Abstract
Objective
Around 40% of oncology patients receive inadequate pain treatment. A previous study reported pain interventions for only 70% of patients who reported unacceptable pain at the self‐service registration desk. The aim of this study is to gain insight in reasons for the absence of pain intervention among oncology patients who reported unacceptable pain.
Methods
In this mixed methods study, 20 patients visiting the oncology outpatient clinic were selected via patient record assessment and interviewed about their perceived reasons for absence of pain intervention.
Results
The reasons mentioned by the patients for absence of pain intervention included reluctance of the patient to discuss pain, no treatment preferred by the patient, focus of the physician on treatment of the disease, pain treatment difficult or impossible, and the perception that pain is an inevitable consequence of the cancer treatment. Almost 50% of the patients considered the physician responsible for the absence of pain intervention.
Conclusion
In conclusion, a variety of reasons for absence of pain intervention are reported by patients, including patient‐related and health professional‐related reasons. Improvements can be made by promoting regular discussion of pain during hospital visits and empowerment of patients.
Keywords: cancer pain, empowerment, oncology, pain management, patients, perception
1. INTRODUCTION
Pain is one of the most frequently experienced symptoms in oncology patients, with moderate to severe pain being reported by over 50% of patients (Bennett et al., 2017). Among other consequences, untreated cancer‐related pain can lead to decreased mobility, social isolation and diminished quality of life for the patient and emotional distress for the patient, family and caregivers (Neufeld et al., 2017; Rodriguez et al., 2019; van den Beuken‐van Everdingen et al., 2016). Pain experienced by oncology patients can be caused by the cancer or treatment or be unrelated to the disease (Fink & Gallagher, 2019).
Previous research concluded that around 40% of all cancer patients receive inadequate treatment for their pain, such as a dose that is too low or the treatment that is initiated too late (Candido et al., 2017; Deandrea et al., 2008; Kasasbeh et al., 2016). Factors that lead to inadequate management of cancer‐related pain can be related to healthcare professionals, the healthcare system, and patients (Kwon, 2014).
A previous study reported that approximately 10% of all cancer patients visiting an outpatient oncology clinic reported unacceptable pain at a self‐service registration desk (Willems et al., 2021). For only 70% of these patients, an intervention for this unacceptable pain, such as pain treatment, further diagnostics, or referral to another (pain) specialism, was reported in the patient record. It remained unclear why no pain interventions were reported in the patient record for the other 30% of patients who reported unacceptable pain (Willems et al., 2021).
Increased insight in the reasons for absence of pain interventions might provide means to improve the pain treatment for oncology patients, which could result in increased well‐being of these patients (Ho et al., 2018). The main aim of this study is to gain insight in the reasons for the absence of pain intervention among oncology patients who report unacceptable pain at the self‐service registration desk. The secondary aim of the study is to assess the characteristics of patients who report unacceptable pain and received no pain intervention. Furthermore, we inquired who patients held responsible for the absence of pain intervention and what changes regarding their pain treatment they would prefer.
2. MATERIALS AND METHODS
2.1. Study design
A prospective, observational and explorative mixed methods study was performed based on a patient record assessment combined with telephone interviews.
2.2. Setting and subjects
The study was performed between April and July 2021 at the oncology centre of a university hospital in the Netherlands. The oncology centre receives almost 40,000 outpatients per year, and every type of cancer is treated. The selection of the participants was done in three steps. Firstly, the information technology department of the oncology centre, selected patients who (a) visited the oncology centre between 6 April and 4 June 2021 for an outpatient consultation with a physician or nurse and/or outpatient treatment at the day care centre and (b) reported their pain as unacceptable at the self‐service registration desk at the entrance of the oncology centre. Secondly, the researcher (HS) made a further selection based on patient record assessment, selecting patients who (c) were 18 years or older at the time of visit, (d) had no intervention for the pain reported in the patient record after the visit to the oncology centre, (e) were diagnosed with an oncological or haematological disease and (f) were Dutch or English speaking. Thirdly, the selected patients received information on the study by telephone, and an information letter and informed consent form were sent either by email or post. Subsequently, based on a short telephone interview, the final selection was performed, selecting patients who (g) perceived themselves as cognitively, emotionally and physically able to answer questions on the phone, (h) agreed to participate in the study via an informed consent form, (i) confirmed that their pain was unacceptable at the time of visit and (j) confirmed that no pain intervention was initiated during their visit. Patients who met all inclusion criteria participated in the present study.
