Frailty has become a condition we as intensivists have been gradually more familiar with. Geriatricians have developed the concept and it includes several age-related changes leading to the hallmarks of frailty: slow walking speed, impaired grip strength, low activity, unintended weight loss, and exhaustion [1]. An early paper about frailty in the intensive care unit (ICU) context was published in 2014 [2] and frailty has since attained considerable attraction and has been found to be closely related to an adverse outcome after ICU admissions [3]. This is most pronounced in the very old ICU patient where it is an independent risk factor for short-term mortality [4]. Frailty not only affects mortality outcomes but has been found to prolong ICU and hospital stay with increased use of organ support [3] as well as a poor quality of life post-hospital discharge [5]. More patients with frailty developed persistent critical illness than patients with no frailty in a recent large cohort study from Australia and New Zealand [6], a condition that affect around 8–10% of ICU survivors. It is also important to acknowledge that frailty is not operating isolated, but is closely associated with other geriatric syndromes as activity of daily life, cognition and multimorbidity [7].
Importantly, frailty is not a static concept and can change in different ways among survivors post-ICU discharge as demonstrated in a study from the Netherlands [8]. In that study 42% of acutely admitted patients developed increased frailty measured with the Clinical Frailty Scale (CFS) after one year, but many patients (35%) also had also reduced frailty. This clearly shows that frailty is not a static parameter that may vary with time but the optimal time to measure changes in frailty after hospital discharge is not clear. However, it can be used to individualise rehabilitation approaches after ICU care [9].
Frailty may be measured or estimated using many methods, and the “gold standard” is the Comprehensive Geriatric Assessment. This takes time and requires a fully co-operable patient and is not possible to use at ICU admission. For this reason, other methods have been used: some using information made from previous diagnostic codes (Frailty Index), and some use information obtained at admission using sources form patients (if possible), caregivers or hospital records. One of the most popular methods is the CFS using a pictographic scale with an explanatory text [10]. Recently, the CFS was used in a large prospective study of 1923 pairs of assessors aimed to study the inter-rater variability of the scale [11]. This study revealed a very high inter-rater agreement (weighted kappa 0.86), also in subgroup analyses. The agreement when comparing information from family or hospital records was better than using only direct patient information, and pairs of raters from same profession performed better than from different professions. Other methods to assess frailty has also been used but found inferior to the CFS in critical ill patients [12]. However, CFS does not only predict short-term outcome but is also a factor predicting 6-month mortality in old ICU patients [13]. Importantly, adding other geriatric parameters on top of CFS do not improve the mortality prediction [7]. Also, the CFS has been released in a new version and other scores such as FRAIL-score have been introduced, however, large scale validation is missing.
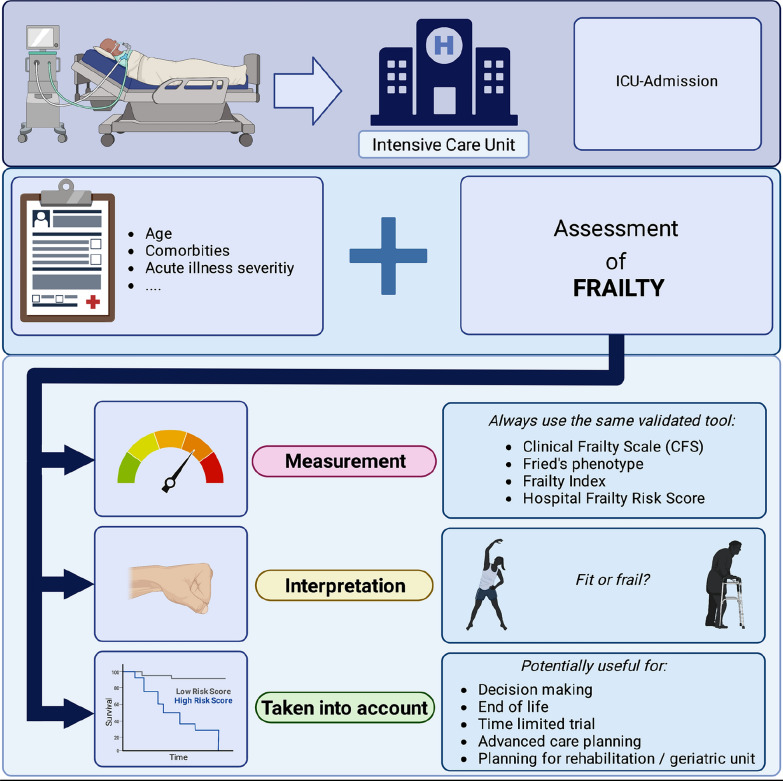
Frailty has attracted much attention during the coronavirus disease 2019 (COVID-19) pandemic. The CFS was initially suggested to use as a triage criterion for ICU admission. Among others, its use has been advocated in the United Kingdom, but CFS was criticized for being less specific when applied to all patients and was later advocated only in patients above age 65 years. In a systematic review [14] frailty as determined by CFS was found to be strongly associated with mortality and concluded that frailty-based patient management should be included in international COVID-19 treatment guidelines. Frailty also proved to be an important factor regarding ICU survival, in particular in the very old patient group. In a prospective multicentre study in Europe, frailty assessed with CFS was found to be more important than age to predict mortality [15]. More specifically, this study found that age was important only in the group of non-frail patients with significant lower mortality with increased age. However, in frail patients, this age difference was non-existent and regardless of age, the outcome was poor with only one of three surviving to 90 days. Increased documentation of the impact of frailty in critical care patients makes it important to be measured, interpreted, and used in the therapy plan [4, 15] (Fig. 1).
