Abstract
Objectives
We examined the effect of fluoridation cessation on children's dental caries experience in the Canadian cities of Calgary (cessation in 2011) and Edmonton (still fluoridated).
Methods
We used a pre‐post cross‐sectional design with comparison group. We studied Grade 2 schoolchildren (approximately 7 years old) 7‐8 years after fluoridation cessation in Calgary, thus capturing children born after cessation occurred. Data collection included a dental examination conducted in school by calibrated dental hygienists, a questionnaire completed by parents, and fingernail clippings for a small subsample. Our overall analytic approach was twofold. We first examined differences in dental caries experience (deft and DMFT, and smooth surface caries based on defs and DMFS) between Calgary and Edmonton and over time (comparing 2018/2019 data to pre‐cessation and early post‐cessation surveys in our setting). Second, we evaluated whether differences were likely to reflect fluoridation cessation in Calgary, rather than other factors.
Results
The prevalence of caries in the primary dentition was significantly higher (P < .05) in Calgary (fluoridation cessation) than in Edmonton (still fluoridated). For example, crude deft prevalence in 2018/2019 was 64.8% (95% CI 62.3‐67.3), n = 2649 in Calgary and 55.1% (95% CI 52.3‐57.8), n = 2600 in Edmonton. These differences were consistent and robust: they persisted with adjustment for potential confounders and in the subset of respondents who were lifelong residents and reported usually drinking tap water; they had widened over time since cessation; and they were corroborated by assessments of dental fluorosis and estimates of total fluoride intake from fingernail clippings. Findings for permanent teeth were less consistent, which likely reflects that 7‐year‐olds have not had the time to accumulate enough permanent dentition caries experience for differences to have become apparent.
Conclusions
Our findings are consistent with an adverse impact of fluoridation cessation on children's dental health in Calgary and point to the need for universal, publicly funded prevention activities—including but not limited to fluoridation.
Keywords: caries, dental health, fluoridation, prevention, public health policy
1. INTRODUCTION
Community water fluoridation—the controlled adjustment of the fluoride content of a public water supply to a level recommended to prevent tooth decay—is a hallmark of universal primary prevention in public health. 1 , 2 Since its initial implementation in the 1940s in communities in Canada and the United States, 3 , 4 fluoridation has been credited with achieving significant—although not uncontested—population‐level benefits to dental health, such as lower prevalence of dental caries in children. 5 , 6 There is consistent evidence for an association between an increase in the level of fluoride in drinking water and an increase in the prevalence of dental fluorosis, which in most cases is mild (i.e. not considered to be of aesthetic concern). 7
Fluoride in drinking water can affect teeth both pre‐eruptively (systemic effect) and post‐eruptively (topical effect). 8 The post‐eruptive mechanism is more effective for preventing tooth decay on the smooth surfaces of the teeth, than on the occlusal pit and fissure surfaces. 9 A comprehensive understanding of the effect of fluoridation thus requires attention to whole teeth as well as to tooth surfaces.
In Canada, population exposure to fluoridation has recently declined, from 43% in 2007 to 39% in 2017, 10 reflecting decisions by municipal governments to cease the practice. The decrease was largely driven by the decision to cease fluoridation in the large city of Calgary, which is the setting of the present research. 11
Research on the implications of fluoridation cessation for dental health is limited. A 2016 systematic review identified research on just 15 instances of cessation, which covered a broad time frame (1956‐2003) and diverse settings (13 countries). Findings pointed more to an increase in dental caries post‐cessation than otherwise, but the literature was geographically and socio‐politically diverse, and variable in methodological quality. 12 A subsequent study in the relatively remote city of Juneau, Alaska, USA, identified that fluoridation cessation was robustly associated with more caries‐related dental procedures (and associated costs) including restorations and treatments, based on Medicaid dental claims billing records, among children and adolescents age 0‐18 years whose family income met Medicaid requirements. 13
Whether or not fluoridation cessation leads to an increase in caries experience is likely to depend on the setting in question. Across Canada, over 90% of dental care services are financed and delivered in the private sector, 14 which results in large numbers of people foregoing dental services due to cost. 15 This includes both access to treatment of caries and protection from consequences of disease such as pain and sepsis, and—with particular relevance to whether or not fluoridation is in place—access to preventive services such as sealants and topical fluoride. This study was conducted in the province of Alberta, where dental care costs are among the highest in Canada. 16 Income inequality in the province is high, 17 and significant social inequities in children's dental problems exist. 18 , 19 In such a setting, one might predict that a universal primary prevention measure like fluoridation would be beneficial, and its cessation problematic, for dental health.
We began to explore this prediction in previous work, where we compared children's dental caries experience in Calgary (fluoridation began in 1991 and ceased in 2011) and Edmonton (still fluoridated, since 1967), 2 to 3 years post‐cessation, compared to available pre‐cessation data (2004/2005). 20 , 21 Although dental caries experience in the primary dentition increased in both cities during the time frame of the study (consistent with trends reported elsewhere), 22 the increase was larger and more consistent in Calgary (fluoridation cessation). We concluded that our findings were consistent with a short‐term adverse effect of fluoridation cessation on children's dental caries experience, and on social inequities in children's dental caries experience, 23 but they required further study to confirm the effect following a longer period of exposure to fluoridation or its absence.
Our objective was therefore to examine the longer‐term effect of fluoridation cessation on children's dental caries experience via a comparison of children in Calgary and Edmonton. This study builds on our previous work by extending the time frame since cessation, which is important for 2 reasons. First, it improves the precision of our exposure variable (exposure to fluoridation). That is, unlike our previous study 21 where children in both cities were exposed to fluoridation until approximately age 3‐4 years, the present study included children born after fluoridation cessation in Calgary. It thus captured the cohort of lifelong child residents who were never exposed to fluoridation (Calgary) and those who were always exposed (Edmonton). 24 Second, it includes early life periods of tooth development, this allows us to consider fluoridation's pre‐ and post‐eruptive effects on the mixed dentition. 25 , 26
2. METHODS
2.1. Study design and setting
The study had a pre‐post cross‐sectional design with comparison group (see Figure 1). Here we present data collected during the 2018/2019 school year, which we compared with data from our previously published pre‐ and post‐cessation surveys. 21
FIGURE 1.
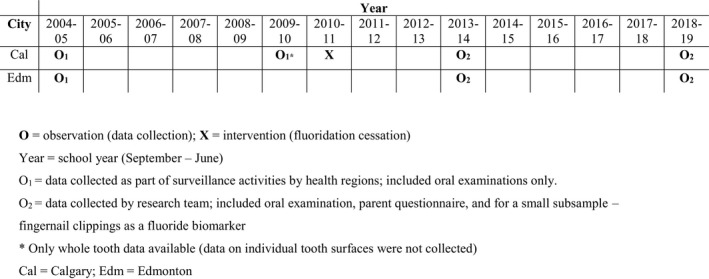
Schematic of study design
Calgary and Edmonton are the 2 largest cities in the province of Alberta, Canada (2016 population approximately 1.24 million and 932 500 respectively). 27 Census data confirmed that they are reasonably well matched. In 2016, Calgary and Edmonton census subdivisions had the following respective characteristics 28 : 18.3% and 17.6% of the population was age 0‐14 years,18.6% and 19.2% reported speaking most often at home a language other than English or French; 31.3% and 30% were immigrants; and 36.2% and 37.1% were visible minorities. Larger differences were evident in the prevalence of low‐income status (12.9% in Calgary; 16.1% in Edmonton) and in the percentage of households with a bachelor's degree or higher (33.2% in Calgary; 27.3% in Edmonton).
Annual water quality reports confirmed fluoridation cessation in Calgary in 2011 and generally continuous fluoridation in Edmonton (see Appendix 1 for details).
