Summary
Weight stigma impacts negatively healthcare quality and hinders public health goals. The aim of this review was to identify strategies for minimizing weight bias among healthcare professionals and explore future research directions. An electronic search was performed in PubMed, PsycINFO and Scopus (until June 2020). Studies on weight stigma reduction in healthcare students, trainees and professionals were assessed based on specific inclusion and exclusion criteria. A narrative synthesis was undertaken to analyze emerging themes. We identified five stigma reduction strategies in healthcare: (i) increased education, (ii) causal information and controllability, (iii) empathy evoking, (iv) weight‐inclusive approach, and (v) mixed methodology. Weight stigma needs to be addressed early on and continuously throughout healthcare education and practice, by teaching the genetic and socioenvironmental determinants of weight, and explicitly discussing the sources, impact and implications of stigma. There is a need to move away from a solely weight‐centric approach to healthcare to a health‐focused weight‐inclusive one. Assessing the effects of weight stigma in epidemiological research is equally important. The ethical argument and evidence base for the need to reduce weight stigma in healthcare and beyond is strong. Although evidence on long‐term stigma reduction is emerging, precautionary action is needed.
Keywords: healthcare professionals, obesity stigma, weight bias
1. INTRODUCTION
Social stigma is a fundamental driver of population health inequalities. 1 Although this has been recognized for decades, 2 detrimental effects of the stigma of body size and weight have gained wider acknowledgement only recently. 3 Societal weight stigma is pervasive 4 , 5 and suggested to be in part driven by the increased blame and shame framing of obesity in media and public health, 6 , 7 , 8 the cultural reinforcement of a slim ideal 9 and proclivities for social stratification. 10 Between 2017 and 2020, weight shaming, a manifestation of weight stigma, decreased slightly in the United States, and although this is promising, blaming individuals with obesity saw little change in the United Kingdom. 11 However, there is substantive evidence to show that weight stigma is unfair and unjustified, it creates health disparities and hampers healthcare and public health efforts. 3 , 12
The stress of stigmatization, from direct experience, but also from stigma suspicion and anticipation, can elicit physiological, psychological and behavioral responses, which harm health over time. Studies show that weight stigma can negatively impact on cortisol, glycated hemoglobin, oxidative stress and C‐reactive protein, 13 as well as promote global dysregulation of lipid and glucose metabolism, and inflammation. 14 People with obesity experience weight stigma frequently, almost daily on average. 15 , 16 When compared with lower weight counterparts, those with measured or self‐perceived overweight have shown blunted cortisol responses to acute stressful stimuli, 17 suggestive of sustained elevated cortisol levels. This is consistent with prior research 18 , 19 , 20 showing that although acute stigmatizing stimuli is associated with cortisol reactivity, blunted cortisol responses are more common after persistent and severe chronic exposure to stressors, including weight‐related stigmatization, which often results in feelings of shame. 21 Although the relationship between adiposity and glucocorticoid dysregulation is complex and several other metabolic and genetic mechanisms have been suggested, 22 weight stigma has been found to contribute to the interindividual variation in stress response 23 among people with obesity. Jung et al. 23 showed that among people with body mass index (BMI) > 30 kg/m2, those with low levels of self‐stigma react to acute psychological stress as predicted with an increase in cortisol secretion, whereas those with medium or high self‐stigma show an atypical blunted cortisol response. When obesity was found to predict physiological dysregulation over a 4‐year period, 29% of this effect was explained by weight discrimination alone. 24 Furthermore, weight stigma is linked to psychological distress, depression, anxiety, 25 low self‐esteem, and body image disturbances, 13 often leading to decreased health motivation 16 and maladaptive coping such as avoidance of timely healthcare, social isolation, reduced physical activity and disordered eating behaviors. 26 Weight stigma has been shown to increase risk of developing obesity, 8 , 27 and it may shorten life‐expectancy, as it is associated with nearly 60% greater mortality risk, not accounted for by traditional physical and psychological risk factors. 28
Mounting evidence shows associations between weight stigma and increased food intake, eating in the absence of hunger, emotional eating, binge eating and long‐term weight gain. 29 , 30 , 31 Multiple experimental studies have shown that weight discriminatory experiences lead to decreased inhibitory control and increased caloric intake. 32 , 33 , 34 These eating behaviors are likely mediated by emotional distress and dysregulation 35 , 36 and should not be considered personal failings but maladaptive coping strategies to unfair treatment. 26 , 37 , 38 , 39 Furthermore, weight stigma is unique compared with other social stigmas, as prejudices tend to be accepted by people across the weight spectrum. 40 Internalized weight bias (IWB) encompasses self‐blame and self‐devaluation that results from endorsing negative social messages around weight and applying them to the self. 3 IWB is believed to explain the relationship between acutely experienced or indirectly perceived weight stigma and maladaptive eating behaviors 41 , 42 , 43 as well as body shame and dissatisfaction, exercise and healthcare behaviors, bodily pain and parental weight talk. 44 Stigma may lead to efforts of escaping discrimination through weight‐loss attempts, 45 and thus, some have argued that it may have a positive role in motivating individuals to engage in health behaviors. However, stigmatization creates a dual and countervailing effect of increasing motivation to engage in unhealthy weight‐control behaviors, while simultaneously decreasing the perceived capacity to control weight, 46 and is consistently linked to adverse health behaviors and decreased long‐term health. 47 , 48 , 49 Moralizing elicits an acute urge to defend one's moral identity, prompting responses that are perhaps visible, but not conducive of health. 50 Furthermore, while the moralized framing of weight common in healthcare may be done with the intention to motivate a desired behavior, it is most likely to have the opposite effect of disengagement and avoidance of said behavior. 50 Hunger et al. 38 have proposed a social identity threat model that elucidates the processes linking weight stigma and the cascade of mechanisms causing the deterioration of physical and psychological health, many of which are bidirectionally linked with eating behaviors. 51 Additionally, the cyclic obesity/weight‐based stigma (COBWEBS) model by Tomiyama 52 represents weight stigma as a positive feedback loop perpetuated by stigma‐induced increased cortisol and eating behaviors, which promote weight gain and thus further stigmatization.
Healthcare is one of the most common contexts where weight stigmatization occurs. 39 Physicians have been reported as the second most common source of weight stigma and discrimination. 39 Remmert et al. 29 found that over 70% of US adults enrolling in a weight loss programme report stigmatizing healthcare incidences. Similarly, Puhl et al. 53 found this proportion to be two thirds among adults in weight management programmes across six different countries. Furthermore, people with obesity are twice as likely to report healthcare discrimination compared with those at lower weight. 54 Extensive evidence highlights strong weight bias among healthcare professionals (HCP) including physicians, nurses, dietitians, psychologists, kinesiologists, students of these disciplines and even obesity specialists. 55 HCPs are unlikely to deliberately discriminate against their patients. For example, when measured by the Harvard Implicit Association Test, a validated measure of unconscious weight bias, most medical and nursing students exhibit stronger bias when compared with what they knowingly self‐report. 56 , 57 Notwithstanding, underlying negative attitudes can lead to enacted stigma, that is, social cues and behaviors that cause the recipient to feel devalued, disrespected or humiliated. Indeed, the majority of weight stigmatizing healthcare experiences reported by patients are not overt, but subtle. 29 These may include avoiding eye‐contact or physical touch, providing unsolicited or over‐simplified weight‐loss advice or not having appropriately sized equipment at hand. Biases behind enacted stigma can be explicit, referring to conscious beliefs, stereotypes and attitudes, or implicit, referring to unconscious and automatic processes. Explicit and implicit bias has been shown to lead to over‐attribution of health problems to weight, less time spent with patients and less patient‐centered, positive affective communication. 58 Additionally, patients with high IWB report greater healthcare avoidance, increased perceived judgement from doctors, lower frequency of obtaining routine check‐ups, less frequent listening and respect from providers, and lower quality healthcare. 53 Thus, unchecked weight bias among HCPs as well as IWB among patients potentially undermines successful diagnosis, treatment, and outcome. 59 , 60
Identifying widely applicable ways to effectively reduce healthcare related weight stigma is urgently needed. In addition to improving healthcare provision, and the health and well‐being of patients with obesity, healthcare that not only avoids, but actively addresses and reduces IWB may help patients better cope with and reduce the effects of stigma until it is minimized in society. Not surprisingly, while stigmatizing does the opposite, 16 , 61 empathetic, non‐stigmatizing weight‐related communication can increase patients' health motivation and intention to comply with health professionals' advice. 62
A recent joint international consensus statement from leading health authorities has called for the elimination of weight stigma, 3 a process essential to achieving public health goals globally. Addressing negative biases in the healthcare community will help advocate for a culture and society where the respect, dignity and care afforded to each person is not dependent on their body weight. Stigma reduction interventions are a current research priority. 27 However, there is a paucity in agreed‐upon, effective and practical strategies to target weight‐related prejudice, which contributes to a lack of strategic anti‐stigma actions. Therefore, the aim of this review was to systematically evaluate current knowledge on strategies for minimizing weight bias in healthcare professionals and to identify future research directions.
2. MATERIALS AND METHODS
2.1. Literature search
A systematic strategy was used to identify weight stigma studies related to healthcare settings and eating behaviors. An electronic search was performed in three online databases (PubMed, PsycINFO and Scopus) from their inception until June 2020. Combinations of the following keywords were used in all databases: “weight bias,” “weight stigma,” “weight discrimination,” “obesity bias,” “obesity stigma,” “obesity discrimination” or “anti‐fat bias”; and “healthcare” or “quality of care,” or “food choice,” “food intake,” “food behav*,” “dietary intake,” “dietary choice” or “eating behav*”. The search strategy was adapted to each database by using additional subject headings in PubMed and PsycINFO. We included papers written in English language and involving human participants. Bibliographies of all included studies were searched manually to identify any literature not retrieved by the main search.
