Abstract
Objectives
Assess changes in access and psychological status during the COVID-19 pandemic in people with spinal cord injury (SCI).
Study Design
Cohort telephone survey study.
Setting
South Florida SCI Model System (SF-SCIMS)
Participants
A convenience sample of 51 individuals with traumatic SCI who had previously completed SCIMS Form II follow-up interviews.
Interventions
Not applicable.
Main Outcome Measure(s)
Questionnaire administration included assessments of resilience, depressive symptoms, satisfaction with life, anxiety, pain, alcohol and substance use, COVID-19 diagnoses and symptoms, and impact of early COVID-19 community restrictions on various aspects of life.
Results
Of the individuals interviewed, 78% reported limited access to their regular activities, 40% to healthcare information and services, 38% to personal protective equipment (PPE), 37% to food/groceries, and 34% to medication refills. Sixteen percent of the participants had at least moderate levels of depression, and 10% had at least moderate levels of anxiety. Statistically significant increases in depressive symptoms (Patient Health Questionnaire 9; P = 0.004) and significant decreases in resilience (SCI-Quality of Life Resilience subscore; P = 0.010) were found when comparing scores on measures of psychological function at the time of the study to scores collected during the previous SCIMS Form II interview (within 2 years pre-COVID-19).
Conclusion(s)
Limitations to basic needs and face-to-face communication can exacerbate challenges in access for persons with disabilities. Our results show increased levels of psychological distress related to decreased access to goods and services in individuals with SCI due to the COVID-19 pandemic. The results of this study can help the SCI community to target strategies for enhanced access, outreach, shared information, and social support in preparation for future community health or weather emergencies.
Key words: Spinal Cord injury, COVID-19, Depression, Anxiety, Mental health
Introduction
In December 2019, the first cases of the novel coronavirus disease 2019 (COVID-19) were reported in Wuhan, China1 and in January 2020, the World Health Organization (WHO) declared the COVID-19 outbreak to be a Public Health Emergency of International Concern. Due to the rapid increase of positive cases, most governments enforced mitigation restrictions that limited the movement of people to reduce the risk of transmission. Although these steps are important to lessen the spread of this disease, they can have both short- and long-term mental and physical health consequences and significantly impact well-being, particularly for vulnerable populations2 such as people with spinal cord injury (SCI).3 Depending on the neurological level of injury of the person with SCI, there are varying degrees of physiological deficits, physical limitations, and secondary health consequences, which require specialized equipment and daily assistance from caregivers that is not required in the general population.4 Therefore, individuals with SCI, especially those with cervical or high thoracic injuries, compose one of the groups in society that is most vulnerable to the impacts of COVID-19 mitigation measures, including social distancing, which may convey an increased burden on both physical and psychological health.5,6
Depressive disorders have an estimated prevalence rate of 22% in the SCI population,7 and clinically significant symptoms of anxiety are reported to occur in approximately 27%.8 The prevalence and severity of depressive symptoms and anxiety might be expected to be increased during the COVID-19 pandemic, as resources have become harder to acquire and social distancing continues.2 Research on the psychological impact of mass trauma (e.g. natural disasters) suggests that the pandemic might particularly harm the mental health of marginalized populations who may have less expansive social support networks.9
Understanding the effects of the COVID-19 outbreak on the mental health of people with SCI may be just as important as understanding its clinical features, transmission patterns, and management. Thus, we undertook the current study in a sample of individuals with SCI in the local South Florida area to evaluate reported limitations in access to necessary resources, changes in psychological and physical health status during the COVID-19 pandemic compared to data collected before the pandemic, and to explore relationships among resource limitations and psychological health.
Methods
Participants
Participants eligible for enrollment were aged 18 years or older, at least one-year post-SCI, had previously consented to enrollment into the South Florida Spinal Cord Injury Model System (SF-SCIMS), as part of the National SCIMS Database, and had completed a SCIMS Form II follow-up interview between February 1, 2018, and January 31, 2020 (i.e. before COVID-19 restrictions in the US). A convenience sample was recruited from this population of eligible participants, with a targeted enrollment of 50 individuals. Potential participants were contacted via phone for recruitment, and a verbal informed consent process was conducted. Institutional Review Board approval was obtained before initiating recruitment.
Procedures
The study was initiated approximately four months after COVID-19 restrictions were instituted in the cities and counties making up the South Florida region (Miami-Dade, Broward, and Monroe counties), with recruitment beginning on August 3, 2020. Questionnaire administration included assessments of resilience, depressive symptoms, satisfaction with life, anxiety, pain, alcohol and substance use, COVID-19 diagnoses and symptoms, and impact of COVID-19 on various aspects of life. Other data were extracted from responses obtained during the most recent, pre-pandemic, SCIMS Form II interview conducted with the participant (between Feb. 1, 2018, and Jan. 31, 2020).
