ABSTRACT
Cigarette smoking is associated with epigenetic changes that may be reversible following smoking cessation. Whole blood DNA methylation was evaluated in Framingham Heart Study Offspring (n = 169) and Third Generation (n = 30) cohort participants at two study visits 6 years apart and in Atherosclerosis Risk in Communities (ARIC) study (n = 222) participants at two study visits 20 years apart. Changes in DNA methylation (delta β values) at 483,565 cytosine-phosphate-guanine (CpG) sites and differentially methylated regions (DMRs) were compared between participants who were current, former, or never smokers at both visits (current-current, former-former, never-never, respectively), versus those who quit in the interim (current-former). Interim quitters had more hypermethylation at four CpGs annotated to AHRR, one CpG annotated to F2RL3, and one intergenic CpG (cg21566642) compared with current-current smokers (FDR < 0.02 for all), and two significant DMRs were identified. While there were no significant differentially methylated CpGs in the comparison of interim quitters and former-former smokers, 106 DMRs overlapping with small nucleolar RNA were identified. As compared with all non-smokers, current-current smokers additionally had more hypermethylation at two CpG sites annotated to HIVEP3 and TMEM126A, respectively, and another intergenic CpG (cg14339116). Gene transcripts associated with smoking cessation were implicated in immune responses, cell homoeostasis, and apoptosis. Smoking cessation is associated with early reversion of blood DNA methylation changes at CpG sites annotated to AHRR and F2RL3 towards those of never smokers. Associated gene expression suggests a role of longitudinal smoking-related DNA methylation changes in immune response processes.
KEYWORDS: Cigarette smoking, DNA methylation, epigenetics, longitudinal analysis
Introduction
Although the global prevalence of cigarette smoking has decreased in the last 20 years, tobacco use remains a leading preventable cause of death worldwide [1–3]. Tobacco use is associated with the development of multiple cancers [4] and chronic diseases, including cardiovascular disease, chronic obstructive pulmonary disease, and pneumonia [5]. Cytosine-phosphate-guanine (CpG) DNA methylation sites reflect reversible epigenetic changes that influence gene expression and a potential mechanism by which tobacco use may lead to adverse health outcomes. DNA methylation at specific CpG sites has been implicated in numerous disease processes, including cancer [6,7], diabetes mellitus [8], osteoporosis [9], and cardiovascular disease [10,11]. In some disease processes, it has been identified as a biomarker of disease and a promising target of prevention and treatment efforts [10,12–14].
Cigarette smoking is associated with altered blood and other tissue DNA methylation patterns [15,16], potentially placing current and former smokers at high risk for smoking-associated disease. Prior studies of current, former, and never smokers have suggested that DNA methylation may revert towards levels observed in never smokers, although differential methylation of some CpG sites persists 30 years after smoking cessation [16–18]. In this study, we used longitudinal data to compare changes in DNA methylation patterns of adults who quit smoking during the study period compared with those who continued to smoke and those who had quit smoking prior to the study period. We hypothesized that smoking cessation would promote reversion of smoking-related methylation of key CpGs towards those of never smokers.
Materials and methods
Study sample
These analyses used data from the Framingham Heart Study (FHS) Offspring (n = 169) and Third Generation (n = 30) cohorts, as well as from the Atherosclerosis Risk in Communities (ARIC) study cohort (n = 222). The FHS samples included participants of European ancestry. FHS Offspring cohort participants attended the eighth (2005–2008; baseline visit) and ninth (2011–2014; follow-up visit) examination cycles. FHS Third Generation cohort participants attended the first (2005–2008; baseline visit) and the second (2008–2010; follow-up visit) examination cycles. The ARIC sample consisted of participants with African ancestry who attended visit 2 (1990–1992; baseline visit) and visit 5 (2011–2013; follow-up visit) clinical examinations.
Protocols for participant examinations and collection of genetic materials were approved by the institutional review boards for each study cohort. All participants provided written informed consent.
Smoking status
Cigarette smoking status at the baseline and follow-up visits was obtained from all participants via questionnaire. Current smokers were those who reported smoking on average at least one cigarette per day during the 12 months prior to collection of the blood sample. Former smokers were those who reported ever smoking at least one cigarette per day but had not smoked within 12 months prior to collection of the blood sample. Never smokers were those who reported never having smoked.
Change in smoking status from the baseline to follow-up visit was categorized based on the above definitions. Current-current smokers were those who were current smokers at both the baseline and follow-up visits. Former-former smokers were those who quit smoking prior to both the baseline and follow-up visits. Never-never smokers were those who had never smoked at both the baseline and follow-up visits. Interim quitters were those participants who were current smokers at the baseline visit and former smokers at the follow-up visit.
Participants who were never smokers at baseline and current smokers at follow-up were not included in the study sample. A group of all non-smoker categories at follow-up included interim quitters, former-former smokers, and never-never smokers.
Sample collection
Fasting whole blood samples were collected at the baseline and follow-up visits for all study participants. Follow-up visits took place 6.4 ± 0.7 years after baseline in the FHS cohort and 20.9 ± 0.9 years after baseline in the ARIC cohort. Additional paired samples were assayed from a random sample of 25 FHS participants for quality control (QC), resulting in a total number of 448 FHS biospecimens (199 pairs plus 25 pairs), and 444 ARIC biospecimens (222 pairs) that were assayed for DNA methylation.
DNA methylation measurement and normalization
Whole blood DNA samples were assayed using the Infinium HumanMethylation450 (Illumina Inc., San Diego, CA). Autosomal and allosomal methylation results were normalized using the beta-mixture quantile (BMIQ) method [19] to correct for probe biases and Noob [20] for background correction and dye-bias equalization, yielding the proportion of methylation per CpG locus (β). DNA methylation values were normalized [21] and the COMBat method [22] was used to correct for batch effects.
