Abstract
Man and environment have a strong connection with each other for their functioning. Environmental toxins which can be natural or manmade result in the loss of this balance by causing systemic inflammatory response within the human body, with the brain being the most affected target end-organ. These problems are more prominent in Third World countries, where environmental regulations laws are either relaxed or non-existent. These neurotoxins play a very important aetiological role in the manifestation of various neurodegenerative diseases, neurodevelopmental disorders and psychiatric disorders. Environmental neurotoxicity results from inhibition of mitochondrial activity, excess oxidative stress leading to neuroinflammation, and promoting apoptosis and neuronal cell death. Having the know-how of these neurotoxins will provide insight into the process of neurodegeneration and will result in further designing of studies to delve into processes and mechanisms of neuronal regeneration and axonal sprouting. This review highlights the various central nervous system disorders associated with exposure to environmental neurotoxins and discusses the way forward to prevent or halt the process of neurodegeneration.
Keywords: Environmental toxins, manmade, natural, neurodegeneration, neuroinflammation
“The simple truth is that we are living in a sea of toxins and it is destroying our bodies and brains.”—Dr. Hyman
INTRODUCTION
Our brain is one of the most important organs which helps us to be the most productive in our society. It is also the most complex in the animal world. Cells follow perfectly sequential processes as it is only when the former stage is completed, and then they move on to the next stage. Any neurotoxin exposure at any stage of the development leads to disruption of this sequence leading to its gross, microscopic and functional impairment manifesting with neurological and psychiatric symptoms in humans for the rest of their life.
Even the matured neuronal cells and their circuitry are very sensitive to toxin-induced injury. The toxin-induced apoptosis of neurons results in disruption of their extensive circuitry which causes varied patterns of clinical signs and symptoms. The central and peripheral nervous system has a protective mechanism in the form of blood–brain barrier (BBB) and blood–axon barrier, respectively. However, some areas in the brain do not have this protection (area postrema, hypothalamus, pineal gland, autonomic ganglia, motor, and sensory nerve terminals) and are therefore susceptible to easy entry and injury by neurotoxins.
ENVIRONMENTAL TOXINS
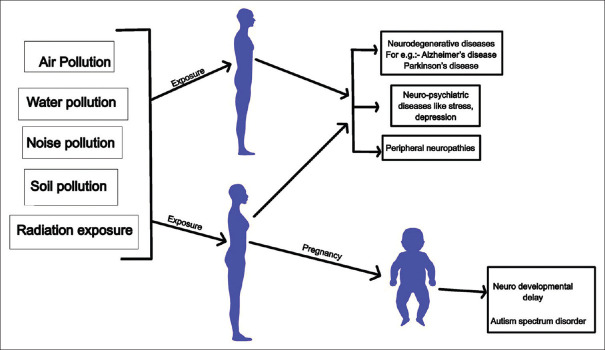
Any poisonous chemical substance and its by-products or organism present in our immediate environment that wrongly affects human health (e.g. carcinogenesis, cardiovascular, respiratory or neurological disorders) are included in the category of environmental toxicants. It is known that they do interfere with the normal physiology of the cells but the underlying mechanisms involved are still not well defined.[1] According to Landrigan et al.,[2] pollution-related diseases have led to approximately 9 million deaths prematurely in 2015, that is, 16% of all deaths globally which accounts for nearly thrice the amount of deaths caused by communicable diseases like HIV, tuberculosis and malaria altogether and 15 times more deaths than that caused by wars and other acts of violence. Figure 1 and Table 1 show various toxins present in our food, water and air.
Figure 1.
Various environmental toxins
Table 1.