2.3. Data collection and outcome
Data were gathered by means of patient record assessment and a telephone interview. The patient record assessment was performed using a data extraction form (see Appendix A). This data extraction form includes patient demographics (age and sex), disease characteristics (type of tumour, presence of metastases and the type of tumour treatment), pain severity (numeric rating scale [NRS] ranging from 0 to 10) and information indicating a pain intervention. To assess whether a pain intervention was discussed during the visit, the patient record was checked for further diagnostics related to pain, a referral to another specialist and the discussion or prescription of additional pain treatment. The interviews were performed using a standardised questionnaire developed for this study (see Appendix B). The questionnaire focused on gaining insight in the patient's perspective on why they received no pain intervention for their unacceptable pain. Furthermore, the researcher inquired whether the pain was discussed at all, and if so, who initiated that discussion. Additionally, the question was asked who the patient held responsible for the pain discussion and treatment. Finally, the questionnaire included questions regarding potential improvements in the treatment of their pain, as proposed by the patient.
This study was exempted from the Human Subjects Act by the medical‐ethical evaluation board of the academic hospital. Furthermore, approval for this study was provided by the Review Ethics Committee of the affiliated university.
2.4. Data analysis
Descriptive statistics were used to analyse the quantitative data from the patient record assessments and the interviews, including mean (standard deviation SD) and range, median (interquartile range IQR, 25th–75th percentile) and number (%). During the analysis, issues with collected data leaving room for multiple interpretations were discussed with an internist specialised in pain and an epidemiologist. Qualitative data were analysed by an inductive content analysis. This content analysis consisted of the description and quantification of the answers of the patients, after which the most frequently indicated answers could be provided when checking for patterns in the comments (Elo & Kyngăs, 2008). The content analysis was discussed with a senior researcher and an epidemiologist and was adapted after a consensus meeting in case of a disagreement.
3. RESULTS
3.1. Response and characteristics of the participants
Between the 6th of April and the 4th of June 2021, a total of 220 patients visiting the oncology outpatient clinic reported their pain as unacceptable at the self‐service registration desk. During the patient record assessment, 69 patients met the inclusion criteria from the first two selection steps (criteria a–f). Approximately one‐third of these 69 patients indicated that their pain was acceptable at the time of the visit, although they reported to have unacceptable pain at the registration desk during their visit to the hospital. These patients indicated they had misread the question, could not understand the question because of an inability to read Dutch, had the registration done by an informal caregiver or wanted to skip the question quickly. Twenty (9%) of the approached patients indicated they did experience unacceptable pain at the time of visit, met all inclusion criteria and were interviewed. The flow of the participants and reasons for exclusion are presented in Figure 1.
FIGURE 1.
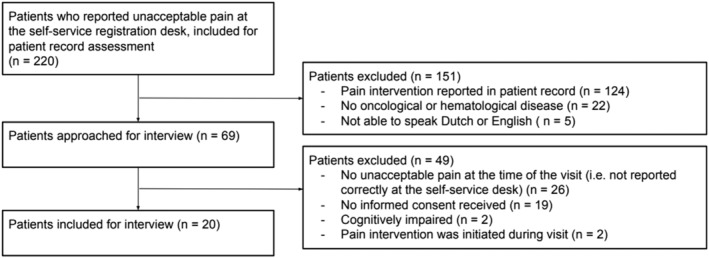
Flow chart of the participants
The baseline characteristics of the included 20 patients are presented in Table 1. The mean age was 62.0 years, ranging from 30 to 85, and 12 (60%) were female. The median pain intensity at registration was NRS 7.0. The included patients had various types of tumours, and the majority had no metastasis. Approximately one‐third of the patients did not receive any anticancer treatment at the time of visit. The majority had a consultation with a physician or nurse, which for some patients was combined with a treatment at the day care centre. The interviews were performed 15.5 days after the visit to the outpatient clinic on average, ranging from 2 to 34 days.
TABLE 1.
Baseline characteristics of patients
| Baseline characteristics | Patients included for interview (n = 20) |
|---|---|
| Age | 62.0 (13.7) |
| Sex | |
| Female | 12 (60%) |
| Male | 8 (40%) |
| Tumour type | |
| Breast | 4 (20%) |
| Multiple myeloma | 4 (20%) |
| Leukaemia | 2 (10%) |
| Lung | 2 (10%) |
| Other | 8 (40%) |
| Metastasis | |
| No | 14 (70%) |
| Yes | 6 (30%) |
| Current treatment a | |
| Chemotherapy | 4 (20%) |
| Immunotherapy | 6 (30%) |
| Hormonal therapy | 2 (10%) |
| Surgery in past 6 weeks | 1 (5%) |
| Radiotherapy in past 6 weeks | 0 (0%) |
| None | 7 (35%) |
| NRS at registration | 7.0 (5.0–8.0) |
| Type of visit | |
| Consultation with physician/nurse | 8 (40%) |
| Treatment at day care centre | 6 (30%) |
| Both | 4 (20%) |
| Unknown | 2 (10%) |
Note: Numbers represent mean (SD), median (IQR) or number (%).
