Abstract
Objective
This study compares the well‐being of rural caregivers with that of the general population and explores the potential drivers of poorer outcomes.
Method
Patient–caregiver dyads (n = 241) residing in regional or remote Queensland, Australia, reported on QoL, chronic illness, caregiver burden, depression, anxiety and stress. Caregiver outcomes were compared with population norms and patient outcomes. Multiple regressions were conducted to identify factors associated with poorer caregiver outcomes.
Results
Caregivers reported lower mental health‐related QoL (M = 0.436, 95% CI = 0.410–0.462) in comparison with age‐matched population norms (M = 0.556, 95% CI = 0.532–0.580). No differences existed between caregiver and population norms for anxiety, stress and depression. Caregiver chronic illness and higher burden were associated with poorer mental and physical QoL, depression, anxiety and stress (η 2s ranging from 0.03 to 0.30). These associations were slightly stronger for male caregivers when compared with female caregivers (η 2s ranging from 0.03 to 0.08).
Conclusion
It is vital that efforts are made to improve rural caregivers' mental and emotional well‐being. Interventions that support caregivers with chronic conditions reduce caregiver burden and take into consideration the unique experience of male caregivers will go some way to addressing this. Future research is needed to identify other drivers of health outcomes in this group.
Keywords: anxiety, cancer, caregiver, depression, quality of life, rural
1. BACKGROUND
Informal caregivers are of immense value to health care systems, saving approximately $80 billion per year in patient care costs in Australia (Carers Australia, 2020). It is estimated that 349 million people worldwide are care‐dependent (World Health Organization [WHO], 2017) with 2.65 million Australians being the primary informal caregiver for someone with a disability or chronic disease (Australian Bureau of Statistics, 2020). Cancer patients are one of the most common recipients of such care worldwide (Girgis & Lambert, 2017; Romito et al., 2013).
Informal caregivers for people with a cancer diagnosis, usually a spouse or family member, take on multiple responsibilities such as providing emotional support, physical care, symptom monitoring and management, and practical support with everyday tasks such as cooking and cleaning (Given et al., 2001; Longacre, 2013; Van Ryn et al., 2011; WHO, 2017). Providing care to a loved one can be a rewarding experience and has been associated with experiencing closer relationships with others and increases in life appreciation, empathy for others better health behaviours (Mosher et al., 2017). However, caring responsibilities, along with the emotional impact of the patient's ill‐health, can also place considerable strain on the physical and mental health of the caregiver leading to decreased quality of life (QoL) and increased psychological distress (Butow et al., 2014; Hanly et al., 2016; Lund et al., 2014; Papastavrou et al., 2009).
Caregivers living in regional and remote areas (i.e., communities with populations below 250,000, situated outside of major service centres) face added challenges compared with those living in metropolitan cities due to social isolation, the requirement for patients to travel to receive treatment and reduced access to local support services, often compounded by socioeconomic disadvantage (Australian Institute of Health and Welfare, 2017a; Crouch et al., 2017; Rosenberg & Eckstrom, 2020; Ugalde et al., 2019). For example, Ugalde et al. (2019) showed that caregivers living in regional and remote Australia experienced logistical challenges, major life adjustments, financial losses and isolation from their community when having to travel with patients for treatment. Recent investigation into the supportive care needs of regional and remote cancer patients revealed several common practical and emotional challenges faced by this group as well as differences in needs according to demographic and patient characteristics such as age, gender and cancer type (Stiller et al., 2021). The burden experienced by caregivers in regional and remote areas has been shown to lead to poor mental health outcomes such as high rates of caregiver depression (Beach et al., 2019; Hanly et al., 2016; Van Ryn et al., 2011).
With almost one third of the Australian population living outside of a major city (Australian Institute of Health and Welfare, 2017b), and predicted increases in cancer incidence (Sung et al., 2021), maintaining the health and well‐being of regional and remote cancer caregivers is an important consideration in the provision of cancer care in Australia. However, inadequate evidence exists to quantify the QoL and psychological wellness of regional and remote cancer caregivers and to identify factors that predict adverse outcomes in this population. This evidence is essential for allocating appropriate support and resources to Australia's vital population of cancer caregivers.
1.1. Study aims
The primary aim of this study was to examine QoL, depression, anxiety and stress in the informal caregivers of cancer survivors living in regional and remote areas and compare these with age‐matched population norms.
Sociodemographic factors, caregiver health and patient health and degree of burden placed on the caregiver has been shown to impact caregiver well‐being (Butow et al., 2014; Hanly et al., 2016; Romito et al., 2013; Ugalde et al., 2019). Therefore, a secondary aim of this study was to explore the potential drivers of poorer outcomes for regional and remote caregivers by testing associations between demographic characteristics, patient outcomes and caregiver burden and health.
2. METHODS
2.1. Participant recruitment
Participants were a subset of caregiver–patient dyads staying at accommodation lodges available to those undergoing cancer treatment more than 50 km from their home. Dyads were recruited as part of a larger project examining the experiences of regional and remote cancer patients in Australia who must travel to receive treatment in major cities. Details of the larger project are provided elsewhere (Dunn et al., 2021; Goodwin et al., 2021). In summary, 402 (49.6%) of cancer patients participating in the larger project nominated a caregiver and provided their contact details to the research team along with permission to contact them. Nominated caregivers over the age of 18 who could read and understand English were eligible for this study. The research team contacted nominated caregivers via telephone inviting them to participate in this study. Invitation packs with consent forms and a questionnaire were sent to those who expressed interest in taking part. Two hundred and fifty‐nine caregivers accepted the invitation to the study and provided informed consent by signing and returning a hard‐copy consent form a self‐completed pen and paper questionnaire. Ethics approval for this study was provided after independent review by a university human research ethics committee (ref. H17REA152).
2.2. Measures
Participants (patients and caregivers) completed a paper‐based self‐administered questionnaire (SAQ) and then took part in a face‐to‐face or telephone interview. The SAQ captured a variety of demographic characteristics, caregiver burden, quality of life, depression, anxiety and stress. SAQs were mailed to participants and were returned via reply‐paid post. Interviews were used to assess caregiver health and patient reports of patient's cancer type and diagnosis date.
2.2.1. Demographics
Caregiver gender, age, country of birth and highest level of education were recorded. The caregiver's residential address was geocoded and mapped to the 2011 statistical area (SA2) boundaries using MapMarker Australia V.15.16.0.21 and MapInfo Pro V.5.0 and classified by Remoteness Area (Australian Bureau of Statistics, 2011b) and Socioeconomic Index for Areas (SEIFA) (Australian Bureau of Statistics, 2011a).
