Abstract
Objective
To conduct the first systematic review critically examining evidence on whether early male circumcision has short‐ and long‐term adverse psychological effects.
Methods
We searched PubMed, EMBASE, SCOPUS, Cochrane Library, and Google Scholar.
Results
Twenty‐four studies with original data met the inclusion criteria. These comprised 11,173 total males, 4340 circumcised in infancy and 6908 uncircumcised. Nineteen were rated 1+, 2++ or 2+, and 5 were rated 2– by SIGN criteria. Neonatal circumcision, particularly without anesthetic, increased vaccination pain response, but had little effect on breastfeeding or cognitive ability. Studies reporting associations with sudden infant death syndrome, autism, alexithymia and impaired sexual function and pleasure had design flaws and were rated 2–. Sexual arousal, touch, pain, and warmth thresholds measured by quantitative sensory testing were not diminished in neonatally circumcised men. Neonatal circumcision was not associated with empathy in men, contradicting the hypothesis that procedural pain causes central nervous system changes. After correcting all associations with socioaffective processing parameters for multiple testing only higher sociosexual desire, dyadic sexual libido/drive, and stress remained significant. The relatively greater sexual activity found in circumcised men might reflect reduced sexual activity in uncircumcised men overall owing to pain and psychological aversion in those with foreskin‐related medical conditions (reverse causality). Most studies employed case‐control designs with limited follow‐up. Studies beyond childhood were prone to confounding.
Conclusion
The highest quality evidence suggest that neonatal and later circumcision has limited or no short‐term or long‐term adverse psychological effects.
Keywords: circumcision male, psychological outcomes, public health, sexual satisfaction, surgical pain
1. INTRODUCTION
Plasticity of the nociceptive system is seen during development. 1 There is evidence that brain regions with sensory and affective components of pain are active in infants, suggesting that the pain experience in infants might closely resemble that in adults. 2 This led to suggestions that acute pain during the neonatal period (weeks 0–4 of life) might have short‐term and/or long‐term adverse psychological consequences. Neonatal male circumcision (NMC) and MC in older boys without anesthetic can cause acute pain. 3 In the United States, most circumcisions are performed in the first week of life. 4 A study determined that 6.5% of neonates exceeded a “neonatal/infant circumcision pain score” of 2/7, compared with 100% after age 4 weeks. 5 Local anesthetic (ring‐block) reduced but did not eliminate pain scores during clamp NMCs. 6 Since 1999, anesthesia for NMC has therefore been recommended. 7
To date a systematic evaluation of the broad range of potential psychological harms claimed by some for MC early in childhood has never been conducted. The aims of this review were to (i) identify psychological, psychophysiological and psychosocial sequelae attributed to NMC and MC of older boys and (ii) then critically examine evidence for and against adverse short‐term or long‐term psychological outcomes.
2. METHODS
2.1. Search strategy and study selection
Table 1 defines all abbreviations. Following PRISMA guidelines (Supplementary material), 8 we performed literature searches to identify articles on male circumcision and psychological, psychophysiological and psychosocial sequalae in infancy and later in life. The review protocol was registered with PROSPERO (number CRD42021236631).
TABLE 1.
Abbreviations
| Abbreviation | Meaning |
|---|---|
| AAP | American Academy of Pediatrics |
| ASD | Autism spectrum disorder |
| BNAS | Brazelton Neonatal Assessment Scale |
| EMBASE | Excerpta Medica database |
| EMLA | Eutectic mixture of local anesthetics (lidocaine 2.5% and prilocaine 2.5%) |
| IIEF | International Index of Erectile Function |
| NICU | Neonatal intensive care unit |
| NMC | Neonatal male circumcision |
| NSHD | National Survey of Health and Development |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta‐Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| RCT | Randomized controlled trial |
| SIDS | Sudden infant death syndrome |
| SIGN | Scottish Intercollegiate Guidelines Network system |
Figure 1 shows the search strategy performed independently by the first two authors of PubMed, EMBASE, SCOPUS, the Cochrane Library, and Google Scholar through to February 28, 2022. Abstracts were screened for original data on short‐term or long‐term behavioral or other psychological effects. The full text of each potentially suitable article was then reviewed independently by the first two authors to determine whether the article met the inclusion criteria above. By “snowballing,” we searched reference lists and related article links of eligible studies to identify additional studies potentially suitable for inclusion. Our searches also identified critiques of studies and author replies. These were cited in the Discussion section.
FIGURE 1.
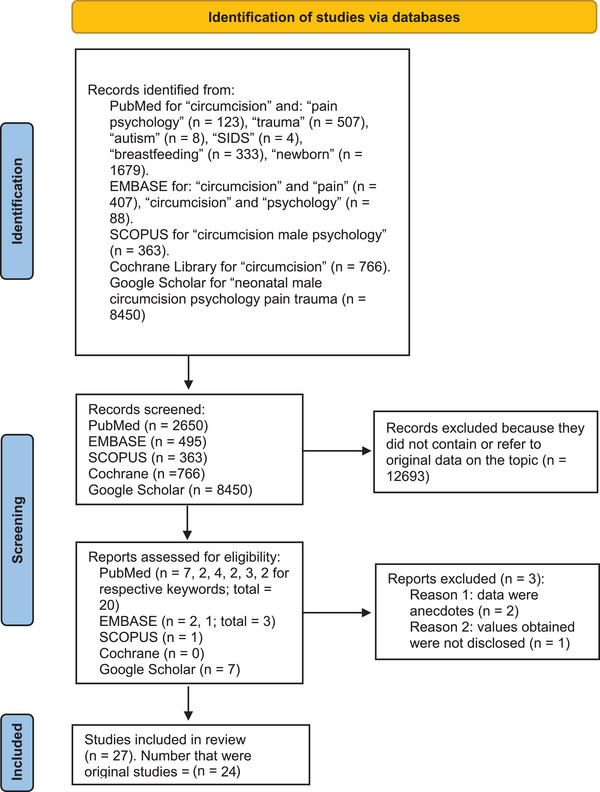
Search strategy diagram as required by PRISMA guidelines. 8 Flowchart shows identification, review, and selection of studies related to possible long‐term psychological effects of NMC
2.2. Quality assessment
Studies were rated using the SIGN system. 9 Only data‐based studies rated Level 2– and above were included.
2.3. Statistical analyses
Interrater reliability of SIGN ratings assigned by the first two authors was determined by the kappa statistic. 10
One of the studies had multiple outcomes 11 and required correction of p values for multiple testing. We performed this using the Holm‐Bonferroni method, 12 an adaptation of the Bonferroni method that controls for the family‐wise error rate (probability that one or more Type I errors will occur) by adjusting the rejection criteria for each individual hypothesis. This simple test has an advantage over the traditional Bonferroni correction, which while reducing the chance of a type I error does so at the expense of a Type II error.
3. RESULTS
3.1. Studies selected
Figure 1 summarizes results of sequential searches in which articles already retrieved were not included again. Keyword combinations and articles meeting the inclusion criteria retrieved by PubMed searches were: “circumcision pain psychology,” 11 , 13 , 14 , 15 , 16 , 17 , 18 “circumcision trauma,” 19 , 20 “circumcision autism,” 21 , 22 , 23 , 24 “circumcision SIDS,” 25 “circumcision breastfeeding,” 26 , 27 , 28 , 29 “circumcision newborn.” 30 , 31 , 32 , 33 , 34 For EMBASE these were “circumcision pain,” 35 , 36 and “circumcision psychology.” 37 A SCOPUS search for “circumcision male psychology” found one further article. 38 The Cochrane Library search did not yield further articles. The Google Scholar search found 6 more articles. 39 , 40 , 41 , 42 , 43 , 44 Snowballing did not identify additional studies. In total, we identified 23 observational studies, 11 , 13 , 14 , 15 , 17 , 18 , 19 , 20 , 21 , 22 , 25 , 26 , 27 , 31 , 32 , 35 , 36 , 37 , 38 , 40 , 44 3 RCTs, 30 , 33 , 43 5 study critiques, 16 , 23 , 34 , 39 , 41 and 2 replies. 24 , 42
Interrater reliability score showed that the scores assigned by the first two authors were at the lower end of the range for “substantial” agreement 10 (κ = 0.812).