Measures extracted from pre-COVID SCIMS Form II interview
Demographic and injury information: Data were extracted regarding current age, time since injury, level of injury, and self-reported sex, race, and ethnicity.
Spinal Cord Injury – Quality of Life (SCI-QOL), short-form Resilience subscale10: The short form of the SCI-QOL Resilience subscale includes 8 items regarding thoughts and activities related to adaptive responses for dealing positively with stressful life events. The participant is asked to respond with how often they experience each of the items, as “never,” “rarely,” “sometimes,” “often,” or “always,” with values assigned to each of these responses from 1 to 5, respectively. A total score is calculated, and a look-up table is used to convert to a t-score that has been calibrated based on data previously collected in participants with SCI.10
Patient Health Questionnaire-9 (PHQ-9)11,12: The PHQ-9 is a validated questionnaire querying the frequency of endorsement of nine symptoms associated with clinical depression during the previous two weeks. Each item is evaluated by the respondent as happening “not at all,” “several days (1-7 days),” “more than half the time (8-12 days),” or “nearly every day.” Total scores range from 0-22, with higher scores representing greater depressive symptoms. The PHQ-9 has been widely used in several participant groups and has specifically been validated in persons with SCI.13,14
Satisfaction with Life Scale (SWLS)15: The original SWLS is a 5-item scale that asks participants to respond with their degree of endorsement of each item using a 7-category Likert-type scale from “strongly disagree” to “strongly agree.” It has been validated in several populations, including in individuals with TBI and SCI.16-18 One of the items in the original questionnaire, “If I could live my life over, I would change almost nothing,” however, has been found to reduce the reliability of the total scores obtained from the scale when it is administered to individuals with trauma-related disabilities.15 Thus, the four-item version was used to calculate a total SWLS score (range 4–28), with higher scores indicative of greater perceived life satisfaction.
Alcohol Use Disorders Identification Test-Concise (AUDIT-C)19: The AUDIT-C asks three questions about the frequency and amount of alcohol consumption, with responses to each question scored on a 0–4 scale, resulting in total scores ranging from 0-12. Higher scores generally indicate a greater likelihood that alcohol consumption may impact the individual’s safety.
World Health Organization – Alcohol, Smoking, and Substance Involvement Screening Test, version 2 (WHO-ASSIST 2)20: The WHO-ASSIST 2 was developed as a screening tool to identify potential substance abuse problems. Participants are asked the frequency of use during the past three months of each of nine different groups of substances.
Perceived health status: Question 1 from the Short Form Health Survey (SF-36)21 is asked of participants during each Form II follow-up: “In general, would you say that your health is excellent, very good, good, fair, or poor?” Responses were scored in an ordinal fashion to allow for a non-parametric assessment of changes in perceived health status.
Pain severity and interference: The participant is asked to rate their “usual level of pain over the past four weeks,” using an 11-point numerical rating scale anchored at 0, for “no pain,” and 10, for “pain so severe you could not stand it.” If the participant responds with at least a “1” on this scale, then a second question is asked: “During the past 4 weeks, how much did pain interfere with your normal work, including both work outside the home and housework (or usual activities)?” Participants are asked to respond by choosing one of the following: not at all, a little bit, moderately, quite a bit, or extremely.
Measures collected during the COVID-19 pandemic study period
The same measures that were extracted from the previous SCIMS Form II follow-up interview (above) were collected during the present study to assess changes that might be due to COVID-19 quarantine. All questions were kept the same, except for the AUDIT-C, for which the time frame was changed from “in the last 12 months” to “in the past 3 months.” In addition to these measures, other variables that were collected during the COVID-19 study period are described below.
Generalized Anxiety Disorder – 7 (GAD-7)22: The GAD-7 assesses the presence and frequency of symptoms of anxiety over the last two weeks using 7 questions with responses scored from 0 to 3 and summed for a total score (range: 0–21). Higher scores indicate greater levels of anxiety.
COVID-19-specific questionnaire: A COVID-19-specific questionnaire was created to target limitations that may be of relevance to those with SCI. We reviewed existing surveys related to people with disabilities and articles published during COVID-19 in the general population and used them as guidance in creating our questionnaire.3,23-25
A set of questions were included to inquire the extent to which access to health care information and services, medication refills, medical equipment, transportation, caregiver assistance, and food had been affected during the COVID-19 pandemic compared to before. The survey also included questions regarding whether they had been diagnosed with the virus (including symptom report), the ease of acquiring protective personal equipment (PPE), and changes in their financial situation during the pandemic.