2.2.2. Patient cancer characteristics
The most recently diagnosed primary cancer site of the patient was obtained via self‐report from the patient and verified against the population‐based Queensland Cancer Register (QCR). Self‐report data were relied on where diagnosis could not be verified by the QCR (n = 22, 9.2%), for example, if the patient had nonmelanoma skin cancer (which is not routinely notified to registries in Australia) or the patient's diagnosis was very recent and had not yet been notified to the QCR. A dummy‐coded variable was created for each cancer type to compare it with all other cancers. Days since diagnosis was calculated based on the completion date of the caregivers SAQ, with cases over 3 years (i.e., 1095 days) truncated.
2.2.3. Chronic conditions
Caregivers completed the Charlson Comorbidities Index. Participants selected from a checklist of common chronic illnesses such as diabetes, arthritis and cardiovascular disease (Charlson et al., 1987). For the current study, a binary variable was created whereby caregivers were coded as suffering from no comorbid conditions or one or more conditions.
2.2.4. Caregiver burden
Subjective caregiver burden was captured using the 22‐item validated Caregiver Burden Scale, with the wording adapted to be specific to caregivers of cancer patients (Elmstaahl et al., 1996). This comprehensive measure covers five dimensions including general strain, isolation, disappointment, emotional involvement and environment. Participants responded to items such as “Do you feel tired and worn out?” and “Do you feel lonely and isolated because of the person with cancer's problem?” on a 4‐point Likert scale ranging from 1 = not at all to 4 = often. The Emstaahl et al. scale is a valid and reliable measure of caregiver burden commonly used in cancer caregiver research (Hudson et al., 2010; Michels et al., 2016). Importantly, the scale includes items reflecting neighbourhood and physical environment that may be particularly relevant to a regional and remote sample. A mean score of all items was calculated with higher scores indicating greater subjective burden. Internal consistency of this global scale in the current study was high at α = 0.94.
2.2.5. Quality of life
Both patients and caregivers completed the 35‐item Assessment of Quality of Life 8 Dimension instrument (AQoL‐8D). The AQoL‐8D provides a reliable and valid instrument for understanding the impacts of cancer on psychosocial health (Maxwell et al., 2016), making it an ideal alternative to many other multiattribute utility measures more suited to economic evaluations (Richardson et al., 2014). Five‐point scale responses are coded so that lower scores reflect poorer QoL on eight psychometrically derived dimensions which form two “super dimensions” including Mental QoL consisting of mental health, relationships, coping and happiness subdimensions and Physical QoL consisting of independent living, senses, pain subdimensions. Weighted aggregate scores ranging from 1 to 100 were generated using the AQoL‐8D syntax for SPSS found at www.aqol.com.au. Higher scores reflected better QoL. Internal consistency for all but one subscale in the current study were acceptable with Cronbach's alphas ranging from α = 0.76 to 0.87. The alpha for the three‐item senses subdimension scale was low at 0.41.
2.2.6. Depression, anxiety and stress
Depression, anxiety and stress were measured for both caregivers and patients using the 21‐item, three‐subscale Depression, Anxiety and Stress Scale (DASS 21; Lovibond & Lovibond, 1995) which has been validated in multiple settings and samples (Lee et al., 2019), while examination in the context of regional and remote cancer caregivers in Australia is limited. Respondents indicated the degree to which each statement applied to them over the past week on a 4‐point Likert scale ranging from 0 = not at all to 3 = almost always. Scores for each subscale were then summed with higher scores indicating more distress. Internal consistency in the current study was high with Cronbach's alphas ranging from α = 0.81 to 0.89.
2.3. Data analysis
Norms, means and 95% confidence intervals (CI) for each of the eight AQoL‐8D dimensions for the 65–74 year old age group from 2016 published norms were utilised as QoL comparisons (see Appendix A; 23). This age group was chosen as 50% of the sample were above 65‐years of age with over a third of the sample falling into this age category. Limited resources were available in the literature at the time of publication for estimating age‐appropriate Australian population norms on the DASS. Means and 95% CI for a 25–90 year old sample from a 2011 Australian study and a 2014 study of Australians between 60 and 85 years of age from the general community (see Appendix A; 25,26) were used a comparison for this study. To compare QoL and anxiety, depression and stress outcomes between are sample and population norms, t‐statistics and p values were calculated based on means, standard deviations and sample sizes. p values under 0.05 were interpreted as significant. Patient and caregiver outcomes were compared using a series of paired t‐tests calculated using the raw individual level data.
To explore potential determinants of poorer outcomes, Pearson's correlations were conducted to assess the zero‐order correlations between caregiver age, caregiver gender, time since diagnosis, cancer type, caregiver chronic illness, patient outcomes and caregiver burden on the Mental and Physical super dimensions of QoL as well as anxiety, stress and depression. Univariate general linear modelling using SPSS software was applied to test the combined effects when all covariates listed above were accounted for by the model. The effects of categorical variables with more than two levels (i.e., remoteness and SEIFA) were assessed using polynomial contrasts.
3. RESULTS
Of the 259 caregivers who consented to be part of the larger project, 241 were included in this study. Caregivers of patients living in major cities (n = 10) or without a cancer diagnosis (n = 1) and those who did not complete the relevant sections of the questionnaire (n = 7) were excluded from analysis. Included caregivers (n = 241) ranged from 18 to 91 years of age (M = 62.1, SD = 12.6), were predominantly female (62.1%) and most commonly a spouse or partner of the patient (81.5%; see Table 1). Most caregivers were born in Australia (81.6%) and lived in inner regional (52.3%) and outer regional (42.7%) settings. The caregiver sample were providing support for patients with a variety of cancer types including breast (20.6%), skin (15.2%), prostate (10.8%), head and neck (12.1%) and gynaecological (9.4%) cancers. Time since diagnosis ranged from 12 days to 25 years; however, the majority of patients were within 2 years of diagnosis (75.9%) at the time of caregiver data collection. Almost half (40.6%) of caregivers reported suffering at least one chronic illness, with the most common being connective tissue disease (24.2%) and diabetes (20.1%). Caregivers reported levels of caregiver burden ranging from 1.00–3.82 out of 4.00 (M = 1.61, SD = 0.57, skew = 1.27).
TABLE 1.
