Abstract
Aims
Cytomegalovirus (CMV) is a preventable cause of neurodevelopmental disability. Australian guidelines recommend that pregnant women are informed about CMV to reduce their risk of infection; however, less than 10% of maternity health professionals routinely provide prevention advice. The aim was to develop and evaluate the effectiveness of an eLearning course for midwives to improve knowledge and confidence about CMV.
Materials and Methods
Participants undertaking the course between March and November 2020 were invited to complete an evaluation questionnaire: before the course (T1), immediately after (T2) and three months post completion (T3). A linear mixed model was used to evaluate change in participant scores; P < 0.05 was considered statistically significant.
Results
Midwives (316/363, 87%), midwifery students (29/363, 8%) and nurses (18/363, 5%) participated. At T1 80% indicated they had not received education about CMV. Total adjusted mean scores for questionnaires completed between T1 (n = 363) and T2 (n = 238) increased significantly (from 17.2 to 22.8, P < 0.001). Limited available T3 scores (n = 27) (−1.7, P < 0.001), while lower than T2, remained higher than at T1 (+3.6, P < 0.001). Participants’ awareness of CMV information resources improved from 10 to 97% from T1 to T2. Confidence in providing CMV advice increased from 6 to 95% between T1 and T2 (P < 0.001) and was maintained at T3. Almost all (99%) participants indicated they would recommend the course to colleagues.
Conclusion
Participants who completed the eLearning course had significantly improved knowledge and confidence in providing advice about CMV. Programs targeting other maternity health professionals should be considered, to further support the implementation of the congenital CMV prevention guidelines.
Keywords: cytomegalovirus, primary prevention, developmental disability, pregnancy, distance education.
INTRODUCTION
Cytomegalovirus (CMV) is a common herpesvirus that is transmitted from person to person via bodily fluids, including urine, saliva, blood and semen. 1 Women who work with and/or care for young children are at the highest risk of acquiring CMV infection. 1 If a pregnant woman acquires CMV for the first time (maternal primary infection) particularly in the first trimester or has CMV reactivation in pregnancy, a resulting congenital infection can cause damage to the developing fetus. 2 In Australia, more than 1800 infants are born with congenital CMV (cCMV) each year. 3 Approximately 400 of these will go on to have long‐term neurodevelopmental disabilities, including progressive sensorineural hearing loss, epilepsy, intellectual impairment and cerebral palsy. 1 , 3 , 4 , 5 , 6 , 7 , 8 , 9
In the absence of an effective vaccine, the best primary prevention strategy for CMV infection in pregnancy is education on hygiene precautions to reduce the risk of maternal infection. 10 Hygiene precautions are effective in reducing CMV seroconversion during pregnancy, and women find receiving information about prevention to be both acceptable and useful. 11 , 12 , 13 , 14 , 15 International and Australian guidelines now recommend that all pregnant women should be provided with information about CMV and steps to reduce the risk of infection in pregnancy. 10 , 16 , 17 , 18
However, awareness of CMV internationally is low. 19 In Australia only one in six pregnant women are aware of the virus, 12 and <10% of maternity health professionals routinely discuss CMV prevention with pregnant women in their care. 20 Barriers to counselling identified to date include lack of knowledge about CMV, prevention strategies and interpreting serology testing; coupled with a lack of confidence discussing CMV; and a lack of clinical guidelines and information resources. 20 The promulgation of new Australian clinical guidelines 16 , 18 provided the impetus for the development of an eLearning course, Congenital cytomegalovirus: prevention is in your hands. The aim of this study was to evaluate the effectiveness of the eLearning course in improving maternity health professionals’ knowledge of CMV and confidence in providing CMV prevention advice to pregnant women.
MATERIAL AND METHODS
We performed an evaluation of maternity health professionals’ knowledge, attitudes and behaviours about CMV, before and after they completed a CMV eLearning course.
