Lee T‐H, Choi JW, Park E‐C. The impact of shift and night work on health related quality of life of working women: findings from the Korea Health Panel. Health Qual Life Outcomes. 2016;14:1‐6. doi: 10.1186/s12955-016-0564-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sun M, Feng W, Wang F, et al. Meta‐analysis on shift work and risks of specific obesity types. Obes Rev. 2018;19:28‐40. doi: 10.1111/obr.12621 [DOI] [PubMed] [Google Scholar]
- 5. Knutsson A, Kempe A. Shift work and diabetes—a systematic review. Chronobiol Int. 2014;31(10):1146‐1151. doi: 10.3109/07420528.2014.957308 [DOI] [PubMed] [Google Scholar]
- 6. Åkerstedt T, Knutsson A, Alfredsson L, Theorell T. Shift work and cardiovascular disease. Scand J Work Environ Health. 1984;10:409‐414. doi: 10.5271/sjweh.2302 [DOI] [PubMed] [Google Scholar]
- 7. Canuto R, Garcez AS, Olinto MT. Metabolic syndrome and shift work: a systematic review. Sleep Med Rev. 2013;17(6):425‐431. doi: 10.1016/j.smrv.2012.10.004 [DOI] [PubMed] [Google Scholar]
- 8. Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol. 2008;28(4):629‐636. doi: 10.1161/ATVBAHA.107.151092 [DOI] [PubMed] [Google Scholar]
- 9. Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011;9(1):48. doi: 10.1186/1741-7015-9-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wilson PW, DAgostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066‐3072. doi: 10.1161/CIRCULATIONAHA.105.539528 [DOI] [PubMed] [Google Scholar]
- 11. Hui WS, Liu Z, Ho SC. Metabolic syndrome and all‐cause mortality: a meta‐analysis of prospective cohort studies. Eur J Epidemiol. 2010;25(6):375‐384. doi: 10.1007/s10654-010-9459-z [DOI] [PubMed] [Google Scholar]
- 12. Khan RJ, Gebreab SY, Sims M, Riestra P, Xu R, Davis SK. Prevalence, associated factors and heritabilities of metabolic syndrome and its individual components in African Americans: the Jackson Heart Study. BMJ Open. 2015;5(10):e008675. doi: 10.1136/bmjopen-2015-008675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Prasad D, Kabir Z, Dash A, Das B. Prevalence and risk factors for metabolic syndrome in Asian Indians: a community study from urban Eastern India. J Cardiovasc Dis Res. 2012;3:204‐211. doi: 10.4103/0975-3583.98895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Karlsson BH, Knutsson AK, Lindahl BO, Alfredsson LS. Metabolic disturbances in male workers with rotating three‐shift work. Results of the WOLF study. Int Arch Occup Environ Health. 2003;76:424‐430. [DOI] [PubMed] [Google Scholar]
- 15. Puttonen S, Viitasalo K, Härmä M. The relationship between current and former shift work and the metabolic syndrome. Scand J Work Environ Health. 2012;38:343‐348. doi: 10.5271/sjweh.3267 [DOI] [PubMed] [Google Scholar]
- 16. Nam JY, Kim J, Cho KH, et al. Associations of sitting time and occupation with metabolic syndrome in South Korean adults: a cross‐sectional study. BMC Public Health. 2016;16:943. doi: 10.1186/s12889-016-3617-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khosravipour M, Khanlari P, Khazaie S, Khosravipour H, Khazaie H. A systematic review and meta‐analysis of the association between shift work and metabolic syndrome: the roles of sleep, gender, and type of shift work. Sleep Med Rev. 2021;57:101427. doi: 10.1016/j.smrv.2021.101427 [DOI] [PubMed] [Google Scholar]
- 18. Wang F, Zhang L, Zhang Y, et al. Meta‐analysis on night shift work and risk of metabolic syndrome. Obes Rev. 2014;15(9):709‐720. doi: 10.1111/obr.12194 [DOI] [PubMed] [Google Scholar]
- 19. Conventions ILOCoEotAo . ILO standards on occupational safety and health: promoting a safe and healthy working environment: International Labour Organization 2009.