Neurotoxins derived from the environment
| Environmental toxin | Examples | Comments |
|---|---|---|
| Chemical toxins | Organic Polychlorinated biphenyls (PCBs) or Chlorinated hydrocarbons, TCDD (2, 3, 7, 8-tetrachlorodibenzo-p-dioxin), Fluorinated organic substances (per- and polyfluoroalkyl substances [PFAs] or perfluorinated compounds [PFCs]) | Used in plastics and rubber products and pigments, dyes. They are persistent in aquatic ecosystems |
| Inorganic compounds Heavy metals like arsenic, mercury, lead and cadmium Warfare agents like Sarin |
Encephalopathies Peripheral neuropathies |
|
| Radiation | Sunlight, x-rays, radio waves, particle radiation, i.e., alpha and beta Particles and neutrons. |
Predispose to cancer, congenital disabilities, or skin burns. |
| Pesticides | DDT Pyrethroids |
Their poor bio-degradability results in bio- accumulation of chemicals and bio-magnification within a food web |
| Biological agents | Phytotoxins - derived from food plants and fruits |
Phytotoxins e.g., Lathyrus sativus causing lathyrism,[3] Litchi fruit causes hypoglycaemic encephalopathy,[4] Cassava ingestion leads to cassavism due to cyanide toxicity,[5] Annona muricata associated with atypical parkinsonism.[6] |
| Mycotoxins - derived as metabolite of fungi which act as neurotoxin for animals and human. |
Ergot, fumonisin B1 and ochratoxin[7,8,9] have neurotoxic effects. Neurological manifestations can include encephalopathy, movement disorders like choreoathetosis, spasms and ballism,[10] epileptic encephalopathy[11] |
|
| Algae toxins Cyanobacteria or blue-green algae bloom in higher temperatures in aquatic ecosystem which is associated with climate change. |
They produce cyanotoxins which can result in neurotoxicity due to seafood poisoning e.g., paralytic shellfish poisoning (PSP), neurotoxic shellfish poisoning (NSP), and amnesic shellfish poisoning (ASP).[12] | |
| Infectious diseases | Neurotropic viruses Bacteria e.g., Diphtheric toxin Protozoa e.g., malaria |
West Nile encephalitis,[13] Zika virus[14] yellow fever,[15] dengue,[15] COVID-19. |
| Air pollutants | Carbon monoxide/Carbon di oxide | Most common and widely distributed air pollutant. |
| Sulphur di oxide | Released from fossil fuels, domestic fires etc. | |
| Lead | Children and pregnant women are affected the most. Affects blood and brain in children. | |
| Ozone | Strongest oxidizing agent. | |
| Particulate matter | Complex mixture of organic and inorganic substances. Coarse particles with an aerodynamic diameter of 2.5 to 10 um (PM10), fine particles of less than 2.5 um (PM2.5) and ultrafine (UFPs) or nano-sized (NP) particles less than 0.1 um. |
DETERMINANTS FOR NEUROTOXICITY BY ENVIRONMENTAL POLLUTANTS
i. Urbanization and climatic changes
The executive summary of the article – “The Lancet Commission on pollution and health”[2] – has highlighted that environmental pollution, especially after the combustion of fossil fuels, is a major determinant for the destruction of the various ecosystems and for bringing about climate change globally. The worst affected are the low and middle-income countries, where by 2050, it is believed that nearly 50% of the global population will be residing especially in urban locations leading to overcrowding, poor air quality and dissemination of various airborne infections.[16]
ii.Time of exposure, concentration and duration of exposure to environmental toxins
Extremes of ages are more severely affected by environmental toxins. Their entry through the placenta in utero or through breast milk post-natally has bad effects on the neurodevelopment of the child as these toxins, even in low concentrations, can cross the BBB to affect the developing brain. Poor hepatic and renal functions and age-related neurodegeneration make the elderly population more vulnerable to the ill-effects of environmental pollutants. Also, depending upon the concentration of the toxins and duration of their exposure, clinical manifestation will vary; for example, acute presentation may occur on exposure to a high concentration of toxin for a short duration and chronic presentation may occur with prolonged exposure to low concentration of toxin.[17]
PATHOGENETIC MECHANISM OF NEURODEGENERATION BY ENVIRONMENTAL TOXINS
The various environmental toxicants enter the central nervous system (CNS) through the BBB [Figure 2]. They use four mechanisms to cross the BBB: first, through a specific channel via transporters; second, using the high lipophilic characteristic of the toxin to pass directly through the plasma membrane; third, the toxin can easily enter through the disrupted BBB; and lastly, direct entry of systemic proinflammatory cytokines produced due to toxins affecting systemic organs like lungs, liver and heart.[18] After entering the CNS, they affect the normal physiological functioning of various cells, including neurons, microglia, astrocytes and oligodendrocytes, leading to stimulation of release of pro-inflammatory cytokines like interleukin-1β (IL-1β), tumour necrosis factor-α and interferon-γ causing neuroinflammation within CNS and neurodegeneration.[19]
Figure 2.
