Abstract
Cardiorespiratory fitness has been substantially associated with health status. However, longitudinal studies on cardiorespiratory fitness and ideal cardiovascular health behavior (ICHB) in adolescents are scarce. The aim of this study was to evaluate the longitudinal association between ICHB (at baseline) and cardiorespiratory fitness (at follow-up). This is a 2-year prospective analysis of 445 adolescents (232 girls) aged 12–18 years. The ICHB was developed by the American Heart Association as meeting the ideal health behaviors for a healthy diet, physical activity, smoking status, and body mass index. ANCOVAS adjusted by age, sex, pubertal stage, socioeconomic status, and cardiorespiratory fitness showed that the higher the number of ICHB metrics accumulated at baseline (from 1 to 4), the higher the cardiorespiratory fitness levels over a 2-year period (p = 0.038). In logistic regressions, after adjusting for potential confounders, the odds ratios for having high cardiorespiratory fitness at follow-up was 4.9 (95% CI, 1.2–20.1, p = 0.02) for those who accumulated all four metrics of ICHB, when compared to those with 1 or less metrics of ICHB. In addition, the higher the number of ICHB metrics accumulated, the higher the likelihood of having a high cardiorespiratory fitness level over a 2-year period (p for trend = 0.01).
Conclusion: We identified a significant association between ICBH and cardiorespiratory fitness in adolescents. Therefore, improving ICBH in adolescence is likely to benefit the cardiorespiratory fitness.
| What is Known: |
| • Smoking status, body mass index, physical activity, and diet are associated to cardiorespiratory fitness in adulthood. |
| • Lifestyle behaviors such as physical activity, smoking, body weight, and healthy diet are individually linked with cardiorespiratory fitness and, however, have not been examined jointly, as combined health behaviors. |
| What is New: |
| • Accumulation of cardiovascular health behavior metrics was positively associated with cardiorespiratory fitness at a 2-year follow-up, in adolescents. |
| • Meeting all the four metrics of ideal cardiovascular health behavior seems important for healthy cardiorespiratory fitness during adolescence. |
Keywords: Aerobic fitness; Metabolic health; Youth, Physical activity, Cardiovascular health behavior
Introduction
Adequate levels of cardiorespiratory fitness reduce the risk of all-cause risk mortality [1–3], incidence of heart diseases [4], and metabolic and other health disorders [5]. Recent research even indicates the possible immunoprotective role of cardiorespiratory fitness against SARS-CoV-2 [6], and highlights the importance of increasing cardiorespiratory fitness in the general population to booster resilience to COVID-19 and other possible pandemics in the future [7]. Due to its diagnostic and prognostic value, cardiorespiratory fitness is considered an essential marker in routine health assessment [1, 8] for chronic disease prevention [3]. In youth, cardiorespiratory fitness is an important predictor of not only physical health [4, 9–16], but also mental health [17, 18], and increases academic achievement [19–22]. Higher cardiorespiratory fitness is associated with lower risk of cardiovascular diseases [9, 10, 23], improved metabolic health [11, 13, 24], and type 2 diabetes, and adds to better lung function [15, 25] and health-related quality of life [26], in adolescents. It has also been shown that cardiorespiratory fitness, in adolescence, is an indicator of higher burden of future disability [27].
Previous research has analyzed individual associations between different cardiovascular health behaviors and cardiorespiratory fitness. Significant associations were found between eating habits [28], smoking [29], body mass index (BMI) [30, 31], and cardiorespiratory fitness level in teens. However, longitudinal data covering all four cardiovascular health behaviors in combination (smoking status, body mass index, physical activity, diet) in adolescence is scarce. Indeed, studies targeting all four cardiovascular health behaviors (not only physical activity) in young age may contribute to health benefits through improvements in cardiorespiratory fitness. In this context, the aim of this study is to verify the association between accumulation of ideal cardiovascular health behavior (at baseline) and cardiorespiratory fitness at 2-year follow-up.
Methods
Study design and sample
The present study is a part of the “Longitudinal Analysis of Biomarkers and Environmental Determinants of Physical Activity (LabMed Physical Activity Study),” a school-based cohort conducted in northern Portugal. A more detailed discussion of sample and recruiting methodologies, processes, and protocols may be found elsewhere [19, 31]. In brief, baseline data for 1229 adolescents aged 12 to 18 years were collected in 2011, and 1011 and 789 patients were reevaluated 1 (follow-up 1) and 2 years later (follow-up 2), respectively. Considering potential refusals to participate in the study due to blood analysis or accelerometer use for 1 week, a “layered consent” was permitted. This allowed participants to consent some parts of the study protocol and not others. For example, an adolescent could perform physical fitness assessments and refuse to undergo blood analysis or accelerometer use. The present analysis consists of 445 adolescents who consented to use the accelerometers and undergo blood analysis. Therefore, at baseline and the 2nd follow-up, 445 adolescents aged 12 to 18 years (232 females) had complete data on the variables of interest for the current study. When compared to the initial sample (n = 1229 vs n = 445), the participants included in the current analysis were similar in terms of age (14.1 ± 1.6 vs 13.8 ± 1.6), body mass index (21 ± 3.8 vs 20.9 ± 3.5), cardiorespiratory fitness (VO2peak mL/kg/min) (42.3 ± 6.8 vs 42.1 ± 6.9), KIDMED score (7.1 ± 2 vs 7.2 ± 2.1), and for non-smokers (90% vs 93%).