Statistical analysis: Descriptive statistics were calculated for demographic and injury characteristics, as well as outcome variables using parametric (mean, SD) or non-parametric (median, intra-quartile range) methods, as appropriate. Wilcoxon signed-rank tests were used to compare pre- vs during- COVID-19 scores/ratings for SCI-QOL Resilience, PHQ-9, SWLS, perceived health status, pain intensity, and pain interference as a within-subject assessment of change. For those measures that were found to have significantly changed during COVID-19 compared to before COVID-19, we pursued further analyses: Spearman’s rho was used for assessment of correlations among the degree of change (pre- vs during-COVID-19) and level of anxiety (GAD-7) and limitations in access during COVID-19. In addition, because our convenience sample was found to be composed of 51% of individuals approximately 1-year post-injury and 49% of individuals between 5 and 16 years post-injury, we performed post-hoc analyses (Mann–Whitney U-test) to compare potential differences in change scores pre- vs during-COVID for our outcome variables. Significance was set at P < 0.05 for all statistical tests, without correction for multiple tests.
Results
Participants
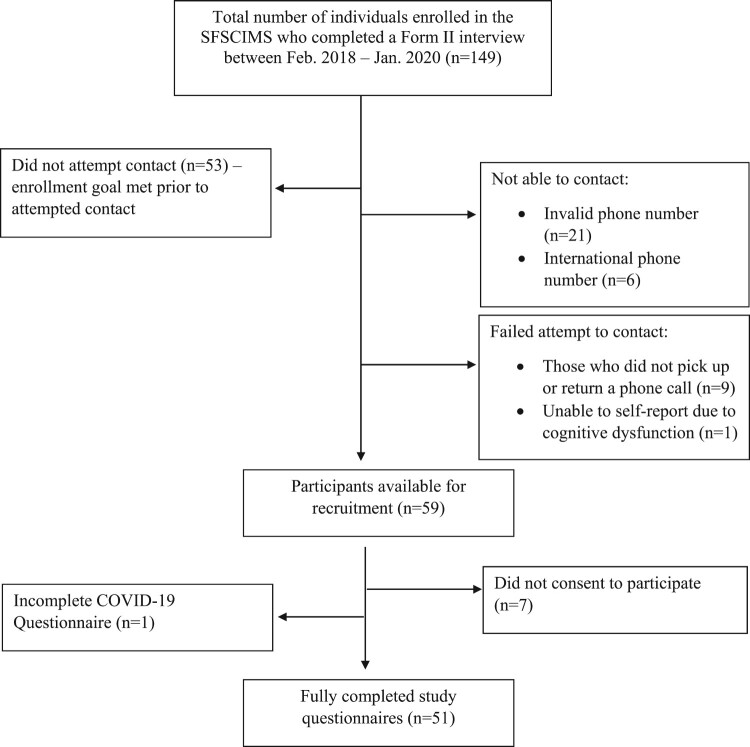
Figure 1 displays the recruitment and enrollment flow chart for the study. A total of 51 individuals who met inclusion criteria were contacted and agreed to complete the phone survey between August 3, 2020, and September 21, 2020. Table 1 presents the demographic and injury information for the survey respondents.
Figure 1.
Recruitment and enrollment of study participants.
Table 1.
Demographic and injury characteristics of study participants.
| Variable | N (%) |
|---|---|
| Total | 51 (100%) |
| Time post injury | |
| 1–2 years | 26 (51%) |
| 5–6 years | 18 (35%) |
| 15–16 years | 7 (14%) |
| Level of injury | |
| Thoracic or Lumbar (paraplegia) | 20 (39%) |
| Cervical (tetraplegia) | 24 (47%) |
| Unknown | 7 (14%) |
| Sex | |
| Male | 48 (94%) |
| Female | 3 (6%) |
| Race | |
| White | 26 (51%) |
| Black | 24 (47%) |
| Other | 1 (2%) |
| Ethnicity | |
| Hispanic | 18 (35%) |
| Non-Hispanic | 33 (65%) |
COVID-19 access limitations
Of the 51 respondents, only one had tested positive for COVID-19 at the time of the study, though he/she reported being asymptomatic (no fever, cough, shortness of breath, chest pain, diarrhea, or other symptoms). Table 2 lists the number and percentages of people who reported changes in access to goods or services, daily activities, and their financial situation due to the COVID-19 pandemic and associated restrictions. Many subjects reported at least some limitation in access to necessities: 78% of participants reported limited access to their regular activities, 40% to healthcare information and services, 38% to PPE, 37% to food/groceries, and 34% to medication refills.
Table 2.
Response frequency related to changes due to COVID-19.
