Background:
Foot drop is a common complication in post-stroke. Patients with foot drop are at high risk for falls and fall-related injuries. Accordingly, it can reduce independence and quality of life in patients. Clinical studies have confirmed that acupuncture is effective in treating foot drop in post-stroke. However, there is a lack of systematic review exploring the efficacy and safety of acupuncture treatment. This study aims to assess the efficacy and safety of acupuncture in the treatment of foot drop in poststroke from the results of randomized controlled trials.
Methods:
We will search articles in 8 electronic databases including the Cochrane Central Register of Controlled Trials, the Web of Science, PubMed, Embase, the China National Knowledge Infrastructure, the Chinese Biomedical Literature Database, Wanfang Data Database, and the Chinese Scientific Journal Database for RCTs of acupuncture treated foot drop in post-stroke from their inception to 10 August 2022. We will analyze the data meeting the inclusion criteria with the RevMan V.5.4 software. Two authors will assess the quality of the study with the Cochrane collaborative risk bias tool. We will evaluate the certainty of the estimated evidence with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method. Data analysis will be performed using STATA 16.0.
Results:
This study will review and evaluate the available evidence for the treatment of foot drop in post-stroke using acupuncture.
Conclusion subsections:
This study will determine the efficacy and safety of acupuncture applied to post-stroke individuals with foot drop.
Keywords: acupuncture, foot drop in post-stroke, protocol, systematic review
1. Introduction
Stroke is a common clinical cerebrovascular disease, including hemorrhagic stroke and ischemic stroke. In recent years, the incidence of stroke has been raised, and it has become the main cause of mortality and disability in the elderly.[1] Surviving patients are often left with limb dysfunction whom more than 80%,[2] and foot drop is one of the common symptoms.[3] As estimated, the incidence rate of foot drop after stroke is as high as 20% to 30%.[4,5] This condition is related to the weakness or lack of voluntary control in ankle dorsiflexors and/or the increased spasticity of plantar flexor muscles.[6–8] Foot drop results in disruption of weight acceptance and weight transfer in the initial foot contact and stance phases and interferes with ankle dorsiflexion during the swing phase of the gait.[9] Thus, foot drop leads to an inefficient walking speed, reduces gait stability,[10] and increases the risk of falls.[11] In this condition, gait impairment may restrict activities of daily living, affect independence, and reduce the quality of life.[12] Therefore, it is important to treat foot drop to ensure a safe gait for stroke patients.
Rehabilitation and physical therapy, drug therapy, and operation therapy are the primary methods in Western medicine to treat foot drop in post-stroke. However, drug treatment has large side effects which hinder the recovery of motor function with long time taking.[13] Two types of physical therapy commonly used today are the installation of an ankle-foot orthosis (AFO) or the use of functional electrical stimulation (FES) via an electronic stimulator. The previous study has shown that AFO can improve gait velocity, cadence, and stride length.[14] But AFO only has an immediate orthotic effect, so the foot drop reoccurs without it. FES is applied to the common peroneal nerve, causing contraction of the tibialis anterior muscle and ankle dorsiflexion, to reduce foot drop.[15] But it has limitations on patient compliance, adaptation, and comfort. As for surgical treatment, most patients cannot accept it because it is traumatic.
Acupuncture is a unique external treatment method of traditional Chinese medicine, which has a history of thousands of years. Acupuncture stimulates acupoints on the body surface, transmits information to the central nervous system, and then stimulates motor nerve cells from the central nervous system, which can stimulate the antagonistic muscle groups and inhibit the spasmodic muscle groups, thereby improving the body’s motor function. Some clinical studies have confirmed the advantages of acupuncture in the treatment of hemiplegic, which can improve the gait of the foot drop in post-stroke.[16,17] However, there is currently no systematic review exploring the efficacy of acupuncture treatment. So this study will collect data on randomized controlled trials (RCTs) of acupuncture for foot drop in post-stroke. These data will be synthesized in a systematic review with meta-analysis to explore the efficacy and safety of acupuncture in the treatment of foot drop in post-stroke, and to provide evidence for clinical decision-making of acupuncture.
2. Methods and analysis
2.1. Design and registration of the review
The protocol has been registered on PROSPERO basing on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement guidelines.[18] The registration number is CRD42022325951.
2.2. Inclusion criteria
2.2.1. Types of studies.
We will collect RCTs (not including quasi-RCTs) of acupuncture in the treatment of foot drop in post-stroke. All eligible trials will be included regardless of language and publication type. Review articles, case series, cohort studies, retrospective studies, and animal experiments that do not meet the requirements will be excluded.