2.2. Target population, sampling, and data collection
The target population was Grade 2 children (approximately age 7 years) enrolled in Public or Separate school systems in cities of Calgary and Edmonton. In 2018/2019, over 90% of all Alberta schoolchildren were enrolled in one of these systems. 29 Grade 2 children, who are in the mixed dentition stage 30 were selected to be consistent with previous surveys. 21
A population‐based sample was drawn from each city using a stratified random sampling procedure; strata were based on neighbourhood income level of school location. In each school that agreed to participate, all families of Grade 2 students were invited to participate. Response rates in 2018/2019 were 53.8% (Edmonton) and 46.7% (Calgary) for schools, and 44.5% (Edmonton) and 43.7% (Calgary) for students in participating schools (i.e. those with both oral examination and questionnaire data, see below). We developed sampling weights that accounted for the probability of selection (as per the sampling frame) and the probability of non‐response, thus increasing the extent to which our samples resembled the underlying target populations. This approach enabled us to handle missing observations within the framework of our survey sampling approach rather than, for example, having to estimate differences between our samples and the target populations. 31
Based on a sample size calculation that included design effects from our previous survey, an anticipated feasible sample size, an alpha of 0.05, and prevalence of primary tooth caries experience as the metric, we had 80% power to detect an increase in caries experience post‐cessation (2013/2014—2018/2019) in Calgary that was larger than the change in Edmonton, and an increase in caries experience post‐cessation in Calgary that was larger than the pre‐cessation increase (2004/2005—2009/2010).
Data collection included 3 components: (i) an oral examination was conducted at school by trained and calibrated assessment teams each consisting of a registered dental hygienist and a clerk; (ii) a paper questionnaire including validated and field‐tested questions drawn from elsewhere 32 , 33 was distributed to and voluntarily completed by parents, and (iii) for a small random subsample in each city (1 participant was randomly selected each week from those with parental consent), fingernail clippings were collected, with no information recorded other than city of residence.
The oral examination followed the protocol from the Iowa Fluoride Study, 34 which is based on the World Health Organization survey criteria 35 and yields whole tooth codes and 2‐digit surface‐specific codes. Assessments were based on all primary teeth and a subset of 12 permanent teeth (central incisors, lateral incisors and 1st molars). In addition to deft, defs, DMFT, and DMFS (see below), presence/absence of dental sealants, and dental fluorosis based on the Tooth Surface Index of Fluorosis [TSIF] criteria 36 were assessed. Dental fluorosis is a marker of ingested fluoride from all sources during the developmental period of early‐erupting permanent teeth, and it generally appears as white lines or flecks on permanent teeth. Intra‐ and inter‐examiner reliability were assessed and found to be high (kappa ≥ 0.80 most of the time, see Appendix 2). Written parent consent and verbal child assent were secured, and a note was sent home to parents that provided the examination outcome and a list of dental treatment options.
Fingernail clippings, which are a valid and reasonably non‐intrusive biomarker for recent fluoride intake, 37 , 38 provided a means of validating the exposure. That is, fingernail estimates of total fluoride intake in 2018/2019 should be higher in Edmonton (still fluoridated) than in Calgary (fluoridation cessation), if not, then fluoridation status is unlikely to account for any differences observed in dental caries experience. Analysis of clippings (see Appendix 3) was blind to city and fluoridation status.
2.3. Primary outcome variables and analysis
We report on tooth and surface‐level measures of caries experience.1 Tooth‐level measures were dental caries experience in the primary dentition (deft) and in the permanent dentition (DMFT). The deft and DMFT are standard index metrics of decay experience. Each tooth present in the mouth was categorized as having no decay experience, having decay (d, D), being extracted or missing due to decay (e, M), or having fillings (f, F).
Tooth surface‐level measures—namely, defs (primary teeth) and DMFS (permanent teeth) —were similarly derived except the categorizations (d, D; f, F; and e, M) were made for each surface of each tooth present in the mouth. Extracted and missing teeth were counted as one surface to be consistent with our previous analysis. 20 We focused specifically on smooth tooth surfaces, using notation of defs‐ss (primary teeth) and DMFS‐SS (permanent teeth). Our designation of smooth surfaces included all surfaces except occlusal surfaces and other surfaces where pit and fissure caries commonly occurs, namely buccal (vestibular) surfaces for teeth 46 and 36, and lingual surfaces for teeth 16 and 26.
The distributions for all dental caries indicators (deft, DMFT, defs‐ss, DMFS‐SS) were skewed with many zero values. Therefore, we considered several versions: the overall mean (average) number of teeth with evidence of caries experience, including those with no caries experience; the prevalence (presence versus absence) of caries experience; and the mean number of teeth with caries experience among children with caries experience (those with non‐zero values).
A single dental fluorosis score (based on the TSIF criteria) was assigned to each child based on the most severe level of fluorosis detected on the central maxillary incisors (permanent teeth only, and only if at least half erupted). Dental fluorosis was expressed as prevalence (% with TSIF ≥ 1); we also report the percent of children with severe (pitting or staining) levels (% with TSIF 4‐7).
Data were analyzed using Stata Version 16.1. 39 We first computed weighted point estimates (mean or %) with 95% confidence intervals (95% CI) for all dental indicators to permit comparison between Calgary and Edmonton samples in 2018/2019. We computed 3 versions of the point estimates: “crude” (i.e. weighted estimates for the full samples), “adjusted” (i.e. weighted estimates, adjusted for covariates gathered via the questionnaire); and “subset” (i.e. crude, weighted estimates for those who, based on questionnaire data, were lifelong residents of Calgary or Edmonton and reported usually drinking tap water). The adjusted estimates and their difference between Calgary and Edmonton were estimated and tested via Poisson, Zero‐inflated Poisson, or logistic regression models (as appropriate). The adjusting variables included all covariates (shown in Table 2), regardless of differences between Calgary or Edmonton, for simplicity.
TABLE 2.
Weighted estimates (percent) with 95% confidence intervals for variables derived from the parent questionnaire, grade 2 students in Calgary and Edmonton in 2018/2019
| Variable | Calgary (F‐cess) | Edmonton (F‐cont) |
|---|---|---|
| General health of child's mouth: % excellent/very good | 50.2 (47.5‐52.8), n = 2595 | 49.6 (47.0‐52.2), n = 2557 |
| Brush twice/day: % yes | 68.7 (66.7‐70.7), n = 2599a | 63.9 (61.4‐66.3), n = 2566 |
| Floss once/day: % yes | 23.3 (21.5‐25.2), n = 2591a | 16.9 (15.1‐18.8), n = 2550 |
| Visit dentist “about once/year for treatment or prevention”: % yes | 88.1 (86.2‐89.7) n = 2599a | 84.6 (82.6‐86.3). n = 2561 |
| Last time visit dentist: % within the last year: % yes | 83.3 (81.1‐85.2), n = 2563a | 79.0 (77.1‐80.8), n = 2511 |
| Dental insurance: % yes | 86.2 (84.6‐87.7), n = 2569 | 84.4 (82.6‐86.0) n = 2514 |
| Fruits & vegetables at least once/day: % yes | 73.5 (70.8‐76.0), n = 2584 | 70.7 (68.5‐72.8), n = 2543 |
| Sugary drinks (i.e. fruit drink, sports drink, non‐diet pop) at least once/day: % no | 92.0 (90.2‐93.5), n = 2584a | 89.1 (87.4‐90.7), n = 2536 |
| Fluoride supplements at home: % yes [ever]b | 6.4 (5.4‐7.6), n = 2564 | 5.0 (4.2‐6.0), n = 2527 |
| Fluoride treatments at the dentist's office: % yes [ever]b | 59.7 (56.6‐62.7), n = 2566a | 50.5 (47.7‐53.3), n = 2509 |
| Fluoride treatments in school program: % yes [ever]b | 21.3 (17.8‐25.4), n = 2555 | 17.5 (14.0‐21.7), n = 2515 |
| Uses fluoride toothpaste: % yesb | 81.8 (79.8‐83.7), n = 2575 | 80.3 (78.4‐82.2), n = 2507 |
| Uses fluoride mouth wash: % yesb | 25.1 (23.3‐27.0), n = 2573a | 20.9 (19.1‐22.8), n = 2514 |
| Household education: % ≥ bachelor's degree | 60.9 (57.0‐64.5), n = 2570a | 52.9 (48.9‐56.8), n = 2536 |
| Home ownership: % yes [with or without mortgage] | 71.4 (67.6‐74.8), n = 2534 | 67.4 (63.8‐70.7), n = 2466 |
| Ethnocultural background: % white | 38.4 (34.1‐42.8), n = 2649 | 33.7 (30.3‐37.3), n = 2600 |
Statistically significant difference (P < .05) between Calgary and Edmonton based on Pearson's chi‐squared statistic.