Power analysis was calculated post hoc, for multiple regression analysis and analysis of covariance (ANCOVA), assuming a power of 80%, an effect size of 0.02, at two-sided 0.05 level.
The study was carried out in accordance with the World Medical Association’s Helsinki Declaration for Human Studies. The study was approved by the Portuguese Data Protection Authority (#1,112,434/2011), the Portuguese Ministry of Science and Education (0,246,200,001/2011), and the Faculty of Sport at the University of Porto. All research participants were informed of the study’s objectives, and signed informed consent was acquired from participating adolescents and their parents or guardians.
Measures
Cardiovascular health behaviors
Based on the American Heart Association definition, four cardiovascular health behaviors (body mass index, smoking behavior, physical activity, and diet) were considered. The determinants for the ideal cardiovascular health behavior metrics were classified according to the recommendations of the American Heart Association for 5- to 19-year-old children and adolescents [32].
Body mass index
In accordance with established protocols, participants’ heights and weight were recorded while they were lightly dressed and barefoot on a portable stadiometer (Seca213, Hamburg, Germany) and a portable electronic weight scale (Tanita Inner Scan BC532, Tokyo, Japan) was used to measure the height and weight of the participants. Weight (kg)/height (m) was used to determine the BMI, or body mass index (m2). We categorized participants according to the WHO [33] criteria for children/adolescents (non-overweight, overweight, and obese). To compose the ICHB metrics, non-overweight participants were classified as ideal and overweight and obese as not ideal.
Dietary assessment
The KIDMED questionnaire (Mediterranean Diet Quality Index for children and adolescents) [34] was used to analyze dietary intake and food consumption, with an index ranging from 0 to 12 points. Participants were classified as having an ideal healthy diet (≥ 8 points), whereas children and adolescents with < 7 points were classified as having a non-ideal healthy diet, as previously reported [35].
Physical activity level
Accelerometers GT1M (ActiGraph, Pensacola, FL, USA) were used to assess physical activity. Participants were instructed to wear the accelerometer on the right side of the hip, with the notch facing up for 5 days in a row (three weekdays and two weekend days) and to take it off for water-based activities. While setting the 2-s epoch length, more precise estimations of physical activity intensity was made. Analyzing the accelerometer data was done using an automated tool for data reduction (ActivLive software v. 6.12, ActiGraph, Pensacola, FL, USA). Non-wear time was identified as periods with 60 min of consecutive zeros. For determining levels of physical activity, the cut-points recommended by Evenson, Catellier et al. [36] were used. More than 60 min of moderate-to-vigorous physical exercise per day was considered an ideal level of physical activity for adolescents [32, 35].
Smoking habits
Self-reported questionnaires were used to collect smoking data. Never smokers were considered having ideal smoking behaviors.
Controlling variables
Pubertal stage
In accordance with Tanner and Whitehouse’s criteria, participants self-assessed their pubertal stage of secondary sex characteristics (breast and pubic hair growth in girls and genital and pubic hair development in boys), which ranged from stage I to V [37].
Socioeconomic status
The Family Affluence Scale 10 was used to determine the socio-economic condition of the adolescents. Based on six questions, the scale had a range of 0 to 13 points. The highest socioeconomic position was indicated with a score of 13. The responses were added together, and a continuum variable was created for the purpose of doing statistical analysis.
Cardiorespiratory fitness
Cardiorespiratory fitness was assessed with the 20-m shuttle run test (20 m SRT). A detailed description of this test can be found elsewhere (Leger run test). The test was performed once, and the number of shuttles performed by each participant was recorded. We estimated the peak oxygen consumption (VO2peak, mL/kg/min) using the equation reported by Leger et al. [38]. The participants were also classified into two cardiorespiratory fitness groups (low and high) according to the proposed cut-off for this population by Ruiz et al. [14].
Statistics analysis
Descriptive data are shown as means and standard deviations. All variables were checked for normality (Kolmogorov–Smirnov test) and presented normal distribution. Numbers (n) and percentage (%) are presented for categorical variables. Independent two-tailed t-tests for continuous variables and chi-square for categorical variables were used to examine sex differences. Paired sample t-test and ANOVA were used to test differences in cardiorespiratory fitness levels by sex at baseline and follow-up.
ANCOVA with Bonferroni post hoc multiple comparison tests was used to assess the differences of cardiorespiratory fitness levels (at baseline and follow-up) across ICHB metrics (at baseline). Cardiorespiratory fitness at follow-up were entered as the dependent variable, ICHB metrics (accumulation of metrics from 0 to 4) was entered as an independent variable, and age, sex, pubertal stage, and socioeconomic status as covariates. Longitudinal analyses were additionally controlled by cardiorespiratory fitness at baseline.
To verify the association between accumulation of ICHB at baseline and cardiorespiratory fitness 2 years later, we conducted logistic analysis to study differences on cardiorespiratory fitness at follow-up by ICHB metrics. Cardiorespiratory fitness at follow-up 2 (high and low) was entered as the dependent variable, ICHB metrics as an independent variable, and age, sex, pubertal stage, socioeconomic status, and cardiorespiratory fitness at baseline as covariates.