2.2.2. Types of patients.
Patients must meet the following requirements: In line with “2016 Guidelines and Consensus on Diagnosis and Treatment of Chinese Cerebrovascular Diseases”, and were first confirmed by cerebral CT or MRI as having a stroke (cerebral infarction or cerebral hemorrhage); age > 18 years old, and disease course < 6 months; have the symptoms of hemiplegia in one limb and foot drop; the Modified Ashworth Scale (MAS) score is grade 1 to 4.
2.2.3. Types of interventions.
In the intervention group, patients received acupuncture, alone or combined with routine rehabilitation treatment (FES, ankle-foot orthoses, and physiotherapy, among others). In the control group, patients only received routine rehabilitation treatment.
2.2.4. Types of outcome measures.
2.2.4.1. Primary outcomes.
Gait speed will be assessed by the 10-m Walk Test (10MWT).It will be calculated as the ratio between distance and time spent (seconds) to walk 10 m.
Spasticity of plantar flexor muscles will be assessed by the MAS.
2.2.5.1. Secondary outcomes.
Anterior tibial muscle strength will be assessed by the Modified Lovett test;
Lower extremity motor function will be assessed by the Fugl-Meyer Assessment Scale (FMA);
Daily living ability will be assessed by the Modified Barthel Index;
The improvement of foot drop will be assessed by the Garceau standard.
2.3. Exclusion criteria
Studies with the following situations will be excluded: foot drop due to a neurological diagnosis other than stroke; the patient has lower limb fractures; studies comparing the same modality of acupuncture with different doses of time, frequency, or duration; conference abstracts without a full published article; duplicated data or data that cannot be extracted.
2.4. Search methods for the identifying of studies
Two reviewers (YG and XG) will independently search the China National Knowledge Infrastructure, the Chinese Biomedical Literature Database, Wanfang Data, the Chinese Scientific Journal Database, the Cochrane Central Register of Controlled Trials, the Web of Science, PubMed, and Embase databases from inception to 10 August 2022. Except for electronic search, we will also hand search the conference summary and trial register. Any disagreement will be resolved by discussion until consensus is reached or by consulting a third researcher (YY).
2.5. Search strategy
The search strategy will be based on the Cochrane handbook guidelines (V.5.1.0) including keywords such as “post-stroke”, “foot drop” or “hemiplegia”, “acupuncture”, and “RCT”. Subsequent searches will use Medical Subject Headings (MeSH) headings, including “post-stroke”, and “acupuncture”, in addition to keywords from the initial retrieval. The reference lists of relevant research articles were reviewed for any additional article searches. The details of the PubMed search strategies are provided in Table 1. Other electronic databases are also suitable for this search strategy.
Table 1.
The search strategy for Pub Med database.
