Abstract
Introduction
The COVID-19 pandemic has negatively impacted health systems globally and widened preexisting disparities. We conducted a scoping review on the impact of the COVID-19 pandemic on women and girls’ access to and utilisation of sexual and reproductive health (SRH) services for contraception, abortion, gender-based and intimate partner violence (GBV/IPV) and sexually transmitted infections (STIs).
Methods
We systematically searched peer reviewed literature and quantitative reports, published between December 2019 and July 2021, focused on women and girls’ (15–49 years old) access to and utilisation of selected SRH services during the COVID-19 pandemic. Included studies were grouped based on setting, SRH service area, study design, population and reported impact. Qualitative data were coded, organised thematically and grouped by major findings.
Results
We included 83 of 3067 identified studies and found that access to contraception, in-person safe abortion services, in-person services for GBV/IPV and STI/HIV testing, prevention and treatment decreased. The geographical distribution of this body of research was uneven and significantly less representative of countries where COVID-19 restrictions were very strict. Access was limited by demand and supply side barriers including transportation disruptions, financial hardships, limited resources and legal restrictions. Few studies focused on marginalised groups with distinct SRH needs.
Conclusion
Reports indicated negative impacts on access to and utilisation of SRH services globally, especially for marginalised populations during the pandemic. Our findings call for strengthening of health systems preparedness and resilience to safeguard global access to essential SRH services in ongoing and future emergencies.
Keywords: COVID-19, HIV, Systematic review, Health systems
WHAT IS ALREADY KNOWN ON THIS TOPIC
Several reports point to the negative impact of the COVID-19 pandemic on access to and utilisation of sexual and reproductive health (SRH) services.
WHAT THIS STUDY ADDS
This scoping review showed that the impact of the COVID-19 pandemic on access to and utilisation of SRH services was global and distributed across several service areas including contraception, in-clinic safe abortion and postabortion care, in-person gender-based and intimate partner violence services and sexually transmitted infection/HIV testing, treatment and prevention.
Critical geographic and demographic research gaps on the impact of the pandemic on SRH remain, especially in East Asia and the Pacific, Latin America and the Caribbean, South Asia, the Middle East and North Africa and among marginalised populations with distinct SRH needs.
We identified barriers to accessing SRH care across the globe related to the pandemic including transportation disruptions, financial hardships, reduced medical supplies and human resources and legal restrictions to abortion care; barriers were more pronounced in countries where restrictions (eg, legal restrictions on abortion) or economic disadvantages existed prepandemic.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Research efforts must focus on under-represented regions, particularly those that have been affected most by COVID-19 restrictions, marginalised groups with distinct SRH needs and understudied concepts such as the incidence and risk of unsafe abortion. Practice and policy adaptations to ensure restored access to SRH services must address identified barriers and should be accompanied by evidence of the efficacy, acceptability and equity of such changes.
Introduction
Since the onset of the COVID-19 pandemic, direct and indirect effects of COVID-19 on health systems have been documented globally. Primary effects of infection with the coronavirus and secondary effects of public health and policy responses have exerted unequal health burdens among various populations.1 2 Infectious disease outbreaks are known to negatively affect human, social, physical and financial capital—livelihood assets that contribute to treatment seeking—leaving people more vulnerable to limited access and utilisation of healthcare including sexual and reproductive health (SRH) services. Indeed, SRH care and outcomes have reportedly declined as a result of the COVID-19 pandemic and associated mitigation efforts such as lockdowns.3 4 At its onset, the public health crisis threatened hard-won progress towards modern contraceptive coverage targets set by the Sustainable Development Goals (SDGs); the United Nations Population Fund estimated that the pandemic interfered with contraceptive use for about 12 million women resulting in as many as 2.7 million unintended pregnancies in its first year.5 In addition, Marie Stopes International estimated that there were 1.2 million unsafe abortions in the first 6 months of the pandemic alone.6 The ongoing threat to safe abortion access is perpetuated by an increase in circumstances that lead to unsafe abortions, such as restrictive abortion policies,7 increased poverty among women8 and clinic closures caused by the pandemic.6 Another vulnerable area of SRH is sexually transmitted infections (STIs) that continue to dominate the healthcare burden of many regions; indeed, HIV is a major global health issue with AIDS being leading cause of death among women of reproductive age.9 At the beginning of the pandemic, it was estimated that in high-burden settings, there could be a 10% increase in deaths due to HIV over 5 years caused by the effect of the COVID-19 pandemic on HIV programmes.10 11
Reduced access to SRH services in the wake of the pandemic is of heightened concern considering the gendered impacts of the pandemic that aggravated existing health disparities for women and girls.6 Containment measures established in response to the pandemic increased the incidence of negative SRH outcomes for women and girls, particularly in low-income and-middle income countries. For instance, school closures resulted in increased risk and incidence of pregnancy among adolescent girls in regions of sub-Saharan Africa, thus exacerbating their SRH needs as far as contraception and safe abortion.12 13 The COVID-19 pandemic also saw increased rates of domestic violence across the globe correlated with increased household economic insecurity, additional childcare work, loss of social networks and isolation, each of which are risk factors for increased violence that disproportionately affects women and, in turn, hinder the ability of women to seek help.1 14 As the pandemic drove an increase in certain SRH needs, the ability to access and use SRH services remains critical. Understanding where, how and for whom access to SRH services was most impacted is essential to ensuring continued restoration of SRH service coverage.
Several reviews have synthesised literature regarding the COVID-19 pandemic and its impact on the health of women and girls. These have primarily focused on maternal and perinatal health,15–18 sexual health and behaviour,17 19 menstrual cyclicity and pregnancy intentions20 and the adoption of practice recommendations for reproductive health services amid the pandemic.21 In this current review, we sought to assess the impact of the COVID-19 pandemic on access to and utilisation of four key SRH service areas that represent major health needs among women and girls of reproductive age: contraception, abortion, gender-based violence (GBV) and intimate partner violence (IPV), and STI, including HIV. These SRH services have, apart from contraception,17 not been included in aforementioned reviews,15 16 18–21 nor have prior reviews reported evidence regarding the specific barriers imposed by the pandemic, included evidence beyond the first year of the pandemic or synthesised both qualitative and quantitative data on a global scale. Here, we aimed to identify geographical, demographic and thematic research gaps and to describe the findings of included research, including barriers to accessing SRH services and the impact of the COVID-19 pandemic on groups with distinct SRH needs.
Methods
Study design
We adopted methods from a scoping review framework22 and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews checklist.23 The study protocol was registered at the open science framework and can be accessed via osf.io/2tk9j.
The objectives were to: (1) describe the impact of the COVID-19 pandemic on access to and utilisation of SRH services; (2) identify research and knowledge gaps in relation to how the COVID-19 pandemic has impacted access to and utilisation of SRH services and (3) identify barriers to access and utilisation. In order to successfully meet these objectives, we used the population, concept and context framework.24
Population
Women and girls of reproductive age (15–49 years old) seeking SRH services. The term ‘women and girls’ is used throughout this review and seeks to encompass all individuals seeking SRH services directed towards people who can become pregnant, have female reproductive anatomy or may be victims of gender-based violence. We acknowledge that not all individuals who seek SRH services identify as women.
Concept
Access to and utilisation of selected SRH services for women and girls. Access is defined as (any measure of) an individual’s ability to seek, reach and receive SRH services during the COVID-19 pandemic, which implicates measures of behavioural, logistic, infrastructural, organisational or policy changes made in response to the pandemic including the impact of lockdowns on these functions.25 We defined utilisation as any measure of peoples’ self-reported or provider’s noted use of SRH services, either in-person or remote through telehealth approaches.
Context
Any country in which the COVID-19 pandemic impacted access to/utilisation of selected SRH services.
Data sources and literature search
We conducted searches of peer-reviewed journals and grey literature in five electronic databases: PubMed, Web of Science, CINAHL, Global Health and WHO Global Index Medicus. Searches were conducted without any limitation with regards to geography, language or year. Search terms related to COVID-19 were used as previously defined by Lazarus et al.26 A detailed description of our search strategy is available in online supplemental appendix 1. We also searched the reference list of all studies relevant to our research question for additional studies.
bmjgh-2022-009594supp001.pdf (168.5KB, pdf)
Study selection
Prior to screening, all references retrieved from searched databases were imported into Covidence (Covidence, Melbourne, Australia). and duplicates were removed. HV and HK screened all abstracts and titles, excluding studies that did not pertain to the SRH focus areas or address the research question. Next, HV and HK screened the full texts of all studies remaining after the title/abstract screening phase. ECL arbitrated conflicts at both stages of screening through mediated discussion.