2.2. Study eligibility and selection
Studies looking at ways to reduce weight stigma in HCPs were assessed. Inclusion criteria included participants who were healthcare professionals, trainees or students and interventional study designs. Studies were excluded when there was no measurement of effects on stigma. Review papers and observational studies were also excluded. Figure 1 illustrates the selection process in more detail.
FIGURE 1.
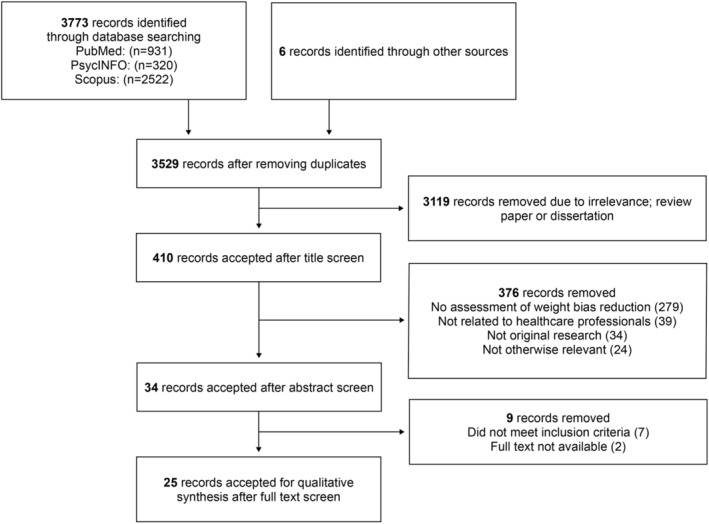
Flow diagram of studies retrieved and included in the scoping review
2.3. Data extraction and synthesis
For all eligible studies, a standardized data extraction table was used to extract data on study authors and year; population and country; intervention type and duration; outcome measures and principal findings. A narrative synthesis was undertaken to identify and analyze emerging themes.
3. RESULTS
3.1. Key characteristics
The initial search identified a total of 3773 records. A total of 25 interventional studies were included in this review from which seven were randomized controlled trials, four were controlled trials and 14 used a pre‐post intervention design. Three trials included HCPs, two included healthcare trainees, 19 included students, and one trial included both professionals, trainees and students, with a total of 3554 participants across all studies. The duration of studies varied from less than 1 day to 3 years. A summary of studies in healthcare professionals, trainees, and students (Table 1) is presented below. A narrative analysis revealed five major strategies: (i) increased education, (ii) causal information and controllability, (iii) empathy evoking, (iv) weight‐inclusive approach, and (v) mixed methodology. Results are presented below according to these strategies.
TABLE 1.
Summary of studies in healthcare professionals, trainees, and students
| Study | Population | Design | Intervention type and duration | Outcome measure | Main findings |
|---|---|---|---|---|---|
| Increased education | |||||
| Barra and Singh Hernandez (2018) | Nursing students (n = 103), USA | Pre‐post intervention | Weekly obesity sensitivity training (15 week) on weight‐based discrimination | Newly constructed 5‐item, 4‐point Likert scale questionnaire | Attitudes improved on all five items of the questionnaire |
| Gayer et al. (2017) | Medical students (n = 718), USA | Controlled trial | Standard obesity curriculum (8–10 h of lectures, virtual patient case presentations) | FPS | Stereotyping decreased (FPS: 3.65 vs. 3.37) and remained significant at 3‐year follow‐up |
| Geller et al. (2018) | Medical students (n = 59), USA | Pre‐post intervention | Ethics seminar within “Obesity, Nutrition, and Behaviour Change” course discussing personal experiences and weight bias norms | IAT, survey | 74% had high implicit bias; 4 months post‐intervention, attitudes improved in 30%, did not change in 53%, and worsened in 10% |
| Jones et al. (2019) | Physiotherapists (n = 27), Canada | Pre‐post intervention | Seminar (8 h) on obesity and osteoarthritis presented by respected opinion leaders | ATOP, BAOP | Beliefs improved (BAOP: 7.4 vs. 22.3), but attitudes towards people with obesity worsened (ATOP: 71.3 vs. 63.5) |
| Nickel et al. (2019) | Physicians, nurses, medical students and nursing trainees (n = 702), Germany | Randomized controlled trial | Video teaching (2.5 min) on obesity disease burden and treatment | FPS | Stereotyping did not change when compared with control group in physicians (FPS: 3.5 vs. 3.5), nurses (FPS: 3.3 vs. 3.3), medical students (FPS: 3.5 vs. 3.6) nor nursing students (FPS: 3.4 vs. 3.4) |
| Causal information and controllability | |||||
| Brochu (2020) | Psychology trainees (n = 45), USA | Pre‐post intervention | Seminar (3 h) on weight controllability and weight bias, informed by attribution‐value model of prejudice and HAES | AFA‐willpower, AFA‐dislike, attitudes toward fat clients | 1‐week post‐intervention, weight controllability beliefs (AFA‐willpower: 4.46 vs. 3.39) and attitudes (AFA‐dislike: 2.36 vs. 2.10) improved |
| Diedrichs and Barlow (2011) | Psychology students (n = 85), Australia | Controlled trial | Lecture (2 h) on behavioral, or multiple causes of obesity and weight bias, informed by HAES | AFAT | Beliefs and attitudes improved and remained significant at 3‐week follow‐up (AFAT: 2.18 vs. 2.04 vs. 2.00) |
| O'Brien et al. (2010) | Health promotion students (n = 159), USA | Randomized controlled trial | Weekly tutorials (3 week) on genetic/socioenvironmental causes of obesity, oral presentation, and written assignment | AFA, BAOP, pen and pencil version of IAT | Beliefs worsened (AFA‐willpower: 4.4 vs. 5.1) and improved (BAOP: 23.8 vs. 20.5), and attitudes (AFA‐dislike: 2.1 vs. 1.7) and implicit bias improved (IAT‐good/bad: 14.2 vs. 10.3, IAT‐lazy/motivated: 11.0 vs. 9.7) in gene/environment group; implicit bias worsened in diet/exercise group (IAT‐good/bad: 14.0 vs. 14.4, IAT‐lazy/motivated: 10.3 vs. 13.1) |
| Persky et al. (2010) | Medical students (n = 110), USA | Randomized controlled trial | Reading short article, clinical encounter via immersive virtual environment | Newly constructed single‐item questionnaire, OPTS | Beliefs improved and stereotyping decreased in genetics group compared with control (OPTS: 3.55 vs. 3.69); stereotyping did not change in behavioral group (OPTS: 3.75) compared with genetic and control groups |
| Empathy evoking | |||||
| Cotugna et al. (2010) | Dietetics students (n = 40), USA | Pre‐post intervention | Following a calorie‐restricted diet (1 week) | FPS, newly constructed questionnaire, journal entries | Stereotyping decreased (t = 3.184, p < 0.05) significantly |
| Harris et al. (1991) | Psychology students (n = 244), USA | Randomized controlled trial | Reading high status or empathy evoking interview with person with obesity together with or without interview with obesity expert | Newly constructed 18‐item, 7‐point Likert scale questionnaire | No changes in attitudes were seen in any of the groups |
| Hunter et al. (2018) | Nursing students (n = 29), UK | Pre‐post intervention | Wearing a bariatric empathy suit (30 min) | NATOOPS, focus group | Some attitudes (NATOOPS‐1: 25 vs. 33, NATOOPS‐2: 64 vs. 82, NATOOPS‐5: 56 vs. 64) improved, but beliefs and stereotyping did not change |
| Kushner et al. (2014) | Medical students (n = 127), USA | Pre‐post intervention | Reading and reviewing two weight stigma articles, clinical encounter (8 min) with standardized patients with overweight, case observations | Newly constructed questionnaire | Empathy increased in 48% and decreased in 23%; stereotyping decreased in 53% and increased in 33%; at 1‐year follow‐up, empathy remained significant, but stereotyping regressed to back to the baseline mean |
| Matharu et al. (2014) | Medical students (n = 129), USA | Randomized controlled trial | Dramatic reading (1 h) of a play script titled “The Most Massive Woman Wins,” nondirective group discussion | AFA, IAT, JSPE, two open‐ended questions | Empathy increased in both groups; attitudes improved only in intervention group (AFA: 42.6 vs. 38.1); implicit bias did not improve (IAT: 0.44 vs. 0.38) |
| Molloy et al. (2016) | Nursing students (n = 70), USA | Pre‐post intervention | Bariatric sensitivity training (1 h) using 6 trigger films (<4 min) with facilitated group debriefing | BAOP, NATOOPS | Beliefs (BAOP: 16.4 vs. 19.0) and some attitudes (NATOOPS‐2: 543 vs. 649, NATOOPS‐3: 515 vs. 452, NATOOPS‐4: 66 vs. 61) improved; at 30‐day follow‐up, beliefs remained significant (BAOP: 18.2), some attitudes (NATOOPS‐1: 571) reverted back |
| Weight‐inclusive approach | |||||
| McVey et al. (2013) | Health promoters (n = 325), Canada | Pre‐post intervention | Interactive workshop on weight bias, intuitive eating, weight‐centric health messaging and mental health promotion, informed by HAES | AFA, SATAQ, semi‐structured interview | Attitudes (AFA: 33.8 vs. 23.99 vs. 25.18) and internalization of sociocultural stereotypes (SATAQ: 13.61 vs. 11.48 vs. 12.28) improved and remained significant at 6‐week follow‐up |
| Werkhoven (2020) | Healthcare students (n = 124), Australia | Pre‐post intervention | Weekly lectures and tutorials (12 week) focusing on nutrition and stigma reduction, informed by HAES | AFA, FSQ, focus group | Attitudes improved (AFA: 47.0 vs. 43.1); stereotyping decreased (FSQ: −0.32 vs. − 0.24, p > 0.05) |
| Mixed methodology | |||||
| Falker et al. (2011) | Health professionals (n = 30), USA | Pre‐post intervention | Self‐learning bariatric sensitivity training (44 pg) aiming to evoke empathy, addressing multiple causes of obesity and weight stigma | Newly constructed survey | Self‐reported attitudes towards patients with obesity improved |
| Luig et al. (2020) | Medical residents (n = 32), Canada | Pre‐post intervention | Lectures with bariatric empathy suit experience, clinical encounter, narrative reflections | ATOP, BAOP, reflective writing | Beliefs improved (BAOP: 19.86 vs. 24.03), but attitudes did not improve (ATOP: 73.15 vs. 69.26) |
| Poustchi et al. (2013) | Medical students (n = 64), USA | Pre‐post intervention | Video (17 min) titled “Weight Bias in Health Care,” interactive discussion | ATOP, BAOP, FPS | Beliefs (BAOP: 16.53 vs. 19.27) and stereotyping (FPS: 3.65 vs. 3.45) improved; attitudes did not improve (ATOP: 66.14 vs. 64.90) |
| Swift et al. (2013) | Nutrition students (n = 43), UK | Randomized controlled trial | Two videos (34 min) titled “Weight Prejudice: Myths and Facts” and “Weight Bias in Healthcare” | Willpower and dislike subscales of AFA, BAOP, FPS, IAT | Beliefs (BAOP: 11.2 vs. 19.9, AFA‐willpower: 5.42 vs. 3.88), attitudes (AFA‐dislike: 1.86 vs. 1.45) and stereotyping (FPS: 3.7 vs. 3.2) improved; implicit bias did not change (IAT‐good/bad: 3.8 vs. 2.7, IAT‐lazy/motivated: 4.5 vs. 2.6); at 6‐week follow‐up, changes in beliefs remained significant (BAOP: 13.7, AFA‐willpower: 4.63), but attitudes (AFA‐dislike: 1.57) and stereotyping (FPS: 3.6) did not |