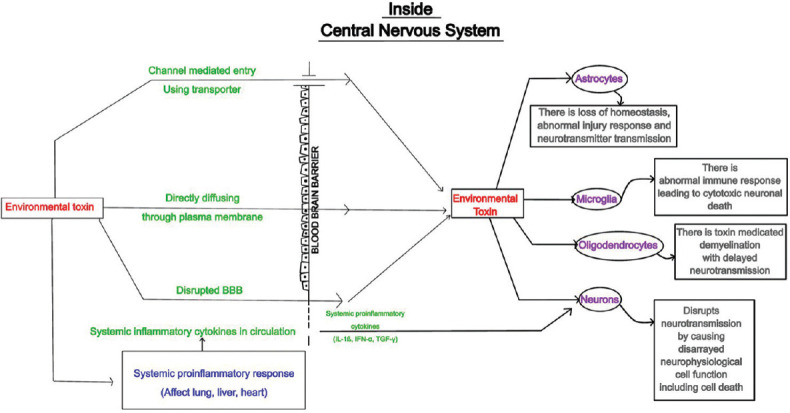
Pathogenetic mechanism of neurotoxicity by various environmental toxins
ENVIRONMENTAL TOXINS AND NEUROLOGICAL DISORDERS
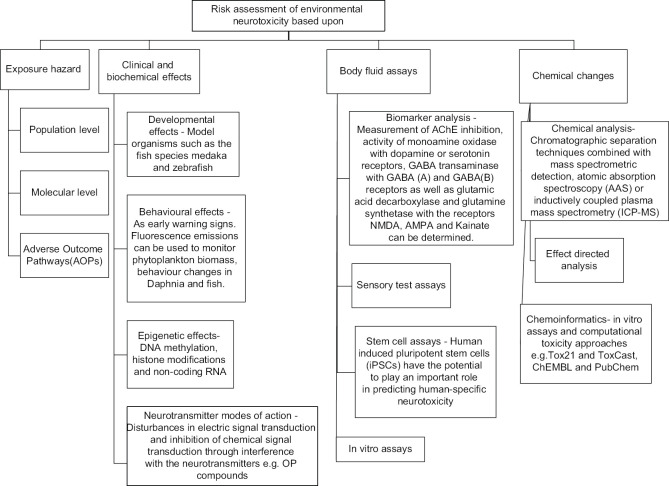
It is a known fact that changes in our immediate environment have direct implications on our mental health [Figure 3]. The exposure of humans to neurotoxins in our environment leads to various neurological clinical manifestations; for example, encephalopathies, dementia, movement disorders, autism, neuropsychiatric symptoms and peripheral neuropathies in isolation or combination. This association is imprecise and unpredictable because there are no well-structured long-term follow-up studies on this issue of great concern.
Figure 3.
Various neurological manifestations to environmental toxins
I. Acute neurological conditions
A. Encephalopathies
Acute exposure to neurotoxins (e.g. lead, aluminium, cannabis and organic solvents) can precipitate features of encephalopathy; for example, headache, delirium, short-term transient memory loss and gait disturbances.[20] These symptoms are temporary and resolve once the patient is isolated from the site of exposure. However, acute encephalopathy can progress to chronic encephalopathy with features of cognitive impairment and psychomotor slowing, especially on exposure to heavy metals like aluminium, cadmium and lead.