Eligibility criteria
This study included original, English language, peer-reviewed research studies presenting quantitative and/or qualitative data, and primary quantitative reports/letters on clinical/programme data from service providers, published between December 2019 to July 2021. These include studies that investigated the impact of the COVID-19 pandemic in relation to four SRH focus areas (contraception, safe abortion, GBV/IPV STIs including HIV), with data on SRH service access/utilisation by women and girls of reproductive age (15–49 years old). We excluded any study that reported effects of the SARS-CoV-2 virus/disease and only included studies that considered impacts of the COVID-19 pandemic response and/or mitigation measures. We excluded studies that did not meet the inclusion criteria on the basis of language, study dates, study type and SRH focus area. We also excluded studies on men as other reviews have focused on the SRH needs of this group during the COVID-19 pandemic.19
Data extraction
Data were extracted by HV using Covidence Data Extraction 2.0. Extracted information from each article included, country, study setting (urban vs rural), SRH service subject area(s), subgroups with distinct SRH needs included in analysis, metrics (units of measurement) and impact of the COVID-19 pandemic. Geographical region was recorded and classification applied according to the World Bank list of regions (June 2020).27
Reporting the results
We synthesised a narrative account of the major findings of included studies regarding the impact of the COVID-19 pandemic on access and utilisation of the four key SRH services. Studies were grouped by SRH focus area, study design, setting, study population and directionality (increase/decrease) in terms of the impact on access and/or utilisation. Qualitative manifest data were coded inductively and grouped into themes representing the major findings relating to how the pandemic impacted access and utilisation.
Patient and public involvement
Patients and the public were not involved in the design, conduct, reporting or dissemination plans of this review.
Results
Screening results
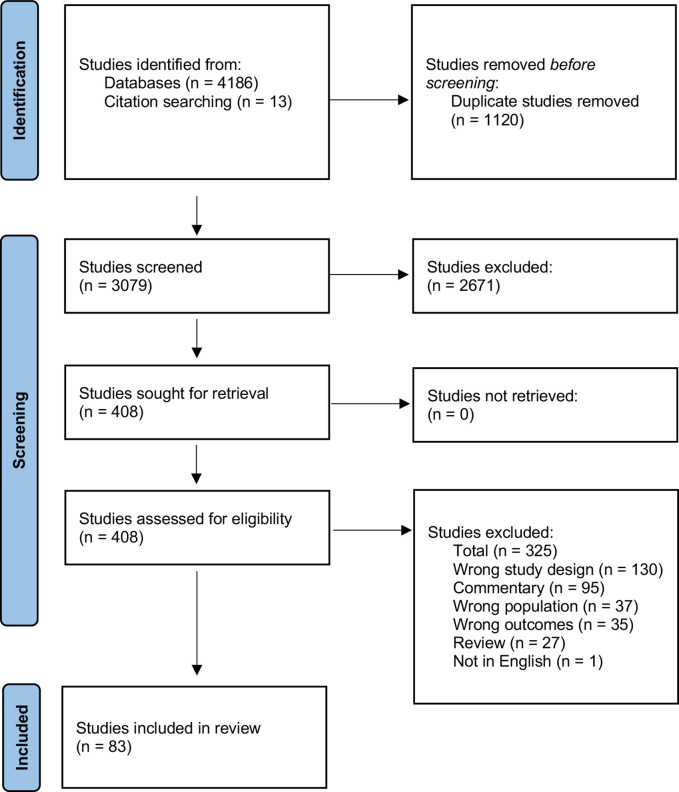
After the initial search, a total of 4186 studies were identified with 1120 duplicates removed. The remaining 3079 studies were subject to title and abstract review; 2671 were excluded at this screening phase. Following the screening of 421 full texts, 83 studies were included in the review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart mapping the results of this screening process is displayed in figure 1.
Figure 1.
PRISMA flow chart of included studies. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Characteristics of included studies
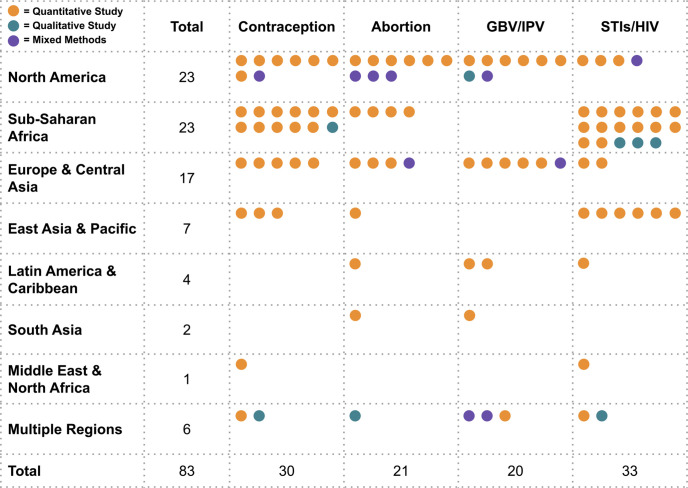
Studies were conducted in all seven major geographical (World Bank) regions of the world; 28% of the studies were done in North America,28–50 28% in sub-Saharan Africa,51–73 20% in Europe and Central Asia,74–90 8% in East Asia & Pacific,91–97 5% in Latin America and the Caribbean,98–101 2% in South Asia102 103 and 1% in the Middle East and North Africa.104 Studies were conducted in more than 34 countries. Of all included studies, 10 were conducted in multiple countries (five or more),79 80 85 90 105–110 six of which spanned multiple geographical regions.105–110 While most studies (61%) did not specify setting, a quarter took place in urban or periurban regions,32 37 38 40 46 48 52 55 56 59 63–66 71 72 81 88 89 96–99 8% in rural areas57 58 60 68 73 91 103 and 7% directly compared outcomes in urban versus rural areas.51 54 61 69 75 87 Online supplemental table 1 displays the characteristics of included studies. There was a relatively even distribution of studies across SRH focus areas: 30 (36%) provided evidence on the impact of the COVID-19 pandemic on access to or utilisation of contraceptive services,28 29 32 35 37 40 42 47 51–54 57 58 63 67 68 71 73 75 78 82 83 88 91 93 97 104 109 110 21 (25%) on abortion services,30 32–35 40 43 49–52 68 73 80 87 89 90 93 99 103 109 20 (24%) on GBV/IPV services28 31 36 38 39 45 46 48 74 76 77 81 84 86 98 101 102 105 107 109 and 33 (40%) on STI-related services.35 40 41 44 53 55–62 64–66 69–73 79 85 91–96 100 104 106 108 Figure 2 illustrates the distribution of studies among each of the four SRH service focus area by region and by study type.
Figure 2.
Distribution of studies by region, SRH service area and study design (n=83). SRH, sexual and reproductive health.
Findings from included studies
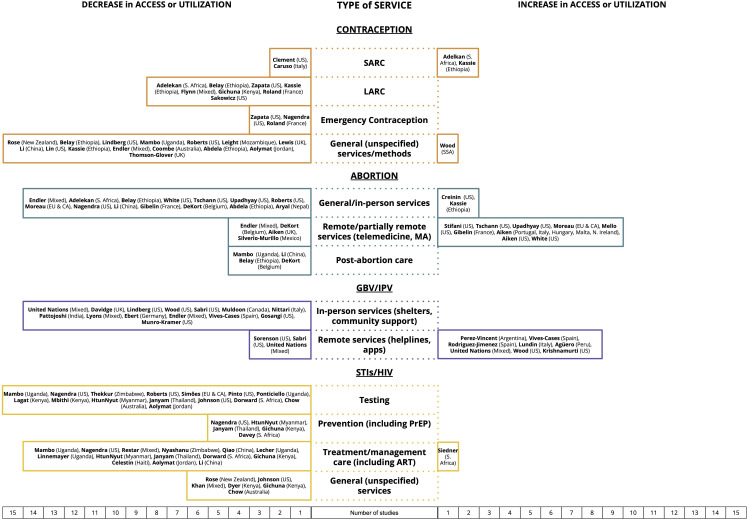
Figure 3 illustrates the number of studies that provide evidence within each SRH service areas, and the directionality of changes to access/utilisation. Further, we present our findings per SRH service area.
Figure 3.
Relative impact of COVID-19 on access and utilisation of SRH services (n=83). SRH, sexual and reproductive health.