The eLearning course was developed by the Cerebral Palsy Alliance Research Institute, CMV Australia and an expert reference group which included midwives, maternal fetal medicine specialists, paediatric infectious disease specialists, a virologist, a neonatologist, epidemiologists and families of children who had been impacted by cCMV. Adult learning principles were applied to the development and provision of the course: taking the course was voluntary, participation self‐initiated; participants controlled the pace of their learning; case examples prompted reflection and active recording; the program was relevant to participants’ practice and aligned with current clinical practice guidelines. 21
The 2‐h course included five modules (Fig. 1). Users accessed the course via the Australian College of Midwives (ACM) Learning Management System (LMS). ACM promoted the course on its website, social media platforms and directly to members via its eNewsletters and member magazine. The course was free, and on completion participants were eligible to claim two continuing professional development (CPD) hours.
Figure 1.
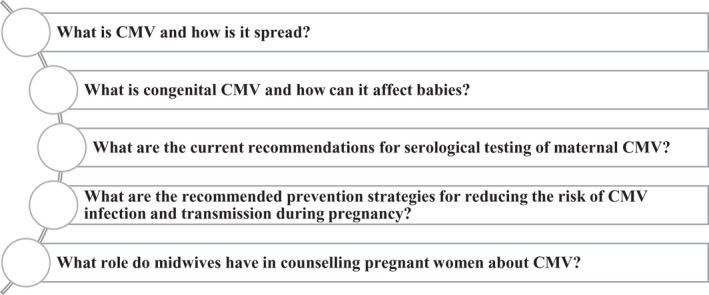
‘Congenital cytomegalovirus: prevention is in your hands’ eLearning course modules.
Participants who undertook the course between March and December 2020 were invited to participate in the evaluation via written text and a participant information sheet embedded in the online course. Participation was optional and included a request to complete three short (<10 min) questionnaires at three time points: pre‐course (T1), immediately post‐course (T2) and three months post‐course completion (T3). A link to the T3 questionnaire was sent to participants by email. An additional automated reminder email was sent to those who did not complete the survey within a month of the initial email, and participants who completed all three questionnaires were eligible to enter a draw to receive a gift voucher. The questionnaires contained multiple‐choice questions and were designed to test participant knowledge against each of the five modules. A score of one or zero was given for each item with a maximum total score of 25. Participants were asked demographic questions: their role, practice location, length of practice, whether they had previously received CMV education, practise regarding CMV counselling in the last month (I counselled every woman/almost all the women/about half the women/no women in my care, I do not discuss CMV, not currently practising), confidence in providing information about CMV (I feel confident about giving advice and answering questions about CMV in pregnancy: strongly agree, agree, neutral, disagree, strongly disagree) and awareness of and where to access CMV resources. Post‐course participants were asked whether they would recommend the course to colleagues, what could be improved and what they perceived the main take‐home course messages to be (Appendix S1).
Statistical analyses
Participant demographic data at each time point was analysed using descriptive statistics. A generalised linear mixed‐effects model with a random intercept was used to evaluate change in participant questionnaire scores at each time point while accounting for within‐subject correlation. As both previous CMV education and length of practice were factors that had a significant effect on the mean score these were controlled for within the model. An ordinal regression model with a random intercept, controlling for prior CMV education and length of practice, was used to investigate changes in participant responses to statements about confidence in giving advice about CMV and CMV counselling practice over time. Changes in participant awareness of CMV resources were investigated using a logistic regression model with a random intercept that similarly controlled for prior CMV education and length of practice. Participant responses regarding the main take‐home messages from the course were categorised by theme. Proportional representation of the frequency of responses under each theme was displayed in a bubble chart using Tableau software. A P‐value of <0.05 was considered statistically significant. Statistical analyses were performed in R, using the packages lme4 and ordinal.
Ethics
This research was conducted with the approval of the University of Sydney Human Research Ethics Committee (Project number: 2019/1020).
RESULTS
Participants
Participants were 87% midwives (316/363), 8% (29/363) midwifery students and 5% (18/363) nurses. Most participants (291/363, ≈80%) had not previously received education about CMV. Length of practice varied widely. Almost all participants were practising in Australia, with the majority in metropolitan public practice (Table 1).
Table 1.