Outlier detection
Because each participant provided paired samples, the removal of an outlier sample resulted in the removal of its pair as well. A principal component analysis (PCA) plot identified one outlier sample that was removed along with its pair; this outlier was from the QC set of samples and thus did not result in a reduced number of participants included in this study. All remaining QC paired samples (n = 24) showed a high correlation with the non-QC paired samples from the same participants (ρ > 0.95).
The remaining samples were then evaluated for potential mismatch between pairs using existing genetic data from a previous study [23]. A panel of 345 single nucleotide polymorphisms (SNPs) that are mutually independent and common (linkage disequilibrium r2 < 0.2, mean allele frequency ≥ 0.4) was selected. Predicted genotypes were derived for the study samples using linear regression on the CpG sites included in this study, and these were compared to the SNP panel. Five samples were identified as mismatches, defined as samples with residual standard deviations ≥ 3.0. These samples and their paired samples were removed but were part of the QC set of samples and did not reduce the total number of included participants.
After the removal of outlier samples and their matched pairs, a total of 880 samples (19 QC, 199 FHS non-QC, 222 ARIC non-QC sample pairs) remained.
Study cohort-specific statistical methods
Baseline and follow-up β values were residualized after accounting for age, sex, imputed blood count fraction [24] (CD4 + T-cells, CD8 + T-cells, NK cells, and monocytes), and assay-specific technical covariates using linear regression. The technical covariates used in FHS included batch, row, and column effects, while in ARIC, the technical covariates also included 4 PCs derived from ExomeChip data reflecting ancestry. Furthermore, because the FHS Offspring and Third Generation cohorts included family members, the FHS cohort-specific analyses were further adjusted for pedigree structure using the R package pedigreemm [25]. The familial structure was modelled as a variance-covariance matrix.
Delta β values were calculated for each CpG site to quantify the within-individual longitudinal change in DNA methylation by subtracting the baseline residualized β value from the follow-up residualized β value. Subsequent separate simple linear regression models were run for each CpG site in the FHS and ARIC cohorts to identify those which were differentially methylated (i.e., CpG sites with a significant difference in delta β value). To examine changes in DNA methylation associated with smoking cessation, we evaluated the difference in delta β values for each CpG site in interim quitters compared with current-current smokers. Furthermore, to evaluate the magnitude of change in DNA methylation after smoking cessation, we compared DNA methylation patterns between interim quitters and former-former smokers. Finally, to confirm previous cross-sectional associations of persistent smoking with altered DNA methylation [17], we compared delta β values for each CpG site between current-current smokers and all non-smoking groups (i.e., interim quitters, former-former smokers, and never-never smokers). Current-current smokers served as the reference group for the first comparison, former-former smokers served as the reference group for the second comparison, and the non-smoking group served as the reference group for the third comparison.
Meta-analysis
Fixed effects meta-analysis was used to combine the results of the FHS and ARIC simple linear regression models to identify differential methylation at 483,565 overlapping CpG sites based on weighted average delta β values. The false discovery rate (FDR) was calculated at each CpG site, and the genomic inflation factor λ was calculated for each comparison. If the λ value was greater than 1.3, a median-based correction [26] was applied to the P value and used to subsequently calculate the FDR.
Regional analysis
We compared the change in differentially methylated regions (DMRs) in interim quitters versus current-current smokers, interim quitters versus former-former smokers, and current-current smokers versus all non-smoking groups. Briefly, DMR analysis identifies significant regions with differential methylation by aggregating significant CpG sites within a specified bandwidth of one another, and DMRs may be significant even in the absence of a genome-wide significant differentially methylated CpG site [27]. DMR analysis was conducted using the R package DMRcate [27]. Meta-analyzed differences in delta β values were used as the input dataset, and default parameters (bandwidth λ = 1000, scaling factor C = 2) were specified [27].
Directional consistency across cohorts
Due to cohort differences in ethnicity and follow-up time, we examined the directional consistency of each meta-analyzed differential delta β value that was nominally significant at P < 0.05 in both the FHS and ARIC cohorts.
Implications of differential DNA methylation: FHS cohorts
Cross-sectional gene expression data were collected on FHS Offspring and Third Generation cohort participants at the ninth and second examination cycles, respectively, as previously described [23]. Briefly, RNA was isolated from whole blood samples. Complementary DNA strands were produced and amplified via quantitative polymerase chain reaction (qPCR). Affymetrix Human Exon 1.0 ST microarrays (Affymetrix, Santa Clara, CA, USA) were used to identify gene transcripts.
Significant CpG sites by smoking group were subsequently used in expression quantitative trait methylation (eQTM) analysis to evaluate the associations of changes in DNA methylation with gene expression at the FHS follow-up visits. We identified significant associations between CpG sites and gene transcripts. Cis CpG-transcript pairs were defined as those where the CpG site was within 500 kb of the transcript, and trans CpG-transcript pairs were defined as those where the CpG site was > 500 kb from the transcript or on different chromosome. Transcripts identified in eQTM analysis were further evaluated in gene set enrichment analysis (GSEA) [28,29] to understand putative pathways affected by smoking-associated changes in DNA methylation.
All analyses were conducted in R version 4.0.2, and statistical significance was assessed at FDR < 0.05.
Results
Sample characteristics
Characteristics of the sample by smoking status are presented in Table 1, and by study cohort in Supplemental Table 1. The study cohort consisted of 112 current-current smokers, 147 interim quitters, 115 former-former smokers, and 65 never-never smokers (Figure 1). Among the 199 FHS study participants, 75 Offspring participants were current-current smokers, 44 Offspring and 30 Third Generation participants were interim quitters, and 50 Offspring participants were former-former smokers. Among the 222 ARIC study participants, 37 were current-current smokers, 73 were interim quitters, 65 were former-former smokers, and 47 were never-never smokers.
Table 1.
