Jose Antonio PeÑas/ Science Photo Library
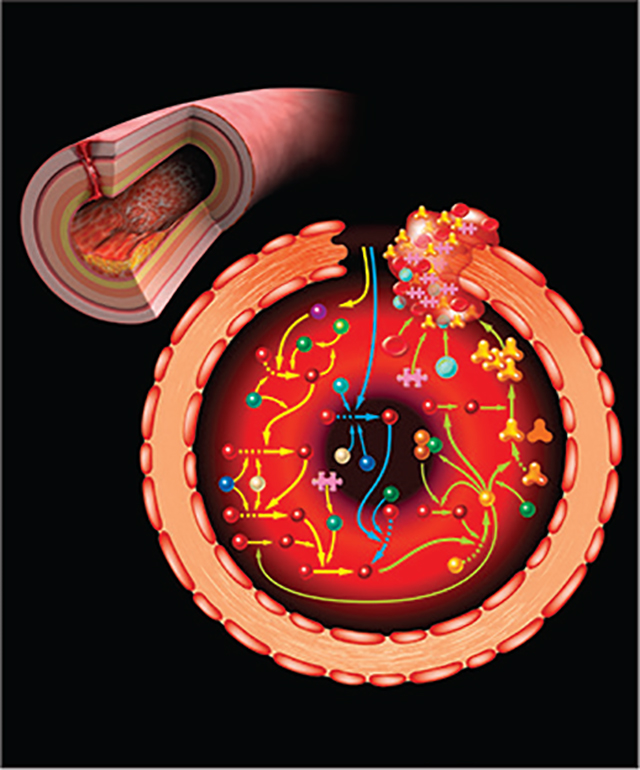
Oral anticoagulants currently used for prevention or treatment of thrombosis inhibit the proteases factor Xa (FXa) or thrombin, or lower the plasma concentrations of their precursors, factor X and prothrombin. Numerous studies document the effectiveness of these agents. However, their use also leads to substantial increases in major and minor bleeding.1,2 This is not surprising; FXa and thrombin are at the core of the system that stems bleeding after blood vessel injury. Drugs targeting these proteases, therefore, can compromise haemostasis, and bleeding restricts the intensity of anticoagulation that can be tolerated. Furthermore, many patients who would benefit from anticoagulation are ineligible for treatment because co-existing conditions place them at unacceptable risk for bleeding. Clearly, safer antithrombotic strategies are required. Specifically, we need to identify drug targets that are important for driving or sustaining pathological thrombus formation, but that are less important to haemostasis than are FXa and thrombin.3 Mounting evidence indicates the plasma protease factor XIa (FXIa) is such a target.
Factor XI (FXI), the precursor of FXIa, is part of the intrinsic pathway of coagulation, which initiates clotting in the activated partial thromboplastin time (aPTT) assay.4 Curiously, although congenital FXI deficiency causes a marked prolongation of the aPTT, it is associated with a mild bleeding disorder.5 Excessive bleeding in FXI deficiency, if it occurs, usually follows trauma to certain tissues (oropharynx or urinary tract). Bleeding into the CNS, gastrointestinal tract, joints, and muscles are not features of FXI deficiency, and spontaneous bleeding is rare. Despite its limited role in haemostasis, there is compelling evidence that FXI contributes to thrombosis, and particularly to venous thromboembolism and ischaemic stroke.6 In phase 2 studies with patients undergoing knee replacement, lowering plasma FXI or inhibiting FXIa reduced the incidence of postoperative venous thromboembolism as well as, or better than, standard treatment.7–10 However, although these studies showed that FXI or FXIa inhibition reduces thrombosis in a specific clinical setting, they were not designed to study the effect on bleeding.
In The Lancet, Jonathan Piccini and colleagues11 present data from PACIFIC-AF, a phase 2 double-blind randomised trial powered to assess bleeding in patients with atrial fibrillation (CHA2DS2-VASc scores ≥2) receiving 12-week courses of the FXIa inhibitor asundexian or the FXa inhibitor apixaban. The primary endpoint was a composite of major or clinically relevant non-major bleeding according to International Society on Thrombosis and Haemostasis criteria. 753 patients were included in the analysis (249 received asundexian 20 mg per day, 254 received asundexian 50 mg per day, and 250 received apixaban twice daily). The mean age was 73·7 years (SD 8·3), 309 (41%) were women, 216 (29%) had chronic kidney disease, and the mean CHA2DS2-VASc score was 3·9 (1·3). Trough concentrations of asundexian reduced FXIa activity by 80–90%, indicating substantial inhibition of the target. Ratios of incidence proportions for the primary endpoint were 0·50 (90% CI 0·14–1·68) for 20 mg asundexian, 0·16 (0·01–0·99) for 50 mg asundexian, and 0·33 (0·09–0·97) for the pooled asundexian doses, compared with apixaban. Results for all bleeding events (including minor bleeding) showed similar reductions in favour of asundexian. Rates of non-bleeding adverse events were similar in the treatment groups.