B. Stroke
There is a strong association between air pollution and stroke.[21] It is a known fact that the toxins in the air (e.g. NO2, SO2, PM2.5 and PM10) are important contributors to vascular thrombotic events responsible for ischemic strokes and acute coronary syndromes.
I. Neurodegenerative disorders
A. Dementia
In a review by Kim et al.,[21] continual exposure to PM2.5 in the air has been strongly associated with developing dementia and Alzheimer's disease. Also, in a study by Cerza et al.,[22] they have found a definitive association between NO2 and ozone in ambient air and first-time hospitalizations for dementia. Clinically, the patient presents with difficulty in immediate recall and new learning capabilities in the preclinical stage due to rapid and progressive grey matter atrophy.
B. Disorders of movement
Cerebellar and extrapyramidal symptoms have been shown to have developed following exposure to environmental toxins.[17] Mercury, Lithium and 5-Fluorouracil have been implicated in the manifestation of the cerebellar syndrome of gait ataxia, incoordination and speech disturbances. Extrapyramidal toxic syndromes include Parkinsonism, dystonias and dyskinesias. A well-known example is excessive exposure to 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine, a toxin present in some drugs of abuse, leading to Parkinsonism.
C. CNS Demyelination
Multiple sclerosis is believed to be causally associated with air pollution. On exposure to particulate matter, especially PM10 and fine dust, there is the release of systemic cytokines like IL-2, IL-6 and macrophage migration inhibitory factor-1 which cross BBB and lead to neuroinflammation and CNS demyelination.[21]
II. Neurodevelopmental delay
There is a strong correlation between exposure to environmental toxins in utero and delay in attainment of developmental milestones, which include cognitive impairment, attention deficits and hyperactivity disorder, behavioural and executive dysfunction and autistic disorders. Various environmental neurotoxins have been implicated in neurodevelopmental disorders – polychlorinated biphenyls, mercury exposure leads to decreased IQ and delayed attention span in children,[23,24] birth defects like microcephaly, autistic disorders on prenatal exposure to organophosphate compounds,[25] cognitive impairment seen with polycyclic aromatic hydrocarbons.[26] Studies have shown that fetal exposure to PM2.5, O3 and fine dust during early pregnancy was associated with reduced levels of brain-derived neurotrophic factor and neurodevelopmental delay with reduced grey-matter volumes in the brain.[27,28] Many environmental chemicals are silently involved in fetal brain damage but are still not documented.
III. Neuropsychiatric manifestations
Environmental pollution and mental health conditions that exist hand in hand through their correlation are controversial. Studies have shown that the risk of having depression increases with prolonged exposure to PM2.5 and even limited exposure to PM10, NO2, SO2 and CO.[29] This is because these air pollutants can stimulate adrenal glands to secrete excess cortisol via the pituitary and hypothalamus[30] which can result in neuroinflammation leading to cognitive impairment and depression.[31] Another mental health disorder associated with environmental neurotoxins is schizophrenia. In a study by Liang et al.,[32] it was shown that short duration exposure to PM10, SO2 and NO2 increases the risk of developing schizophrenia.