| No | Search terms |
|---|---|
| #1 | post-stroke.ti,mesh. |
| #2 | poststroke.ti,ab. |
| #3 | Apoplectic.ti,ab. |
| #4 | after stroke.ti,ab. |
| #5 | Cerebral hemorrhage. ti,ab. |
| #6 | Cerebral embolism |
| #7 | #1 or #2 or #3 or #4 or #5 or #6 |
| #8 | acupuncture.ti,mesh. |
| #9 | acupoint.ti,ab. |
| #10 | fire-needle.ti,ab. |
| #11 | three-edged needle.ti,ab. |
| #12 | plum blossom needle.ti,ab. |
| #13 | pinprick.ti,ab. |
| #14 | needle therapy.ti,ab. |
| #15 | needle.ti,ab. |
| #16 | #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 |
| #17 | randomized controlled trial.pt. |
| #18 | randomized.ab. |
| #19 | trial.ab. |
| #20 | #17 or #18 or #19 |
| #21 | #7 and #16 and #20 |
2.6. Data extraction
2.6.1. Study selection.
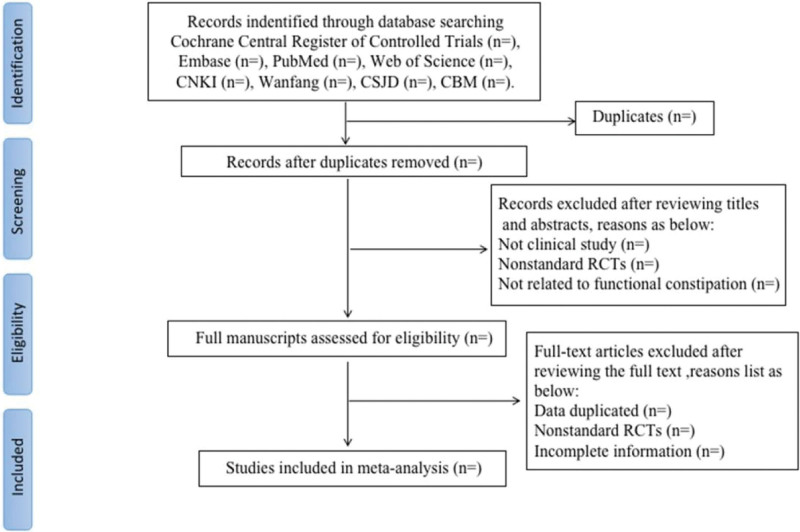
Records from databases and other resources will be uploaded to a database created in EndNote software(X.9.3.3). Two review authors (YG and XG) will independently evaluate the titles and abstracts of all citations found from the above search strategy. We will obtain the full text of all potentially suitable articles to further assess eligibility based on the inclusion/exclusion criteria. The disagreement will be resolved by consensus or mediated by a third author (YY). The final selection process will follow the PRISMA guidelines,[18]as shown in Figure 1.
Figure 1.
Flow chart of the search process.
2.6.2. Data extraction and management.
Two reviewers (YG and XG) will independently apply the inclusion and exclusion criteria to assess each retrieved study’s eligibility. The data will then be extracted from the selected studies for inclusion using a data collection form and recorded in an Excel file. The following data will be extracted: study characteristics such as author, year of publication, country where the study was conducted, study period, original inclusion criteria, total number of people included in the study; population characteristics such as type of stroke, mean age, and time from diagnosis; intervention characteristics such as type, duration, and frequency; outcomes such as the 10MWT, MAS score, FMA, Modified Lovett test, Modified Barthel Index, and the Garceau standard. Disagreements in data collection will be resolved by consensus, with any ongoing differences in opinion arbitrated by a third reviewer (YY). If possible, we will contact the author of the article to provide additional relevant information.
2.7. Risk of bias assessment
Two review authors (YG and XG) will assess the internal validity of included studies by using the Cochrane Handbook for Systematic Reviews of Interventions.[19] The following domains will be assessed: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), incomplete outcome data (attrition bias), outcome assessment (detection bias), selection of the reported result (reporting bias), and other biases (such as pre-sample size estimation, early stop of trial). Results from these questions will be graphed and assessed using Review Manager 5.4. Each item will be evaluated in three categories: low risk of bias, unclear bias, and high risk of bias. Any discrepancies will be resolved by reviewing the original article and discussing it with the third author (YY) to reach a consensus.
2.8. Measures of treatment effect
Data will be subjected to statistical analysis using RevMan5.4 software. For continuous variables, we will present mean differences with standard deviations, or median and interquartile range. For dichotomous variables, we will report the overall mean proportion (%) of the population. The 95% CI will be presented for both dichotomous and continuous outcomes.
2.8.1. Missing data management.
We will obtain the missing data by contacting the original authors of the papers via email or telephone if possible. Otherwise, we will analyze the available information and conduct a sensitivity analysis to explore the potential impact of insufficient information on the results of the meta-analysis.
2.9. Heterogeneity assessment
Statistical heterogeneity will be assessed with the I2 statistic. We will interpret it using the following criteria: I2 values of 25% is considered low levels of heterogeneity, 50% indicated moderate levels, and 75% indicated high levels.[20] Since low or moderate heterogeneity suggests little variability among these studies, the data will be analyzed in a fixed-effects model.[21] When significant heterogeneity occurs among the studies (P < .05, I2 > 50%), a random-effect model will be performed to analyze the data.
2.10. Assessment of reporting biases
Reporting bias will be assessed by Egger’s regression asymmetry test.[22] A P value < .05 in the Egger test is considered statistically significant. STATA V.16.0.b software will be used to perform Egger test.
2.11. Subgroup analysis
We plan to carry out the following subgroup analyses to explore possible sources of heterogeneity: different types of stroke, the course of the disease, different types of acupuncture, different times of treatment, and different types of routine rehabilitation methods. If the data is insufficient, the qualitative synthesis will be conducted instead of the quantitative synthesis. We will use the formal test for subgroup interactions in Review Manager V.5.4.