“No” (comparison category) includes responses of “don't know.”
Second, we examined and compared trends over time in the prevalence of dental indicators between Calgary and Edmonton samples using a difference‐in‐differences approach. 40 This analysis included pre‐cessation (2004/2005 and 2009/2010 [Calgary only]), early post‐cessation (2013/2014), and later post‐cessation (2018/2019) data points. Crude estimates were used because adjusted and subset estimates were not available for pre‐cessation surveys due to absence of a questionnaire. For prevalence of deft, defs‐ss, DMFT, DMFS‐SS, and dental fluorosis, we tested whether the post‐cessation (2013/2014—2018/2019) change in Calgary differed from that in Edmonton. For deft prevalence only, as per our power calculation, we also tested whether Calgary's post‐cessation change differed from its pre‐cessation (2004/2005—2009/2010) change.
Third, to explore the potential role of professional treatment services, we compared 2018/2019 weighted point estimates (%) with 95% CI between Calgary and Edmonton samples for a variable that disaggregated the deft and DMFT indices into untreated (decayed) and treated (extracted/missing due to caries and filled) components. To assess the potential role of professional preventive services, we compared the proportions, in 2018/2019, of children with preventive dental sealants which, as noted above, was also assessed as part of the oral examination.
Finally, we considered the findings of the fingernail clipping analysis for consistency with the other data. Specifically, we compared Calgary and Edmonton estimates of mean (95% CI) and median (inter‐quartile range) fluoride content (µg/g) from the fingernail clippings that we collected from a random subsample in each city.
The study was approved by the Conjoint Health Research Ethics Board at the University of Calgary (REB18‐0273) and the Health Research Ethics Board at the University of Alberta (Pro00081226).
3. RESULTS
Sample sizes for indicators of dental caries experience in 2018/2019 were: n = 2649 (Calgary deft and defs‐ss), n = 2627 (Calgary DMFT and DMFS‐SS), n = 2600 (Edmonton deft and defs‐ss) and n = 2569 (Edmonton DMFT and DMFS‐SS). Analyses that included covariates were based on lower numbers due to missing or unusable questionnaire responses, which were generally small.
3.1. Comparison of dental health indicators between Calgary and Edmonton samples in 2018/2019
Table 1 shows weighted point estimates (mean or %) with 95% CI for all dental indicators including crude, covariate‐adjusted (see Table 2 for a list of covariates), and subset (lifelong residents in Calgary or Edmonton who reported usually drinking tap water) estimates.
TABLE 1.
Weighted estimates (mean or percent) with 95% confidence intervals of dental caries experience (deft, defs‐ss, DMFT, DMFS‐SS) and fluorosis (TSIF) for Calgary and Edmonton samples of grade 2 students in 2018/2019
| City | Indicator | 1. Crude | 2. Adjusted | 3. Subset |
|---|---|---|---|---|
| Primary teeth: deft | ||||
| Calgary | Mean deft | 3.6 (3.4‐3.8), n = 2649a | 3.1 (2.9‐3.3), n = 2317a | 3.2 (2.9‐3.4), n=918a |
| % deft ≥ 1 | 64.8 (62.3‐67.3), n = 2649a | 66.1 (63.6‐68.6), n = 2317a | 60.8 (57.0‐64.5), n=918a | |
| Mean deft if ≥ 1 | 5.5 (5.3‐5.7), n = 1690a | 5.4 (5.3‐5.6), n = 1458a | 5.2 (5.0‐5.5), n=554a | |
| Edmonton | Mean deft | 2.6 (2.4‐2.8), n = 2600 | 2.6 (2.5‐2.8), n = 2217 | 2.0 (1.7‐2.3), n = 799 |
| % deft ≥ 1 | 55.1 (52.3‐57.8), n = 2600 | 54.3 (51.4‐57.2), n = 2217 | 44.5 (39.9‐49.2), n = 799 | |
| Mean deft if ≥ 1 | 4.7 (4.5‐5.0), n = 1421 | 4.6 (4.4‐4.8), n = 1185 | 4.5 (4.1‐4.8), n = 350 | |
| Primary teeth: defs‐ss | ||||
| Calgary | Mean defs‐ss | 6.2 (5.7‐6.8), n = 2649a | 5.5 (5.0‐6.0), n = 2317a | 5.2 (4.5‐5.8), n=918a |
| % defs‐ss ≥ 1 | 60.4 (57.8‐62.9), n = 2649a | 61.5 (58.8‐64.1), n = 2317a | 56.4 (52.4‐60.3), n= 918a | |
| Mean defs‐ss if ≥ 1 | 10.3 (9.7‐10.9), n = 1568 | 9.8 (9.3‐10.4), n = 1352 | 9.1 (8.2‐10.0), n = 513 | |
| Edmonton | Mean defs‐ss | 5.2 (4.7‐5.7), n = 2600 | 4.4 (4.0‐4.8), n = 2217 | 4.0 (3.3‐4.8), n = 799 |
| % defs‐ss ≥ 1 | 50.7 (48.0‐53.4), n = 2600 | 49.9 (47.1‐52.7), n = 2217 | 40.8 (36.3‐45.4), n = 799 | |
| Mean defs‐ss if ≥ 1 | 10.2 (9.5‐10.8), n = 1306 | 9.6 (9.0‐10.2), n = 1096 | 9.8 (8.5‐11.1), n = 319 | |
| Permanent teeth: DMFT | ||||
| Calgary | Mean DMFT | 0.33 (0.28‐0.37), n = 2627a | 0.30 (0.25‐0.34), n = 2296a | 0.26 (0.20‐0.33), n = 912 |
| % DMFT ≥ 1 | 18.1 (16.1‐20.3), n = 2627a | 16.8 (14.5‐19.1), n = 2296a | 15.4 (12.4‐18.9), n = 912 | |
| Mean DMFT if ≥ 1 | 1.8 (1.7‐1.9), n=456a | 1.8 (1.7‐1.9), n=388a | 1.7 (1.6‐1.9), n=134a | |
| Edmonton | Mean DMFT | 0.21 (0.17‐0.25), n = 2569 | 0.19 (0.16‐0.22), n = 2194 | 0.19 (0.13‐0.24), n = 791 |
| % DMFT ≥ 1 | 13.6 (11.5‐16.0), n = 2569 | 12.5 (10.4‐14.6), n = 2194 | 12.4 (9.6‐15.9), n = 791 | |
| Mean DMFT if ≥ 1 | 1.5 (1.4‐1.6), n = 350 | 1.5 (1.4‐1.6), n = 300 | 1.5 (1.4‐1.6), n = 95 | |
| Permanent teeth: DMFS‐SS | ||||
| Calgary | Mean DMFS‐SS | 0.05 (0.03‐0.07), n = 2627 | 0.04 (0.02‐0.06), n = 2296 | 0.04 (0.01‐0.06), n = 912 |
| % DMFS‐SS ≥ 1 | 2.6 (1.9‐3.4), n = 2627 | 2.0 (1.3‐2.7), n = 2296 | 1.5 (0.80‐2.7), n = 912 | |
| Mean DMFS‐SS if ≥ 1 | 2.01 (1.7‐2.4), n = 60 | 1.93 (1.62‐2.25), n = 51 | 2.3 (1.6‐3.0), n = 13 | |
| Edmonton | Mean DMFS‐SS | 0.05 (0.03‐0.07), n = 2569 | 0.05 (0.03‐0.07), n = 2194 | 0.05 (0.02‐0.09), n = 791 |
| % DMFS‐SS ≥ 1 | 2.6 (2.0‐3.3), n = 2569 | 2.3 (1.5‐3.0), n = 2194 | 2.4 (1.4‐4.0), n = 791 | |
| Mean DMFS‐SS if ≥ 1 | 2.03 (1.6‐2.4), n = 65 | 1.94 (1.59‐2.30), n = 58 | 0.04 (0.01‐0.06), n = 912 | |
| Fluorosis | ||||
| Calgary | % TSIF 1‐7 | 8.3 (6.6‐10.3), n = 1620a | 7.7 (5.9‐9.6), n = 1406a | 6.2 (4.3‐8.9), n=570a |
| Edmonton | % TSIF 1‐7 | 19.4 (16.3‐22.9), n = 1402 | 18.3 (14.9‐21.6), n = 1206 | 18.8 (14.4‐24.2), n = 423 |
Crude = weighted but unadjusted for covariates.
