Abstract
Objectives
To explore the personal and/or medical reasons patients on active surveillance (AS) have, or consider having, further definitive treatment for their prostate cancer. Research suggests up to 50% of patients on AS will discontinue within 5 years, though reasons for discontinuation from the patient's perspective is under‐explored.
Methods
Prostate cancer patients who were or had been on AS for at least 6 months were recruited. A questionnaire assessed reasons for receiving/considering definitive treatment and the extent to which reasons were personal or medical. Clinical information was extracted from a state‐level population registry. A subset of participants were interviewed to further explore questionnaire responses.
Results
One‐hundred and‐three individuals completed the survey; 33 were also interviewed. Fifty‐four survey participants (52%) had discontinued AS for definitive treatment. Common reasons for discontinuation were evidence of disease progression, doctor recommendation, desire to act, and fear of progression. Many participants who considered or had treatment reported weighing medical and personal factors equally in their decision. Interview participants described strongly considering any amount of disease progression and personal factors such as fear of progression, family concerns, and adverse vicarious experiences when deciding whether to pursue treatment.
Conclusion
Both medical and personal factors are considered when deciding whether to discontinue AS. Identifying predictors of discontinuation is essential for informing supportive care services to improve AS management.
Keywords: active surveillance, decision making, mixed methods research, prostate cancer, psycho‐oncology, qualitative research
1. INTRODUCTION
Active surveillance (AS) is the recommended best‐available treatment option for individuals with low risk prostate cancer. 1 It involves routine surveillance of biological markers of the disease through prostate specific antigen (PSA) tests, digital rectal examinations, biopsies, and magnetic‐resonance imaging (MRI). 1 Transition to definitive treatment (e.g., prostatectomy or radiotherapy) is generally recommended upon significant disease progression which results in risk reclassification. 1 Currently, there is no globally‐recognised criterion of initiation, follow‐up procedures, or triggers for intervention; therefore, AS practices vary greatly across clinicians and countries. 2
Approximately 50% of patients discontinue AS within 5 years, the majority of which with evidence of significant disease progression. 3 , 4 Whilst AS discontinuation rates are commonly reported, 4 , 5 , 6 the extent to which discontinuation is triggered by disease progression and/or other personal reasons requires further research, especially from the patient perspective. Emerging research suggests this decision may be influenced by both medical (e.g., disease progression, doctor recommendation) and personal reasons (e.g., anxiety, pressure from family), at least for some people. 6 , 7 , 8 For instance, in a cohort study, Lang et al 8 reported that in those who had transitioned from AS to definitive treatment at 3 years post‐diagnosis, 69% had done so for medical reasons, 31% for a mix of personal and medical reasons, and 8% for solely personal reasons. However, this study only illustrated personal reasons as either ‘spousal encouragement’ or ‘unspecified’. 8 A more fine‐grained understanding of the personal reasons men transition to definitive treatment is needed to assist in targeting supportive care interventions, thereby encouraging adherence and improved mental wellbeing. In this study, a mixed‐methods approach was used to identify and explore the reasons men discontinue or consider discontinuing AS to receive definitive treatment.
2. METHODOLOGY
2.1. Sample
Participants for this study were sampled from a larger case‐control study designed to examine social‐ecological factors associated with discontinuing AS. Unfortuantely further recruitment from other Australian states was unable to proceed due to COVID‐19. 9 Given data collection from South Australia had already been completed, the present study reports this cross‐sectional data. Participants were recruited through the South Australian Prostate Cancer Clinical Outcomes Collaborative (SA‐PCCOC), which captures 90% of all diagnosed prostate cancer survivors in the state. 10 SA‐PCCOC identified patients eligible using the following criteria: diagnosed with prostate cancer between January 2014 and October 2019, initially monitored through AS for at least six months, 18+ years old, and had consented to be contacted for research projects through SA‐PCCOC. As per the original case‐control design, participants were then identified as either cases (patients identified as transitioning to treatment with weak evidence of disease progression) or controls (patients currently on AS or patients who had transitioned with strong evidence of disease progression), and were matched 1:4. This resulted in N = 270 eligible participants for recruitment. In the present study, participants were not analysed according to their case/control status. A recruitment flowchart is presented in Figure 1.
FIGURE 1.
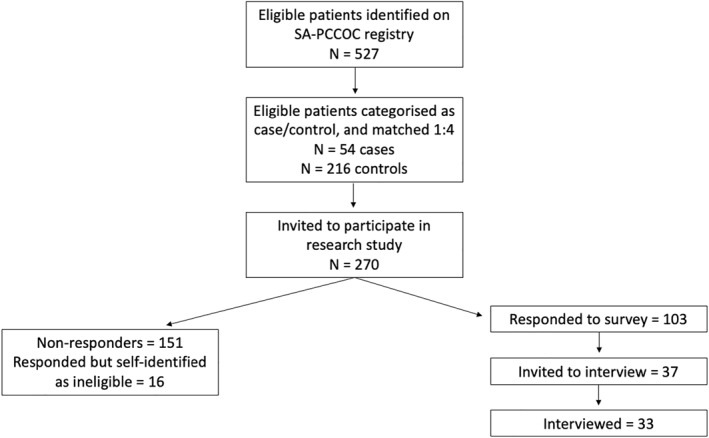
Participant recruitment flow chart
Eligibility criteria for interviews included: completed survey, provided contact information on the returned consent form, had access to a telephone, and spoke English.