Participant demographic and blood count characteristics by longitudinal smoking status.
| Current-current smokers (n = 112) | Interim quitters (n = 147) | Former-former smokers (n = 115) | Never smokers (n = 47) | |
|---|---|---|---|---|
| Age at baseline, years | 57.9 ± 7.7 | 52.6 ± 10.2 | 57.7 ± 7.0 | 55.0 ± 5.5 |
| Age at follow-up, years | 68.8 ± 7.7 | 65.9 ± 13.0 | 71.9 ± 6.2 | 76.0 ± 5.6 |
| Female, % | 58% | 37% | 45% | 47% |
| Cell count, baseline | ||||
| CD8T cell fraction | 0.12 ± 0.05 | 0.11 ± 0.05 | 0.13 ± 0.05 | 0.12 ± 0.04 |
| CD4T cells | 0.19 ± 0.07 | 0.19 ± 0.06 | 0.19 ± 0.06 | 0.18 ± 0.06 |
| NK cells | 0.03 ± 0.04 | 0.05 ± 0.05 | 0.05 ± 0.05 | 0.11 ± 0.05 |
| B cells | 0.07 ± 0.03 | 0.06 ± 0.03 | 0.07 ± 0.03 | 0.08 ± 0.04 |
| Monocytes | 0.09 ± 0.02 | 0.09 ± 0.03 | 0.09 ± 0.03 | 0.09 ± 0.03 |
| Granulocytes | 0.50 ± 0.11 | 0.51 ± 0.12 | 0.47 ± 0.12 | 0.43 ± 0.12 |
| Cell count, follow-up | ||||
| CD8T cell fraction | 0.11 ± 0.04 | 0.11 ± 0.05 | 0.11 ± 0.06 | 0.10 ± 0.04 |
| CD4T cells | 0.19 ± 0.07 | 0.18 ± 0.07 | 0.17 ± 0.07 | 0.16 ± 0.07 |
| NK cells | 0.03 ± 0.04 | 0.07 ± 0.07 | 0.09 ± 0.07 | 0.13 ± 0.06 |
| B cells | 0.06 ± 0.02 | 0.06 ± 0.03 | 0.06 ± 0.05 | 0.06 ± 0.04 |
| Monocytes | 0.10 ± 0.02 | 0.10 ± 0.03 | 0.11 ± 0.03 | 0.11 ± 0.03 |
| Granulocytes | 0.52 ± 0.09 | 0.48 ± 0.11 | 0.48 ± 0.13 | 0.45 ± 0.13 |
Abbreviations: NK, natural killer
Figure 1.
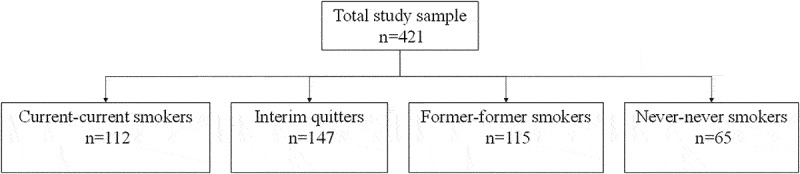
Study sample smoking status categories.
Genomic inflation λ
Genomic inflation λ values prior to and after applying corrections are presented in Supplemental Table 2. The FHS analysis of the interim quitters vs. former-former smokers revealed inflation (λ = 1.46) and was the only comparison for which the inflation correction was applied. All remaining comparisons for both the FHS and ARIC cohorts had λ values less than 1.3 and were not corrected.
Interim quitters vs. current-current smokers
Delta β values for six CpG sites differed significantly between interim quitters and current smokers (Table 2). Differential methylation at four of the six sites was annotated to the AHRR (aryl hydrocarbon receptor repressor) gene, and differential methylation at one of the remaining sites was annotated to the F2RL3 (coagulation factor II receptor-like 3) gene. At all six significant CpG sites, interim quitters had larger delta β values than current-current smokers, and the direction of the difference in delta β values was consistent within both the FHS and ARIC cohorts.
Table 2.
Differences in delta β values for CpG sites differing between interim quitters (n = 147) and current-current smokers (n = 112) at FDR < 0.05.
| CpG site | Location (hg19) | Gene symbol | Difference in delta β± SE | FDR | Cohort-specific delta β direction (FHS, ARIC)* |
|---|---|---|---|---|---|
| cg05575921 | chr5:373378 | AHRR | 0.0414 ± 0.0044 | 4.69E-15 | ++ |
| cg23576855 | chr5:373299 | AHRR | 0.0332 ± 0.0052 | 3.08E-05 | ++ |
| cg14817490 | chr5:392920 | AHRR | 0.0208 ± 0.0038 | 0.007 | ++ |
| cg26703534 | chr5:377358 | AHRR | 0.0187 ± 0.0035 | 0.007 | ++ |
| cg21566642 | chr2:233284661 | – | 0.0205 ± 0.0039 | 0.010 | ++ |
| cg03636183 | chr19:17000585 | F2RL3 | 0.0195 ± 0.0037 | 0.014 | ++ |
* + indicates a positive cohort-specific delta β value, – indicates a negative cohort-specific delta β value.
Abbreviations: CpG, cytosine-phosphate-guanine; SE, standard error; FDR, false discovery rate; FHS, Framingham Heart Study; ARIC, Atherosclerosis Risk in the Community; AHRR, aryl hydrocarbon receptor repressor; F2RL3, coagulation factor II receptor-like 3
Delta β values for the 23,497 CpG sites at a nominal P value < 0.05 are presented in Supplemental Table 3. Of these nominally significant delta β values, directionality was consistent between the two study cohorts among 84% (19,854 sites).
Two DMRs were identified between interim quitters and current-current smokers: chr5: 373,299–373,378 and chr7: 27,184,125–27,184,316 (Supplemental Table 4). These DMRs overlapped with the AHRR gene and with genes for RNA (HOXA-AS3, SNORA15, HOXA3, RP1-170O19.22).