Adjusted = weighted and adjusted for all covariates in Table 2.
Subset = weighted, crude estimates (to maximize n) for the subset of respondents who, based on questionnaire data, were lifelong residents of Calgary and Edmonton and reported usually drinking tap water.
Calgary, ceased fluoridation in 2011; Edmonton—continuous fluoridation.
TSIF = Tooth Surface Index of Fluorosis. Of those with any fluorosis, the percent with staining or pitting (TSIF 4‐7) was <1% in both cities (0.1% in Calgary and 0.5% in Edmonton).
Calgary estimate differs significantly from Edmonton estimate, P < .05. For crude and subset estimates, statistical significance was based on Pearson Chi Square test (for proportions) or adjusted Wald test (for means). For adjusted estimates, statistical significance was tested via Poisson, Zero‐inflated Poisson, or logistic regression models (as appropriate) that adjusted for covariates shown in Table 2.
Focusing first on dental caries experience in the primary dentition (deft, defs‐ss), Table 1 shows that estimates (mean and prevalence) in 2018/2019 were statistically significantly higher in Calgary (fluoridation cessation) than in Edmonton (still fluoridated). This difference was evident in the crude estimates (first column of Table 1), it was robust to adjustment for covariates (second column) and it persisted in the subset (third column). For example, the covariate‐adjusted prevalence of deft was 66.1% (63.6‐68.6) in Calgary and 54.3% (51.4‐57.2) in Edmonton, while the covariate‐adjusted prevalence of defs‐ss was 61.5% (58.8‐64.1) in Calgary and 49.9% (47.1‐52.7) in Edmonton. The 1 exception was the mean number of smooth surface caries among those with caries experience (mean defs‐ss if defs‐ss ≥ 1), which did not differ between Calgary and Edmonton.
For the permanent dentition, the mean DMFT, and the prevalence of DMFT, in 2018/2019 were significantly higher in Calgary (fluoridation cessation) than in Edmonton (still fluoridated) in the crude and adjusted analyses (first and second columns of Table 1). For example, the covariate‐adjusted prevalence of DMFT was 16.8% (14.5‐19.1) in Calgary and 12.5% (10.4‐14.6) in Edmonton. Although the DMFT estimates in the Calgary subset appeared higher than those in Edmonton (third column of Table 1), the differences were not statistically significant at the 0.05 level (for example, DMFT prevalence for the subset was 15.4% [12.4‐18.9] in Calgary and 12.4% [9.6‐15.9] in Edmonton, no statistical difference at 0.05 level). For smooth surface caries in the permanent dentition (DMFS‐SS), there were no statistically significant differences between Calgary and Edmonton samples.
Table 1 also shows that the crude prevalence of dental fluorosis (% TSIF ≥ 1) was statistically significantly lower in Calgary (fluoridation cessation) at 8.3% (6.6‐10.3) than in Edmonton (still fluoridated) children at 19.4% (16.3‐22.9). This difference was also evident in the adjusted analysis and in the subset. Of those with any fluorosis, the percent with staining or pitting (TSIF 4‐7) was less than 1% in both cities: 0.1% in Calgary and 0.5% in Edmonton.
3.2. Change over time (2004/2005—2018/2019) in dental indicators in Calgary and Edmonton samples
Figure 2 (and Table S1) illustrates the trends over time in crude prevalence of deft, defs‐ss, DMFT, DMFS‐SS, and dental fluorosis.
FIGURE 2.
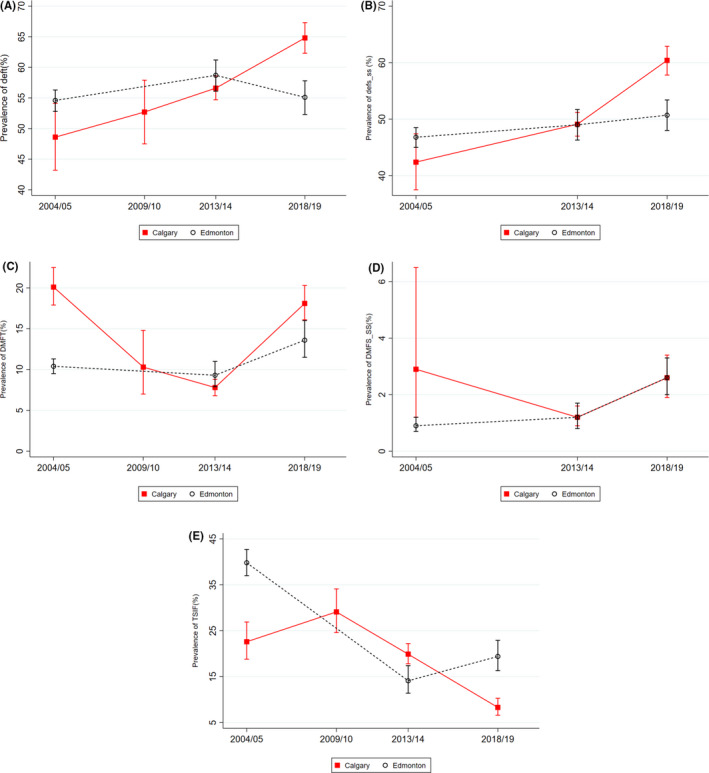
Trends over time in dental caries experience and fluorosis (crude, weighted estimates) for Grade 2 schoolchildren in Calgary and Edmonton. Fluoridation cessation in Calgary occurred in 2011. A, Trends over time in prevalence (with 95% confidence interval) of dental caries in primary teeth (deft ≥ 1) among Grade 2 students in Calgary (2004/2005, 2009/2010, 2013/2014, and 2018/2019) and Edmonton (2004/2005, 2013/2014, 2018/2019). B, Trends over time in prevalence (with 95% confidence interval) of smooth surface dental caries in primary teeth (defs‐ss ≥ 1) among Grade 2 students in Calgary and Edmonton (2004/2005, 2013/2014, 2018/2019). C, Trends over time in prevalence (with 95% confidence intervals) of dental caries in permanent teeth (DMFT ≥ 1) among Grade 2 students in Calgary (2004/2005, 2009/2010, 2013/2014, and 2018/2019) and Edmonton (2004/2005, 2013/2014, 2018/2019). D, Trends over time in prevalence (with 95% confidence interval) of smooth surface dental caries in permanent teeth (DMFS‐SS ≥ 1) among Grade 2 students in Calgary and Edmonton (2004/2005, 2013/2014, 2018/2019). E, Trends over time in prevalence (with 95% confidence interval) of dental fluorosis (TSIF ≥ 1) among Grade 2 students in Calgary (2004/2005, 2009/2010, 2013/2014, and 2018/2019) and Edmonton (2004/2005, 2013/2014, 2018/2019)
For the primary dentition (Figure 2A and B), the post‐cessation change in caries prevalence in Calgary was significantly larger than that in Edmonton, for deft (coefficient [95% CI] for difference of changes: 0.2 [0.1‐0.3], P < .001) and for defs‐ss (coefficient [95% CI] for difference of changes: 0.2 [0.1‐0.2], P < .001). For example, in Calgary, deft prevalence increased from 56.6% (54.7‐58.6) in 2013/2014 to 64.8% (62.3‐67.3) in 2018/2019, while in Edmonton it went from 58.7% (56.1‐61.2) in 2013/2014 to 55.1% (52.3‐57.8) in 2018/2019. For deft prevalence, Calgary's post‐cessation change did not differ significantly from its pre‐cessation change (from 48.6% [43.2‐54.1] in 2004/2005 to 52.7% [47.5‐57.9 in 2009/2010) (coefficient [95% CI] for difference of changes: 0.0 [−0.0 to 0.1], P = .28).
For the permanent dentition, the post‐cessation change in DMFT prevalence (Figure 2C) in Calgary (from 7.8% [6.8‐8.8] in 2013/2014 to 18.1% [16.1‐20.3] in 2018/2019) was significantly larger than in Edmonton (from 9.3% [7.9‐11.0] in 2013/2014 to 13.6% [11.5‐16.0] in 2018/2019) (coefficient [95% CI] for difference of changes: 0.1 [0.0‐0.1], P < .001). However, for DMFS‐SS prevalence (Figure 2D), the post‐cessation change was essentially identical in Calgary and Edmonton (coefficient [95% CI] for difference of changes: 0.0 [−0.0 to 0.0], P = .60).