2.1.1. Evidence of disease progression in sample
Disease progression was determined using the following clinical information at diagnosis and follow‐ups: Gleason Score, PSA test results, and Biopsy results (i.e., positive cores identified). We classified participants into three categories, indicating the level of evidence available indicating significant disease progression had occurred; Strong, Moderate, and Weak. See supplementary material (appendix 1) for specific criteria.
2.2. Survey testing, measures and analyses
2.2.1. Survey testing
Following identification of eligible participants through SA‐PCCOC, pilot testing on the survey was conducted. The survey underwent two separate pilot tests for (a) readability and (b) response rate prior to dissemination of the final version. In the readability pilot, the survey was reviewed by four prostate cancer survivors and two health profressionals, and adjustments were made based on their feedback. Changes to the study procedure (including the provision of unconditional monetary incentives to all remaining participants) and survey length were made given the outcomes of the response rate pilot test, which was conducted with N = 32 eligible participants.
Following pilot testing, remaining eligible participants (n = 238) were sent the study materials. Reminder letters were sent to non‐responders 2 weeks later. Surveys completed on paper, or the phone were entered into RedCap, 11 , 12 which also hosted the online version of the survey. Additional clinical data was retrieved from the SA‐PCCOC database for participants who completed the survey, including demographics and treatment information.
2.2.2. Survey measures
The present study examined survey responses on men's reasons for transitioning from AS to definitive treatment, or if still on AS, the reasons they had considered having definitive treatment. Fifteen items were assessed on a 5‐point Likert scale ranging from 1 (doesn't apply to me) to 5 (strongly applies to me). In analysis, categories were collapsed into three categories; Doesn't apply, Minimally/Somewhat applies, and Very‐much/Strongly applies. See Table 1 for all items. The main reason for treatment/considering treatment was also assessed on a visual analogue scale (VAS), where zero indicated purely personal reasons and 100 indicated purely medical/clinical reasons. These items were informed by previous literature 7 , 13 and purpose‐written by the research team (see supplementary material appendix 2). The full survey also included validated measures and purpose‐written questions on demographics, anxiety, depression, coping strategies, physical activity, social support, supportive care needs, their relationship with doctors, and their experiences on AS. Findings related to these measures will be reported elsewhere.
TABLE 1.
Reasons for treatment in participants who had undergone definitive treatment after active surveillance (AS)
| Reason item | N | Doesn't apply. N (%) | Minimally/Somewhat applies. N (%) | Very much/Strongly applies. N (%) | Mean (SD) |
|---|---|---|---|---|---|
| Medical reasons | |||||
| PSA increase | 50 | 2 (4%) | 13 (26%) | 35 (70%) | 4 (1) |
| Doctor recommendation | 48 | 4 (8.3%) | 10 (20.8%) | 34 (70.8%) | 3.9 (1.2) |
| Biopsy | 46 | 6 (13.1%) | 11 (23.9%) | 29 (63%) | 3.6 (1.3) |
| Gleason score increase | 45 | 12 (26.7%) | 6 (13.3%) | 27 (60%) | 3.3 (1.6) |
| DRE | 44 | 37 (84.1%) | 3 (6.8%) | 4 (9.1%) | 1.4 (1) |
| Medical comorbidities | 43 | 32 (74.4%) | 7 (16.3%) | 4 (9.3%) | 1.6 (1.2) |
| Personal reasons | |||||
| Desire to act | 47 | 13 (27.7%) | 10 (21.3%) | 24 (51.1%) | 3.2 (1.6) |
| Fear of cancer | 44 | 28 (63.6%) | 8 (18.2%) | 8 (18.2%) | 1.9 (1.3) |
| Pressure from others | 46 | 29 (63%) | 10 (21.7%) | 7 (15.2%) | 1.9 (1.3) |
| Uncertainty | 40 | 27 (67.5%) | 9 (22.5%) | 4 (10%) | 1.7 (1.1) |
| Anxiety | 45 | 34 (75.6%) | 10 (22.2%) | 1 (2.2%) | 1.4 (0.8) |
| Tired of waiting | 42 | 33 (78.6%) | 7 (16.7%) | 2 (4.8%) | 1.4 (0.9) |
| Inconvenient protocol | 43 | 39 (90.7%) | 4 (9.3%) | 0 (0%) | 1.1 (0.4) |
| Depression | 43 | 39 (90.7%) | 4 (9.3%) | 0 (0%) | 1.1 (0.5) |
2.2.3. Survey analyses
Descriptive statistics for demographics, considering treatment, reasons for undergoing definitive treatment, and main reason for undergoing treatment were calculated in R. 14
2.3. Interviews
Participants were sampled using Criterion‐I purposeful sampling technique. This involves identifying and selection participants according to predetermined criterion of importance, which enables researchers to deepen the understanding of results from information‐rich cases. 15 Participants with VAS scores under 70, had considered leaving AS, were located in outer regional/remote areas, and had reported higher scores of anxiety, depression, and unmet supportive care needs were prioritised for interview selection. All participants were interviewed by lead author Megan McIntosh (MMh; who had prior qualitative research experience). Interviews were semi‐structured, and followed a topic guide (see supplementary material appendix 3) which explored experiences on AS, reasons for treatment or considering treatment, and treatment experiences. Interviews were audio recorded and transcribed verbatim, taking an average 31 min to complete. Braun and Clarke have recommended thematic saturation should not be the primary aim of sample size calculations and recruitment when conducting thematic analysis. 16 Rather, all participants who met elibility and sampling criteria were invited to ensure richness of data to address the research questions.