Contraception services
Nearly one-third of studies (24, 30%) provided evidence of a decrease in access or utilisation of contraceptive services, evenly distributed across various contexts and populations.28 29 35 37 40 42 47 51–53 63 68 71 73 75 78 83 88 91 93 97 104 109 110 Utilisation of short-acting reversible contraception (SARC) was analysed by four studies in total,47 51 68 88 all of which provided evidence of reduced utilisation. Of these studies, two conducted in sub-Saharan Africa showed mixed results with an increase in SARC utilisation in some clinical contexts.51 68 Nonetheless, a large majority of included studies showed a decline in access to and utilisation of long-acting reversible contraception (LARC). Included studies found substantial declines in the administration of injectables and placement of LARCs,29 37 51 52 68 71 78 110 a reduction in tubal ligation procedures,52 challenges with scheduling LARC removal29 and reduced provision of emergency contraception.29 75 78
Many studies referenced access to contraceptive services more broadly—not specified by LARC/SARC—and 15 reported decreases in family planning attendance, appointment availability and declines in unspecified contraceptive method utilisation.28 35 42 52 53 63 68 73 75 83 91 93 97 104 109 For instance, Belay et al.52 noted a 27% reduction in clinic visits for contraception and a 67% reduction in postpartum visits in one tertiary hospital in Ethiopia, while 55% of clinics surveyed in a study in the USA had to cancel or postpone contraceptive visits due to the pandemic.35 More generally, among a survey of SRH clinicians and stakeholders in 29 countries, 86% perceived that access to contraceptive services was less or much less because of the pandemic.109 Only one study showed a slight increase in overall contraceptive utilisation in sub-Saharan Africa.54
Safe abortion services
In-person services for abortion were overwhelmingly curtailed during COVID-19 while remote services, such as online consultations for mailed medical abortion pills, saw an uptick in use. Fourteen studies documented a decrease in access to or utilisation of abortion services, including in-person services such as testing and consultations, medical abortion dispensation and surgical abortion procedures.30 33–35 40 51 52 73 80 87 89 93 103 109 These studies, which generally took place in areas with restrictive abortion policies, described precipitous drops in abortion clinic operations, evidenced by a 16% reduction in safe abortion services in Ethiopia,52 a 38% decrease in abortions performed in Texas,30 closure of 35% and 21% of SRH clinics providing abortion in the South and Midwest of the USA, respectively35 and a 26% decline in women accessing safe abortion services during lockdown in Nepal.103 Several studies reported difficulty accessing in-person services, which led some abortion clinics to remove requirements for ultrasounds and Rh factor testing to reduce the need for in-person visits.33 34 87 Access to postabortion care was negatively impacted as reported in China,93 Ethiopia,52 Uganda53 and Belgium.89 Two studies described an increase in abortion service utilisation at tertiary care facilities in the US49 and among teenagers in Ethiopia.68
Decreases in access or utilisation of remote or partially remote abortion services were described by three studies.88 89 108 Endler et al and DeKort et al observed declines in at-home medical abortion utilisation, and Aiken et al.90 found that telemedicine abortion requests through Women on Web, an online telemedicine abortion service, increased significantly in Portugal, Italy, Hungary, Malta and Northern Ireland, while they decreased significantly in the UK. This decrease is speculated to be caused by a change in abortion legislation in the UK, whereby access to no-test abortions through the formal health sector significantly increased. Several countries made policy changes during the pandemic to allow for medical abortion through telemedicine; these policy changes were more likely to be implemented in countries with liberal abortion laws, compared with countries with strict abortion laws.90 Nine studies found an increase in access and utilisation of remote or partially remote abortion services in countries with relatively liberal abortion laws.30 32–34 43 50 80 87 90
GBV and IPV services
Studies (14, 17%) on the impact of the COVID-19 pandemic on services for GBV/IPV described decreases in access or utilisation of in-person services.28 31 36 38 39 45 46 48 74 76 77 81 84 86 98 101 102 105 107 109 These studies described limited access to information and service availability,86 102 105 107 109 diversion of resources for GBV and sexual assault examinations to COVID-19 relief and limited medical resources to support survivors,31 38 39 81 105 a decrease in vacancies in shelters and operational capacity of safe-housing services,31 74 curtailed mutual aid, community support, advocacy and intervention services36 74 76 102 and challenges or delays in seeking support on being quarantined with an abuser.28 46 A multicountry survey found that financial instability and mobility restrictions robbed many women of the resources and mechanisms needed to leave the perpetrator of violence and seek refuge.107
Generally, remote (not in person) services for GBV and IPV saw higher rates of utilisation during the COVID-19 pandemic compared with before the pandemic. Indeed, eight studies found increases in utilisation of remote services for women experiencing GBV or IPV in high-income countries (HIC) and upper-middle income countries (UMIC).31 45 76 77 84 98 101 105 Calls to domestic violence helplines and antiviolence centres increased in Argentina,98 Spain,76 77 Italy,84 Peru,101 Malaysia, China, Somalia, Tunisia, Uruguay, Saint Vincent and Grenadines, Kenya, India and Zimbabwe.105 Wood et al.31 described a 51% increase in video conferences to provide client services at IPV and sexual assault-oriented agencies in the USA and Krishnamurti et al.45 found an increase in utilisation of an app-based IPV assessment during the shelter-in-place order in the USA. Despite a general increase in remote service utilisation, three studies documented decreases in utilisation of mobile services; two of these took place in the USA and found decreases in calls to ‘911’ and a sexual assault crisis hotline48 and reduced use of helplines by immigrant women experiencing IPV.36 In a multinational survey led by the United Nations, decreases in calls to helplines, hotlines, police and health centres in Ethiopia, Nepal, Trinidad and Tobago and Rwanda were reported.105
STIs/HIV services
Nearly half of included studies (40, 48%) found a decrease in access or utilisation of STIs/HIV services.35 40 41 44 53 55–62 64–66 69–73 79 85 91–96 100 104 106 108 STI testing reductions were reported in Uganda,53 the USA,35 Jordan,104 Thailand95 and Uganda.60 Simões et al.79 found that 95% of community STI testing clinics in 53 countries in Europe and Central Asia experienced decreased testing for all STIs, while Nagendra et al and Chow et al noted significant reductions in asymptomatic STI screening in the USA and Australia, respectively.40 96 Two US studies also reported reductions in testing volumes for chlamydia and gonorrhoea.41 44 The negative impact of the pandemic on HIV testing was documented in two studies in Kenya,61 66 one in the USA40 and one in Myanmar.94 Access to STI prevention services was also negatively impacted by the pandemic as documented by five studies. Among these findings were an 80% decrease in pre-exposure prophylaxis (PrEP) initiations and follow-up in the USA,40 qualitative reports of reduced barrier prevention and PrEP outreach services for sex workers in Myanmar,94 Thailand95 and Kenya,71 and increased incidence of missed PrEP follow-up visits among vulnerable women in South Africa.72
Evidence of the negative impact of the pandemic on access to services for treatment and management of STIs was reported by 14 studies.40 53 59 62 64 69 71 92–95 100 104 106 Difficulty accessing antiretroviral treatment (ART) was reported in several countries with a high incidence of HIV, including Zimbabwe,59 Uganda,53 64 South Africa,69 Kenya71 and Haiti,100 as well as Myanmar,94 Thailand,95 China92 93 and the USA.40 Lecher et al.62 found that viral load testing to monitor HIV status among PLWH decreased by 71% in all President’s Emergenct Plan For AIDS Relief (PEPFAR) -supported countries in March 2020. Restar et al.106 reported that less than half of trans and non-binary people living with HIV(PLWH) surveyed in a multicountry study perceived themselves to have unburdened access to HIV treatment. Seven additional studies noted a decrease in access to unspecified STI-related services.44 70 71 91 96 104 108 Only one study reported an increase in utilisation of STI-related services immediately after lockdown in South Africa.57 Three studies found that the COVID-19 pandemic did not significantly impact access to PrEP,65 availability of clinic visits for ART73 or HIV clinic operations.85
Reported barriers to access or utilisation of services
Several studies (33, 40%) provided evidence regarding challenges to access and utilisation of SRH services that were caused by the COVID-19 pandemic (table 1). Online supplemental figure 1 illustrates how reported barriers were distributed within each SRH focus area. Transportation and mobility restrictions, such as shutdown of public transport, curfews and abuse by police/soldiers at roadblocks, limited access to contraceptive services and GBV/IPV services in particular.35 53 59 60 64 65 71 83 91–93 97 103 105 107–109 On the demand side, increased financial burdens due to the pandemic, including the ability to pay for face masks, transportation and childcare, were reported equally within all SRH service areas except abortion.28 36 42 53 61 64 71 107 108 In addition, lack of information,53 59 83 86 91 105 fear of contracting COVID-19 at a service location and lack of privacy to schedule or attend appointments resulted in reduced SRH service access and utilisation.35 36 60 61 64 71 83 91 97 105 108 109 Self-censorship of needs also limited access to care for some individuals who sought contraception and STI/HIV services.82 90 On the supply side, limited availability of medical and social resources such as stockouts, shortages of staff, clinic closures and decrease in shelters were reported to have prohibited utilisation of services for all SRH services, HIV/STI, GBV/IPV and contraception especially.31 35 36 40 44 53 59 62 64 71 74 79 83 85 92 97 105 107 109 Furthermore, although telehealth was put in place as a response to COVID-19 as a way of improving access, technological challenges were reported as a barrier to care for some seeking contraception, GBV/IPV and abortion services.29 31 32 36 89 105 Finally, certain legal restrictions related to IPV/GBV (one study) and abortion (three studies), including labelling safe abortion as a non-essential service, negatively affected SRH service availability.34 35 80 107
Table 1.