Data analysis was performed using the Statistical Package for the Social Sciences for Windows (Version 26.0 SPSS Inc., Chicago, IL). A p value < 0.05 denoted statistical significance. Power analysis was calculated with G*Power (version 3.1.9.2, Dusseldorf, Germany).
Results
Baseline characteristics of the participants are presented in Table 1.
Table 1.
Characteristics of study participants
| Characteristics at baseline | Total (445) | Boys (213) | Girls (232) |
|---|---|---|---|
| Age (year) | 13.8 (± 1.6) | 13.7 (± 1.5) | 13.9 (± 1.6) |
| Body mass index (kg/m2) | 20.9 (± 3.5) | 20.7 (± 3.5) | 21.03 (± 3.5) |
| KIDMED index | 7.21 (± 2.0) | 7.11 (± 2.1) | 7.3 (± 1.8) |
| Moderate-to-vigorous physical activity (min/day) | 56.5 (± 20.6) | 62.3 (± 19.8) | 51.1 (± 19.9)* |
| Socioeconomic Status | 6.5 (± 1.6) | 6.6 (± 1.5) | 6.8 (± 1.5) |
| Pubertal status A: ≤ III/IV/V (%) | 46/43/11 | 54/35/11 | 38/51/11 |
| Pubertal status B: ≤ III/IV/V (%) | 32/49/19 | 39/50/11 | 26/48/26 |
| Cardiovascular health behaviors | |||
| Nonsmokers, n (%) | 416 (93) | 197 (92) | 222 (95) |
| Non-overweight, n (%) | 329 (73) | 163 (76) | 168 (72) |
| Physically active, n (%) | 147 (33) | 96 (44) | 52 (22)* |
| Healthy diet, n (%) | 207 (46) | 97 (45) | 111 (47) |
*Significantly different from girls (p < 0.05)
Pubertal stage A, breast development in girls; genital development in boys. Pubertal stage B, pubic hair development
Overall, most of the participants were nonsmokers (93%) and had a normal BMI for age and sex (73%). However, less than a half of adolescents were eating healthy (46%) and only (33%) of total sample adhered to physical activity guidelines. Boys were more physically active than girls (p < 0.05).
Descriptive characteristics of participants according to cardiovascular health behaviors and cardiorespiratory fitness are shown in Table 2. In girls, both at baseline and follow-up, cardiorespiratory fitness was higher for those who met the ideal tobacco, BMI, and dietary pattern metrics (p < 0.05), whereas for boys, higher cardiorespiratory fitness was observed for those who met ideal BMI and dietary pattern metrics (p < 0.05; baseline and follow-up), and ideal physical activity at baseline (p < 0.05).
Table 2.
Cardiorespiratory fitness levels at baseline and at follow-up by cardiovascular health behaviors at baseline
| Cardiovascular health behaviors | Cardiorespiratory fitness (VO2max, in mL/min/kg) | |||
|---|---|---|---|---|
| Girls | Boys | |||
| Baseline | 2-year follow-up 2 | Baseline | 2-year follow-up | |
| Tobacco | ||||
| Ideal | 36.9 (± 4.7)* | 37.9 (± 4.9)* | 46.1 (± 6.2) | 46.9 (± 6.9) |
| Non-ideal | 36.6 (± 4.8) | 34.4 (± 6.3) | 45.5 (± 6.2) | 44.9 (± 7.2) |
| Body mass index | ||||
| Ideal | 39.9 (± 4.7)* | 38.5 (± 5.2)* | 47.5 (± 5.8)* | 48.1 (± 6.9)* |
| Non-ideal | 37.2 (± 4.1) | 35.7 (± 4.2) | 41.3 (± 4.6) | 42.6 (± 6.1) |