| “Compared to before the COVID-19 pandemic … ” (n (%)) | ||||||
|---|---|---|---|---|---|---|
| How difficult has it been to … | Extremely difficult | Somewhat difficult | A little difficult | Same | Easy | Not applicable |
| get health care info | 8 (15.7%) | 0 (0%) | 11 (21.6%) | 27 (52.9%) | 2 (3.9%) | 3 (5.9%) |
| get med refills | 4 (7.8%) | 0 (0%) | 12 (23.5%) | 29 (56.9%) | 2 (4%) | 4 (7.8%) |
| acquire PPE | 4 (7.8%) | 9 (17.6%) | 5 (9.8%) | 29 (56.9%) | 4 (7.8%) | |
| acquire medical equipment | 2 (3.9%) | 7 (13.7%) | 8 (15.7%) | 0 (0%) | 13 (25.5%) | 21 (41.2%) |
| access food/groceries/ household supplies | 2 (3.9%) | 7 (13.7%) | 10 (19.6%) | 31 (60.8%) | 1 (2.0%) | 0 (0%) |
| access transportation for med appointments | 1 (2.0%) | 7 (13.7%) | 4 (7.8%) | 30 (58.8%) | 2 (4.0%) | 7 (13.7%) |
| How much have your daily activities or routines changed? | Extreme Amount | Moderate Amount | A little | No change | Don’t know | |
| 9 (17.6%) | 15 (29.4%) | 16 (31.4%) | 11 (21.6%) | 0 (0%) | ||
| How much has contact with your caregiver changed? | Significantly less contact | Slightly less contact | No change | More contact | Do not have a caregiver | |
| 2 (3.9%) | 5 (9.8%) | 19 (37.3%) | 0 (0%) | 25 (49.0%) | ||
| How much has your financial situation changed? | Significantly worse | Moderately worse | Slightly worse | No change | Improved | Don’t know |
| 3 (5.9%) | 5 (9.8%) | 5 (9.8%) | 37 (72.5%) | 1 (2%) | 0 (0%) | |
Psychological and physical health
Scores on all measures of psychological function and severity of other health conditions at the time of the study, and at the time of the previous Form II interview (pre-COVID-19), are reported in Table 3. Resilience (SCI-QOL Resilience t-scores) was significantly decreased (P = 0.010) and depressive symptoms (PHQ-9 scores) were significantly increased (P = 0.004) compared to data collected pre-COVID-19. However, ratings of overall satisfaction with life were unchanged (P = 0.861). Anxiety symptoms collected via the GAD-7 during COVID-19 revealed that 30% of those interviewed had mild to severe anxiety. Because no measures of anxiety are included in Form II of the National SCIMS Database, we could not compare pre- vs during- COVID-19 anxiety symptoms. Instead, participants were also asked to report their perceived change in anxiety: 51% of participants reported they felt more anxious during the pandemic compared to prior (8% “significantly more anxious” and 43% “slightly more anxious”).
Table 3.
Psychological and physical heath pre-COVID-19 and during-COVID-19.
| Variable | Pre-COVID-19 (prior Form II interview, within 2 years of COVID-19) | During COVID-19 (Aug – Sept 2020) | Wilcoxon signed-rank test: Z (P-value) |
|---|---|---|---|
| SCI-QOL Resilience subscale t-score | Mean: 55.4; SD: 8.4 Median: 53.5; IQR: 17 |
Mean: 51.5; SD: 8.8 Median: 50.7; IQR: 14 |
2.57 (0.010)a |
| PHQ-9 | Mean: 2.3; SE: 3.1 Median: 1.0; IQR: 3 |
Mean: 4.2; SD: 4.3 Median: 3.5; IQR: 6 |
2.89 (0.004)a |
| Minimal depressive symptoms N (%) | 44 (86%) | 30 (58%) | |
| Mild symptoms | 6 (12%) | 13 (26%) | |
| Moderate symptoms | 1 (2%) | 5 (10%) | |
| Moderately-severe symptoms | 0 (0%) | 3 (6%) | |
| Severe symptoms | 0 (0%) | 0 (0%) | |
| SWLS | Mean: 17.8; SD: 6.0 Median: 18.0; IQR: 9 |
Mean: 17.2; SD: 6.6 Median: 17; IQR:12 |
0.175 (0.861) |
| GAD-7 | NA (not collected) | Mean: 3.3; SD: 4.6 Median: 1; IQR: 5 |
NA |
| None or minimal symptoms | 36 (71%) | ||
| Mild symptoms | 10 (20%) | ||
| Moderate symptoms | 3 (6%) | ||
| Severe symptoms | 2 (4%) | ||
| AUDIT-C | Mean: 1.2; SD: 1.8 Median: 0; IQR: 2 |
Mean: 1.3; SD: 1.8 Median: 0; IQR: 3 |
0.452 (0.651) |
| No problem | 49 (96%) | 48 (94%) | |
| Hazardous drinking or abuseb | 2 (4%) | 3 (6%) | |
| WHO-ASSIST 2c | |||
| Tobacco use | 8 (16%) | 6 (12%) | |
| Cannabis | 11 (22%) | 10 (20%) | |
| Sedatives | 2 (4%) | 3(6%) | |
| Opioids | 1(2%) | 4(8%) | |
| Other | 1(2%) | 1(2%) | |
| Pain severity | Mean: 5.0; SD: 3.0 Median: 6.0; IQR:3 |
Mean: 4.4; SD: 3.3 Median: 5.0; IQR:7 |
0.842 (0.400) |
| Pain interference with work or daily activities | Mean: 1.8; SD: 1.3 Median: 2; IQR: 2 |
Mean: 1.2; SD: 1.2 Median: 1; IQR: 2 |
3.10 (0.002)a |
| Perceived health status | Mean: 2.7; SD: 0.77 Median: 2; IQR: 1 |
Mean: 2.7; SD:1.0 Median: 3; IQR: 1 |
−0.102 (0.919) |
| Excellent | 4 (7.8%) | 6 (11.8%) | |
| Very good | 11 (21.6%) | 13 (25.5%) | |
| Good | 30 (58.8%) | 22 (43.1%) | |
| Fair | 6 (11.8%) | 8 (15.7%) | |
| Poor | 0 (0%) | 2 (3.9%) |
p < 0.05.