2.12. Sensitivity analysis
When possible, we will perform sensitivity analysis by eliminating low-quality trials to explore the effects of the trial’s bias risk on primary outcomes.
2.13. Grading the quality of evidence
The quality of evidence regarding patient outcomes will be used and assessed by the Grading of Recommendations Assessment, Development, and Evaluation methodology (GRADE; https://www.Gradeworkinggroup.org/). GRADE will be used to summarize the limitations in design, consistency, directness, precision, and publication bias. The quality of each piece of evidence will be divided into four levels: high, medium, low, and very low.
3. Ethics and dissemination
This systemic review will evaluate the efficacy and safety of acupuncture in the treatment of foot drop in post-stroke. Since all included data will be obtained from published articles, it does not require ethical approval and will be published in a peer-reviewed journal. The results may contribute to improving the therapeutic strategy of patients with foot drop in post-stroke.
4. Discussion
Foot drop after stroke is a relatively common type of sequelae that is mainly caused by central nervous system injury.[23] The patient tends to an abnormal posture such as “circling gait” due to foot drop, which will hinder the establishment of normal mobility mode and affect the recovery of lower limb motor function in hemiplegia.[24] Acupuncture can stimulate the meridians to improve local blood circulation in the brain tissue of stroke patients and improve neurological deficits. And acupuncture also can eliminate contractures of the posterior calf muscles, improve the muscle group tension of the posterior calf and achieve the effect of treating foot drop.[25,26] By acupuncture Indwelling the traction stimulation for soft tissue, the contraction force of muscle fibers is enhanced, and unidirectionally pulling the front calf muscle group strongly, which can achieve the effect of straightening. Compared with rehabilitation training, acupuncture has the characteristics of convenient operation, low cost, and a wide range of indications. Some studies show acupuncture is good at treating foot drop and has been clinically verified. However, from the existing literature, and considering the lack of meta-analyses exploring the effects of acupuncture, we cannot make evidence-based inferences about the clinical benefit of acupuncture for foot drop in post-stroke. This review aims to determine the efficacy and safety of acupuncture applied to post-stroke individuals with foot drop. We will analyze the effect of acupuncture combined or not with other therapies on gait speed, muscle strength, lower extremity motor function, daily living ability, and the improvement of foot drop.
Author contributions
Conceptualization: Ying Gao.
Formal analysis: Ying Gao, Xiaochao Gang.
Investigation: Ying Gao, Xiaochao Gang.
Methodology: Xiaochao Gang, Yue Yuan.
Supervision: Ying Gao, Xiao Yan Gong.
Writing – original draft: Ying Gao, Xiaochao Gang, Yue Yuan, Kai Yin.
Writing – review & editing: Xiao Yan Gong.
Funding acquisition: Xiaochao Gang.
Data curation: Yue Yuan, Kai Yin.
Software: Kai Yin.
Abbreviations:
- AFO =
- ankle-foot orthosis
- FES =
- functional electrical stimulation
- FMA =
- the Fugl-Meyer Assessment Scale
- MAS =
- the Modified Ashworth Scale
- RCTs =
- randomized controlled trials, the 10-m Walk Test (10MWT).
The datasets generated during and/or analyzed during the current study are publicly available.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The authors have no conflicts of interest to disclose.
This work was supported by National College Students Innovation and Entrepreneurship Training Program in 2021 (grant number: 202110199019).
How to cite this article: Gao Y, Gang X, Yuan Y, Yin K, Gong X. Efficacy and safety of acupuncture in the treatment of foot drop in post-stroke: A protocol for systematic review and meta-analysis. Medicine 2022;101:40(e30994).