Interim quitters vs. former-former smokers
While there were no genome-wide significant differences in delta β values between interim quitters and former-former smokers (Supplemental Table 5), 106 DMRs were identified between interim quitters and former-former smokers (Supplemental Table 6). More than half of these DMRs (n = 56) overlapped with expression of small nucleolar RNAs. Of the 9,873 nominally significant delta β values (i.e., P< 0.05), directionality was consistent among 86% (8,507 sites) between the two cohorts.
Current-current smokers vs. all non-smoker categories
Delta β values at nine CpG sites differed significantly between current-current smokers and all non-smoking groups (i.e., interim quitters, former-former smokers, and never-never smokers combined; Table 3). Besides the six CpG sites identified in the analysis of interim quitters versus current-current smokers, there was greater hypermethylation of CpG sites annotated to HIVEP3 (human immunodeficiency virus type I enhancer-binding protein 3), TMEM126A (transmembrane protein 126A), and an intergenic CpG site cg14339116. The direction of the difference in delta β values was consistent between the two cohorts across all nine CpG sites.
Table 3.
Differences in delta β values for CpG sites differing between current-current smokers (n = 112) and all non-smoking categories (n = 309) at FDR < 0.05.
| CpG site | Location (hg19) | Gene symbol | Difference in delta β± SE | FDR | Cohort-specific delta β direction (FHS, ARIC)* |
|---|---|---|---|---|---|
| cg05575921 | chr5:373378 | AHRR | −0.0407 ± 0.004 | 4.80E-18 | – |
| cg23576855 | chr5:373299 | AHRR | −0.0327 ± 0.0047 | 7.52E-07 | – |
| cg26703534 | chr5:377358 | AHRR | −0.0212 ± 0.0031 | 1.42E-06 | – |
| cg14817490 | chr5:392920 | AHRR | −0.0195 ± 0.0034 | 0.001 | – |
| cg03636183 | chr19:17000585 | F2RL3 | −0.0188 ± 0.0034 | 0.002 | – |
| cg21566642 | chr2:233284661 | – | −0.0187 ± 0.0035 | 0.006 | – |
| cg16145216 | chr1:42385662 | HIVEP3 | 0.0134 ± 0.0026 | 0.015 | ++ |
| cg24639862 | chr11:85359006 | TMEM126A | 0.0009 ± 0.0002 | 0.030 | ++ |
| cg14339116 | chr9:77062053 | – | 0.0059 ± 0.0012 | 0.044 | ++ |
* + indicates a positive cohort-specific delta β value, – indicates a negative cohort-specific delta β value.
Abbreviations: CpG, cytosine-phosphate-guanine; SE, standard error; FDR, false discovery rate; FHS, Framingham Heart Study; ARIC, Atherosclerosis Risk in the Community; AHRR, aryl hydrocarbon receptor repressor; F2RL3, coagulation factor II receptor-like 3; HIVEP3, human immunodeficiency virus type I enhancer-binding protein 3; TMEM126A, transmembrane protein 126A
Delta β values for the 24,934 CpG sites that had a nominal P value <0.05 are presented in Supplemental Table 7. Of these, directionality of the delta β values was consistent among 86% (22,783 sites).
Three DMRs were identified between current-current smokers and all non-smoking groups: chr2: 233,284,402–233,284,934, chr5: 373,299–373,887, and chr7: 27,184,159–27,184,375 (Supplemental Table 8). The most significant region (chr5) overlapped with the AHRR gene. The remaining regions on chromosomes 2 and 7 overlapped with RNA genes (AC068134.5, HOXA-AS3, HOXA3, RP1-170O19.22).
eQTM and GSEA
The six CpG sites that were differentially methylated in interim quitters as compared with current-current smokers were significantly associated with expression of 519 unique transcripts in eQTM analysis (Supplementary Table 9). Methylation of CpG sites annotated to AHRR and F2RL3 was associated with expression of leucine-rich repeat neuronal 3 (LRRN3), G protein-coupled receptor 15 (GPR15), and phosphotyrosine interaction domain containing 1 (PID1). GSEA for the 519 gene transcripts showed enrichment of pathways involved in regulation of the immune and inflammatory responses (Supplementary Table 10).
The nine CpG sites that were differentially methylated in current-current smokers as compared with all non-smokers at follow-up were significantly associated with expression of 606 unique transcripts (Supplementary Table 11). Among these, methylation of the CpG site annotated to HIVEP3 was also associated with expression of SAM and SH3 domain containing 1 (SASH1). Methylation of the CpG site annotated to TMEM126A was associated with expression of transmembrane protein 45 b (TMEM45B) and Ras converting enzyme 1 (RCE1). GSEA for the 606 gene transcripts showed enrichment of pathways involved in immune and inflammatory responses, cell metabolism, and apoptosis (Supplementary Table 12).
Discussion
Using smoking status and DNA methylation assessed at two time points, we identified multiple CpG sites that displayed changes in methylation following smoking cessation. This study was carefully designed to capitalize on existing biological specimens and it included analyses of longitudinal changes in DNA methylation and associated gene expression. We found that DNA methylation changes at CpG sites annotated to AHRR and F2RL3 were consistently hypermethylated towards non-smoking levels following smoking cessation. Differences in methylation changes at CpG sites annotated to two additional genes, HIVEP3 and TMEM126A, were also observed between current-current smokers compared to all non-smokers. We did not observe any significant differences in the change in DNA methylation between interim quitters and former-former smokers, although heterogeneity in these groups may have led to the identification of more than 100 DMRs between these groups.