hazardous drinking: AUDIT-C score ≥ 4 for men, AUDIT-C score ≥ 3 for women.
Because reported prevalence and frequency of use was low, data are presented for the total number of people who endorsed any use ≥ 1 during the past 3 months.; Cocaine, amphetamines, inhalants, and hallucinogens were not reported as being used either before or during-COVID by any participants (0%), thus these substances were not listed in the table.
There were no differences in the use of alcohol (AUDIT-C) and other substances (WHO-ASSIST 2) when comparing pre-COVID-19 to during-COVID-19 responses across our sample. Similarly, ratings of perceived health status before- vs during-COVID-19 did not change, which was consistent with results from the direct question asking participants to report their perceived degree of change in health due to COVID-19 restrictions (21.6% said health was better, 64.3% said health was the same, and 12.9% said health was worse). Differences in ratings of pain intensity were not significant, but the impact of pain on work or daily activities was significantly decreased during COVID-19 (during-COVID-19 median = 1 (“a little bit”) vs. pre-COVID-19 median = 2 (“moderately”); P = 0.002).
Comparison of changes in health between those who were 1–2 years post-injury and those who were at least 5 years post-injury
Because our convenience sample resulted in 51% of the sample being between 1 and 2 years post-injury, and 49% being injured at least 5 years prior, we investigated whether changes in the study outcome variables differed between these two groups. Mann–Whitney U tests indicated that there were no significant differences in the degree of change (pre-COVID-19 vs during-COVID-19) for any of the outcome variables of interest (resilience, depressive symptoms, satisfaction with life, pain, pain impact, wperceived health status), with the exception of alcohol consumption. The group of individuals who were 1–2 years post-injury had a greater change in AUDIT-C scores (alcohol use) than the ≥ 5-year post-injury group (P = 0.012). Despite the significant difference found in the AUDIT-C change scores across these two groups, the rate of problematic drinking was relatively low across both groups. In the recently-injured group (n = 26), 1 individual scored within the hazardous drinking range (≥ 4 for men, and ≥ 3 for women) on the AUDIT-C prior to COVID-19, and 2 scored in this range during COVID-19. This trend was reversed in those who were injured 5 or more years: of the 25 individuals in this group, 5 fell into the hazardous drinking range prior to COVID-19, and 4 were in this range at the time of the study (during COVID-19).
Associations among changes in physical and mental health and COVID-19 access and levels of anxiety
For those measures that showed significant changes across the full sample during COVID-19 compared to before COVID-19 (PHQ-9, SCI-QOL Resilience, and pain interference ratings), we assessed their association with participants’ reports of access limitations due to COVID-19 restrictions (Table 4). Increases in PHQ-9 scores were significantly associated with symptoms of anxiety (GAD-7) and greater reported limitations in access to health care information and services, PPE, food/groceries, and changes in daily activities, but not with access to medication refills, transportation, or caregiver services. Decreases in SCI-QOL Resilience subscores were significantly associated with difficulties in access to food/groceries, but none of the other access variables queried, or to anxiety. Changes in the impact of pain on work or activities were significantly correlated with access to transportation.
Table 4.
Spearman’s rho correlations (and P-value) among physical and mental health and access limitations during COVID-19.
| Limitations in access to: | ||||||||
|---|---|---|---|---|---|---|---|---|
| GAD-7 | Health care info | Med refills | PPE | Food/ groceries | Transpor-tation | Daily Activities | Caregiver | |
| Change in PHQ-9 score | 0.400 (0.004)* | −0.337 (0.019)* | −0.204 (0.168) | −0.311 (0.033)* | −0.331 (0.018)* | −0.282 (0.064) | −0.292 (0.038)* | −0.223 (0.116) |
| Change in SCI-QOL Resilience subscore | −0.267 (0.061) | 0.276 (0.060) | 0.283 (0.056) | 0.098 (0.518) | 0.298 (0.036)* | 0.135 (0.386) | 0.128 (0.377) | 0.109 (0.451) |
| Change in pain interference rating | 0.065 (0.650) | −0.158 (0.283) | −0.223 (0.131) | −0.205 (0.167) | −0.047 (0.743) | −0.316* (0.037) | −0.189 (0.185) | −0.112 (0.436) |
Discussion
Currently, there is limited information on the impact of COVID-19 and social distancing/isolation on vulnerable populations, such as individuals with SCI. To our knowledge, this is the first study that has compared “baseline” (i.e. pre-COVID-19 pandemic) and current (i.e. during COVID-19 pandemic) measures of mental health in individuals with SCI. In addition, the questions included in our survey provide valuable information about associations between access to necessities and mental health during the current COVID-19 pandemic. This information can help provide better care and support to individuals with an SCI during this time and better prepare the SCI community to lessen the impact of future public health emergencies on psychological health.