| Physical activity | ||||
| Ideal | 39.8 (± 5.1) | 38.7 (± 5.5) | 46.8 (± 6.1)* | 47.3 (± 6.9) |
| Non-ideal | 38.9 (± 4.6) | 37.4 (± 4.8) | 45.1 (± 6.1) | 46.1 (± 7) |
| Dietary pattern | ||||
| Ideal | 40.1 (± 4.5)* | 38.4 (± 5.1)* | 46.8 (± 6.0)* | 47.8 (± 6.5)* |
| Non-ideal | 38.3 (± 4.7) | 37.8 (± 4.9) | 45.3 (± 6.2) | 45.9 (± 7.2) |
*Different from non-ideal (p < 0.05 for all)
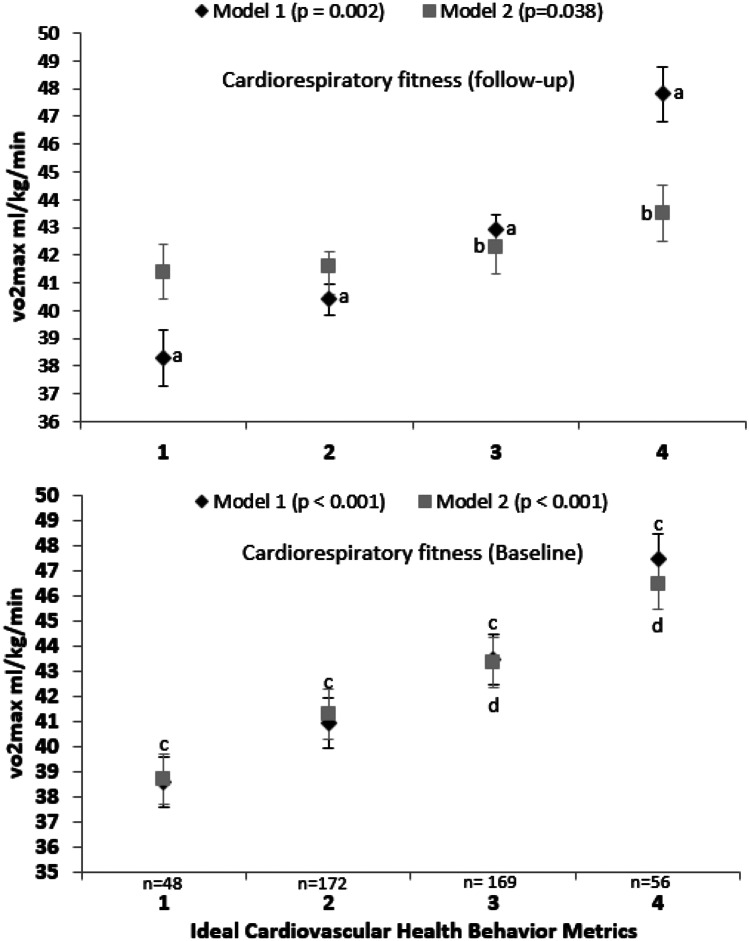
ANCOVA (Fig. 1) showed the differences on cardiorespiratory fitness levels (at baseline and follow-up) by ICHB metrics (at baseline) in two models (unadjusted “model 1” and adjusted “model 2”). Cross-sectional analyses show a significant difference of cardiorespiratory fitness at baseline and all 4 ICHB metrics at baseline (model 1, F(3, 441) = 25. 41, p > 0.001, and model 2, F(3, 435) = 24. 95, p > 0.001). Longitudinal analyses show a significant difference of cardiorespiratory fitness (follow-up) and accumulation of all 4 metrics (baseline) in model 1 (F(3, 441) = 20.69, p > 0.001) and accumulation of 3 and 4 ICHB metrics (baseline) in model 2 (F(3, 434) = 2.61, p = 0.038).
Fig. 1.
Differences on cardiorespiratory fitness levels (at baseline and follow-up) by ideal cardiovascular health behaviors (at baseline). Model 1: unadjusted. Model 2: adjusted for age, sex, pubertal status, and socioeconomic status. The longitudinal analysis (follow-up) was additionally adjusted for its corresponding baseline levels. a Significantly different from all. b Significantly different from 1 and 2. c Significantly different from all. d Significantly different from all
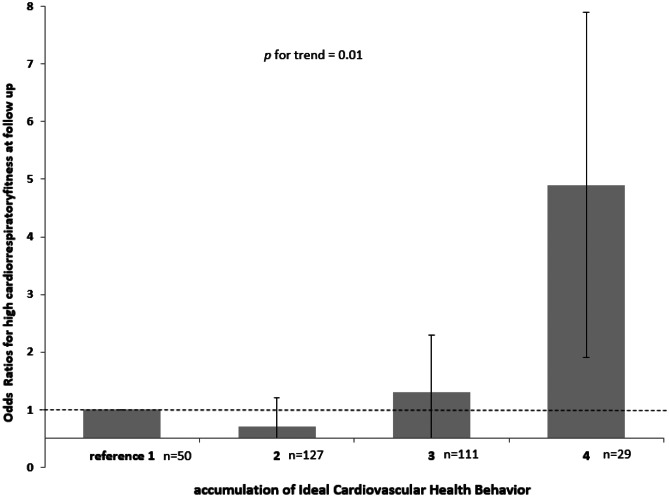
Figure 2 shows the odds for high cardiorespiratory fitness at 2-year follow-up by accumulated metrics of ideal cardiovascular health behavior at baseline. Analyses showed a significant association between ICHB at baseline and cardiorespiratory fitness (p for trend = 0.01), at 2-year follow-up, after adjustment for age, sex, pubertal status, socioeconomic status, and cardiorespiratory fitness at baseline. The odds ratios for having high cardiorespiratory fitness at follow-up were 0.7 for 2 metrics (95% confidence interval [CI], 0.3–1.6) (p = 0.46), 1.3 for 3 metrics (95% CI, 0.6–3.12, p = 0.45), and for 4 metrics 4.9 (95% CI, 1.2–20.1, p = 0.02) when compared to those with 1 or less accumulated metrics of ideal cardiovascular health behaviors, after adjustments for potential confounders.
Fig. 2.
Odds ratios of ideal cardiovascular health behavior metrics (and 95% confidence interval) for high cardiorespiratory fitness at 2-year follow-up, adjusted for age, sex, pubertal status, and socioeconomic status and cardiorespiratory fitness at baseline
Discussion
Our study showed that the accumulation of cardiovascular health behavior metrics was associated with cardiorespiratory fitness at 2-year follow-up.