Cigarette smoking has been long known to play a role in multiple disease processes, including cardiovascular diseases, respiratory diseases, multiple cancers, and dementia [30–32]. Smoking is also associated with increased inflammation and reduced immune response [33–35], and the increased risk of lung cancer [36] and atherosclerotic heart disease [37] persists even after smoking cessation. The association of cigarette smoking with alterations in DNA methylation has been studied extensively in cross-sectional epigenetic studies, and a potential mechanism by which cigarette smoking may increase disease risk is through direct DNA damage via exposure to carcinogenic toxins [16,38], effects on gene expression [39,40], and hypoxia [41,42]. Previous studies have suggested that smoking cessation results in partial reversal of the DNA methylation changes associated with smoking [17,18]. Time since quitting smoking appears to be associated with greater reversal of DNA methylation patterns to non-smoking levels, although most dynamic epigenetic changes reverse within 5 years of smoking cessation [17].
Our study identified reversion of DNA methylation changes in genes involved in the immune response in adults who quit smoking. Pathway enrichment analysis for the CpG sites that were relatively hypomethylated in current-current smokers pointed to pathways involving response to cytokines and activation of immune cells, highlighting upregulation of the immune response associated with cigarette smoking. These CpG sites were further enriched in cell homoeostasis and apoptosis pathways, perhaps reflecting impairment of healthy cellular metabolism due to cigarette smoking [43,44]. While we measured DNA methylation in whole blood-derived DNA, the association of cigarette smoking with these cellular pathways has previously been established in epithelial [43,45–47], skeletal muscle [48,49], and buccal [16] cells. The adverse effects of cigarette smoking on these tissues may subsequently contribute to the development of chronic diseases, including lung cancer and cardiovascular disease [50]. Additionally, liver abnormalities, lipid metabolism, and neurogenesis pathways were also enriched in GSEA, suggesting a role for DNA methylation and subsequent gene expression in smoking-related liver disease, vascular disease, and dementia.
In this study, we identified six CpG sites that had consistently greater hypomethylation in current-current smokers as compared to non-smokers, regardless of whether the non-smoker group consisted of interim quitters only or of never-never smokers, former-former smokers, and interim quitters. These CpG sites, annotated to AHRR and F2RL3, have been reported as being associated with smoking status in prior studies [16–18, 51, 52]. Of note, we have previously shown that methylation of the CpGs cg05575921 (AHRR), cg03636183 (F2RL3), and cg21566642 (intergenic) also does not return to non-smoking levels even after 30 years [17], which may contribute to the consistency of differences in delta β values that we observe in the interim quitters versus current-current smokers and the current-current smokers versus all non-smoking groups comparisons. Differential methylation in interim quitters versus current-current smokers was associated with the expression of more than 500 unique genes, with the most significant genes being LRRN3 and GPR15 [53–55]. Our eQTM analysis of current-current smokers compared to all non-smokers also identified these same associations, aligning with previous studies that have shown consistent differential expression of these genes in smokers as compared with non-smokers [54]. While our study evaluated methylation in whole blood samples, hypomethylation of LRRN3 and GPR15 has specifically been found in lymphoid cells, suggesting a possible role for these genes in smoking-associated disease development [55]. Methylation of CpG sites annotated to AHRR and F2RL3 may mediate the relationship between smoking and LRRN3 expression [54].
Methylation of CpG sites annotated to the AHRR gene, as well as DMRs that overlap with the AHRR gene on chromosome 5, was most frequently and significantly associated with longitudinal changes in smoking status in this study. AHRR is associated with tobacco use and has been studied for its relationship with smoking status in numerous other studies [17,18, 56–58]. Hypomethylation of the AHRR gene is associated with inactivation of the aryl hydrocarbon receptor (AhR) pathway which is implicated in the response to smoke exposure in immune cells and is potentially a pathway by which smoking leads to the development of lung cancer or cardiovascular disease [50,59]. Epigenome-wide association studies have shown that higher smoking levels are associated with lower methylation at CpG sites annotated to AHRR [56,60], while smoking cessation is associated with reversion towards higher levels of methylation at these sites [58]. Indeed, AHRR-annotated CpG sites in our study were differentially methylated between interim quitters and current-current smokers, as well as between current-current smokers and all other groups, providing additional evidence for reversion at these sites relatively early following smoking cessation.
Our study also validates the role of F2RL3 in the context of smoking and smoking cessation. Greater pack-years of smoking was previously reported to be associated with hypomethylation of the F2RL3 gene[61], and hypomethylation of this gene may partially mediate the association between smoking and heart disease, lung cancer, and mortality [59,62,63]. Accordingly, we found that interim quitters had more hypermethylation than current-current smokers and current-current smokers had more hypomethylation than all non-smoking groups at the CpG site cg03636183, annotated to F2RL3, in our study. Furthermore, a recent 11-year longitudinal study of 1,032 adults found 432 differentially methylated CpG sites in interim quitters as compared with current-current smokers (at nominal P< 0.05), and similarly found hypermethylation of CpG sites annotated to AHRR and F2RL3 following smoking cessation[18].
Analysis of the current-current smokers compared with all non-smoking groups additionally identified significantly hypermethylation at CpG sites annotated to HIVEP3 and TMEM126A and at the intergenic CpG cg14339116. Prior cross-sectional analysis has shown that HIVEP3 is hypermethylated in current versus never smokers, and it may play a role in the development of osteoporosis [17,51,52]. Differential methylation of cg16145216, annotated to HIVEP3, was associated with the expression of 83 unique genes, with the top three most significant genes being SASH1, PID1, and LRRN3. Whole blood expression of SASH1 is decreased in smokers compared with non-smokers, and differential expression of SASH1 by smoking status has been observed previously [64,65]. The role of smoking-associated hypermethylation at CpG sites cg24639862 (TMEM126A) and cg14339116 is less clear, as these sites have not been identified in prior studies of smoking cessation.