- 20. Mohanty A, Kabi A, Mohanty AP. Health problems in healthcare workers: a review. J Family Med Prim Care. 2019;8:2568‐2572. doi: 10.4103/jfmpc.jfmpc_431_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. dEttorre G, Pellicani V. Preventing shift work disorder in shift health‐care workers. Saf Health Work. 2020;11:244‐247. doi: 10.1016/j.shaw.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Keller SM, Berryman P, Lukes E. Effects of extended work shifts and shift work on patient safety, productivity, and employee health. AAOHN J. 2009;57(12):497‐504. doi: 10.1177/216507990905701204 [DOI] [PubMed] [Google Scholar]
- 23. Mion D Jr, Pierin AM, Bambirra AP, et al. Hypertension in employees of a University General Hospital. Revista do Hospital das Clínicas. 2004;59(6):329‐336. doi: 10.1590/S0041-87812004000600004 [DOI] [PubMed] [Google Scholar]
- 24. Frank E, Biola H, Burnett CA. Mortality rates and causes among U.S. physicians. Am J Prev Med. 2000;19:155‐159. PMID: The full text of this article is available via AJPM Online at: http://www.elsevier.com/locate/ajpmonline [DOI] [PubMed] [Google Scholar]
- 25. Shan Z, Li Y, Zong G, et al. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ. 2018;363:k4641. doi: 10.1136/bmj.k4641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, Uaphanthasath R, Wiwatanadate P. Shift work and burnout among health care workers. Occup Med. 2014;64(4):279‐286. doi: 10.1093/occmed/kqu009 [DOI] [PubMed] [Google Scholar]
- 27. Wang Y, Yu L, Gao Y, et al. Association between shift work or long working hours with metabolic syndrome: a systematic review and dose–response meta‐analysis of observational studies. Chronobiol Int. 2021;38:318‐333. doi: 10.1080/07420528.2020.1797763 [DOI] [PubMed] [Google Scholar]
- 28. Davila EP, Florez H, Fleming LE, et al. Prevalence of the metabolic syndrome among US workers. Diabetes Care. 2010;33(11):2390‐2395. doi: 10.2337/dc10-0681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Joseph B, Joseph M. The health of the healthcare workers. Indian J Occup Environ Med. 2016;20:71‐72. doi: 10.4103/0019-5278.197518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112(17):2735‐2752. doi: 10.1161/CIRCULATIONAHA.105.169404 [DOI] [PubMed] [Google Scholar]
- 32. Cleeman J, Grundy S, Becker D, Clark L. Expert panel on detection, evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP III). Jama. 2001;285(19):2486‐2497. doi: 10.1001/jama.285.19.2486 [DOI] [PubMed] [Google Scholar]
- 33. Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the US. Diabetes Care. 2005;28(11):2745‐2749. doi: 10.2337/diacare.28.11.2745 [DOI] [PubMed] [Google Scholar]
- 34. Moy FM, Bulgiba A. The modified NCEP ATP III criteria maybe better than the IDF criteria in diagnosing Metabolic Syndrome among Malays in Kuala Lumpur. BMC Public Health. 2010;10:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13:147‐153. doi: 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 36. Barili F, Parolari A, Kappetein PA, Freemantle N. Statistical primer: heterogeneity, random‐or fixed‐effects model analyses? Interact Cardiovasc Thorac Surg. 2018;27:317‐321. doi: 10.1093/icvts/ivy163 [DOI] [PubMed] [Google Scholar]
- 37. Korsiak J, Tranmer J, Day A, Aronson KJ. Sleep duration as a mediator between an alternating day and night shift work schedule and metabolic syndrome among female hospital employees. Occup Environ Med. 2018;75(2):132‐138. doi: 10.1136/oemed-2017-104371 [DOI] [PubMed] [Google Scholar]
- 38. Kumar SE, Antonisamy B, Kirupakaran H, Alex RG. A cross‐sectional study among hospital employees—metabolic syndrome and shift work. Indonesian J Occup Safety Health. 2021;10(2):258‐264. doi: 10.20473/ijosh.v10i2.2021.258-264 [DOI] [Google Scholar]
- 39. Pietroiusti A, Neri A, Somma G, et al. Incidence of metabolic syndrome among night‐shift healthcare workers. Occup Environ Med. 2010;67(1):54‐57. doi: 10.1136/oem.2009.046797 [DOI] [PubMed] [Google Scholar]