To the best of our knowledge, this is the first study to report the longitudinal association between ICBH (smoking status, body mass index, physical activity, diet) and cardiorespiratory fitness in adolescents. Adolescence is a critical period of human development characterized by profound physiological changes, and adherence to healthy habits is particularly relevant at this stage of life, since these may influence essential indicators linked to future health outcomes, such as cardiorespiratory fitness. Indeed, cardiorespiratory fitness is considered a critical hallmark for health during youth, and maximal oxygen uptake (VO2 max) a good indicator for it [39].
In addition, our results show that as increase the number of ICHB metrics as higher the cardiorespiratory fitness levels over 2 years. Moreover, those adolescents who had at least 3 or 4 ICHB were significantly different from all others groups (from 1 to 4). Our findings are in line with Ruiz and colleagues who reported a cross-sectional associations between cardiorespiratory fitness and ICHB among European children and adolescents [40]. However, we have extended those results by involving a longitudinal cohort and our results highlight that meeting the ICHB metrics seems important for healthy cardiorespiratory fitness levels 2 years later, in adolescents. In adolescence, ICHB (smoking, BMI, physical activity, and diet) is associated with both mental and physical well-being which leads to an active and healthy lifestyle, reduce the prevalence of mental illnesses [17, 18], and display prognostic ability for all-cause and disease-specific mortality outcomes in adulthood [41]. Despite the fact that our results will need to be confirmed or ruled out by future studies with adolescents, it seems important that ICHB associated with cardiorespiratory fitness at 2-year follow-up, given that it has been shown that adolescence with higher levels of cardiorespiratory fitness tend to perceive their health as better in terms of physical functioning, emotional well-being, self-esteem, and social and family functioning [42]. Another large population-based prospective study showed the impact of cardiorespiratory fitness in adolescence in the prevention of future neurotic disorders [17]. Increasing cardiorespiratory fitness is not only beneficial to adolescents’ mental well-being [18], but also with academic achievement [20, 43]. The effect of how each ICHB component may affect cardiorespiratory fitness in adolescents is not well established. But, it is known that diet [43], physical activity [44], smoke, and obesity [45] have been individually associated with cardiorespiratory fitness.
A recent study showed gender differences in the prevalence of each component of the ICHB [46] and we observed similar trend in our research; we found girls engaged in less ideal physical activity than boys, but have often a healthy diet. Adolescent boys smoking prevalence is usually greater in other adolescent groups [47], which is in line with our results were. Gender plays a significant role in health behaviors throughout the lifespan [48]. During the socialization process, boys are encouraged to be more active than girls [48], whereas among girls, body image dissatisfaction has been associated with healthier eating choices [49]. Important to mention, that our longitudinal analysis were adjusted for potential confounds such as sex, age, pubertal stage and socioeconomic status.
Without an ideal level of cardiovascular health behaviors during adolescence, a significant health benefit is lost, which may result in unacceptably high rates of adult-onset CVD [50]. However, early intervention and prevention actions targeting adolescent ideal cardiorespiratory fitness level have been associated with the maintenance of health parameters in later life [51]. Our findings highlight the need to promote healthy behaviors altogether in order to attained healthy cardiorespiratory fitness levels, in adolescents.
This study has several strengths. First, our research includes four main components of ICHB such as smoking status, body mass index, physical activity, diet and not only discusses the relationship between single component with cardiorespiratory fitness, but also integrates each component to show its relationship more intuitively by using the form of standardized scores. Second, by analyzing a longitudinal cohort we highlight that meeting all the four metrics of ICHB was important for cardiorespiratory fitness 2 years later in adolescents. And finally, the fact that we used objective measures of physical activity and a validated fitness test should also be considered a strength of this study. This study is not without limitations. Firstly, the results are not generalizable due to the sample not being nationally representative. Secondly, the ICHB was assed only in baseline; hence longitudinal research in adolescents is needed verify the changes in ICHB and its effects. Lastly, it should also be noted that the formation of the ICHB metrics relies on the use of binary variables and on the assumption that all components contained in this score contribute in the same way to the final index.
In summary, we identified a significant association between ICBH at baseline and cardiorespiratory fitness over 2 years in adolescents. Therefore, improving ICBH in adolescence is likely to benefit the cardiorespiratory fitness.
Abbreviations
- ICHB
Ideal cardiovascular health behavior
- BMI
Body mass index
- CVD
Cardiovascular disease
- SRT
Shuttle run test
Authors’ contributions
César Agostinis-Sobrinho and Rute Santos designed and carried out the initial analyses, drafted the initial manuscript, and participated in data collection, participated in the study design, interpretation of data and revised the manuscript; Luis Lopes and Carla Moreira participated in the study design, reviewed and data interpretation; Justina Kievišienė, Viney Prakash Dubey, Sigute Norkiene, and Alona Rauckienė-Michaelsson participated in data interpretation and reviewed the manuscript; and all authors revised and approved the final manuscript as submitted.
Funding
Rute Santos is supported by the Portuguese Foundation for Science and Technology (CEECIND/01069/2017; FCT/UIDB/00617/2020 and ITR—LA/P/0064/2020). Luis Lopes is supported by the Portuguese Foundation for Science and Technology (CEECIND/01089/2017; FCT/UIDB/00617/2020 and ITR—LA/P/0064/2020.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval
The study was carried out in accordance with the World Medical Association’s Helsinki Declaration for Human Studies. The study was approved by the Portuguese Data Protection Authority (#1112434/2011), the Portuguese Ministry of Science and Education (0246200001/2011), and the Faculty of Sport at the University of Porto.