Thematic summary of the reasons and reported challenges related to reduced access and utilisation of SRH services (n=33)
| Cause | Description | Study settings (n) | References |
| Transportation restrictions and disruptions (n=16) |
|
Australia (1), China (1), Kenya (1), Nepal (1), New Zealand (1), Uganda (3), UK (1), USA (2), Zimbabwe (1), mixed (4) | 34 41 52 58 59 63 64 70 82 90 91 96 102 104 106–108 |
| Financial burdens (n=9) |
|
Kenya (2), Uganda (2), USA (3), mixed (2) | 27 35 41 52 60 63 70 106 107 |
| Limited medical or social resources (n=19) |
|
Australia (1), China (1), Kenya (1), Uganda (3), UK (2), USA (5), Zimbabwe (1), EU&CA* (2), mixed (3) | 30 34 35 39 43 52 58 61 63 70 73 78 82 84 91 96 104 106 108 |
| Lack of information (n=6) |
|
Germany (1), New Zealand (1), Uganda (1), UK (1), Zimbabwe (1) mixed (1) | 52 58 82 85 90 104 |
| Legal restrictions and disruptions (n=4) |
|
US (2), EU&CA* (1), mixed (1) | 34 35 80 107 |
| Fear, safety or privacy concerns (n=12) |
|
Australia (1), Kenya (2), New Zealand (1), Uganda (2), UK (1), USA (2), mixed (3) | 34 35 59 60 63 70 82 90 96 104 107 108 |
| Technological challenges (n=6) |
|
Belgium (1), USA (4), SSA† (1) | 29 31 32 36 89 105 |
| Self-censorship of needs (n=2) |
|
New Zealand (1), UK (1) | 82 90 |
*EU&CA refers to Europe and Central Asia.
†SSA refers to sub-Saharan Africa.
IPV, intimate partner violence; SRH, sexual and reproductive health.
Impact of the COVID-19 pandemic on individuals with specific SRH needs
A minority of studies (16, 19%) included one or more subgroups with specific SRH needs in their analysis.28 36 42 53 65 68 70 71 75 83 91 93–95 105 106 Overall, these studies point to a negative impact on both access and utilisation of SRH services for these subpopulations who already experience disproportionately limited access to services (table 2). Among this subset of studies, seven described the impact on adolescents53 68 70 75 83 91 93 and three discussed the experiences of LGBTQIA+individuals28 91 106; these groups more commonly experienced self-censorship of needs and lack of information about available SRH care. One study described the impact on displaced people and refugees105 and four reported the impact on racial and ethnic minorities, immigrant groups or Indigenous peoples28 36 42 91; distinct hardships such as financial barriers to care were exacerbated for women who faced multiple forms of discrimination. Significant loss of income as well as travel restrictions affected the ability of sex workers to access STI testing, prevention and treatment services, as reported in four studies.65 71 94 95
Table 2.
The impact of the COVID-19 pandemic on subgroups with distinct SRH needs (n=16)
| Subgroup | Study (author, setting) | Impact of COVID-19 |
| Adolescents | Rose (New Zealand)91 |
Young people faced barriers for SRH care during lockdown including self-censorship of care-seeking, lack of privacy or transportation, lack of information about service availability and COVID-19 related concerns. |
| Mambo (Uganda)53 | Access to SRH information and services diminished among youths during lockdown due to lack of transportation, distance to health facilities and high cost of services. | |
| Thomson-Glover (UK)75 | Adolescents in both rural and urban settings exhibited a substantial decrease in attendance at sexual health services and less frequently used emergency contraception. | |
| Lewis (UK)83 | Young women and reported significant difficulties accessing contraception, including condoms, during the pandemic. Challenges were associated with a lack of in person appointments to start, stop, switch or continue contraceptive methods, lack of information about available care, fear of contracting COVID-19, risking privacy to access contraception and self-censorship of SRH needs. | |
| Li (China)93 | About one-third of sexually active adolescents reported difficulties accessing abortion, postabortion care, STI advice and management or contraceptives due to COVID-19. | |
| Kassie (Ethiopia)68 | The proportion of teenage pregnancy increased during the pandemic as well as the proportion of teenagers using abortion services, possibly indicating reduced access or utilisation of birth control among this group. | |
| Dyer (Kenya)70 | COVID-19 impacted adolescents living with HIV’s ability to access medical support and some had difficulty refilling ARVs, resulting a relatively high rate of missed ARV treatments. | |
| LGBTQIA+ identifying individuals | Rose (New Zealand)91 |
Respondents who identified as LGBTQIA+ were as likely as non-identifying respondents to have received SRH care during lockdown. |
| Lindberg (USA)28 | COVID-19 caused women to delay or cancel accessing SRH providers for contraception, an impact that was more pronounced for sexual minority women. | |
| Restar (mixed)106 | COVID-19 imposed burdens on accessing HIV treatment and prescription refills among trans and non-binary people living with HIV; nearly one-third of respondents reported not having access to an HIV provider since pandemic control measures were implemented. | |
| Displaced People and Refugees | United Nations (mixed)105 | COVID-19 resulted in a decrease in reporting of violence against women and limited access to social and health services; the situation is exacerbated for women and girls who face multiple forms of discrimination, such as refugees and migrant workers. |
| Racial and ethnic minorities, immigrant groups and Indigenous peoples | Rose (New Zealand)91 |
Indigenous Māori women were less likely than NZ European, Pacific Islander or Asian respondents to have been able to access SRH care during the pandemic. |
| Lindberg (USA)28 | Hispanic and non-Hispanic black women were more likely to have experienced pandemic-related delays or cancellations of contraceptive care or other SRH services. | |
| Sabri (USA)36 | Immigrant survivors of IPV, particularly those who are undocumented, faced distinct hardships in accessing care due to greater financial hurdles and lack of public benefits such as unemployment and government assistance including medical insurance. | |
| Lin (USA)42 | Racial minority women disproportionately struggled to access contraceptive care, including being able to access a pharmacy, afford care, get a prescription or get a LARC method replaced or removed; this was largely due to decreased financial assets. | |
| Sex workers | Mantell (Kenya)65 | Though the pandemic did not significantly impact sex workers enrolled in an active RCT’s access to provided PrEP, where access was impacted it was primarily due to difficulties travelling to pick up medication. |
| Htun Nyunt (Myanmar)94 | COVID-19 impacted HIV prevention services such as condom distribution and HIV testing for female sex workers. The pandemic caused a decrease in ART initiation immediately following stay-at-home order. Most HIV services were returned to prepandemic levels by June 2020. | |
| Janyam (Thailand)95 | COVID-19 significantly impacted sex workers' ability to access STI testing a treatment as well as STI prevention services such as condoms, PrEP and drug treatment services. Sex workers with HIV reported difficulties accessing ART. Loss of access may be explained in part by significant loss of income and travel restrictions. | |
| Gichuna (Kenya)71 | COVID-19 restriction measures has had detrimental impacts on access to SRH services for sex workers living in informal settlements outside of Nairobi. Curfews, police mistreatment, fear of COVID-19, social distancing measures, contraceptive shortages and financial losses contribute to reduced access/utilisation of contraception and HIV treatment. |
ART, antiretroviral treatment; IPV, intimate partner violence; LARC, long-acting reversible contraception; SRH, sexual and reproductive health.
Discussion
In this scoping review, we found that women and girls faced reduced access to key SRH services globally due to the COVID-19 pandemic and related mitigation efforts, which resulted in decreased utilisation of SRH services compared with previous years. We found that there were significant gaps in the geographical distribution of this body of research. The majority of included research has been conducted on populations in North America and sub-Saharan Africa, with a disproportionate focus on the USA at the national level (22 out of 83). Overall, studies were significantly less representative of countries in East Asia and the Pacific—where COVID-19 restrictions were very strict111—Latin America and the Caribbean, South Asia, the Middle East and North Africa compared with North America, sub-Saharan Africa, Europe and Central Asia. Differences in demand for SRH services cannot entirely explain the geographical unevenness of this research field. For example, as of 2019, the abortion rate per 1000 women of reproductive age was highest in West Asia and North Africa, a region in which no studies were conducted to assess the impact of the COVID-19 pandemic on abortion access, and second highest in South Asia, which only had one study on this topic.112
We found that decreases in contraceptive access and utilisation during to the COVID-19 pandemic were observed globally, which compromises progress towards the SDGs and may leave millions of women vulnerable to unwanted pregnancies.3 113 We found that the same barriers that prevented women from accessing contraception also prevented access to abortion consultations, procedures and postabortion care. It is known that when barriers to safe abortion exist, such as legal restrictions, women are more likely to turn to unsafe methods.114 However, none of the included studies reported on utilisation of unsafe abortion methods to compensate for reduced access to safe abortion. Consequently, it remains unclear whether efforts aimed at increasing the portion of abortions that are safely self-managed curbed a projected increase in unsafe abortion. Many studies reported that COVID-19 mitigation measures inadvertently reduced access to GBV/IPV related circumstances; this is particularly troubling as researchers have determined a correlation between pandemic stressors and IPV115 with an increase in the incidence of IPV during stay-at-home orders.116 The increase in IPV incidence may be the cause of the increase in utilisation of remote GBV/IPV services; however, more research is necessary to identify the effectiveness of remote GBV prevention and intervention services.117
Specific challenges posed by the COVID-19 pandemic on SRH services are critical to understand in order to restore and ensure access to essential SRH care during future pandemics. We saw that some reported challenges were distributed unevenly across geographical regions and selected SRH services. For instance, challenges such as reliance on public transportation, living far from SRH service providers, relying on income from a job sector affected by the pandemic and technology-related issues were cited more often in studies from countries in sub-Saharan Africa such as Uganda, Zimbabwe and Kenya. These countries are classified as low and lower middle income and experience significantly higher rates of poverty than the global average27; thus, this trend in reported barriers reflects a disproportionate burden of the COVID-19 pandemic in economically disadvantaged settings.53 59–61 64 65 71 103 Concurrently, limited resources, such as clinic closures, stock outs and financial burdens were reported less frequently in studies focusing on abortion services. In response to social distancing measures and limited in-person service capacity, many SRH service providers, particularly in the USA and Europe, reported that they adopted telemedicine as a service delivery model, primarily for abortion, but also for contraceptive counselling and GBV/IPV. In many settings, telemedicine is a highly acceptable alternative to in-person treatment as it can reduce risk of contracting COVID-19, minimise travel time and increase patient ease and comfort.32 34 91 108 Our review findings support the notion that the pandemic has accelerated a shift from in-person care to self-management through telemedicine, which may have maintained access to safe abortion services89 and could partly explain why abortion services were less impacted by both supply and demand side challenges. Still, telehealth may have limitations in some circumstances such as lack of privacy,91 technological challenges29 32 105 and reduced perceived comfort and safety related to GBV/IPV services.31 36 Further research is warranted to inform where telemedicine in connection to SRH services is beneficial and where it may exacerbate healthcare inequities.
