Abstract
Paediatric cervical spine trauma, though rare, is difficult to detect as the injuries are often soft-tissue injuries and thus not visible using conventional radiography. A 6-and-a-half-year-old child presented with neck pain following a fall. A thorough radiological workup over several days demonstrated soft-tissue injuries, undetected by initial cervical X-rays, requiring MRI to definitively prove. The patient recovered with conservative treatment.
Teaching Point: Paediatric cervical spine injuries often present with soft tissue injuries, which can missed on X-rays and require further imaging to detect.
Keywords: cervical spine injury, soft tissue injury, ligament injury, paediatric cervical spine, spine trauma
Introduction
Paediatric cervical spine trauma is rare, with an incidence only half of that of the adult population (1–1.3%), generally due to motor vehicle crashes (MVCs) (57.51%), followed by falls and sports [1,2]. Paediatric patients tend to suffer far more serious sequelae, up to 60% suffering permanent neurological damage and 40 to 50% dying, with death being inversely proportional to age [2].
Importantly, children are more susceptible to spinal cord injury without radiographic abnormality than adults, though by age 8 to 10 the injury pattern resembles that of the adult population as the spine has matured [2].
Case History
A 6-and-a-half-year-old boy presented to the emergency department with neck pain after falling from a bouncy castle. Initially, a cervical X-ray was ordered where a C3-C4 retrolisthesis was described (Figure 1). The patient was discharged with a foam collar, ibuprofen, and a follow-up orthopaedic appointment and CT exam. The CT exam was performed three days later, revealing a 2mm C4-C5 anterolisthesis, an increased interspinous process space, but no fractures (Figure 2), therefore the previous X-ray’s findings weren’t confirmed. The following day an MRI revealed C5-C6 interspinous ligament oedema, suggestive of a sprain, and superficial posterior paraspinal muscle oedema around C2 (Figures 3, 4). An orthopaedic surgeon prescribed physiotherapy and saw the patient once more a month later, at which point the patient showed no signs of lasting damage.
Figure 1.
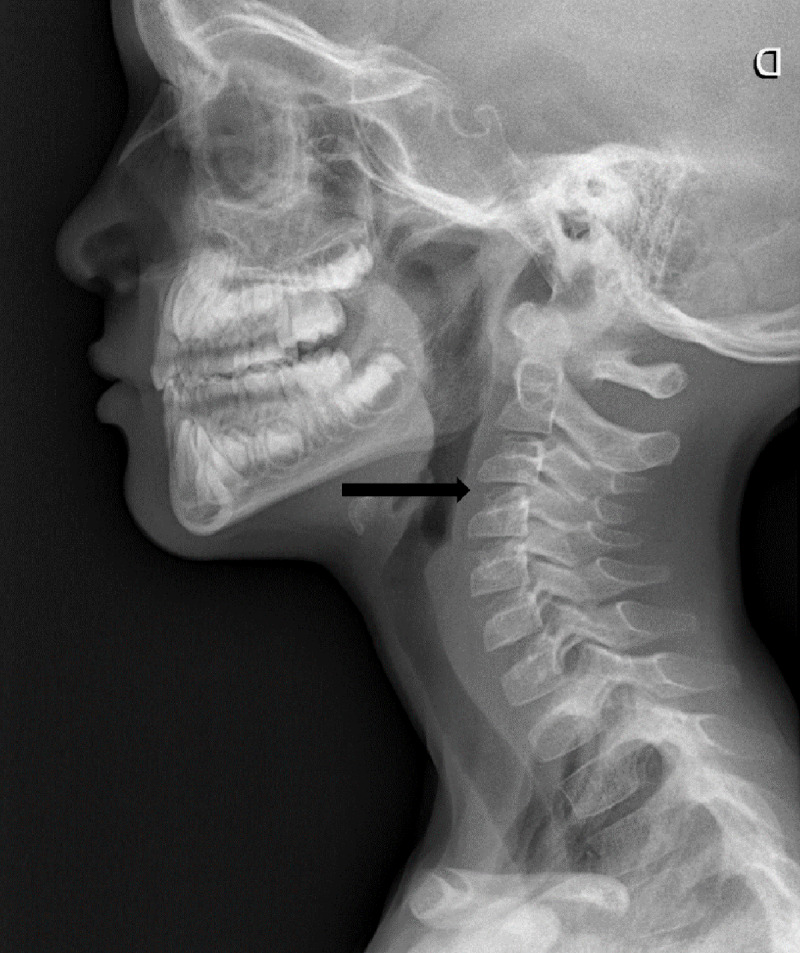
Initial lateral cervical X-ray where a discrete C3-C4 dislocation was described.