3.2. Evaluation of studies for relevance
After closer scrutiny, three studies did not meet the inclusion criteria: two because the data reported were anecdotes 18 , 19 and one because the values obtained were not disclosed. 31 We therefore assigned each of these a Level 3 rating, which led to their exclusion. Participants in the third study 31 were, moreover, recruited via an author‐managed anticircumcision facility, so risking bias, included merged information from women and gay men of their sexual experiences with uncircumcised and neonatally circumcised men, leading the study authors to conclude that much larger representative samples were needed.
Thus 24 studies, comprising 4340 males circumcised early in life and 6908 uncircumcised males, met the inclusion criteria. Table 2 summarizes the studies retrieved, quality rating, country, number of subjects, and key findings, following PRISMA guidelines. 8
TABLE 2.
Quantitative studies retrieved, quality rating, 9 country, n values, and summary of key statistics
| Study | Rating* | Country | Circumcised | Uncirc. | Difference in parameter shown | p or HR |
|---|---|---|---|---|---|---|
| Infant behavioral responses | ||||||
| Marshall et al. 33 | 2+/2+ | USA | 14 NMC day 2 vs. | – | 87% change in behav. category. | <0.0001 |
| 12 NMC at 3 weeks | – | 16% change in behav. category | ||||
| Dixon et al. 13 | 2+/2+ | USA | 15 anesth. | NA | 0.1–0.2× | <0.05 |
| 16 no anesth. | NA | 0.07–0.3× | ||||
| Taddio et al. 14 | 2+/2+ | Canada | 30 NMC | 12 | 0.3–2.8× | 0.01–0.02 |
| Russell and Chaseling 35 | 2+/2– | Australia | 208 anesth. | – | 99% pain‐free | – |
| Taddio et al. 30 | 2++/2++ | Canada | 29 anesth. | 32 | 1.2–1.9× | <0.05 |
| 26 no anesth. | – | 1.6–2.2× | <0.05 | |||
| Breast‐ and bottle‐feeding outcomes | ||||||
| Marshall et al. 33 | 1+/1+ | USA | 27 on day 2 vs. 32 on day 3 | – | ±2%–26% | > 0.5 |
| Fergusson et al. 26 | 2++/2++ | NZ | 124 NMC | 508 | ±1.4%–24% | ≥ 0.3 |
| Gattari et al. 32 | 2+/2+ | USA | 42 NMC pre vs. post | – | ±9%–11% | 0.11–0.22 |
| Mondzelewski et al. 27 | 2+/2++ | USA | 245 at <24 h | 552 at 24–72 h | ±0%–5% | 0.5–0.6 |
| Tan et al. 44 | 2+/2– | USA | 98 NMC | No “n” | 4–6 months: OR 0.38 | 0.016 |
| ≥6 months: OR 0.33 | 0.004 | |||||
| O'Callanan et al. 28 | 2++/2++ | USA | 846 NMC | 263 | 84% vs. 84% | 0.95 |
| Akova and Budagova 29 | 2+/2+ | Turkey | 75 NMC | – | 0.2%–1.3% | 0.18–0.995 |
| Sudden infant death syndrome | ||||||
| Elhaik 25 | 2–/2– | 15 countries | Per 10% increase in circ | – | 0.0001% | 0.01 |
| US states | ±7%–0.7% | 0.008 | ||||
| Autism spectrum disorder | ||||||
| Bauer and Kriebel 22 | 2++/2+ | USA and other | NMC rates per 10% increase | – | 0.002% increase | HR: 1.7–2.3 |
| Frisch and Simonsen 21 | 2–/2– | Denmark | 32 circ'd at <24 months | 1325 | 1.5× | HR: 1.1–3.0 |
| Cognitive ability later in childhood | ||||||
| Fergusson et al. 26 | 2++/2++ | NZ | 124 NMC | 508 | ±0.3%–1% | 0.5–0.9 |
| Satisfaction with circumcision status and body image | ||||||
| Schlossberger et al. 38 | 2+/2+ | USA | 59 NMC | 14 | 23% | <0.001 |
| Bossio et al. 37 | 2+/2+ | Canada | 367 NMC | 290 | ±2%–260% | Not signific |
| Alexithymia | ||||||
| Bollinger and Van Howe 36 | 2–/2– | Any (Internet) | 192 NMC | 64 | 19.9% | 0.0029 |
| Brain structure‐function correlates | ||||||
| Ullman et al. 20 | 2–/2– | Germany | 2 NMC and 7 later circ | 11 | ±0.1–1.9 | 0.36–0.94 |
| Sexual function and pleasure | ||||||
| Payne et al. 15 | 2++/2++ | Canada | 18 NMC | 19 | ±0 | Not signific |
| Bossio et al. 17 | 2+/2+ | Canada | 30 NMC | 32 | ±0 | Not signific |
| Hammond and Carmack 40 | 2–/2– | Any (Internet) | 786 NMC and 222 later circ | – | Nonanalytical | – |
| Socioaffective processing | ||||||
| Miani et al. 11 | 2+/2+ | USA | 408 NMC | 211 | ±2–148% | 0.54‐ <0.001 |
SIGN9 ratings: 1+, well conducted RCTs with a low risk of bias; 2++, high‐quality case‐control or cohort studies with a very low risk of confounding, bias, or chance and a high probability that the relationship is causal; 2+, well‐conducted case‐control or cohort studies with a low risk of confounding, bias, or chance and a moderate probability that the relationship is causal; 2–, case‐control or cohort studies with a high risk of confounding, bias, or chance and a significant risk that the relationship is not causal.
Abbreviations: anesth, anesthesia; behav., behavior; circ, circumcised; HR, hazard ratio; NA, not available; NMC, neonatal males circumcised; signific, significant; uncirc, uncircumcised.
3.3. Infant behavioral responses to neonatal MC pain/anesthesia
Using the BNAS (27 behavioral items), a study of 26 infants randomly assigned to either NMC on day 2 or at 3 weeks without anesthesia found a diversity of responses, indicating differences in coping style. 43 Whereas 90% of the early NMC group changed behavioral categories of average, subdued, or hyperactive for at least 4 h after NMC, and these persisted in one‐third for at least 22 h, such changes were seen in only 16% of the delayed NMC group (p < 0.0001).
A San Diego NMC study utilizing the BNAS found 15 infants given dorsal penile nerve block anesthesia remained more attentive to animate and inanimate stimuli and were more likely to quieten themselves when disturbed, compared with 16 given placebo saline injections. 13 Intergroup comparisons were small but significant (p <0.05). Smoothness and maturity of motor behaviors in the anesthesia group showed the expected rate of improvement and recovery. Behavioral differences were still evident on the day following NMC.