Fig. 1.
Frailty assessment in the ICU
In summary, frailty should be evaluated in clinical practice in old ICU patients. The body of evidence recently accumulated can be translated into a specific to-do list in clinical practice:
It is important to be consistent in the use of frailty assessment method to familiarize the ICU to the same “tool” and do comparisons over time.
The tool should have been validated and proven valuable in controlled studies (e.g. CFS), should be easy to use and easy to understand and learn by the ICU staff.
It is important that the reference time is the level of frailty prior to the acute illness leading to a hospital or ICU admission (usually 2 weeks prior to the admission).
Together with other parameters it can be helpful in admission decision as well as in end-of life discussions later in the ICU.
Even if it is firmly documented to be a good clinical predictors of severe outcomes, it cannot be used alone with sufficient clinical precision in individual patients.
In conclusion, frailty in intensive care medicine must be measured, interpreted, and taken into account to improve individual care and resource allocation.
Acknowledgements
The following members of the VIP study group were collaborators in this study: Jesper Fjølner (Department of Anaesthesia and Intensive Care, Viborg Regional Hospital, Viborg, Denmark); Raphael Romano Bruno (Heinrich-Heine-University Duesseldorf, Medical Faculty, Department of Cardiology, Pulmonology and Vascular Medicine, Duesseldorf, Germany); Malte Kelm (Heinrich-Heine-University Duesseldorf, Medical Faculty, Department of Cardiology, Pulmonology and Vascular Medicine, Duesseldorf, Germany); Michael Beil (Department of Medical Intensive Care, Hadassah University Medical Center, Jerusalem, Israel); Sigal Sviri (Department of Medical Intensive Care, Hadassah University Medical Center, Jerusalem, Israel); Wojciech Szczeklik (Center for Intensive Care and Perioperative Medicine, Jagiellonian University Medical College, Krakow, Poland); Susannah Leaver (General Intensive care, St George´s University Hospitals NHS Foundation trust, London, United Kingdom); Dylan W. De Lange (Department of Intensive Care Medicine, University Medical Center, University Utrecht, the Netherlands).
Funding
CJ reports that institutional support has been received by the German Research Council (SFB 1116) as well as the State of North Rhine Westphalia (Giga for Health: 5GMedizincampus. NRW, Project number 005-2008-0055). The support of the VIP studies in France by a grant from Fondation Assistance Publique-Hôpitaux de Paris pour la recherche is greatly appreciated. In Norway, the VIP studies were supported by a grant from the Health Region West. In addition, the funding was received by a grant from the European Open Science Cloud (EOSC) by the European Commission for a study of the VIP project. Open Access funding enabled and organized by Projekt DEAL. Deutsche Forschungsgemeinschaft, CRC 1116, State Northrhine Westfalia, 005-2008-0055, Assistance Publique—Hôpitaux de Paris, Health Region West, European Open Science Cloud.
Declarations
Conflicts of interest
The authors declare that they have no competing interests.
Footnotes
Jesper Fjølner, Raphael Romano Bruno, Malte Kelm, Michael Beil, Sviri Sigal, Wojciech Szczeklik, Susannah Leaver, and Dylan W. De Lange.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Christian Jung, Email: Christian.jung@med.uni-duesseldorf.de.