2.3.1. Interview analysis
Transcripts were analysed using Braun and Clarke's reflexive thematic analysis method. 16 , 17 This involves six key steps: Familiarisation, Coding, Create Themes, Revise Themes, Define Themes, Writing. The Familiarisation and Coding steps were performed by MM and Melissa J Opozda (MJO), who both have experience in qualitative research and thematic analysis. All transcripts were then re‐analysed by MM and themes were created. MM and MJO then revised and formally defined the themes, and a thematic map was created to illustrate the relationship between themes. Themes and the thematic map were reviewed and finalised by all authors. Results were written with transcript excerpts to illustrate the findings.
3. RESULTS
3.1. Participants
One hundred and three participants completed the survey and consent form (38% response rate). The average participant was married (83%), retired (64%), had completed post‐secondary education (70%), and lived in an Australian state capital city (71%). See Table 2 for complete breakdown of demographics.
TABLE 2.
Participant demographics and clinical information
| All participants (n = 103) | Treatment (n = 53) | Active surveillance (n = 48) | |
|---|---|---|---|
| Age at diagnosis: Mean (SD) | 64.5 (6.6) | 63.7 (7.1) | 65.4 (5.6) |
| Age at diagnosis range: years | 48–75 | 48–75 | 49–74 |
| Time on active surveillance: Mean years (SD) | 2.5 (1.4) | 2 (1.2) | 3.2 (1.1) |
| Current treatment status: N (%) | |||
| Had treatment | 53 (51.4%) | ‐ | ‐ |
| On active surveillance | 48 (46.6%) | ‐ | ‐ |
| Ceased all treatment with no follow‐up care a | 2 (1.9%) | ‐ | ‐ |
| Treatment type: N (%) b | |||
| Prostatectomy | ‐ | 33 (62.3%) | ‐ |
| Radiation | ‐ | 23 (43.4%) | ‐ |
| Other (e.g., Hormone Therapy) | ‐ | 2 (3.8%) | ‐ |
| Marital status: N (%) | |||
| Single | 3 (2.9%) | 3 (5.7%) | 0 |
| Married/De facto/Partnered | 86 (83.5%) | 42 (79.2%) | 43 (89.6%) |
| Divorced/Separated | 9 (8.7%) | 5 (9.4%) | 3 (6.3%) |
| Widowed | 5 (4.9%) | 3 (5.7%) | 2 (4.2%) |
| Employment: N (%) | |||
| Working (full or part time) | 32 (31%) | 14 (26.4%) | 17 (35.4%) |
| Retired | 66 (64.1%) | 35 (66%) | 30 (62.5%) |
| Unemployed | 5 (4.9%) | 4 (7.6%) | 1 (2.1%) |
| Education: N (%) | |||
| Primary | 3 (2.9%) | 0 | 3 (6.3%) |
| Secondary | 27 (26.2%) | 16 (30.2%) | 11 (22.9%) |
| Vocational Training/Education | 36 (35%) | 16 (30.2%) | 18 (37.5%) |
| University | 37 (35.9%) | 21 (39.6%) | 16 (33.3%) |
| Location c : N (%) | |||
| Remote | 5 (4.9%) | 2 (3.7%) | 3 (6.4%) |
| Outer regional | 11 (10.7%) | 6 (11.1%) | 4 (8.5%) |
| Inner regional | 14 (13.6%) | 4 (7.4%) | 9 (19.1%) |
| Major city | 73 (70.9%) | 42 (77.8%) | 31 (66%) |
| Diagnostic biopsy type: N (%) | |||
| Transperineal | 21 (20.4%) | 12 (22.6%) | 8 (16.7%) |
| Transrectal Ultrasound (guided) | 30 (29.1%) | 15 (28.3%) | 14 (29.2%) |
| Transurethral resection of prostate | 12 (11.7%) | 3 (5.7%) | 9 (18.8%) |
| Not reported | 40 (38.8%) | 23 (43.4%) | 16 (33.3%) |
| Received repeat biopsy: N (%) | 63 (61.2%) | 30 (56.6%) | 31 (64.6%) |
| Time between diagnostic and repeat biopsy: Mean months (SD) | 17.4 (12.7) | 18.5 (12.2) | 16.5 (13.6) |
| Repeat biopsy type: N (%) | |||
| Transperineal | 36 (57.1%) | 17 (56.7%) | 18 (58.1%) |
| Transrectal Ultrasound (guided) | 21 (33.3%) | 9 (30%) | 12 (38.7%) |
| Transurethral resection of prostate | 4 (6.4%) | 3 (10%) | 1 (3.2%) |
| Not reported | 2 (3.2%) | 1 (3.3%) | 0 |
| MRI conducted (prior/post diagnosis): N (%) | 68 (66%) | 39 (73.6%) | 27 (56.3%) |
The two participants who reported they ‘ceased all treatment with no follow‐up care’ were not grouped into the AS or treatment categories, though their demographics have been included in the total sample.