Enthusiasm for drugs targeting FXI or FXIa is based on the promise that such agents will uncouple desired antithrombotic effects from deleterious anti-haemostatic effects.3 PACIFIC-AF is the first in-human trial to show a reduction in bleeding with an FXIa inhibitor when compared with standard treatment. The results contribute to a growing body of evidence that justifies pursuing antithrombotic strategies that target FXI or FXIa. However, the study has limitations. PACIFIC-AF was designed as a phase 2 dose-finding study, and it was not powered to test differences in rates of thrombosis between groups. Furthermore, the number of bleeding events was only half of the anticipated number (ten compared with 20 events), and no major bleeding events were observed. Therefore, although asundexian is likely to have caused less bleeding than apixaban, the results did not allow the magnitude of the effect to be accurately determined. The authors point out a strong correlation between minor and major bleeding in other anticoagulation trials.12 However, this concept might not be useful for studies comparing an FXIa inhibitor to conventional anticoagulation. More than 60 years of experience with patients lacking FXI indicate that they are not more prone to intracranial or gastrointestinal haemorrhage than the general population. Given this, compared with FXa inhibitors, FXIa inhibitors might not only be associated with fewer bleeding episodes, but also with types of bleeding events that are less life-threatening. Studies designed to investigate this possibility are required.
Acknowledgments
I receive funding from the US National Institutes of Health for research into the roles of FXI and other plasma proteins in thrombosis and inflammation. I receive or have received consulting fees from companies with interests in targeting FXI or FXIa for therapeutic purposes (Anthos Therapeutics, Aronora, Bayer, Bristol-Myers Squibb, Ionis, Janssen, and Novartis), including Bayer, the sponsor of the PACIFIC-AF trial, but unrelated to asundexian. I serve, or have served, on boards of clinical trials of FXIa inhibitors run by Bristol-Myers Squibb and Janssen and have received travel honoraria to attend meetings at the invitation of Anthos Therapeutics.
References
- 1.Jiang H, Jiang Y, Ma H, Zeng H, Lv J. Effects of rivaroxaban and warfarin on the risk of gastrointestinal bleeding and intracranial hemorrhage in patients with atrial fibrillation: systematic review and meta-analysis. Clin Cardiol 2021; 44: 1208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wysowski DK, Nourjah P, Swartz L. Bleeding complications with warfarin use: a prevalent adverse effect resulting in regulatory action. Arch Intern Med 2007; 167: 1414–19. [DOI] [PubMed] [Google Scholar]
- 3.Hsu C, Hutt E, Bloomfield DM, Gailani D, Weitz JI. Factor XI inhibition to uncouple thrombosis from hemostasis: JACC review topic of the week. J Am Coll Cardiol 2021; 78: 625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohammed BM, Matafonov A, Ivanov I, et al. An update on factor XI structure and function. Thromb Res 2018; 161: 94–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.James P, Salomon O, Mikovic D, Peyvandi F. Rare bleeding disorders—bleeding assessment tools, laboratory aspects and phenotype and therapy of FXI deficiency. Haemophilia 2014; 20 (suppl 4): 71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Preis M, Hirsch J, Kotler A, et al. Factor XI deficiency is associated with lower risk for cardiovascular and venous thromboembolism events. Blood 2017; 129: 1210–15. [DOI] [PubMed] [Google Scholar]
- 7.Büller HR, Bethune C, Bhanot S, et al. Factor XI antisense oligonucleotide for prevention of venous thrombosis. N Engl J Med 2015; 372: 232–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weitz JI, Bauersachs R, Becker B, et al. Effect of osocimab in preventing venous thromboembolism among patients undergoing knee arthroplasty: the FOXTROT randomized clinical trial. JAMA 2020; 323: 130–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verhamme P, Yi BA, Segers A, et al. Abelacimab for prevention of venous thromboembolism. N Engl J Med 2021; 385: 609–17. [DOI] [PubMed] [Google Scholar]
- 10.Weitz JI, Strony J, Ageno W, et al. Milvexian for the prevention of venous thromboembolism. N Engl J Med 2021; 385: 2161–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Piccini JP, Caso V, Connolly SJ, et al. Safety of the oral factor XIa inhibitor asundexian compared with apixaban in patients with atrial fibrillation (PACIFIC-AF): a multicentre, randomised, double-blind, double-dummy, dose-finding phase 2 study. Lancet 2022; published online April 3. https://doi.org/S0140-6736(22)00456-1. [DOI] [PubMed] [Google Scholar]
- 12.Bahit MC, Lopes RD, Wojdyla DM, et al. Non-major bleeding with apixaban versus warfarin in patients with atrial fibrillation. Heart 2017; 103: 623–28. [DOI] [PMC free article] [PubMed] [Google Scholar]