We found that 33.3% and 23.5% of individuals in our geographic and time-limited study sample reported at least some increased difficulty in accessing medical supplies and transportation. This is similar to the results of Stillman et al.,3 who reported that 42% and 21.3% of their sample of individuals with SCI had concerns about access to these necessities during COVID-19.
Our study also reported difficulty in obtaining health care information (37.3%), medication refills (31.3%), access to food/groceries/household supplies (37.2%), and PPE (35.2%). These limitations may be explained by shortages of supplies,26 decreased availability of medical appointments,27,28 price surges, and limitations on in-person interactions that are needed to acquire these supplies. For those individuals who reported extreme difficulties in accessing health care information (15.7%), medication refills (7.8%), and medical equipment (3.9%), these barriers to access represent potentially life-threatening situations.
Compared to previous epidemics and environmental disasters, this pandemic has been predicted to result in high levels of anxiety and depression.27 Despite our small sample size, we found both significant increases in depressive symptoms and significant decreases in resilience, suggesting convergent validity across these measures and likely reflect a true change in psychological function across the target population. The impact of these changes, however, was not mimicked by significant changes in scores on the Satisfaction With Life Scale. This may be due to insufficient sensitivity of the SWLS to short-term changes, or due to its only moderate association with mental health/mood when assessed in the SCI population.18 Levels of anxiety and depressive symptoms in individuals with SCI in the South Florida region during the time of social isolation are similar to those that have been reported in the general population during the same period of COVID-19 social isolation. Studies from the United States, China, and Australia28-30 have reported moderate-to-severe depressive symptoms in 16.5% to 22.1% of the general population during COVID-19, similar to the 16% of our sample that fell into these depressive categories. This was complemented by our finding that the severity of depressive symptoms was significantly higher when testing within-subject changes in PHQ-9 scores during the pandemic compared to pre-pandemic scores (P = 0.004). When examining potential reasons for changes in psychological status during the COVID-19 pandemic, we found several significant correlations indicating that increased restriction to access (healthcare information and services, food, PPE, normal activities) may have impacted depressive symptoms.
With regard to anxiety, studies in the general population have reported 14%, 20.5%, and 28.8%28–30 of people with moderate-to-severe anxiety symptoms during this time of COVID-19 mitigation measures, whereas only 10% of our sample had anxiety that fell into the moderate-to-severe range. The lower levels of anxiety in our sample of individuals with SCI may represent a higher baseline level of flexibility in people after an SCI, as they have had to adapt to many changes and access limitations in their life due to their physical disability. Thus, the additional impact of stressors due to COVID-19 may not impart the same level of anxiety that it does in the general population.
Results of the statistically significant decreased levels of resilience compared to pre-pandemic levels in our sample are not surprising given the operational definition of resilience that was used to develop the SCI-QOL Resilience subscale. Resilience was defined as “the process of successfully adapting to significant sources of stress or trauma, facilitated by an individual's psychological resources, life experiences, and environment”.10,31 Thus, decreases in resilience may be thought of as resulting from the decrease in psychological resources (i.e. increased depressive symptoms) and the reduction in environmental supports (e.g. decreased access to health care information, access to food/groceries) that occurred during the COVID-19 pandemic. In our assessments of alcohol (AUDIT-C) and other substance use (WHO-ASSIST2), we did not find increases in consumption of most substances during COVID-19 compared to before COVID-19, with an exception for opioids, which was reported by 1 person before the pandemic, and increased to 4 people during COVID-19. In recent data reported by the CDC, 13.3% of individuals in the general population started using or increased the use of, different substances as coping mechanisms during the pandemic.32 Our results suggest that individuals with SCI may not be as likely to increase substance and alcohol use as that reported for the general population. However, despite low levels of alcohol use overall in our sample, there was a small, but significantly greater increase in alcohol use for more newly injured individuals compared to those injured 5 or more years.
With regard to chronic pain and its impact, a significant change in pain intensity rating was not found, but a significant decrease in pain interference on work or usual activities (P = 0.002) was found. Given the tight link between chronic pain and psychological function,33 it is somewhat unexpected that severity of pain did not increase during the pandemic compared to before. In fact, the impact of pain on work or activities significantly decreased during this time of heightened psychological distress. Unfortunately, questions directly addressing the reasons for changes in pain impact were not collected in this study. Possible explanations for these findings are that activities outside of the home were limited, which may have mitigated the impact of mood to increase some types of pain (e.g. that due to muscle strain or overuse), and, further, that because individuals may have engaged in less work or were able to work from home, the perceived impact of pain on this activity was reduced.