- 40. Lajoie P, Aronson KJ, Day A, Tranmer J. A cross‐sectional study of shift work, sleep quality and cardiometabolic risk in female hospital employees. BMJ Open. 2015;5(3):e007327. doi: 10.1136/bmjopen-2014-007327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mohebbi I, Shateri K, Seyedmohammadzad M. The relationship between working schedule patterns and the markers of the metabolic syndrome: comparison of shift workers with day workers. Int J Occup Med Environ Health. 2012;25(4):383‐391. doi: 10.2478/s13382-012-0051-5 [DOI] [PubMed] [Google Scholar]
- 42. Ritonja J, Aronson KJ, Day AG, Korsiak J, Tranmer J. Investigating cortisol production and pattern as mediators in the relationship between shift work and cardiometabolic risk. Can J Cardiol. 2018;34(5):683‐689. doi: 10.1016/j.cjca.2018.02.006 [DOI] [PubMed] [Google Scholar]
- 43. Farha RA, Alefishat E. Shift work and the risk of cardiovascular diseases and metabolic syndrome among Jordanian employees. Oman Med J. 2018;33(3):235‐242. doi: 10.5001/omj.2018.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Froy O. The relationship between nutrition and circadian rhythms in mammals. Front Neuroendocrinol. 2007;28(2–3):61‐71. doi: 10.1016/j.yfrne.2007.03.001 [DOI] [PubMed] [Google Scholar]
- 45. Niazi E, Saraei M, Aminian O, Izadi N. Frequency of metabolic syndrome and its associated factors in health care workers. Diabetes Metab Syndr Clin Res Rev. 2019;13(1):338‐342. doi: 10.1016/j.dsx.2018.10.013 [DOI] [PubMed] [Google Scholar]
- 46. Jung H, Dan H, Pang Y, et al. Association between dietary habits, shift work, and the metabolic syndrome: The Korea nurses' health study. Int J Environ Res Public Health. 2020;17(20):1‐13. doi: 10.3390/ijerph17207697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yang X, Di W, Zeng Y, et al. Association between shift work and risk of metabolic syndrome: a systematic review and meta‐analysis. Nutr Metab Cardiovasc Dis. 2021;31(10):2792‐2799. doi: 10.1016/j.numecd.2021.06.007 [DOI] [PubMed] [Google Scholar]
- 48. Copertaro A, Bracci M, Barbaresi M, Santarelli L. Assessment of cardiovascular risk in shift healthcare workers. Eur J Cardiovasc Prev Rehabil. 2008;15(2):224‐229. doi: 10.1097/HJR.0b013e3282f364c0 [DOI] [PubMed] [Google Scholar]
- 49. Carpio Arias TV, Mogrovejo Arias DC, Nicolalde Cifuentes TM, Tapia Veloz EC, De Zeeuw CI, Vinueza Veloz MF. Sleep quality does not mediate the negative effects of chronodisruption on body composition and metabolic syndrome in healthcare workers in Ecuador. Diabetes Metab Syndr Clin Res Rev. 2021;15:397‐402. doi: 10.1016/j.dsx.2021.01.017 [DOI] [PubMed] [Google Scholar]
- 50. Holanda NCP, de Castro Moreno CR, Marqueze EC. Metabolic syndrome components: is there a difference according to exposure to night work? Chronobiol Int. 2018;35(6):801‐810. doi: 10.1080/07420528.2018.1450267 [DOI] [PubMed] [Google Scholar]
- 51. Kirk M, VanDenKerkhof E, Janssen I, Tranmer J. The influence of work patterns on indicators of cardiometabolic risk in female hospital employees. J Nurs Adm. 2015;45(5):284‐291. doi: 10.1097/NNA.0000000000000199 [DOI] [PubMed] [Google Scholar]
- 52. Kalsbeek A, la Fleur S, Fliers E. Circadian control of glucose metabolism. Mol Metab. 2014;3(4):372‐383. doi: 10.1016/j.molmet.2014.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gooley JJ. Circadian regulation of lipid metabolism. Proc Nutr Soc. 2016;75:440‐450. doi: 10.1017/S0029665116000288 [DOI] [PubMed] [Google Scholar]
- 54. Kervezee L, Kosmadopoulos A, Boivin DB. Metabolic and cardiovascular consequences of shift work: the role of circadian disruption and sleep disturbances. Eur J Neurosci. 2020;51(1):396‐412. doi: 10.1111/ejn.14216 [DOI] [PubMed] [Google Scholar]
- 55. Montagnana M, Salvagno GL, Lippi G. Circadian variation within hemostasis: an underrecognized link between biology and disease? Seminars in Thrombosis and Hemostasis © Thieme Medical Publishers. 2009;35(01):023‐033. doi: 10.1055/s-0029-1214145 [DOI] [PubMed] [Google Scholar]
- 56. Garaulet M, Madrid JA. Chronobiology, genetics and metabolic syndrome. Curr Opin Lipidol. 2009;20:127‐134. doi: 10.1097/MOL.0b013e3283292399 [DOI] [PubMed] [Google Scholar]
