Abstract
Few studies have documented the pathways through which individual level variables mediate the effects of neighborhoods on health. This study used structural equation modeling to examine if neighborhood characteristics are associated with depressive symptoms, and if so, what factors mediated these relationships. Cross-sectional data came from a sample of mostly rural, older adults in North Carolina (n=1,558). Mediation analysis indicated that associations among neighborhood characteristics and depressive symptoms were mediated by loneliness (standardized indirect effect=−0.19, p<0.001), physical activity (standardized indirect effect= −0.01, p=0.003), and perceived individual control (standardized indirect effect=−0.07, p=0.02) with loneliness emerging as the strongest mediator. Monitoring such individual mediators in formative and process evaluations may increase the precision of neighborhood-based interventions and policies.
Keywords: depression, neighborhoods, mediation, loneliness, older adults
INTRODUCTION
Neighborhoods influence health and wellbeing, but the mechanisms of these effects are not well understood. Taking depression as an example, while at least six systematic reviews in the past decade (1-6) have examined if neighborhood features are associated with depression and/or mental health, few of the included studies examined how neighborhood characteristics are associated with outcomes. This stands in contrast to the number of theories and conceptual frameworks that have been developed to illustrate how neighborhoods affect health (see work on social determinants of health (7), social disorganization theory (8) and conceptual models from Diez Roux & Mair (9), Brown et al. (10), Carpiano (11), Blair et al. (12), and Kawachi & Berkman (13)). In these conceptual models, characteristics of the neighborhood economic environment (e.g., neighborhood poverty, disadvantage, or racial segregation) are thought to influence characteristics of the neighborhood physical environment (e.g., environmental exposures, food, physical activity, and recreation resources, services), and characteristics of the neighborhood social environment (e.g., safety, norms, cohesion, capital) (9). In turn, characteristics of the neighborhood physical and social environments are then associated with health outcomes both directly and indirectly through various mediators, including but not limited to:
Psychosocial processes (e.g., social support, loneliness, stress, resiliency, sense of control, sense of fear and anxiety) (9, 12)
Health behaviors, including physical activity (7-11, 14, 15)
Access to resources, medical care, and quality of medical care (7, 9, 10, 15)
Most of these conceptual models were built for general use, without regard to specific populations or settings. However, some research suggests that neighborhoods are particularly important for older adults since they 1) are less mobile than younger adults (16), which may make them more likely to rely on resources within their neighborhoods; 2) may lose social contacts as they age (17), thereby increasing the importance of social cohesion, and 3) may not leave their neighborhoods as much as younger adults who may be working or have other obligations (18). In addition, most older adults (nearly 80%) own their homes (19) and have lived in their neighborhoods for a number of years, thereby increasing aggregate exposure to residential neighborhood effects. The number and magnitude of these factors suggest that older adults may have a heightened vulnerability to certain neighborhood features and make research on neighborhoods and older adults especially useful (18, 20).
Previous research among older adults has especially highlighted the importance of perceptions of neighborhood environment for health and wellbeing. For instance, the causal model of neighborhood effects on aging (18), which is an extension of the ecological model of aging developed by Lawton et al. (21), highlights the importance of social integration (including social cohesion and safety), physical aspects of place (e.g., noise, deterioration), and available services and resources (including access to resources for physical activity, transportation, shops), in addition to socioeconomic conditions. In line with this conceptual model, research has shown that the negative effect of perceived safety on physical activity is particularly pronounced among older adults (18), that perceived access to resources (e.g., perceiving there to be attractive features in the nearby environment for outdoor activities, or perceiving nature to be a facilitator of exercise) is associated with better mobility of older adults (22), especially older adults with difficulties in walking (23), and that low perceived social cohesion is associated with decreased social participation (24). While understudied, researchers suggest that greater social cohesion in a neighborhood can lead residents to be more willing to help one another, make residents feel more secure, increase opportunities for social activity and engagement, and increase opportunities for residents to organize for what they need (18).
Moreover, most studies investigating neighborhoods and health of older adults have been conducted in urban environments, with few studies examining whether associations between neighborhoods and health extend to rural and suburban areas (18). Studying how neighborhoods relate to the health and wellbeing of older adults in rural neighborhoods may be important for two reasons. First, the concept of a “neighborhood” may be more difficult to define in rural areas (25), and so, we need empirical research documenting what neighborhood characteristics, if any, are important for older adults in non-urban areas. Second, older adults in rural areas may be even more vulnerable than those in urban areas, given disparities in health between rural and urban environments (26) and that sparseness of rural areas may make it more difficult for older adults to access resources and social connections. Therefore, documenting the influence of neighborhoods on older adults’ health in rural areas may guide needed interventions to improve health.
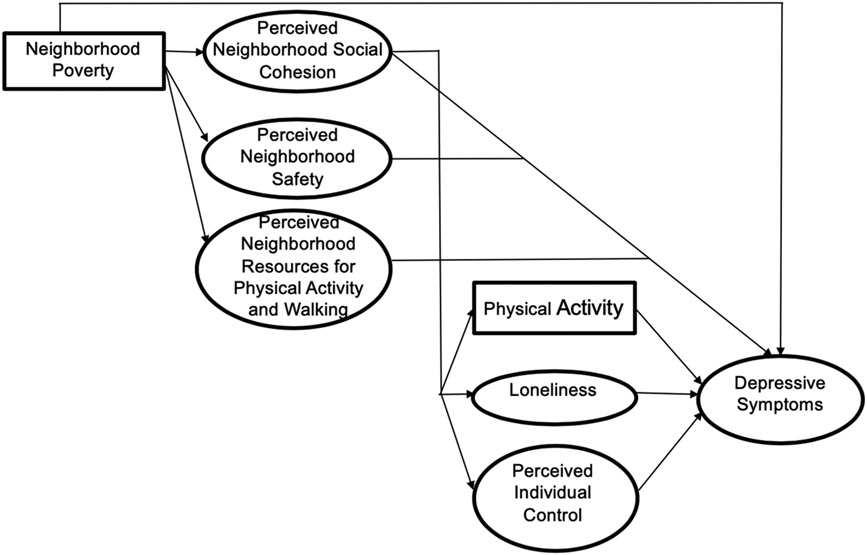
Guided by previous research, we hypothesized that—among older adults living in primarily rural neighborhoods—four neighborhood characteristics (i.e., poverty, perceived social cohesion, perceived resources for physical activity, and perceived safety) would be associated with depressive symptoms via effects on physical activity, loneliness, and perceived individual control. An illustration of these pathways can be seen in Figure 1. We focused on depressive symptoms as our outcome given that depression is a major public health problem (27), particularly for older adults (28), the leading cause of disability worldwide (29), and a well-studied outcome for neighborhood research (1-6).
Figure 1.
Conceptual model for proposed structural equation model pathways for adults from the T2 wave of the Johnston County Osteoarthritis Project, Johnston County, North Carolina, 2006-2011
Note: Ovals denote latent variables; measurement model and control variables not shown for simplicity.
METHODS
Participants and Procedures
Data for this study come from a population-based prospective cohort of knee and hip osteoarthritis (OA) among African American and White individuals (the Johnston County Osteoarthritis Project, “JoCo OA”) (30). Although the parent study was designed to capture OA prevalence and risk factors, we used the data to examine how neighborhood characteristics were associated with wellbeing among a large sample of older adults. Participants were not selected on the basis of whether they did or did not have any specific health condition, including arthritis. Recruitment occurred in Johnston County, North Carolina (NC), which at the time of this study, was classified as a mostly rural county (31). Details on the study design, data collection procedures, and study population are detailed in previous publications (30). In brief, the study was designed to be representative of civilian, non-institutionalized African Americans and White individuals over the age of 45 who resided in one of six towns or townships in Johnston County, NC for at least one year, were living in the county at the time of study enrollment, and physically and mentally capable of completing the study protocol. Data were collected in-person. All participants provided informed written consent at the time of recruitment. The study was approved by the Institutional Review Boards of the University of North Carolina Schools of Medicine and Public Health and the Centers for Disease Control and Prevention. The analytical sample for this study uses the T2: 2006-2011 cohort of adults. We chose this wave of data collection since it was the only wave in which neighborhood charactersitics were measured.