| Rukavina et al. (2008) | Kinesiology students (n = 69), USA | Pre‐post intervention | Multicomponent intervention including lecture (75 min), group activity and service‐learning project | AFAT, ERT | Beliefs improved (AFAT‐blame: 3.2 vs. 3.41, AFAT‐physical: 3.17 vs. 3.21, AFAT‐social: 4.1 vs. 4.1), but attitudes and stereotyping did not change |
| Rukavina et al. (2010) | Kinesiology students (n = 78), USA | Controlled trial | Multicomponent intervention including interactive discussions, audio tape listening, perspective taking, role‐playing and service‐learning project | AFAT, IAT, ERT | Beliefs about controllability (AFAT‐blame 2.88 vs. 2.59) and social value (AFAT‐social: 2.04 vs. 1.97) improved; attitudes, stereotyping and implicit bias did not change |
| Wiese et al. (1992) | Medical students (n = 75), USA | Randomized controlled trial | Seminar (2 h) including video, reading article about genetic causes of obesity, role‐playing, reflective writing | Newly constructed questionnaire | Beliefs, attitudes and stereotyping improved; at 1‐year follow‐up, changes in beliefs and stereotyping remained significant |
| Wijayatunga et al. (2019) | Kinesiology students (n = 67), USA | Controlled trial | Lecture (80 min), video, empathy‐evoking group activities and reflective writing | AFAT, IAT | Beliefs improved and remained significant at 4‐week follow‐up (AFAT‐blame: 2.79 vs. 2.43 vs. 2.40, AFAT‐physical: 2.59 vs. 2.63 vs. 2.53, AFAT‐social: 1.72 vs. 1.77 vs. 1.76); implicit bias did not change significantly (0.55 vs. 0.91) |
Abbreviations: AFA, Anti‐Fat Attitudes Questionnaire; AFAT, Anti‐Fat Attitudes Test; ATOP, Attitude Towards Obese Persons; BAOP, Beliefs About Obese Persons; ERT, Explicit Rating Test; FPS, Fat Phobia Scale; FSQ, Fat Stereotypes Questionnaire; HAES, Health at Every Size; IAT, Implicit Attitude Test; JSPE, Jefferson Scale of Physician Empathy; NATOOPS, Nurses Attitudes Towards Obesity and Obese Patients Scale; OPTS, Obese Persons Trait Survey; SATAQ, Sociocultural Attitudes Towards Appearance Questionnaire.
3.2. Reducing weight stigma among healthcare professionals and students
3.2.1. Increased education
Literature on medical education suggests that HCPs feel inadequate in caring for patients with obesity. 63 Negative attitudes towards people with overweight or obesity may be shaped by experiences with poor treatment success, patient non‐adherence and poor long‐term outcome data that result from inadequate knowledge and skills. A possible solution has been to develop educational programmes on obesity and weight‐related health. 64 Five studies used strategies based upon increasing knowledge of obesity in both students 65 , 66 , 67 and HCPs. 68 , 69
The first study used a brief 2.5‐min video that focused on the etiology and treatment of obesity and showed no influence on weight bias in medical students, nurse trainees, nurses or physicians. 69 In contrast, a comprehensive obesity curriculum delivered to medical students over 3 years did show small, but significant reductions in bias as assessed by the Fat‐Phobia Scale questionnaire; this was maintained at 1‐year follow‐up. 66 However, resulting values still indicated moderate amounts of weight bias and the clinical relevance of this change is unclear.
Three of the educational studies highlighted a social influence component, 65 , 67 , 68 which is the idea that social factors have a strong impact on people's beliefs and attitudes. 70 Accordingly, Jones et al. 68 trialed an 8‐h educational seminar on obesity and osteoarthritis among physiotherapists. The seminar was delivered by respected obesity experts and opinion leaders and the content centered around the complex causes and complications of obesity. Although results showed moderate improvements in beliefs about weight controllability, negative attitudes increased after the seminar. The authors noted that seminar discussions tended to focus on practical and safety considerations, which might have contributed to worsening of attitudes by emphasizing the difficulties of working with patients with obesity. Geller et al. 67 studied the impact of an ethics seminar embedded within a standard obesity, nutrition and behavior change course. The session revolved around group discussions on the personal experiences (74% struggled with their weight) and social norms (70% showed a thin‐preference on the Implicit Attitudes Test among students). Four months after course completion, 30% of students self‐reported improved attitudes, 53% reported no change and 10% reported more negative attitudes. Barra and Singh Hernandez 65 trialed a 15‐week medical practicum and obesity sensitivity training in nursing students. The education was supported by weekly exchange of ideas on weight bias and its effects on patient care, with results showing a decrease in negative attitudes and many students articulated awareness and remorse regarding their bias. Based on Lewin's theory of planned change, 71 the intervention involved the identification and correction of old behaviors and the planning and executing of new ones, aiming to establish a new status quo, which was later observed in students' improved communication style.
Cross‐sectional data suggest that increased general education and a deeper understanding of obesity alone is likely to be insufficient for reducing weight stigma 72 and in contrast, bias may actually increase as a result. 73 This may be due to the enforcement of and further socialization to weight stigma norms that are commonly expressed in health‐related education and working environments. 74 The degree of social influence is dependent on the clarity of social norms expressed by group members, 70 and thus, even a single person, such as faculty role models, 75 can have immediate and long‐term effects on student's views and opinions on obesity. The implicit and explicit communication of social norms in educational interventions warrants careful attention, given the possibility of changing bias in both directions. Another possible explanation for the lack of stigma reduction through increased knowledge relates to the content of standard obesity education, which tends to discuss weight from an individualized and medicalized perspective. 76 Indeed, focusing on individual behaviors as drivers of and as solutions to weight‐related health has been show to increase implicit bias in previous studies. 77 Therefore, health education needs improvement perhaps not only through the introduction of broader uncontrollable determinants of weight, but also through discussions of the harm caused by social and cultural norms and messages concerning body weight. Opportunities to practice non‐stigmatizing care throughout the education may further support this aim. This may be achieved with inclusive imagery and medical instruments as well as positive patient interactions.
3.2.2. Causal information and controllability
In line with attribution theory, weight bias is arguably shaped by beliefs about the controllability, and thus responsibility, over body weight. Implying that weight is under an individual's control elicits blame, giving justifications to stigmatizing beliefs and stereotypes. Although attributions of behavioral causes of obesity have been shown to predict stronger weight bias, 77 , 78 genetic determinism has been shown to decrease bias. 79 As such, investigators have looked to reduce stigma by changing beliefs about an individual's control over their body weight. Four trials in healthcare students investigated the effects of providing causal information, focusing on the genetic and/or socioenvironmental determinants of weight. 80 , 81 , 82 , 83
Reading about the genetic determinants of body weight before a virtual clinical encounter led to reduced controllability beliefs when compared with reading about behavioral determinants, or reading nothing. 83 Negative stereotyping reduced in the genetic condition when compared with control, but not when compared with the behavioral condition. However, students who received genetic information gave patients less health screening advice, possibly indicating the need for filling in the gap in health communication knowledge when weight‐loss advice is not the central focus to care. Diedrichs and Barlow 81 investigated the effects of 2‐h lectures, which focused either on the multiple determinants or only behavioral determinants of obesity. The multiple determinants lecture involved a detailed study of the empirical evidence demonstrating the multifactorial and uncontrollable nature of weight, as well as practical strategies for avoiding weight stigmatization and promoting Health at Every Size (HAES) principles with patients and in research. Post‐intervention and at 3‐week follow‐up, students who received the multiple determinants lecture showed fewer negative beliefs and attitudes towards people with obesity. The behavioral determinants lecture, following standard curriculum and aiming to increase knowledge about risk factors and treatments of obesity, did not reduce students' beliefs nor attitudes. Notably, the control group, who received no lecture, showed significant increase in social disparagement of people with obesity at both timepoints. However, this should be interpreted with caution as baseline levels of disparagement were significantly lower in this group and the increase in bias may reflect regression to the mean. In another study, three weekly tutorials that presented research on the uncontrollable determinants of weight were successful in improving measures of explicit and implicit attitudes, whereas tutorials focusing on behavioral determinants showed an increase in negative implicit attitudes. 82 However, although beliefs about controllability decreased when presenting genetic/environmental information, this was not found to be a mediating factor for attitudes in this study. Although post hoc tests revealed a decrease in the dislike subscale of anti‐fat attitudes in the genes/environment group, scores in the willpower subscale, indicating attribution of blame, increased. This, the authors explain, might have been due to regression to the mean, but could also reflect stable beliefs that people with obesity should lose weight regardless of the level of controllability and thus they must require high levels of willpower to overcome any barriers.