Consent to participate
All research participants were informed of the study’s objectives, and signed informed consent was acquired from participating adolescents and their parents or guardians.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
César Agostinis-Sobrinho, Email: cesaragostinis@hotmail.com.
Justina Kievišienė, Email: justina.kievisiene@gmail.com.
Alona Rauckienė-Michaelsson, Email: alona.rauckiene-michaelsson@ku.lt.
Viney Prakash Dubey, Email: vineydreamz@gmail.com.
Sigute Norkiene, Email: sigute.norkiene@gmail.com.
Carla Moreira, Email: carla_m_moreira@sapo.pt.
Rute Santos, Email: rutemarinasantos@hotmail.com.
References
- 1.Lee D, Artero EG, Sui X, Blair SN. Mortality trends in the general population : the importance of cardiorespiratory fitness. 2010 doi: 10.1177/1359786810382057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mandsager K, Harb S, Cremer P, Phelan D, Nissen SE, Jaber W. Association of Cardiorespiratory Fitness With Long-term Mortality Among Adults Undergoing Exercise Treadmill Testing. 2018;1:1–12. doi: 10.1001/jamanetworkopen.2018.3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaminsky LA, Arena R, Ellingsen Ø, Harber MP, Myers J, Ozemek C, et al. Progress in Cardiovascular Diseases Cardiorespiratory fi tness and cardiovascular disease - the past, present, and future. Prog Cardiovasc Dis. 2019;62:86–93. doi: 10.1016/j.pcad.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Lindgren M, Bo M (2021) The importance of physical activity and cardiorespiratory fitness for patients with heart failure. 176. 10.1016/j.diabres.2021.108833 [DOI] [PubMed]
- 5.McKinney J, Lithwick DJ, Morrison BN, Nazzari H, Isserow SH, Heilbron B, Krahn AD (2016) The health benefits of physical activity and cardiorespiratory fitness. B C Med J 58:131–7
- 6.Zbinden-Foncea H, Francaux M, Deldicque L, Hawley JA. Does High Cardiorespiratory Fitness Confer Some Protection Against Proinflammatory Responses After Infection by SARS-CoV-2 ? The Calm Before the Storm : Cytokine. Obesity. 2020;00:1–4. doi: 10.1002/oby.22849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bak EE, Väisänen D, Ekblom B, Blom V, Kallings LV, Hemmingsson E, et al. Cardiorespiratory fitness and lifestyle on severe COVID - 19 risk in 279, 455 adults : a case control study. Int J Behav Nutr Phys Act. 2021;18:1–16. doi: 10.1186/s12966-021-01198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Despres J (2016) Physical Activity, Sedentary Behaviours, and Cardiovascular Health : When Will Cardiorespiratory Fitness Become a Vital Sign ? Can J Cardiol 1–9. 10.1016/j.cjca.2015.12.006 [DOI] [PubMed]
- 9.Agostinis-Sobrinho C, Ruiz JR, Moreira C, Abreu S, Lopes L, Oliveira-Santos J, et al. Cardiorespiratory Fitness and Blood Pressure: A Longitudinal Analysis. J Pediatr. 2018;192:130–135. doi: 10.1016/j.jpeds.2017.09.055. [DOI] [PubMed] [Google Scholar]
- 10.Agostinis-Sobrinho CA, Ruiz JR, Moreira C, Abreu S, Luís L, Oliveira-Santos J, et al. Cardiorespiratory fitness and inflammatory profile on cardiometabolic risk in adolescents from the LabMed Physical Activity Study. Eur J Appl Physiol. 2017;117:2271–2279. doi: 10.1007/s00421-017-3714-x. [DOI] [PubMed] [Google Scholar]
- 11.Mintjens S, Menting MD, Daams JG, van Poppel MNM, Roseboom TJ, Gemke RJBJ. Cardiorespiratory fitness in childhood and adolescence affects future cardiovascular risk factors: a systematic review of longitudinal studies. Sport Med. 2018;48:2577–2605. doi: 10.1007/s40279-018-0974-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agostinis-Sobrinho C, Rosário R, Santos R, Norkiene S, Mota J, Rauckienė-Michaelsson A et al (2020) Higher cardiorespiratory fitness levels may attenuate the detrimental association between weight status, metabolic phenotype and c-reactive protein in adolescents—a multi-cohort study. Nutrients 12. 10.3390/nu12051461 [DOI] [PMC free article] [PubMed]
- 13.Neto AS, Sasaki JE, Mascarenhas LPG, Boguszewski MCS, Bozza R, Ulbrich AZ et al (2011) Physical activity, cardiorespiratory fitness, and metabolic syndrome in adolescents : A cross-sectional study [DOI] [PMC free article] [PubMed]
- 14.Ruiz JR, Cavero-Redondo I, Ortega FB, Welk GJ, Andersen LB, Martinez-Vizcaino V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br J Sports Med. 2016;50:1451–1458. doi: 10.1136/bjsports-2015-095903. [DOI] [PubMed] [Google Scholar]
- 15.Raghuveer Geeta et al (2020) Cardiorespiratory Fitness in Youth : An Important Marker of Health. 101–18. 10.1161/CIR.0000000000000866 [DOI] [PMC free article] [PubMed]
- 16.ME C et al (2020) Mental Health, Substance Use, and Suicidal Ideation During the COVID-19. 69:2018–9