Some participants received more than one treatment, therefore the percentage does not equal 100.
Location determined by postcodes and classified using the Australian Statistical Geographical Classification – Remoteness Area framework. 27
Of the 103 participants, 53 (51%) participants had discontinued AS and since undergone definitive treatment, and 48 (47%) participants were currently on AS. In patients who had discontinued AS, 11 had strong evidence of progression, 19 moderate evidence, and 23 weak evidence of progression. Two participants reported on the survey they had ceased all treatments and were not attending any follow‐up for their cancer, however both participants received a repeat biopsy. Approximinately 61% of participants received a repeat biopsy an average of 17 months after diagnosis.
The average time on AS was 2.1 years (SD = 1.3) for those who had since undergone treatment, and 3.3 years (SD = 1.1) for those currently on AS. Thirty percent of those currently on AS (n = 14) reported that they had considered discontinuing to have definitive treatment. The average time for those currently on AS who had considered leaving was 4 years (SD = 0.9), versus 4.3 years (SD = 0.9) for those who had not considered discontinuing.
3.2. Reasons for leaving active surveillance
The most common reasons participants who went onto have definitive treatment endorsed to have very much or strongly influenced their decision included a rise in PSA level (70%), receiving a doctor's recommendation to have further treatment (60%), a change in Gleason score (63%) or change in repeat biopsy results (70%), experienced fear of cancer progression (18%), or had a strong desire to do something to cure the cancer (51%). Few people reported comorbidities or anxiety strongly influenced their decision. See Table 1 for a complete overview.
Tables were produced to examine the reasons for leaving AS by level of disease progression evidence (strong, weak moderate; see supplementary material appendix 4). In brief, average scores endorsing medical reasons were marginally higher among those with highest levels of evidence for disease progression. Similarly, participants with weaker evidence for progression more strongly endorsed personal reasons, though again differences were marginal.
3.3. Balance of medical and personal reasons impacting decision making
Figure 2 displays the VAS scores for people who discontinued AS to undergo definitive treatment (N = 44, 10 missing) and those who have considered ceasing AS for definitive treatment (N = 11, 3 missing). The majority of participants reported both personal and medical reasons influenced decision making, but to varying degrees. Among those who had received treatment, almost half had a VAS indicating their main reason for AS discontinuation was medically and personally balanced (i.e., VAS score of 50) or was tipped towards personal (i.e., VAS of 0–50). Another third had a VAS score indicating reasons were predominantly medical (i.e., VAS score of 90+). In participants still on AS, many indicated their desire for treatment was medically and personally balanced (VAS score of 50), or trended towards predominantly medical reasons (VAS scores of 75+).
FIGURE 2.
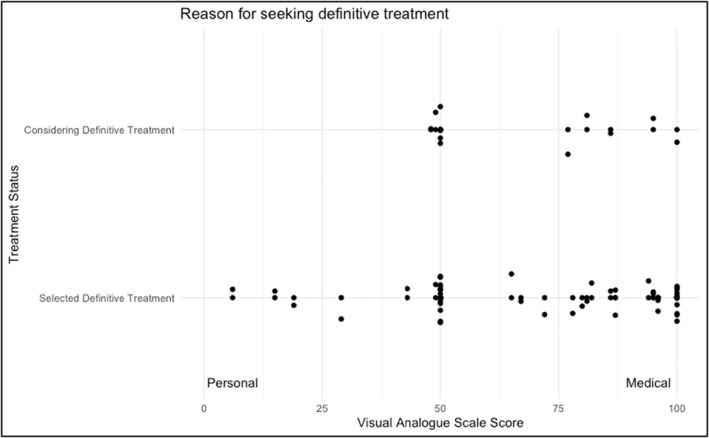
Visual analogue scale (VAS) scores reflecting reasons for having/wanting definitive treatment in participants
When analysed by disease progression (in participants who had discontinued AS), average VAS scores were generally higher in the ‘Strong’ progression group (M = 72.8, SD = 22.1) versus the Moderate (M = 65.6, SD = 25.7) and Weak (M = 69, SD = 30.6) groups.
3.4. Qualitative sample
Thirty‐three participants were interviewed. Of these, 10 (30.3%) were still on AS at the time of the interview (although one had a prostatectomy upcoming). The remaining 23 interviewees (69.7%) had left AS and had undergone definitive treatment for their prostate cancer. Most interview participants were married (82%), retired (61%), educated beyond high school (79%), and lived in a major city (64%).