Participants’ roles, practise details and previous cytomegalovirus (CMV) education
|
Pre‐course questionnaire (T1) |
Post‐course questionnaire (T2) |
three‐month follow‐up questionnaire (T3) |
|
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| n = 363 | n = 238 | n = 27 | |
| Role | |||
| Midwife | 298 (82.1) | 200 (84) | 22 (81.5) |
| Midwife with endorsement | 18 (5.0) | 11 (4.6) | 3 (11.1) |
| Midwifery student | 29 (9.0) | 14 (5.9) | |
| Other † | 18 (5.0) | 13 (5.5) | 2 (7.4) |
| Missing | 0 | 0 | 0 |
| Time practising in the field | |||
| Student | 30 (8.3) | 15 (6.3) | |
| Less than 5 years | 114 (31.4) | 76 (31.9) | 2 (7.4) |
| 5–9 years | 63 (17.4) | 38 (16.0) | 4 (14.8) |
| 10–14 years | 51 (14.0) | 35 (14.7) | 7 (25.9) |
| 15 years or more | 105 (28.9) | 74 (31.1) | 14 (51.9) |
| Missing | 0 | 0 | 0 |
| Practice location – country | |||
| Australia | 354 (97.5) | 230 (97.5) | 27 (100) |
| Overseas ‡ | 8 (2.2) | 6 (2.5) | ‐ |
| Missing | 3 | 2 | 0 |
| Australian practice state/territory | |||
| ACT/NSW | 101 (29.1) | 71 (31.4) | 11 (40.7) |
| NT | 6 (1.7) | 2 (0.9) | 1 (3.7) |
| QLD | 73 (21.0) | 43 (19.0) | 7 (25.9) |
| VIC | 81 (23.3) | 59 (26.1) | 2 (7.4) |
| SA | 24 (6.9) | 15 (6.6) | ‐ |
| TAS | 3 (0.9) | 2 (0.9) | ‐ |
| WA | 59 (17.0) | 34 (15.0) | 4 (14.8) |
| Not practising/practising outside of Australia | 16 | 12 | 0 |
| Practice location – remoteness | |||
| Metropolitan | 221 (60.9) | 144 (60.5) | 15 (55.6) |
| Regional | 95 (26.2) | 65 (27.3) | 7 (25.9) |
| Rural | 38 (10.5) | 23 (9.7) | 3 (11.1) |
| Remote | 9 (2.5) | 6 (2.5) | 2 (7.4) |
| Missing | 0 | 0 | 0 |
| Practice type | |||
| Public practice | 272 (74.9) | 181 (76.1) | 21 (77.8) |
| Private practice | 22 (6.1) | 15 (6.3) | 3 (11.1) |
| Mixed public and private | 22 (6.1) | 14 (5.9) | 2 (7.4) |
| N/A currently not working | 20 (5.5) | 15 (6.3) | 1 (3.7) |
| N/A currently a student | 27 (7.4) | 13 (5.5) | ‐ |
| Missing | 0 | 0 | 0 |
| Previously received CMV education | |||
| Yes | 72 (19.8) | 47 (19.7) | 7 (25.9) |
| No | 291 (80.2) | 191 (80.3) | 20 (74.1) |
| Missing | 0 | 0 | 0 |
Other includes fertility nurse, registered nurses, maternal and child health nurse.
Botswana, Estonia, Indonesia, Ireland, Japan, New Zealand, Singapore.
Participant knowledge
Questionnaires were completed by 363 participants at T1, 238 at T2 (66%) and 27 at T3 (7%). Adjusted total mean scores between T1 and T2 significantly improved with an increase of +5.56 (from 17.2 to 22.8, P < 0.001). Using limited available T3 data, the total mean score decreased between T2 and T3 (−1.71, p < 0.001); however, the mean T3 score remained significantly higher than prior to the course (20.8, +3.6, P < 0.001) (Table 2).
Table 2.