Figure 2.
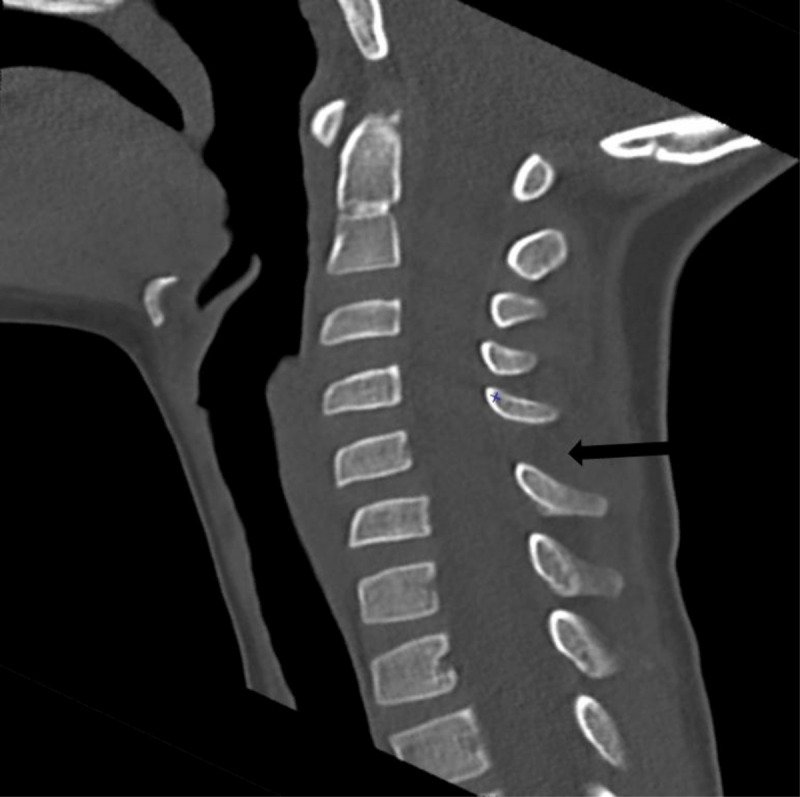
Follow-up CT exam revealing C4-C5 anterolisthesis and an increase in the corresponding interspinous space.
Figure 3.
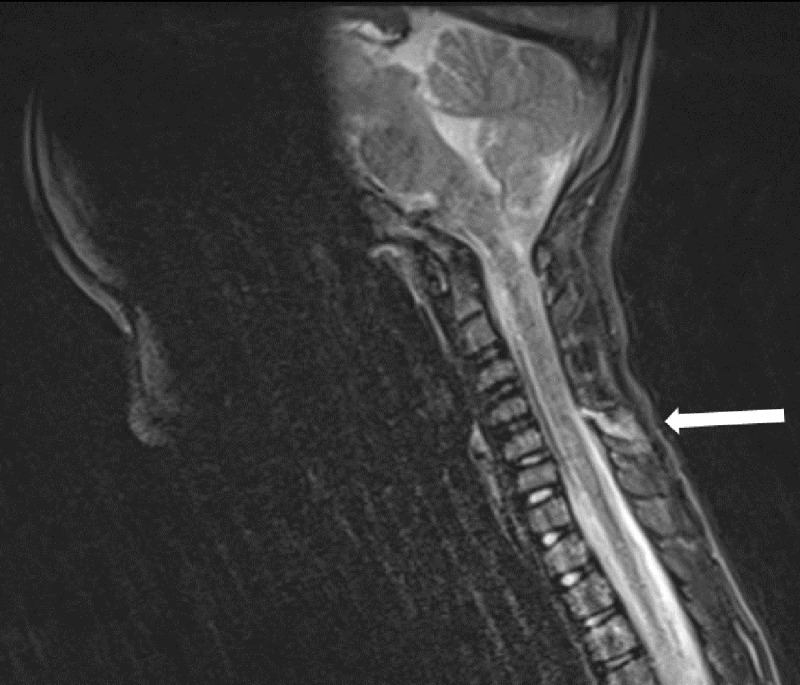
MRI showing C5-C6 interspinous ligament oedema.