Percentage facial action, percent cry duration, and visual analogue scale pain rating, scored by a research assistant from videotaped recordings, found that after NMC without anesthesia, pain response to routine vaccination at age 4–6 months was higher than in demographically matched uncircumcised boys, suggesting memory of pain affected subsequent pain perception and response to pain. 14 A subsequent double‐blind RCT found significantly lower pain scores at vaccination in uncircumcised boys compared with boys who underwent NMC without anesthetic, whereas an intermediate pain response was found for a group in which topical EMLA anesthetic was applied 60–80 min prior to NMC. 30 Other investigators reported virtual elimination of circumcision pain when EMLA was applied 1 h prior to NMC. 35
3.4. Breast‐ and bottle‐feeding outcomes
A longitudinal study in New Zealand of a birth cohort comprising neonates who underwent NMC and uncircumcised neonates found that, over the course of 4 months, there was no difference between each in initiation of, duration of, or stopping of, breastfeeding. 26 A San Diego study found that timing of NMC did not affect exclusive breastfeeding in the first 2 weeks of life. 27 Bottle‐feeding before and after NMC was also unaffected in a Michigan study. 32 A Connecticut study found no effect of NMC on exclusive breastfeeding or length of hospital stay. 28 A US mid‐west study found no significant difference in mother‐infant interactions for 43 discrete behaviors during 4 hospital feeding sessions comparing neonates randomized to receive NMC without anesthesia on day 2 postbirth and neonates whose NMC was delayed to day 3. 33 A New York study found that, compared with uncircumcised male siblings, infants circumcised within the first 3 days of life breastfed for 4 fewer weeks, and were less likely to breastfeed for 4–6 months (49% vs. 71%, p = 0.016) or for more than 6 months (29% vs. 55%, p = 0.004), leading the authors to suggest that NMC be delayed until breastfeeding is properly established. 44 The New Zealand longitudinal study found no difference in breastfeeding‐associated outcomes, such as being less prone to gastrointestinal problems and asthma. 26 A Turkish study of 75 boys aged 0–4 months found no change in sleep or feeding, but an increase in maternal attachment value after NMC. 29
3.5. Sudden infant death syndrome
Elhaik hypothesized that allostatic load (the wear and tear on the body that accumulates as an individual is exposed to repeated or chronic stress) stemming from pain, stress, or trauma from NMC could be an explanation for SIDS. 25 As support, in 15 intercountry comparisons, he found NMC and prematurity to be associated with SIDS. 25
3.6. Autism spectrum disorder
Analysis of a Danish national medical records databank found 4986 ASD cases among 342,877 boys (4.4% Muslim) aged 0–9 years. 21 Of these, 2903 of probable Muslim background and 444 other Danish boys underwent circumcision. Overall, ASD risk was seen in 32 circumcised boys aged 0–4 years (HR = 1.80; 1.24–2.63) but not in 23 circumcised boys aged 5–9 years (HR = 1.15; 95% CI 0.75–1.77). For boys circumcised before the age of 24 months (n = 32) ASD risk between 0–9 years of age was elevated (HR = 1.41; 95% CI 1.05–1.90), but for boys circumcised at age ≥ 24 months (n = 7) an increased, but nonsignificant, risk was seen (HR = 1.96; 95% CI 0.93–4.14). The authors concluded that “circumcision pain” causes ASD. No overall association was found with hyperkinetic disorder or asthma.
A US study by Bauer and Kriebel used neonatal circumcision of boys as a proxy for examining neonatal acetaminophen (paracetamol) exposure as a risk factor for ASD. 22 A strong correlation was found for 9.16 million boys born after 1995, but not for 9.76 million born before 1995. Since widespread use of acetaminophen to control pain after circumcision occurred in the former age group, coupled with experimental and clinical evidence linking acetaminophen metabolism pathways to ASD etiology, the authors concluded that acetaminophen, not circumcision, may be a cause of ASD. 22
3.7. Cognitive ability later in childhood
The longitudinal birth cohort study in New Zealand examined neonatally circumcised and uncircumcised boys annually from age 1 to age 16 years and at ages 18, 21, and 25 years. 26 NMC had no adverse effect on cognitive ability (IQ at age 8–9 years and scholastic ability at age 13). 26
3.8. Satisfaction with circumcision status and body image
A San Francisco study comparing 9‐ to 11‐year‐old boys circumcised neonatally with uncircumcised boys found the NMC group had higher satisfaction with their circumcision status (p < 0.001), whereas general body image did not differ. 38
A study that included American (44.4%), Canadian (27.5%), European (16.9%), and men from other countries (age 33.0 ± 12.5 SD years; 51.7% heterosexual, 16.6% homosexual, and 31.6% bisexual) found that 64.2% of 366 men circumcised neonatally and 42.5% of 106 circumcised in childhood reported lower happiness with their circumcision status compared with 12.8% of 47 men circumcised as adults and 5.5% of 286 uncircumcised men (p < 0.001). 37 There was no difference in satisfaction with body image, self‐consciousness, and male genital image between the groups. Men unhappy with their circumcision status reported slightly lower sexual functioning assessed by IIEF scores. 37
3.9. Alexithymia
Alexithymia is an idiopathic personality trait characterized by difficulty identifying and describing an individual's own, or other peoples’ emotions, social attachment, and interpersonal relations. Like many personality traits, alexithymia is believed to result from complex interaction between genetics and environment. Bollinger and Van Howe argued that early trauma, such as NMC pain (presumably when performed without anesthesia) affects brain structures leading to alexithymia. 36 Their study of 64 uncircumcised men and 236 circumcised men (192 circumcised in infancy) found a 6.1 point (19.9%) higher alexithymia score in circumcised men (p = 0.0029). 36 A critique of the study 39 and a reply 42 were retrieved in our literature searches and are presented in Section 4.
3.10. Limbic‐hypothalamic‐pituitary‐adrenal axis activity and psychological correlates
Objective and subjective stress and trauma markers were measured in 9 circumcised and 10 uncircumcised Jewish males aged 20–36 years in Dresden, Germany. 20 Circumcision did not alter long‐term limbic‐hypothalamic‐pituitary‐adrenal axis activity, subjective stress perception, anxiety, depressiveness, physical complaints, nor sense of coherence and resilience. Rather, an increase in the glucocorticoid levels indicated to the authors a healthy lifestyle and appropriate functioning. The authors concluded that their findings provide evidence that NMC does not promote psychological trauma. However, only 2 of the 9 circumcised subjects had undergone ritual NMC on day 8, whereas 7 were circumcised later. A much larger study evaluating men circumcised neonatally is required to extend these preliminary findings.
3.11. Sexual function and pleasure
It has been argued that adverse psychological effects from NMC pain reduce sexual function and pleasure. Hammond and Carmack conducted an online survey of 1008 circumcised men (78% circumcised in early infancy; 58% heterosexual) who all believed they had been harmed by their circumcision. 40 The authors pointed out that this was a subset, and that most men did not believe that their infant circumcision had led to long‐term harm. Participants were self‐selected by an advertisement on “foreskin restoration websites, blogs devoted to men's issues, and through genital autonomy‐related social media,” calling for volunteers to participate in a study of “male circumcision trauma.”
Psychological factors influence sexual arousal. When assessed by quantitative genital and nongenital sensory testing using thermal imaging of the penis of healthy age‐matched 18‐ to 45‐year‐old men in Montreal, including circumcised (probably in infancy) and uncircumcised men, there was no difference in IIEF scores or sexual arousal measured by the penile temperature reached during exposure to a 10‐min film involving consenting adults engaged in oral and coital activity. 13 During arousal, baseline penile temperature in uncircumcised men was lower and underwent a greater increase to reach the level achieved more quickly by circumcised men (p < 0.05). 15 A decrease in touch sensitivity was seen in both groups when exposed to the erotic film compared with the control film. Aroused uncircumcised (p < 0.05) and circumcised (p < 0.01) men were more sensitive to touch on their forearm than their penile glans or shaft.
An Ontario study by Bossio et al. compared matched circumcised and uncircumcised Canadian men aged 18–37 years (mean 24.2 ± 5.1 SD). In Canada, most circumcisions are performed neonatally. They found no difference in touch and pain thresholds using quantitative sensory testing, nor warmth and pain thresholds using a thermal analyser. 17 IIEF scores showed no difference in sexual functioning between circumcised and uncircumcised men. The study therefore did not support NMC pain having a long‐term adverse effect on penile sensation. The authors concluded that, “this study challenges past research suggesting that the foreskin is the most sensitive part of the adult penis.” 17
3.12. Socioaffective processing
Miani et al. surveyed socioaffective processing in 408 US men circumcised within one month of birth and 211 uncircumcised men recruited using a neutral platform. 11 They reported that NMC “might” impact socioaffective traits or behavior in adulthood. The study claimed neonatally circumcised men had higher levels of avoidance and anxiety, perceived stress, and emotional instability, but no significant difference in empathy and trust.
The study tested 21 parameters, including 12 with p values < 0.05. It failed to correct for multiple testing. When we performed a Holm‐Bonferroni correction only three p values remained significant (Table 3). The most statistically significant was ∼18% higher sociosexual desire among neonatally circumcised men. Significance also remained for dyadic sexual libido/drive (∼7% higher) and stress (∼14% higher). Miani stated that, “The psychological differences that we found … are not sufficiently severe in themselves to be suggestive of pathology.”