When teaching from a weight‐centric perspective, causality interventions may unwittingly reinforce negative values towards higher weight. The attribution‐value model of prejudice adds that social bias increases when, in addition to responsibility, the stigmatized characteristic is negatively valued. 84 This model was applied by Brochu 80 who investigated the effects of a 3‐h seminar, addressing weight controllability beliefs, plus negative attitudes and size acceptance. There was a strong emphasis on social justice, decreasing the negative value of overweight and obesity and encouraging a weight‐inclusive paradigm. Measured 1‐week post‐intervention, the seminar was successful in reducing dislike and negative attitudes toward people with obesity. Mediation analysis showed that the reduction in weight controllability beliefs explained these results. However, due to absence of control group, these results should be considered preliminary.
Although studies manipulating controllability beliefs in the general population have yielded mixed efficacy in reducing stigma, 85 studies in healthcare populations are encouraging. This may be a reflection of the science literacy of this population. Previous studies have found that people in the general population may not believe briefly presented genetic information about obesity. 77 Even a third of medical students in the genetics group in the study by Persky and Eccelston 83 showed “mis‐match” responses. Although it is not clear as to why this was the case, it might reflect strongly held beliefs that weight is a personal responsibility pertinent to the clarity, persuasiveness and depth of the information being presented. However, healthcare students and professionals may be more willing to change their views on weight controllability if new information is delivered together with weight‐inclusive health promotion strategies that may improve health regardless of weight status. Thus, when aiming to educate individuals on weight controllability, it is imperative that the information is clear and convincing and delivered in depth.
3.2.3. Empathy evoking
Empathy, the ability to understand the lived experience of another and to communicate that understanding, 86 is essential to effective therapeutic care. 87 Empathy‐evoking interventions aim to change attitudes and reduce weight stigma by increasing acceptance and liking of individuals with obesity. 88 Additionally, limited evidence suggests that in general, weight‐biased attitudes are more easily influenced compared with weight‐biased beliefs. 88 Although beliefs are often rooted in various personal experiences, available information and knowledge, and are measured via questions on the causes of body weight, attitudes arise from core values and feelings, and are measured via questions on what other people are like, what they can do and how they should be treated. Six studies have investigated the effects of evoking empathy as a strategy to reduce weight stigma. 89 , 90 , 91 , 92 , 93 , 94
Reading about weight stigma, followed by a brief 8‐min interaction with a patient led to significant improvements in empathy and stereotyping in medical students. 92 However, at 1‐year follow‐up, while empathy remained, negative stereotyping reverted back to the baseline mean. In another study where participants read an interview with a person with obesity, designed to evoke either status or empathy and coupled with or without an interview with an obesity expert, no significant changes occurred in any condition. 90 Reading the expert interview did increase participants' knowledge of obesity, but this did not contribute to changes in attitudes.
Molloy et al. 94 showed nursing students six 4‐min videos, depicting stigmatizing and emotive patient scenarios. Beliefs and negative attitudes decreased significantly post‐intervention. However, at 30‐days follow‐up, attitudes regarding negative feelings towards, the characteristics of, and supportive roles in caring for patients with obesity reverted back to the baseline mean. Furthermore, although weight‐biased beliefs in this cohort improved and changes remained significant after follow‐up, scores were still reflective of unacceptable levels of bias as assessed by the Beliefs About Obese Persons questionnaire. Similarly, in another study in nursing students, wearing a bariatric empathy suit for 30‐min reduced negative attitudes in three of five weight bias measurement domains. 91 In a post‐intervention focus group, students described the experience as “hard,” “feeling trapped,” and “embarrassing,” and later recognized that caring for patients with obesity can be “emotionally draining” and “stressful.” No follow‐up was done, and how this impacted weight stigma in the long‐term is unknown. Furthermore, others have argued that if empathy‐building is not possible without wearing a costume to assume a stigmatized identity, then doing so will be unlikely to be meaningful 95 because there is a notable proportion of individuals in whom empathy‐building interventions produce paradoxical effects. 85 People who respond better to this method on the other hand will be able to see that effect using less debatable methods.
Matharu et al. 93 used dramatic play reading to promote active empathic engagement in medical students. This was compared with a standard 1‐h lecture on the medical management of obesity. Empathy increased in both groups similarly, but attitudes improved significantly only in the theatre group, whereas implicit bias remained unchanged in both. Given that empathy increased similarly in both groups, it is possible that the decreased reporting on explicit attitudes was influenced by social desirability because the discriminatory nature of weight bias was made salient only in the theatre group. Moreover, after 4 months, a follow‐up survey revealed that students in the theatre group did not show increased recognition of weight stigma as something that needed to be addressed in society. However, they were more likely to take a patient‐centered approach to obesity care, whereas students receiving the standard lecture were more likely to take a prescriptive approach and recommend weight loss and exercise. Finally, to increase reflective skills and reduce healthcare students' negative attitudes, Cotugna et al. 89 had dietetic and health promotion students follow a 1 week 1200–1500 kcal diet, commonly prescribed in weight management. In journal comments, students expressed their difficulty dealing with hunger and social events with 35% not being able to successfully restrict their calories. Limited post‐intervention results showed self‐reported increases in empathy and a significant reduction in negative stereotyping.
The utility and long‐term effects of empathy‐evoking interventions in healthcare populations is unclear. Research shows that empathy does not necessarily decrease weigh stigma. 85 , 96 Daníelsdóttir et al. 85 have argued that evoking empathy is ineffective when it emphasizes the negative aspects of obesity, which reinforces stereotypes of helplessness and weakness. They suggested that rather than eliciting pity, a more constructive aim might be to emphasize size acceptance, respect and the human right for dignity. Size acceptance may be an effective strategy for both HCPs and patients, as accepting one's size, including when living with obesity, has shown to reduce stigma in others. 97
3.2.4. Weight‐inclusive approach
Concerns over the long‐term ineffectiveness 98 , 99 and unintentional negative consequences, 100 , 101 including stigmatization, of the dominant weight‐centric health paradigm have drawn research attention to weight‐inclusive approaches. 102 , 103 , 104 The weight‐inclusive approach differs from other approaches in this review by not operating from a priori assumptions that weight loss is achievable, beneficial, safe and necessary for everyone with higher weight. Two interventions 105 , 106 focused on a weight‐inclusive approach to health and combined this with weight bias awareness.
A full‐day interactive professional development workshop decreased anti‐fat attitudes and internalized weight stereotypes in health practitioners, which remained significant at 6‐week follow‐up. 105 The workshop discussed the potential downfalls of weight‐centric healthcare, and taught principles of intuitive eating and mental health promotion. The educational component was supported by salience of stigma reduction goals e.g. one activity included writing weight‐based stereotypes on paper and later tearing it up, symbolizing awareness and rejection of such beliefs. In a post‐intervention survey, the participants described the workshop materials as “credible, current, and evidence‐based.” Although still significant, results at follow‐up started to drift, suggesting the need for continuing long‐term support. This was voiced by the participants in follow‐up interviews as well. Werkhoven 106 investigated an undergraduate nutrition elective taught from a HAES perspective. A 12‐week curriculum with 3‐h of lectures, tutorials and practical group activities each week led to a strong increase in nutrition knowledge and a moderate decrease in all measured domains of anti‐fat attitudes as assessed by the Anti‐fat Attitudes Questionnaire. 106 Stereotyping as assessed by the Fat Stereotypes Questionnaire also decreased, but the result did not reach significance. For both measures, post‐intervention levels reflected a low degree of weight bias.
One way in which adopting a weight‐inclusive paradigm may reduce weight bias is by framing obesity not only as a medical and public health issue, but a human rights issue, emphasizing that all individuals, regardless of weight status, deserve dignity and have the right to equal quality healthcare. 107 Another way is by advocating for size diversity and acceptance, 97 , 108 supported by research demonstrating that health promotion is not necessarily dependent on weight loss. 109 , 110 Focusing on modifiable health behaviors rather than weight may help build better provider‐patient relationships by empowering both parties. Although results from current studies are promising, conclusions are limited by absence of controlled studies and further research is needed.
3.2.5. Mixed methodology
It may be that due to the complex nature of bias formation, a combination of established as well as other strategies are required. Eight interventions utilized a mix of various methods, mostly causal information, empathy evoking and stigma awareness raising. With most interventions being delivered in lecture or tutorial format, with or without additional video, reflective writing or role‐play components.
Two interventions combined general education and causal information. 111 , 112 A self‐learning online module, designed to address the multiple causes of obesity and increase awareness of weight stigma, was shown to decrease the likelihood of stigmatizing attitudes in HCPs 1‐month after completion. 111 However, results were based on participants' subjective evaluation of their awareness and attitudes of obesity, bearing risk of social desirability bias. Luig et al. 112 assessed a pilot course aiming to improve family medicine residents' knowledge and confidence with obesity counselling. The program focused on general knowledge and counselling skills, but combined lectures with a bariatric empathy suit experience and reflective writing. Weight stigma was not explicitly addressed in the course. Although the residents' beliefs about the causes of obesity improved, negative attitudes towards people with obesity remained high.
Two interventions had participants watching one (17‐min) 113 or two (totaling 34‐min) 114 anti‐stigma videos produced at Yale University. The videos employed strategies of weight controllability, empathy evoking and stereotype countering. Beliefs and stereotypes towards people with obesity improved in both trials. Attitudes improved only in the study by Swift et al. 114 Furthermore, Swift et al. 114 had a 6‐week follow‐up in which improved beliefs remained significant, whereas attitudes retreated back to baseline. Implicit bias did not change at any point. In both interventions, the video(s) were positively rated by both faculty and students. Still, given that attitudes did not change or started to drift with time, such brief interventions may benefit from repeated exposure, practical activities and facilitated discussions. Poustchi et al. 113 had participants engage in discussion after the viewing but the conversation was focused on participants' experiences encountering patients with obesity, which might have contributed to the unchanged attitudes by negative value attributions. Anticipating and focusing on the narrative of the “difficult patient” has been shown to increase weight bias in medical students. 115 Thus, not all discussions and activities around stigma are conducive to its reduction.