PROSPERO registration number: CRD42022325951
References
- [1].Chen M, Wu B, Lou X, et al. A self-adaptive foot-drop corrector using functional electrical stimulation (FES) modulated by tibialis anterior electromyography (EMG) dataset. Med Eng Phys. 2013;35:195–204. [DOI] [PubMed] [Google Scholar]
- [2].Aqueveque P, Ortega P, Pino E, et al. After stroke movement impairments: a review of current technologies for rehabilitation. Tan U, (ed). In Physical disabilities—therapeutic implications. IntechOpen Limited: London, UK. 2017. [Google Scholar]
- [3].Sheffler LR, Chae J. Hemiparetic Gait. Phys Med Rehabil Clin N Am. 2015;26:611–23. [DOI] [PubMed] [Google Scholar]
- [4].Pilkar R, Ramanujam A, Nolan KJ. Alterations in spectral attributes of surface electromyograms after utilization of a foot drop stimulator during post-stroke gait. Front Neurol. 2017;8:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Thibaut A, Moissenet F, Perri CD, et al. Brain plasticity after implanted peroneal nerve electrical stimulation to improve gait in chronic stroke patients: two case reports. NeuroRehabilitation. 2017;40:251–8. [DOI] [PubMed] [Google Scholar]
- [6].Chisholm AE, Perry SD, McIlroy WE. Correlations between ankle-foot impairments and dropped foot gait deviations among stroke survivors. Clin Biomech (Bristol, Avon). 2013;28:1049–54. [DOI] [PubMed] [Google Scholar]
- [7].Stewart JD. Foot drop: where, why and what to do? Pract Neurol. 2008;8:158–69. [DOI] [PubMed] [Google Scholar]
- [8].Pittock SJ, Moore AP, Hardiman O, et al. A double-blind randomised placebo-controlled evaluation of three doses of botulinum toxin type A (Dysport) in the treatment of spastic equinovarus deformity after stroke. Cerebrovasc Dis. 2003;15:289–300. [DOI] [PubMed] [Google Scholar]
- [9].Duncan PW. Stroke disability. Phys Ther. 1994;74:399–407. [DOI] [PubMed] [Google Scholar]
- [10].Nolan KJ, Yarossi M. Weight transfer analysis in adults with hemiplegia using ankle foot orthosis. Prosthet Orthot Int. 2011;35:45–53. [DOI] [PubMed] [Google Scholar]
- [11].Tyson SF, Crow JL, Connell L, et al. Sensory impairments of the lower limb after stroke: a pooled analysis of individual patient data. Top Stroke Rehabil. 2013;20:441–9. [DOI] [PubMed] [Google Scholar]
- [12].Li S, Francisco GE, Zhou P. Post-stroke hemiplegic gait: new perspective and insights. Front Physiol. 2018;9:1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Guo T. Comparison of the therapeutic effects of three kinds of oral antispasmodic drugs on limb spasm after stroke. Chinese J Rehab Theory Pract. 2012;18:453– 5. Chinese [Google Scholar]
- [14].Abe H, Michimata A, Sugawara K, et al. Improving gait stability in stroke hemiplegic patients with a plastic ankle-foot orthosis. Tohoku J Exp Med. 2009;218:193–9. [DOI] [PubMed] [Google Scholar]
- [15].Everaert DG, Stein RB, Abrams GM, et al. Effect of a foot-drop stimulator and ankle-foot orthosis on walking performance after stroke: a multicenter randomised controlled trial. Neurorehabil Neural Repair. 2013;27:579–91. [DOI] [PubMed] [Google Scholar]
- [16].Lei C, Yang X, Song L. Clinical observation on treatment of foot drop after apoplexy with three ankle acupuncture. Chin Med Emergency. 2014;23:1517–1519. Chinese. [Google Scholar]
- [17].Qian L. Clinical observation of Xingnao Kaiqiao acupuncture combined with rehabilitation training in the treatment of foot drop after stroke. Traditional Chin Med Technol China. 2016;23:325–326. Chinese. [Google Scholar]
- [18].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Rao S, Han X, Shi M, et al. Associations of the serotonin transporter promoter polymorphism (5-HTTLPR) with bipolar disorder and treatment response: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;89:214–26. [DOI] [PubMed] [Google Scholar]
- [22].Sterne JA, Egger M, Smith GD. Systematic reviews in health care:investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Shaikh MF, Salcic Z, Wang KI, et al. Bipedal gait model for precise gait recognition and optimal triggering in foot drop stimulator: a proof of concept. Med Biol Eng Comput. 2018;56:1731–46. [DOI] [PubMed] [Google Scholar]
- [24].Li WL, Tong L, Zhang WJ. Efficacy of action observation therapy based on mirror neuron theory in patients with foot drop after stroke. Chin J Rehabil. 2019;34:569–572. Chinese [Google Scholar]
- [25].Qi Y, Shen J. Acupuncture combined with rehabilitation training for foot drop after stroke. Zhongguo Zhen Jiu. 2016;36:679–82. [DOI] [PubMed] [Google Scholar]
- [26].Liu S, Chi XF, Kuang WC, et al. Clinical trials of treatment of post-stroke foot drop by fire-needling plus stuck-needle-stretching. Zhen Ci Yan Jiu. 2019;44:367–72. [DOI] [PubMed] [Google Scholar]