Patients could receive more than one treatment.
3.2. Discussion of pain during hospital visit
Fourteen of the 20 patients indicated that their pain was discussed during the visit to the hospital to the oncology centre; however, no pain treatment was initiated. Figure 2 shows whether the pain was discussed during the visit and who initiated the discussion. Four patients indicated that their pain was not discussed. Of the 14 patients who discussed their pain during the visit, 11 took the initiative themselves to discuss pain. In two cases, the physician took the initiative, and one patient indicated the discussion of pain was a shared initiative.
FIGURE 2.
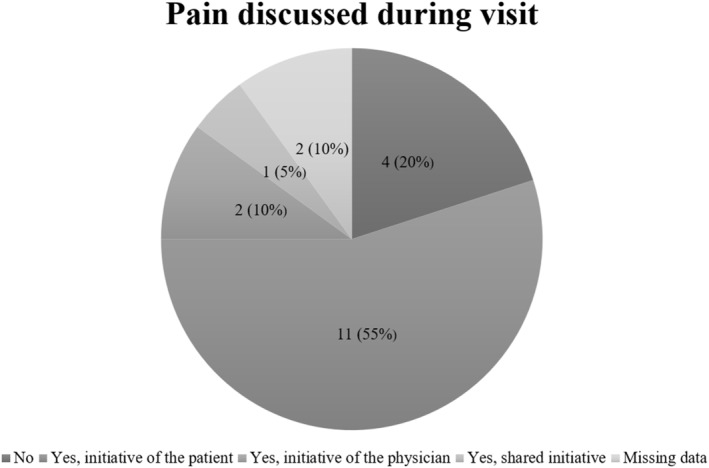
Pain discussed during visit
3.3. Reasons for absence of pain intervention
There was a variety of reasons for absence of pain intervention mentioned by the participants. In Table 2, the reasons mentioned are presented per patient. The reasons that were most often indicated by the patients were that their physicians primarily focused on treating the disease, and thus paid less attention to potential symptoms such as pain (n = 6), and that they themselves preferred no pain treatment at that moment (n = 6). Of the six patients that did not prefer any pain treatment, four patients indicated they were reluctant to take pain medication, and the two other patients thought pain treatment unnecessary due to the short duration of pain and rejected a referral to another specialist. Underlying feelings for the reluctance for pain medication were concerns about the side effects of medication, fear of dependency on medication, fear of damaging one's body if no pain is felt and the perception that the pain is not caused by cancer.
TABLE 2.
Reasons for absence of pain intervention
| Reasons mentioned a | Person considered by the patient as responsible for the absence of pain intervention b | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physician | Patient | Both physician and patient | No one | |||||||||||||||||
| Patients | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
| Physician only focused on treatment of disease | X | X | X | X | X | X | ||||||||||||||
| Reluctance for intervention by patient | X | X | X | X | X | X | X | |||||||||||||
| Reluctance to mention pain by patient | X | X | X | X | ||||||||||||||||
| Pain intervention complicated or impossible | X | X | X | X | ||||||||||||||||
| Unknown cause of pain | X | X | X | X | ||||||||||||||||
| Pain inevitable part of treatment | X | X | X | X | ||||||||||||||||
| No attention for person behind the disease | X | X | ||||||||||||||||||
| Pain with different cause, treatment elsewhere | X | X | ||||||||||||||||||
| Regulation of pain in own hands | X | |||||||||||||||||||
Patients could indicate more than one reason.
40% of the patients (n = 8) held only the physician responsible for the absence of pain intervention in their treatment, 15% (n = 3) held themselves responsible, and 20% (n = 4) reported a shared responsibility. The remaining 25% (n = 5) stated that no one was responsible.
Two other reasons that were mentioned by several patients were reluctance to mention pain to the physician (n = 4), and the physician indicating that further pain intervention was difficult or impossible (n = 4). Patients experienced reluctance to start the discussion of pain, because of fear that the cancer treatment might be delayed or terminated (n = 2), an expectation that the health professional would regard them as complaining (n = 1) or a feeling of uselessness because no offer of pain intervention is expected (n = 1). The four patients that indicated that pain treatment was complicated provided the following explanations: extensive comorbidity (n = 1), no availability of alternative pain interventions without feared side effects (n = 1) and an unknown cause of pain (n = 2).