Participant responses to knowledge evaluation questionnaires, unadjusted and adjusted means and estimated change between time points
|
T1 Pre‐course questionnaire n = 363 Unadjusted mean (SD) |
T1 Pre‐course questionnaire n = 363 Adjusted mean (95% CI) |
T2 Post‐course questionnaire n = 238 Unadjusted mean (SD) |
T2 Post‐course questionnaire n = 238 Adjusted mean (95% CI) |
T1–T2 Est. Change P |
T3 three‐month follow‐up questionnaire n = 27 Unadjusted mean (SD) |
T3 three‐month follow‐up questionnaire n = 27 Adjusted mean (95% CI)e |
T2–T3 Est. Change P |
T1–T3 Est. Change P |
|
|---|---|---|---|---|---|---|---|---|---|
| MODULES Maximum score = 5 | |||||||||
|
Module 1 What CMV † is and how it is spread |
3.1 (1.4) | 3.1 (3.0, 3.3) | 4.7 (0.6) | 4.7 (4.50, 4.85) |
1.6 <0.001 |
4.5 (0.6) | 4.4 (4.0, 4.8) |
−0.2 <0.05 |
1.3 <0.001 |
|
Module 2 What cCMV‡ is and how it can affect babies |
2.8 (1.0) | 2.7 (2.6, 2.9) | 4.1 (0.8) | 4.0 (3.92, 4.19) |
1.3 <0.001 |
3.6 (0.9) | 3.4 (3.0, 3.7) |
−0.7 (0.001) |
0.6 <0.001 |
|
Module 3 The current recommendations for serological testing of maternal CMV |
3.8 (0.9) | 3.8 (3.7, 3.9) | 4.7 (0.7) | 4.6 (4.51, 4.77) |
0.9 <0.001 |
4.6 (0.7) | 4.3 (4.0, 4.6) |
−0.3 < 0.05 |
0.5 <0.001 |
|
Module 4 The recommended prevention strategies for reducing the risk of CMV infection and transmission during pregnancy |
3.1 (1.4) | 3.1 (2.9, 3.2) | 4.5 (0.6) | 4.5 (4.35, 4.70) |
1.4 <0.001 |
4.1 (0.5) | 4.0 (3.6, 4.4) |
−0.5 <0.001 |
0.9 <0.001 |
|
Module 5 The role of midwives in counselling pregnant women about CMV |
4.5 (0.8) | 4.5 (4.4, 4.6) | 4.9 (0.3) | 4.9 (4.71, 4.48) |
0.4 <0.001 |
4.9 (0.3) | 4.7 (4.5, 4.9) |
No change 0.3 |
0.2 0.06 |
| TOTAL SCORE Maximum score = 25 | |||||||||
| Total Score | 17.3 (3.6) | 17.2 (16.8, 17.6) | 22.9 (2.1) | 22.8 (22.3, 23.2) |
5.6 <0.001 |
21.7 (1.9) | 20.8 (19.7, 21.8) |
−1.7 <0.001 |
3.6 <0.001 |
The bold differentiate the data in columns with Adjusted versus Unadjusted Data.
CMV: cytomegalovirus.
cCMV: congenital cytomegalovirus.
Investigation of changes in adjusted mean scores by module revealed significant improvements across all modules between T1 and T2 (P < 0.001). Participant knowledge varied across modules, with the lowest adjusted baseline mean scores for Module 2 and Module 4 (adjusted mean T1 scores 2.7 and 3.1, respectively). Participants had the most difficulty correctly answering questions pertaining to neonatal signs of cCMV disease (eg petechial rash), long‐term outcomes (eg most babies born with cCMV will not have cCMV disease, but cCMV can cause hearing loss, intellectual impairment, epilepsy and cerebral palsy), risk reduction (eg avoid contact with saliva) and how long children excrete CMV (eg up to two years). 22 , 23
Module 5 included content about CMV information resources for pregnant women, maternity health professionals and the general community. Key learnings from Modules 1 to 4 (eg CMV is the most common infection passed from mother to baby during pregnancy) were also summarised in this module. Participants had high scores at all time points for Module 5 (adjusted mean at T1:4.5, T2 4.9, T3 4.7) with no significant changes observed between T2 and T3 or between T1 and T3.
Participant confidence
Changes in participant confidence were measured by response to the following statement ‘Ifeel confident about giving advice and answering questions about CMV in pregnancy’. At T1, 22/262 (6%) of midwives indicated that they agreed or strongly agreed with this statement compared with 227/238 (95%) at T2 (T1–T2: P < 0.001). Limited data available at T3 indicated that 19/27 (70%) agreed or strongly agreed with this statement (T1–T3: P < 0.001).