Regional analysis characterized consistent differential methylation of two regions: one overlapped with the AHRR gene on chromosome 5, and the other overlapped with three homeobox HOX genes on chromosome 7: HOXA-AS3 (homeobox A cluster antisense RNA 3) and RP1-170O19.22, which are associated with long non-coding RNA, and HOXA3 (homeobox A3). Additionally, while we did not observe significant differential changes in methylation between interim quitters and former-former smokers, we identified more than 100 DMRs between interim quitters and former-former smokers. Many of these overlapped with genes coding for small nucleolar RNA: non-coding RNA that are dysregulated in tobacco smokers and which may be associated with smoking, cancer, and tumorigenesis, and may represent residual differences in cancer risk that are associated with varying time since quitting smoking [66–68]. Several of the small nucleolar RNA genes that are overexpressed in cancer appeared in the DMR comparison of interim quitters to former-former smokers, including SNORA42, SNORD33, and SNORD66 [67,69].
We may have been unable to detect significant differences in specific CpG sites between interim quitters and former-former smokers due to early reversion of perturbed DNA methylation levels following smoking cessation [17], or due to limitations in study design. To increase generalizability and sample size, we combined data from the FHS and ARIC study cohorts; these cohorts have different ancestry (European versus African, respectively) and different follow-up periods (6 years versus 20 years). Because methylation reversion after smoking cessation is time-dependent, it is possible that the expected difference between the interim quitters and former-former smokers was obscured due to heterogeneity in the cohorts.
Another limitation was that we were unable to evaluate time since quitting smoking in the FHS interim quitters due to the unavailability of data and the short time period between the baseline and follow-up study visits. As such, we were also unable to account for differences in the time of smoking cessation to time of sample collection. We were also unable to test either the association of time since quitting smoking with changes in DNA methylation or the age of smoking cessation with changes in DNA methylation. Emphasizing a need to interpret the results of this study with caution.
Our study nonetheless had several strengths, the first of which was the experimental design that used reliable ascertainment of smoking status and validated methods to account for any influence of technical covariates on methylation levels. Analysis of DNA methylation patterns is susceptible to bias introduced by batch effects [70], but statistical processing and meta-analysis of the discovery and replication results in our study minimized these effects. We were able to evaluate longitudinal changes in DNA methylation in our sample, and we included samples from two different study visits in both FHS and ARIC cohorts. The different follow-up windows between studies also allowed for the identification of CpG sites and regions that were consistently associated with smoking status; furthermore, the consistency of directionality across the FHS and ARIC cohorts supported robust associations at the CpG sites identified in these analyses regardless of the overall heterogeneity of the cohorts. Finally, we were able to link longitudinal DNA methylation data with gene expression data in a smaller sample of our study cohort to suggest possible effects of observed DNA methylation changes on gene expression and, subsequently, in biological pathways and disease processes.
In conclusion, we identified differential DNA methylation patterns by smoking status following smoking cessation with a reversion of perturbed DNA methylation of multiple CpG sites towards values observed in never smokers. CpG sites annotated to and regions overlapping with AHRR were sensitive to changes in smoking status, and methylation of some CpG sites annotated to this gene may revert to never-smoking levels early after smoking cessation. Differentially methylated CpG sites annotated to F2RL3 also appeared to revert towards never smoking levels; these genes and have been found to be associated with a change in smoking status in external studies. Finally, the changes in DNA methylation patterns that accompany smoking and smoking cessation affect downstream changes in gene expression in pathways that are implicated in the development of cardiovascular disease and other chronic diseases.
Supplementary Material
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
Funding Statement
The Framingham Heart Study was supported by NIH contract N01-HC-25195. The analytical component of this project was funded by the NHLBI Division of Intramural Research (D. Levy, Principal Investigator). This project was further supported by funding from the American Heart Association (G. O’Connor, Principal Investigator, Transcriptomic and Epigenetic Signatures of Tobacco Exposure). D.L.D. is supported by NIH [P01HL132825, P01HL114501 and an Alpha-1 Foundation Research Grant]. The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the U.S. Department of Health and Human Services (contract numbers HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700004I and HHSN268201700005I). Funding was also supported in part by 5RC2HL102419 and R01NS087541.
Disclosure statement
D.L.D. has received support from Bayer and honoraria from Novartis.
Disclaimer
The views and opinions expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the U.S. Department of Health and Human Services.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/15592294.2021.1985301
References
- [1].GBD 2015 . Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the global burden of disease study 2015. Lancet. 2017;389(10082):1885–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].GBD 2015 . Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1659–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jamal A, Phillips E, As G, et al. Current Cigarette Smoking Among Adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gallaway MS, Henley SJ, Steele CB, et al. Surveillance for cancers associated with tobacco use — United States, 2010-2014. MMWR Surveill Summ. 2018;67(12):1–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].U.S. Department of Health and Human Services . The health consequences of smoking: 50 years of progress. A report of the Surgeon General. Atlanta; 2014.