Sample characteristics
| n | % a | |
|---|---|---|
| Age in years | ||
| <40 | 11 | 4.6% |
| 40–50 | 24 | 10.1% |
| 50–64 | 88 | 37.1% |
| 65–74 | 84 | 35.4% |
| 75+ | 30 | 12.7% |
| Gender | ||
| Female | 149 | 62.1% |
| Male | 91 | 37.9% |
| Highest level of education | ||
| Year 10 or below | 94 | 41.6% |
| Senior high school | 31 | 13.7% |
| Tertiary (Tafe/Uni) | 101 | 44.7% |
| ABTI | ||
| No | ||
| Yes | ||
| Country of birth | ||
| Australia | 169 | 81.6% |
| United Kingdom | 16 | 7.7% |
| New Zealand | 10 | 4.8% |
| Other | 12 | 5.8% |
| Area‐level disadvantage | ||
| 1st quartile (lowest) | 113 | 47.3% |
| 2nd | 84 | 35.1% |
| 3rd | 36 | 15.1% |
| 4th quartile (highest) | 6 | 2.5% |
| Remoteness | ||
| Inner regional | 125 | 52.3% |
| Outer regional | 102 | 42.7% |
| Remote and very remote | 12 | 5.0% |
| Cancer type (patient) | ||
| Breast | 46 | 20.6% |
| Skin | 34 | 15.2% |
| Prostate | 24 | 10.8% |
| Head and neck | 27 | 12.1% |
| Gynaecological | 21 | 9.4% |
| Colorectal | 16 | 7.2% |
| Lung | 13 | 5.8% |
| Non‐Hodgkin lymphoma | 13 | 5.8% |
| Brain | 5 | 2.2% |
| Other | 24 | 10.8% |
| Relationship to patient | ||
| Spouse/partner | 167 | 81.5% |
| Other relative | 24 | 11.7% |
| Other nonrelative | 14 | 6.8% |
| Chronic illness | ||
| Rheumatoid arthritis | 29 | 14.2% |
| Diabetes | 25 | 12.3% |
| Cancer | 23 | 11.3% |
| Cardiovascular disease | 20 | 9.8% |
| Other | 9 | 4.4% |
| Mean | SD | |
|---|---|---|
| Caregiver burden | 1.61 | 0.57 |
| Depression | 2.89 | 3.68 |
| Anxiety | 1.92 | 2.91 |
| Stress | 4.04 | 3.85 |
Calculated based on non‐missing data.
Caregivers reported significantly lower QoL for all domains within the Mental QoL super dimension (d ranges from 0.32 to 0.51) and in the Senses domain (d = 0.27) when compared with population norms (see Figure 1 and Appendix A). No significant differences were apparent between caregivers and population norms for anxiety and stress, however, caregiver depression was slightly higher than population norms (d = 0.19; see Figure 2 and Appendix A). Caregivers reported significantly higher QoL in the Physical and Mental QoL super dimensions when compared with patients (d ranges from 0.22 to 0.53) however, they reported relatively similar scores on the mental health subdimension of QoL. Caregiver anxiety was significantly lower than patient anxiety, (d = 0.25), but caregivers and patients reported relatively similar levels of depression and stress.
FIGURE 1.
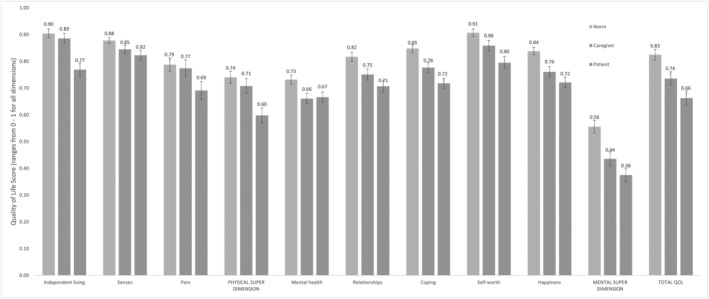
Comparison of mean QoL across patient and caregiver groups and age‐adjusted (65–74 y.o) population norms (95% CI error bars)
FIGURE 2.
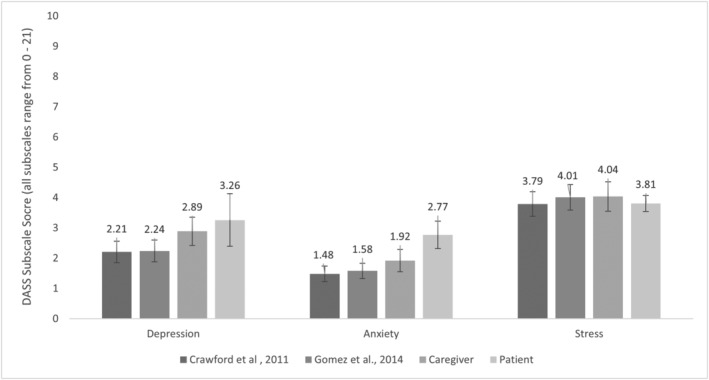
Comparison of mean depression, anxiety and stress across patient and caregiver groups and population norms (95% CI error bars)
Zero‐order correlations suggested that age was moderately, positively associated with the Mental QoL super dimension and weakly, negatively associated with the Physical QoL super dimension (see Table 2). Increased geographical remoteness was weakly associated with higher levels of Physical QoL, and greater comorbidities and caregiver burden were moderately associated with lower Physical QoL. Caregiver burden was strongly associated with poorer outcomes on all mental health related outcome variables. Patient Mental QoL super dimension scores shared small association with higher caregiver Mental QoL and lower caregiver depression and stress.
TABLE 2.
Zero‐order correlations between covariates and outcomes
| Mental QoL (super dimension) | Physical QoL (super dimension) | Depression | Anxiety | Stress | |
|---|---|---|---|---|---|
| Age | 0.216 ** | −0.134* | −0.107 | −0.048 | −0.147* |
| Gender | −0.105 | 0.027 | 0.070 | 0.060 | 0.055 |
| Days since diagnosis | −0.029 | −0.055 | −0.003 | 0.085 | 0.019 |
| SES | −0.019 | 0.040 | −0.011 | −0.025 | 0.055 |
| Remoteness | 0.044 | 0.196 * | −0.006 | −0.047 | −0.046 |
| Chronic illness | −0.101 | −0.255 ** | 0.109 | 0.132 | 0.069 |
| Caregiver burden | −0.581 ** | −0.272 ** | 0.578 ** | 0.402 ** | 0.586 ** |
| Patient cancer type | |||||
| Breast | 0.031 | 0.004 | −0.059 | −0.052 | −0.054 |
| Head and neck | −0.028 | 0.081 | 0.064 | 0.038 | 0.029 |
| Prostate | 0.032 | −0.145* | −0.053 | −0.008 | −0.062 |
| Gynaecological | 0.090 | −0.073 | −0.034 | 0.009 | 0.024 |
| Patient outcomes | |||||
| Mental QoL | 0.244 ** | 0.037 | −0.195 * * | −0.073 | −0.185 ** |
| Physical QoL | 0.053 | 0.054 | −0.077 | −0.098 | −0.109 |
| Depression | −0.108 | 0.079 | 0.086 | 0.001 | 0.068 |
| Anxiety | −0.041 | 0.018 | 0.046 | 0.018 | 0.054 |
| Stress | −0.105 | 0.088 | 0.053 | −0.010 | 0.144* |
Abbreviation: QoL, quality of life.