- 17.Nyberg J, Henriksson M, Åberg MAI, Rosengren A, Söderberg M, Åberg ND, et al. Cardiovascular fitness in late adolescent males and later risk of serious non-affective mental disorders: A prospective, population-based study. Psychol Med. 2018;48:416–425. doi: 10.1017/S0033291717001763. [DOI] [PubMed] [Google Scholar]
- 18.Eddolls WTB, McNarry MA, Lester L, Winn CON, Stratton G, Mackintosh KA. The association between physical activity, fitness and body mass index on mental well-being and quality of life in adolescents. Qual Life Res. 2018;27:2313–2320. doi: 10.1007/s11136-018-1915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oliveira-Santos J, Santos R, Moreira C, Abreu S, Lopes L, Agostinis-Sobrinho C, et al. Ability of Measures of Adiposity in Identifying Adverse Levels of Inflammatory and Metabolic Markers in Adolescents. Child Obes. 2016;12:135–146. doi: 10.1089/chi.2015.0124. [DOI] [PubMed] [Google Scholar]
- 20.Marques A, Santos DA, Hillman CH, Sardinha LB (2017) How does academic achievement relate to cardiorespiratory fitness, self-reported physical activity and objectively reported physical activity : a systematic review in children and adolescents aged 6 – 18 years. 1–11. 10.1136/bjsports-2016-097361 [DOI] [PubMed]
- 21.Meijer A, Königs M, de Bruijn AGM, Visscher C, Bosker RJ, Hartman E, et al. Cardiovascular fitness and executive functioning in primary school-aged children. Dev Sci. 2021;24:1–13. doi: 10.1111/desc.13019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meijer A, Pouwels PJW, Smith J, Visscher C, Bosker RJ, Hartman E, et al. The relationship between white matter microstructure, cardiovascular fitness, gross motor skills, and neurocognitive functioning in children. J Neurosci Res. 2021;99:2201–2215. doi: 10.1002/jnr.24851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindgren M, Maria A, Schio L, Tore K (2017) Cardiorespiratory fitness and muscle strength in late adolescence and long-term risk of early heart failure in Swedish men. Eur J Prev Cardiol 1–9. 10.1177/2047487317689974 [DOI] [PubMed]
- 24.Agostinis-Sobrinho C, Ramírez-Vélez R, García-Hermoso A, Rosário R, Moreira C, Lopes L, et al. The combined association of adherence to Mediterranean diet, muscular and cardiorespiratory fitness on low-grade inflammation in adolescents: a pooled analysis. Eur J Nutr. 2019;58:1–8. doi: 10.1007/s00394-018-1812-0. [DOI] [PubMed] [Google Scholar]
- 25.Ortega FB, Ruiz JR, Castillo MJ, Sjöström M. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes (Lond) 2008;32:1–11. doi: 10.1038/sj.ijo.0803774. [DOI] [PubMed] [Google Scholar]
- 26.Agostinis-Sobrinho C, Werneck A de O, Kievišienė J, Moreira C, Ramírez-Vélez R, Rosário R et al (2021) Ideal cardiovascular health status and health-related quality of life in adolescents: the labmed physical activity study. Rev Paul Pediatr 39. 10.1590/1984-0462/2021/39/2019343 [DOI] [PMC free article] [PubMed]
- 27.Henriksson P, Shiroma EJ, Henriksson H, Tynelius P, Berglind D, Löf M et al (2020) Fit for life ? Low cardiorespiratory fitness in adolescence is associated with a higher burden of future disability. Br J Sport Med Epub Ahead Prin 1–2. 10.1136/bjsports-2020-102605 [DOI] [PMC free article] [PubMed]
- 28.Howe AS, Skidmore PML, Parnell WR, Wong JE, Lubransky AC, Black KE. Cardiorespiratory fitness is positively associated with a healthy dietary pattern in New Zealand adolescents. Public Health Nutr. 2016;19:1279–1287. doi: 10.1017/S1368980015002566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flouris AD, Faught BE, Klentrou P. Cardiovascular disease risk in adolescent smokers: Evidence of a ’smoker lifestyle. J Child Heal Care. 2008;12:221–231. doi: 10.1177/1367493508092509. [DOI] [PubMed] [Google Scholar]
- 30.Aires L, Silva P, Silva G, Santos MP, Ribeiro JC, Mota J. Intensity of physical activity, Cardiorespiratory Fitness, and body mass index in youth. J Phys Act Heal. 2010;7:54–59. doi: 10.1123/jpah.7.1.54. [DOI] [PubMed] [Google Scholar]
- 31.Agostinis-Sobrinho C, Santos R, Moreira C, Abreu S, Lopes L, Oliveira-Santos J, et al. Association between serum adiponectin levels and muscular fitness in Portuguese adolescents: LabMed Physical Activity Study. Nutr Metab Cardiovasc Dis. 2016;6:517–524. doi: 10.1016/j.numecd.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 32.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The american heart association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 33.Organization WH (2006) WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development