TABLE 3.
| Parameter | p | Corrected p |
|---|---|---|
| Attachment: anxiety | 0.011 | 0.18 (NS) |
| Attachment: avoidance | 0.004 | 0.072 (NS) |
| Personality: openness | 0.660 | 0.66 (NS) |
| Conscientiousness | 0.025 | 0.35 (NS) |
| Extraversion | 0.321 | 1.0 (NS) |
| Agreeableness | 0.010 | 0.17 (NS) |
| Neuroticism | 0.100 | 0.90 (NS) |
| Stability | 0.011 | 0.17 (NS) |
| Plasticity | 0.402 | 1.0 (NS) |
| Empathy: perspective taking | 0.161 | 1.0 (NS) |
| Perspective: empathic concern | 0.275 | 1.0 (NS) |
| Trust: toward institutions | 0.222 | 1.0 (NS) |
| Trust: toward known people | 0.256 | 1.0 (NS) |
| Trust: toward strangers | 0.536 | 1.0 (NS) |
| Sociosexuality: behavior | 0.026 | 0.34 (NS) |
| Sociosexuality: attitude | 0.049 | 0.49 (NS) |
| Sociosexuality: desire | <0.0001 | 0.0019* |
| Sexual libido: solitary | 0.038 | 0.46 (NS) |
| Sexual libido: dyadic | 0.001 | 0.020* |
| Stress | 0.001 | 0.019* |
| Sensation seeking | 0.044 | 0.48 (NS) |
Statistically significant after Holm‐Bonferroni correction by the formula p(i) ≥ α /(K–i + 1), where K = number of p values.
Abbreviation: NS, not significant.
4. DISCUSSION
This systematic review presents the existing evidence concerning whether or not early MC has potential short‐term or long‐term psychological harm. The review includes whether or not there are effects on pain response in infancy, breast‐feeding outcomes, SIDS, autism spectrum disorder, cognitive abilities later in childhood, body image, alexithymia, psychological response to stress, sexual satisfaction, and socioaffective processing. We will now present a critical evaluation of the key findings for each of these before reaching a conclusion.
4.1. Pain
The finding that NMC using local anesthesia ameliorated the later pain response to needle vaccination provided evidence that infants remember pain. Taddio et al. therefore recommended that local anesthetic be used to reduce NMC pain. 30 , 45 Such advice was incorporated into the AAP 1999 infant male circumcision policy. 7 Hypothetically, we posit that a study in which the sequence of NMC and vaccination was reversed might show a similar pain score result as NMC first and vaccination second. We also wonder whether greater response to later pain might be a feature of the learning process of the child? It is well appreciated that during the parturition process the mother experiences pain. But not often mentioned is that mechanical pressure on the neonate during its passage through the vaginal canal during birth might cause the neonate to experience pain as well. Theoretically, resilience mechanisms should apply to each party during parturition. Newborns delivered vaginally show higher pain expression than those delivered by cesarean section. 46 It would therefore be interesting to repeat the studies by Taddio et al. on infants delivered by cesarean section.
4.2. Breast‐ and bottle‐feeding outcomes
Among the seven studies identified there was little support for the argument that NMC disrupts breastfeeding. Nor were bottle‐feeding outcomes disrupted. Only one study found a difference, namely that in a cohort of infants circumcised within the first 3 days after birth, the number of months of breastfeeding was significantly less than for uncircumcised neonates. 44
4.3. Sudden infant death syndrome
In the SIDS study, SIDS prevalence was as high in countries with low NMC prevalence (e.g., NZ, 0.80/1000) as in countries with high NMC prevalence (USA, 0.81/1000). Compared to countries with low SIDS prevalence (0–0.2/1000), SIDS prevalence was 0.30/1000 in low NMC prevalence Norway. NMC prevalence was assumed to be 100% in Muslims. However, many Islamic circumcisions occur well past the age when SIDS occurs. 47 , 48 Local anesthesia during NMC was not considered. Nor was the fact that NMC takes a few minutes 49 rather than Elhaik's assumption of half an hour of procedural stress, as applies to older children and men. Differences were found in SIDS prevalence between US states according to percentage of non‐Hispanic white (high NMC prevalence) and Hispanic white (lower NMC prevalence) ethnicities. The potential impact of socioeconomic differences was not considered. The association reported in Elhaik's study does not prove causation. 41 Multiple factors have contributed to reduced SIDS deaths in recent decades. 50 Sleeping position is important. Advice in Western countries from the mid‐to‐late 20th century to place babies in the prone position greatly increases risk of SIDS. 51 Given that cultural factors influence the position in which babies are put to sleep, 51 the effects in Elhaik's cross‐cultural study 25 could have been caused by sleeping position.
4.4. Autism spectrum disorder
In the autism study, criticisms 16 , 34 mentioned that overall statistical significance was marginal (hazard ratio 1.46; 95% CI 1.11–2.96). In response, Frisch and Simonsen acknowledged that their study had limited statistical power. 24 We calculated that ASD in their general population was 4986/342,877×100 = 1.45%. In the circumcised group we calculated ASD prevalence to be 55/(2903 + 444) × 100 = 1.64%. The difference between these figures is 13% rather than the 46%–62% claimed. Critics pointed out that only 11% of Muslim boys in the study were recorded as being circumcised, that a significant association with ASD diagnosis was found in boys under the age of 4 years, but association was not significant in boys aged 5–9 years, which was relevant to alternative explanations. 16 Medications for post‐NMC analgesia, specifically acetaminophen, found in 1994 to be effective for managing post‐NMC pain, 52 led the AAP to recommend acetaminophen in 1999. 7 Supporting acetaminophen rather than NMC being responsible for ASD, Bauer and Kriebel found the association of NMC with ASD was “considerably weaker” prior to 1995. 22 Acetaminophen breakdown by sulfation is the primary metabolic route in children, and is very much lower in neonates, and even more so in ASD. 22 Bauer criticized the Danish ASD study for falsely suggesting that her group's findings applied to NMC. 53 And she explained why older boys in the Danish study (born before the 1999 guidelines 7 ) showed only a weak association of circumcision with ASD, whereas those born after 1999 showed a stronger association, 16 , 53 thus supporting the acetaminophen hypothesis.
Another Danish study found an astonishingly high ASD prevalence (7.2%) in uncircumcised boys, 34 leading the authors to suggest that the 1.5% figure reported for Danish boys aged 0–9 years (98.9% uncircumcised) in Frisch and Simonsen's ASD study 21 indicated confounding. Other ASD prevalence estimates for Denmark were 0.69% in male children overall 54 and 1.65% in 10‐year‐old boys. 55
Critics recommended conducting a study to examine ASD in uncircumcised infant males who had experienced painful cystitis, which is caused by urinary tract infections (10‐times more common in uncircumcised male infants). 16 One critic suggested that Frisch and Simonsen's study involved only those assessed for ASD, not those who remained undiagnosed, and that parents who are more aware of ASD symptoms are more “likely to present their children for early assessment.” 23 Ava Neyer stated that the study was flawed, that even if pain perception in autistic children is higher than neurotypical children, it would be quite a stretch to speculate that lifelong deficits in stress response show that early pain causes autism. 56 Rather than deficits in their stress response she suggested that autistic children may find the world more inherently stressful because of other mechanisms. She also suggested that the huge differences in cultural background between circumcised and uncircumcised boys in the study may mean that cultural differences contributed to the findings. She questioned why circumcision might be a risk factor for only classic autism, and emphasized the need for a confirmatory study, something that has not happened in the six years since the study was published. Carsten Obel, who studies children's mental disorders at Aarhus University, Denmark, was similarly skeptical, suggesting that rather than circumcision there could easily be another explanation, such as cultural or other differences between parents who want their boy circumcised and those who don't. 57
A survey evaluating a comprehensive array of emotional problems in 19,850 preschool children in 24 societies 58 and in 6470 children aged 6–16 years in 31 societies 59 found severity of such problems between different countries varied, and was independent of circumcision prevalence estimates. 60 It was mentioned in the Discussion section of a 1978 study of circumcision and tonsillectomy rates by Calnan et al. 61 that the 1946 UK National Survey of Health and Development birth cohort showed no difference in developmental and behavioral indices between circumcised and uncircumcised boys.