- [6].Bakulski KM, Dou J, Lin N, et al. DNA methylation signature of smoking in lung cancer is enriched for exposure signatures in newborn and adult blood. Sci Rep. 2019;9(1):4576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Pfeifer GP, Denissenko MF, Olivier M, et al. Tobacco smoke carcinogens, DNA damage and p53 mutations in smoking-associated cancers. Oncogene. 2002;21(48):7435–7451. [DOI] [PubMed] [Google Scholar]
- [8].Dayeh T, Volkov P, Salö S, et al. DNA methylation analysis of human pancreatic islets from type 2 diabetic and non-diabetic donors identifies candidate genes that influence insulin secretion. PLoS Genet. 2014;10(3):e1004160–e1004160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cheishvili D, Parashar S, Mahmood N, et al. Identification of an epigenetic signature of osteoporosis in blood DNA of postmenopausal women. J Bone Miner Res. 2018;33(11):1980–1989. [DOI] [PubMed] [Google Scholar]
- [10].Kim M, Long TI, Arakawa K, et al. DNA methylation as a biomarker for cardiovascular disease risk. PLoS One. 2010;5(3):e9692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Andrea B, Michiel R, Be J.. Cardiovascular Epigenetics. Circ Cardiovasc Genet. 2010;3(6):567–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Martens JW, Margossian AL, Schmitt M, et al. DNA methylation as a biomarker in breast cancer. Future Oncol. 2009;5(8):1245–1256. [DOI] [PubMed] [Google Scholar]
- [13].Leygo C, Williams M, Jin HC, et al. Methylation as a noninvasive epigenetic biomarker for the detection of cancer. Dis Markers. 2017;2017:3726595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].L-x H, Z-h T, Q-s H, et al. DNA Methylation: a potential biomarker of chronic obstructive pulmonary disease. Front Cell Dev Biol. 2020;8:585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Br J, JF F, Yousefi P, et al. DNA Methylation in Newborns and Maternal Smoking in Pregnancy: genome-wide Consortium Meta-analysis. Am J Hum Genet. 2016;98(4):680–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Teschendorff AE, Yang Z, Wong A, et al. Correlation of smoking-associated DNA methylation changes in buccal cells with DNA methylation changes in epithelial cancer. JAMA Oncol. 2015;1(4):476–485. [DOI] [PubMed] [Google Scholar]
- [17].Joehanes R, Ac J, Re M, et al. Epigenetic Signatures of Cigarette Smoking. Circ Cardiovasc Genet. 2016;9(5):436–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].P-a D, C-h J, JE J, et al. Smoking and blood DNA methylation: an epigenome-wide association study and assessment of reversibility. Epigenetics. 2020;15(4):358–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Teschendorff AE, Marabita F, Lechner M, et al. A beta-mixture quantile normalization method for correcting probe design bias in Illumina Infinium 450 k DNA methylation data. Bioinformatics. 2013;29(2):189–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Triche JTJ, Weisenberger DJ, Van Den Berg D, et al. Low-level processing of Illumina Infinium DNA Methylation BeadArrays. Nucleic Acids Res. 2013;41(7):e90–e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Irizarry RA, Ladd-Acosta C, Carvalho B, et al. Comprehensive high-throughput arrays for relative methylation (CHARM). Genome Res. 2008;18(5):780–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Jiao C, Zhang C, Dai R, et al. Positional effects revealed in Illumina methylation array and the impact on analysis. Epigenomics. 2018;10(5):643–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Joehanes R, Zhang X, Huan T, et al. Integrated genome-wide analysis of expression quantitative trait loci aids interpretation of genomic association studies. Genome Biol. 2017;18(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Houseman EA, Accomando WP, Koestler DC, et al. DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinformatics. 2012;13(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Vazquez AI, Bates DM, Rosa GJM, et al. Technical note: an R package for fitting generalized linear mixed models in animal breeding. J Anim Sci. 2010;88(2):497–504. [DOI] [PubMed] [Google Scholar]
- [26].Devlin B, Roeder K. Genomic control for association studies. Biometrics. 1999;55(4):997–1004. [DOI] [PubMed] [Google Scholar]
- [27].Peters TJ, Buckley MJ, Statham AL, et al. R, Clark SJ, Molloy PL. De novo identification of differentially methylated regions in the human genome. Epigenetics Chromatin. 2015;8(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci. 2005;102(43):15545– 15550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Liberzon A, Birger C, Thorvaldsdóttir H, et al. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Syst. 2015;1(6):417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Centers for Disease Control and Prevention . How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general. Atlanta; 2010. [PubMed]
- [31].Deal JA, Power MC, Palta P, et al. Relationship of cigarette smoking and time of quitting with incident dementia and cognitive decline. J Am Geriatr Soc. 2020;68(2):337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Elbejjani M, Auer R, Dolui S, et al. Cigarette smoking and cerebral blood flow in a cohort of middle-aged adults. J Cereb Blood Flow Metab. 2019;39(7):1247–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Holt PG, Keast D. Environmentally induced changes in immunological function: acute and chronic effects of inhalation of tobacco smoke and other atmospheric contaminants in man and experimental animals. Bacteriol Rev. 1977;41(1):205–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].McCrea KA, Ensor JE, Nall K, et al. Altered cytokine regulation in the lungs of cigarette smokers. Am J Respir Crit Care Med. 1994;150(3):696–703. [DOI] [PubMed] [Google Scholar]
- [35].Bauer M, Fink B, Thürmann L, et al. Tobacco smoking differently influences cell types of the innate and adaptive immune system-indications from CpG site methylation. Clin Epigenetics. 2016;7(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].United States Public Health Service Office of the Surgeon General . Smoking cessation: a report of the surgeon general. Washington, DC; 2020.