For dental fluorosis (Figure 2E), the post‐cessation change in prevalence in Calgary (i.e. a decrease from 19.9% [17.8‐22.2]) in 2013/2014 to 8.3% [6.6‐10.3] in 2018/2019) differed significantly from the change in Edmonton (i.e. an increase from 14.1% [11.4‐17.4] in 2013/2014 to 19.4% [16.3‐22.9]) in 2018/2019) (coefficient [95% CI] for difference of changes: −0.1 [−0.2 to −0.1], P < .001).
3.3. Consideration of other data sources
As shown in Table 3, the proportion of children with treated tooth decay (complete or partial caries care) was significantly higher in Calgary (fluoridation cessation) than in Edmonton (still fluoridated), while the proportion with untreated tooth decay (no caries care) was higher in Edmonton. For example, the proportion with complete caries care was 35.4% (33.4‐37.5) in Calgary and 23.8% (21.8‐25.9) in Edmonton, while the proportion with no caries care was 10.8% (9.4‐12.4) in Calgary and 16.4% (15.0‐17.9) in Edmonton. The proportion of children with dental sealants did not differ between the 2 cities: 27.7% [25.1‐30.5] in Calgary compared with 26.4% [23.2‐29.7] in Edmonton.
TABLE 3.
Weighted estimates (percent) with 95% confidence intervals for treated and untreated components of deft/DMFT, and for presence of dental sealants, grade 2 students in Calgary and Edmonton in 2018/2019
| Variable | Calgary (F‐cess) | Edmonton (F‐cont) | |
|---|---|---|---|
| Treatment level category | No decay experience | 32.7 (30.3‐35.2)a | 41.9 (39.2‐44.7) |
| Complete caries care | 35.4 (33.4‐37.5)a | 23.8 (21.8‐25.9) | |
| Partial caries care | 21.0 (18.7‐23.5)a | 17.8 (15.9‐20.0) | |
| No caries care | 10.8 (9.4‐12.4)a | 16.4 (15.0‐17.9) | |
| Total | n = 2627 | n = 2569 | |
| Dental sealants | Presence of sealants | 27.7 (25.1‐30.5), n = 2627 | 26.4 (23.2‐29.7), n = 2569 |
No decay experience: no decay, no extractions, no fillings.
Complete caries care: no decay; one or more instance of extraction or filling.
Partial caries care: one or more instance of decay; one or more instance of extraction or filling.
No caries care: one or more instance of decay; no extractions or fillings.
Statistically significant difference (P < .05) between Calgary and Edmonton based on Pearson's chi‐squared statistic.
Analysis of 65 fingernail clipping samples (n = 31 in Edmonton, n = 34 in Calgary) in 2018/2019 showed statistically significant differences (P < .0001 based on a Mann‐Whitney test) between the 2 cities, with the Calgary sample (fluoridation cessation) having lower fluoride concentrations than the Edmonton sample (still fluoridated). The mean (95% CI) total fluoride estimate (µg/g) was 1.1 (0.9 to 1.2) in Calgary and 1.6 (1.3 to 1.8) in Edmonton. The median (inter‐quartile range) was 1.0 (0.7 to 1.2) µg/g in Calgary and 1.3 (1.3 to 1.5) µg/g in Edmonton.
4. DISCUSSION
We examined the effects of fluoridation cessation in Calgary, Canada (occurred in 2011) on dental caries experience, via a comparison of population‐based samples of Grade 2 schoolchildren in Calgary and in Edmonton where fluoridation remains in place. By collecting data in 2018/2019, we included a cohort of child residents who were born following cessation and would thus have lifelong exposure to fluoridation (Edmonton) or its absence (Calgary), including pre‐ and post‐eruptive effects.
For primary teeth, findings were consistent with an adverse effect of fluoridation cessation on dental caries experience. Prevalence of dental caries, including smooth surface caries, was higher in Calgary (fluoridation cessation) than in Edmonton (still fluoridated). This difference had widened since our previous survey in 2013/2014, it was robust to adjustment for potential confounders, and it persisted in the (considerably smaller) subset of respondents who reported being lifelong residents of Calgary or Edmonton and usually drinking tap water. The effects were corroborated by our observation that the prevalence of dental fluorosis was significantly higher in Edmonton (still fluoridated) than in Calgary (fluoridation cessation) (see more below), and by the fingernail clippings, which confirmed significantly lower total fluoride intake in Calgary (fluoridation cessation) than in Edmonton (still fluoridated).
Differences in dental caries experience between Calgary and Edmonton did not appear to be an artifact of differences in preventive dental care (i.e. dental sealant application) or dental treatment (based on treated versus untreated components of the deft and DMFT), which if anything was greater in Calgary. The reasons for higher levels of caries care in Calgary were not specifically examined. They could include differences in socioeconomic circumstances (which, as per the census information provided above, and the data presented in Table 2, tend to be higher on average in Calgary than in Edmonton), differences in parental behaviour (for example, if parents in Calgary take their child to the dentist more often because of the absence of fluoridation; as per Table 2, regular dental visits were more common in Calgary than in Edmonton), or differences in dental professional behaviour. Consistent with the latter explanation, we elsewhere observed that dental hygienists working in fluoridation cessation communities in Alberta, compared to those working in communities where fluoridation was still in place, were more likely to report certain practice adaptations in response to cessation. 41
For one of our primary dentition measures—namely, the average number of teeth with evidence of smooth surface caries among those with caries experience—estimates did not differ between Calgary and Edmonton samples. This observation is consistent with fluoridation as primary prevention, which would be expected to influence incidence (new cases) of disease.
Findings were less consistent for permanent teeth. Although mean and prevalence of DMFT were higher in Calgary (fluoridation cessation) than in Edmonton (still fluoridated) in the full sample and when adjusting for covariates, the difference was small and was reduced to statistical non‐significance when we considered the subset who reported being lifelong residents of Calgary or Edmonton and usually drinking tap water. Moreover, when examining smooth surface caries in the permanent dentition, there were no differences between Calgary and Edmonton, and this absence of effect was consistent across measures and models.
These findings likely reflect study design elements; namely, the age of the children and the amount of time that their permanent teeth have been exposed to the oral environment, which limited our ability to observe an equally strong effect of fluoridation in both primary and permanent teeth at the same point in time. 30 Consistent with what is known about the greater significance of the post‐eruptive effect for smooth surface caries, 42 it would be necessary to study children whose permanent teeth have been in the mouth long enough to show tooth decay, including fluoride‐related differences in tooth decay, at a level that is apparent in visual inspections. To adequately investigate the effect of fluoridation (including cessation) on dental caries in permanent teeth, it would be necessary to study children who are at least 9 years of age, and preferably 12 years of age. 33 , 42 , 43 Inclusion of older children, as well as other measures of disease such as experience of acute dental caries events or emergency service utilization, 44 are important recommendations for future research.
With respect to dental fluorosis, we observed that prevalence was significantly higher in Edmonton (still fluoridated) than in Calgary (fluoridation cessation). To further explore reasons for higher prevalence in Edmonton than in Calgary, we ran a post hoc cross‐tabulation of fluorosis status (yes/no) by fluoride exposure variables from the questionnaire (see Table 2). We found that, among children with dental fluorosis, the fluoride exposure variables were consistently higher (P < .05) in Edmonton (still fluoridated) than in Calgary (cessation).2 This suggests that the higher prevalence of dental fluorosis in Edmonton was not only due to fluoridated drinking water in that city and may have reflected other fluoride sources.
Although estimates of fluorosis were higher in Edmonton than in Calgary, it is important to note that nearly all cases (>99%) in both cities were mild, which is in line with national estimates. 15 We did not have information on parental satisfaction with dental appearance. However, if concerns about appearance were significant (e.g. in Edmonton, where fluorosis was higher), one might expect those concerns to be reflected in the question about parental satisfaction with the general health of their child's mouth (Table 2). This was not the case: parental reports of the general health of their child's mouth were very similar in Calgary and Edmonton (50.2% and 49.6%, respectively, rated their child's mouth health as excellent or very good).