Significant at p < 0.01.
Significant at p < 0.05.
When entered into multivariate models alongside chronic illness, caregiver burden, cancer type, SES, gender and days since diagnosis, age and remoteness were, for the most part, no longer significantly associated with outcomes. Adjusting for covariates, caregivers who were younger, had one or more comorbidities, or reported higher levels of caregiver burden reported lower levels of Mental QoL (see Table 3). Together these predictors explained 33.9% of the variance in the Mental QoL super dimension.
TABLE 3.
General linear models predicting caregiver outcomes
| Mental QoL | Physical QoL | Depression | Anxiety | Stress | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model adjusted R 2 | 0.40 | 0.15 | 0.37 | 0.19 | 0.32 | ||||||||||
| F | p | Partial η 2 | F | p | Partial η 2 | F | p | Partial η 2 | F | p | Partial η 2 | F | p | Partial η 2 | |
| Age | 4.22 | 0.04 | 0.03 | 3.54 | 0.06 | 0.02 | 0.02 | 0.90 | 0.00 | 0.41 | 0.52 | 0.00 | 0.05 | 0.82 | 0.00 |
| Gender | 0.62 | 0.43 | 0.00 | 0.61 | 0.43 | 0.00 | 0.44 | 0.51 | 0.00 | 0.20 | 0.66 | 0.00 | 0.06 | 0.81 | 0.00 |
| Days since diagnosis | 1.84 | 0.18 | 0.01 | 0.11 | 0.74 | 0.00 | 1.81 | 0.18 | 0.01 | 0.17 | 0.68 | 0.00 | 3.94 | 0.05 | 0.02 |
| SES | 0.10 | 0.76 | 0.00 | 0.01 | 0.93 | 0.00 | 2.20 | 0.14 | 0.01 | 0.59 | 0.44 | 0.00 | 3.77 | 0.05 | 0.02 |
| Remoteness | 0.55 | 0.65 | 0.01 | 0.78 | 0.50 | 0.01 | 1.24 | 0.30 | 0.02 | 0.58 | 0.63 | 0.01 | 0.03 | 0.99 | 0.00 |
| Comorbidity | 12.13 | <0.01 | 0.07 | 7.87 | <0.01 | 0.05 | 9.34 | <0.01 | 0.06 | 5.22 | 0.02 | 0.03 | 6.35 | 0.01 | 0.04 |
| Caregiver burden | 55.46 | <0.01 | 0.26 | 16.41 | <0.01 | 0.09 | 82.33 | <0.01 | 0.34 | 39.00 | <0.01 | 0.20 | 69.33 | <0.01 | 0.30 |
| Cancer type | |||||||||||||||
| Breast | 0.23 | 0.63 | 0.00 | 0.11 | 0.74 | 0.00 | 0.74 | 0.39 | 0.00 | 0.11 | 0.74 | 0.00 | 0.00 | 0.99 | 0.00 |
| Head and neck | 0.10 | 0.75 | 0.00 | 0.36 | 0.55 | 0.00 | 0.07 | 0.79 | 0.00 | 0.01 | 0.94 | 0.00 | 0.02 | 0.89 | 0.00 |
| Prostate | 0.24 | 0.62 | 0.00 | 5.60 | 0.02 | 0.03 | 0.25 | 0.62 | 0.00 | 0.05 | 0.82 | 0.00 | 0.14 | 0.71 | 0.00 |
| Gynaecological | 1.20 | 0.27 | 0.01 | 0.09 | 0.77 | 0.00 | 1.93 | 0.17 | 0.01 | 1.41 | 0.24 | 0.01 | 0.58 | 0.45 | 0.00 |
| Patient outcomes | |||||||||||||||
| Mental QoL | 2.53 | 0.11 | 0.02 | 0.64 | 0.43 | 0.00 | 0.63 | 0.43 | 0.00 | 0.00 | 0.96 | 0.00 | 0.07 | 0.79 | 0.00 |
| Physical QoL | 0.39 | 0.53 | 0.00 | 0.74 | 0.39 | 0.00 | 0.04 | 0.85 | 0.00 | 2.09 | 0.15 | 0.01 | 0.60 | 0.44 | 0.00 |
| Depression | 0.21 | 0.65 | 0.00 | 1.44 | 0.23 | 0.01 | 0.12 | 0.73 | 0.00 | 0.79 | 0.38 | 0.00 | 2.06 | 0.15 | 0.01 |
| Anxiety | 0.33 | 0.57 | 0.00 | 0.06 | 0.81 | 0.00 | 0.43 | 0.51 | 0.00 | 0.57 | 0.45 | 0.00 | 0.23 | 0.63 | 0.00 |
| Stress | 0.00 | 0.98 | 0.00 | 0.18 | 0.67 | 0.00 | 3.95 | 0.05 | 0.02 | 0.41 | 0.52 | 0.00 | 0.87 | 0.35 | 0.01 |
Note: Bold = significant at p < 0.01.
When adjusting for covariates, caregivers who had one or more chronic condition, those with higher levels of caregiver burden, and those who were caring for someone with prostate cancer reported lower levels of Physical QoL. Together, these predictors explained 14.5% of the variance in Physical QoL.
When adjusting for covariates, caregivers who had one or more chronic condition and those who reported higher levels of caregiver burden reported higher levels of depression, anxiety and stress explaining 36.8%, 18.7% and 31.9% of the variance in each outcome variable, respectively.
Given the moderate effects of caregiver burden on outcomes and known gender differences in cancer caregiver needs and experiences (Stiller et al., 2021), post hoc analyses were conducted to assess potential moderating role of gender. An independent t‐test showed no significant difference between male and female caregiver burden t(221) = −1.27, p = 204. However, when the main analysis was repeated with a gender by caregiver burden interaction term, it was evident that associations between caregiver burden and higher depression F = 5.42, p = 0.02, η 2 = 0.03, anxiety F = 12.71, p < 0.01, η 2 = 0.08 and stress F = 6.06, p < 0.02, η 2 = 0.04 and lower Physical QoL F = 6.83, p = 0.01, η 2 = 0.04 were slightly stronger for male caregivers when compared with female caregivers.