Figure 4.

MRI showing left superficial posterior paramedian muscle oedema around C2.
Comment
Most paediatric vertebral injuries involve the cervical spine, as opposed to lumbar and thoracic spine injuries in adults [2]. They also more commonly involve ligament injury instead of bone injury [2]. The reason is that children’s ligaments are more lax than in adults and disproportionately weaker, which – alongside a proportionally larger head, horizontal facets, anteriorly wedge-shaped vertebral bodies, and incomplete ossification – increases the freedom of motion in children’s cervical spines as well as making those under 8 more susceptible to spinal injuries [1,2].
Eight predictors of cervical spine injuries, the PERCARN (Pediatric Emergency Care Applied Research Network) criteria, allowing detection of up to 98% of cervical spine injuries, are altered mental status, focal neurological deficit, torticollis, substantial torso injury, neck pain, predisposing medical conditions, diving, and high-risk MVCs [2,3].
The Easter Association for the Surgery of Trauma (EAST) deems CT the best initial modality regardless, in contrast to the American College of Radiology’s recommendations, which prefer X-rays [3]. For high-risk patients, CT exam is the preferred initial modality [2,3].
Lateral radiography is the most sensitive view for paediatric spine injury, though only 74–85% sensitive for fractures [2,3]. The odontoid view is controversial, being difficult to obtain, and adding little diagnostic information according to some, but increasing sensitivity up to 94% according to others [2,3]. Flexion and extension radiographs are not recommended initially but may be useful to follow up suspected ligamentous laxity [2,3]. Evaluation of spinal alignment involves assessment of the craniocervical junction, the anterior vertebral and posterior vertebral lines, spinolaminar lines, and posterior spinous lines [2,3].
The use of CT as a screening tool is debated, with some studies showing superior sensitivity whilst others finding no differences for significant injuries when compared to standard radiographs [2]. It should be noted, however, that even a negative CT exam cannot fully exclude spinal injury without corroborating clinical findings, in which case an MRI may be needed if one is unable to fully clear a cervical spine within three days [2,3].
Finally, MRI is the most specific and sensitive method for paediatric spine trauma but has limited availability and is subject to other technical barriers like the need for anaesthesia [2]. However, MRI is the preferred method in acute neurological abnormalities [2].
In the paediatric population soft tissue and ligamentous injuries are more common and may be the only signs of injury [2,3]. These can present as soft tissue swelling, as was the case for our patient, or osseous misalignment [2]. Some signs, such as prevertebral oedema, epidural hematoma and interspinal or paraspinal oedema are present in over 50% of cervical spine injury cases [3].
Of the types of injuries than can occur AOSpine B injuries (distraction) occur most frequently in children under 3 and decrease with age. These tend to be injuries of the posterior tension band, seen as widening of the interspinous distance or uncovering of the facets [3].
The clinical significance of findings such as soft tissue contusion, oedema in the interspinous ligaments with intact anterior and middle pillars and isolated disruption of the nuchal ligament is unclear [3]. When a paediatric cervical spine lesion is detected, however, around 30–40% of will require surgery [3].
Conclusion
Paediatric spine injuries are relatively rare, can be difficult to detect, and are an important entity due to their high morbidity, mortality, and the frequent necessity of surgery [2,3]. The imaging approach is both case and centre specific, with either radiography or CT being the preferred initial modality.
Competing Interests
The authors have no competing interests to declare.
References
- 1.Madura CJ, Johnston JM. Classification and management of pediatric subaxial cervical spine injuries. Neurosurg Clin N Am. 2017; 28(1): 91–102. DOI: 10.1016/j.nec.2016.07.004 [DOI] [PubMed] [Google Scholar]
- 2.McAllister AS, Nagaraj U, Radhakrishnan R. Emergent imaging of pediatric cervical spine trauma. Radiographics. 2019; 39(4): 1126–1142. DOI: 10.1148/rg.2019180100 [DOI] [PubMed] [Google Scholar]
- 3.Wang MX, Beckmann NM. Imaging of pediatric cervical spine trauma. Emerg Radiol. 2021; 28(1): 127–141. DOI: 10.1007/s10140-020-01813-1 [DOI] [PubMed] [Google Scholar]