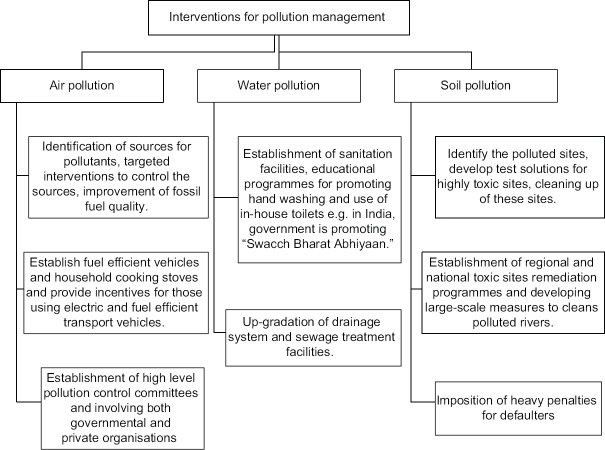
ENVIRONMENTAL NEUROTOXICITY ASSESSMENT
Humans and other living organisms are exposed to different classes of environmental toxins with a broad range of adverse consequences. In a review by Legradi et al.,[33] it has been highlighted that it is challenging to identify various neurotoxins and develop novel neurotoxicity testing methods. Moreover, current testing is not allowed for screening populations at a large scale and is limited only to medium and high production volume chemical compounds. Also, their neurotoxic effects on other organisms in our ecosystem are not considered for testing. Figure 4 shows various key components for the assessment of environmental neurotoxicity.
Figure 4.
Components for risk assessment of environmental neurotoxicity
The United States Environmental Protection Agency and the Organization for Economic Co-operation and Development guidelines focus on clinical presentations, measurements of motor activity, sensory response to stimuli and neuropathological examinations.[34] The USA and European Union (EU) have developed separate guidelines for developmental neurotoxicity testing, which include measurements of developmental landmarks and primitive reflexes, motor activity, auditory startle test, learning and memory tests, and neuropathology. Recent legislations [e.g. REACH (Registration Evaluation and Authorization of Chemicals) and the Cosmetics Directive (76/768/EEC) in the EU] have been keeping a strong control as far as registering the increasing number of chemicals that are being developed for commercial purpose.
ENVIRONMENTAL NEUROTOXICITY: INDIAN PERSPECTIVE
The data projecting the incidence and prevalence of various neurological diseases due to environmental neurotoxicity in the Indian population is scarce. A study by doctors at the Ecotoxicology facility at the All India Institute of Medical Sciences (AIIMS) in 2019 confirmed that nearly 35 of 216 patients referred to their clinic had “excessive” amounts of heavy metals and toxins (iron, mercury, lead, chromium and fluoride) in their bodies detected on blood and urine samples who presented with various cancers, neurodevelopmental disorders and bone disorders among other serious conditions. Another study conducted by Central Water Commission found that India's 42 rivers had at least two toxic heavy metals beyond the permissible limit, with lead being the most common pollutant. River Ganga was found to be polluted with five heavy metals, namely chromium, copper, nickel, lead and iron. According to the report, mining, milling, plating and surface finishing industries are the main sources of heavy metal pollution in these rivers.[35]
In India, environmental pollution is a national crisis. It has been rated as one of the most polluted countries in the world. The Environmental Protection Index 2016 score has ranked India at 141 position out of the 180 countries studied. In India, various legislations related to preventing water and air pollution (Water Prevention and Control of Pollution Act, 1974; Air Prevention and Control of Pollution Act, 1981), environmental protection (Environment Protection Act, 1986), forest conservation (Forest Conservation Act, 1980) and biodiversity protection (Biological Diversity Act, 2002) have been passed but there is laxity in the administrative will to implement these laws. There is an urgent need for setting up an independent environmental regulatory body with no political interference and also to step up the penalty and liability mechanism, that is, “Polluter pays principle”.
In an article by Divyanu Jain et al., it is mentioned that during the coronavirus disease (COVID-19) pandemic, when a lockdown was imposed in India in 2020, there was a significant improvement in air quality in 88 cities across the country.[36] This was possible because industrial activities and mass transportation were at a halt for a significant period.