4.5. Cognitive ability later in childhood
Although we found only one study, this was rated high quality as it involved long‐term follow‐up of a birth cohort with periodic assessments at ages 1–25 years. 26 None of the parameters tested differed between circumcised and uncircumcised boys.
4.6. Satisfaction with circumcision status and body image
Higher satisfaction with MC status was observed among neonatally circumcised prepubescent boys compared with uncircumcised boys 26 The authors of this US study speculated that this could have stemmed from a perception among the uncircumcised boys that their penile appearance differed from the majority of their peers. Among men, studies have generally found most were satisfied with their MC status. 37 It was suggested that the minority having negative attitudes were men circumcised early in life, meaning that they had had no say in the matter. Since this attitude fits with the narrative of anticircumcision activists that MC be delayed until the male can decide for himself whether or not to be circumcised, the dissatisfaction felt could stem from exposure to social media where such arguments are prominent (see Subsection 4.11). However, rather than MC status, size of the penis has generally been found to be a much more important factor for satisfaction.
4.7. Alexithymia
The US alexithymia study was criticized because subjects were recruited by advertisements with the title “Male Circumcision trauma survey,” placed on anti‐MC websites, making this self‐selected sample of men likely to hold anti‐MC views unrepresentative of the general population. Critics noticed that the overall prevalence of alexithymia in the cohort (30% in circumcised and 15% in uncircumcised men) was over 3 times higher than the <10% prevalence in the general population, 39 although in Finland, where circumcision is uncommon, alexithymia was found in 17% of men. 62 The Bollinger and Van Howe study stated “age at time of circumcision was not a factor,” so it is likely that circumcision trauma at any age, not just in the neonatal period, would have to be invoked in alexithymia etiology. The authors conceded that circumcision pain itself did not seem to affect alexithymia acquisition, that potential selection bias was a primary weakness, and that the findings were preliminary, requiring replication. 42 Psychiatric problems were reported to be more common in men unhappy at having been circumcised. 63 Body dysmorphic disorder has been linked to alexithymia. 64 Bollinger and Van Howe cited an article stating that there is, “strong empirical support for alexithymia being a stable personality trait rather than just a consequence of psychological distress.” 65 They cited intercountry comparisons of MC and alexithymia prevalence to support their arguments, but such comparisons are strongly prone to confounding. 42 Large surveys of an extensive array of emotional problems across dozens of countries 58 , 59 found no apparent association of these with estimated MC prevalence in each country. 60 While some, but not all, 66 studies found that men exhibit higher alexithymia scores than women, sex differences did not correlate with published estimates of MC prevalence in the countries studied.
4.8. Limbic‐hypothalamic‐pituitary‐adrenal axis activity and psychological correlates
There was only one study of brain and psychological parameters comparing circumcised and uncircumcised males. 20 Although no change was found in long‐term limbic‐hypothalamic‐pituitary‐adrenal axis activity, subjective stress perception, anxiety, depressiveness, physical complaints, sense of coherence and resilience, only 2 of the 9 circumcised subjects had undergone ritual NMC on day 8, whereas 7 were circumcised later. All were Jewish. A much larger study evaluating men circumcised neonatally is required to extend these preliminary findings.
4.9. Sexual function and pleasure
A recent systematic review of all studies found that in high‐quality studies circumcision at any age did not adversely affect sexual function and pleasure, whereas studies supporting an adverse effect were rated as low quality. 67 No differences in sexual function, 68 , 69 , 70 , 71 sensation and sexual pleasure 69 were found in earlier systematic reviews and in meta‐analyses of circumcision and sexual function. 69 , 71 The most recent meta‐analysis of all data, including from studies of men circumcised neonatally, found that circumcised men had on average 28% lower ejaculatory latency time (p < 0.00001), 58% lower erectile dysfunction (p < 0.006), and 64% less pain during sexual intercourse (p = 0.007). 71 Psychological factors might influence some of these parameters. However, the findings argue against a role for NMC pain contributing to later sexual problems. By contrast, higher‐quality studies found no adverse effects of circumcision (including NMC) on sexual function, sensation, or pleasure.
4.10. Socioaffective processing
In the survey by Miani et al., 11 the authors stated that they expected empathy to be lower in the NMC group because painful NICU procedures were found to be associated with reduced subcortical gray matter and reduced white matter in frontal and parietal regions, 72 , 73 structures associated with empathic processing. 74 , 75 But their study found no difference in empathy. Since alexithymia is linked to empathy, 76 the finding also undermines Bollinger and Van Howe's claim that NMC is a cause of alexithymia. 36 Miani et al. interpreted elevation in desire and libido, as well as perceived stress, in men circumcised neonatally in a negative light. But in a study mentioned earlier, quantitative genital and nongenital sensory testing found no difference in erectile responses between circumcised and uncircumcised men. 15 Further, the studies discussed above showed that circumcised men experience similar or greater sexual pleasure and are less likely to suffer sexual dysfunction. Phimosis in uncircumcised adolescent and young adult males 77 , 78 , 79 , 80 can impede sexual activity, with adverse effects on mental health. 81 Circumcised males have reduced risk of candidiasis. 82 , 83 Candida albicans antibodies are elevated in schizophrenia independent of potential confounders, 84 so it would be interesting to compare schizophrenia prevalence between circumcised and uncircumcised men.
Contrary to Miani et al.’s interpretation, their data suggest that psychological effects of sexual problems in uncircumcised men might explain why desire and libido was lower than in circumcised men (reverse causation). Recent systematic reviews found an overall preference by women for the circumcised penis because of esthetics, hygiene, fellatio, ease of vaginal penetration, less frequent dyspareunia, and reduced risk of infection. 85 , 86 Men in Miani et al.’s study were American. A 1988 survey of mid‐western American women found a strong (71%–83%) preference for circumcised penises for sexual intercourse, visual erotic appeal, giving manual penis stimulation, and fellatio, even in women who had only ever had sexual experience with uncircumcised men. 87 Could women's preferences explain why Miani et al. found (nonsignificantly) more circumcised men were in sexual relationships?
Circumcised men in Miani et al.’s study were older than uncircumcised men (36.0 vs. 32.8 years; p < 0.001). Since stress increases with age it was included as a covariate. The German study by Ullmann et al. found no differences in stress perception, anxiety, and depression between circumcised and uncircumcised men. 20 Since Miani et al. found no association of NMC with empathy, NMC pain does not appear likely to affect the brain structures responsible.
Like many of the studies in our review, Miani et al.’s results were based on participant self‐reports, which the authors conceded could lead to social desirability bias that, “might have hindered participants from answering honestly.” Moreover, circumcision status was self‐identified, which the authors conceded can be unreliable. In support, they cited a study of adolescent boys in Texas in which 7% of those who were ascertained as circumcised by physical examination thought that they were uncircumcised, and 23% did not know their status. 88
Miani et al. did not explore the possible effect of NMC procedural pain relief on adult behaviors and traits. This was a major weakness, given that the average age of the circumcised participants was 36 years, implying that participants underwent NMC during the 1970s and 1980s. A 1998 study found that just 45% of responding physicians provided pain relief for NMC at that time. 89 A large, but unknown, proportion of the circumcised participants in Miani et al. probably underwent NMC without anesthesia, whereas nowadays anesthesia is recommended for all circumcisions. 7 , 90 Similarly, we do not know how many men were circumcised in the first few days after birth, when pain is much less than for MC at ≥ 4 weeks of age. 5
As a limitation, Miani et al. stated that, “MTurk [Amazon Mechanical Turk] populations, like ours, when compared to the US population as a whole, tend to be younger and more educated, but reported lower incomes and higher unemployment.”