Two studies used lectures combined with video, articles, role‐play and reflective writing. 116 , 117 Both aimed to change controllability beliefs and evoke empathy and in both studies stereotyping decreased, whereas beliefs and attitudes improved according to some, but not all subscales. These changes remained significant at both 4‐week and 1‐year follow‐up. Wijayatunga et al. 117 found that participants exhibited high implicit weight bias, which remained unchanged. Importantly, a control group, who received a traditional obesity curriculum centering exercise and diet in weight management, was more likely to show increased implicit bias at 4‐week follow‐up. 117
Finally, two studies in kinesiology students combined lectures, addressing the multi‐factorial determinants of weight and the prevalence and effects of weight stigma, with empathy‐evoking activities and an additional field‐based service‐learning project. 118 , 119 In both, beliefs about controllability improved, but attitudes and stereotypes did not. Contrary to test scores, reflective writing revealed that many students had strong beliefs about personal control over weight. 118 This somewhat higher resistance to change may relate to the field of study, as exercise science related disciplines tend to focus on physique and thinness. 120 Rukavina et al. 119 also measured implicit bias, which improved, but did not reach significance and thus, remained strong among the students. Again, explicit bias increased in the control group taking other classes, highlighting the possible accumulating negative effects of not addressing weight stigma in health education. 119
There is a lack of evidence to suggest that using either single or multiple methods is better for reducing weight stigma. 121 Most mixed methods interventions in this review were successful in changing participants' beliefs about the uncontrollable causes of obesity and in reducing blame. However, changing attitudes and implicit bias remained a challenge. Future studies that can better quantify the effects of and interactions between single approaches within a context of mixed methodology are needed. This could mean studying parallel groups with increasing number of methods or taking a stepped approach in which non‐responders receive a different type of intervention.
4. LIMITATIONS
Given that research regarding strategies to reduce weight stigma is currently preliminary, a narrative analysis was favored in this review to allow for discussion of emerging themes. To overcome selection bias that may characterize a traditional narrative review, a systematic database search was performed; however, there was no standardized quality assessment of the individual studies, which may reduce the strength of conclusions. Furthermore, this review focused on weight stigma reduction in HCPs, which aims to avoid future stigmatization in the healthcare setting. Although outside the scope of this study, it is important to note that many patients across the weight spectrum experience IWB, 122 which has the potential to interfere with the patient‐provider relationship regardless of the level of bias and behavior of the professional. The role of HCPs in detecting and helping to reduce IWB in patients, especially in weight management services, deserves more attention.
5. CONCLUSIONS
This review looked at weight stigma reduction strategies in healthcare. Interventions involving the reduction weight bias among current and future HCPs were included. Although still more research is needed, the growing interest in weight stigma is encouraging. Around half of the studies included in this review were conducted in the past 5 years alone, providing valuable insight as we start taking broad action towards eradicating weight bias in healthcare and in society. Based on our findings, we offer three prime recommendations for stigma reduction pertaining to health education, practice and research.
First, there is a need to educate all healthcare students about the complex factors regulating body weight and address weight stigma, its prevalence, origins and impact, explicitly. The failure to address stigma among current and future HCPs upholds bias formation. Our findings show that biomedical education alone does not reduce stigma and, in most studies, control groups, when included, exhibited increased bias over time. Targeting healthcare students early on and throughout their education may be particularly beneficial because they are in the process of forming their beliefs and attitudes toward overweight and obesity, and may be more receptive to new paradigm‐shifting information. Indeed, a meta‐analysis on the malleability of weight bias by Lee et al. 88 found that effect sizes, although not statistically significant, were considerably larger in student samples compared with professionals or trainees. While there were only four studies involving HCPs in this review, the results support this notion. Therefore, revisions to current healthcare curricula are welcomed, accounting for both the causal attribution of personal responsibility for weight and the negative value of fat. This could be achieved by ensuring there are lectures on the complexity of obesity including genetic and socioenvironmental determinants of weight regulation, as well as the science of weight‐inclusive health promotion. In this review, interventions that were based on or informed by causal information, and/or critical weight science and HAES were successful in improving explicit bias, whereas empathy‐evoking was less successful. One important distinction between, for example, the weight‐inclusive approach and the less effective empathy‐evoking approach may be in the feelings they provoke. Rather than eliciting pity by emphasizing the hardships of living with obesity, a more productive approach to reducing stigma could be to highlight common humanity and the civil right to healthcare.
Second, there is a need to move away from a solely weight‐centric approach to healthcare to a more health‐focussed approach including weight‐inclusivity. Equally important to the question of “how not to,” is the question of “how and what” we provide in healthcare services. Our findings indicate that clinical encounters are an important element in the formation of HCPs beliefs and attitudes. In several studies, negative expectations or experiences regarding patient care, compliance and outcomes contributed to weight bias retention. All healthcare facilities should be equipped with appropriately sized instruments including, but not limited to, chairs, blood pressure cuffs and gowns. Importantly, being aware of and able to use interventions that improve patients' health regardless of their weight or weight change has the potential to reduce HCPs negative experiences and stereotypes of the so called “difficult patient,” and instead promote a mutually beneficial provider‐patient relationship focussed on health. Data show that patients benefit psychologically and physically from weight‐inclusive programmes that address IWB, the psychological aspects of eating, and the social experience of living with overweight or obesity. 102 , 123 Addressing IWB is likely to be of greatest benefit when delivered within a weight‐inclusive health promotion programme and before commencing with behavioral weight loss because IWB is higher in those seeking weight loss when compared with the general population. 124 It remains questionable whether and to what extent a weight‐loss goal reinforces beliefs about weight controllability and blame, and is thus in itself stigmatizing. 125 Furthermore, working to decrease IWB within weight‐loss programmes may prove challenging because a weight‐loss goal may make improvements in IWB conditional on weight loss and maintenance. Screening for and addressing IWB in people with overweight or obesity looking to improve their eating behaviors, while also funding, designing and implementing long‐term stigma reducing interventions, may help to reduce weight bias in HCPs, as it enables continuous reinforcement and enactment on anti‐weight stigma values. Additionally, although the responsibility of reducing weight stigma in healthcare settings must fall on the provider, reducing IWB can empower patients to advocate for care they deserve.
Lastly, when conducting research on the relationship between weight, health and mortality, there is a need to ensure that researchers measure and account for the confounding and/or mediating effects of weight stigma. 24 , 28 , 126 Weight stigma, as experienced and/or internalized, is largely absent from current epidemiological research, which informs medical, political, and social discourse. Preliminary research shows that a significant proportion of the relationship between obesity and health outcomes can be explained not by body weight itself, but by the negative experiences commonly shared by people with overweight and obesity. More research is needed to understand this relationship and to highlight the importance of weight stigma on health outcomes in the scientific community.
Although the ethical argument and evidence base for the need to reduce stigma in healthcare and beyond is strong, research attention needs to move towards finding rigorous empirical evidence into the specific approaches to reduce weight stigma not just in the short term but in the long‐term. Designing robust, randomized controlled trials with large population sizes and sufficient follow‐up will uphold this aim. Nevertheless, the magnitude and consequences of the issue demand precautionary action, even as evidence is still emerging. Eradicating weight stigma in society should be treated as a public health priority. This requires a whole systems approach, with co‐operation of a wide range of stakeholders among whom HCPs, educators, researchers and policymakers as well as patients play an essential role.
CONFLICT OF INTERESTS
The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Obesity Reviews. This scoping review is based on published data and does not contain sensitive clinical study or patient data. RLB reports receiving consulting fees from Pfizer, Eli‐Lilly, Gila Therapeutics Inc., and ViiV Healthcare and consulting fees, lecture fees from Novo Nordisk and participating in clinical trials for Novo Nordisk. AB reports receiving consulting and lecture fees from Novo Nordisk outside the submitted work; and is the Vice Chair of Specialist Obesity Group of the BDA, and on the Medical Advisory Board and shareholder of Reset Health Clinics Ltd.
AUTHOR CONTRIBUTIONS
AZK conceived the study; AZK, BT, AB, and RLB contributed to the study design and methodology; AZK was responsible for the oversight of the study; BT with support from AZK screened the selected manuscripts included in the review and prepared the draft. All authors contributed to the writing and critical revision of the manuscript and gave final approval.
ACKNOWLEDGMENTS
The authors would like to thank Dr Marialena Trivella for her guidance with the study design, as well as the UCL Division of Medicine and the National Institute for Health Research for support of this project and publication. RLB is funded by National Institute for Health Research grant RP‐2015‐06‐005 (https://www.nihr.ac.uk/).