Measures
A list of all measures used in this study can be found in the appendix (Table A).
Outcome.
We used the Center for Epidemiological Studies Depression (CES-D) scale to assess depressive symptoms. The CES-D is one of the most widely used scales to assess levels of depressive symptomology (32). Developed in 1977, the CES-D was intended to assess epidemiology of depression in the general population, rather than diagnosis at clinical intake (32). While items were chosen from previously validated depression scales and based on symptoms of depression in clinical cases, the CES-D was not designed to reflect diagnostic criteria of depression at the time of its development (32). In contrast to other widely used measures, such as the Beck Depression Inventory, the CES-D focuses more on affective aspects of depression, rather than depression cognitions (33).
The CES-D contains 20 items that assess whether symptoms had occurred in the week prior to the interview. Response options range from 0 to 3, which refer to frequency of the symptoms (i.e., “rarely or none of the time” to “all of the time”). The CES-D was originally posited to have a four-factor structure composed of depressed affect, positive affect, somatic activity, and interpersonal issues (32). However, more than 20 alternative factor structures—including a unidimensional factor structure (34)—have been reported (35). In practice, many researchers (including Radloff, the original developer of the CES-D) report a total score, thereby treating the measure as unidimensional (34). We therefore analyzed depressive symptoms as a unidimensional latent variable. Although a cut-off point of 16 (total possible score range 0 – 60) has been used in previous research to indicate risk for moderate or severe depression (36), we conceptualized and analyzed CES-D scores as a continuum in order to maximize sensitivity of the measure. For consistency, we refer to the latent variable comprised of CES-D items as “depressive symptoms” throughout this manuscript.
Neighborhood characteristics.
We measured four neighborhood characteristics.
Neighborhood poverty.
We defined neighborhood poverty as the percentage of households with income below the poverty line within a census block group. We compiled these data from the 2010 U.S. Census, that bounded the time in which T2 data were gathered, 2006-2011. We used census block groups as the unit of analysis, since they are the smallest administrative boundary from the census that includes economic data. Census block groups generally contain between 600 and 3,000 people (37).
Perceived neighborhood social cohesion.
We measured perceived neighborhood social cohesion using 5-item measure of Social Cohesion and Trust of Sampson and colleagues (38). An example item is: “people around here are willing to help their neighbors” (1=strongly agree, 5= strongly disagree). Previous studies have found high reliability for this scale (Cronbach’s alpha of 0.82 and 0.86 at two different time points) and consistency over time (test-retest intra class correlation, ICC: 0.90; 95% CI: 0.84, 0.94) (39). Supporting validity, the scale has also been used in a variety of research studies assessing social cohesion / social capital (3, 40, 41).
Perceived neighborhood resources for physical activity and walking.
We measured perceived neighborhood resources for physical activity and walking using 11 items from the Walking and Exercise Environment scale (39). This scale assesses opportunities for exercise in individuals’ neighborhoods. An example item is: “my neighborhood offers many opportunities to be physically active” (1=strongly agree, 5= strongly disagree). Previous studies have shown this scale to have high reliability and consistency over time (test-retest ICC: 0.88; 95% CI: 0.79, 0.93) (39).
Perceived neighborhood safety.
We measured perceived neighborhood safety with three items. An example item is: “I feel safe walking in my neighborhood during the evening” (1=strongly agree, 5= strongly disagree). Previous studies have demonstrated these items to be reliable and consistent over time (test-retest ICC: 0.80; 95% CI: 0.67, 0.88) (39).
Mediators.
We selected three mediators based on their importance in previous research.
Physical activity.
We assessed physical activity using items from the 2001-2009 Behavioral Risk Factor Surveillance System (BRFSS) (42), which classifies individuals as inactive, insufficiently active, or active. Following guidelines for use of the BRFSS physical activity questions(42), to be classified as meeting recommended goals for moderate activity, a respondent needed to report 5 or more days of moderate activity with 30 or more minutes per day. To be classified as meeting recommended goals for vigorous activity, a respondent needed to report 3 or more days of vigorous activity with 20 or more minutes per day. An individual who met the moderate goal, the vigorous goal, or both was classified as “active” while an individual who reported some moderate activity, vigorous activity, or both but did not meet the goals for either moderate or vigorous activity was classified as “insufficiently active.” Otherwise, individuals were classified as “inactive.”
Loneliness.
We assessed loneliness using four items from the Strong Ties scale (43), which asks participants: “How often are you bothered by not…” 1) “having a close companion?”, 2) “seeing people you feel close to?”, 3) “having enough close friends?”, and 4) “having someone who shows you love and affection?” (1=all of the time, 5=never). Items were reverse coded so that higher scores indicate more loneliness. These items have been used in previous research (44-47) and have been found to be reliable (Cronbach’s alpha = 0.89) (45). Additionally, moderate correlations with other constructs, such as social contacts (45) and depressive symptoms (46), suggest these items are valid.
Perceived individual control.
To assess perceived individual control, we used two items from Israel et al.’s Perceived Control Scale (48). These items were: “I have control over the decisions that affect my life” and “I am satisfied with the amount of control I have over decisions that affect my life” (1=strongly agree to 5=strongly disagree). We reverse-coded items so that higher scores indicate more control. These items have been used in previous research studies and found to be reliable (Cronbach’s alpha = 0.83) (49-51).
Control variables.
Control variables assessed included standard demographic variables as well as health-related variables that could independently be associated with depressive symptoms and neighborhood context. Specifically, we assessed race / ethnicity (White or Black / African American), education (categorized as less than high school or high school or greater), BMI (based on measured height and weight, a continuous variable), gender (male or female), age (a continuous variable), health insurance status (categorized as public insurance, private insurance, or none), and number of comorbidities (assessed using a disease inventory index). We also assessed knee OA status as a control variable using radiography and the Kellgren and Lawrence (KL) grade, which scores OA severity on a scale of 0-4 (52). We classified individuals with scores of 2-4 in at least one knee as having knee OA. Otherwise, we classified individuals as not having knee OA.
Data Analysis
Descriptive statistics.
Descriptive statistics included means, standard deviations, and frequencies of all identified demographic variables, neighborhood variables, and depressive symptoms. Bivariate correlation analyses were used to assess relationships among neighborhood variables and depressive symptoms. We conducted descriptive statistics using SAS version 9.4 survey procedures (SAS Inc., Cary, NC, USA).
Confirmatory factor analysis and structural equation modeling.
To examine how neighborhood characteristics were related to depressive symptoms through the proposed mediators, we used structural equation modeling (SEM) (53). We chose to use SEM since we were testing complex mediation models (multiple sequential mediators), had several hypothesized latent variables, and needed to control for clustering of observations within neighborhoods. Prior to using SEM, we verified that there were no significant interactions among any of the exposures and mediators.
Using MPlus version 7, we followed a two-step structural equation modeling approach to establish the quality of the measurement model using confirmatory factor analysis (CFA) and test the full general SEM (54). We first used CFA to evaluate the fit of six latent variables: 1) perceived neighborhood social cohesion, 2) perceived neighborhood resources for physical activity and walking, 3) perceived neighborhood safety, 4) loneliness, 5) perceived individual control, and 6) depressive symptoms. These variables were specified as latent variables because they represent unobservable (i.e., latent) constructs and they were measured using multiple items (combined into scales), which thereby makes CFA appropriate. We examined neighborhood poverty and physical activity as observed variables. We entered the remaining control variables into the models as observed variables.
After determining adequate fit of the measurement models using CFA and making any necessary modifications, we assessed the fit of the structural model controlling for clustering at the neighborhood census block group level (using type=complex), which adjusts standard errors using an empirical correction. As seen in Figure 1, our SEM contains three main pathways: 1) the pathway from neighborhood poverty to perceived neighborhood environment, 2) the pathway from perceived neighborhood environment to the proposed mediators, and 3) the pathway from the proposed mediators to depressive symptoms.
