Abstract
Torque control of maxillary incisors is very important in maxillary protrusion patients with first premolars extraction, but the efficacy of maxillary incisor retraction of clear aligners is still controversial now. This retrospective study was aimed to compare the retraction effects between Damon Q and Invisalign® appliances in patients with first premolar extractions. 59 patients (33 cases with Damon Q and 26 cases with Invisalign®) with first premolar extraction were selected in this study. Subsequently, patients of each group were allocated into three subgroups according to the pretreatment value of U1-NA (°). The retraction effects of maxillary incisors and upper lips were accessed by the variations of cephalometric, overbite and overjet measurements. Treatment duration with Invisalign® (31.4 ± 6.4 months) was longer than Damon Q (27.7 ± 6.3 months) (P = .03). The angular measurements, U1-NA (°) and U1-SN (°) showed more lingual crown inclinations in Invisalign® group than Damon Q group (P ≤ .04). When evaluating linear measurements, the retractions of the maxillary incisors and upper lip positions showed no significant differences (P ≥ .13). Invisalign® group also showed more lingual crown retractions and labial root deviations compared to Damon Q group in subgroup Ⅲ (P ≤ .037). As regards to the molar relationship, Invisalign® displayed less Class Ⅰ molar relationship than Damon Q group. The increased overbite of anterior incisors was also showed in the Invisalign® treatment group (P ≤ .047). Invisalign® was not sufficiently effective in retracting maxillary incisors compared with Damon Q appliances. Invisalign® led to more lingual inclination movement and increased overbite.
Keywords: Damon Q, extraction, Invisalign®, maxillary incisor retraction
1. Introduction
Nowadays, more than 16.8% of patients seek orthodontic treatment due to protruded maxillary incisors and a convex profile.[1–3] For patients with dental protrusion, the extraction of first premolars can reduce the protrusion of maxillary incisors, alleviate the incompetent upper lips, and achieve a favorable straight profile.[2,4,5] Torque control of maxillary incisors is very important for achieving good results, such as anterior aesthetic. Conventional fixed appliances have been adopted as effective tools to manage the reposition of protruded incisors.[6,7] Self-ligating brackets (SLBs) were designed to reduce bracket/wire friction during mechanical sliding[8] and therefore facilitate alignment,[9] increase intervals between activations, and reduce chairside time.[10] Among SLBs, Damon Q was proven to produce the lowest friction[11] and the largest corrections in the protrusion directions.[12]
With the technology developed, clear aligners have become increasingly common choices because of the growing number of adult patients asking for aesthetic and comfortable alternatives.[13] However, the efficacy of maxillary incisor retraction of clear aligners, especially for maxillary protrusion patients, is still controversial now. Rossini et al and Li et al[14,15] reported that Invisalign® was not sufficiently effective in retracting maxillary incisors compared with traditional fixed appliances in 2015. Sfondrini et al[16] claimed that Invisalign® was as effective as self-ligating appliances (Damon Q and 3M) in incisor retraction for non-extraction patients in 2018. Dai et al[17] found Invisalign® resulted in more teeth inclination and less retraction than predicted for maxillary central incisors in 2019.
To investigate the maxillary incisors retraction effect of Invisalign® and Damon Q systems, patients with first premolars extraction were included in this retrospective study. Treatment effects were evaluated with the change of cephalometric, overbite and overjet measurements. The crown and root retraction of maxillary central incisors and upper lips position change were further accessed in three subgroups according to the pretreatment maxillary incisors’ inclination. The result from our study should more evidence for Invisalign® treatment in the maxillary protrusion patients with first premolars extraction.
2. Materials and methods
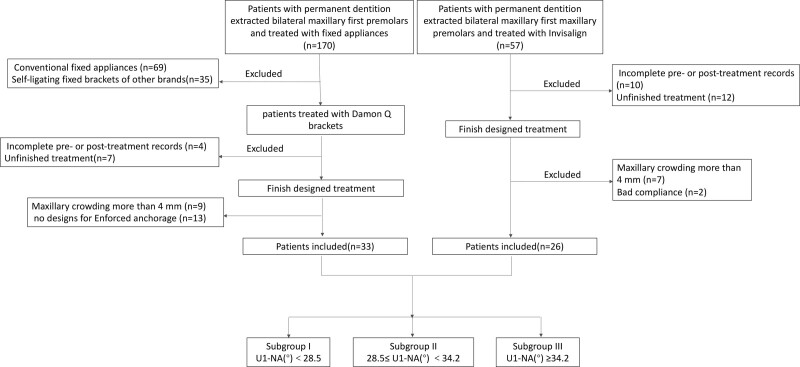
Our research protocol was ethically approved by the Ethical Standards of Nanjing Stomatological Hospital, Medical School of Nanjing University (NJSH-2021NL-87). Sixty-one patients from the Orthodontic Department of Nanjing Stomatological Hospital, Medical School of Nanjing involved in this study (Fig. 1). Informed consent was obtained from each participant. Thirty-three patients were treated with Damon Q, and twenty-six were treated with Invisalign®.