Talumaa B, Brown A, Batterham RL, Kalea AZ. Effective strategies in ending weight stigma in healthcare. Obesity Reviews. 2022;23(10):e13494. doi: 10.1111/obr.13494
REFERENCES
- 1. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813‐821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nancy K. Discrimination and health inequities. Int J Health Serv. 2014;44(4):643‐710. doi: 10.2190/HS.44.4.b [DOI] [PubMed] [Google Scholar]
- 3. Rubino F, Puhl RM, Cummings DE, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26(4):485‐497. doi: 10.1038/s41591-020-0803-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spahlholz J, Baer N, König HH, Riedel‐Heller SG, Luck‐Sikorski C. Obesity and discrimination ‐ a systematic review and meta‐analysis of observational studies. Obes Rev. 2016;17(1):43‐55. [DOI] [PubMed] [Google Scholar]
- 5. Andreyeva T, Puhl RM, Brownell KD. Changes in Perceived Weight Discrimination Among Americans, 1995–1996 Through 2004–2006. Obesity. 2008;16(5):1129‐1134. [DOI] [PubMed] [Google Scholar]
- 6. Baker P, Brookes G, Atanasova D, Flint SW. Changing frames of obesity in the UK press 2008–2017. Soc Sci Med. 2020;264:113403. [DOI] [PubMed] [Google Scholar]
- 7. Puhl RM, Heuer CA. Obesity stigma: Important considerations for public health. Am J Public Health. 2010;100(6):1019‐1028. doi: 10.2105/AJPH.2009.159491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tomiyama AJ, Carr D, Granberg EM, et al. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med. 2018;16(1):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brewis AA, Wutich A, Falletta‐Cowden A, Rodriguez‐Soto I. Body Norms and Fat Stigma in Global Perspective. Curr Anthropol. 2011;52(2):269‐276. [Google Scholar]
- 10. Strings S. Women (Re)making whiteness: the sexual exclusion of the fat “Black” Irish. Ethn Racial Stud. 2020;43(4):672‐689. [Google Scholar]
- 11. Kyle TK. Weight shaming appears to be declining more in the USA than in the UK. AAAS. https://eurekalert.org/pub_releases/2020-09/eaft-wsa083120.php. Published 2020. Accessed 07/01/2021, 2020.
- 12. Brown A, Flint SW, Batterham RL. Pervasiveness, impact and implications of weight stigma. eClinicalMedicine. 2022;47:101408. doi: 10.1016/j.eclinm.2022.101408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu Y‐K, Berry DC. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: A systematic review. J Adv Nurs. 2018;74(5):1030‐1042. doi: 10.1111/jan.13511 [DOI] [PubMed] [Google Scholar]
- 14. Vadiveloo M, Mattei J. Perceived Weight Discrimination and 10‐Year Risk of Allostatic Load Among US Adults. Ann Behav Med. 2017;51(1):94‐104. doi: 10.1007/s12160-016-9831-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Friedman KE, Ashmore JA, Applegate KL. Recent experiences of weight‐based stigmatization in a weight loss surgery population: Psychological and behavioral correlates. Obesity. 2008;16(SUPPL. 2):S69‐S74. [DOI] [PubMed] [Google Scholar]
- 16. Vartanian LR, Pinkus RT, Smyth JM. Experiences of weight stigma in everyday life: Implications for health motivation. Stigma Health (Washington, DC). 2018;3(2):85‐92. doi: 10.1037/sah0000077 [DOI] [Google Scholar]
- 17. McCleary‐Gaddy AT, Miller CT, Grover KW, Hodge JJ, Major B. Weight Stigma and Hypothalamic‐Pituitary‐Adrenocortical Axis Reactivity in Individuals Who Are Overweight. Ann Behav Med. 2019;53(4):392‐398. doi: 10.1093/abm/kay042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Himmelstein MS, Incollingo Belsky AC, Janet Tomiyama A. The weight of stigma: Cortisol reactivity to manipulated weight stigma. Obesity. 2015;23(2):368‐374. [DOI] [PubMed] [Google Scholar]
- 19. Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic‐pituitary‐adrenocortical axis in humans. Psychol Bull. 2007;133(1):25‐45. doi: 10.1037/0033-2909.133.1.25 [DOI] [PubMed] [Google Scholar]
- 20. Schvey NA, Puhl RM, Brownell KD. The stress of stigma: exploring the effect of weight stigma on cortisol reactivity. Psychosom Med. 2014;76(2):156‐162. doi: 10.1097/PSY.0000000000000031 [DOI] [PubMed] [Google Scholar]
- 21. Hatzenbuehler ML, McLaughlin KA. Structural stigma and hypothalamic‐pituitary‐adrenocortical axis reactivity in lesbian, gay, and bisexual young adults. Ann Behav Med. 2014;47(1):39‐47. doi: 10.1007/s12160-013-9556-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. van der Valk ES, Savas M, van Rossum EFC. Stress and Obesity: Are There More Susceptible Individuals? Curr Obes Rep. 2018;7(2):193‐203. doi: 10.1007/s13679-018-0306-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jung F, Bae Y, Kratzsch J, Riedel‐Heller S, Luck‐Sikorski C. Internalized weight bias and cortisol reactivity to social stress. Cogn Affect Behav Neurosci. 2020;20(1):49‐58. doi: 10.3758/s13415-019-00750-y [DOI] [PubMed] [Google Scholar]
- 24. Daly M, Sutin AR, Robinson E. Perceived Weight Discrimination Mediates the Prospective Association Between Obesity and Physiological Dysregulation: Evidence From a Population‐Based Cohort. Psychol Sci. 2019;30(7):1030‐1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Alimoradi Z, Golboni F, Griffiths MD, Broström A, Lin C‐Y, Pakpour AH. Weight‐related stigma and psychological distress: A systematic review and meta‐analysis. Clin Nutr (Edinburgh, Scotland). 2019;39(7):2001–2013. doi: 10.1016/j.clnu.2019.10.016 [DOI] [PubMed] [Google Scholar]
- 26. Hayward LE, Vartanian LR, Pinkus RT. Weight Stigma Predicts Poorer Psychological Well‐Being Through Internalized Weight Bias and Maladaptive Coping Responses. Obesity. 2018;26(4):755‐761. doi: 10.1002/oby.22126 [DOI] [PubMed] [Google Scholar]
- 27. Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274‐289. doi: 10.1037/amp0000538 [DOI] [PubMed] [Google Scholar]
- 28. Sutin AR, Stephan Y, Terracciano A. Weight Discrimination and Risk of Mortality. Psychol Sci. 2015;26(11):1803‐1811. doi: 10.1177/0956797615601103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Remmert JE, Convertino AD, Roberts SR, Godfrey KM, Butryn ML. Stigmatizing weight experiences in health care: Associations with BMI and eating behaviours. Obes Sci Pract. 2019;5(6):555‐563. doi: 10.1002/osp4.379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nolan LJ, Eshleman A. Paved with good intentions: Paradoxical eating responses to weight stigma. Appetite. 2016;102:15‐24. doi: 10.1016/j.appet.2016.01.027 [DOI] [PubMed] [Google Scholar]
- 31. Cheng MY, Wang S‐M, Lam YY, Luk HT, Man YC, Lin C‐Y. The relationships between weight bias, perceived weight stigma, eating behavior, and psychological distress among undergraduate students in Hong Kong. J Nerv Ment Dis. 2018;206(9):705‐710. doi: 10.1097/NMD.0000000000000869 [DOI] [PubMed] [Google Scholar]
- 32. Araiza AM, Wellman JD. Weight stigma predicts inhibitory control and food selection in response to the salience of weight discrimination. Appetite. 2017;114:382‐390. doi: 10.1016/j.appet.2017.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Major B, Hunger JM, Bunyan DP, Miller CT. The ironic effects of weight stigma. J Exp Soc Psychol. 2014;51:74‐80. doi: 10.1016/j.jesp.2013.11.009 [DOI] [Google Scholar]
- 34. Schvey NA, Puhl RM, Brown KD. The impact of weight stigma on caloric consumption. Obesity. 2011;19(10):1957‐1962. doi: 10.1038/oby.2011.204 [DOI] [PubMed] [Google Scholar]
- 35. Ashmore JA, Friedman KE, Reichmann SK, Musante GJ. Weight‐based stigmatization, psychological distress, & binge eating behavior among obese treatment‐seeking adults. Eat Behav. 2008;9(2):203‐209. doi: 10.1016/j.eatbeh.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 36. Douglas V, Varnado‐Sullivan P. Weight stigmatization, internalization, and eating disorder symptoms: The role of emotion dysregulation. Stigma Health. 2016;1(3):166‐175. doi: 10.1037/sah0000029 [DOI] [Google Scholar]
- 37. Himmelstein MS, Puhl RM, Quinn DM. Weight stigma and health: The mediating role of coping responses. Health Psychol. 2018;37(2):139‐147. doi: 10.1037/hea0000575 [DOI] [PubMed] [Google Scholar]
- 38. Hunger JM, Major B, Blodorn A, Miller CT. Weighed Down by Stigma: How Weight‐Based Social Identity Threat Contributes to Weight Gain and Poor Health. Soc Person Psych Compass. 2015;9(6):255‐268. doi: 10.1111/spc3.12172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Puhl RM, Brownell KD. Confronting and coping with weight stigma: An investigation of overweight and obese adults. Obesity. 2006;14(10):1802‐1815. doi: 10.1038/oby.2006.208 [DOI] [PubMed] [Google Scholar]
- 40. Schwartz MB, Vartanian LR, Nosek BA, Brownell KD. The influence of one's own body weight on implicit and explicit anti‐fat bias. Obesity. 2006;14(3):440‐447. doi: 10.1038/oby.2006.58 [DOI] [PubMed] [Google Scholar]
- 41. Carels RA, Hlavka R, Selensky JC, Solar C, Rossi J, Caroline Miller J. A daily diary study of internalised weight bias and its psychological, eating and exercise correlates. Psychol Health. 2019;34(3):306‐320. doi: 10.1080/08870446.2018.1525491 [DOI] [PubMed] [Google Scholar]
- 42. O'Brien KS, Latner JD, Puhl RM, et al. The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite. 2016;102:70‐76. doi: 10.1016/j.appet.2016.02.032 [DOI] [PubMed] [Google Scholar]
- 43. Puhl RM, Moss‐Racusin CA, Schwartz MB. Internalization of weight bias: Implications for binge eating and emotional well‐being. Obesity. 2007;15(1):19‐23. doi: 10.1038/oby.2007.521 [DOI] [PubMed] [Google Scholar]