In SEM, indirect effects are calculated as the product of the pathway from independent variable to the mediator (a path) and the pathway from the mediator to the outcome (b path) (55). In contrast to estimating effects in separate regression models, SEM simultaneously estimates direct and indirect effects (56). Also in SEM, indirect effects are tested using bootstrapping, which involves taking multiple repeated samples from the dataset. For each bootstrapped sample, the model is refit and estimates for all the parameters (including path coefficeints and standard errors) are obtained. From these values, confidence intervals are calculated.
To determine the fit of the measurement model and SEM, we used a priori, well-established criteria, including the chi-square test (p-value should be >0.05; however, model fit can still be adequate if this p-value is <0.05 since chi-square is dependent on sample size (57)); the Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) (CFI, TLI should be >0.95 (58, 59)); the root mean square error of approximation (RMSEA, should be <0.08 (60, 61)); and standardized factor loadings (should be >0.30 (62)). The model illustrated in Figure 1 was tested. Given that all manifest variables were ordinal (measured on a 1-5 scale), we used weighted least squares means and variance adjusted (WLSMV) estimation, which is appropriate for data with non-normal distributions (53). Although parameter estimates are more difficult to estimate using WLSMV because a probit model is used, previous researchers have used WLSMV to analyze mediation (63-65) and this approach avoids bias associated with the inclusion of categorical indicators. Our sample included participants with full data on covariates. In our models, 139 participants (approximately 8.2% of the sample) were missing some of the observed exogenous variables (i.e., control variables) and excluded by MPlus. For all analyses, we set critical α = .05 and used 2-tailed statistical tests.
Sensitivity Analyses.
We conducted two sensitivity analyses. In the first, we analyzed separately somatic and non-somatic depressive symptoms on the CES-D, since it is possible that they would be differentially associated with neighborhood characteristics and mediators. Somatic symptoms included items 1, 2, 5, 7, 11, and 20 from the CES-D and referred to whether individuals were bothered by things, had a poor appetite, had trouble keeping their mind on what they were doing, felt that everything was an effort, had restless sleep, and could not get going (35). Remaining items assessed non-somatic symptoms related to affect (e.g., “I felt sad”), anhedonia (e.g., “I enjoyed life”), and interpersonal concerns (e.g., “People wer unfriendly”). Second, sensitivity analyses evaluated whether relationships remained apparent when the sample was confined only to those with chronic conditions to determine whether relationships between neighborhood context and depressive symptoms varied by chronic disease status (see Appendix Table A for the list of included chronic conditions). Third, sensitivity analyses evaluated whether relationships remained apparent when the sample was confined only to those with OA (knee or hip) plus another chronic condition.
RESULTS
Descriptive Statistics
Details on the demographic characteristics of participants are presented in Table 1. The sample was composed of adults who were on average 68.1 years old (SD: 9.1). Participants were diverse, with a substantial number of African Americans (31.2%) and individuals without a high school degree (21.8%). Almost half of participants (44.5%) had radiographic knee OA and on average, had 1.7 other comorbidities. Overall, 90.9% of the sample reported at least one chronic condition. Additionally, participants reported few depressive symptoms (mean CES-D score: 6.6, SD: 7.5, possible range: 0-60), although 11.4% had scores at or above 16 suggestive of moderate or severe depression.
Table 1.
Participant characteristics of adults from the T2 wave of the Johnston County Osteoarthritis Project, Johnston County, North Carolina, 2006-2011, n=1697
| Characteristic | N (%) or mean (SD) |
|---|---|
| Race | |
| White | 1167 (68.8) |
| African American or Black | 530 (31.2) |
| Gender | |
| Male | 552 (32.5) |
| Female | 1145 (67.5) |
| Age (range 50-95), mean (SD) | 68.1 (9.1) |
| BMI (range 12.6-78.1), mean (SD) | 31.5 (7.2) |
| Education | |
| High school or greater | 1297 (78.2) |
| Less than high school | 362 (21.8) |
| Health insurance | |
| Public | 1176 (69.3) |
| Private | 412 (24.3) |
| None | 109 (6.4) |
| Number of comorbidities (range 0-11) a | 1.7 (1.3) |
| Knee OA a | |
| No | 910 (55.5) |
| Yes | 729 (44.5) |
| Neighborhood poverty (range 0-44), mean (SD) | 16.7 (10.3) |
| Perceived neighborhood social cohesion (range 5-25), mean (SD) | 18.9 (3.6) |
| Perceived neighborhood resources for physical activity and walking (range 11-55), mean (SD) | 35.9 (6.2) |
| Perceived neighborhood safety (range 3-15) | 11.0 (2.3) |
| Loneliness (range 4-20), mean (SD) | 6.2 (2.7) |
| Perceived individual control (range 2-10), mean (SD) | 8.0 (1.5) |
| Physical activity | |
| Inactive | 484 (28.7) |
| Insufficiently active | 627 (37.2) |
| Sufficiently active | 573 (34.0) |
| Depressive symptoms (range 0-60), mean (SD) | 6.6 (7.5) |
91% of the sample had at least one chronic disease defined using a disease inventory index and radiographic assessments of knee OA. 52% of the sample had OA (knee or hip) plus another chronic disease.
Confirmatory Factor Analysis
The measurement model with no modifications had a moderate fit to the data (See Appendix Table B). Two latent variables had poor initial fit: the measure for perceived neighborhood resources for physical activity and walking and that for loneliness. After reviewing correlation matrices for the 11 items making up the factor for neighborhood resources for physical activity and walking, we included 4 items in the revised model (“My neighborhood offers many opportunities to be physically active,” “It is pleasant to walk in my neighborhood,” “There are enough trees in my neighborhood to provide shade,” and “In my neighborhood, the streets or sidewalks are in good condition”). We chose these items based on both empirical (inter-item correlations > 0.40) and theoretical evidence from previous literature, suggesting streets, shade, and neighborhood aesthetics are important domains for walkability in rural neighborhoods (66). Loneliness was left unmodified from the widely used version we employed (43). Although the RMSEA value (0.12; 95% CI: 0.19, 0.15) was above the desired 0.06 cut-off (60, 61), the model demonstrated adequate fit based on the other indices and modifications would not have been theoretically or empirically based.
Bivariate Correlations
Bivariate analyses revealed significant relationships among most latent and observed variables in the hypothesized directions (Table 2). Correlations of neighborhood poverty with other neighborhood variables ranged from −0.11 to −0.26 (all p-values <0.05), while correlations among perceived neighborhood social cohesion, perceived neighborhood resources for physical activity and walking, and perceived neighborhood safety were moderate to high, ranging from 0.66 to 0.75 (all p-values <0.001). These three neighborhood characteristics were all significantly associated with the three selected mediators (physical activity, loneliness, and perceived individual control, all p-values <0.001). Finally, depressive symptoms were moderately associated with all variables, except for neighborhood poverty for which there was a weak, but still statistically significant association (r=0.08, p=0.03).
Table 2.