Overall, these findings confirmed and strengthened those from our short‐term evaluation of fluoridation cessation in Calgary, especially concerning primary teeth. 20 , 21 Dental caries in the primary dentition can significantly affect children's health and well‐being, 44 , 45 , 46 and an association between decay incidence in primary teeth and permanent teeth is well established, 43 thus supporting the importance of preventing caries in the primary dentition.
Study limitations included, first, our inability to rule out all potential confounding variables due to a combination of the observational nature of the research, the timing of the surveys (the closest pre‐cessation data [2009/2010] was only available for Calgary), and idiosyncratic features of individual surveys such as the absence of a questionnaire (2004/2005, 2009/2010). By building a research project around existing pre‐cessation data sources (which were conducted as part of health region surveillance activities and not for research purposes) and Calgary's decision to cease fluoridation, we have made productive use of the best available data in our setting, to inform local policy deliberations. Second, our assessment of fluorosis did not specifically include the criterion of bilateral symmetry as a requirement for presence of fluorosis; this would, if anything, lead to a slight overestimate of fluorosis prevalence estimates. However, examiners were calibrated to the TSIF index and the various criteria used for determining fluorosis (as opposed to non‐fluoride opacities) including an understanding of how fluorosis appears related to the area affected, shape of lesions, demarcation, teeth affected (including the principle of bilateral symmetry) and colour. 47 Although our methods may slightly overestimate fluorosis prevalence, we do not expect that this would occur differentially in the 2 cities (thus unlikely to confound the comparisons). The water quality reports and results of the fingernail clipping analysis additionally corroborate differences in fluorosis estimates between the 2 settings. 48
In summary, we observed significant and consistent differences in dental caries experience in the primary dentition between Grade 2 children in Calgary (fluoridation cessation) and Edmonton (still fluoridated), Canada, 7‐8 years following cessation in Calgary. Our findings are consistent with an adverse impact of fluoridation cessation on children's dental health in Calgary, and point to the need for universally, publicly funded prevention activities including, but not limited to fluoridation. Our study makes a rigorous contribution to the relatively sparse and methodologically variable literature on fluoridation cessation. Key strengths included: (i) a strong study design with a comparison community and multiple data points; (ii) large, population‐representative samples of children; (iii) high‐quality data collected by trained and calibrated experts who demonstrated high levels of accuracy and consistency; and (iv) multiple sources of post‐cessation data (e.g. oral health examinations, questionnaire, fingernail clippings) to permit corroboration. A1
CONFLICT OF INTEREST
There are no conflicts of interest to declare.
Supporting information
TABLE S1
ACKNOWLEDGEMENTS
This study was funded by a research grant from the Canadian Institutes of Health Research (CIHR) (PJT‐156258). Dr Lindsay McLaren was supported by an Applied Public Health Chair research award funded by CIHR (Institute of Population & Public Health and Institute of Musculoskeletal Health & Arthritis), the Public Health Agency of Canada, and Alberta Innovates—Health Solutions (CIHR ID CPP‐137907). Dr Cynthia Weijs was supported by a CIHR Health System Impact Fellowship, 2017‐2020 (Award # 403867). We are grateful to Dr Marília Afonso Rabelo Buzalaf, Professor of Biochemistry and Cariology at the University of São Paulo, for performing the analysis of fluoride concentrations from fingernail samples. We also extend our sincere thanks to the dental hygienists and clerks who worked on the project, and to the participating school boards, schools, and families.
APPENDIX 1.
TABLE A1.
Fluoride content of municipal drinking water for 2 major water treatment plants in Calgary and Edmonton, 2005‐2019 a . Range (mg/L) and average (if available)
| Year | Calgary (F‐cess)b | Edmonton (F‐cont) | ||
|---|---|---|---|---|
| Bearspaw plant | Glenmore plant | Rossdale plant | EL Smith plant | |
| 2005 | 0.6 to 0.8 | 0.7 to 0.8 | 0.7 to 1.0 (avg: 0.8) | 0.7 to 0.9 (avg: 0.8) |
| 2006 | 0.7 to 0.7 | 0.6 to 0.8 | 0.8 to 0.9 (avg: 0.8) | 0.7 to 0.9 (avg: 0.8) |
| 2007 | 0.6 to 0.7 | 0.7 to 0.7 | 0.5 to 0.9 (avg: 0.7) | 0.1 to 0.9 (avg: 0.8)c |
| 2008 | 0.7 to 0.7 | 0.6 to 0.7 | 0.1 to 0.9d (avg: 0.8) | 0.0 to 0.8c (avg: 0.4) |
| Overall average for both plants: 0.6 | ||||
| 2009 | 0.7 to 0.7 | 0.6 to 0.8 | 0.7 to 0.9 (avg: 0.8) | 0.7 to 0.8 (avg: 0.7) |
| 2010 | 0.7 to 0.7 | 0.6 to 0.9 | 0.6 to 0.8 (avg: 0.7) | 0.7 to 0.8 (avg: 0.7) |
| 2011 | 0.1 to 0.7e | 0.1 to 0.7e | 0.6 to 0.8 (avg: 0.7) | 0.1 to 0.8f (avg: 0.6) |
| 2012 | 0.1 to 0.1 | 0.2 to 0.3 | 0.0 to 0.8g (avg: 0.5) | 0.6 to 0.8 (avg: 0.7) |
| 2013 | 0.1 to 0.2 | 0.1 to 0.3 | 0.6 to 0.8 (avg: 0.7) | 0.6 to 0.8 (avg: 0.7) |
| 2014 | 0.1 to 0.3 (for both plants) | 0.6 to 0.9 (avg: 0.7) | 0.5 to 0.9 (avg: 0.7) | |
| 2015 | 0.1 to 0.1 (avg: 0.1) | 0.2 to 0.3 (avg: 0.3) | 0.6 to 0.8 (avg: 0.7) | 0.6 to 0.8 (avg: 0.7) |
| 2016 | 0.1 to 0.1 (avg: 0.1) | 0.2 to 0.3 (avg: 0.2) | 0.6 to 0.8 (avg: 0.7) | 0.6 to 0.8 (avg: 0.7) |
| 2017 | 0.1 to 0.2 (avg: 0.1) | <0.1 to 0.3 (avg: 0.2) | 0.6 to 0.8 (avg: 0.7) | 0.6 to 0.8 (avg: 0.7) |
| 2018 | 0.1 to 0.2 (avg: 0.1) | 0.2 to 0.3 (avg: 0.2) | 0.6 to 0.8 (avg: 0.7) | 0.5 to 0.8 (avg: 0.7) |
| 2019 | 0.1 to 0.3 (avg: 0.2) | 0.1 to 0.3 (avg: 0.2) | 0.6 to 0.8 (avg: 0.7) | <0.1 to 0.8 (avg: 0.5) |
The information provided is for treated water entering the distribution system, as recorded in water quality reports for Calgary and Edmonton. The information was not always available in the same format across the 15‐year time period.
Fluoride content of untreated water in Calgary 2005‐2013 range: 0.1 to 0.2 (Bearspaw), 0.2 to 0.3 (Glenmore).
Note: As of September 26, 2007 the fluoride lower limit was relaxed due to chemical supply shortages and construction at the EL Smith plant (approved by Alberta Environment). The shortage was relieved and construction was completed by July 2008 and fluoride levels returned to normal.
No note, but average for Rossdale for 2008 was 0.8 mg/L.
City of Calgary ceased fluoridation of its drinking water on May 19, 2011, as per approval amendment 476‐02‐01.
Note: Fluoride was not added to EL Smith WTP between September 8 and October 21 due to construction work on fluoride system.
Note: Fluoride was not added to Rossdale WTP between July 22 and November 29 due to construction work on fluoride system.
APPENDIX 2. Summary of findings from assessments of intra‐ and inter‐examiner reliability, conducted as part of the 2018/2019 survey only.
We had 2 assessment teams in each city; each team consisted of one registered dental hygienist who conducted the assessment and one clerk who assisted with the assessment and recorded the data directly into Epi InfoTM 49 software using a laptop. Evidence supports the use of dental hygienists as examiners in caries prevalence studies as achieving similar results to dentists. 50 Teams underwent training and calibration led by a public health dentist with expertise in population‐based oral health assessment and survey methods, including the criteria used in the various indices for this survey.