4.11. Societal influences
Societal influences on psychological outcomes of NMC should be considered. Messages by anti‐NMC lobby groups telling men that their NMC damaged them sexually dominate Internet searches using “circumcision” as a keyword, as well being prominent on social media. 91 Men with sexual problems too embarrassed to consult medical practitioners for advice and effective treatment may succumb to the false narratives of websites informing them that NMC caused their problems. 41 A recurring theme is that they were content with their MC status until they read about MC, whereupon they became distressed. 92 Thus, men with normal sexual function who believe the fallacies may think that their sex life has been diminished by their NMC, causing anxiety and resentment of their parents’ decision to have them circumcised. 93 Over 40 studies have shown consistently that the more well‐informed men are about MC the more positive they are about it. 94 We contend that it is misinformation that breeds negative psychological consequences, not MC itself.
A 2012 systematic review found a strong correlation between depression and sexual dysfunction. 95 The distress may extend to other aspects of mental health. 41 Such falsehoods may cause distress in vulnerable men, especially those with sexual problems, influencing data collected in studies such as the one by Miani et al. 11 Similarly, critics of Hammond and Carmack's study 40 suggested that the pervasive nature of online anticircumcision propaganda might sow false beliefs in gullible or vulnerable men, so explaining the survey results. 41 Hammond and Carmack study 40 was found to have a one‐sided design and the findings were deemed unreliable. 41
4.12. Limitations
Limitations of our systematic review include the fact that the available data are almost all cross‐sectional or case‐control rather than longitudinal. Since most studies involve low numbers of subjects, they lack sufficient power to generate reliable results. All available studies involved western cultures. In most, circumcision was neonatal. For each topic there were few studies and within a topic if there were multiple papers the study design varied. Together, this precluded us from performing meta‐analyses. Many of the survey studies had serious flaws in design and some were prone to bias because recruitment strategies likely resulted in overrepresentation of participants with particular views. For example, in a Facebook post of January 7, 2014, an anticircumcision group (The Whole Network) encouraged its followers to participate in the survey by Bossio et al., 37 thereby biasing the sample. Bossio et al. suggested that lower happiness among a subgroup of men who were circumcised neonatally could be attributed to their lack of choice in the decision. They also suggested that psychological interventions targeting men who have negative attitudes toward their genitals may prove helpful. The authors recognized that their sample likely overrepresented men with polarized attitudes toward circumcision, as they were probably more motivated to complete the lengthy online survey than men with neutral or less negative attitudes. 37
Overrepresentation of men who have sex with men was evident in some surveys. 37 , 40 , 96 , 97 Most studies we identified for inclusion examined data for men who engaged in sexual activity with women. Thus, studies recruiting men who have sex with men are needed. We are aware of only one study that recruited only men (and women) who were currently in a sexual relationship with a man (average 4.2 ± 5.2 SD years; range 3 months to 35.3 years). 96 The men, in contrast to the women, reported higher levels of satisfaction with uncircumcised male partners. Given that there were only 28 men in the study (46% born in Canada, 36% born in the United States, and the rest elsewhere), the authors suggested that the findings should be regarded as preliminary, and required replication using a larger sample. Recruitment involved print advertisements placed on the campus of Queen's University, Ontario, but also on social media, so risking overrepresentation of anti‐NMC activists. Additional research employing stronger study designs, larger numbers of participants, and longer follow‐up is indicated.
4.13. Conclusion
Our critical evaluation of published evidence finds no convincing support for NMC having any substantial adverse effect on psychological outcomes. The findings should help practitioners in counseling parents considering circumcision for a child, and men who may wonder if their NMC has caused them psychological harm.
CONFLICT OF INTEREST
BM and GC are members of the Circumcision Academy of Australia, a not‐for‐profit, government registered, medical association that provides evidence‐based information on male circumcision to parents, practitioners and others, as well as contact details of doctors who perform the procedure. SM is an editor of, and contributor to, http://www.circfacts.org, a website that provides evidence‐based information on male circumcision. SB is a clinical psychologist in a group private practice mental health clinic and wishes to point out that the views expressed in this article do not necessarily reflect those of Cornerstone Therapy & Recovery Center where he works. JK is coinventor of a circumcision device patented by University of Washington. The authors have no financial, religious, or other affiliations that might influence the topic of male circumcision.
Supporting information
Supporting Information
ACKNOWLEDGMENTS
The authors acknowledge the technical assistance of Jim Matthews, MStat of the Sydney Informatics Hub, a Core Research Facility of the University of Sydney.
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Morris BJ, Moreton S, Bailis SA, Cox G, Krieger JN. Critical evaluation of contrasting evidence on whether male circumcision has adverse psychological effects: A systematic review. J Evid Based Med. 2022;15:123–135. 10.1111/jebm.12482
REFERENCES
- 1. van den Hoogen NJV, Patijn J, Tibboel D, Joosten EA. Neonatal plasticity of the nociceptive system: mechanisms, effects, and treatment of repetitive painful procedures during NICU admittance. Curr Pharm Des. 2017;23:5902‐5910. [DOI] [PubMed] [Google Scholar]
- 2. Goksan S, Hartley C, Emery F, et al. fMRI reveals neural activity overlap between adult and infant pain. Elife. 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Warnock F, Sandrin D. Comprehensive description of newborn distress behavior in response to acute pain (newborn male circumcision). Pain. 2004;107:242‐255. [DOI] [PubMed] [Google Scholar]
- 4. Jacobson DL, Balmert LC, Holl JL, Rosoklija I, Davis MM, Johnson EK. Nationwide circumcision trends: 2003 to 2016. J Urol. 2021;205:257‐263. [DOI] [PubMed] [Google Scholar]
- 5. Banieghbal B. Optimal time for neonatal circumcision: an observation‐based study. J Pediatr Urol. 2009;5:359‐362. [DOI] [PubMed] [Google Scholar]
- 6. Sinkey RG, Eschenbacher MA, Walsh PM, et al. The GoMo study: a randomized clinical trial assessing neonatal pain with Gomco vs Mogen clamp circumcision. Am J Obstet Gynecol. 2015;212:664. e661‐668. [DOI] [PubMed] [Google Scholar]
- 7. American Academy of Pediatrics . Task Force on Circumcision. Circumcision policy statement. Pediatrics. 1999;103:686‐693. [PubMed] [Google Scholar]
- 8. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334‐336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276‐282. [PMC free article] [PubMed] [Google Scholar]
- 11. Miani A, Di Bernardo GA, Højgaard AD, et al. Neonatal male circumcision is associated with altered adult socio‐affective processing. Heliyon. 2020;6:e05566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65‐70. [Google Scholar]
- 13. Dixon S, Snyder J, Holve R, Bromberger P. Behavioral effects of circumcision with and without anesthesia. J Dev Behav Pediatr. 1984;5:246‐250. [PubMed] [Google Scholar]