Although few studies included populations such as refugees, ethnic minorities, lesbian, bisexual, transgender, queer, intersex, and asexual (LGBTQIA+) individuals and adolescents, our findings suggest that the COVID-19 pandemic has disproportionately impacted SRH access and utilisation for groups with specific SRH needs. The SRH needs of these groups differ only slightly from women in general; however, distinct barriers to accessing care engender unique needs in order to achieve sexual and reproductive justice.118–121 For instance, displaced people and refugees are at a heightened risk of sexual assault and gender-based violence in crisis settings105 but face increased barriers to access to SRH services during humanitarian emergencies; this is characterised by discontinuation of contraceptive services, increased rates of unsafe abortion and substandard STI and HIV care.122 It can be assumed that these challenges were aggravated during the pandemic; however, more evidence is necessary to properly inform the extent of harm to refugee populations. LGBTQIA+ individuals have similar SRH needs to adults and adolescents; however, accessing these needs is often prohibited by stigma, discrimination and even violence.123 Most lesbian, gay and transgender youth have not disclosed their sexual orientation to healthcare providers124; this undermines care quality and poses difficulties in collecting accurate data on the specific needs of this group. This may be reflected in the dearth of studies characterising their experiences during the pandemic.
Indigenous people are another population with distinct SRH needs who have and continue to face disempowerment, discrimination and erasure and have consistently been insufficiently addressed in healthcare policies and programmes, particularly during infectious disease outbreaks.118–121 Indigenous women worldwide are at an increased risk of GBV including sexual and physical abuse125; as global rates of sexual assault and violence increase during pandemics, it is imperative to understand and address access to SRH care including GBV services for Indigenous women. Only a small number of studies looked at the impact of the COVID-19 pandemic on sex workers,65 71 94 95 who require consistent access to contraceptives and STI/HIV services. This may be because in-person sex work was difficult during social distancing making this population especially hard to reach. The fact that only one included study considered the perspectives of people with intersecting identities or who face multiple forms of discrimination highlights a significant research gap that must be bridged in order to fully appreciate the impact of the COVID-19 pandemic.
The findings of this review have implications for policy, research and practice. We highlight the geographical unevenness of this research field and suggest the allocation of research to regions, particularly Latin America, the Caribbean, South Asia, the Middle East and North Africa, in which the impacts of the COVID-19 pandemic on SRH are less understood. Moreover, research efforts should prioritise study populations with intersecting identities for which barriers to SRH care are exacerbated and marginalised groups who faced a disproportionate burden of impact by the COVID-19 pandemic. Specific research questions have arisen from this review, such as the impact of the pandemic on the incidence and risk of unsafe abortion. Insofar as policy, supply-side barriers to care may be alleviated by automatic allocation of funds and resources to maintain SRH services during public health emergencies. This review provides evidence for liberal policies with regard to reproductive choice, as countries with laws that protect abortion access tended to report an increase in utilisation of safe, remote abortion services, while settings with more restrictive laws reported a decrease in abortion access. Banke-Thomas and Yaya117 highlighted service delivery adaptations that have been implemented to resolve demand-side barriers such as free ride shares to clinics,126 family planning commodity delivery6 and informational social media campaigns.127 Given supply-side barriers such as transportation disruptions and fear of clinic attendance, clinical practices adaptations that minimise the frequency of or combine provider visits (eg, contraception and STI testing/treatment) may increase accessibility. Further research on the efficacy, equity and acceptability of these interventions is necessary to inform their continued use.
A key strength of this review is the breadth of systematic database screening and number of studies reviewed. The scoping review protocol allowed for consideration and inclusion of various study designs within multiple SRH subject areas. We included studies from a variety of settings, representing research from high-income to low-income countries, which showcased the inherent disparities in SRH research volume among certain regions. This work is also strengthened by the inclusion of research that examined the unique impact of the COVID-19 pandemic on groups with distinct SRH needs. A limitation of this work is that it excluded studies not published in English, which may have incorporated bias in the geographical distribution of published research.
Conclusion
We found that the COVID-19 pandemic impacted access to and utilisation of contraceptive services, safe abortion services, IPV/GBV and STI/HIV services negatively across the globe. The studies included in this review reported reduced utilisation of contraception services, particularly LARC, and diminished access to safe abortion services, which threaten progress towards the SDGs. Furthermore, survivors of GBV and IPV faced reduced access to in-person services such as shelters and social support networks, despite increased demand. Access and utilisation of HIV/STI testing, prevention, treatment/care and counselling were also curtailed by the COVID-19 pandemic. Our work evidences the scarcity of SRH research in settings with high burden of disease and on marginalised groups with distinct SRH needs, underscoring a theme of widened health disparities caused by the pandemic. As the COVID-19 pandemic continues, findings from this review highlight the importance of maintaining access to SRH services to ensure that traction towards global development goals are not lost. There is a clear need for policy and practice adaptations that maintain and improve access to SRH services now and in future public health crises.
Acknowledgments
We are grateful to search expert Anja Vikingson, at Karolinska Institutet, Solna, who supported the creation and adaptations of the search strategy.
Footnotes
Handling editor: Seye Abimbola
Twitter: @Moazzam2000
Contributors: AT conceived of the research aim and conceptualised together with AC, ECL and KG-D. AC, AT, ECL, ME, HV, HK and KG-D designed the study. AC and HV created the search strategy, and HV conducted the literature searches. Data were collected and organised by HV as first reviewer, and HK as second reviewer supported by ECL and ME as senior reviewers and supervised by AC. AC is the guarantor of this work. All authors contributed to interpretation and writing and approved of the final version of the manuscript.
Funding: This work was partly funded by the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the WHO.
Disclaimer: The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The views expressed in this article are those of the authors and do not represent the views of the WHO or HRP.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Wenham C. The gendered impact of the COVID-19 crisis and post-crisis period, 2020. [Google Scholar]
- 2.Wenham C, Smith J, Davies SE, et al. Women are most affected by pandemics — lessons from past outbreaks. Nature 2020;583:194–8. 10.1038/d41586-020-02006-z [DOI] [PubMed] [Google Scholar]
- 3.Riley T, Sully E, Ahmed Z, et al. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low- and middle-income countries. Int Perspect Sex Reprod Health 2020;46:73–6. 10.1363/46e9020 [DOI] [PubMed] [Google Scholar]
- 4.Cousins S. COVID-19 has “devastating” effect on women and girls. The Lancet 2020;396:301–2. 10.1016/S0140-6736(20)31679-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UNFPA . Impact of COVID-19 on family planning: what we know one year into the pandemic, 2021. [Google Scholar]
- 6.Church K, Gassner J, Elliott M. Reproductive health under COVID-19 - challenges of responding in a global crisis. Sex Reprod Health Matters 2020;28:1773163–3. 10.1080/26410397.2020.1773163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nash E. State policy trends 2021: the worst year for abortion rights in almost half a century; 2021.