Awareness of CMV education resources available for pregnant women and families
Prior to completing the course (T1) very few participants (37/361, 10%) were aware of available CMV education resources. At T2, 232/238 (97%) (P ≤ 0.001) of respondents were aware of how to access free CMV education resources for women and families through the Department of Health, Cerebral Palsy Alliance Research Institute and CMV Australia.
Providing advice to women about CMV
At T1 and T3 participants were asked about their practice in providing CMV advice to women in their care over the previous month. At T1, 70% (188/270) of practicing midwives indicated they did not discuss CMV with women in their care. Analysis of available data at T3 showed that this had dropped to 22% (5/22) (P < 0.001) (Supplemental Figure S1).
Main take‐home messages from the course
At T2 participants were asked to list their main take‐home messages from the course. The most common response (122/183 respondents, 66%) was the importance of educating all women about CMV infection. This was followed by the simple hygiene strategies for reducing the risk/prevention of CMV transmission (75/183 respondents, 41%) and that CMV is very common (36/183 respondents, 20%). (See Figure 2.)
Figure 2.
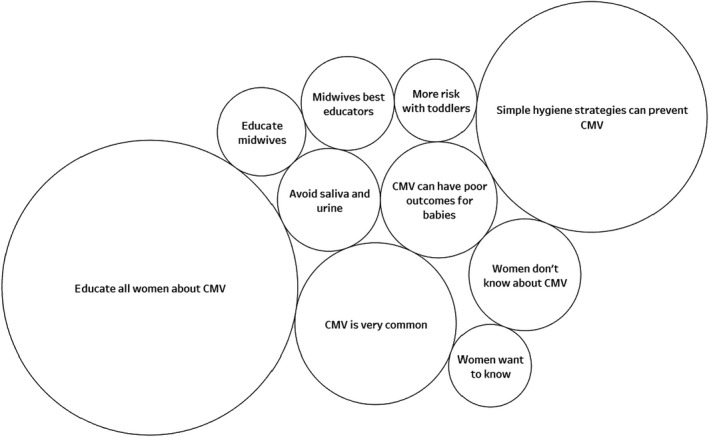
Proportional representation of main take‐home messages immediately post‐course by theme.
Changes and recommendations
At T2, a small proportion (24/296, 8%) of respondents indicated they had experienced some difficulty navigating the course. A minority (5/296, 2%) felt that the course should contain more information, while others (3/296, 1%) reported it was too long. Almost all (233/238, 99%) indicated that they would recommend the course to their colleagues.
DISCUSSION
Counselling about CMV hygiene practices has been shown to reduce rates of seroconversion in pregnant women. 11 , 14 , 15 However, in Australia, CMV counselling in prenatal or antenatal care is often neglected. 20 The Congenital cytomegalovirus: prevention is in your hands eLearning course was designed using adult learning principles and developed to support the implementation of the 2019/20 cCMV prevention guidelines which recommend that pregnant women and women planning pregnancy are given information about CMV prevention. 16 , 18 Midwives’ knowledge about CMV and confidence in providing CMV advice improved significantly after course completion. This knowledge translated into self‐reported behaviour change as midwives indicated that they were more likely to provide information to pregnant women about CMV after completing the course. This research supports the effectiveness of the eLearning delivery model and highlights the demand for appropriate education and support for maternity health professionals to ensure women and families receive important CMV prevention advice.