3.5. Overview of themes
Men discussed a wide range of reasons they considered or had transitioned off AS to have definitive treatment. Ultimately, most participants were primarily motivated by medical reasons, though their decision was significantly supported or influenced by personal reasons. We identified three major themes: “Disease progression indicates need for action”, “A desire to act now”, and “Fear, worry, and uncertainty”. We did not note any major differences in themes between patients' post‐treatment and those still on AS, and as such results are reported together. Participants' reasons for treatment are illustrated in a thematic map (see Figure 3), with the larger ovals depicting reasons more often discussed by participants, and the smaller ovals reflecting reasons less commonly discussed.
FIGURE 3.
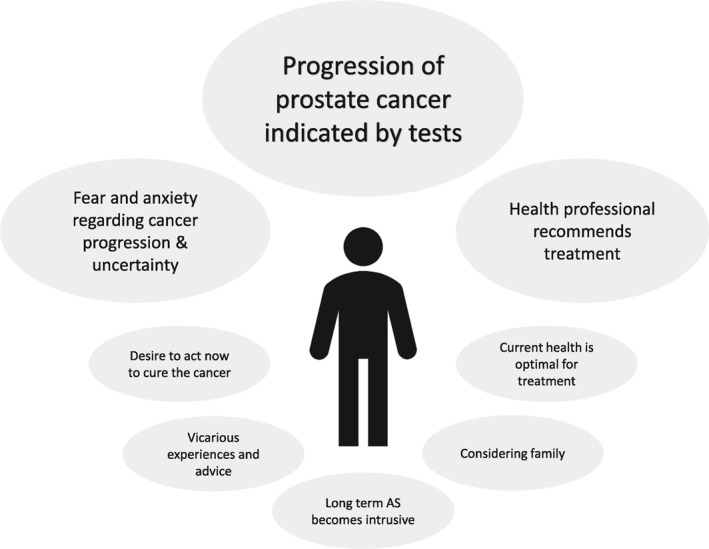
Thematic map of themes
3.5.1. Disease progression indicates need for treatment
By far the most common reason participants stated they had or considered having treatment was because their doctor made the recommendation to do so. Some participants noted they sought advice from several doctors before making the decision to transition from AS to treatment.
“I did toy with the idea, you know, should I wait another 12 months. And he advised it wouldn't be a good idea” P16058, Prostatectomy
Participants also explained that any disease progression identified from PSA, Gleason, MRI, or biopsy results often prompted them to discuss treatment options with their doctor. In almost all cases, participants considered any level of progression to be the first reason they considered and underwent definitive treatments. Men on AS said they would seek definitive treatments if or when tests indicated the cancer had progressed, irrespective of if this level consitituted disease reclassification.
“I've gone from having a low PSA to quite a high PSA, my PSA started fluctuating… So there was obviously something happening… When we got to the serious decision‐making stage… I'm thinking, you know, at least to take [Dr M's] advice to explore what surgery options are open to me.” P15132, Prostatectomy.
3.5.2. A desire to act now
“Well, I mean, cancer is not good in your body, and it can spread. So I think the sooner you get rid of it, the better. That's my opinion.” P14774, Active Surveillance but scheduled for Prostatectomy.
Several participants expressed a clear and intense desire to seek definitive treatments as soon as possible after diagnosis. For some, this was not offered or recommended at diagnosis and patients were advised to wait until the cancer had progressed further. In other circumstances, although progression was detected doctors advised participants that they could remain on AS. However, some participants viewed the doctor's mention of progression and having provided the option to undergo treatment as a reason to have definitive treatment and felt staying on AS would be risky. Despite being eligible for AS, participants often felt that having definitive treatments would provide more control over outcomes and were fearful that the cancer would progress outside the prostate.
“This why I was pushing the doctor to do something like surgery. But before then it was just too small. He went active surveillance. For me, I was always pushing, no no, I don’t want that. Remove it please.” P9160, Prostatectomy, Radiation, and Hormone Therapy.
Some participants who had been on AS for several years expressed that their decision to have treatment was also influenced by the nature of AS follow‐up. The regular tests, particularly annual biopsies, and mental load of continuing to watch for disease progression, became tiring and inconvenient for participants over time.
“I almost got tired, I guess. I guess of having nine years of just sitting there wondering what's going on. Mentally I was just done.” P15132, Prostatectomy.
Several patients also mentioned that their decision to transition off AS and pursue definitive treatment was influenced by the state of their current health, such as their age, fitness, and life expectancy. Participants felt that seizing the opportunity to have treatment while they were still ‘young and healthy’ would assist their recovery.
“And it, ah, occurred to me that if I was going to do anything, I might as well do it now. While I’m still reasonably active and so forth, and could recover, I would hope. Without too much difficulty.” P10433, Brachytherapy.
3.5.3. Fear, worry, and uncertainty
Participants often reported ongoing fears that the cancer would progress undetected, and they could be at risk of metastases or dying. It was common for participants to fear that delaying treatment was risky, as their PSA test might increase suddenly and it would be ‘too late’ to treat or cure the cancer. Ongoing anxiety or concerns that progression would occur too quickly were common reasons why participant sought or had considered treatment.