4. DISCUSSION
These findings show that caregivers of cancer patients living in regional and remote areas are experiencing poorer than average mental health‐related QoL which is exacerbated by increasing caregiver burden and poor caregiver health. This likely reflects the emotional, physical and social toll of caring for a sick friend or relative (Jayani & Hurria, 2012; Mackenzie et al., 2007) and a reduced capacity to attend to their own health due to their caregiving responsibilities (Mosher et al., 2013). Disparities may also reflect added challenges associated with caring for someone with cancer living in a regional or remote are. In particular, moderate disparities in coping and happiness dimensions were evident. This is consistent with findings from Australian and international research showing that caregivers from outside major cities report difficulty coping with the combined burdens of extensive travel, maintaining employment and delivering patient care and the way in which these can reduce their capacity to enjoy life (Arksey & Glendinning, 2008; Hinojosa et al., 2014; Hussain et al., 2018).
The degree of caregiver burden, as shown in this study and in previous research, has strong associations with emotional and psychological distress (Balfe et al., 2018; Beach et al., 2019; Butow et al., 2014; Papastavrou et al., 2009). However, caregivers in this study did not appear to suffer from higher levels of depression or stress and reported only slightly higher levels of anxiety than the general population. Potentially this finding reflects the diffuse and chronic nature of depression, anxiety and stress symptoms, which, some suggest, are less affected by external situational stressors as opposed to internal resources and cognitive dispositions (Johnson & Sarason, 1978). Taking on the role of caring for someone with cancer may impede one's ability to function and experience the most out of life when compared with their age‐matched peers, but this, in itself, may not make substantial changes to ongoing levels of emotional distress.
The current findings suggest that caregivers on average fare no better than the cancer patients for whom they care in terms of depression and mental health as a single dimension of QoL. This may indicate that a cancer diagnosis has a similarly negative effect on both caregiver and patient in these domains. Interestingly, associations between patient and caregiver outcomes were small and patient outcomes did not share any variance with caregiver outcomes above and beyond the burden experienced by caregivers. This highlights the importance of addressing both caregiver and patient well‐being separately with equal levels of importance. According to these findings, improving the mental health of the patient may not have a large effect on the caregiver and vice versa.
The literature suggests that female caregivers often experience higher levels of burden than male caregiver (Schrank et al., 2016; Stenberg et al., 2014). This was not evident in the current findings; however, higher levels of burden were more strongly associated with poorer outcomes on depression, anxiety, stress and physical QoL for male caregivers when compared with female caregivers. This is consistent with other research suggesting that caregiver burden tends to manifest differently between male and female caregivers (Treichel et al., 2020). The increased impact of burden on outcomes for male caregivers evident here may reflect typically masculine traits that decrease one's ability to effectively deal with or reduce burden. For example, emotional help‐seeking behaviour is less common in males (Kessler et al., 1981). This could leave some male caregivers more susceptible to the emotional distress associated with caring for someone with cancer and is an important avenue for future research into improving the well‐being of all cancer caregivers.
In terms of physical health, caregivers reported significantly poorer QoL than age‐matched norms in the senses dimension which reflects sight, hearing and communication deficits. Over 40% of cancer caregivers in this regional and remote sample reported suffering from at least one chronic illness themselves which was associated with physical and emotional outcomes. This evidence reinforces recent calls for increased attention to be paid to addressing the needs of vulnerable caregivers who may need extra support (Jayani & Hurria, 2012; Lambert et al., 2019). In fact, when caregiver burden and chronic illness is accounted for, current findings suggested that factors such age, remoteness or patient outcomes have little association with caregiver well‐being. This indicates that, of all of the variables considered here, caregiver burden and caregiver chronic illness are the most important to address when in developing strategies to support regional and remote cancer caregivers. This is consistent with the recent consensus around future directions for research into supporting cancer caregivers. For example, in 2019, a panel of caregivers, clinicians, researchers and administrators agreed screening for and addressing caregiver burden (particularly financial) should be a priority moving forward (Lambert et al., 2019). The top priority identified in this study was home‐care interventions. These would be particularly beneficial for regional and remote caregivers with limited access to services who are dealing with symptoms of chronic illness themselves affecting their ability to carry out the physical aspects of care. The feasibility and optimal mode of delivery of home‐care interventions are important considerations in regional and remote settings. Distance and poor internet access can hinder in‐person and online delivery in these settings. Interventions delivered via the telephone are promising in terms of effectiveness and acceptability (Chi & Demiris, 2015; Ownsworth et al., 2021), however, combining multiple modes of contact could provide caregivers with both the practical and emotional support they require.
4.1. Strengths and limitations
This study was the first to assess the QoL of regional and remote cancer caregivers in Australia and assess their functioning relative to population norms. The findings provide novel insight into the well‐being of this caregiver population. Normative data on the AQoL‐8D and DASS‐21 measures are not available for regional and remote noncaregiver or major city caregiver groups at the time of publication meaning these direct comparisons could not be made. There is evidence to suggest that living outside of a major city can have a detrimental impact on QoL (Winterton & Warburton, 2011); however, future research is needed to confirm the role that geographical isolation plays in driving poorer outcomes for cancer caregivers.
This study provides some insight into factors that are associated with poorer outcomes for regional and remote caregivers; however, an extensive range of variables were not included and many other factors may explain further variance in outcomes, or confound associations presented here. Additionally, given the cross‐sectional nature of the study, causation cannot be implied. It is equally plausible that caregiver mental and emotional outcomes lead to higher perceptions of caregiver burden. Nevertheless, the benefits of reducing caregiver burden are supported. Other limitations to consider include the exclusion of non‐English speaking participants who are estimated to make up 6.9% of people living outside of major cities in Australia (Language Spoken at Home, n.d.) and the fact that 50% of the sample were aged below the QoL 65‐year old population comparison group. For these reasons, generalisation of results For these reasons, generalisation of results to groups outside the sample parameters should be applied with caution.
4.2. Conclusion
The mental and emotional well‐being of regional and remote cancer caregivers is poorer than that of age‐matched Australian population norms. It is paramount to address this in order to maintain their capacity to support regional and remote patients who are already at a higher risk of poor outcomes. It is recommended that interventions are devised to support cancer caregivers who have chronic conditions and to reduce caregiver burden. These should take into consideration the unique effects of caregiving on the emotional health of male caregivers. Future research is needed to identify other drivers of health outcomes in this group. It is clear that the mental health of cancer caregivers in regional and remote areas should be a key priority for intervention. Failure to acknowledge and appropriately support rural caregivers could result in a significant impost upon the health system if those supporting rural cancer patients are overburdened or incapacitated.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The authors would like to thank all the participants of this study. We would also like to acknowledge the invaluable support of our research volunteers, research assistants and Cancer Council lodge staff. Open access publishing facilitated by University of Southern Queensland, as part of the Wiley ‐ University of Southern Queensland agreement via the Council of Australian University Librarians.