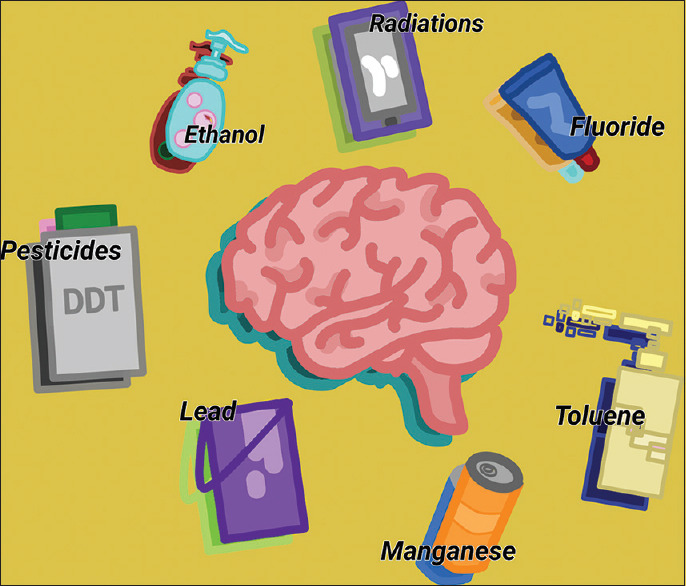
ENVIRONMENTAL NEUROTOXINS: FUTURE DIRECTIONS
Environmental planning has two major aspects of the formation of policies and their implementation, which include comprehensive growth management and environmental pollution control. It is mandatory that urban development planning must protect and conserve the natural resources and other ecosystems as any disturbance in the eco-balance can cause serious harm to humans and other living organisms. Environmental pollution control policies are concerned with air, water and soil pollution. The key components of these policies include environmental planning, land development policies and the designing of pollution-free transportation systems for stopping greenhouse gas emissions. Also, education of the masses, making them aware of environmental health concerns and public action are the best ways to minimize risks from environmental neurotoxins. Figure 5 provides a brief overview of various interventions needed for controlling environmental pollution.
Figure 5.
Various Interventions for management of environmental pollution
CONCLUSION
Environmental chemicals with neurotoxic effects can result in a wide range of neurological and psychiatric disorders such as Parkinson's disease, Alzheimer's dementia, encephalopathies to subtle memory and cognition alteration, headaches and depression. This can occur even after the many years have elapsed between exposure and neurological manifestation. Also, there are no policies for screening populations at large for testing the environmental toxins. It is prudent to combine clinical, epidemiological and toxicological studies with cost-effective quantitative risk assessment when use and exposure warrant. Newer biological markers for assessing subclinical neurotoxic effects need to be developed by in vitro analysis and animal-based studies. Better exposure-surveillance systems are to be developed to mitigate the effects of toxin exposure. There is a dire need to formulate experimental designs for studies to provide information regarding the risk-assessment process on exposure to environmental neurotoxic agents.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chin NP. Environmental toxins: Physical, social, and emotional. Breastfeed Med. 2010;5:223–4. doi: 10.1089/bfm.2010.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu NN, et al. The lancet commission on pollution and health. Lancet. 2018;391:462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- 3.Dwivedi MP, Prasad BG. An epidemiological study of lathyrism in the district of Rewa, Madhya Pradesh. Indian J Med Res. 1964;52:81–116. [PubMed] [Google Scholar]
- 4.Palmer VS, Tshala-Katumbay DD, Spencer PS. Plants with neurotoxic potential in undernourished subjects. Rev Neurol. 2019;175:631–40. doi: 10.1016/j.neurol.2019.07.015. [DOI] [PubMed] [Google Scholar]
- 5.Kashala-Abotnes E, Okitundu D, Mumba D, Boivin MJ, Tylleskär T, Tshala-Katumbay D. Konzo: A distinct neurological disease associated with food (cassava) cyanogenic poisoning. Brain Res Bull. 2019;145:87–91. doi: 10.1016/j.brainresbull.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caparros-Lefebvre D, Elbaz A. Possible relation of atypical Parkinsonism in the French West Indies with consumption of tropical plants: A case-control study. Caribbean Parkinsonism study group. Lancet. 1999;354:281–6. doi: 10.1016/s0140-6736(98)10166-6. [DOI] [PubMed] [Google Scholar]