“I thought, my wife and I discussed it quite a lot… she was really concerned. And I guess I was concerned as well a little bit that, yeah it was internal, which was okay, so it was contained within the prostate, but there was always that fear… if it does get out and gets into your system elsewhere, I knew it could take off pretty quickly. And then you're, you know, you're fighting a bigger battle. It's probably best to get it done before it goes.” P14835, Prostatectomy.
Participants also discussed the influence that other people's experiences with prostate cancer had on their desire for treatment. Negative vicarious experiences of prostate cancer and hearing ‘horror stories’, whether directly from friends or family or indirectly online or via the media, was described as a reason participants had experienced fears of progression and desired treatment as soon as possible. Delaying treatment by remaining on AS in such cases was viewed as riskier than having treatment and avoiding the consequences that they had heard others had experienced.
“Keeping in mind though, that an old friend of mine got prostate cancer at about the same age as I did and said ‘oh nah, I'm not worried about it. You die with it rather than from it’. But eight years later, he was dead from it. So I've always had in the back of my mind. You know, keep an eye on it. What I'm trying to say, I think it's been, It's been at the back of my mind and a little bit concerning” P15005, Active surveillance but scheduled for Prostatectomy.
Participants also explained they chose to have treatment often because they wanted to ensure they would continue to be around for their family, and that having definitive treatment would reduce their family's worry.
“During that period, it was horrible, you know, I was a little bit depressed you know, knowing that I'd been diagnosed with this. And we have a big family, my children are still young. How am I meant to leave them if I die, earlier like this?” P9160, Prostatectomy, Radiation, and Hormone Therapy.
4. DISCUSSION
This study investigated the reasons people transition, or consider transitioning, from AS to definitive treatments. Results indicate that the reasons patients decide to leave AS are more complex than the literature often suggests.
Previous literature reporting rates of AS discontinuation often categorise participants according to progression criteria available on cancer registries, 4 , 6 and have rarely explored participants' own perspectives of reasons for discontinuation, nor considered the extent to which personal reasons influence those with evidence of disease progression. This may actually hinder health professionals from providing support to patients questioning when to transition to definitive treatment. Our results suggest that patients on AS often consider a variety of medical and personal factors when deciding whether to continue on AS or undergo definitive treatment, regardless of strength of evidence for disease progression. Evidence of disease progression, regardless of whether it meets criteria for disease reclassification, is considered strongly by men as a reason to pursue definitive treatment. In addition, we found patients may still consider and pursue treatment irrespective of whether the doctor states such progression warrants intervention. Participants in this study described feeling anxious when any evidence of cancer progression was detected. Cancer progression, or the fear of it, prompted participants to consider their future and the impact that delaying definitive treatment could have on their own health and their family. Fear of cancer recurrence is a significant issue for people with a cancer history, and several successful interventions have been developed. 18 , 19 Lessons from this literature may be useful to address fear of cancer progression in this population, whilst dispelling common misconceptions regarding prostate cancer and treatment (e.g., prostate cancer progresses rapidly) and promoting positive vicarious experiences of AS.
Several of the personal reasons, such as fear of progression and family pressure, have been identified in previous research. 7 , 8 , 13 Significant research has reported low levels of anxiety in men on AS, which often reduces or remains stable over time. 20 , 21 , 22 , 23 However, much of this research recruited patients from cancer centres which specialise in AS, which may have resulted in improved AS management and greater acceptance from both patients and doctors. Recent research conducted with patients from non‐specialist AS cancer centres have found men on AS experience more fear of cancer progression and generalised anxiety (immediately and long‐term) than those who have definitive treatment. 24 , 25 Further research is required to provide a more representative understanding of distress in AS patients, with consideration of crucial time‐points (for example, prior to treatment choice and follow‐up appointments.
4.1. Study limitations
Despite our novel findings, the limitations must be considered. The original case‐control study, which was paused due to COVID‐19, planned to recruit from multiple Australian states. The intended larger sample size would have enabled investigation into predictors of AS discontinuation. Despite this, we were able to recruit 103 participants into the study and collected both quantitative and qualitative data. In addition, the registry does not collect data on education or marital status, and the representativeness of our sample in regard to the registry population was difficult to determine. However, our sample is similar to the registry population in terms of age and location. 26 Finally, our study did not recruit participants whose primary language was not English, therefore results may not be generalisable to patients from culturally and linguistically diverse backgrounds.
4.2. Conclusion & clinical implications
Our mixed‐methods investigation of the reasons men on AS undergo or consider having definitive treatment indicates that both clinical factors and personal factors are strongly considered by patients during this process. Identifying predictors of discontinuing AS with and without evidence of disease progression or risk reclassification may further assist health professionals in targeting patients for support during the first few years on AS, when emotional distress and discontinuation rates are higher. Lessons from interventions targeting fear of cancer recurrence may be useful for guiding the development of supportive care interventions to address fear of cancer progression in this population. However, additional strategies to target other personal reasons, such as family pressure and negative vicarious experiences, are also expected to be useful.