APPENDIX A. MEANS, STANDARD DEVIATIONS, AND CONFIDENCE INTERVALS FOR AGE MATCHED NORMS, CAREGIVERS AND PATIENTS
| Norm | Caregiver | Patient | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable/dimension | M | SD | LCI | UCI | M | SD | LCI | UCI | M | SD | LCI | UCI |
| AQoL‐8D | ||||||||||||
| Independent living | 0.904 | 0.174 | 0.888 | 0.920 | 0.886 | 0.144 | 0.868 | 0.904 | 0.769 | 0.192 | 0.744 | 0.794 |
| Senses | 0.878 | 0.120 | 0.867 | 0.889 | 0.845 | 0.127 | 0.829 | 0.861 | 0.823 | 0.137 | 0.805 | 0.841 |
| Pain | 0.788 | 0.271 | 0.763 | 0.813 | 0.774 | 0.249 | 0.742 | 0.806 | 0.691 | 0.258 | 0.658 | 0.724 |
| PHYSICAL SUPER DIMENSION | 0.740 | 0.245 | 0.717 | 0.763 | 0.708 | 0.216 | 0.681 | 0.735 | 0.598 | 0.215 | 0.570 | 0.626 |
| Mental health | 0.732 | 0.179 | 0.715 | 0.749 | 0.661 | 0.154 | 0.642 | 0.680 | 0.666 | 0.150 | 0.647 | 0.685 |
| Relationships | 0.817 | 0.183 | 0.800 | 0.834 | 0.751 | 0.164 | 0.730 | 0.772 | 0.707 | 0.165 | 0.686 | 0.728 |
| Coping | 0.848 | 0.157 | 0.833 | 0.863 | 0.777 | 0.150 | 0.758 | 0.796 | 0.718 | 0.150 | 0.699 | 0.737 |
| Self‐worth | 0.907 | 0.146 | 0.893 | 0.921 | 0.859 | 0.153 | 0.840 | 0.878 | 0.795 | 0.176 | 0.772 | 0.818 |
| Happiness | 0.838 | 0.148 | 0.824 | 0.852 | 0.761 | 0.153 | 0.742 | 0.780 | 0.721 | 0.153 | 0.701 | 0.741 |
| MENTAL SUPER DIMENSION | 0.556 | 0.260 | 0.532 | 0.580 | 0.436 | 0.207 | 0.410 | 0.462 | 0.375 | 0.194 | 0.350 | 0.400 |
| TOTAL QOL | 0.825 | 0.216 | 0.805 | 0.845 | 0.736 | 0.196 | 0.711 | 0.761 | 0.663 | 0.208 | 0.636 | 0.690 |
| DASS 21 (Crawford et al., 2011 ) | ||||||||||||
| Depression | 2.210 | 3.600 | 1.855 | 2.565 | 2.890 | 3.680 | 2.425 | 3.355 | 3.260 | 3.510 | 2.390 | 4.130 |
| Anxiety | 1.480 | 2.600 | 1.224 | 1.736 | 1.920 | 2.910 | 1.553 | 2.287 | 2.770 | 2.460 | 2.315 | 3.225 |
| Stress | 3.790 | 4.100 | 3.386 | 4.194 | 4.040 | 3.850 | 3.554 | 4.526 | 3.810 | 3.552 | 3.545 | 4.075 |
| DASS 21 (Gomez et al., 2014 ) | ||||||||||||
| Depression | 2.24 | 3.01 | 1.880 | 2.600 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Anxiety | 1.58 | 2.10 | 1.329 | 1.831 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Stress | 4.01 | 3.53 | 3.588 | 4.432 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
Note: Norms sourced from: Maxwell A, Özmen M, Iezzi A, Richardson J. Deriving population norms for the AQoL‐6D and AQoL‐8D multiattribute utility instruments from web‐based data. Quality of life research. 2016;25(12):3209–19. Crawford J, Cayley C, Lovibond PF, Wilson PH, Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self‐report mood scales (BAI, BDI, CRSD, CES‐D, DASS, DASS‐21, STAI‐X, STAI‐Y, SRDS and SRAS). Australian Psychologist. 2011;46(1):3–14. Gomez R, Summers M, Summers A, Wolf A, Summers JJ. Depression Anxiety Stress Scales‐21: Factor structure and test–retest invariance, and temporal stability and uniqueness of latent factors in older adults. Journal of Psychopathology and Behavioural Assessment. 2014;36(2):308–17.
Goodwin, B. C. , Crawford‐Williams, F. , Ireland, M. , March, S. , Chambers, S. K. , Aitken, J. F. , & Dunn, J. (2022). The quality of life of regional and remote cancer caregivers in Australia. European Journal of Cancer Care, 31(4), e13587. 10.1111/ecc.13587
[Correction added on 13 May 2022, after first online publication: CAUL funding statement has been added.]
DATA AVAILABILITY STATEMENT
Data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Arksey, H. , & Glendinning, C. (2008). Combining work and care: Carers' decision‐making in the context of competing policy pressures. Social Policy & Administration, 42(1), 1–18. [Google Scholar]
- Australian Bureau of Statistics . (2011a). ABS. Stat SEIFA by Local Government Area (LGA). ABS. http://stat.data.abs.gov.au/Index.aspx?? DataSetCode=ABS_SEIFA_LGA [Accessed 7 November 2019] [Google Scholar]
- Australian Bureau of Statistics . (2011b). Australian Statistical Geography Standard (ASGS): Correspondences. Cat. No. 1270.0.55.006. ABS. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1270.0.55.006July%202011?OpenDocument [Accessed 7 November 2019] [Google Scholar]
- Australian Bureau of Statistics . (2020). Disability, Ageing and Carers, Australia: Summary of Findings, 2018. https://www.abs.gov.au/statistics/health/disability/disability-ageing-and-carers-australia-summary-findings/latest-release
- Australian Institute of Health and Welfare . (2017a). Australia's welfare 2017. In Brief. 2017. Australia's welfare series numbe 1. AUS 214. AIHW. [Google Scholar]
- Australian Institute of Health and Welfare . (2017b). Rural and remote health.