3.4. Perceived responsibility for absence of pain intervention
During the interviews, the patients reflected on the perceived responsibility for the absence of pain intervention as perceived by the patients, which is displayed alongside the reasons for absence of pain intervention in Table 2. The largest group of eight patients held the physician responsible for the absence of pain intervention. An argument for the physician's responsibility provided by two patients was that the physician is the expert and should thus know when to inquire about or initiate treatment for a patient's pain. Other arguments mentioned were that the physician could not discover the cause of pain and that the physician should be more considerate of the severe side effects of pain medication. Three patients indicated they consider the initiative to start a discussion about a pain intervention their own responsibility. Four patients indicated it was a shared responsibility of patient and physician. There were also five patients who indicated that in their opinion, no one was responsible for not receiving an intervention.
3.5. Changes in pain treatment preferred by the patients
All patients were asked whether they would prefer changes in the way their pain is treated. Of the 19 patients who answered this question, five patients indicated that they would prefer their pain to be discussed every consultation or visit. One patient specifically indicated that she did often not mention her pain during online consultations in the current COVID‐19 crisis and thus would prefer the physician to initiate the discussion during the online consultations. Four patients would like to discuss additional pain medication during their consultation, one patient wanted the pain to be further diagnosed, and one patient preferred both. Seven patients were satisfied with their current pain treatment and would not prefer any change.
4. DISCUSSION
4.1. Main results and reflection
The majority of interviewed patients indicated that their pain was discussed during the hospital visit, mostly from the patients' initiative. The reasons for absence of pain intervention as perceived by the patient included, among other, reluctance of the patient to discuss pain during the hospital visit, reluctance of the patient to receive treatment, lack of attention of the physician for the pain or other symptoms, lack of treatment possibilities and the perception of pain as an inevitable part of the treatment.
Only 20% (n = 4) of the patients did not discuss their as inacceptable perceived pain during the visit to the outpatient clinic. This is a relatively low percentage compared to what is shown in previous research, where a percentage of almost 50% of patients did not discuss pain symptoms (Penalba et al., 2019).
In past studies, barriers for adequate cancer‐related pain management have been identified (Kwon, 2014; Timmerman et al., 2019; van den Beuken‐van Everdingen et al., 2016; van den Beuken‐van Everdingen et al., 2018; Wright et al., 2019). The current study recognises that a wide variety of these barriers are still applicable in 2021. Kwon (2014) distinguished healthcare professional‐related, healthcare system‐related and patient‐related factors that might lead to inadequate pain management, which can be recognised in our collected data. The difficulty to discuss their pain and reluctance to take medication indicated by the patients are among patient‐related factors potentially leading to lacking pain management (Kwon, 2014; van den Beuken‐van Everdingen et al., 2018). Covid‐19 and the resulting online consultations could be a complicating factor for easy discussion of pain. This is recognised by multiple studies and was also mentioned by one of the patients in this study (Chen et al., 2020; Donaghy et al., 2019). Therefore, an online consultation might not always be an adequate replacement for a real‐life consultation. Causes for the reluctance to use medication mentioned in previous studies such as side effects of pain medication and fear of dependency have not yet been solved, since the same reasons are still provided by the included patients in this study (Bruera & Paice, 2015; Kwekkeboom et al., 2021; van den Beuken‐van Everdingen et al., 2016). A recent study on patient‐related barriers to adequate cancer‐related pain management, such as fears of addiction, even showed that these barriers were increasingly reported between 2002 and 2020 (Kwekkeboom et al., 2021). Although knowledge of patient‐related barriers can be helpful for tackling some uncertainty or fear in the patients, complete removal of these barriers might be very difficult (Kwekkeboom et al., 2021). For these patients, the harms and benefits of their options should be considered, and a shared decision between patient and healthcare professional should be made to initiate or reject a pain intervention. Healthcare professional‐related factors previously recognised in literature but still mentioned in this study encompass the lack of attention for pain during clinical encounters, such as no routine discussion and measurement of pain by physicians or nurses (Kwon, 2014; van den Beuken‐van Everdingen et al., 2018). Finally, identified healthcare system‐related factors are the lack of appropriate treatment (e.g. without severe side effects), possibly caused by the lack of innovation in the pharmacological and non‐pharmacological treatment of pain recognised in previous literature, and insufficient time and resources to enable healthcare professionals to pay attention to pain management (Kwon, 2014; van den Beuken‐van Everdingen et al., 2018).
There are also barriers to adequate pain management identified in previous studies that were not mentioned by the patients in the current study. Barriers such as lack of knowledge among health professionals, financial restrictions, availability of medicines, and reluctance of health professionals to prescribe pain medication are frequently mentioned in literature, but were not observed in the current study. These barriers might be harder to identify for the patient group, and would be revealed more often when inquiring for potential reasons for absence of pain interventions among health professionals (Al‐Ghabeesh et al., 2020; Bruera & Paice, 2015; Kwon, 2014; Scarborough & Smith, 2018, pp. 20–22; van den Beuken‐van Everdingen et al., 2018).