Correlation matrix of observed and latent variables for adults from the T2 wave of the Johnston County Osteoarthritis Project, Johnston County, North Carolina, 2006-2011, n=1697
| 1.Neighborhood poverty |
2.Perceived neighborhood social cohesion |
3.Perceived neighborhood resources for physical activity and walking |
4.Perceived neighborhood safety |
5.Physical activity |
6.Loneliness | 7.Perceived individual control |
8.Depressive symptoms |
|
|---|---|---|---|---|---|---|---|---|
| 1 | -- | −0.18 *** | −0.11 * | −0.26 *** | −0.14 *** | 0.03 | 0.01 | 0.08 * |
| 2 | -- | 0.66 *** | 0.74 *** | 0.13 *** | −0.34 *** | 0.45 *** | −0.30 *** | |
| 3 | -- | 0.68 *** | 0.13 *** | −0.34 *** | 0.65 *** | −0.32 *** | ||
| 4 | -- | 0.14 *** | −0.28 *** | 0.35 *** | −0.26 *** | |||
| 5 | -- | −0.17 *** | 0.06 | −0.22 *** | ||||
| 6 | -- | −0.36 *** | 0.56 *** | |||||
| 7 | -- | −0.27 *** | ||||||
| 8 | -- |
Note, in final structural models, a higher order factor comprised of perceived neighborhood social cohesion, perceived neighborhood resources for physical activity and walking and perceived neighborhood safety was modeled. Correlations of this factor (perceived neighborhood environment) with poverty were −0.20***, with perceived individual control were 0.58***, with physical activity were 0.16***, and with loneliness were −0.39*** and with depressive symptoms were −0.35.***
Boldface denotes significance at p<0.05
p<.05
p<.01
p<.001
Structural Equation Model
The initial hypothesized structural equation model had a relatively good fit to the data, but several of the associations among perceived neighborhood social cohesion, perceived neighborhood resources for physical activity and walking, perceived neighborhood safety, and the proposed mediators were not in the expected direction based on bivariate correlational results. We hypothesized that this was due to high correlations among the three perceived neighborhood characteristics (ranging from 0.66 to 0.75). When multicollinearity is present, the introduction of additional predictors into the model can diminish the regression coefficient and significance of a predictor, and the regression coefficient can even reverse in sign (67). We therefore fit a model with a higher order factor (labeled “perceived neighborhood environment”), which was comprised of these three neighborhood characteristics (social cohesion, resources for physical activity/walking, safety) and only specified pathways that were significant in the bivariate correlations at p<.05.
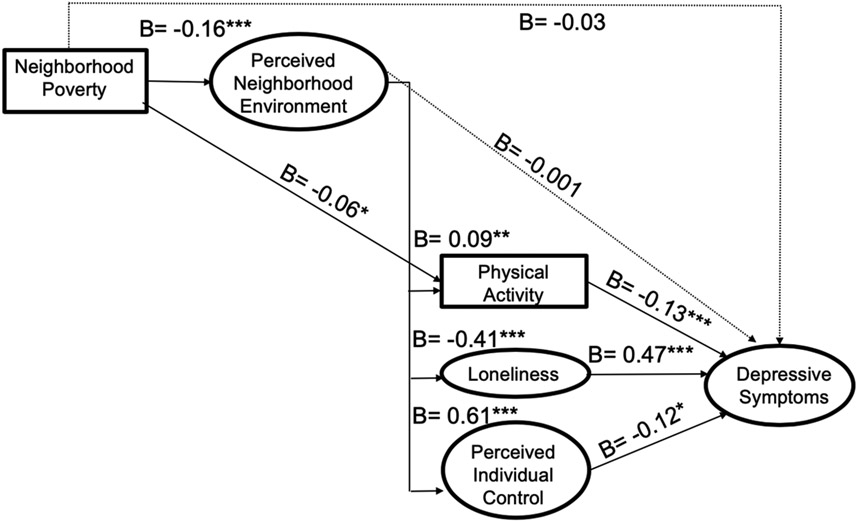
Results from the structural equation model can be seen in Table 3 and are displayed visually in Figure 2. We found the model represented in Figure 1 demonstrated adequate fit with respect to the following metrics: RMSEA = 0.02 (95% CI: 0.02, 0.02), CFI = 0.96, and TLI =0.96. We selected this model as the final model.
Table 3.
Results from the structural equation model for adults from the T2 wave of the Johnston County Osteoarthritis Project, Johnston County, North Carolina, 2006-2011, n=1558
| Exogenous variables |
Endogenous variables | ||||
|---|---|---|---|---|---|
| Perceived neighborhood environment |
Physical activity |
Loneliness | Perceived individual control |
Depressive symptoms |
|
| Poverty | B= −0.16*** | B= −0.06* | -- | -- | B= −0.03 |
| Perceived neighborhood environment | -- | B= 0.09** | B= −0.41*** | B= 0.61*** | B= −0.001 |
| Physical activity | -- | -- | -- | -- | B= −0.13*** |
| Loneliness | -- | -- | -- | -- | B= 0.47*** |
| Perceived individual control | -- | B= −0.12* | |||
Notes
N=1558 (139 observations were deleted because they were missing on all individual control variables). All relationships controlled for race, gender, BMI, education, health insurance status, number of comorbidities, age, and knee OA status. All relationships also controlled for clustering using type=complex. Beta coefficients (B) are standardized.
p<.05
p<.01
p<.001
Model Fit:
Chi-Square value (p-value): 1724.40, p<.001; RMSEA: 0.02 (95% CI: 0.02, 0.02); CFI: 0.96; TLI: 0.96
- Perceived neighborhood environment → Physical activity → Depressive symptoms: B = −0.01 (95% CI: −0.02, −0.004), p=0.003
- Perceived neighborhood environment → Loneliness → Depressive symptoms: B = −0.19 (95% CI: −0.23, −0.16), p<0.001
- Perceived neighborhood environment → Perceived individual control → Depressive symptoms: B = −0.07 (95% CI: −0.13, −0.01), p=0.02
- Poverty → physical activity → depressive symptoms: B= 0.008 (95% CI: 0.000, 0.02), p=0.06
- Poverty → perceived neighborhood environment → depressive symptoms: B= 0.000 (95% CI: −0.02, 0.02), p=0.98
- Poverty → perceived neighborhood environment → Physical activity → Depressive symptoms: B=0.002 (95% CI: 0.000, 0.003), p=0.01
- Poverty → perceived neighborhood environment → loneliness → depressive symptoms: B= 0.03 (95% CI: 0.02, 0.05), p<0.001
- Poverty → perceived neighborhood environment → perceived individual control -→ depressive symptoms: B= 0.01 (95% CI: 0.001, 0.02), p=0.03
- Poverty → perceived neighborhood environment → Physical activity: B= −0.02 (95% CI: −0.03, −0.004), p=0.009
Figure 2.
Final conceptual model with direction and significance of parameter estimates for adults from the T2 wave of the Johnston County Osteoarthritis Project, Johnston County, North Carolina, 2006-2011, n=1558
Notes: Dashed arrows indicate a non-significant pathway. All parameter estimates can be seen in Table 3. Circles denote latent variables; measurement model and control variables not shown for simplicity. Model adjusts for: race, gender, BMI, education, health insurance status, number of comorbidities, age, knee OA status, and clustering within neighborhoods. Chi-Square (p-value): 1724.40, p<.001); RMSEA: 0.02 (95% CI: 0.02, 0.02); CFI: 0.96; TLI: 0.96.
* p<0.05; ** p<0.01; *** p<0.001
We found neighborhood poverty was significantly negatively associated with perceived neighborhood environment (B=−0.16, p<0.001) and physical activity (B=−0.06, p=0.04), but not with depressive symptoms. In turn, perceived neighborhood environment was significantly associated with increased physical activity (B=0.09, p=0.005), less loneliness (B=−0.41, p<0.001), and increased perceived individual control (B=0.61, p<0.001), but not depressive symptoms (B=−0.001, p=0.98), despite their significance in bivariate correlations. All three mediators were significantly associated with depressive symptoms in the expected directions (physical activity and depressive symptoms: B=−0.13, p<0.001; loneliness and depressive symptoms: B=0.47, p<0.001; and perceived individual control and depressive symptoms: B=−0.12, p=0.01).
In addition, we observed a number of indirect effects. The hypothesized pathways from perceived neighborhood environment to depressive symptoms through the proposed mediators were all significant (standardized beta coefficients ranging from B= −0.01 to B= −0.19, p-values <0.05). Specifically, the indirect effect for perceived neighborhood environment on depressive symptoms through loneliness was B=−0.19; 95% CI: −0.23, −0.16; p<0.001; the indirect effect through perceived individual control was B=−0.07; 95% CI: −0.13, −0.01; p=0.02; and the indirect effect through physical activity was B=−0.01; 95% CI: −0.02, −0.004; p=0.003. Loneliness emerged as the strongest of the three mediators, as demonstrated through the non-overlapping 95% confidence intervals of the indirect effects.