Figure 1.
The sampling flow chart.
2.1. Patients and eligibility criteria
Patient eligibility criteria: ANB (°): 2-8 and U1-NA (°): ≥ 22.8; Extraction of bilateral maxillary first premolars and mandibular first or second premolars; Mild maxillary crowding (<4 mm); and Complete records. Exclusion criteria: Craniofacial defects, syndromes or skeletal deformities; History of trauma on the maxillary teeth; and History of orthodontic treatment.
In order to analyze the retraction effects detailly, all patients were allocated into 3 subgroups according to the protrusion degree of maxillary incisors. The allocation was based on the normal mean (22.8) and standard deviation (5.7) obtained for U1-NA (°). Subgroup I: 22.8 ≤ U1-NA (°) < 28.5 (Mean + 1 SD); Subgroup II: 28.5 (Mean + 1 SD) ≤ U1-NA (°) < 34.2 (Mean + 2 SD); Subgroup III: U1-NA (°) ≥ 34.2 (Mean + 2 SD). The sampling process is shown in Figure 1.
2.2. Treatment design
Damon Q: 0.022 × 0.028-inch slot brackets with standard prescription torque (+15° and +6° for maxillary central and lateral incisors, respectively) and 0.019 × 0.025-inch stainless steel wire were used to retract the maxillary incisors. Transpalatal arches and maxillary second molars were included to reinforce anchorage.
Invisalign®: All aligners (Align Technology, San Jose, CA) were designed and manufactured under the G6 protocol. Distal bodily movement of the canines was followed by the inclination of the maxillary anterior teeth. The torque expression was accomplished by Power Ridge technology. The Invisalign® was instructed for wearing more than 22 hours a day. All patients were guided to change each aligner for two weeks and use chewies every day.
2.3. Lateral cephalometric radiographs
Lateral cephalometric radiographs standardized with head posture and maximal intercuspation were taken by an X-ray cephalograph (ORTHOCEPH OC200 D; Instrumentarium Dental, Tuusula, Finland). The computerized cephalometric measurements were performed using Dolphin Imaging software (Dolphin Imaging & Management Solutions, 11.5, Oakdale, CA).
U1-NA (°), U1-NA (mm), U1-SN (°) and maxillary lip to E-plane (mm) were selected to evaluate the maxillary incisors retraction effect of Damon Q and Invisalign®. The root retractions of maxillary central incisors were evaluated with the distance to the NA plane of apical point (U1R-NA (mm)). If the variation of U1R-NA (mm) is larger than 0, it means the root has been lingually retracted. If the variation of U1R-NA (mm) shows negative numbers, it means the root moved labially.
The measurements were performed on all of the images independently by two investigators (Jiping Chen and Lu Zhang). Intraclass correlation coefficient (ICC) tests were used to assess the intraoperator and interoperator errors. The average ICC for interrater reliability was 0.88, and the average ICCs for intrarater reliability were 0.93 and 0.94 for the two investigators respectively.
2.4. Statistical analysis
Statistical analysis was performed with SPSS® Statistics 24 software (SPSS Statistics, version 24.0; IBM, Armonk, NY). The normality and homogeneity of the data were tested with the Shapiro–Wilk and Levene tests. The chi-square test was used to evaluate the distributions of age and sex in each group. Differences between the two groups with respect to skeletal pattern, labiolingual inclination of the maxillary central incisors, and facial profile before and after orthodontic treatment as well as their variations were compared by Independent samples t test. The Mann–Whitney U test was adopted if normality or homogeneity of variables was not met. Multiple comparisons of the cephalometric measurements among subgroups were performed by ANOVA with the LSD post hoc test. The Kruskal–Wallis test with the Nemenyi post hoc test was adopted if normality or homogeneity of variables was not met. For all tests, the significance level was set at P < .05.
3. Results
As shown in Tables 1 and 2, the demographic distributions and cephalometric measurements (T0) before treatment showed no significant difference (P ≥ .06) between Damon Q and Invisalign® groups, which confirms the two groups were matched for age, sex and malocclusion. Compared with 27.7 ± 6.3 months for Damon Q group, longer treatment duration was obtained for Invisalign® group (31.4 ± 6.4 months) (P = .03) (Table 1).
Table 1.
Demographic composition of the study sample.
| Damon Q (n = 33) | Invisalign® (n = 26) | P value | |
|---|---|---|---|
| Age (yr) | 21.4 ± 6.6 | 23.8 ± 7.1 | .20 |
| Gender | |||
| Male | 7 | 5 | .85 |
| Female | 26 | 21 | |
| Treatment duration (mo) | 27.7 ± 6.3 | 31.4 ± 6.4 | .03 |
The age and sex distribution for Damon Q and Invisalign® were matched and showed no significant difference (P = .20). The treatment duration of Invisalign® was 31.4 ± 6.4 mo, statistically longer than Damon Q (P = .03). Age was expressed in ages and treatment duration was expressed in months. Independent t test and chi-square test were used separately to evaluate the distribution of different parameters between Damon Q and Invisalign®.