- 57. Sooriyaarachchi P, Jayawardena R, Pavey T, King N. Shift work and body composition: a systematic review and meta‐analysis. Minerva Endocrinol. 2021. doi: 10.23736/S2724-6507.21.03534-X [DOI] [PubMed] [Google Scholar]
- 58. Ribeiro RP, Marziale MHP, Martins JT, Ribeiro PHV, Robazzi MLCC, Dalmas JC. Prevalence of metabolic syndrome among nursing personnel and its association with occupational stress, anxiety and depression. Rev Lat am Enfermagem. 2015;23(3):435‐440. doi: 10.1590/0104-1169.0383.2573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Maury E, Ramsey KM, Bass J. Circadian rhythms and metabolic syndrome: from experimental genetics to human disease. Circ Res. 2010;106(3):447‐462. doi: 10.1161/CIRCRESAHA.109.208355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cappuccio FP, Taggart FM, Kandala N‐B, et al. Meta‐analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619‐626. doi: 10.1093/sleep/31.5.619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dyck D, Heigenhauser GJ, Bruce CR. The role of adipokines as regulators of skeletal muscle fatty acid metabolism and insulin sensitivity. Acta Physiol. 2006;186:5‐16. doi: 10.1111/j.1748-1716.2005.01502.x [DOI] [PubMed] [Google Scholar]
- 62. Lechleitner M. Obesity and the metabolic syndrome in the elderly—a mini‐review. Gerontology. 2008;54:253‐259. doi: 10.1159/000161734 [DOI] [PubMed] [Google Scholar]
- 63. Boden G, Shulman G. Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and β‐cell dysfunction. Eur J Clin Invest. 2002;32:14‐23. doi: 10.1046/j.1365-2362.32.s3.3.x [DOI] [PubMed] [Google Scholar]
- 64. Friedman J. Fat in all the wrong places. Nature. 2002;415(6869):268‐269. doi: 10.1038/415268a [DOI] [PubMed] [Google Scholar]
- 65. Norton EC, Dowd BE, Maciejewski ML. Odds ratios—current best practice and use. Jama. 2018;320(1):84‐85. doi: 10.1001/jama.2018.6971 [DOI] [PubMed] [Google Scholar]
- 66. Norton EC, Dowd BE. Log odds and the interpretation of logit models. Health Serv Res. 2018;53:859‐878. doi: 10.1111/1475-6773.12712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wolk R, Somers VK. Sleep and the metabolic syndrome. Exp Physiol. 2007;92(1):67‐78. doi: 10.1113/expphysiol.2006.033787 [DOI] [PubMed] [Google Scholar]
- 68. Tsou MT, Chen JY. Burnout and metabolic syndrome among healthcare workers: is subclinical hypothyroidism a mediator? J Occup Health. 2021;63(1):e12252. doi: 10.1002/1348-9585.12252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Carraro JCC, Mansego ML, Milagro FI, et al. LINE‐1 and inflammatory gene methylation levels are early biomarkers of metabolic changes: association with adiposity. Biomarkers. 2016;21:625‐632. doi: 10.3109/1354750X.2016.1171904 [DOI] [PubMed] [Google Scholar]
- 70. Campos‐Andrade C, Hernández‐Fernaud E, Lima M‐L. A better physical environment in the workplace means higher well‐being? A study with healthcare professionals. Psyecology. 2013;4:89‐110. doi: 10.1174/217119713805088324 [DOI] [Google Scholar]
- 71. Dahl Lassen A, Thorsen AV, Haapala I, et al. Food at work around the clock—the Nordic model: report from a Nordic Workshop, November 4, 2016, Copenhagen, Denmark. National Food Institute: 2017. [Google Scholar]
- 72. Harden A, Peersman G, Oliver S, Mauthner M, Oakley A. A systematic review of the effectiveness of health promotion interventions in the workplace. Occup Med. 1999;49(8):540‐548. doi: 10.1093/occmed/49.8.540 [DOI] [PubMed] [Google Scholar]
- 73. Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol. 2014;19:149‐180. doi: 10.1111/bjhp.12052 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1: Search strategy
Figure S1. The pooled estimate of after removing the study Arias et al
Figure S2. The pooled estimate of unadjusted ORs
Figure S3. The pooled estimate of adjusted ORs
Figure S4. Pooled risk estimates of night shift work and metabolic syndrome for nurses
Figure S5. Funnel plots to assess publication bias
Table S1. Quality analysis
Table S2. Recommended policies and interventions to reduce the incidence of MetS among shift workers.