- 14. Taddio A, Goldbach M, Ipp M, Stevens B, Koren G. Effect of neonatal circumcision on pain responses during vaccination in boys. Lancet. 1995;345:291‐292. [DOI] [PubMed] [Google Scholar]
- 15. Payne K, Thaler L, Kukkonen T, Carrier S, Binik Y. Sensation and sexual arousal in circumcised and uncircumcised men. J Sex Med. 2007;4:667‐674. [DOI] [PubMed] [Google Scholar]
- 16. Morris BJ, Wiswell TE. ‘Circumcision pain’ unlikely to cause autism. J R Soc Med. 2015;108:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bossio JA, Pukall CF, Steele SS. Examining penile sensitivity in neonatally circumcised and intact men using quantitative sensory testing. J Urol. 2016;195:1848‐1853. [DOI] [PubMed] [Google Scholar]
- 18. Goldman R. The psychological impact of circumcision. BJU Int. 1999;83(Suppl 1):93‐102. [DOI] [PubMed] [Google Scholar]
- 19. Boyle GJ, Goldman R, Svoboda JS, Fernandez E. Male circumcision: pain, trauma and psychosexual sequelae. J Health Psychol. 2002;7:329‐343. [DOI] [PubMed] [Google Scholar]
- 20. Ullmann E, Licinio J, Barthel A, et al. Circumcision does not alter long‐term glucocorticoids accumulation or psychological effects associated with trauma‐ and stressor‐related disorders. Transl Psychiat. 2017;7:e1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Frisch M, Simonsen J. Ritual circumcision and risk of autism spectrum disorder in 0‐ to 9‐year‐old boys: national cohort study in Denmark. J R Soc Med. 2015;108:266‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bauer AZ, Kriebel D. Prenatal and perinatal analgesic exposure and autism: an ecological link. Environ Health. 2013;12:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Anonymous . Circumcision and autism. Arch Dis Child. 2015;100:369. [DOI] [PubMed] [Google Scholar]
- 24. Frisch M, Simonsen J. Circumcision‐autism link needs thorough evaluation: response to Morris and Wiswell. J R Soc Med. 2015;108:297‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Elhaik E. Neonatal circumcision and prematurity are associated with sudden infant death syndrome (SIDS). J Clin Transl Res. 2019;4:136‐151. [PMC free article] [PubMed] [Google Scholar]
- 26. Fergusson DM, Boden JM, Horwood LJ. Neonatal circumcision: effects on breastfeeding and outcomes associated with breastfeeding. J Paediatr Child Health. 2008;44:44‐49. [DOI] [PubMed] [Google Scholar]
- 27. Mondzelewski L, Gahagan S, Johnson C, Madanat H, Rhee K. Timing of circumcision and breastfeeding initiation among newborn boys. Hosp Pediatr. 2016;6:653‐658. [DOI] [PubMed] [Google Scholar]
- 28. O'Callahan C, Te S, Husain A, Rosener SE, Hussain N. The effect of circumcision on exclusive breastfeeding, phototherapy, and hospital length of stay in term breastfed newborns. Hosp Pediatr. 2020;10:516‐522. [DOI] [PubMed] [Google Scholar]
- 29. Akova F, Budagowa G. How does circumcision performed under regional anesthesia affect sleep, feeding, and maternal attachment in babies aged 0–4 months? J Pediatr Surg. 2022:Epub ahead of print 7 January 2022. [DOI] [PubMed] [Google Scholar]
- 30. Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1997;349:599‐603. [DOI] [PubMed] [Google Scholar]
- 31. Boyle GJ, Bensley GA. Adverse sexual and psychological effects of male infant circumcision. Psychol Rep. 2001;88:1105‐1106. [DOI] [PubMed] [Google Scholar]
- 32. Gattari TB, Bedway AR, Drongowski R, Wright K, Keefer P, Mychaliska KP. Neonatal circumcision: is feeding behavior altered? Hosp Pediatr. 2013;3:362‐365. [DOI] [PubMed] [Google Scholar]
- 33. Marshall RE, Porter FL, Rogers AG, Moore J, Anderson B, Boxerman SB. Circumcision: II. Effects upon mother‐infant interaction. Early Hum Dev. 1982;7:367‐374. [DOI] [PubMed] [Google Scholar]
- 34. Sneppen I, Thorup J. Foreskin morbidity in uncircumcised males. Pediatrics. 2016;137:e20154340. [DOI] [PubMed] [Google Scholar]
- 35. Russell CT, Chaseling J. Topical anaesthesia in neonatal circumcision: a study of 208 consecutive cases. Aust Fam Physician. 1996;25:S30‐34. [PubMed] [Google Scholar]
- 36. Bollinger D, Van Howe RS. Alexithymia and circumcision trauma: a preliminary investigation. Int J Men's Health. 2011;10:184‐195. [Google Scholar]
- 37. Bossio JA, Pukall CF. Attitude toward one's circumcision status is more important than actual circumcision status for men's body image and sexual functioning. Arch Sex Behav. 2018;47:771‐781. [DOI] [PubMed] [Google Scholar]
- 38. Schlossberger NM, Turner RA, Irwin CE, Jr. Early adolescent knowledge and attitudes about circumcision —methods and implications for research. J Adolesc Health. 1992;13:293‐297. [DOI] [PubMed] [Google Scholar]
- 39. Morris BJ, Waskett JH. Claims that circumcision increases alexithymia and erectile dysfunction are unfounded: A critique of Bollinger and Van Howe's “Alexithymia and circumcision trauma: a preliminary investigation.” Int J Men's Health. 2012;11:177‐181. [Google Scholar]
- 40. Hammond T, Carmack A. Long‐term adverse outcomes from neonatal circumcision reported in a survey of 1,008 men: an overview of health and human rights implications. Int J Hum Rights. 2017;21:189‐218. [Google Scholar]
- 41. Bailis SA, Moreton S, Morris BJ. Critical evaluation of a survey claiming “Long‐term adverse outcomes from neonatal circumcision.” Adv Sex Med. 2019;9:67‐109. [Google Scholar]
- 42. Bollinger D, Van Howe R. Preliminary results are preliminary, not “unfounded”: reply to Morris and Waskett. Int J Men's Health. 2012;11:181‐184. [Google Scholar]
- 43. Marshall RE, Stratton WC, Moore JA, Boxerman SB. Circumcision I: effects on newborn behavior. Infant Behav Dev. 1980;3:1‐14. [Google Scholar]
- 44. Tan AG, Noble L, Jain S, Shajan A, Craik D. The effect of early circumcision on breastfeeding duration using sibling comparisons. Pediatrics. 2019;144:273 [Google Scholar]
- 45. Taddio A, Stevens B, Craig K, et al. Efficacy and safety of lidocaine‐prilocaine cream for pain during circumcision. N Engl J Med. 1997;336:1197‐1201. [DOI] [PubMed] [Google Scholar]
- 46. Schuller C, Känel N, Müller O, et al. Stress and pain response of neonates after spontaneous birth and vacuum‐assisted and cesarean delivery. Am J Obstet Gynecol. 2012;207:416. e411‐416. [DOI] [PubMed] [Google Scholar]
- 47. Anwer AW, Samad L, Iftikhar S, Baig‐Ansari N. Reported male circumcision practices in a Muslim‐majority setting. Biomed Res Int. 2017;2017:4957348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sahin F, Beyazova U, Akturk A. Attitudes and practices regarding circumcision in Turkey. Child Care Health Dev. 2003;29:275‐280. [DOI] [PubMed] [Google Scholar]
- 49. Morris BJ, Waskett JH, Banerjee J, et al. A ‘snip’ in time: what is the best age to circumcise? BMC Pediatr. 2012;12:article 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Goldstein RD, Trachtenberg FL, Sens MA, Harty BJ, Kinney HC. Overall postneonatal mortality and rates of SIDS. Pediatrics. 2016;137. [DOI] [PubMed] [Google Scholar]
- 51. Sperhake J, Jorch G, Bajanowski T. The prone sleeping position and SIDS. Historical aspects and possible pathomechanisms. Int J Legal Med. 2018;132:181‐185. [DOI] [PubMed] [Google Scholar]
- 52. Howard CR, Howard FM, Weitzman ML. Acetaminophen analgesia in neonatal circumcision: the effect on pain. Pediatrics. 1994;93:641‐646. [PubMed] [Google Scholar]
- 53. Bauer AZ. PubMed Commons, comment. 2015. http://www.ncbi.nlm.nih.gov/pubmed/25573114 (accessed 14 February 2021)
- 54. Parner ET, Thorsen P, Dixon G, et al. A comparison of autism prevalence trends in Denmark and Western Australia. J Autism Dev Disord. 2011;41:1601‐1608. [DOI] [PubMed] [Google Scholar]
- 55. Schendel DE, Thorsteinsson E. Cumulative incidence of autism Into adulthood for birth cohorts in Denmark, 1980–2012. JAMA. 2018;320:1811‐1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Neyer A. The problem with articles on autism risks and how to evaluate studies. Or why circumcision is unlikely to increase rates of autism. The Chimerical Capuchin. 2015. https://chimericalcapuchin.wordpress.com/2015/01/10/the‐problem‐with‐articles‐on‐autism‐risks‐and‐how‐to‐evaluate‐studies/ (accessed 14 February 2021) [Google Scholar]