- [37].Kianoush S, Yakoob MY, Al-Rifai M, et al. Associations of cigarette smoking with subclinical inflammation and atherosclerosis: ELSA-Brasil (The Brazilian Longitudinal Study of Adult Health). J Am Heart Assoc. 2017;6(6). DOI: 10.1161/JAHA.116.005088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Suter M, Abramovici A, Showalter L, et al. In utero tobacco exposure epigenetically modifies placental CYP1A1 expression. Metabolism. 2010;59(10):1481–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lee EW, D’Alonzo GE. Cigarette smoking, nicotine addiction, and its pharmacologic treatment. Arch Intern Med. 1993;153(1):34–48. [PubMed] [Google Scholar]
- [40].Han L, Lin IG, Hsieh CL. Protein binding protects sites on stable episomes and in the chromosome from de novo methylation. Mol Cell Biol. 2001;21(10):3416–3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Lee KWK, Pausova Z. Cigarette smoking and DNA methylation. Front Genet. 2013;4:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Liu Q, Liu L, Zhao Y, et al. Hypoxia induces genomic DNA demethylation through the activation of HIF-1α and transcriptional upregulation of MAT2A in hepatoma cells. Mol Cancer Ther. 2011;10(6):1113–1123. [DOI] [PubMed] [Google Scholar]
- [43].Liu Q, Zhao M, Chen W, et al. Mainstream cigarette smoke induces autophagy and promotes apoptosis in oral mucosal epithelial cells. Arch Oral Biol. 2020;111:104646. [DOI] [PubMed] [Google Scholar]
- [44].Wang G, Zhou H, Strulovici-Barel Y, et al. Role of OSGIN1 in mediating smoking-induced autophagy in the human airway epithelium. Autophagy. 2017;13(7):1205–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Bazzini C, Rossetti V, Civello DA, et al. Short- and long- term effects of cigarette smoke exposure on glutathione homeostasis in human bronchial epithelial cells. Cell Physiol Biochem. 2013;32(suppl 1):129–145. [DOI] [PubMed] [Google Scholar]
- [46].Bernhard D, Pfister G, Huck CW, et al. Disruption of vascular endothelial homeostasis by tobacco smoke—impact on atherosclerosis. FASEB J. 2003;17(15):2302–2304. [DOI] [PubMed] [Google Scholar]
- [47].Toda N, Okamura T. Cigarette smoking impairs nitric oxide-mediated cerebral blood flow increase: implications for Alzheimer’s disease. J Pharmacol Sci. 2016;131(4):223–232. [DOI] [PubMed] [Google Scholar]
- [48].Nogueira L, Bm T, Fl L-R, et al. Cigarette smoke directly impairs skeletal muscle function through capillary regression and altered myofibre calcium kinetics in mice. J Physiol. 2018;596(14):2901–2916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Ajime TT, Serré J, RCI W, et al. Weeks of smoking cessation reverse cigarette smoke-induced skeletal muscle atrophy and mitochondrial dysfunction in mice. Nicotine Tob Res. 2020. DOI: 10.1093/ntr/ntaa016 [DOI] [PubMed] [Google Scholar]
- [50].Chen Y, Widschwendter M, Teschendorff AE. Systems-epigenomics inference of transcription factor activity implicates aryl-hydrocarbon-receptor inactivation as a key event in lung cancer development. Genome Biol. 2017;18(1):236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Wilson R, Wahl S, Pfeiffer L, et al. The dynamics of smoking-related disturbed methylation: a two time-point study of methylation change in smokers, non-smokers and former smokers. BMC Genomics. 2017;18(1):805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Christiansen C, JE C-F, Domingo-Relloso A, et al. Novel DNA methylation signatures of tobacco smoking with trans-ethnic effects. Clin Epigenetics. 2021;13(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Vink JM, Jansen R, Brooks A, et al. Differential gene expression patterns between smokers and non-smokers: cause or consequence? Addict Biol. 2017;22(2):550–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Maas SCE, Mens MMJ, Kühnel B, et al. Smoking-related changes in DNA methylation and gene expression are associated with cardio-metabolic traits. Clin Epigenetics. 2020;12(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].You C, Wu S, Zheng SC, et al. A cell-type deconvolution meta-analysis of whole blood EWAS reveals lineage-specific smoking-associated DNA methylation changes. Nat Commun. 2020;11(1):4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Bojesen SE, Timpson N, Relton C, et al. AHRR (cg05575921) hypomethylation marks smoking behaviour, morbidity and mortality. Thorax. 2017;72(7):646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Philibert R, Dogan M, Beach SRH, et al. AHRR methylation predicts smoking status and smoking intensity in both saliva and blood DNA. Am J Med Genet Part B, Neuropsychiatr Genet Off Publ Int Soc Psychiatr Genet. 2020;183(1):51–60. [DOI] [PubMed] [Google Scholar]
- [58].Philibert R, Hollenbeck N, Andersen E, et al. Reversion of AHRR demethylation is a quantitative biomarker of smoking cessation. Front Psychiatry. 2016;7:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Fasanelli F, Baglietto L, Ponzi E, et al. Hypomethylation of smoking-related genes is associated with future lung cancer in four prospective cohorts. Nat Commun. 2015;6(1):10192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].McCartney DL, Stevenson AJ, Hillary RF, et al. Epigenetic signatures of starting and stopping smoking. EBioMedicine. 2018;37:214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Wan ES, Qiu W, Baccarelli A, et al. Cigarette smoking behaviors and time since quitting are associated with differential DNA methylation across the human genome. Hum Mol Genet. 2012;21(13):3073–3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Breitling LP, Salzmann K, Rothenbacher D, et al. F2RL3 methylation, and prognosis in stable coronary heart disease. Eur Heart J. 2012;33(22):2841–2848. [DOI] [PubMed] [Google Scholar]
- [63].Zhu K, Meng Q, Zhang Z, et al. Aryl hydrocarbon receptor pathway: role, regulation and intervention in atherosclerosis therapy (Review). Mol Med Rep. 2019;20:4763–4773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Beineke P, Fitch K, Tao H, et al. A whole blood gene expression-based signature for smoking status. BMC Med Genomics. 2012;5(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Verdugo RA, Zeller T, Rotival M, et al. Graphical modeling of gene expression in monocytes suggests molecular mechanisms explaining increased atherosclerosis in smokers. PLoS One. 2013;8(1):e50888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Nogueira Jorge NA, Wajnberg G, Ferreira CG, et al. snoRNA and piRNA expression levels modified by tobacco use in women with lung adenocarcinoma. PLoS One. 2017;12(8):e0183410–e0183410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Liao J, Yu L, Mei Y, et al. Small nucleolar RNA signatures as biomarkers for non-small-cell lung cancer. Mol Cancer. 2010;9(1):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Zou AE, Ku J, Honda TK, et al. Transcriptome sequencing uncovers novel long noncoding and small nucleolar RNAs dysregulated in head and neck squamous cell carcinoma. RNA. 2015;21(6):1122–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Mei Y-P, Liao J-P, Shen J, et al. Small nucleolar RNA 42 acts as an oncogene in lung tumorigenesis. Oncogene. 2012;31(22):2794–2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Price EM, Robinson WP. Adjusting for batch effects in DNA methylation microarray data, a lesson learned. Front Genet. 2018;9:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