Initial training and calibration took place at the beginning of data collection (October 2018), and included a 1‐day didactic session and a 1‐day hands‐on session in a school. Then, in a process designed to permit continual quality assurance and improvement, calibration was revisited throughout the 9‐month data collection period (October 2018—June 2019); those periodic calibration sessions permitted us to gather data with which to estimate intra‐ and inter‐examiner reliability. Intra‐examiner reliability was assessed at 3 occasions (November/December 2018, February 2019, April/May 2019) during the 9‐month data collection period in each city, and inter‐examiner reliability was assessed at 2 occasions (December 2018 and March 2019) when all 4 teams convened in one city. We estimated intra‐ and inter‐rater reliability based on data collected at these sessions using the kappa statistic, using interpretations described by McHugh. 51
Intra‐rater reliability estimates were based on repeat assessments (2 assessments per examiner) of a total of 106 randomly selected children, over 3 occasions. For presence of cavitation (d2‐3), based on a total of 14 840 observations (140 tooth surfaces × 106 children), intra‐rater reliability was ‘strong’ or better (kappa ≥ 0.80) 100% of the time. For fluorosis, based on a total of 106 observations (single assessment per child × 106 children), intra‐rater reliability was ‘strong’ (kappa = 0.87).
Inter‐rater reliability estimates were based on assessments of a total of 18 randomly selected children by all 4 examiners, over 2 occasions. For presence of cavitation (d2‐3), based on a total of 2520 observations (140 tooth surfaces × 18 children), inter‐rater reliability was ‘strong’ or better (kappa ≥ 0.8) 82.7% of the time. For fluorosis, based on a total of 18 observations (single assessment per child × 18 children), inter‐rater reliability was ‘moderate’ (kappa = 0.77). When considering Calgary and Edmonton teams separately (i.e. the 2 Calgary teams together, against the 2 Edmonton teams together), the patterns of agreement were broadly similar in the 2 cities: specifically, for presence of cavitation, inter‐rater reliability was ‘strong’ or better (kappa ≥ 0.8) 85.7% of the time in Calgary, and 86.4% of the time in Edmonton.
APPENDIX 3. Details of analysis of fingernail clippings (small random sub‐sample in each city) in 2018/2019, as provided by the lead scientist.
Each nail clipping was cleaned with deionized water using an interdental brush, sonicated in deionized water for 10 minutes, dried at 60°C and weighed. The fluoride concentrations of the nail clippings were determined after overnight, hexamethyldisiloxane‐ facilitated diffusion 52 as modified by Whitford, 53 using the ion‐specific electrode (Orion Research, Cambridge, MA, USA, model 9409) and a miniature calomel reference electrode (Fisher Scientific accumet, No. 13‐620‐79), both coupled to a potentiometer (Orion Research, Cambridge, MA, USA, model EA 940). During the diffusion process, the solutions in the non‐wettable Petri dishes (Falcon, No. 1007) were gently swirled on a rotatory shaker. Fluoride standards (0.0095, 0.019, 0.095, 0.190 and 0.950 μg) were prepared by serial dilution of a stock‐standard containing 0.1 M fluoride (Orion 940906) in triplicate and diffused in the same manner as the samples. In addition, nondiffused fluoride standards were prepared with the same solutions (0.05 M NaOH, 0.20 M acetic acid, plus NaF) that were used to prepare the diffused standards and samples. The nondiffused standards were made up to have exactly the same fluoride concentrations as the diffused standards. Comparison of the millivolt readings demonstrated that the fluoride in the diffused standards had been completely trapped and analyzed. The millivoltage potentials were converted to fluoride concentrations using a standard curve with a coefficient correlation of r = .9993. Samples weighing ≥10 mg (80% of the samples) were analyzed in duplicate. The mean repeatability of the readings, based on the duplicate samples, was 98%.
McLaren L, Patterson SK, Faris P, et al. Fluoridation cessation and children’s dental caries: A 7‐year follow‐up evaluation of Grade 2 schoolchildren in Calgary and Edmonton, Canada. Community Dent Oral Epidemiol. 2022;50:391–403. 10.1111/cdoe.12685
Footnotes
The term “dental caries experience” includes currently decayed and unrestored teeth/surfaces, restored teeth/surfaces, and teeth missing due to caries to distinguish it from other terms (e.g. tooth decay; caries) that may only include current, unrestored decay.
In particular, the percent [95% CI] who responded “yes” (vs. “no” or “don't know”) for Calgary and Edmonton, respectively, was: 4.9% [1.5‐14.5] and 22.1% [14.5‐32.2] for fluoride supplements at home; 7.1% [5.3‐9.4] and 18.3% [14.8‐22.3] for fluoride treatment at dentist office; 9.4% [5.6‐15.3] and 25% [17.7‐34.1] for fluoride treatment in school program; 8% [6.2‐10.3] and 18.4% [15.2‐22.0] for use of fluoride toothpaste; and 8.3% [5.5‐12.4] and 21.1% [15.9‐27.3] for use of fluoride mouthwash.
REFERENCES
- 1. Burt BA, Eklund SA Dentistry, Dental Practice, and the Community, 5th edn. Philadelphia, PA: W.B. Saunders; 1999. [Google Scholar]
- 2. Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427‐432. [DOI] [PubMed] [Google Scholar]
- 3. Ast DB, Finn SB, McCaffrey I. The Newburgh‐Kingston caries fluorine study: Dental findings after three years of water fluoridation. Am J Public Health Nations Health. 1950;40(6):716‐724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brown HK, McLaren HR, Josie GH, Stewart BJ. The Brantford‐Sarnia‐Stratford fluoridation caries study 1955 report. Can J Public Health. 1956;47:149‐159. [PubMed] [Google Scholar]
- 5. Iheozor‐Ejiofor Z, Worthington HV, Walsh T, et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2015;6:CD010856. 10.1002/14651858.CD010856.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rugg‐Gunn AJ, Spencer AJ, Whelton HP, et al. Critique of the review of ‘Water fluoridation for the prevention of dental caries’ published by the Cochrane Collaboration in 2015. Br J Dent. 2016;220(7):335‐340. [DOI] [PubMed] [Google Scholar]
- 7. Canadian Agency for Drugs and Technologies in Health (CADTH) . Community Water Fluoridation Programs: A Health Technology Assessment—Review of Dental Caries and Other Health Outcomes. Ottawa: CADTH; 2019. https://www.cadth.ca/community‐water‐fluoridation‐programs‐health‐technology‐assessment [Google Scholar]
- 8. Featherstone JDB. Prevention and reversal of dental caries: Role of low level fluoride. Community Dent Oral Epidemiol. 1999;27:31‐40. [DOI] [PubMed] [Google Scholar]
- 9. Groeneveld A, Van Eck AA, Backer DO. Fluoride in caries prevention: Is the effect pre‐ or post‐eruptive? J Dent Res. 1990;69:751‐755. [DOI] [PubMed] [Google Scholar]
- 10. Public Health Agency of Canada (PHAC) . The State of Community Water Fluoridation across Canada, 2017 Report. Prepared by the Public Health Capacity and Knowledge Management Unit, Quebec Region for the Office of the Chief Dental Officer of Canada. PHAC. https://www.canada.ca/en/services/health/publications/healthy‐living/community‐water‐fluoridation‐across‐canada‐2017.html [Google Scholar]
- 11. O’Neill B, Kapoor T, McLaren L. Politics, science, and termination: A case study of water fluoridation policy in Calgary in 2011. Rev Policy Res. 2018;36(1):99‐120. [Google Scholar]