Overall, results from this study contribute to the understanding of psychological health related to the COVID-19 pandemic and its impact on access to basic needs in the SCI population. However, the interpretation of these results should be considered with several limitations in mind. First, the small sample size (n = 51), with a higher percentage of males (94%) than is representative of the general population of individuals with SCI in the US (78%),34 and the restricted geographic area (South Florida), limits the generalizability of our results. While the small sample size may have limited our ability to detect changes for some measures due to reduced statistical power (increased probability of Type II error), we were still able to show changes in depressive symptoms and resilience and relate these changes to limitations in access to necessary supplies, information, and activities. Second, we collected data during a small snapshot of time, between 8/3/2020 and 9/21/2020, which clearly limits the implications of our study, but were necessary given the uncertainty of the duration of the imposed restrictions. Since the time of our interviews, the COVID-19 pandemic has continued to impose limitations in daily life, and this long duration of at least moderate social isolation may further impact psychological health to a greater extent than is reported here. Limited information about COVID-19 risk and management for persons with SCI had been made available to consumers and it is unclear whether those with SCI felt at high risk.6 Fourth, some of the questions that were used to assess perceived changes in daily activities and contact with caregivers did not have balanced response categories, with more response options geared toward negative responses. This may have unintentionally biased participant responses. Finally, the use of a convenience sample introduces a bias in reporting. It is possible that individuals who had more psychological difficulties during the period of the study were less likely to answer their phones and thus we could not obtain data from them. Consequently, our results may reflect an under-reporting of the severity of the impact that the COVID-19 epidemic has had on the well-being of individuals in the SCI community.
The COVID-19 virus created an unexpected social situation that many people have never experienced before. Limitations to basic needs and face-to-face communication exacerbated challenges in access for persons with disabilities. Our results show increased levels of depression and decreased levels of resilience compared to pre-pandemic levels in individuals with SCI. The results of this study can help the SCI community recognize the need for enhanced access, outreach, information, and social support during this time and in preparing for emergencies, epidemics, and natural disasters in the future. To meet these needs, infrastructure aimed at enabling the rapid rollout of telehealth and internet-based support group services and at acquiring and distributing healthcare supplies (e.g. gloves, catheters, medications, PPE), should be developed within local communities to better serve their vulnerable populations.
Acknowledgments
We would like to thank Eleuterio Baliwis, RN, BSN for assistance with participant recruitment and data collection.
Funding Statement
The contents of this manuscript were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90SI5023). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Disclaimer statements
Data availability statement The data that support the findings of this study are available from two sources: (a) “Baseline” or pre-COVID-19 data are available from the National SCI Statistical Center, as part of the NIDILRR-supported SCI Model Systems [https://www.nscisc.uab.edu/Research/NSCISC_DatabasePublicUse]; (b) Data collected specifically for this study (during-COVID-19 data) are available from the corresponding author, ERF, upon reasonable request.
Statement of ethics This study was reviewed and approved by the Institutional Review Board of the University of Miami. Study number: 20100501. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Conflict of interests The authors attest that they have no financial or other conflicts of interest.
References
- 1.Ahn DG, Shin HJ, Kim MH, Lee S, Kim HS, Myoung J, et al. . Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel Coronavirus Disease 2019 (COVID-19). J Microbiol Biotechnol 2020;30(3):313–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Javed B, Sarwer A, Soto EB, Mashwani ZU.. The coronavirus (COVID-19) pandemic's impact on mental health. Int J Health Plann Manage 2020;35(5):993–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stillman MD, Capron M, Alexander M, Di Giusto ML, Scivoletto G.. COVID-19 and spinal cord injury and disease: results of an international survey. Spinal Cord Ser Cases 2020;6(1):21. doi: 10.1038/s41394-020-0275-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kennelly MJ. Caring for people with spinal cord injury in the time of COVID-19: redefining the meaning of “essential”. J Spinal Cord Med 2020;43(5):563–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexander M. Pandemics, climate change, and disability related to SCI. Spinal Cord Ser Cases 2020;6(1):36. doi: 10.1038/s41394-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henzel MK, Shultz JM, Dyson-Hudson TA, Svircev JN, DiMarco AF, Gater Jr DR.. Initial assessment and management of respiratory infections in persons with spinal cord injuries and disorders in the COVID-19 era. J Am Coll Emerg Physicians Open 2020;1(6):1404–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams R, Murray A.. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil 2015;96(1):133–40. [DOI] [PubMed] [Google Scholar]