Sixty percent of the patients (n = 12) reported the responsibility of the absence of pain intervention as no one's, their own or a combination between themselves and their physician. The resulting 40% (n = 8) held only the physician responsible for the absence of pain intervention in their treatment. Several arguments provided for the responsibility could be recognised in the reasons for absence of pain intervention mentioned. Patients who held the physician responsible often indicated that the physicians only focus on treatment of the disease, whereas patients who considered the pain discussion their own responsibility often reported personal reluctance for pain medication.
Additionally, the majority of the patients would like to see some changes in their pain treatment, such as regular discussion of their pain, additional medication or diagnostics. These changes in pain management as suggested by the patients might contribute to a reduction in both healthcare professional‐related and healthcare system‐related inadequate pain management (Fairchild, 2010; Kwon, 2014). However, 35% of the patients (n = 7) were satisfied with their current care.
Finally, approximately one‐third of the patients who did not receive a pain intervention despite reporting unacceptable pain at the self‐service registration desk indicated during the second check (before the interview) that their pain was not unacceptable at the time of the visit. The relatively high number of mistakes in this patient group was caused by reasons such as the misunderstanding of the question for both Dutch and non‐Dutch patients, the registration done by an informal caregiver or a lack of attention given to the questions when registering. Additionally, if these mistakes occur consistently, this could lead to misleading results in studies among the patients reporting their pain. However, a previous study has shown that the NRS and the (non‐)acceptable pain question are well compatible (Willems et al., 2021). Therefore, most likely both measurement methods are useful, since multiple pain assessment methods are essential for adequate pain management (van Boekel et al., 2017). Proper measurement and reporting of pain can even have a positive impact on the pain of oncology patients and will support the quick identification of issues with pain management (Haumann et al., 2017; Magee et al., 2019). However, the results of the current study have shown that additional attention for and explanation of the questions at the registration desks is necessary.
4.2. Limitations and strengths
A limitation of the study is the relatively small number of participants. This seems partly caused by the COVID‐19 crisis, which led to an increase in online consultations instead of face‐to‐face consultations (Boehm et al., 2020; Onesti et al., 2020). Patients with an online consultation did not visit the oncology centre and as a result did not register at the self‐service registration desk, which automatically led to exclusion of these patients. This might have resulted in selection bias.
A second limitation is the period between visit to the hospital and selection for this study that could have led to recall bias. However, to call patients, for example, the day after their visit was infeasible for the IT department and the researchers.
The strength of this study is the mixed methods nature of the study. Mixed methods approaches usually yield a comprehensive picture of the real‐life situation. Due to the qualitative interviews, in‐depth data could be acquired from the participants. Because the questionnaires were asked via telephone, an explanation could be asked for certain answers, which led to a high level of detail in the answers. The explorative data from the patients' perspectives can be used for hypotheses about the potential reasons for absence of pain intervention.
4.3. Recommendations
Several recommendations can be made based on the present study. First, we recommend to improve the communication between physician and patient about pain by stimulating the physicians to proactively discuss the pain, to confirm whether the patient is content with the proposed pain treatment and to measure cancer‐related or cancer treatment‐related pain during consultations (van Boekel et al., 2017; van den Beuken‐van Everdingen et al., 2018).
Second, the empowerment of patients should be supported in order to stimulate them to discuss pain and pain interventions during the visits to the outpatient clinic. Creating awareness among patients of the importance of reporting the severity of their pain during hospital visits, either at a self‐service registration desk or in person, can contribute to this empowerment. A suggested intervention that supports the development of patient empowerment in pain management is the improvement of shared decision making by letting the patient inquire about possible options for pain interventions, the related potential harms and benefits and the chances of those harms and benefits (Shepherd et al., 2016).
5. CONCLUSION
In conclusion, there is a variety of reasons for absence of pain intervention among patients with unacceptable pain. Important patient‐related reasons were reluctance of the patient to discuss pain and receive further treatment. A wide variety of factors indicated by the patients show up in previous studies, which emphasises the undiminished need to tackle these issues. Therefore, we recommend to improve communication regarding pain management between patient and physician, and the empowerment of patients.
CONFLICT OF INTEREST
No funding was received for this study, and none of the authors has a conflict of interest with respect to this article.
AUTHOR CONTRIBUTIONS
Hester Stoorvogel: Methodology, participant selection, data collection, data analysis, writing—original draft, visualisation, writing—review and editing. Jolanda van Haastregt: Methodology, writing—review and editing, supervision. Maurice Theunissen: Conceptualization, methodology, writing—review and editing, supervision. Janna Schoenmaekers: Writing—review and editing. Ann Hoeben: Writing—review and editing. Marieke van den Beuken‐van Everdingen: Conceptualization, methodology, writing—review and editing, supervision.