- 7.Spencer PS. Biological principles of chemical neurotoxicity. In: Spencer PS, Schaumburg HH, editors. Experimental and Clinical Neurotoxicology. 2nd ed. New York: Oxford; 2000. pp. 3–54. doi: 10.1136/jnnp.70.3.421j. [Google Scholar]
- 8.Pitt JL, Miller JD. A concise history of mycotoxin research. J Agric Food Chem. 2017;65:7021–33. doi: 10.1021/acs.jafc.6b04494. [DOI] [PubMed] [Google Scholar]
- 9.Paradells S, Rocamonde B, Llinares Benadero C, Herranz-P’erez V, Jimenez M, Garcia-Verdugo JM, et al. Neurotoxic effects of ochratoxin-a on the subventricular zone of adult mouse brain. J Appl Toxicol. 2015;35:737–51. doi: 10.1002/jat.3061. [DOI] [PubMed] [Google Scholar]
- 10.He F, Zhang S, Qian F, Zhang C. Delayed dystonia with striatal CT lucencies induced by a mycotoxin (3-nitropropionic acid) Neurology. 1995;45:2178–83. doi: 10.1212/wnl.45.12.2178. [DOI] [PubMed] [Google Scholar]
- 11.Spencer PS, Mazumder R, Palmer VS, Lasarev MR, Stadnik RC, King P, et al. Environmental, dietary and case-control study of Nodding Syndrome in Uganda: A post-measles brain disorder triggered by malnutrition? J Neurol Sci. 2016;369:191–203. doi: 10.1016/j.jns.2016.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Wang DZ. Neurotoxins from marine dinoflagellates: A brief review. Mar Drugs. 2008;6:34971. doi: 10.3390/md20080016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davies FG. The historical and recent impact of Rift Valley fever in Africa. Am J Trop Med Hyg. 2010;83:73–4. doi: 10.4269/ajtmh.2010.83s2a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beckham JD, Pastula DM, Massey A, Tyler KL. Zika virus as an emerging global pathogen: Neurological complications of Zika virus. JAMA Neurol. 2016;73:875–9. doi: 10.1001/jamaneurol.2016.0800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powell JR. Mosquito-borne human viral diseases: Why Aedes aegypti? Am J Trop Med Hyg. 2018;98:1563–5. doi: 10.4269/ajtmh.17-0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reis J, Spencer PS, Román GC, Buguet A. Environmental neurology in the tropics. J Neurol Sci. 2021;421:117287. doi: 10.1016/j.jns.2020.117287. doi: 10.1016/j.jns. 2020.117287. [DOI] [PubMed] [Google Scholar]
- 17.Harris JB, Blain PG. Neurotoxicology: What the neurologist needs to know. J Neurol Neurosurg Psychiatry. 2004;75(Suppl 3):iii29–34. doi: 10.1136/jnnp.2004.046318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Block ML, Calderón-Garcidueñas L. Air pollution: Mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32:506–16. doi: 10.1016/j.tins.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cannon JR, Timothy Greenamyre J. The role of environmental exposures in neurodegeneration and neurodegenerative diseases. Toxicol Sci. 2011;124:225–50. doi: 10.1093/toxsci/kfr239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schaumburg HH. Human neurotoxic disease. In: Spencer PS, Schaumburg HH, editors. Experimental and Clinical Neurotoxicology. Oxford: Oxford University Press; 2000. pp. 55–82. [Google Scholar]
- 21.Kim H, Kim WH, Kim YY, Park HY. Air pollution and central nervous system disease: A review of the impact of fine particulate matter on neurological disorders. Front Public Health. 2020;8:575330. doi: 10.3389/fpubh.2020.575330. doi: 10.3389/fpubh. 2020.575330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cerza F, Renzi M, Gariazzo C, Davoli M, Michelozzi P, Forastiere F, et al. Long-term exposure to air pollution and hospitalization for dementia in the Rome longitudinal study. Environ Health. 2019;18:72. doi: 10.1186/s12940-019-0511-5. doi: 10.1186/s12940-019-0511-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobson JL, Jacobson SW. Intellectual impairment in children exposed to polychlorinated biphenyls in utero. N Engl J Med. 1996;335:783–9. doi: 10.1056/NEJM199609123351104. [DOI] [PubMed] [Google Scholar]