The majority (>80%) of participants reported they had not received CMV education prior to completing this course. This was evident in terms of low pre‐course knowledge of the routes of transmission, clinical outcomes of cCMV disease and awareness of strategies to reduce the risk of transmission. In line with previous research, pre‐course confidence was low, with most midwives not providing CMV advice to women in their care. 19 , 20 , 24
The midwives involved in this study reported they were aware of the importance of their role in informing pregnant women about CMV, as evidenced by high baseline scores for Module 5. Specific barriers to providing advice have been identified by maternity health professionals in Australia and include a (previous) lack of clinical guidelines to guide practice, a (previous) lack of educational resources for parents, lack of knowledge, concern that CMV advice could make parents anxious and the incorrect belief that cCMV infection is rare, with prevention impossible. 20 By addressing each of these items in turn within the eLearning course it was possible to significantly improve CMV knowledge, participant confidence and the proportion of midwives providing CMV advice to women. This mirrors previous research which identified that the best‐informed maternity health professionals counsel women on CMV hygiene precautions most frequently. 25 Supporting midwives to feel confident in sharing CMV risk reduction strategies is important as midwives are a trusted source of information for pregnant women 12 and are well placed to share information regarding cCMV in the same way they do for less common congenital infections (eg listeria and toxoplasmosis) and other important healthy pregnancy behaviours, such as avoiding smoking and alcohol. 16 , 26 , 27
The use of an eLearning format had a number of advantages. Compared with face‐to‐face teaching, an online format enhanced national reach, including those living in rural and remote areas, and ensured consistency of content. It also provided flexible, self‐paced learning. By embedding videos within the course, participants learnt from topic experts and from families who had been impacted by cCMV. Launched in March 2020, at the beginning of the first wave of COVID‐19 and the subsequent lockdowns in many Australian states, the eLearning format was an accessible and inexpensive option for delivering CMV education. eLearning is becoming more popular, and emerging research suggests this format is as effective as traditional learning approaches and acceptable to maternity health professionals. 28 , 29 , 30
The main limitation of this study was the loss of participants to follow‐up at T3. Despite our best efforts to encourage completion of all three questionnaires including reminder emails and the opportunity to enter a draw to win a gift voucher, the three‐month follow‐up numbers were 7.4% (27/363) of baseline participant numbers. This introduces a high risk of bias in T3 outcomes due to missing data. The use of mixed‐effects models goes some way to mitigating this issue; the inclusion of a random intercept helps to account for baseline differences between dropouts and non‐dropouts. To investigate this issue further we considered the effect of demographic features in the T3 group in the linear mixed‐effects model. Practice type and location in the T3 group were comparable to the larger baseline group, and these factors had no‐significant impact on the model. The T3 group had higher proportions of participants who had practised for >15 years and who had had previous cCMV education, and these had a significant effect in the model. To control for any confounding effect of length of practice and previous cCMV education on the outcomes considered, these factors were included in the mixed‐effects models used in the analyses.
A further limitation was that we did not explore what other strategies could support implementation of the CMV prevention guidelines beyond this education piece, for example engaging dedicated implementation leaders. These leaders could identify hospital‐specific enablers and barriers to implementation; location‐specific solutions to these barriers; in‐servicing solutions to support education for new staff; mechanisms to ensure educational materials are readily available, and could complete auditing of whether pregnant women are given CMV prevention advice to measure implementation progress. 26 , 31 New research is required to investigate whether these kinds of strategies would be useful for CMV prevention messaging, and whether they lead to a reduction in cCMV infection.
This is the first CMV education course for midwives to be developed and evaluated in the Australian context. The evaluation of this freely available resource demonstrated engagement from midwives and midwifery students from across Australia, with participation spread across metropolitan, rural and remote regions. To date more than 800 midwives have registered for this course which continues to be freely available through ACM. Building on this success, programs targeting other maternity health professional groups (eg obstetricians and general practitioners) and women planning pregnancy should be developed to support implementation of CMV prevention messaging. Freely accessible CMV educational resources and informed healthcare workers practicing according to national practice cCMV guidelines 16 , 18 are strong foundations for reducing and preventing the neurodevelopmental disabilities associated with cCMV infection.
Supporting information
Figure S1. Proportion of midwives who provided CMV advice in the last month.
Appendix S1. Questionnaires.