AUTHOR CONTRIBUTIONS
All authors contributed to the study conception and design. Material preparation, data collection, analysis, and the manuscript draft was primarily performed by Megan McIntosh. Remaining authors provided critical feedback and assistance through all stages of the study (material preparation, data collection, analysis, and manuscript drafts). All authors read and approved the final manuscript.
CONFLICT OF INTEREST
The authors declare there are no conflicts of interest.
CONSENT TO PARTICIPATE & PUBLISH
Informed consent was obtained from all individual participants. All authors confirm that all participants provided informed consent for their de‐identified data to be included in this manuscript.
ETHICS APPROVAL
Ethics approval for this project was obtained through the Southern Adelaide Local Health Network (SAHLN). Approval number: HREC/19/SAC/88.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
We would like to extend our gratitude to the prostate cancer survivors who participated in this study. We would also like to thank the team at SA‐PCCOC for assisting in recruitment and data collection. This study was funded by a Below the Belt research grant through the Australian and New Zealand Urogenital and Prostate Cancer Trials Group. Author MM was supported by an Australian Government Research Stipend during her PhD and received further support from well as the Freemasons Centre for Male Health and Wellbeing.
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
McIntosh M, Opozda MJ, O’Callaghan M, Vincent AD, Galvão DA, Short CE. Why do men with prostate cancer discontinue active surveillance for definitive treatment? A mixed methods investigation. Psychooncology. 2022;31(8):1420‐1430. 10.1002/pon.5947
DATA AVAILABILITY STATEMENT
Data will be made available on Figshare. Please contact the corresponding author.
REFERENCES
- 1. Sanda MG, Cadeddu JA, Kirkby E, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options [Internet]. J Urol. 2018;199:683‐690. 10.1016/j.juro.2017.11.095. http://www.ncbi.nlm.nih.gov/pubmed/29203269 [DOI] [PubMed] [Google Scholar]
- 2. Kinsella N, Helleman J, Bruinsma S, et al. Active surveillance for prostate cancer: a systematic review of contemporary worldwide practices [Internet]. Transl Androl Urol. 2018;7:83‐97. 10.21037/tau.2017.12.24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5861285/pdf/tau‐07‐01‐83.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kinsella N, Beckmann K, Cahill D, et al. A single educational seminar increases confidence and decreases dropout from active surveillance by 5 Years after diagnosis of prostate cancer [Internet]. Eur Urol Oncol. 2019;2(4):464‐470. Elsevier [cited 2019 Jul 23]. https://www.sciencedirect.com/science/article/abs/pii/S2588931118301676?via%3Dihub [DOI] [PubMed] [Google Scholar]
- 4. Bokhorst LP, Valdagni R, Rannikko A, et al. A decade of active surveillance in the PRIAS study: an update and Evaluation of the criteria used to recommend a switch to active treatment [Internet]. Eur Urol. 2016;70:954‐960. 10.1016/j.eururo.2016.06.007. https://www.europeanurology.com/article/S0302‐2838(16)30277‐9/pdf [DOI] [PubMed] [Google Scholar]
- 5. Hamdy FC, Donovan JL, Lane JA, et al. 10‐Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer [Internet]. N Engl J Med. 2016;375:1415‐1424. https://www.nejm.org/doi/pdf/10.1056/NEJMoa1606220 [DOI] [PubMed] [Google Scholar]
- 6. Van Hemelrijck M, Ji X, Helleman J, et al. Reasons for discontinuing active surveillance: assessment of 21 centres in 12 countries in the movember GAP3 consortium [Internet]. Eur Urol. 2019;75:523‐531. https://www.ncbi.nlm.nih.gov/pubmed/30385049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Berger Z, Yeh J, Carter H, Pollack C. Characteristics and experiences of patients with localized prostate cancer who left an active surveillance program [Internet]. Patient. 2014;7:427‐436. 10.1007/s40271-014-0066-z. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4332784/pdf/nihms659349.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lang MF, Tyson MD, Alvarez JR, et al. The influence of psychosocial constructs on the adherence to active surveillance for localized prostate cancer in a prospective, population‐based cohort [Internet]. Urology. 2017;103:173‐178. 10.1016/j.urology.2016.12.063. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5410889/pdf/nihms859135.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McIntosh M. Why Do Men Leave Active Surveillance? A Case‐Control Study Examining Factors Contributing to Non‐adherence (Protocol) [Internet]. ANZCTR; 2020. [cited 2021 Mar 22]. http://www.anzctr.org.au/Trial/Registration/TrialReviewx?id=379100&isReview=true [Google Scholar]
- 10. SA‐PCCOC. SA Prostate Cancer Registry [Internet]. [cited 2022 Mar 7]. https://www.prostatehealth.org.au/sa‐prostate‐cancer‐registry/