In addition, poverty was significantly associated with depressive symptoms through physical activity and perceived neighborhood environment (B=0.002, p= 0.01), loneliness and perceived neighborhood environment (B=0.03, p<0.001), and perceived individual control and perceived neighborhood environment (B=0.01, p=0.03). Finally, poverty was significantly associated with physical activity through perceived neighborhood environment (B= −0.02, p= 0.009).
Overall, all variables (neighborhood and control) explained 42% of the variance in depressive symptoms, 20% of the variance in loneliness, 37% of the variance in perceived individual control, and 13% of the variance in physical activity. Alone (including direct and indirect effects), neighborhood variables explained 12% of the variance in depressive symptoms, 15% of the variance in loneliness, 37% of the variance in perceived individual control, and 4% of the variance in physical activity.
Sensitivity Analysis
Results from sensitivity analyses can be seen in the Appendix (Tables C, D, and E). When analyzing somatic and non-somatic depressive symptoms separately, all paths noted above were confirmed, with the exception that perceived individual control no longer mediated the effects of perceived neighborhood characteristics on somatic depressive symptoms (B=−0.05, p=0.06) (Table C). Perceived individual control did, however, mediate the effects of perceived neighborhood characteristics on non-somatic depressive symptoms (B=−0.08, p=0.02). In addition, we found that results did not change when only including adults with at least one chronic disease (Table D). However, when only including adults with OA (knee or hip) and another chronic disease, we found that perceived individual control was no longer associated with depressive symptoms (B=−0.07, p=0.14) and perceived neighborhood environment was no longer associated with physical activity (B=0.05, p=0.20) (Table E). Accordingly, physical activity and perceived individual control no longer mediated the effects of perceived neighborhood environment on depressive symptoms and the only significant mediator was loneliness (B=0.052, p<0.001).
DISCUSSION
Among this sample of older adults—91% of whom reported having at least one chronic condition—several neighborhood characteristics were associated with depressive symptoms. Within this pattern of results, two interesting findings were observed. First, neighborhood factors were strongly associated with depressive symptoms and this relationship was mediated by individual-level variables. This observation suggests that both individual-level and neighborhood-level characteristics may be important for future interventions looking to improve mental health outcomes. These findings also suggest that aging in place interventions, in particular, could focus attention on how neighborhood environment could be improved, in addition to making modifications to older adults’ home environments. Second, we found that loneliness emerged as the strongest mediator of neighborhood characteristics on depressive symptoms. These findings have a number of important implications for public health practice and research, as discussed below.
Little research has examined how neighborhood characteristics are associated with health. In this study, we found three variables completely mediated the effects of perceived neighborhood environment on depressive symptoms. These results suggest the importance of these three variables—physical activity, loneliness, and perceived individual control—as behavioral and psychosocial mediators of the effects of neighborhood factors on depression. Additionally, we found that physical activity, loneliness, and perceived individual control mediated the effects of the perceived neighborhood environment on depressive symptoms and that when taking these indirect effects into account, there were no direct effects from poverty or the perceived neighborhood environment on depressive symptoms. Although randomized controlled trials changing neighborhood disadvantage or poverty are almost nonexistent and not particularly feasible, though notable examples do exist (68), our findings suggest that interventions could focus on changing modifiable factors that mediate relationships between neighborhood disadvantage and health. Furthermore, other neighborhood aspects, such as social cohesion or resources for physical activity, might be changed using relatively easy methods (e.g., increasing vegetation and common spaces to encourage social interaction (69) and improving infrastructure such as lighting and sidewalks to encourage physical activity (70)).
Interestingly, the strongest pathway through which neighborhood characteristics influenced depressive symptoms was loneliness. At least two previous studies have found that neighborhood residential satisfaction, social connections, safety, and collective efficacy are associated with loneliness (71, 72), although not many studies have examined relationships between neighborhoods and loneliness. This lack of research is surprising since social relationships are fundamental among primates (73) and directly influence biological processes underlying health outcomes (74). Indeed, in a meta-analysis of 148 longitudinal studies, Holt-Lundstad et al. found a 50% reduction in mortality for individuals with strong social relationships, which was comparable with reductions in mortality attributable to quitting smoking (75). As loneliness and social isolation continue to emerge as risk factors for premature mortality (76), our findings suggest that interventions designed to improve depressive symptoms among older adults living in primarily rural neighborhoods may choose to focus on loneliness. This need not be to the exclusion of perceived individual control and physical activity, each of which also emerged as significant, but weaker, mediators.
It should be noted that loneliness and depressive symptoms are related to one another. Indeed, one of the items in the CES-D asks about loneliness. However, studies (using factor analysis and SEM) have shown that these concepts can be thought of as related but conceptually distinct (77). For instance, in a longitudinal study of adults aged 50-67 in Illinois, loneliness and depressive symptoms were associated with one another (controlling for demographic and other psychosocial variables), but emerged as separate constructs with reciprocal influence in latent variable growth models (77). Evidence from our study confirms these findings given that loneliness was associated with both somatic and non-somatic depressive symptoms factors. Thus, our results suggest that loneliness is associated with depressive symptoms even when depressive symptoms is modeled without the item related to loneliness. Moreover, the fact that the CES-D contains many items (19/20) that are not related to loneliness suggests that there is much to depressive symptoms besides loneliness.
We also found that perceived individual control and physical activity were significant, albeit weaker, mediators of the effects of perceived neighborhood environment on depressive symptoms. A number of studies have found strong relationships between neighborhood characteristics and physical activity (78, 79), including among older adults (80). Research has also shown that greater physical activity can have protective effects against depression (81). That we found physical activity to mediate the relationship between perceived neighborhood environment and depressive symptoms is therefore perhaps unsurprising. Less research has established links between neighborhood characteristics and perceived individual control, however some studies have found significant associations (82). Researchers hypothesize that neighborhoods with higher socioeconomic status and greater informal social control (i.e., neighborhoods in which residents are able to help regulate and keep their neighborhood safe) can increase opportunities and resources available to residents, thereby making residents feel more in control over their own circumstances (82). Perceived individual control is also thought to be a key component of successful coping strategies; for instance, in dealing with stressful life events, individuals with greater perceived control are more able to respond in appropriate, adaptive ways (83, 84). In future interventions and policies designed to change neighborhood characteristics and/or perceptions of neighborhood characteristics, it may be helpful to measure and assess how the three significant mediators identified here (loneliness, physical activity, and perceived individual control) are associated with outcomes. This monitoring, which could occur during process evaluations, could help researchers understand how interventions are effective or ineffective (56). If researchers find significant mediated pathways, then they could allocate more resources to target those mechanisms in future studies. Non-significant pathways can also tell researchers that those mechanisms may not be important and resources can be more effectively allocated.
In our study and as in previous research (65), we found stronger associations with depressive symptoms for neighborhood perceptions versus area-level measures of the neighborhood environment that are independent of residents’ perception (in this case, neighborhood poverty). It is important to note that perceptions of neighborhood variables are not true measures of the “neighborhood” or “contextual neighborhood effects.” Instead, they are individual-level characteristics that are distinct from area-level estimates of the neighborhood. Both types of measures (area-level measures of neighborhood environment and self-reported perceptions of neighborhood environment) are important to examine when conducting research on neighborhoods and health since they provide different pieces of information (65). For instance, area-level measures of neighborhood environment are not subject to self-report bias and provide rich information that can be qualitatively hard for residents to provide (e.g., % of residents in poverty). However, they are also usually based on census data and may not provide information on the full range of neighborhood domains that influence health. Perceptions of neighborhood environment, on the other hand, may more directly align with individual’s experiences and reflect how individuals interact with their neighborhoods, but are typically limited by same source bias. In other words, individuals with a particular disposition (i.e., individuals who are less physically active or individuals with more chronic conditions) may rate their environments as less satisfactory than individuals with a different disposition (65). Importantly, with SEM, we are able to partly control for these effects by regressing neighborhood perceptions on individual-level characteristics, such as age, race, BMI, and others (65). While it is possible that other unmeasured variables may have affected individuals’ perceptions of their neighborhood environments, our analyses begin to disentangle the potential bias that self-reported assessments of neighborhoods may contain (65) although other biases (e.g., reverse causality) remain possible interpretations of findings.