APPENDIX A. DATA EXTRACTION FORM
Unacceptable pain in oncology: The patients' perspective on reasons for absence of pain interventions
Data extraction form for patient record assessment after registration at self‐service desk including:
Patient characteristics
Diagnosis
Treatment oncological disease
Intervention for pain as mentioned in patient record
Participant number:
Date of visit: __ ‐ __ ‐ 2021
Date of entering data in database: __ ‐ __ ‐ 2021
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
Name of patient: … … …………………………………………………………… ….
Date of birth: __ __‐__ __ ‐ __ __ __ __
Patient number (SAP): … … …………………………………………… … …
Patient characteristics:
Gender: M/F
Age: __ years
Diagnosis and cancer treatment
Type of tumour: … ……………………………………………………… ….
Metastases: yes/no
Currently receiving disease‐focused treatment: yes/no
If yes:
-
○
chemotherapy
-
○
immune therapy
-
○
hormone therapy
-
○
surgery in the past six weeks
-
○
radiation therapy in the past six weeks
Pain‐specific characteristics
Numeric Rating Scale (NRS) at self‐service registration desk: __ __
Pain reported in patient record during consult/treatment: yes/no
Pain intervention in patient record
Further diagnostics during consult: yes/no
Referral to other specialist during consult: yes/no
If yes, referral to … … …………………………………………………………………… …..
Pain medication altered /added/discussed during following consult:
-
○
none
-
○
paracetamol
-
○
NSAID (nonsteroidal anti‐inflammatory drug)
-
○
weak opioid
-
○
strong opioid
-
○
(tricyclic) antidepressant
-
○
gabapentinoid (anti‐epileptics)
Other interventions: yes/no
If yes:
-
○
TENS (transcutaneous electrical nerve stimulation)
-
○
capsaicin (plaster/cream)
-
○
splanchnic nerves block in the past six months
-
○
chordotomy in the past six months
APPENDIX B. QUESTIONNAIRE
Unacceptable pain in oncology: The patients' perspective on reasons for absence of pain interventions
Questionnaire for interview with patient by phone
Participant number: ___
Date of call: __ ‐ __ ‐ 2021
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
Name: … … …………………………………………………………… ….
Date of birth: __ ‐ __ ‐ ____
Patient number (SAP): … … ………………………………………… … …
Phone number: ____ ‐ ______________.
Report for interview with patients with unacceptable pain during last visit Oncology Center:
Good morning/afternoon Mr. /Mrs. … …,
You're speaking with Hester Stoorvogel from the Oncology Center in Maastricht.
I called you … … … (when) to inform you about this study and I received the informed consent form from you. As you have read, we are evaluating the care for unacceptable pain of our patients. I would like to ask you the questions now. Is this a convenient time for you and are you feeling good enough to answer the questions? (If not, can I call you back at another time? … … …………… …)
Absence of pain intervention
I would like to ask some questions about your previous visit to the Oncology Center.
- Did you discuss your pain during that visit (with your physician/a nurse/etc.)
- Yes/no
- Has there been (a discussion of) an intervention for your pain? Such as a referral, additional pain medication, further diagnostics, etc.
-
If yes, which? ➔ continue with Question 5.… … ……………………………………………………… … …
- If no: ➔ continue with question 3.
-
- Can you indicate why you think that no pain intervention was discussed or offered for your unacceptable pain?
- Yes/no
- Explanation: … ………………………………………………………………………………………………………………………………………………………………………………………………………………………………… … …
- Would you prefer that your physician/nurse always discusses your pain during a consultation or visit?
- Yes/no
- Explanation: … ………………………………………………………………………………………………………………………………………………………………………………………………………………………………… … …
- Did you feel free to mention your pain yourself?
- Yes/no
- Explanation: … ………………………………………………………………………………………………………………………………………………………………………………………………………………………………… … …
- With whom do you think the reason for the absence of pain intervention lies?
- Neither/ patient /physician or nurse/both patient and physician/attendant of patient/other … … …………… … …
- Explanation … … ………………………………………………………… …..
- Would you like to see changes in the treatment of your pain?
- Yes/no
- If yes, what would you like to change?
- … … ………………………………………………………………………………… ….
- Do you give permission to pass on what we just discussed to my supervisor and your treating physician?
- Yes/partly/no
- Explanation … … …………………………………………………………………… ….