- Balfe, M. , O'Brien, K. M. , Timmons, A. , Butow, P. , O'Sullivan, E. , Gooberman‐Hill, R. , & Sharp, L. (2018). Informal caregiving in head and neck cancer: Caregiving activities and psychological well‐being. European Journal of Cancer Care, 27(2), e12520. 10.1111/ecc.12520 [DOI] [PubMed] [Google Scholar]
- Beach, S. R. , Kinnee, E. , & Schulz, R. (2019). Caregiving and place: Combining Geographic Information System (GIS) and survey methods to examine neighborhood context and caregiver outcomes. Innovation in Aging, 3(3), igz025. 10.1093/geroni/igz025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butow, P. N. , Price, M. A. , Bell, M. L. , Webb, P. M. , Defazio, A. , Friedlander, M. , Group, A. O. C. S. , & Investigators, L. S. (2014). Caring for women with ovarian cancer in the last year of life: A longitudinal study of caregiver quality of life, distress and unmet needs. Gynecologic Oncology, 132(3), 690–697. 10.1016/j.ygyno.2014.01.002 [DOI] [PubMed] [Google Scholar]
- Carers Australia . Replacement value of unpaid care in Australia rises to $77.9 billion per year. (2020). https://www.carersaustralia.com.au/replacement-value-of-unpaid-care-in-australia-rises-to-77-9-billion-per-year/
- Charlson, M. E. , Pompei, P. , Ales, K. L. , & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- Chi, N.‐C. , & Demiris, G. (2015). A systematic review of telehealth tools and interventions to support family caregivers. Journal of Telemedicine and Telecare, 21(1), 37–44. 10.1177/1357633X14562734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford, J. , Cayley, C. , Lovibond, P. F. , Wilson, P. H. , & Hartley, C. (2011). Percentile norms and accompanying interval estimates from an Australian general adult population sample for self‐report mood scales (BAI, BDI, CRSD, CES‐D, DASS, DASS‐21, STAI‐X, STAI‐Y, SRDS, and SRAS). Australian Psychologist, 46(1), 3–14. 10.1111/j.1742-9544.2010.00003.x [DOI] [Google Scholar]
- Crouch, E. , Probst, J. C. , & Bennett, K. (2017). Rural‐urban differences in unpaid caregivers of adults. Rural and Remote Health, 17(4), 61. 10.22605/RRH4351 [DOI] [PubMed] [Google Scholar]
- Dunn, J. , Goodwin, B. , Aitken, J. F. , March, S. , Crawford‐Williams, F. , Ireland, M. , Ralph, N. , Zajdlewicz, L. , Rowe, A. , & Chambers, S. K. (2021). Are National Cancer Control Indicators for patient experiences being met in regional and remote Australia? A cross‐sectional study of cancer survivors who travelled for treatment. BMJ Open, 11(2), e042507. 10.1136/bmjopen-2020-042507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmstaahl, S. , Malmberg, B. , & Annerstedt, L. (1996). Caregivers burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Archives of Physical Medicine and Rehabilitation, 77(2), 177–182. 10.1016/S0003-9993(96)90164-1 [DOI] [PubMed] [Google Scholar]
- Girgis, A. , & Lambert, S. (2017). Cost of informal caregiving in cancer care. Cancer Forum, 41(2), 16. [Google Scholar]
- Given, B. A. , Given, C. W. , & Kozachik, S. (2001). Family support in advanced cancer. CA: A Cancer Journal for Clinicians, 51(4), 213–231. 10.3322/canjclin.51.4.213 [DOI] [PubMed] [Google Scholar]
- Gomez, R. , Summers, M. , Summers, A. , Wolf, A. , & Summers, J. J. (2014). Depression Anxiety Stress Scales‐21: Factor structure and test‐retest invariance, and temporal stability and uniqueness of latent factors in older adults. Journal of Psychopathology and Behavioral Assessment, 36(2), 308–317. 10.1007/s10862-013-9391-0 [DOI] [Google Scholar]
- Goodwin, B. C. , Chambers, S. , Aitken, J. , Ralph, N. , March, S. , Ireland, M. , Rowe, A. , Crawford‐Williams, F. , Zajdlewicz, L. , & Dunn, J. (2021). Cancer‐related help‐seeking in cancer survivors living in regional and remote Australia. Psycho‐Oncology, 30(7), 1068–1076. 10.1002/pon.5643 [DOI] [PubMed] [Google Scholar]
- Hanly, P. , Maguire, R. , Balfe, M. , Hyland, P. , Timmons, A. , O'Sullivan, E. , Butow, P. , & Sharp, L. (2016). Burden and happiness in head and neck cancer carers: The role of supportive care needs. Supportive Care in Cancer, 24(10), 4283–4291. 10.1007/s00520-016-3261-8 [DOI] [PubMed] [Google Scholar]
- Hinojosa, R. , Hinojosa, M. S. , & Chiara, T. (2014). Rural caregivers and social isolation: Some properties and dimensions. Journal of Rural Social Sciences, 29(2), 2. [Google Scholar]
- Hudson, P. L. , Trauer, T. , Graham, S. , Grande, G. , Ewing, G. , Payne, S. , Stajduhar, K. I. , & Thomas, K. (2010). A systematic review of instruments related to family caregivers of palliative care patients. Palliative Medicine, 24(7), 656–668. 10.1177/0269216310373167 [DOI] [PubMed] [Google Scholar]
- Hussain, R. , Wark, S. , & Ryan, P. (2018). Caregiving, employment and social isolation: Challenges for rural carers in Australia. International Journal of Environmental Research and Public Health, 15(10), 2267. 10.3390/ijerph15102267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayani, R. , & Hurria, A. (2012). Caregivers of older adults with cancer. Seminars in Oncology Nursing, 28(4), 221–225. 10.1016/j.soncn.2012.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, J. H. , & Sarason, I. G. (1978). Life stress, depression and anxiety: Internal‐external control as a moderator variable. Journal of Psychosomatic Research, 22(3), 205–208. 10.1016/0022-3999(78)90025-9 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Brown, R. L. , & Broman, C. L. (1981). Sex differences in psychiatric help‐seeking: Evidence from four large‐scale surveys. Journal of Health and Social Behavior, 22, 49–64. 10.2307/2136367 [DOI] [PubMed] [Google Scholar]
- Lambert, S. D. , Ould Brahim, L. , Morrison, M. , Girgis, A. , Yaffe, M. , Belzile, E. , Clayberg, K. , Robinson, J. , Thorne, S. , Bottorff, J. L. , Duggleby, W. , Campbell‐Enns, H. , Kim, Y. , & Loiselle, C. G. (2019). Priorities for caregiver research in cancer care: An international Delphi survey of caregivers, clinicians, managers, and researchers. Supportive Care in Cancer, 27(3), 805–817. 10.1007/s00520-018-4314-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Language Spoken at Home . Australia. Community profile. (n.d.). Retrieved December 9, 2021, https://profile.id.com.au/australia/language?? WebID=245