ACKNOWLEDGEMENTS
We would like to acknowledge the support of the expert reference group which includes the author group and Adam Bartlett, Meagan Bielski, Caroline Carr, Kate Dyer, Amye Eden, Wendy Foster, Shona Goldsmith, Beverley Hall, Wendy Hermel, John Keogh, Tanya Martin, Brendan McMullan, Natasha Nassar, Shauna Newman, Michael Peek, Hala Phipps, Karen Richards and Alice Welby. Additionally, we would like to thank Bree, Mitch, Dylan and Dax Pennie, Tracy Donavon and Mel Lewis for their support in developing the eLearning content for the eLearning module. We acknowledge and thank the Australian College of Midwives Education Team for their support in the development of the eLearning module, with special thanks to Cassie Powditch. HSS received salary support through a National Health and Medical Research Council of Australia Early Career Fellowship (no. 1144566) and Australasian Cerebral Palsy Clinical Trials Network. Funding to support the development of the eLearning course was received from Cerebral Palsy Alliance Grants Foundation, Gandel Philanthropy, The Profield Foundation and CMV Australia. Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Conflicts of Interest: The authors report no conflicts of interest.
Contributor Information
Hayley Smithers‐Sheedy, Email: hsmitherssheedy@cerebralpalsy.org.au.
Katherine Swinburn, Email: kath.swinburn@cerebralpalsy.org.au.
REFERENCES
- 1. Manicklal S, Emery VC, Lazzarotto T et al. The "silent" global burden of congenital cytomegalovirus. Clin Microbiol Rev 2013; 26: 86–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cheeran MC, Lokensgard JR, Schleiss MR. Neuropathogenesis of congenital cytomegalovirus infection: disease mechanisms and prospects for intervention. Clin Microbiol Rev 2009; 22: 99–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McMullan BJ, Palasanthiran P, Jones CA et al. Congenital cytomegalovirus–time to diagnosis, management and clinical sequelae in Australia: opportunities for earlier identification. Med J Aust 2011; 194: 625–629. [DOI] [PubMed] [Google Scholar]
- 4. Kenneson A, Cannon MJ. Review and meta‐analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev Med Virol 2007; 17: 253–276. [DOI] [PubMed] [Google Scholar]
- 5. Smithers‐Sheedy H, Raynes‐Greenow C, Badawi N et al. Congenital cytomegalovirus among children with cerebral palsy. J Pediatr 2017; 181: 267–271.e1. [DOI] [PubMed] [Google Scholar]
- 6. Smithers‐Sheedy H, Raynes‐Greenow C, Badawi N et al. Congenital cytomegalovirus is associated with severe forms of cerebral palsy and female sex in a retrospective population‐based study. Dev Med Child Neurol 2014; 56(9): 846–852. [DOI] [PubMed] [Google Scholar]
- 7. Dollard SC, Grosse SD, Ross DS. New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Rev Med Virol 2007; 17: 355–363. [DOI] [PubMed] [Google Scholar]
- 8. Townsend CL, Forsgren M, Ahlfors K et al. Long‐term outcomes of congenital cytomegalovirus infection in Sweden and the United Kingdom. Clin Infect Dis 2013; 56: 1232–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Grosse SD, Ross DS, Dollard SC. Congenital cytomegalovirus (CMV) infection as a cause of permanent bilateral hearing loss: a quantitative assessment. J Clin Virol 2008; 41: 57–62. [DOI] [PubMed] [Google Scholar]
- 10. Rawlinson WD, Boppana SB, Fowler KB et al. Congenital cytomegalovirus infection in pregnancy and the neonate: consensus recommendations for prevention, diagnosis, and therapy. Lancet Infect Dis 2017; 17(6): 177–188. [DOI] [PubMed] [Google Scholar]
- 11. Picone O, Vauloup‐Fellous C, Cordier AG et al. A 2‐year study on cytomegalovirus infection during pregnancy in a French hospital. BJOG 2009; 116: 818–823. [DOI] [PubMed] [Google Scholar]
- 12. Lazzaro A, Vo ML, Zeltzer J et al. Knowledge of congenital cytomegalovirus (CMV) in pregnant women in Australia is low, and improved with education. Aust NZ J Obstet Gynaecol 2019; 59: 843–849. [DOI] [PubMed] [Google Scholar]
- 13. Thackeray R, Magnusson BM. Women's attitudes toward practicing cytomegalovirus prevention behaviors. Prev Med Rep 2016; 4: 517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vauloup‐Fellous C, Picone O, Cordier AG et al. Does hygiene counseling have an impact on the rate of CMV primary infection during pregnancy? Results of a 3‐year prospective study in a French hospital. J Clin Virol 2009; 46(Suppl 4): S49–S53. [DOI] [PubMed] [Google Scholar]
- 15. Revello MG, Tibaldi C, Masuelli G et al. Prevention of primary cytomegalovirus infection in pregnancy. EBioMedicine 2015; 2: 1205–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Department of Health . Clinical Practice Guidelines: Pregnancy Care. Canberra: Australian Government Department of Health, 2020. [Google Scholar]
- 17. Palasanthiran P, Starr M, Jones C, Giles M. Management of perinatal infections. In: Palasanthiran P, Starr M, Jones C, Giles M, eds. Australasian Society for Infectious Diseases, 2014. [Google Scholar]
- 18. RANZCOG . Prevention of congenital cytomegalovirus (CMV) infection. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists 2019.