- 44. Bidstrup H, Brennan L, Kaufmann L, de la Piedad Garcia X. Internalised weight stigma as a mediator of the relationship between experienced/perceived weight stigma and biopsychosocial outcomes: a systematic review. Int J Obes (Lond) 2022;46(1):1–9. doi: 10.1038/s41366-021-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Meadows A, Higgs S. Internalised weight stigma moderates the impact of a stigmatising prime on eating in the absence of hunger in higher‐ but not lower‐weight individuals. Front Psychol. 2019;10:1022. doi: 10.3389/fpsyg.2019.01022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Major B, Rathbone JA, Blodorn A, Hunger JM. The Countervailing Effects of Weight Stigma on Weight‐Loss Motivation and Perceived Capacity for Weight Control. Pers Soc Psychol Bull. 2020;46(9):1331‐1343. [DOI] [PubMed] [Google Scholar]
- 47. Wellman JD, Araiza AM, Newell EE, McCoy SK. Weight stigma facilitates unhealthy eating and weight gain via fear of fat. Stigma Health. 2018;3(3):186‐194. doi: 10.1037/sah0000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Vartanian LR, Porter AM. Weight stigma and eating behavior: A review of the literature. Appetite. 2016;102:3‐14. doi: 10.1016/j.appet.2016.01.034 [DOI] [PubMed] [Google Scholar]
- 49. Lee KM, Hunger JM, Tomiyama AJ. Weight stigma and health behaviors: evidence from the Eating in America Study. Int J Obes (Lond). 2021;45(7):1499‐1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Täuber S, Gausel N, Flint SW. Weight bias internalization: The maladaptive effects of moral condemnation on intrinsic motivation. Front Psychol. 2018;9:1836. doi: 10.3389/fpsyg.2018.01836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lin CY, Strong C, Latner JD, Lin YC, Tsai MC, Cheung P. Mediated effects of eating disturbances in the association of perceived weight stigma and emotional distress. Eat Weight Disord. 2020;25(2):509‐518. [DOI] [PubMed] [Google Scholar]
- 52. Tomiyama A. Weight stigma is stressful. A review of evidence for the Cyclic Obesity/Weight‐Based Stigma model. Appetite. 2014;82:8‐15. [DOI] [PubMed] [Google Scholar]
- 53. Puhl RM, Lessard LM, Himmelstein MS, Foster GD. The roles of experienced and internalized weight stigma in healthcare experiences: Perspectives of adults engaged in weight management across six countries. PLoS ONE. 2021;16(6):e0251566. doi: 10.1371/journal.pone.0251566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hansson LM, Näslund E, Rasmussen F. Perceived discrimination among men and women with normal weight and obesity. A population‐based study from Sweden. Scand J Public Health. 2010;38(6):587‐596. doi: 10.1177/1403494810372266 [DOI] [PubMed] [Google Scholar]
- 55. Puhl RM, Heuer CA. The Stigma of Obesity: A Review and Update. Obesity. 2009;17(5):941‐964. doi: 10.1038/oby.2008.636 [DOI] [PubMed] [Google Scholar]
- 56. Miller DP, Spangler JG, Vitolins MZ, et al. Are medical students aware of their anti‐obesity bias? Acad Med. 2013;88(7):978‐982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. George TP, DeCristofaro C, Murphy PF. Unconscious Weight Bias Among Nursing Students: A Descriptive Study. Healthcare (Basel). 2019;7(3):106. doi: 10.3390/healthcare7030106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319‐326. doi: 10.1111/obr.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fitzgerald C, Hurst S. Implicit bias in healthcare professionals: A systematic review. BMC Med Ethics. 2017;18(1):19. doi: 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Nyblade L, Stockton MA, Giger K, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Med. 2019;17(1):25. doi: 10.1186/s12916-019-1256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Alberga AS, Edache IY, Forhan M, Russell‐Mayhew S. Weight bias and health care utilization: A scoping review. Prim Health Care Res Dev. 2019;20:e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hayward LE, Neang S, Ma S, Vartanian LR. Discussing weight with patients with overweight: Supportive (not stigmatizing) conversations increase compliance intentions and health motivation. Stigma Health (Washington, DC). 2020;5(1):53‐68. [Google Scholar]
- 63. Fatima Cody S, Erica DJ, Mechelle DC, Rebecca LE, Lee MK. The Role of Obesity Training in Medical School and Residency on Bariatric Surgery Knowledge in Primary Care Physicians. Int J Family Med. 2015;2015:841249‐841248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Vitolins MZ, Crandall S, Miller D, Ip E, Marion G, Spangler JG. Obesity Educational Interventions in U.S. Medical Schools: A Systematic Review and Identified Gaps. Teach Learn Med. 2012;24(3):267‐272. doi: 10.1080/10401334.2012.692286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Barra M, Singh Hernandez SS. Too big to be seen: Weight‐based discrimination among nursing students. Nurs Forum. 2018;53(4):529‐534. doi: 10.1111/nuf.12282 [DOI] [PubMed] [Google Scholar]
- 66. Gayer GG, Weiss J, Clearfield M. Fundamentals for an Osteopathic obesity designed study: The effects of education on osteopathic medical students' attitudes regarding obesity. J am Osteopathic Assoc. 2017;117(8):495‐502. doi: 10.7556/jaoa.2017.099 [DOI] [PubMed] [Google Scholar]
- 67. Geller G, Watkins PA. Addressing medical students' negative bias toward patients with obesity through ethics education. AMA J Ethics. 2018;20(10):948‐959. doi: 10.1001/amajethics.2018.948 [DOI] [PubMed] [Google Scholar]
- 68. Jones CA, Forhan M. Addressing weight bias and stigma of obesity amongst physiotherapists. Physiother Theory Pract. 2021;37(7):808‐816. [DOI] [PubMed] [Google Scholar]
- 69. Nickel F, Tapking C, Benner L, et al. Video Teaching Leads to Improved Attitudes Towards Obesity‐a Randomized Study with 949 Participants. Obes Surg. 2019;29(7):2078‐2086. doi: 10.1007/s11695-019-03804-9 [DOI] [PubMed] [Google Scholar]
- 70. Zitek EM, Hebl MR. The role of social norm clarity in the influenced expression of prejudice over time. J Exp Soc Psychol. 2007;43(6):867‐876. [Google Scholar]
- 71. Batras D, Duff C, Smith BJ. Organizational change theory: implications for health promotion practice. Health Promot Int. 2016;31(1):231‐241. [DOI] [PubMed] [Google Scholar]
- 72. Wynn T, Islam N, Thompson C, Myint KS. The effect of knowledge on healthcare professionals' perceptions of obesity. Obes Med. 2018;11:20‐24. doi: 10.1016/j.obmed.2018.06.006 [DOI] [Google Scholar]
- 73. O'Brien KS, Hunter JA, Banks M. Implicit anti‐fat bias in physical educators: physical attributes, ideology and socialization. Int J Obes (Lond). 2007;31(2):308‐314. doi: 10.1038/sj.ijo.0803398 [DOI] [PubMed] [Google Scholar]
- 74. Rathbone JA, Cruwys T, Jetten J, Barlow FK. When stigma is the norm: How weight and social norms influence the healthcare we receive. J Appl Soc Psychol. 2020. doi: 10.1111/JASP.12689 [DOI] [Google Scholar]
- 75. Phelan SM, Puhl RM, Burke SE, et al. The mixed impact of medical school on medical students' implicit and explicit weight bias. Med Educ. 2015;49(10):983‐992. doi: 10.1111/medu.12770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bergen M, Mollen D. Teaching Sizeism: Integrating Size into Multicultural Education and Clinical Training. Women Therapy. 2019;42(1–2):164‐180. [Google Scholar]
- 77. Teachman BA, Gapinski KD, Brownell KD, Rawlins M, Jeyaram S. Demonstrations of implicit anti‐fat bias: the impact of providing causal information and evoking empathy. Health Psychol. 2003;22(1):68‐78. doi: 10.1037/0278-6133.22.1.68 [DOI] [PubMed] [Google Scholar]
- 78. Puhl RM, Latner JD, O'Brien K, Luedicke J, Danielsdottir S, Forhan M. A multinational examination of weight bias: predictors of anti‐fat attitudes across four countries. Int J Obes (Lond). 2015;39(7):1166‐1173. doi: 10.1038/ijo.2015.32 [DOI] [PubMed] [Google Scholar]
- 79. Hilbert A. Weight stigma reduction and genetic determinism. PLoS ONE. 2016;11(9):e0162993. doi: 10.1371/journal.pone.0162993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Brochu PM. Testing the effectiveness of a weight bias educational intervention among clinical psychology trainees. J Appl Soc Psychol. 2020. doi: 10.1111/jasp.12653 [DOI] [Google Scholar]
- 81. Diedrichs PC, Barlow FK. How to lose weight bias fast! Evaluating a brief anti‐weight bias intervention. Br J Health Psychol. 2011;16(4):846‐861. [DOI] [PubMed] [Google Scholar]
- 82. O'Brien KS, Puhl RM, Latner JD, Mir AS, Hunter JA. Reducing anti‐fat prejudice in preservice health students: A randomized trial. Obesity. 2010;18(11):2138‐2144. doi: 10.1038/oby.2010.79 [DOI] [PubMed] [Google Scholar]
- 83. Persky S, Eccleston CP. Impact of genetic causal information on medical students' clinical encounters with an obese virtual patient: Health promotion and social stigma. Ann Behav Med. 2011;41(3):363‐372. doi: 10.1007/s12160-010-9242-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Crandall CS, D'Anello S, Sakalli N, Lazarus E, Nejtardt GW, Feather NT. An Attribution‐Value Model of Prejudice: Anti‐Fat Attitudes in Six Nations. Pers Soc Psychol Bull. 2016;27(1):30‐37. doi: 10.1177/0146167201271003 [DOI] [Google Scholar]