This is one of few studies that has focused on neighborhood characteristics among older adults living in primarily rural neighborhoods. Our findings suggest that characteristics of rural neighborhoods, like those of urban neighborhoods, are influential for the health and wellbeing of older adults. This finding is perhaps unsurprising given the large body of research documenting the importance of neighborhoods on health. However, we did find that perceived neighborhood characteristics were particularly influential. Rural neighborhoods can be particularly challenging to define and while many researchers examining urban neighborhoods use administrative units, such as census block groups, such an approach may not work for rural neighborhoods since the same administrative unit will span a larger distance in sparsely populated areas (25). For this reason, perceived neighborhood environment may more closely reflect an individual’s experience with what they understand to be their neighborhood.
In 2014, 14.5% (46 million) of the US population was aged 65 or older; by 2060, this figure will reach 23.5% (98 million) (85). As adults continue to live longer, health care spending will likely increase, particularly for chronic diseases, which represent 95% of all health care costs for older adults in the US (86). Innovative strategies to maintain and promote the quality of life of older adults are needed. One such strategy is promoting “aging in place” including facilitating older adults remaining in their own “homes and communities safely, independently, and comfortably, regardless of age, income, or ability level” (87). Despite the importance of both home and community environments, most interventions tailored to older adults have focused on making improvements to individual homes (e.g., making modifications and adaptions to homes in order to prevent accidents or falls, improving functional ability of features in homes, providing services in homes, removing barriers that would prevent older adults from continuing to live at home, etc.) (88). The results from this study suggest that both poverty and perceived neighborhood environment are important correlates of quality of life and that actionable strategies to improve them (e.g., the focus on common spaces, etc. noted above (69) (89)) that should be explored in designing public health interventions for older adults in rural areas.
Limitations
There are several limitations to our findings. First, because we used cross-sectional, observational data, we were unable to assess temporal order. Causal inference methods for mediation have been developed to more accurately quantify direct and indirect effects by using sensitivity analyses to examine potential violations of assumptions (e.g., no measured confounding on different pathways from exposures to outcomes) (90, 91). While causal inference methods have a number of benefits over traditional methods for assessing mediation, we chose to use SEM because we estimated multiple sequential mediators, we were interested in analyzing several latent variables, and we needed to control for clustering of observations within neighborhoods. It is important to note that a number of requirements would need to be met before using our findings to make causal claims (e.g., theory was used to decide how variables should be ordered, competing explanations are ruled out, etc.) (92).
Second, since all measures (except neighborhood poverty) were subject to self-report, it is possible that depressed or lonely individuals could have rated their neighborhoods differently than individuals who were not depressed or not lonely. Third, we did not control for individual-level income data, which may have partially accounted for the observed effects, especially those related to neighborhood poverty. While we included measures of education and health insurance status as control variables, which have been used as proxies of income in previous studies, further research controlling for income and examining interactions between neighborhood income and individual income will be important.
Fourth, there was a limited amount of missing data for control variables and a small number of observations (approximately 8.2% of the sample) were excluded from analyses, which could have biased results. Fifth, this study relied on a specific population—older adults in Johnston County, NC. The use of this specific population may limit generalizability to other settings, such as other counties in NC or states in the US and other populations. However, prevalence of chronic disease in this sample (90.9%) was similar to prevalence reported from a large, nationally representative sample of older adults in 2008 (92.2%) (93). Sixth, although we examined loneliness, perceived individual control, and physical activity as constructs that were separate from depressive symptoms, it is possible that they could represent symptoms of depression. Seventh, the RMSEA value for loneliness in our CFA was higher than our a prioi criterion of 0.08, which could have inflated some fit indices.
Finally, it is also important to note that participants included in these analyses were selected from a prospective cohort study and originally invited to participate between 1991-1997 (baseline) or 2003-2004 (for cohort enrichment). By the T2 wave of data collection (2006-2011), many individuals had died. It is possible that individuals surviving to the T2 wave of data collection may have been healthier at baseline than those not studied at T2 (referred to as “survivor bias”). Indeed, compared to participants not included in the T2 wave, participants included in the T2 wave were significantly more likely at baseline to be younger, female, or White; to have a high school degree or higher, have a high managerial or professional job, and live in a neighborhood with fewer households below the poverty line; and to have a BMI of 30 or greater, fewer comorbidities, and lower CES-D scores. These additional analyses can be found in the Appendix (Table E).
Conclusions
In this sample of mostly rural, older adults of whom many had radiographic knee OA (44.5%) or other chronic conditions (total = 91%), poverty and perceived neighborhood environment were associated with reports of depressive symptoms through loneliness, perceived individual control, and physical activity. Specifically, poverty was associated with worse perceived neighborhood environment. In turn, a better perceived neighborhood environment was associated with less loneliness, an increased sense of control, and increased physical activity, which were then associated with fewer depressive symptoms, altogether accounting for 42% of the variance in depressive symptoms (along with control variables). Loneliness was the strongest mediator of neighborhood characteristics on depression. These findings suggest that both individual-level mediators and neighborhood context are important correlates of depressive symptoms among older adults. Aging in place interventions, in particular, could focus attention on how neighborhood environment could be improved, in addition to making modifications to older adults’ individual home environments.
Supplementary Material
Funding and Role of Funding Source:
The parent study was supported in part by the Association of Schools of Public Health and the Centers for Disease Control and Prevention (S043, S1734, S3486), the Centers for Disease Control and Prevention (U01 DP003206 and U01 DP006266), and by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (RO1 AR053898-P60 AR30701, P60 AR049465, P60 AR064166). All statements in this publication, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Associations of Schools of Public Health, CDC or NIAMS. Support for this study was also provided by a Dissertation Completion Fellowship from the University of North Carolina at Chapel Hill Graduate School. This research was independent from funders. The funder had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Competing Interests: The authors declare: no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Transparency Declaration: The lead author (SDK) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
Ethics Approval: At baseline, all participants provided informed written consent at the time of recruitment. The study was approved by the Institutional Review Boards of the University of North Carolina Schools of Medicine and Public Health (IRB #92-0583) and the Centers for Disease Control and Prevention.