- 57. Sjøgren K. [Researchers find link between autism and circumcision]. (in Danish). Videnskab.dk [science.dk]. 2015. https://videnskab.dk/krop‐sundhed/forskere‐finder‐sammenhaeng‐mellem‐autisme‐og‐omskaering (accessed 14 February 2021)
- 58. Rescorla LA, Achenbach TM, Ivanova MY, et al. International comparisons of behavioral and emotional problems in preschool children: parents' reports from 24 societies. J Clin Child Adolesc Psychol. 2011;40:456‐467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rescorla L, Achenbach TM, Ivanova MY, et al. Behavioral and emotional problems reported by parents of children ages 6 to 16 in 31 societies. J Emotional Behav Disorders. 2007;15:130‐142. [Google Scholar]
- 60. Morris BJ, Wamai RG, Henebeng EB, et al. Estimation of country‐specific and global prevalence of male circumcision. Popul Health Metr. 2016;14:article 4 (13 pages). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Calnan M, Douglas JWB, Goldstein H. Tonsillectomy and circumcision: comparison of two cohorts. Int J Epidemiol. 1978;7:79‐85. [DOI] [PubMed] [Google Scholar]
- 62. Salminen JK, Saarijärvi S, Aärelä E, Toikka T, Kauhanen J. Prevalence of alexithymia and its association with sociodemographic variables in the general population of Finland. J Psychosom Res. 1999;46:75‐82. [DOI] [PubMed] [Google Scholar]
- 63. Mohl PC, Adams R, Greer DM, Sheley KA. Prepuce restoration seekers: psychiatric aspects. Arch Sex Behav. 1981;10:383‐393. [DOI] [PubMed] [Google Scholar]
- 64. Fenwick AS, Sullivan KA. Potential link between body dysmorphic disorder symptoms and alexithymia in an eating‐disordered treatment‐seeking sample. Psychiat Res. 2011;189:299‐304. [DOI] [PubMed] [Google Scholar]
- 65. Taylor GJ, Bagby RM, Parker JDA. Disorders of Affect Regulation: Alexithymia in Medical and Psychiatric Illness. Cambridge, UK: Cambridge University Press; 1997. [Google Scholar]
- 66. Mason O, Tyson M, Jones C, Potts S. Alexithymia: its prevalence and correlates in a British undergraduate sample. Psychol Psychother. 2005;78:113‐125. [DOI] [PubMed] [Google Scholar]
- 67. Morris BJ, Krieger JN. The contrasting evidence concerning the effect of male circumcision on sexual function, sensation, and pleasure: a systematic review. Sex Med. 2020;8:577‐598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction? A systematic review. J Sex Med. 2013;10:2644‐2657. [DOI] [PubMed] [Google Scholar]
- 69. Tian Y, Liu W, Wang JZ, Wazir R, Yue X, Wang KJ. Effects of circumcision on male sexual functions: a systematic review and meta‐analysis. Asian J Androl. 2013;15:662‐666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shabanzadeh DM, Düring S, Frimont‐Moller C. Male circumcision does not result in inferior perceived male sexual function—a systematic review. Dan Med J. 2016;63:A5245. [PubMed] [Google Scholar]
- 71. Yang Y, Wang X, Bai Y, Han P. Circumcision does not have effect on premature ejaculation: a systematic review and meta‐analysis. Andrologia. 2018;50:e12851. [DOI] [PubMed] [Google Scholar]
- 72. Brummelte S, Grunau RE, Chau V, et al. Procedural pain and brain development in premature newborns. Ann Neurol. 2012;71:385‐396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Smith GC, Gutovich J, Smyser C, et al. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann Neurol. 2011;70:541‐549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Bernhardt BC, Singer T. The neural basis of empathy. Annu Rev Neurosci. 2012;35:1‐23. [DOI] [PubMed] [Google Scholar]
- 75. Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3:71‐100. [DOI] [PubMed] [Google Scholar]
- 76. Banzhaf C, Hoffmann F, Kanske P, et al. Interacting and dissociable effects of alexithymia and depression on empathy. Psychiatry Res. 2018;270:631‐638. [DOI] [PubMed] [Google Scholar]
- 77. Gairdner D. The fate of the foreskin, a study of circumcision. Br Med J. 1949;2:1433‐1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Osmond TE. Is routine circumcision advisable? J Roy Army Med Corp. 1953;99:254. [PubMed] [Google Scholar]
- 79. Morris BJ, Matthews JG, Krieger JN. Prevalence of phimosis in males of all ages: systematic review. Urology. 2020;135:124‐132. [DOI] [PubMed] [Google Scholar]
- 80. Mao LM, Templeton DJ, Crawford J, et al. Does circumcision make a difference to the sexual experience of gay men? Findings from the Health in Men (HIM) Cohort. J Sex Med. 2008;5:2557‐2561. [DOI] [PubMed] [Google Scholar]
- 81. Yang L, Ruan LM, Yan ZJ, Cheng Y, Wang GY, Ji YX. Sexual function and mental state in patients with redundant prepuce or phimosis. Zhonghua Nan Ke Xue. 2010;16:1095‐1097. [PubMed] [Google Scholar]
- 82. Ferris JA, Richters J, Pitts MK, et al. Circumcision in Australia: further evidence on its effects on sexual health and wellbeing. Aust N Z J Public Health. 2010;34:160‐164. [DOI] [PubMed] [Google Scholar]
- 83. Iskit S, Ilkit M, Turc‐Bicer A, Demirhindi H, Turker M. Effect of circumcision on genital colonization of Malassezia spp. in a pediatric population. Med Mycol. 2006;44:113‐117. [DOI] [PubMed] [Google Scholar]
- 84. Severance EG, Gressitt KL, Stallings CR, et al. Candida albicans exposures, sex specificity and cognitive deficits in schizophrenia and bipolar disorder. NPJ Schizophr. 2016;2:article 16018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Morris BJ, Hankins CA, Lumbers ER, et al. Sex and male circumcision: Women's preferences across different cultures and countries: a systematic review. Sex Med. 2019;7:145‐161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Grund JM, Bryant TS, Toledo C, et al. Association of male circumcision with women's knowledge of its biomedical effects and with their sexual satisfaction and function: a systematic review. AIDS Behav. 2019;23:1104‐1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Williamson ML, Williamson PS. Women's preferences for penile circumcision in sexual partners. J Sex Educ Ther. 1988;14:8‐12. [Google Scholar]
- 88. Risser JM, Risser WL, Eissa MA, Cromwell PF, Barratt MS, Bortot A. Self‐assessment of circumcision status by adolescents. Am J Epidemiol. 2004;159:1095‐1097. [DOI] [PubMed] [Google Scholar]
- 89. Stang HJ, Snellman LW. Circumcision practice patterns in the United States. Pediatrics. 1998;101:E51‐E56. [DOI] [PubMed] [Google Scholar]
- 90. American Academy of Pediatrics Task Force on Circumcision . Male circumcision. Pediatrics. 2012;130:e756‐e785.22926175 [Google Scholar]
- 91. Stern MJ. How circumcision broke the Internet . Slate. 2013. http://www.slate.com/articles/health_and_science/medical_examiner/2013/09/intactivists_online_a_fringe_group_turned_the_internet_against_circumcision.html (accessed 11 Aprril 2021)
- 92. Anonymous. CircumcisionGrief . Reddit. 2022. https://www.reddit.com/r/CircumcisionGrief/ (accessed 15 March 2022)
- 93. CircumcisionChoice . Intactivism is a Mental Disorder. CircumcisionChoice.com. 2019. https://www.circumcisionchoice.com/single‐post/mentaldisorder (accessed 16 March 2022)
- 94. Moreton S. Do false beliefs predict increased circumcision satisfaction in men? Adv Sex Med. 2020;10:42‐55. [Google Scholar]
- 95. Tan HM, Tong SF, Ho CC. Men's health: sexual dysfunction, physical, and psychological health–is there a link? J Sex Med. 2012;9:663‐671. [DOI] [PubMed] [Google Scholar]
- 96. Bossio JA, Pukall CF, Bartley K. You either have it or you don't: the impact of male circumcision status on sexual partners. Can J Hum Sexuality. 2015;24:104‐119. [Google Scholar]
- 97. Bronselaer GA, Schober JM, Meyer‐Bahlburg HF, T'sjoen G, Vlietinck R, Hoebeke PB. Male circumcision decreases penile sensitivity as measured in a large cohort. BJU Int. 2013;111:820‐827. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