- 85. Daníelsdóttir S, O'Brien KS, Ciao A. Anti‐Fat Prejudice Reduction: A Review of Published Studies. Obes Facts. 2010;3(1):47‐58. doi: 10.1159/000277067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Derksen F, Bensing J, Lagro‐Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76‐e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S. The Role of Empathy in Health and Social Care Professionals. Healthcare (Basel). 2020;8(1):26. doi: 10.3390/healthcare8010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Lee M, Ata RN, Brannick MT. Malleability of weight‐biased attitudes and beliefs: A meta‐analysis of weight bias reduction interventions. Body Image. 2014;11(3):251‐259. doi: 10.1016/j.bodyim.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 89. Cotugna N, Mallick A. Following a calorie‐restricted diet may help in reducing healthcare students' Fat‐Phobia. J Community Health. 2010;35(3):321‐324. doi: 10.1007/s10900-010-9226-9 [DOI] [PubMed] [Google Scholar]
- 90. Harris MB, Walters LC, Waschull S. Altering Attitudes and Knowledge about Obesity. J Soc Psychol. 1991;131(6):881‐884. [DOI] [PubMed] [Google Scholar]
- 91. Hunter J, Rawlings‐Anderson K, Lindsay T, Bowden T, Aitken LM. Exploring student nurses' attitudes towards those who are obese and whether these attitudes change following a simulated activity. Nurse Educ Today. 2018;65:225‐231. doi: 10.1016/j.nedt.2018.03.013 [DOI] [PubMed] [Google Scholar]
- 92. Kushner RF, Zeiss DM, Feinglass JM, Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Med Educ. 2014;14(1):53. doi: 10.1186/1472-6920-14-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Matharu K, Shapiro JF, Hammer RR, Kravitz RL, Wilson MD, Fitzgerald FT. Reducing obesity prejudice in medical education. Educ Health: Change Learn Pract. 2014;27(3):231‐237. doi: 10.4103/1357-6283.152176 [DOI] [PubMed] [Google Scholar]
- 94. Molloy MA, Sabol VK, Silva SG, Guimond ME. Using Trigger Films as a Bariatric Sensitivity Intervention: Improving Nursing Students' Attitudes and Beliefs About Caring for Obese Patients. Nurse Educ. 2016;41(1):19‐24. doi: 10.1097/NNE.0000000000000225 [DOI] [PubMed] [Google Scholar]
- 95. Meadows A, Daníelsdóttir S, Calogero R, O'Reilly C. Why fat suits do not advance the scientific study of weight stigma. Obesity. 2017;25(2):275‐275. doi: 10.1002/oby.21742 [DOI] [PubMed] [Google Scholar]
- 96. Gloor JL, Puhl RM. Empathy and perspective‐taking: Examination and comparison of strategies to reduce weight stigma. Stigma Health (Washington, DC). 2016;1(4):269‐279. [Google Scholar]
- 97. Murakami JM, Latner JD. Weight acceptance versus body dissatisfaction: Effects on stigma, perceived self‐esteem, and perceived psychopathology. Eat Behav. 2015;19:163‐167. doi: 10.1016/j.eatbeh.2015.09.010 [DOI] [PubMed] [Google Scholar]
- 98. Fildes A, Charlton J, Rudisill C, Littlejohns P, Prevost AT, Gulliford MC. Probability of an Obese Person Attaining Normal Body Weight: Cohort Study Using Electronic Health Records. Am J Publ Health (1971). 2015;105(9):e54‐e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Nordmo M, Danielsen YS, Nordmo M. The challenge of keeping it off, a descriptive systematic review of high‐quality, follow‐up studies of obesity treatments. Obes Rev. 2019;21(1):e12949. [DOI] [PubMed] [Google Scholar]
- 100. Montani JP, Schutz Y, Dulloo AG. Dieting and weight cycling as risk factors for cardiometabolic diseases: who is really at risk? Obes Rev. 2015;16(S1):7‐18. doi: 10.1111/obr.12251 [DOI] [PubMed] [Google Scholar]
- 101. Schaumberg K, Anderson D. Dietary restraint and weight loss as risk factors for eating pathology. Eat Behav. 2016;23:97‐103. doi: 10.1016/j.eatbeh.2016.08.009 [DOI] [PubMed] [Google Scholar]
- 102. Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J. 2011;10:9. doi: 10.1186/1475-2891-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Hunger JM, Smith JP, Tomiyama AJ. An Evidence‐Based Rationale for Adopting Weight‐Inclusive Health Policy. Soc Issues Policy Rev. 2020;14(1):73‐107. [Google Scholar]
- 104. Tylka TL, Annunziato RA, Burgard D, et al. The weight‐inclusive versus weight‐normative approach to health: evaluating the evidence for prioritizing well‐being over weight loss. J Obes. 2014;2014:983495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. McVey GL, Walker KS, Beyers J, Harrison HL, Simkins SW, Russell‐Mayhew S. Integrating weight bias awareness and mental health promotion into obesity prevention delivery: a public health pilot study. Prev Chronic Dis. 2013;10:E46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Werkhoven T. Designing, implementing and evaluating an educational intervention targeting weight bias and fat stereotyping. J Health Psychol. 2020;26(12):2084‐2097. doi: 10.1177/1359105319901310 [DOI] [PubMed] [Google Scholar]
- 107. Patterson D, Buse K, Magnusson R, Toebes B. Identifying a human rights‐based approach to obesity for States and civil society. Obes Rev. 2019;20(Suppl 2):45‐56. doi: 10.1111/obr.12873 [DOI] [PubMed] [Google Scholar]
- 108. Calogero RM, Tylka TL, Mensinger JL, Meadows A, Daníelsdóttir S. Recognizing the Fundamental Right to be Fat: A Weight‐Inclusive Approach to Size Acceptance and Healing From Sizeism. Women Therapy. 2019;42(1–2):22‐44. [Google Scholar]
- 109. Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. Fatness on All‐Cause Mortality: A Meta‐Analysis. Prog Cardiovasc Dis. 2014;56(4):382‐390. doi: 10.1016/j.pcad.2013.09.002 [DOI] [PubMed] [Google Scholar]
- 110. Carlsson AC, Wändell PE, Gigante B, Leander K, Hellenius M‐L, de Faire U. Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all‐cause mortality regardless of body mass index: A cohort study. Int J Cardiol. 2013;168(2):946‐952. doi: 10.1016/j.ijcard.2012.10.045 [DOI] [PubMed] [Google Scholar]
- 111. Falker AJ, Sledge JA. Utilizing a bariatric sensitivity educational module to decrease bariatric stigmatization by healthcare professionals. Bariatric Nurs Surg Patient Care. 2011;6(2):73‐78. doi: 10.1089/bar.2011.9974 [DOI] [Google Scholar]
- 112. Luig T, Wicklum S, Heatherington M, et al. Improving obesity management training in family medicine: Multi‐methods evaluation of the 5AsT‐MD pilot course. BMC Med Educ. 2020;20(1):5. doi: 10.1186/s12909-019-1908-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Poustchi Y, Saks NS, Piasecki AK, Hahn KA, Ferrante JM. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013;45(5):345‐348. [PMC free article] [PubMed] [Google Scholar]
- 114. Swift JA, Tischler V, Markham S, et al. Are anti‐stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6(1):91‐102. doi: 10.1159/000348714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Goss AL, Rethy L, Pearl RL, De Lisser HM. The “difficult” cadaver: weight bias in the gross anatomy lab. Med Educ Online. 2020;25(1):1742966. doi: 10.1080/10872981.2020.1742966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wiese HJ, Wilson JF, Jones RA, Neises M. Obesity stigma reduction in medical students. Int J Obes Relat Metab Disord. 1992;16(11):859‐868. [PubMed] [Google Scholar]
- 117. Wijayatunga NN, Kim Y, Butsch WS, Dhurandhar EJ. The effects of a teaching intervention on weight bias among kinesiology undergraduate students. Int J Obes (Lond). 2019;43(11):2273‐2281. doi: 10.1038/s41366-019-0325-0 [DOI] [PubMed] [Google Scholar]
- 118. Rukavina PB, Li W, Rowell MB. A service learning based intervention to change attitudes toward obese individuals in kinesiology pre‐professionals. Soc Psychol Educ. 2008;11(1):95‐112. doi: 10.1007/s11218-007-9039-6 [DOI] [Google Scholar]
- 119. Rukavina PB, Li W, Shen B , Sun H. A service learning based project to change implicit and explicit bias toward obese individuals in kinesiology pre‐professionals. Obes Facts. 2010;3(2):117‐126. doi: 10.1159/000302794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Harris J. Physical education teacher education students' knowledge, perceptions and experiences of promoting healthy, active lifestyles in secondary schools. Physical Education and Sport Pedagogy: School physical education curricula for future generations: Global neo‐liberalism? Global Lessons? 2014;19(5):466‐480. [Google Scholar]
- 121. Alberga AS, Pickering BJ, Alix Hayden K, et al. Weight bias reduction in health professionals: a systematic review: Weight bias reduction in health professionals. Clin Obes. 2016;6(3):175‐188. doi: 10.1111/cob.12147 [DOI] [PubMed] [Google Scholar]
- 122. Romano KA, Heron KE, Henson JM. Examining associations among weight stigma, weight bias internalization, body dissatisfaction, and eating disorder symptoms: Does weight status matter? Body Image. 2021;37:38‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Schaefer JT, Magnuson AB. A review of interventions that promote eating by internal cues. J Acad Nutr Diet. 2014;114(5):734‐760. doi: 10.1016/j.jand.2013.12.024 [DOI] [PubMed] [Google Scholar]
- 124. Pearl RL, Himmelstein MS, Puhl RM, Wadden TA, Wojtanowski AC, Foster GD. Weight bias internalization in a commercial weight management sample: prevalence and correlates. Obes Sci Pract. 2019;5(4):342‐353. doi: 10.1002/osp4.354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Reinka M, Quinn D, Puhl R. Examining the relationship between weight controllability beliefs and eating behaviors: The role of internalized weight stigma and BMI. Appetite. 2021;164:105257. doi: 10.1016/j.appet.2021.105257 [DOI] [PubMed] [Google Scholar]
- 126. Sutin AR, Terracciano A. Perceived Weight Discrimination and Obesity. PLoS ONE. 2013;8(7):e70048. [DOI] [PMC free article] [PubMed] [Google Scholar]