REFERENCES
- 1.Richardson R, Westley T, Gariepy G, Austin N, Nandi A: Neighborhood socioeconomic conditions and depression: a systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology. 2015, 50:1641–1656. [DOI] [PubMed] [Google Scholar]
- 2.Kim D: Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic Reviews. 2008, 30:101–117. [DOI] [PubMed] [Google Scholar]
- 3.Mair C, Diez Roux AV, Galea S: Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. Journal of Epidemiology and Community Health. 2008, 62:940–946, 948 p following 946. [DOI] [PubMed] [Google Scholar]
- 4.Evans GW: The built environment and mental health. Journal of Urban Health. 2003, 80:536–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Truong KD, Ma S: A systematic review of relations between neighborhoods and mental health. J Ment Health Policy Econ. 2006, 9:137–154. [PubMed] [Google Scholar]
- 6.Gong Y, Palmer S, Gallacher J, Marsden T, Fone D: A systematic review of the relationship between objective measurements of the urban environment and psychological distress. Environment International. 2016, 96:48–57. [DOI] [PubMed] [Google Scholar]
- 7.Braveman P, Egerter S, Williams DR: The social determinants of health: coming of age. Annual Review of Public Health. 2011, 32:381–398. [DOI] [PubMed] [Google Scholar]
- 8.Shaw CR, McKay HD: Juvenile delinquency and urban areas. Chicago. 1996, 19421:19692. [Google Scholar]
- 9.Diez Roux AV, Mair C: Neighborhoods and health. Annals of the New York Academy of Sciences. 2010, 1186:125–145. [DOI] [PubMed] [Google Scholar]
- 10.Brown AF, Ettner SL, Piette J, et al. : Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiologic Reviews. 2004, 26:63–77. [DOI] [PubMed] [Google Scholar]
- 11.Carpiano RM: Toward a neighborhood resource-based theory of social capital for health: can Bourdieu and sociology help? Social Science and Medicine. 2006, 62:165–175. [DOI] [PubMed] [Google Scholar]
- 12.Blair A, Ross NA, Gariepy G, Schmitz N: How do neighborhoods affect depression outcomes? A realist review and a call for the examination of causal pathways. Social Psychiatry and Psychiatric Epidemiology. 2014, 49:873–887. [DOI] [PubMed] [Google Scholar]
- 13.Kawachi I, Berkman LF: Social Cohesion, Social Capital, and Health. In Berkman LF, Kawachi I and Glymour M (eds), Social epidemiology: Oxford University Press, 2014. [Google Scholar]
- 14.Browning CR, Cagney KA: Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. Journal of Health and Social Behavior. 2002:383–399. [PubMed] [Google Scholar]
- 15.Brown AF, Ang A, Pebley AR: The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. American Journal of Public Health. 2007, 97:926–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manini TM: Mobility decline in old age: A time to intervene. Exercise and Sport Sciences Reviews. 2013, 41:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charles S, Carstensen LL: Social and Emotional Aging. Annual Review of Psychology. 2010, 61:383–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glass TA, Balfour JL: Neighborhoods, aging, and functional limitations. In Kawachi I and Berkman L (eds), Neighborhoods and health. Oxford, UK: Oxford University Press, 2003, 303–334. [Google Scholar]
- 19.Pew Research Center: In a recovering market, homeownership rates are down sharply for blacks, young adults. Retrieved October 18, 2017, from http://www.pewsocialtrends.org/2016/12/15/in-a-recovering-market-homeownership-rates-are-down-sharply-for-blacks-young-adults/
- 20.Berkman LF, Glass T: Social integration, social networks, social support, and health. Social epidemiology. 2000, 1:137–173. [Google Scholar]
- 21.Lawton MP, Nahemow L: Ecology and the aging process. 1973. [Google Scholar]
- 22.Eronen J, von Bonsdorff M, Rantakokko M, Rantanen T: Environmental facilitators for outdoor walking and development of walking difficulty in community-dwelling older adults. Eur J Ageing. 2014, 11:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keskinen KE, Rantakokko M, Suomi K, Rantanen T, Portegijs E: Nature as a facilitator for physical activity: Defining relationships between the objective and perceived environment and physical activity among community-dwelling older people. Health Place. 2018, 49:111–119. [DOI] [PubMed] [Google Scholar]
- 24.Latham K, Clarke PJ: Neighborhood Disorder, Perceived Social Cohesion, and Social Participation Among Older Americans: Findings From the National Health & Aging Trends Study. Journal of Aging and Health. 2018, 30:3–26. [DOI] [PubMed] [Google Scholar]
- 25.De Marco A, De Marco M: Conceptualization and measurement of the neighborhood in rural settings: A systematic review of the literature. Journal of Community Psychology. 2010, 38:99–114. [Google Scholar]
- 26.Singh GK, Siahpush M: Widening rural–urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. Journal of Urban Health. 2014, 91:272–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenberg PE, Fournier A-A, Sisitsky T, Pike CT, Kessler RC: The economic burden of adults with major depressive disorder in the United States (2005 and 2010). The Journal of clinical psychiatry. 2015, 76:155–162. [DOI] [PubMed] [Google Scholar]
- 28.Chapman DP, Perry GS: Depression as a major component of public health for older adults. Preventing Chronic Disease. 2008, 5:A22. [PMC free article] [PubMed] [Google Scholar]
- 29.Friedrich MJ: Depression is the leading cause of disability around the world. JAMA. 2017, 317:1517–1517. [DOI] [PubMed] [Google Scholar]
- 30.Jordan JM: An Ongoing Assessment of Osteoarthritis in African Americans and Caucasians in North Carolina: The Johnston County Osteoarthritis Project. Transactions of the American Clinical and Climatological Association. 2015, 126:77–86. [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau: 2010 Census Urban and Rural Classification and Urban Area Criteria. Retrieved October 17, 2017, from https://www.census.gov/geo/reference/ua/urban-rural-2010.html
- 32.Radloff LS: The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991, 20:149–166. [DOI] [PubMed] [Google Scholar]
- 33.Muñoz RF, Ying Y-W: The prevention of depression: Research and practice: JHU Press, 2002. [Google Scholar]
- 34.Edwards MC, Cheavens JS, Heiy JE, Cukrowicz KC: A Reexamination of the Factor Structure of the Center for Epidemiologic Studies Depression Scale: Is a One-Factor Model Plausible? Psychological Assessment. 2010, 22:711–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carleton RN, Thibodeau MA, Teale MJ, et al. : The center for epidemiologic studies depression scale: a review with a theoretical and empirical examination of item content and factor structure. PloS One. 2013, 8:e58067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ: Assessing depressive symptoms in five psychiatric populations: a validation study. American Journal of Epidemiology. 1977, 106:203–214. [DOI] [PubMed] [Google Scholar]
- 37.U.S. Census Bureau: Geographic Terms and Concepts - Block Groups. Retrieved Nov 28, 2017, from https://www.census.gov/geo/reference/gtc/gtc_bg.html
- 38.Sampson RJ, Raudenbush SW, Earls F: Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997, 277:918–924. [DOI] [PubMed] [Google Scholar]
- 39.Echeverria SE, Diez-Roux AV, Link BG: Reliability of self-reported neighborhood characteristics. Journal of Urban Health. 2004, 81:682–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mair C, Diez Roux AV, Shen M, et al. : Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the multiethnic study of atherosclerosis. Annals of Epidemiology. 2009, 19:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin KR, Shreffler J, Schoster B, Callahan LF: Associations of perceived neighborhood environment on health status outcomes in persons with arthritis. Arthritis Care & Research. 2010, 62:1602–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention: A Data Users Guide to the BRFSS Physical Activity Questions. Retrieved May 21, 2016, from http://www.cdc.gov/brfss/pdf/PA%20RotatingCore_BRFSSGuide_508Comp_07252013FINAL.pdf
- 43.Dean A, Lin N: The stress-buffering role of social support. Problems and prospects for systematic investigation. Journal of Nervous and Mental Disease. 1977, 165:403–417. [DOI] [PubMed] [Google Scholar]
- 44.O’Connor G, Fitzpatrick K: Do Place and Time Make a Difference? Examining Quality of Life Among Homeless Persons in Northwest Arkansas and Birmingham. Community Mental Health Journal. 2017, 53:334–339. [DOI] [PubMed] [Google Scholar]
- 45.De Vellis R, De Vellis BM, Sauter S, Harring K, Cohen J: Predictors of pain and functioning in arthritis. Health Education Research. 1986, 1:61–67. [Google Scholar]
- 46.Coty M-B, Wallston KA: Problematic social support, family functioning, and subjective well-being in women with rheumatoid arthritis. Women and Health. 2010, 50:53–70. [DOI] [PubMed] [Google Scholar]