- 8.Azcona G, Bhatt A, Encarnacion J. From insights to action: gender equality in the wake of COVID-19 United Nations; 2020. [Google Scholar]
- 9.Barton-Knott S. Forty years into the HIV epidemic, AIDS remains the leading cause of death of women of reproductive age-UNAIDS calls for BOLD action. 20th International AIDS Conference, 2020. [Google Scholar]
- 10.Hogan AB, Jewell BL, Sherrard-Smith E, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;8:e1132–41. 10.1016/S2214-109X(20)30288-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guaraldi G, Borghi V, Milic J, et al. The impact of COVID-19 on UNAIDS 90-90-90 targets: calls for new HIV care models. Open Forum Infect Dis 2021;8:1–4. 10.1093/ofid/ofab283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goga A, Bekker LG, Van de Perre P, et al. Centring adolescent girls and young women in the HIV and COVID-19 responses. The Lancet 2020;396:1864–6. 10.1016/S0140-6736(20)32552-6 [DOI] [PubMed] [Google Scholar]
- 13.Zulaika G, Bulbarelli M, Nyothach E, et al. Impact of COVID-19 lockdowns on adolescent pregnancy and school dropout among secondary schoolgirls in Kenya. BMJ Glob Health 2022;7:e007666. 10.1136/bmjgh-2021-007666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UN Women . COVID-19 and ending violence against women and girls UN Women Headquaters; 2020. [Google Scholar]
- 15.Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health 2021;9:e759–72. 10.1016/S2214-109X(21)00079-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kotlar B, Gerson E, Petrillo S, et al. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health 2021;18:10. 10.1186/s12978-021-01070-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolarinwa OA, Ahinkorah BO, Seidu A-A, et al. Mapping evidence of impacts of covid-19 outbreak on sexual and reproductive health: a scoping review. Healthcare 2021;9. 10.3390/healthcare9040436. [Epub ahead of print: 08 04 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Townsend R, Chmielewska B, Barratt I, et al. Global changes in maternity care provision during the COVID-19 pandemic: a systematic review and meta-analysis. EClinicalMedicine 2021;37:100947. 10.1016/j.eclinm.2021.100947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar N, Janmohamed K, Nyhan K, et al. Sexual health (excluding reproductive health, intimate partner violence and gender-based violence) and COVID-19: a scoping review. Sex Transm Infect 2021;97:402–10. 10.1136/sextrans-2020-054896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mukherjee TI, Khan AG, Dasgupta A, et al. Reproductive justice in the time of COVID-19: a systematic review of the indirect impacts of COVID-19 on sexual and reproductive health. Reprod Health 2021;18:252. 10.1186/s12978-021-01286-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tolu LB, Feyissa GT, Jeldu WG. Guidelines and best practice recommendations on contraception and safe abortion care service provision amid covid-19 pandemic: Scoping review. EJRH 2021;13:11–20. 10.21203/rs.3.rs-25326/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141–6. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 23.Tricco A, Zarin LE, O’Brien K. Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) checklist section. Ann Intern Med 2018;169:11–12. 10.7326/M18-0850.2 [DOI] [Google Scholar]
- 24.Peters MD, Godfrey CM, McInerney P. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI scoping reviews, 2015. [Google Scholar]
- 25.Obrist B, Iteba N, Lengeler C, et al. Access to health care in contexts of livelihood insecurity: a framework for analysis and action. PLoS Med 2007;4:1584–8. 10.1371/journal.pmed.0040308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lazarus JV, Palayew A, Rasmussen LN, et al. Searching PubMed to retrieve publications on the COVID-19 pandemic: comparative analysis of search strings. J Med Internet Res 2020;22:e23449. 10.2196/23449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World bank (world development indicators), list of economies (June 2020), 2020
- 28.Lindberg L, VandeVusse A, Mueller J. Early impacts of the COVID-19 pandemic: findings from the 2020 Guttmacher survey of reproductive health experiences. New York: Guttmacher Instutute, 2020. 10.1363/2020.31482 [DOI] [Google Scholar]
- 29.Zapata LB, Curtis KM, Steiner RJ, et al. COVID-19 and family planning service delivery: findings from a survey of U.S. physicians. Prev Med 2021;150:106664. 10.1016/j.ypmed.2021.106664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White K, Kumar B, Goyal V, et al. Changes in abortion in Texas following an executive order ban during the coronavirus pandemic. JAMA 2021;325:691–3. 10.1001/jama.2020.24096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wood L, Schrag RV, Baumler E, et al. On the front lines of the COVID-19 pandemic: occupational experiences of the intimate partner violence and sexual assault workforce. J Interpers Violence 2022;37:NP9345–66. 10.1177/0886260520983304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stifani BM, Avila K, Levi EE. Telemedicine for contraceptive counseling: an exploratory survey of US family planning providers following rapid adoption of services during the COVID-19 pandemic. Contraception 2021;103:157–62. 10.1016/j.contraception.2020.11.006 [DOI] [PubMed] [Google Scholar]
- 33.Tschann M, Ly ES, Hilliard S, et al. Changes to medication abortion clinical practices in response to the COVID-19 pandemic. Contraception 2021;104:77–81. 10.1016/j.contraception.2021.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Upadhyay UD, Schroeder R, Roberts SCM. Adoption of no-test and telehealth medication abortion care among independent abortion providers in response to COVID-19. Contracept X 2020;2:100049. 10.1016/j.conx.2020.100049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roberts SCM, Schroeder R, Joffe C. COVID-19 and independent abortion providers: findings from a rapid-response survey. Perspect Sex Reprod Health 2020;52:217–25. 10.1363/psrh.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sabri B, Hartley M, Saha J, et al. Effect of COVID-19 pandemic on women's health and safety: a study of immigrant survivors of intimate partner violence. Health Care Women Int 2020;41:1294–312. 10.1080/07399332.2020.1833012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sakowicz A, Matovina C, Imeroni S, et al. 591 the association between COVID-19 related health services changes and postpartum contraception. Am J Obstet Gynecol 2021;224:S372. 10.1016/j.ajog.2020.12.612 [DOI] [Google Scholar]
- 38.Muldoon KA, Denize KM, Talarico R, et al. COVID-19 pandemic and violence: rising risks and decreasing urgent care-seeking for sexual assault and domestic violence survivors. BMC Med 2021;19:20. 10.1186/s12916-020-01897-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Munro-Kramer ML, Cannon LM, Scheiman L, et al. Accessing healthcare services during the COVID-19 pandemic: the plight of sexual assault survivors. J Forensic Nurs 2021;17:93–7. 10.1097/JFN.0000000000000326 [DOI] [PubMed] [Google Scholar]
- 40.Nagendra G, Carnevale C, Neu N, et al. The potential impact and availability of sexual health services during the COVID-19 pandemic. Sex Transm Dis 2020;47:434–6. 10.1097/OLQ.0000000000001198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pinto CN, Niles JK, Kaufman HW, et al. Impact of the COVID-19 pandemic on chlamydia and gonorrhea screening in the U.S. Am J Prev Med 2021;61:386–93. 10.1016/j.amepre.2021.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin TK, Law R, Beaman J, et al. The impact of the COVID-19 pandemic on economic security and pregnancy intentions among people at risk of pregnancy. Contraception 2021;103:380–5. 10.1016/j.contraception.2021.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mello K, Smith MH, Hill BJ, et al. Federal, state, and institutional barriers to the expansion of medication and telemedicine abortion services in Ohio, Kentucky, and West Virginia during the COVID-19 pandemic. Contraception 2021;104:111–6. 10.1016/j.contraception.2021.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson KA, Burghardt NO, Tang EC, et al. Measuring the impact of the COVID-19 pandemic on sexually transmitted diseases public health surveillance and program operations in the state of California. Sex Transm Dis 2021;48:606–13. 10.1097/OLQ.0000000000001441 [DOI] [PubMed] [Google Scholar]
- 45.Krishnamurti T, Davis AL, Quinn B, et al. Mobile remote monitoring of intimate partner violence among pregnant patients during the COVID-19 shelter-in-place order: quality improvement pilot study. J Med Internet Res 2021;23:e22790. 10.2196/22790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gosangi B, Park H, Thomas R, et al. Exacerbation of physical intimate partner violence during COVID-19 pandemic. Radiology 2021;298:E38–45. 10.1148/radiol.2020202866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clement J, Jacobi M, Greenwood BN. Patient access to chronic medications during the Covid-19 pandemic: evidence from a comprehensive dataset of US insurance claims. PLoS One 2021;16:e0249453. 10.1371/journal.pone.0249453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sorenson SB, Sinko L, Berk RA. The endemic amid the pandemic: seeking help for violence against women in the initial phases of COVID-19. J Interpers Violence 2021;36:4899–915. 10.1177/0886260521997946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Creinin MD, Tougas H, Wilson M, et al. Coronavirus disease 2019 impact on abortion care at a northern California tertiary family planning program. Am J Obstet Gynecol 2021;225:94-95. 10.1016/j.ajog.2021.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aiken ARA, Starling JE, Gomperts R, et al. Demand for Self-Managed online telemedicine abortion in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Obstet Gynecol 2020;136:835–7. 10.1097/AOG.0000000000004081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adelekan T, Mihretu B, Mapanga W, et al. Early effects of the COVID-19 pandemic on family planning utilisation and termination of pregnancy services in Gauteng, South Africa: March–April 2020. Wits J Clin Med 2020;2:91–52. 10.18772/26180197.2020.v2n2a7 [DOI] [Google Scholar]