- Lee, J. , Lee, E.‐H. , & Moon, S. H. (2019). Systematic review of the measurement properties of the Depression Anxiety Stress Scales–21 by applying updated COSMIN methodology. Quality of Life Research, 28(9), 2325–2339. 10.1007/s11136-019-02177-x [DOI] [PubMed] [Google Scholar]
- Longacre, M. L. (2013). Cancer caregivers information needs and resource preferences. Journal of Cancer Education, 28(2), 297–305. 10.1007/s13187-013-0472-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond, S. H. , & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales (2nd. ed.). Psychology Foundation. [Google Scholar]
- Lund, L. , Ross, L. , Petersen, M. A. , & Groenvold, M. (2014). Cancer caregiving tasks and consequences and their associations with caregiver status and the caregivers relationship to the patient: A survey. BMC Cancer, 14(1), 1–13. 10.1186/1471-2407-14-541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie, C. S. , Smith, M. C. , Hasher, L. , Leach, L. , & Behl, P. (2007). Cognitive functioning under stress: Evidence from informal caregivers of palliative patients. Journal of Palliative Medicine, 10(3), 749–758. 10.1089/jpm.2006.0171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell, A. , Özmen, M. , Iezzi, A. , & Richardson, J. (2016). Deriving population norms for the AQoL‐6D and AQoL‐8D multi‐attribute utility instruments from web‐based data. Quality of Life Research, 25(12), 3209–3219. 10.1007/s11136-016-1337-z [DOI] [PubMed] [Google Scholar]
- Michels, C. T. , Boulton, M. , Adams, A. , Wee, B. , & Peters, M. (2016). Psychometric properties of carer‐reported outcome measures in palliative care: A systematic review. Palliative Medicine, 30(1), 23–44. 10.1177/0269216315601930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher, C. E. , Adams, R. N. , Helft, P. R. , O'Neil, B. H. , Shahda, S. , Rattray, N. A. , & Champion, V. L. (2017). Positive changes among patients with advanced colorectal cancer and their family caregivers: A qualitative analysis. Psychology & Health, 32(1), 94–109. 10.1080/08870446.2016.1247839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher, C. E. , Jaynes, H. A. , Hanna, N. , & Ostroff, J. S. (2013). Distressed family caregivers of lung cancer patients: An examination of psychosocial and practical challenges. Supportive Care in Cancer, 21(2), 431–437. 10.1007/s00520-012-1532-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownsworth, T. , Chan, R. J. , Jones, S. , Robertson, J. , & Pinkham, M. B. (2021). Use of telehealth platforms for delivering supportive care to adults with primary brain tumors and their family caregivers: A systematic review. Psycho‐Oncology, 30(1), 16–26. 10.1002/pon.5549 [DOI] [PubMed] [Google Scholar]
- Papastavrou, E. , Charalambous, A. , & Tsangari, H. (2009). Exploring the other side of cancer care: The informal caregiver. European Journal of Oncology Nursing, 13(2), 128–136. 10.1016/j.ejon.2009.02.003 [DOI] [PubMed] [Google Scholar]
- Richardson, J. , Iezzi, A. , Khan, M. A. , & Maxwell, A. (2014). Validity and reliability of the Assessment of Quality of Life (AQoL)‐8D multi‐attribute utility instrument. The Patient‐Patient‐Centered Outcomes Research, 7(1), 85–96. 10.1007/s40271-013-0036-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romito, F. , Goldzweig, G. , Cormio, C. , Hagedoorn, M. , & Andersen, B. L. (2013). Informal caregiving for cancer patients. Cancer, 119, 2160–2169. 10.1002/cncr.28057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, M. W. , & Eckstrom, E. (2020). Geographic differences in the unpaid caregiver experience from the National Study of caregiving (NSOC). Rural and Remote Health, 20(4), 6062. 10.22605/RRH6062 [DOI] [PubMed] [Google Scholar]
- Schrank, B. , Ebert‐Vogel, A. , Amering, M. , Masel, E. K. , Neubauer, M. , Watzke, H. , Zehetmayer, S. , & Schur, S. (2016). Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psycho‐Oncology, 25(7), 808–814. 10.1002/pon.4005 [DOI] [PubMed] [Google Scholar]
- Stenberg, U. , Cvancarova, M. , Ekstedt, M. , Olsson, M. , & Ruland, C. (2014). Family caregivers of cancer patients: Perceived burden and symptoms during the early phases of cancer treatment. Social Work in Health Care, 53(3), 289–309. 10.1080/00981389.2013.873518 [DOI] [PubMed] [Google Scholar]
- Stiller, A. , Goodwin, B. C. , Crawford‐Williams, F. , March, S. , Ireland, M. J. , Aitken, J. F. , Dunn, J. , & Chambers, S. K. (2021). The supportive care needs of regional and remote cancer caregivers. Under Review, 28(4), 3041–3057. 10.3390/curroncol28040266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung, H. , Ferlay, J. , Siegel, R. L. , Laversanne, M. , Soerjomataram, I. , Jemal, A. , & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Treichel, C. A. d. S. , Jardim, V. M. D. R. , Kantorski, L. P. , & Alves, P. F. (2020). Gender differences in the manifestation of burden among family caregivers of people with mental disorders. International Journal of Mental Health Nursing, 29(6), 1120–1130. 10.1111/inm.12752 [DOI] [PubMed] [Google Scholar]
- Ugalde, A. , Blaschke, S. , Boltong, A. , Schofield, P. , Aranda, S. , Phipps‐Nelson, J. , Chambers, S. K. , Krishnasamy, M. , & Livingston, P. M. (2019). Understanding rural caregivers experiences of cancer care when accessing metropolitan cancer services: A qualitative study. BMJ Open, 9(7), e028315. 10.1136/bmjopen-2018-028315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryn, M. , Sanders, S. , Kahn, K. , Van Houtven, C. , Griffin, J. M. , Martin, M. , Atienza, A. A. , Phelan, S. , Finstad, D. , & Rowland, J. (2011). Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psycho‐Oncology, 20(1), 44–52. 10.1002/pon.1703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2017). Integrated care for older people (ICOPE): Guidelines on community‐level interventions to manage declines in intrinsic capacity. World Health Organization. [PubMed] [Google Scholar]
- Winterton, R. , & Warburton, J. (2011). Does place matter? Reviewing the experience of disadvantage for older people in rural Australia. Rural Society, 20(2), 187–197. 10.5172/rsj.20.2.187 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data that support the findings of this study are available from the corresponding author upon reasonable request.