Stoorvogel, H. , van Haastregt, J. , Theunissen, M. , Schoenmaekers, J. , Hoeben, A. , van den Beuken‐van Everdingen, M. (2022). Unacceptable pain in oncology: The patients' perspective on reasons for absence of pain interventions. European Journal of Cancer Care, 31(5), e13628. 10.1111/ecc.13628
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Al‐Ghabeesh, S. H. , Bashayreh, I. H. , Saifan, A. R. , Rayan, A. , & Alshraifeen, A. A. (2020). Barriers to effective pain management in cancer patients from the perspective of patients and family caregivers: A qualitative study. Pain Management Nursing, 21, 238–244. 10.1016/j.pmn.2019.07.011 [DOI] [PubMed] [Google Scholar]
- Bennett, M. , Paice, J. A. , & Wallace, M. (2017). Pain and opioids in Cancer care: Benefits, risks, and alternatives. American Society of Clinical Oncology Educational Book, 37, 705–713. 10.1200/EDBK_180469 [DOI] [PubMed] [Google Scholar]
- Boehm, K. , Ziewers, S. , Brandt, M. P. , Sparwasser, P. , Haack, M. , Willems, F. , Thomas, A. , Dotzauer, R. , Höfner, T. , Tsaur, I. , Haferkamp, A. , & Borgmann, H. (2020). Telemedicine online visits in urology during the COVID‐19 pandemic‐potential, risk factors, and patients' perspective. European Urology, 78, 16–20. 10.1016/j.eururo.2020.04.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruera, E. , & Paice, J. A. (2015). Cancer pain management: Safe and effective use of opioids. American Society of Clinical Oncology Educational Book, 35, 593–599. 10.14694/EdBook_AM.2015.35.e593 [DOI] [PubMed] [Google Scholar]
- Candido, K. D. , Kusper, T. M. , & Knezevic, N. N. (2017). New cancer pain treatment options. Current Pain and Headache Reports, 21, 12. 10.1007/s11916-017-0613-0 [DOI] [PubMed] [Google Scholar]
- Chen, M. , Liu, X. , Zhang, J. , Sun, G. , Gao, Y. , Shi, Y. , Baker, P. , Zeng, J. , Zheng, Y. , Luo, X. , & Qi, H. (2020). Characteristics of online medical care consultation for pregnant women during the COVID‐19 outbreak: Cross‐sectional study. BMJ Open, 10, e043461. 10.1136/bmjopen-2020-043461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deandrea, S. , Montanari, M. , Moja, L. , & Apolone, G. (2008). Prevalence of undertreatment in cancer pain. A review of published literature. Annals of Oncology, 19, 1985–1991. 10.1093/annonc/mdn419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaghy, E. , Atherton, H. , Hammersley, V. , McNeilly, H. , Bikker, A. , Robbins, L. , Campbell, J. , & McKinstry, B. (2019). Acceptability, benefits, and challenges of video consulting: A qualitative study in primary care. British Journal of General Practice, 69, 586–594. 10.3399/bjgp19X704141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo, S. , & Kyngăs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62, 107–115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Fairchild, A. (2010). Under‐treatment of cancer pain. Current Opinion in Supportive and Palliative Care, 4, 11–15. 10.1097/SPC.0b013e328336289c [DOI] [PubMed] [Google Scholar]
- Fink, R. M. , & Gallagher, E. (2019). Cancer pain assessment and measurement. Seminars in Oncology Nursing, 35, 229–234. 10.1016/j.soncn.2019.04.003 [DOI] [PubMed] [Google Scholar]
- Haumann, J. , Joosten, E. B. A. , & van den Beuken‐van Everdingen, M. H. J. (2017). Pain prevalence in cancer patients: Status quo or opportunities for improvement. Current Opinion in Supportive and Palliative Care, 11, 99–104. 10.1097/SPC.0000000000000261 [DOI] [PubMed] [Google Scholar]
- Ho, K. Y. , Ahn, J. S. , Calimag, M. M. , Chao, T. C. , Kim, Y. C. , Moon, H. , Tho, L. M. , Xia, Z. J. , & You, D. (2018). Inadequate treatment practices for pain relief and adverse event management in cancer patients across 10 countries/regions in Asia: A call for greater efforts to improve standards for patient care. Asia‐Pacific Journal of Clinical Oncology, 14, 159–166. 10.1111/ajco.12696 [DOI] [PubMed] [Google Scholar]
- Kasasbeh, M. A. M. , McCabe, C. , & Payne, S. (2016). Cancer‐related pain management: A review of knowledge and attitudes of healthcare professionals. European Journal of Cancer Care, 26, e12625. 10.1111/ecc.12625 [DOI] [PubMed] [Google Scholar]