- 11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)‐A metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377‐381. Academic Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners [Internet]. J Biomed Inf. 2019;95:103208. Academic Press Inc. [cited 2021 Jan 12]. 10.1016/j.jbi.2019.103208. https://linkinghub.elsevier.com/retrieve/pii/S1532046419301261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kinsella N, Stattin P, Cahill D, et al. Factors influencing men’s choice of and adherence to active surveillance for low‐risk prostate cancer: a mixed‐method systematic review [Internet]. Eur Urol. 2018;74:261‐280. 10.1016/j.eururo.2018.02.026. https://www.europeanurology.com/article/S0302‐2838(18)30176‐3/pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. R Core Team . R: A Language and Environment for Statistical Computing [Internet]. R Foundation for Statistical Computing; 2019. https://www.r‐project.org [Google Scholar]
- 15. Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research [Internet]. Adm Policy Ment Heal Ment Heal Serv Res. 2015;42:533‐544. Springer New York LLC [cited 2021 Mar 22]. 10.1007/s10488-013-0528-y. https://link.springer.com/article/10.1007/s10488‐013‐0528‐y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Braun V, Clarke V, Hayfield N, Terry G. Thematic analysis [Internet]. Handb Res Methods Heal Soc Sci. 2019:843‐860. Springer Singapore [cited 2021 Mar 23]. 10.1007/978-981-10-5251-4_103 [DOI] [Google Scholar]
- 17. Braun V, Clarke V. Successful Qualitative Research: A Practical Guide for Beginnners. SAGE Publications Ltd; 2013. [Google Scholar]
- 18. Tauber NM, O’Toole MS, Dinkel A, et al. Effect of psychological intervention on fear of cancer recurrence: a systematic review and meta‐analysis. J Clin Oncol. American Society of Clinical Oncology. 2019;37(31):2899‐2915. 10.1200/jco.19.00572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hall DL, Luberto CM, Philpotts LL, Song R, Park ER, Yeh GY. Mind‐body interventions for fear of cancer recurrence: a systematic review and meta‐analysis [Internet]. Psycho Oncol. 2018;27:2546‐2558. John Wiley & Sons, Ltd [cited 2021 Jul 14]. https://onlinelibrary.wiley.com/doi/10.1002/pon.4757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bellardita L, Valdagni R, van Den Bergh R, et al. How does active surveillance for prostate cancer affect quality of life? A systematic review [Internet]. Eur Urol. 2015;67:637‐645. 10.1016/j.eururo.2014.10.028. https://www.europeanurology.com/article/S0302‐2838(14)01101‐4/pdf [DOI] [PubMed] [Google Scholar]
- 21. van den Bergh RCN, Essink‐Bot ML, Roobol MJ, Schröder FH, Bangma CH, Steyerberg EW. Do anxiety and distress increase during active surveillance for low risk prostate cancer? J Urol. 2010;183:1786‐1791. No longer published by Elsevier. [DOI] [PubMed] [Google Scholar]
- 22. Punnen S, Cowan JE, Dunn LB, Shumay DM, Carroll PR, Cooperberg MR. A longitudinal study of anxiety, depression and distress as predictors of sexual and urinary quality of life in men with prostate cancer [Internet]. BJU Int. 2013;112:E67‐E75. John Wiley & Sons, Ltd [cited 2021 May 18]. https://bjui‐journals.onlinelibrary.wiley.com/doi/full/10.1111/bju.12209 [DOI] [PubMed] [Google Scholar]
- 23. Venderbos LDF, Bergh RCN, Roobol MJ, et al. A longitudinal study on the impact of active surveillance for prostate cancer on anxiety and distress levels. Psycho Oncol. 2015;24(3):348‐354. 10.1002/pon.3657 [DOI] [PubMed] [Google Scholar]
- 24. Nilsson R, Næss‐Andresen TF, Myklebust TÅ, Bernklev T, Kersten H, Haug ES. Fear of recurrence in prostate cancer patients: a cross‐sectional study after radical prostatectomy or active surveillance [Internet]. Eur Urol Open Sci. 2021;25:44‐51. Elsevier B.V. [cited 2021 May 3]. 10.1016/j.euros.2021.01.002. https://linkinghub.elsevier.com/retrieve/pii/S2666168321000021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ruane‐McAteer E, Porter S, O’Sullivan J, Dempster M, Prue G. Investigating the psychological impact of active surveillance or active treatment in newly diagnosed favorable‐risk prostate cancer patients: a 9‐month longitudinal study [Internet]. Psycho Oncol. 2019. John Wiley & Sons, Ltd [cited 2019 Jul 23]. https://onlinelibrary.wiley.com/doi/abs/10.1002/pon.5161 [DOI] [PubMed] [Google Scholar]
- 26. Ruseckaite R, Beckmann K, O’Callaghan M, et al. A retrospective analysis of Victorian and South Australian clinical registries for prostate cancer: trends in clinical presentation and management of the disease [Internet]. BMC Cancer. 2016;16:1‐11. BioMed Central [cited 2021 Jul 14]. https://bmccancer.biomedcentral.com/articles/10.1186/s12885‐016‐2655‐9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Australian Statistical Geographical Classification ‐ Remoteness Area | Australian Government Department of Health. https://www.health.gov.au/health‐workforce/health‐workforce‐classifications/australian‐statistical‐geographical‐classification‐remoteness‐area [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
Data will be made available on Figshare. Please contact the corresponding author.