- 52.Belay L, Hurisa T, Abbas F. Effect of COVID-19 pandemic on safe abortion and contraceptive services and mitigation measures: a case study from a tertiary facility in Ethiopia. EJRH 2020;12:51–7. [Google Scholar]
- 53.Mambo SB, Sikakulya FK, Ssebuufu R. Factors that influences access and utilisation of sexual and reproductive health services among Ugandan youths during the COVID-19 pandemic lockdown: an online cross-sectional survey. Research Square 2020. 10.21203/rs.3.rs-48529/v4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wood SN, Karp C, OlaOlorun F, et al. Need for and use of contraception by women before and during COVID-19 in four sub-Saharan African geographies: results from population-based national or regional cohort surveys. Lancet Glob Health 2021;9:e793–801. 10.1016/S2214-109X(21)00105-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thekkur P, Takarinda KC, Timire C, et al. Operational research to assess the real-time impact of COVID-19 on TB and HIV services: the experience and response from health facilities in Harare, Zimbabwe. Trop Med Infect Dis 2021;6. 10.3390/tropicalmed6020094. [Epub ahead of print: 31 May 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thekkur P, Tweya H, Phiri S, et al. Assessing the impact of COVID-19 on TB and HIV programme services in selected health facilities in Lilongwe, Malawi: operational research in real time. Trop Med Infect Dis 2021;6. 10.3390/tropicalmed6020081. [Epub ahead of print: 19 May 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Siedner MJ, Kraemer JD, Meyer MJ, et al. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: a longitudinal cohort study. medRxiv 2020. 10.1101/2020.05.15.20103226. [Epub ahead of print: 20 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Siedner MJ, Kraemer JD, Meyer MJ, et al. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: an interrupted time series analysis. BMJ Open 2020;10:e043763. 10.1136/bmjopen-2020-043763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nyashanu M, Chireshe R, Mushawa F, et al. Exploring the challenges of women taking antiretroviral treatment during the COVID-19 pandemic lockdown in peri-urban Harare, Zimbabwe. Int J Gynaecol Obstet 2021;154:220–6. 10.1002/ijgo.13771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ponticiello M, Mwanga-Amumpaire J, Tushemereirwe P, et al. "everything is a mess": how COVID-19 is impacting engagement with HIV testing services in rural Southwestern Uganda. AIDS Behav 2020;24:3006–9. 10.1007/s10461-020-02935-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lagat H, Sharma M, Kariithi E, et al. Impact of the COVID-19 pandemic on HIV testing and assisted partner notification services, Western Kenya. AIDS Behav 2020;24:3010–3. 10.1007/s10461-020-02938-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lecher SL, Naluguza M, Mwangi C, et al. Notes from the field: impact of the COVID-19 Response on Scale-Up of HIV viral load testing - PEPFAR-supported countries, January-June 2020. MMWR Morb Mortal Wkly Rep 2021;70:794–5. 10.15585/mmwr.mm7021a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Leight J, Hensly C, Chissano M, et al. Short-term effects of the COVID-19 state of emergency on contraceptive access and utilization in Mozambique. PLoS One 2021;16:e0249195. 10.1371/journal.pone.0249195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Linnemayr S, Jennings Mayo-Wilson L, Saya U, et al. HIV care experiences during the COVID-19 pandemic: mixed-methods telephone interviews with Clinic-Enrolled HIV-infected adults in Uganda. AIDS Behav 2021;25:28–39. 10.1007/s10461-020-03032-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mantell JE, Franks J, Lahuerta M, et al. Life in the balance: young female sex workers in Kenya weigh the risks of COVID-19 and HIV. AIDS Behav 2021;25:1323–30. 10.1007/s10461-020-03140-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mbithi I, Thekkur P, Chakaya JM, et al. Assessing the real-time impact of COVID-19 on TB and HIV services: the experience and response from selected health facilities in Nairobi, Kenya. Trop Med Infect Dis 2021;6. 10.3390/tropicalmed6020074. [Epub ahead of print: 10 May 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Karp C, Wood SN, Guiella G, et al. Contraceptive dynamics during COVID-19 in sub-Saharan Africa: longitudinal evidence from Burkina Faso and Kenya. BMJ Sex Reprod Health 2021;47:252–60. 10.1136/bmjsrh-2020-200944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kassie A, Wale A, Yismaw W. Impact of coronavirus Diseases-2019 (COVID-19) on utilization and outcome of reproductive, maternal, and newborn health services at governmental health facilities in South West Ethiopia, 2020: comparative cross-sectional study. Int J Womens Health 2021;13:479–88. 10.2147/IJWH.S309096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dorward J, Khubone T, Gate K, et al. The impact of the COVID-19 lockdown on HIV care in 65 South African primary care clinics: an interrupted time series analysis. Lancet HIV 2021;8:e158–65. 10.1016/S2352-3018(20)30359-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dyer J, Wilson K, Badia J, et al. The psychosocial effects of the COVID-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav 2021;25:68–72. 10.1007/s10461-020-03005-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gichuna S, Hassan R, Sanders T, et al. Access to healthcare in a time of COVID-19: sex workers in crisis in Nairobi, Kenya. Glob Public Health 2020;15:1430–42. 10.1080/17441692.2020.1810298 [DOI] [PubMed] [Google Scholar]
- 72.Davey DLJ, Bekker L-G, Mashele N, et al. Prep retention and prescriptions for pregnant women during COVID-19 lockdown in South Africa. Lancet HIV 2020;7:e735. 10.1016/S2352-3018(20)30226-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Abdela SG, Berhanu AB, Ferede LM, et al. Essential healthcare services in the face of COVID-19 prevention: experiences from a referral hospital in Ethiopia. Am J Trop Med Hyg 2020;103:1198–200. 10.4269/ajtmh.20-0464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Davidge S. A perfect storm: the impact of the Covid-19 pandemic on domestic abuse survivors and the services supporting them. Bristol, UK: Women’s Aid; 2020. https://www.womensaid.org.uk/a-perfect-storm-the-impact-of-the-covid-19-pandemic-on-domestic-abuse-survivors-and-the-services-supporting-them/ [Google Scholar]
- 75.Thomson-Glover R, Hamlett H, Weston D, et al. Coronavirus (COVID-19) and young people's sexual health. Sex Transm Infect 2020;96:473–4. 10.1136/sextrans-2020-054699 [DOI] [PubMed] [Google Scholar]
- 76.Vives-Cases C, Parra-Casado DL, Estévez JF, et al. Intimate partner violence against women during the COVID-19 Lockdown in Spain. Int J Environ Res Public Health 2021;18:9. 10.3390/ijerph18094698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rodriguez-Jimenez R, Fares-Otero NE, García-Fernández L. Gender-based violence during COVID-19 outbreak in Spain. Psychol Med 2020:1–2. 10.1017/S0033291720005024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roland N, Drouin J, Desplas D, et al. Effects of the coronavirus disease 2019 (COVID-19) Lockdown on the use of contraceptives and ovulation Inductors in France. Obstet Gynecol 2021;137:415–7. 10.1097/AOG.0000000000004281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Simões D, Stengaard AR, Combs L, et al. Impact of the COVID-19 pandemic on testing services for HIV, viral hepatitis and sexually transmitted infections in the who European region, March to August 2020. Euro Surveill 2020;25. 10.2807/1560-7917.ES.2020.25.47.2001943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moreau C, Shankar M, Glasier A, et al. Abortion regulation in Europe in the era of COVID-19: a spectrum of policy responses. BMJ Sex Reprod Health 2021;47:e14. 10.1136/bmjsrh-2020-200724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nittari G, Sagaro GG, Feola A, et al. First surveillance of violence against women during COVID-19 lockdown: experience from "niguarda" hospital in Milan, Italy. Int J Environ Res Public Health 2021;18. 10.3390/ijerph18073801. [Epub ahead of print: 06 04 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lete I, Novalbos J, de la Viuda E, et al. Impact of the lockdown Due to COVID-19 pandemic in the use of combined hormonal oral contraception in Spain - results of a National Survey: encovid. Open Access J Contracept 2021;12:103–11. 10.2147/OAJC.S306580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lewis R, Blake C, Shimonovich M, et al. Disrupted prevention: condom and contraception access and use among young adults during the initial months of the COVID-19 pandemic. An online survey. BMJ Sex Reprod Health 2021;47:269-276. 10.1136/bmjsrh-2020-200975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lundin R, Armocida B, Sdao P, et al. Gender-based violence during the COVID-19 pandemic response in Italy. J Glob Health 2020;10:20359. 10.7189/jogh.10.020359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kowalska JD, Skrzat-Klapaczyńska A, Bursa D, et al. HIV care in times of the COVID-19 crisis - Where are we now in Central and Eastern Europe? Int J Infect Dis 2020;96:311–4. 10.1016/j.ijid.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ebert C, Steinert JI. Prevalence and risk factors of violence against women and children during COVID-19, Germany. Bull World Health Organ 2021;99:429–38. 10.2471/BLT.20.270983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gibelin K, Agostini A, Marcot M, et al. COVID-19 impact in abortions' practice, a regional French evaluation. J Gynecol Obstet Hum Reprod 2021;50:102038. 10.1016/j.jogoh.2020.102038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Caruso S, Rapisarda AMC, Minona P. Sexual activity and contraceptive use during social distancing and self-isolation in the COVID-19 pandemic. Eur J Contracept Reprod Health Care 2020;25:445–8. 10.1080/13625187.2020.1830965 [DOI] [PubMed] [Google Scholar]