- Kwekkeboom, K. , Serlin, R. C. , Ward, S. E. , LeBlanc, T. W. , Ogunseitan, A. , & Cleary, J. (2021). Revisiting patient‐related barriers to cancer pain management in the context of the US opioid crisis. Pain, 162, 1840–1847. 10.1097/j.pain.0000000000002173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon, J. H. (2014). Overcoming barriers in cancer pain management. Journal of Clinical Oncology, 32, 1727–1733. 10.1200/JCO.2013.52.4827 [DOI] [PubMed] [Google Scholar]
- Magee, D. , Bachtold, S. , Brown, M. , & Farquhar‐Smith, P. (2019). Cancer pain: Where are we now? Pain Management, 9, 63–79. 10.2217/pmt-2018-0031 [DOI] [PubMed] [Google Scholar]
- Neufeld, N. J. , Elnahal, S. M. , & Alvarez, R. H. (2017). Cancer pain: A review of epidemiology, clinical quality and value impact. Future Oncology, 13, 833–841. 10.2217/fon-2016-0423 [DOI] [PubMed] [Google Scholar]
- Onesti, C. E. , Rugo, H. S. , Generali, D. , Peeters, M. , Zaman, K. , Wildiers, H. , Harbeck, N. , Martin, M. , Cristofanilli, M. , Cortes, J. , Tjan‐Heijnen, V. , Hurvitz, S. A. , Berchem, G. , Tagliamento, M. , Campone, M. , Bartsch, R. , de Placido, S. , Puglisi, F. , Rottey, S. , … Jerusalem, G. (2020). Oncological care organisation during COVID‐19 outbreak. ESMO Open, 5, e000853. 10.1136/esmoopen-2020-000853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penalba, V. , Deshields, T. L. , & Klinkenberg, D. (2019). Gaps in communication between cancer patients and healthcare providers: Symptom distress and patients' intentions to disclose. Support Care Cancer, 27, 2039–2047. 10.1007/s00520-018-4442-4 [DOI] [PubMed] [Google Scholar]
- Rodriguez, C. , Ji, M. , Wang, H. L. , Padhya, T. , & McMillan, S. C. (2019). Cancer pain and quality of life. Journal of Hospice & Palliative Nursing, 21, 116–123. 10.1097/NJH.0000000000000507 [DOI] [PubMed] [Google Scholar]
- Scarborough, B. M. , & Smith, C. B. (2018). Optimal pain management for patients with cancer in the modern era. CA: A Cancer Journal for Clinicians, 68, 182–196. 10.3322/caac.21453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd, H. L. , Barratt, A. , Jones, A. , Bateson, D. , Carey, K. , Trevena, L. J. , McGeechan, K. , Del Mar, C. B. , Butow, P. N. , Epstein, R. M. , Entwistle, V. , & Weisberg, E. (2016). Can consumers learn to ask three questions to improve shared decision making? A feasibility study of the ASK (AskShareKnow) patient‐clinician communication model (®) intervention in a primary health‐care setting. Health Expectations, 19, 1160–1168. 10.1111/hex.12409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmerman, L. , Stronks, D. L. , & Huygen, F. J. (2019). The relation between patients' beliefs about pain medication, medication adherence, and treatment outcome in chronic pain patients: A prospective study. Clinical Journal of Pain, 35, 941–947. 10.1097/AJP.0000000000000760 [DOI] [PubMed] [Google Scholar]
- van Boekel, R. L. M. , Vissers, K. C. P. , van der Sande, R. , Bronkhorst, E. , Lerou, J. G. C. , & Steegers, M. A. H. (2017). Moving beyond pain scores: Multidimensional pain assessment is essential for adequate pain management after surgery. Public Library of Science One, 12, e0177345. 10.1371/journal.pone.0177345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Beuken‐van Everdingen, M. H. J. , Hochstenbach, L. M. J. , Joosten, E. A. J. , Tjan‐Heijnen, V. C. G. , & Janssen, D. J. A. (2016). Update on prevalence of pain in patients with cancer: Systematic review and meta‐analysis. Journal of Pain and Symptom Management, 51, 1070–1090.e9. 10.1016/j.jpainsymman.2015.12.340 [DOI] [PubMed] [Google Scholar]
- van den Beuken‐van Everdingen, M. H. J. , van Kuijk, S. M. J. , Janssen, D. J. A. , & Joosten, E. A. J. (2018). Treatment of pain in cancer: Towards personalised medicine. Cancers, 10, 502. 10.3390/cancers10120502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willems, A. A. J. M. , Kudrashou, A. F. , Theunissen, M. , Hoeben, A. , & van den Beuken van Everdingen, M. H. J. (2021). Measuring pain in oncology outpatients: Numeric rating scale versus acceptable/non‐acceptable pain. A prospective single center study. Pain Practice, 21, 871–876. 10.1111/papr.13053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, E. M. , El‐Jawahri, A. , Temel, J. S. , Carr, A. , Safren, S. A. , Park, E. R. , Pirl, W. F. , Bruera, E. , & Traeger, L. (2019). Patient patterns and perspectives on using opioid regimens for chronic cancer pain. Journal of Pain and Symptom Management, 57, 1062–1070. 10.1016/j.jpainsymman.2019.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