- 24.Grandjean P, Landrigan PJ. Neurobehavioral effects of developmental toxicity. Lancet Neurol. 2014;13:330–8. doi: 10.1016/S1474-4422(13)70278-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rauh VA, Perera FP, Horton MK, Whyatt RM, Bansal R, Hao X, et al. Brain anomalies in children exposed prenatally to a common organophosphate pesticide. Proc Natl Acad Sci. 2012;109:7871–76. doi: 10.1073/pnas.1203396109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jedrychowski WA, Perera FP, Camann D, Spengler J, Butscher M, Mroz E, et al. Prenatal exposure to polycyclic aromatic hydrocarbons and cognitive dysfunction in children. Environ Sci Pollut Res. 2015;22:3631–9. doi: 10.1007/s11356-014-3627-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ha S, Yeung E, Bell E, Insaf T, Ghassabian A, Bell G, et al. Prenatal and early life exposures to ambient air pollution and development. Environ Res. 2019;174:170–5. doi: 10.1016/j.envres.2019.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sram RJ, Veleminsky M, Jr, Veleminsky M, Sr, Stejskalova J. The impact of air pollution to central nervous system in children and adults. Neuro Endocrinol Lett. 2017;38:389–96. [PubMed] [Google Scholar]
- 29.Zeng Y, Lin R, Liu L, Liu Y, Li Y. Ambient air pollution exposure and risk of depression: A systematic review and meta-analysis of observational studies. Psychiatry Res. 2019;276:69–78. doi: 10.1016/j.psychres.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 30.Hajat A, Hazlehurst MF, Golden SH, Merkin SS, Seeman T, Szpiro AA, et al. The cross-sectional and longitudinal association between air pollution and salivary cortisol: Evidence from the Multi-Ethnic study of atherosclerosis. Environ Int. 2019;131:105062. doi: 10.1016/j.envint.2019.105062. doi: 10.1016/j.envint. 2019.105062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomson EM, Filiatreault A, Guenette J. Stress hormones as potential mediators of air pollutant effects on the brain: Rapid induction of glucocorticoid-responsive genes. Environ Res. 2019;178:108717. doi: 10.1016/j.envres.2019.108717. doi: 10.1016/j.envres. 2019.108717. [DOI] [PubMed] [Google Scholar]
- 32.Liang Z, Xu C, Cao Y, Kan HD, Chen RJ, Yao CY, et al. The association between short-term ambient air pollution and daily outpatient visits for schizophrenia: A hospital-based study. Environ Pollut. 2019;244:102–8. doi: 10.1016/j.envpol.2018.09.142. [DOI] [PubMed] [Google Scholar]
- 33.Legradi JB, Di Paolo C, Kraak MHS, et al. An ecotoxicological view on neurotoxicity assessment. Environ Sci Eur. 2018;30:46. doi: 10.1186/s12302-018-0173-x. doi: 10.1186/s12302-018-0173-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giordano G, Costa LG. Developmental neurotoxicity: Some old and new issues. ISRN Toxicol. 2012;2012:814795. doi: 10.5402/2012/814795. doi: 10.5402/2012/814795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Status of trace and toxic metals in Indian Rivers. River Data Compilation-2; Directorate Central Water Commission, Department of Water Resources, River Development & Ganga Rejuvenation. Ministry of Jal Shakti. August. 2019 [Google Scholar]
- 36.Jain D, Jain AK. Pollution: Past, present and future-an Indian perspective. Curr Sci. 2020;119:1087–92. [Google Scholar]