- 12. McLaren L, Singhal S. Does cessation of community water fluoridation lead to an increase in tooth decay? A systematic review. J Epidemiol Community Health. 2016;70:934‐940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Meyer J, Margaritis V, Mendelsohn A. Consequences of community water fluoridation cessation for medicaid‐eligible children and adolescents in Juneau, Alaska. BMC Oral Health. 2018;215. 10.1186/s12903-018-0684-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Canadian Academy of Health Sciences (CAHS) . Improving Access to Oral Health Care for Vulnerable People Living in Canada. Ottawa: CAHS; 2014. https://cahs‐acss.ca/wp‐content/uploads/2015/07/Access_to_Oral_Care_FINAL_REPORT_EN.pdf [Google Scholar]
- 15. Health Canada . Report on the Findings of the Oral Health Component of the Canadian Health Measures Survey, 2007‐2009. Ottawa, ON: Minister of Health; 2010. [Google Scholar]
- 16. Quiñonez C. Dentistry in Alberta: Time for a Checkup?. Edmonton, AB: Parkland Institute; 2020. https://www.parklandinstitute.ca/dentistry_in_alberta_media [Google Scholar]
- 17. Flanagan G. From gap to chasm: Alberta’s increasing income inequality. Edmonton, AB: Parkland Institute; 2015. https://www.parklandinstitute.ca/from_gap_to_chasm [Google Scholar]
- 18. Shi C, Faris P, McNeil DA, et al. Ethnic disparities in children’s oral health: Findings from a population‐based survey of grade 1 and 2 schoolchildren in Alberta, Canada. BMC Oral Health. 2018;18:1. 10.1186/s12903-017-0444-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shi C, Aparicio‐Ting F, Faris P, Patterson S, McLaren L. Small area contextual effects on children’s dental caries in Alberta: A multilevel analysis. Can J Public Health. 2021;112:773‐781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McLaren L, Patterson S, Thawer S, et al. Measuring the short‐ term impact of fluoridation cessation on dental caries in grade 2 children using tooth surface indices. Community Dent Oral Epidemiol. 2016;44(3):274‐282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McLaren L, Patterson S, Thawer S, et al. Exploring the short‐ term impact of community water fluoridation cessation on children’s dental caries: A natural experiment in Alberta. Canada. Public Health (Elsevier). 2017;146:56‐64. [DOI] [PubMed] [Google Scholar]
- 22. Edelstein BL. The dental caries pandemic and disparities problem. BMC Oral Health. 2006;6(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McLaren L, McNeil D, Potestio M, et al. Equity in children’s dental caries before and after cessation of community water fluoridation: differential impact by dental insurance status and geographic material deprivation. Int J Equity Health. 2016;15:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Singhal S, Farmer J, McLaren L. Methodological considerations for designing a community water fluoridation cessation study. Community Dent Oral Epidemiol. 2017;45(3):193‐200. [DOI] [PubMed] [Google Scholar]
- 25. Cho H‐J, Jin B‐H, Park D‐Y, et al. Systemic effect of water fluoridation on dental caries prevalence. Community Dent Oral Epidemiol. 2014;42(4):341‐348. [DOI] [PubMed] [Google Scholar]
- 26. Singh KAA, Spencer J, Armfield JM. Relative effects of pre‐and posteruption water fluoride on caries experience of permanent first molars. J Public Health Dent. 2003;63(1):11‐19. [DOI] [PubMed] [Google Scholar]
- 27. Statistics Canada . Focus on Geography Series, 2016 Census. https://www12.statcan.gc.ca/census‐recensement/2016/as‐sa/fogs‐spg/select‐Geo‐Choix.cfm?Lang=Eng&GK=CSD&TOPIC=1
- 28. Statistics Canada . Census Profile, 2016 Census. https://www12.statcan.gc.ca/census‐recensement/2016/dp‐pd/prof/search‐recherche/lst/results‐resultats.cfm?Lang=E&TABID=1&G=1&Geo1=&Code1=&Geo2=&Code2=&GEOCODE=48&type=0
- 29. Government of Alberta . Student Population Statistics. https://www.alberta.ca/student‐population‐statistics.aspx
- 30. Kuthy RA, Ashton JJ. Eruption pattern of permanent molars: Implications for school‐based dental sealant programs. J Public Health Dent. 1989;49(1):7‐14. [DOI] [PubMed] [Google Scholar]
- 31. Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: John Wiley & Sons; 1987. [Google Scholar]
- 32. Centers for Disease Control and Prevention . Division of Oral Health. Oral Health Data Tools. Atlanta, Georgia: CDC. https://www.cdc.gov/oralhealth/data‐tools/index.htm [Google Scholar]
- 33. Statistics Canada . Canadian Health Measures Survey, Cycle 1. Ottawa: Statistics Canada. https://www23.statcan.gc.ca/imdb‐bmdi/document/5071_D2_T1_V1‐eng.htm [Google Scholar]
- 34. Warren JJ, Levy SA, Kanellis MJ. Dental caries in the primary dentition: Assessing prevalence of cavitated and noncavitated lesions. J Public Health Dent. 2002;62(2):109‐141. [DOI] [PubMed] [Google Scholar]
- 35. World Health Organization (WHO) . Oral Health Surveys: Basic Methods, 5th edn. Geneva: World Health Organization; 2013. [Google Scholar]
- 36. Rozier RG. Epidemiologic indices for measuring the clinical manifestations of dental fluorosis: overview and critique. Adv Dent Res. 1994;8(1):39‐55. [DOI] [PubMed] [Google Scholar]
- 37. Pessan JP, Buzalaf MAR. Historical and recent biological markers of exposure to fluoride. Monogr Oral Sci. 2011;22:52‐65. [DOI] [PubMed] [Google Scholar]
- 38. Whitford GM, Sampaio FC, Arneberg P, von der Fehr FR. Fingernail fluoride: A method for monitoring fluoride exposure. Caries Res. 1999;33:462‐467. [DOI] [PubMed] [Google Scholar]
- 39. StataCorp . Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 40. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: The difference‐in‐differences approach. JAMA. 2014;312(22):2401‐2402. [DOI] [PubMed] [Google Scholar]
- 41. Thawer S, Shi C, Weijs C, McLaren L. Exploring reported dental hygiene practice adaptations in response to water fluoridation status. Can J Dent Hyg. 2018;52(2):110‐121. [Google Scholar]
- 42. Groenveld A. Longitudinal study of prevalence of enamel lesions in a fluoridated and non‐fluoridated area. Comm Dent Oral Epid. 1985;13(3):159‐163. [DOI] [PubMed] [Google Scholar]
- 43. Lynch RJM. The primary and mixed dentition, post‐eruptive enamel maturation and dental caries: A review. Int J Dent J. 2013;63:3‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Canadian Institute for Health Information (CIHI) . Treatment of Preventable Dental Cavities in Preschoolers: A Focus on Day Surgery Under General Anesthesia. Ottawa: CIHI; 2013. https://publications.gc.ca/site/eng/9.698831/publication.html?wbdisable=true [Google Scholar]
- 45. Alberta Health Services (AHS) . Oral Health Action Plan. AHS Provincial Oral Health Office, Healthy Public Policy Unit. 2016. https://www.albertahealthservices.ca/assets/info/oh/if‐oh‐action‐plan.pdf [Google Scholar]
- 46. Rowan‐Legg A. Oral Care for Children—A Call for Action. Canadian Paediatric Society. 2018. https://www.cps.ca/en/documents/position/oral‐health‐care‐for‐children [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Horowitz HS. Indexes for measuring dental fluorosis. J Public Health Dent. 1986;46(4):179‐183. [DOI] [PubMed] [Google Scholar]
- 48. Revelo‐Mejía IA, Hardisson A, Rubio C, Gutiérrez AJ, Paz S. Dental fluorosis: the risk of misdiagnosis—A review. Biol Trace Elem Res. 2021;199(5):1762‐1770. [DOI] [PubMed] [Google Scholar]
- 49. Centers for Disease Control and Prevention . Epi Info™ (Public Domain Software). https://www.cdc.gov/epiinfo/index.html
- 50. Mauriello SM, Bader JD, Disney JA, Graves RC. Examiner agreement between hygienists and dentists for caries prevalence examinations. J Pub Health Dent. 1990;50(1):32‐37. [DOI] [PubMed] [Google Scholar]
- 51. McHugh ML. Interrater reliability: The kappa statistic. Biochem Med (Zagreb). 2012;22(3):276‐282. [PMC free article] [PubMed] [Google Scholar]
- 52. Taves DR. Separation of fluoride by rapid diffusion using hexamethyldisiloxane. Talenta. 1968;15(9):969‐974. [DOI] [PubMed] [Google Scholar]
- 53. Whitford GM. The Metabolism and Toxicity of Fluoride. Monographs in Oral Science, 2nd edn. Basel: Karger; 1996. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TABLE S1