- 34.Serra-Majem L, Ribas L, Ngo J, Ortega RM, García A, Pérez-Rodrigo C et al (2004) Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr 7:931–5. 10.1079/PHN2004556 [DOI] [PubMed]
- 35.Agostinis-Sobrinho C, García-Hermoso A, Ramírez-Vélez R, Moreira C, Lopes L, Oliveira-Santos J, et al. Longitudinal association between ideal cardiovascular health status and muscular fitness in adolescents: The LabMed Physical Activity Study. Nutr Metab Cardiovasc Dis. 2018;28:892–899. doi: 10.1016/j.numecd.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 36.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26:1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 37.Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51:170–179. doi: 10.1136/adc.51.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Léger LA, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. J Sports Sci. 1988;6:93–101. doi: 10.1080/02640418808729800. [DOI] [PubMed] [Google Scholar]
- 39.López-Bueno R, Calatayud J, Andersen LL, Casaña J, Ezzatvar Y, Casajús JA et al (2021) Correction to: cardiorespiratory fitness in adolescents before and after the COVID-19 confinement: a prospective cohort study. Eur J Pediatr 180:2295. 10.1007/s00431-021-04029-8. 10.1007/s00431-021-04107-x [DOI] [PMC free article] [PubMed]
- 40.Ruiz JR, Huybrechts I, Cuenca-Garcia M, Artero EG, Labayen I, Meirhaeghe A et al (2014) Cardiorespiratory fitness and ideal cardiovascular health in European adolescents. Heart 1–8. 10.1136/heartjnl-2014-306750 [DOI] [PubMed]
- 41.Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DL, Kaminsky LA. Cardiorespiratory Fitness and Mortality in Healthy Men and Women. J Am Coll Cardiol. 2018;72:2283–2292. doi: 10.1016/j.jacc.2018.08.2166. [DOI] [PubMed] [Google Scholar]
- 42.Cesar E (2019) Journal of Exercise Science & Fitness Muscular fi tness and cardiorespiratory fi tness are associated with health-related quality of life : Results from labmed physical activity study. 17:55–61. 10.1016/j.jesf.2019.01.002 [DOI] [PMC free article] [PubMed]
- 43.Galan-Lopez P, Sánchez-Oliver AJ, Ries F, González-Jurado JA (2019) Mediterranean diet, physical fitness and body composition in sevillian adolescents: A healthy lifestyle. Nutrients 11. 10.3390/nu11092009 [DOI] [PMC free article] [PubMed]
- 44.Santos R, Mota J, Okely AD, Pratt M, Moreira C, Coelho-E-Silva MJ, et al. The independent associations of sedentary behaviour and physical activity on cardiorespiratory fitness. Br J Sports Med. 2014;48:1508–1512. doi: 10.1136/bjsports-2012-091610. [DOI] [PubMed] [Google Scholar]
- 45.Prieto-Benavides DH, García-Hermoso A, Izquierdo M, Alonso-Martínez AM, Agostinis-Sobrinho C, Correa-Bautista JE et al (2019) Cardiorespiratory Fitness Cut-Points are Related to Body Adiposity Parameters in Latin American Adolescents. Medicina (Kaunas) 55. 10.3390/medicina55090508 [DOI] [PMC free article] [PubMed]
- 46.Gande N, Pechlaner R, Bernar B, Staudt A, Stock K, Hochmayr C, et al. Cardiovascular health behaviors and associations of sex, age, and education in adolescents - results from the EVA Tyrol study. Nutr Metab Cardiovasc Dis. 2021;31:1286–1292. doi: 10.1016/j.numecd.2020.11.002. [DOI] [PubMed] [Google Scholar]
- 47.Pahkala K, Hietalampi H, Laitinen TT, Viikari JSA, Rönnemaa T, Niinikoski H, et al. Ideal cardiovascular health in adolescence effect of lifestyle intervention and association with vascular intima-media thickness and elasticity (the special turku coronary risk factor intervention project for children [STRIP] Study) Circulation. 2013;127:2088–2096. doi: 10.1161/CIRCULATIONAHA.112.000761. [DOI] [PubMed] [Google Scholar]
- 48.Lampinen EK, Eloranta AM, Haapala EA, Lindi V, Väistö J, Lintu N, et al. Physical activity, sedentary behaviour, and socioeconomic status among Finnish girls and boys aged 6–8 years. Eur J Sport Sci. 2017;17:462–472. doi: 10.1080/17461391.2017.1294619. [DOI] [PubMed] [Google Scholar]
- 49.Bibiloni MDM, Pich J, Pons A, Tur JA (2013) Body image and eating patterns among adolescents. BMC Public Health 13. 10.1186/1471-2458-13-1104 [DOI] [PMC free article] [PubMed]
- 50.Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127:1369–1376. doi: 10.1161/CIRCULATIONAHA.113.001559. [DOI] [PubMed] [Google Scholar]
- 51.Garciá-Hermoso A, Ramírez-Vélez R, Garciá-Alonso Y, Alonso-Martínez AM, Izquierdo M. Association of Cardiorespiratory Fitness Levels during Youth with Health Risk Later in Life: A Systematic Review and Meta-analysis. JAMA Pediatr. 2020;174:952–960. doi: 10.1001/jamapediatrics.2020.2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.