the VIP study group:
Jesper Fjølner, Raphael Romano Bruno, Malte Kelm, Michael Beil, Sviri Sigal, Wojciech Szczeklik, Susannah Leaver, and Dylan W. De Lange
References
- 1.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.M255. [DOI] [PubMed] [Google Scholar]
- 2.McDermid RC, Bagshaw SM. Scratching the surface: the burden of frailty in critical care. Intensive Care Med. 2014;40:740–742. doi: 10.1007/s00134-014-3246-3. [DOI] [PubMed] [Google Scholar]
- 3.Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, Sibley S, Rockwood K. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43:1105–1122. doi: 10.1007/s00134-017-4867-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flaatten H, De Lange DW, Morandi A, Andersen FH, Artigas A, Bertolini G, Boumendil A, Cecconi M, Christensen S, Faraldi L, Fjolner J, Jung C, Marsh B, Moreno R, Oeyen S, Ohman CA, Pinto BB, Soliman IW, Szczeklik W, Valentin A, Watson X, Zaferidis T, Guidet B, group VIPs The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (>/= 80 years) Intensive Care Med. 2017;43:1820–1828. doi: 10.1007/s00134-017-4940-8. [DOI] [PubMed] [Google Scholar]
- 5.Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, Artiuch B, Ibrahim Q, Stollery DE, Rokosh E, Majumdar SR. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186:E95–102. doi: 10.1503/cmaj.130639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darvall JN, Bellomo R, Bailey M, Young PJ, Rockwood K, Pilcher D. Impact of frailty on persistent critical illness: a population-based cohort study. Intensive Care Med. 2022;48:343–351. doi: 10.1007/s00134-022-06617-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, Szczeklik W, Artigas A, Morandi A, Andersen F, Zafeiridis T, Jung C, Moreno R, Walther S, Oeyen S, Schefold JC, Cecconi M, Marsh B, Joannidis M, Nalapko Y, Elhadi M, Fjolner J, Flaatten H, group VIP The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46:57–69. doi: 10.1007/s00134-019-05853-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geense W, Zegers M, Dieperink P, Vermeulen H, van der Hoeven J, van den Boogaard M. Changes in frailty among ICU survivors and associated factors: results of a one-year prospective cohort study using the Dutch Clinical Frailty Scale. J Crit Care. 2020;55:184–193. doi: 10.1016/j.jcrc.2019.10.016. [DOI] [PubMed] [Google Scholar]
- 9.Galimberti S, Graziano F, Maas AIR, Isernia G, Lecky F, Jain S, Sun X, Gardner RC, Taylor SR, Markowitz AJ, Manley GT, Valsecchi MG, Bellelli G, Citerio G, Center TBI, participants T-T, investigators Effect of frailty on 6-month outcome after traumatic brain injury: a multicentre cohort study with external validation. Lancet Neurol. 2022;21:153–162. doi: 10.1016/S1474-4422(21)00374-4. [DOI] [PubMed] [Google Scholar]
- 10.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flaatten H, Guidet B, Andersen FH, Artigas A, Cecconi M, Boumendil A, Elhadi M, Fjolner J, Joannidis M, Jung C, Leaver S, Marsh B, Moreno R, Oeyen S, Nalapko Y, Schefold JC, Szczeklik W, Walther S, Watson X, Zafeiridis T, de Lange DW, Group VIPS Reliability of the clinical frailty scale in very elderly ICU patients: a prospective European study. Ann Intensive Care. 2021;11:22. doi: 10.1186/s13613-021-00815-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruno RR, Wernly B, Flaatten H, Scholzel F, Kelm M, Jung C. The hospital frailty risk score is of limited value in intensive care unit patients. Crit Care. 2019;23:239. doi: 10.1186/s13054-019-2520-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haas LEM, Boumendil A, Flaatten H, Guidet B, Ibarz M, Jung C, Moreno R, Morandi A, Andersen FH, Zafeiridis T, Walther S, Oeyen S, Leaver S, Watson X, Boulanger C, Szczeklik W, Schefold JC, Cecconi M, Marsh B, Joannidis M, Nalapko Y, Elhadi M, Fjolner J, Artigas A, de Lange DW, group VIPs Frailty is associated with long-term outcome in patients with sepsis who are over 80 years old: results from an observational study in 241 European ICUs. Age Ageing. 2021;50:1719–1727. doi: 10.1093/ageing/afab036. [DOI] [PubMed] [Google Scholar]
- 14.Rottler M, Ocskay K, Sipos Z, Gorbe A, Virag M, Hegyi P, Molnar T, Eross B, Leiner T, Molnar Z. Clinical frailty scale (CFS) indicated frailty is associated with increased in-hospital and 30-day mortality in COVID-19 patients: a systematic review and meta-analysis. Ann Intensive Care. 2022;12:17. doi: 10.1186/s13613-021-00977-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jung C, Flaatten H, Fjolner J, Bruno RR, Wernly B, Artigas A, Bollen Pinto B, Schefold JC, Wolff G, Kelm M, Beil M, Sviri S, van Heerden PV, Szczeklik W, Czuczwar M, Elhadi M, Joannidis M, Oeyen S, Zafeiridis T, Marsh B, Andersen FH, Moreno R, Cecconi M, Leaver S, Boumendil A, De Lange DW, Guidet B, group Cs The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care. 2021;25:149. doi: 10.1186/s13054-021-03551-3. [DOI] [PMC free article] [PubMed] [Google Scholar]