- 89.De Kort L, Wouters E, Van de Velde S. Obstacles and opportunities: a qualitative study of the experiences of abortion centre staff with abortion care during the first COVID-19 lockdown in Flanders, Belgium. Sex Reprod Health Matters 2021;29:180–95. 10.1080/26410397.2021.1921901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aiken ARA, Starling JE, Gomperts R, et al. Demand for self-managed online telemedicine abortion in eight European countries during the COVID-19 pandemic: a regression discontinuity analysis. BMJ Sex Reprod Health 2021;47:238–45. 10.1136/bmjsrh-2020-200880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rose SB, Garrett SM, McKinlay EM, et al. Access to sexual healthcare during New Zealand's COVID-19 lockdown: cross-sectional online survey of 15-24-year-olds in a high deprivation region. BMJ Sex Reprod Health 2021;47:277–84. 10.1136/bmjsrh-2020-200986 [DOI] [PubMed] [Google Scholar]
- 92.Qiao S, Yang X, Sun S, et al. Challenges to HIV service delivery and the impacts on patient care during COVID-19: perspective of HIV care providers in Guangxi, China. AIDS Care 2021;33:559–65. 10.1080/09540121.2020.1849532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li G, Tang D, Song B, et al. Impact of the COVID-19 pandemic on partner relationships and sexual and reproductive health: cross-sectional, online survey study. J Med Internet Res 2020;22:e20961. 10.2196/20961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Htun Nyunt O, Wan NMA, Soan P, et al. How Myanmar is working to maintain essential services for people living with HIV and key populations during the Covid-19 pandemic. J Int Assoc Provid AIDS Care 2021;20:232595822110177. 10.1177/23259582211017742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Janyam S, Phuengsamran D, Pangnongyang J, et al. Protecting sex workers in Thailand during the COVID-19 pandemic: opportunities to build back better. WHO South East Asia J Public Health 2020;9:100–3. 10.4103/2224-3151.294301 [DOI] [PubMed] [Google Scholar]
- 96.Chow EPF, Hocking JS, Ong JJ, et al. Sexually transmitted infection diagnoses and access to a sexual health service before and after the National Lockdown for COVID-19 in Melbourne, Australia. Open Forum Infect Dis 2021;8:10. 10.1093/ofid/ofaa536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Coombe J, Kong F, Bittleston H, et al. Contraceptive use and pregnancy plans among women of reproductive age during the first Australian COVID-19 lockdown: findings from an online survey. Eur J Contracept Reprod Health Care 2021;26:1–14. 10.1080/13625187.2021.1884221 [DOI] [PubMed] [Google Scholar]
- 98.Perez-Vincent SM, Carreras E, Gibbons MA. COVID-19 Lockdowns and domestic violence: evidence from two studies in Argentina. Inter-American Development Bank, 2020. 10.18235/0002490 [DOI] [Google Scholar]
- 99.Silverio-Murillo A, Hoehn-Velasco L, Balmori de la Miyar JR, et al. COVID-19 and women's health: examining changes in mental health and fertility. Econ Lett 2021;199:109729. 10.1016/j.econlet.2021.109729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Celestin K, Allorant A, Virgin M, et al. Short-term effects of the COVID-19 pandemic on HIV care utilization, service delivery, and continuity of HIV antiretroviral treatment (art) in Haiti. AIDS Behav 2021;25:1366–72. 10.1007/s10461-021-03218-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Agüero JM. COVID-19 and the rise of intimate partner violence. World Dev 2021;137:7. 10.1016/j.worlddev.2020.105217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pattojoshi A, Sidana A, Garg S, et al. Staying home is NOT 'staying safe': a rapid 8-day online survey on spousal violence against women during the COVID-19 lockdown in India. Psychiatry Clin Neurosci 2021;75:64–6. 10.1111/pcn.13176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Aryal S, Nepal S, Ballav Pant S. Safe abortion services during the COVID -19 pandemic: a cross-sectional study from a tertiary center in Nepal. F1000Res 2021;10:112. 10.12688/f1000research.50977.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Aolymat I. A cross-sectional study of the impact of COVID-19 on domestic violence, menstruation, genital tract health, and contraception use among women in Jordan. Am J Trop Med Hyg 2020;104:519–25. 10.4269/ajtmh.20-1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.United Nations Women Headquarters . Impact of COVID-19 on violence against women and girls and service provision: un women rapid assessment and findings, 2020. Available: https://www.unwomen.org/-/media/headquarters/attachments/sections/library/publications/2020/impact-of-covid-19-on-violence-against-women-and-girls-and-service-provision-en.pdf?la=en&vs=0
- 106.Restar AJ, Garrison-Desany HM, Adamson T, et al. HIV treatment engagement in the context of COVID-19: an observational global sample of transgender and nonbinary people living with HIV. BMC Public Health 2021;21:901. 10.1186/s12889-021-10977-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lyons M, Brewer G. Experiences of intimate partner violence during lockdown and the COVID-19 pandemic. J Fam Violence 2022;37:1–9. 10.1007/s10896-021-00260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Khan MS, Rego S, Rajal JB, et al. Mitigating the impact of COVID-19 on tuberculosis and HIV services: a cross-sectional survey of 669 health professionals in 64 low and middle-income countries. PLoS One 2021;16:e0244936. 10.1371/journal.pone.0244936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Endler M, Al-Haidari T, Benedetto C, et al. How the coronavirus disease 2019 pandemic is impacting sexual and reproductive health and rights and response: results from a global survey of providers, researchers, and policy-makers. Acta Obstet Gynecol Scand 2021;100:571–8. 10.1111/aogs.14043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Flynn AC, Kavanagh K, Smith AD, et al. The impact of the COVID-19 pandemic on pregnancy planning behaviors. Womens Health Rep 2021;2:71–7. 10.1089/whr.2021.0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hale T, Angrist N, Goldszmidt R, et al. A global panel database of pandemic policies (Oxford COVID-19 government response Tracker). Nat Hum Behav 2021;5:529–38. 10.1038/s41562-021-01079-8 [DOI] [PubMed] [Google Scholar]
- 112.Bearak J, Popinchalk A, Ganatra B, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990-2019. Lancet Glob Health 2020;8:e1152–61. 10.1016/S2214-109X(20)30315-6 [DOI] [PubMed] [Google Scholar]
- 113.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev 2010;32:152–74. 10.1093/epirev/mxq012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Berer M. National laws and unsafe abortion: the parameters of change. Reprod Health Matters 2004;12:1–8. 10.1016/S0968-8080(04)24024-1 [DOI] [PubMed] [Google Scholar]
- 115.Gresham AM, Peters BJ, Karantzas G, et al. Examining associations between COVID-19 stressors, intimate partner violence, health, and health behaviors. J Soc Pers Relat 2021;38:2291–307. 10.1177/02654075211012098 [DOI] [Google Scholar]
- 116.Piquero AR, Jennings WG, Jemison E, et al. Domestic violence during the COVID-19 pandemic - Evidence from a systematic review and meta-analysis. J Crim Justice 2021;74:101806. 10.1016/j.jcrimjus.2021.101806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Banke-Thomas A, Yaya S. Looking ahead in the COVID-19 pandemic: emerging lessons learned for sexual and reproductive health services in low- and middle-income countries. Reprod Health 2021;18:248. 10.1186/s12978-021-01307-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ehrenpreis JE, Ehrenpreis ED. A historical perspective of healthcare disparity and infectious disease in the native American population. Am J Med Sci 2022;363:288–94. 10.1016/j.amjms.2022.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Summers JA, Baker MG, Wilson N. New Zealand’s experience of the 1918-19 inn uenza pandemic: a systematic review after 100 years. NZMJ 2018;131:1487. [PubMed] [Google Scholar]
- 120.Boggild AK, Yuan L, Low DE, et al. The impact of influenza on the Canadian first nations. Can J Public Health 2011;102:345–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Groom AV, Hennessy TW, Singleton RJ, et al. Pneumonia and influenza mortality among American Indian and Alaska native people, 1990-2009. Am J Public Health 2014;104 Suppl 3:S460–9. 10.2105/AJPH.2013.301740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Amiri M, El-Mowafi IM, Chahien T, et al. An overview of the sexual and reproductive health status and service delivery among Syrian refugees in Jordan, nine years since the crisis: a systematic literature review. Reprod Health 2020;17:1–20. 10.1186/s12978-020-01005-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher– lancet commission. The Lancet 2018;391:2642–92. 10.1016/S0140-6736(18)30293-9 [DOI] [PubMed] [Google Scholar]
- 124.Meckler GD, Elliott MN, Kanouse DE, et al. Nondisclosure of sexual orientation to a physician among a sample of gay, Lesbian, and bisexual youth. Arch Pediatr Adolesc Med 2006;160:1248. 10.1001/archpedi.160.12.1248 [DOI] [PubMed] [Google Scholar]
- 125.Alsalem R. Violence against Indigenous women and girls, 2022. Available: https://www.ohchr.org/en/calls-for-input/calls-input/call-inputs-report-violence-against-indigenous-
- 126.Marie Stopes International . Resilience, Adaptation, and Action: MSI’s Response to COVID-19; 2020.
- 127.Serving SARA during the COVID-19 pandemic: lessons learned in family planning adaptations, 2021
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-009594supp001.pdf (168.5KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.