- 19. Midgley G, Smithers‐Sheedy H, McIntyre S et al. Congenital cytomegalovirus prevention, awareness and policy recommendations ‐ a scoping study. Infect Disord Drug Targets 2020; 20: 291–302. [DOI] [PubMed] [Google Scholar]
- 20. Shand AW, Luk W, Nassar N et al. Cytomegalovirus (CMV) infection and pregnancy‐potential for improvements in Australasian maternity health providers' knowledge. J Matern Fetal Neonatal Med 2018; 31: 2515–2520. [DOI] [PubMed] [Google Scholar]
- 21. Collins J. Education techniques for lifelong learning: principles of adult learning. Radiographics 2004; 24: 1483–1489. [DOI] [PubMed] [Google Scholar]
- 22. Adler SP. Cytomegalovirus and child day care. Evidence for an increased infection rate among day‐care workers. N Engl J Med 1989; 321: 1290–1296. [DOI] [PubMed] [Google Scholar]
- 23. Pass RF, Little EA, Stagno S et al. Young children as a probable source of maternal and congenital cytomegalovirus infection. N Engl J Med 1987; 316: 1366–1370. [DOI] [PubMed] [Google Scholar]
- 24. Pereboom MTR, Manniën J, Spelten ER et al. Maternal cytomegalovirus infection prevention: the role of Dutch primary care midwives. Midwifery 2014; 30: 1196–1201. [DOI] [PubMed] [Google Scholar]
- 25. Fellah T, Sibiude J, Vauloup‐Fellous C et al. Evolution of awareness and knowledge of congenital cytomegalovirus infection among health care providers in France between 2011 and 2018. J Clin Virol 2020; 129: 104335. [DOI] [PubMed] [Google Scholar]
- 26. Andrews CJ, Ellwood DA, Gordon A et al. Stillbirth in Australia 2: Working together to reduce stillbirth in Australia: the Safer Baby Bundle initiative. Women Birth 2020; 33: 514–519. [DOI] [PubMed] [Google Scholar]
- 27. Women want to know FARE. https://fare.org.au/women‐want‐to‐know/ 2021.
- 28. Sinclair PM, Kable A, Levett‐Jones T, Booth D. The effectiveness of Internet‐based e‐learning on clinician behaviour and patient outcomes: a systematic review. Int J Nurs Stud 2016; 57: 70–81. [DOI] [PubMed] [Google Scholar]
- 29. Vaona A, Banzi R, Kwag KH et al. E‐learning for health professionals. Cochrane Database Syst Rev 2018; 1: CD011736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. D'Aloja P, Maraschini A, Lega I et al. Acceptance of e‐learning programs for maternity health care professionals implemented by the Italian obstetric surveillance system. J Contin Educ Health Prof 2020; 40: 289–292. [DOI] [PubMed] [Google Scholar]
- 31. Gatman K, May R, Crowther C. Survey on use of antenatal magnesium sulphate for fetal neuroprotection prior to preterm birth in Australia and New Zealand ‐ Ongoing barriers and enablers. Aust NZ J Obstet Gynaecol 2020; 60: 44–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Proportion of midwives who provided CMV advice in the last month.
Appendix S1. Questionnaires.