- 47.Brown GK, Wallston KA, Nicassio PM: Social Support and Depression in Rheumatoid Arthritis: A One-Year Prospective Study. Journal of Applied Social Psychology. 1989, 19:1164–1181. [Google Scholar]
- 48.Israel BA, Checkoway B, Schulz A, Zimmerman M: Health education and community empowerment: conceptualizing and measuring perceptions of individual, organizational, and community control. Health Education Quarterly. 1994, 21:149–170. [DOI] [PubMed] [Google Scholar]
- 49.Taylor AW, Chittleborough C, Gill TK, et al. : Relationship of social factors including trust, control over life decisions, problems with transport and safety, to psychological distress in the community. Social Psychiatry and Psychiatric Epidemiology. 2012, 47:465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Taylor AW, Kelly G, Dal Grande E, et al. : Population levels of wellbeing and the association with social capital. BMC Psychol. 2017, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim J-R, Jeong B, Park K-S, Kang Y-S: Association of social capital at the individual level with physical activity in communities with high mortality in Korea. Health Promotion International. 2016:daw017. [DOI] [PubMed] [Google Scholar]
- 52.Neogi T, Zhang Y: Epidemiology of osteoarthritis. Rheumatic Disease Clinics of North America. 2013, 39:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bowen NK, Guo S: Structural equation modeling: Oxford University Press, 2011. [Google Scholar]
- 54.Anderson JC, Gerbing DW: Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988, 103:411. [Google Scholar]
- 55.Gunzler D, Chen T, Wu P, Zhang H: Introduction to mediation analysis with structural equation modeling. Shanghai archives of psychiatry. 2013, 25:390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fairchild AJ, McDaniel HL: Best (but oft-forgotten) practices: mediation analysis. American Journal of Clinical Nutrition. 2017, 105:1259–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jöreskog KG: A general approach to confirmatory maximum likelihood factor analysis. Psychometrika. 1969, 34:183–202. [Google Scholar]
- 58.Tucker LR, Lewis C: A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973, 38:1–10. [Google Scholar]
- 59.Bentler PM: Comparative fit indexes in structural models. Psychological Bulletin. 1990, 107:238–246. [DOI] [PubMed] [Google Scholar]
- 60.Steiger JH, Lind JC: Statistically based tests for the number of common factors. annual meeting of the Psychometric Society, Iowa City, IA: 1980. [Google Scholar]
- 61.Kline RB: Principles and practice of structural equation modeling: Guilford press, 2011. [Google Scholar]
- 62.Cabrera-Nguyen P: Author guidelines for reporting scale development and validation results in the Journal of the Society for Social Work and Research. Journal of the Society for Social Work and Research. 2010, 1:99–103. [Google Scholar]
- 63.Mason WA, Kosterman R, Haggerty KP, et al. : Gender moderation and social developmental mediation of the effect of a family-focused substance use preventive intervention on young adult alcohol abuse. Addictive Behaviors. 2009, 34:599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sawatzky R, Ratner PA, Johnson JL, Kopec JA, Zumbo BD: Self-reported physical and mental health status and quality of life in adolescents: a latent variable mediation model. Health Qual Life Outcomes. 2010, 8:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weden MM, Carpiano RM, Robert SA: Subjective and objective neighborhood characteristics and adult health. Social Science and Medicine. 2008, 66:1256–1270. [DOI] [PubMed] [Google Scholar]
- 66.Kegler MC, Alcantara I, Haardorfer R, et al. : Rural Neighborhood Walkability: Implications for Assessment. J Phys Act Health. 2015, 12 Suppl 1:S40–45. [DOI] [PubMed] [Google Scholar]
- 67.Pedhazur E: Multiple regression in behavioral research: Explanation and prediction . United States: Thomson Learning. Inc, 1997. [Google Scholar]
- 68.Ludwig J, Sanbonmatsu L, Gennetian L, et al. : Neighborhoods, obesity, and diabetes--a randomized social experiment. New England Journal of Medicine. 2011, 365:1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kweon B-S, Sullivan WC, Wiley AR: Green Common Spaces and the Social Integration of Inner-City Older Adults. Environment and Behavior. 1998, 30:832–858. [Google Scholar]
- 70.Hajna S, Ross NA, Joseph L, Harper S, Dasgupta K: Neighbourhood Walkability and Daily Steps in Adults with Type 2 Diabetes. PloS One. 2016, 11:e0151544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Prieto-Flores ME, Fernandez-Mayoralas G, Forjaz MJ, Rojo-Perez F, Martinez-Martin P: Residential satisfaction, sense of belonging and loneliness among older adults living in the community and in care facilities. Health Place. 2011, 17:1183–1190. [DOI] [PubMed] [Google Scholar]
- 72.Kearns A, Whitley E, Tannahill C, Ellaway A: ‘Lonesome town’? Is loneliness associated with the residential environment, including housing and neighborhood factors? Journal of Community Psychology. 2015, 43:849–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Harlow HF, Harlow M: Learning to love. American Scientist. 1966, 54:244–272. [PubMed] [Google Scholar]
- 74.Uchino BN: Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006, 29:377–387. [DOI] [PubMed] [Google Scholar]
- 75.Holt-Lunstad J, Smith TB, Layton JB: Social relationships and mortality risk: a meta-analytic review. PLoS Medicine. 2010, 7:e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Holt-Lunstad J: The Potential Public Health Relevance of Social Isolation and Loneliness: Prevalence, Epidemiology, and Risk Factors. Public Policy & Aging Report. 2017, 27:127–130. [Google Scholar]
- 77.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA: Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and Aging. 2006, 21:140. [DOI] [PubMed] [Google Scholar]
- 78.McNeill LH, Kreuter MW, Subramanian SV: Social environment and physical activity: a review of concepts and evidence. Social Science and Medicine. 2006, 63:1011–1022. [DOI] [PubMed] [Google Scholar]
- 79.Sallis JF, Bowles HR, Bauman A, et al. : Neighborhood environments and physical activity among adults in 11 countries. American Journal of Preventive Medicine. 2009, 36:484–490. [DOI] [PubMed] [Google Scholar]
- 80.Yen IH, Michael YL, Perdue L: Neighborhood environment in studies of health of older adults: a systematic review. American Journal of Preventive Medicine. 2009, 37:455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Strawbridge WJ, Deleger S, Roberts RE, Kaplan GA: Physical activity reduces the risk of subsequent depression for older adults. American Journal of Epidemiology. 2002, 156:328–334. [DOI] [PubMed] [Google Scholar]
- 82.Moore S, Daniel M, Bockenholt U, et al. : Associations among socioeconomic status, perceived neighborhood control, perceived individual control, and self-reported health. Journal of Community Psychology. 2010, 38:729–741. [Google Scholar]
- 83.Skinner EA, Zimmer-Gembeck MJ: Perceived control and the development of coping. The Oxford handbook of stress, health, and coping. 2011:35–59. [Google Scholar]
- 84.Dijkstra M, Homan AC: Engaging in rather than disengaging from stress: Effective coping and perceived control. Frontiers in Psychology. 2016, 7:1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.U.S. Census Bureau: Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Retrieved Dec 18, 2017, from https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf
- 86.Hoffman C, Rice D, Sung HY: Persons with chronic conditions. Their prevalence and costs. JAMA. 1996, 276:1473–1479. [PubMed] [Google Scholar]
- 87.Centers for Disease Control and Prevention: Healthy Places Terminology. Retrieved December 18, 2017, from https://www.cdc.gov/healthyplaces/terminology.htm
- 88.Wiles JL, Leibing A, Guberman N, Reeve J, Allen RES: The Meaning of “Aging in Place” to Older People. The Gerontologist. 2012, 52:357–366. [DOI] [PubMed] [Google Scholar]
- 89.Brown SC, Mason CA, Lombard JL, et al. : The relationship of built environment to perceived social support and psychological distress in Hispanic elders: the role of "eyes on the street". J Gerontol B Psychol Sci Soc Sci. 2009, 64:234–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.VanderWeele TJ: A unification of mediation and interaction: A 4-way decomposition (Vol 25, pg 749, 2014). Epidemiology. 2016, 27:E36–E36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Petersen ML, Sinisi SE, van der Laan MJ: Estimation of direct causal effects. Epidemiology. 2006:276–284. [DOI] [PubMed] [Google Scholar]
- 92.Preacher KJ, Zhang Z, Zyphur MJ: Alternative methods for assessing mediation in multilevel data: The advantages of multilevel SEM. Structural Equation Modeling. 2011, 18:161–182. [Google Scholar]
- 93.Hung WW, Ross JS, Boockvar KS, Siu AL: Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC Geriatrics. 2011, 11:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.