- 8.Le J, Dorstyn D.. Anxiety prevalence following spinal cord injury: a meta-analysis. Spinal Cord 2016;54(8):570–8. [DOI] [PubMed] [Google Scholar]
- 9.Goldmann E, Galea S.. Mental health consequences of disasters. Annu Rev Public Health 2014;35:169–83. [DOI] [PubMed] [Google Scholar]
- 10.Victorson D, Tulsky DS, Kisala PA, Kalpakjian CZ, Weiland B, Choi SW.. Measuring resilience after spinal cord injury: development, validation and psychometric characteristics of the SCI-QOL Resilience item bank and short form. J Spinal Cord Med 2015;38(3):366–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spitzer RL, Kroenke K, Williams JB.. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. primary care evaluation of mental disorders. Patient Health questionnaire. JAMA 1999;282(18):1737–44. [DOI] [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB.. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams RT, Heinemann AW, Neumann HD, Fann JR, Forchheimer M, Richardson EJ, et al. . Evaluating the Psychometric Properties and responsiveness to change of 3 depression measures in a sample of persons With Traumatic Spinal Cord injury and major depressive disorder. Arch Phys Med Rehabil 2016;97(6):929–37. [DOI] [PubMed] [Google Scholar]
- 14.Titman R, Liang J, Craven BC.. Diagnostic accuracy and feasibility of depression screening in spinal cord injury: A systematic review. J Spinal Cord Med 2019;42(sup1):99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amtmann D, Bocell FD, Bamer A, Heinemann AW, Hoffman JM, Juengst SB, et al. . Psychometric Properties of the Satisfaction With Life Scale in people With Traumatic brain, Spinal Cord, or burn injury: A National Institute on disability, Independent Living, and Rehabilitation Research Model System study. Assessment 2019;26(4):695–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schumaker JF, Shea JD, Monfries MM, Groth-Marnat G.. Loneliness and life satisfaction in Japan and Australia. J Psychol 1993;127(1):65–71. [DOI] [PubMed] [Google Scholar]
- 17.Zanon C, Bardagi MP, Layous K, Hutz CS.. Validation of the Satisfaction with Life Scale to Brazilians: evidences of measurement noninvariance across Brazil and US. Soc Indic Res 2014;119(1):443–53. [Google Scholar]
- 18.Post MW, van Leeuwen CM, van Koppenhagen CF, de Groot S.. Validity of the life Satisfaction questions, the life Satisfaction questionnaire, and the Satisfaction With Life Scale in persons With Spinal Cord injury. Arch Phys Med Rehabil 2012;93(10):1832–7. [DOI] [PubMed] [Google Scholar]
- 19.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA.. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. ambulatory care Quality improvement project (ACQUIP). Alcohol Use Disorders Identification test. Arch Intern Med 1998;158(16):1789–95. [DOI] [PubMed] [Google Scholar]
- 20.The alcohol, Smoking and substance Involvement Screening test (ASSIST): development, reliability and feasibility. Addiction 2002;97(9):1183-94. [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Kosinski M, Keller SD.. A 12-item short-form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Kroenke K, Williams JB, Löwe B.. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 23.Drum CE, Ditsch J, Oberg A, Cooper K, Carlin R.. COVID-19 & adults with disabilities: health and health care access- comparative analysis of online survey results By type of disability. Rockville (MD: ): American Association on Health and Disability; 2020. [Google Scholar]
- 24.Emerson E, Stancliffe R, Hatton C, Llewellyn G, King T, Totsika V, et al. . The impact of disability on employment and financial security following the outbreak of the 2020 COVID-19 pandemic in the UK. J Public Health (Oxf) 2021;43(3):472–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karlsson U, Fraenkel C-J.. Complete protection from covid-19 is possible for health workers. Br Med J 2020;370:m2641. doi: 10.1136/bmj.m2641. [DOI] [PubMed] [Google Scholar]
- 26.Ranney ML, Griffeth V, Jha AK.. Critical supply shortages - The need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med 2020;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 27.Galea S, Merchant RM, Lurie N.. The mental health consequences of COVID-19 and physical distancing: The Need for prevention and early intervention. JAMA Intern Med 2020;180(6):817–8. [DOI] [PubMed] [Google Scholar]
- 28.Newby JM, O'Moore K, Tang S, Christensen H, Faasse K.. Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One 2020;15(7):e0236562. doi: 10.1371/journal.pone.0236562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. . Immediate psychological responses and associated factors during the Initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi EPH, Hui BPH, Wan EYF.. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 2020;17(10):3740. doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Windle G, Bennett KM, Noyes J.. A methodological review of resilience measurement scales. Health Qual Life Outcomes 2011;9(1):8. doi: 10.1186/1477-7525-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Czeisler M, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. . Mental health, substance Use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69(32):1049–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tran J, Dorstyn DS, Burke AL.. Psychosocial aspects of spinal cord injury pain: a meta-analysis. Spinal Cord 2016;54(9):640–8. [DOI] [PubMed] [Google Scholar]
- 34.National Spinal Cord Injury Statistical Center . Facts and figures at a glance. Birmingham (AL: ): University of Alabama at Birmingham; 2021. [Google Scholar]