Table 2.
Descriptive statistics of pretreatment (T0), post-treatment (T1) and treatment variations (T0-T1).
| Damon Q | Invisalign® | Significance between | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| T0① | T1② | T0-T1③ | T0④ | T1⑤ | T0-T1⑥ | ①④ | ②⑤ | ③⑥ | |||
| SNA (°) | 82.00 ± 3.64 | 81.49 ± 3.60 | 0.51 ± 0.81 | 82.94 ± 2.88 | 82.39 ± 2.53 | 0.55 ± 2.07 | 0.15* | 0.29 | 0.84* | ||
| SNB (°) | 76.59 ± 3.32 | 76.36 ± 3.37 | 0.23 ± 0.91 | 78.79 ± 4.71 | 77.38 ± 3.26 | 1.41 ± 3.20 | 0.08 | 0.24 | 0.19* | ||
| ANB (°) | 5.41 ± 2.05 | 5.17 ± 1.95 | 0.24 ± 0.84 | 4.91 ± 2.04 | 5.02 ± 1.76 | −0.10 ± 1.87 | 0.97* | 0.76 | 0.33* | ||
| MP-SN (°) | 35.77 ± 7.11 | 35.89 ± 7.09 | −0.12 ± 2.00 | 37.33 ± 8.82 | 36.71 ± 7.08 | 0.62 ± 5.36 | 0.69* | 0.66 | 0.96* | ||
| Y-axis (°) | 72.13 ± 3.83 | 71.96 ± 5.33 | 0.17 ± 3.11 | 72.82 ± 5.63 | 73.00 ± 4.40 | −0.18 ± 2.91 | 0.78* | 0.97* | 0.97* | ||
| MP-FH (°) | 29.87 ± 7.54 | 30.02 ± 7.68 | −0.15 ± 4.21 | 32.64 ± 9.53 | 30.77 ± 8.82 | 1.87 ± 8.16 | 0.32* | 0.73 | 0.99* | ||
| U1-NA (°) | 32.29 ± 5.03 | 15.92 ± 6.25 | 16.38 ± 5.22 | 34.76 ± 7.51 | 14.26 ± 6.12 | 20.50 ± 7.88 | 0.25 | 0.31 | 0.03 | ||
| U1-NA (mm) | 8.10 ± 1.80 | 2.50 ± 2.26 | 5.59 ± 2.28 | 9.19 ± 2.51 | 2.47 ± 2.23 | 6.72 ± 2.41 | 0.06 | 0.96* | 0.13* | ||
| U1R-NA (mm) | 4.21 ± 1.59 | 3.85 ± 1.50 | −0.35 ± 1.35 | 4.14 ± 2.40 | 3.21 ± 1.90 | −0.98 ± 2.01 | 0.96 | 0.15 | 0.16 | ||
| U1-SN (°) | 114.29 ± 5.38 | 97.44 ± 6.35 | 16.85 ± 5.23 | 117.68 ± 8.11 | 96.66 ± 6.82 | 21.02 ± 8.62 | 0.07 | 0.65 | 0.04 | ||
| Maxillary Lip to E-plane (mm) | 1.95 ± 2.23 | -0.70 ± 2.61 | 2.02 ± 1.51 | 2.04 ± 2.64 | -0.32 ± 1.68 | 2.36 ± 2.11 | 0.88 | 0.66 | 0.47 | ||
There was no significant difference between two groups in skeletal, dental and soft tissue parameters in pretreatment (T0). More lingual crown inclinations were obtained in Invisalign® group compared to Damon Q group (P ≤ .04) when evaluating angular variations of U1-NA (°) and U1-SN (°). Linear retractions of the maxillary incisors and upper lip positions for both groups showed no significance (P ≥ .13).
Independent t test and Mann–Whitney U test were used.
3.1. Comparisons of cephalometric measurements pre- and post-treatment for Damon Q and Invisalign® group
The pretreatment skeletal, dental and soft tissue parameters for Damon Q and Invisalign® group displayed no significance (Table 2). When evaluating angular variations of U1-NA (°) and U1-SN (°), Invisalign® group showed more lingual crown inclinations than Damon Q group (P ≤ .04) (Table 2). The inclination changes of U1-NA (°) ranged from 29.3° to 7.1° and from 33.6° to 7.2° in Damon Q and Invisalign® group respectively (Fig. 2A). The inclination changes of U1-SN (°) ranged from 28.7° to 7.7°and from 35.2° to 6.0° in Damon Q and Invisalign® group respectively (Fig. 2B). Damon Q and Invisalign® group showed no significance in linear retractions of the maxillary incisors and upper lip positions (P ≥ .13) (Table 2).
Figure 2.
Variations of U1-NA (°) and U1-SN (°) over treatment for individual patient. The variations of U1-NA (°) (A) and U1-SN (°) (B) with Damon Q ranged from 29.3° to 7.1°and 28.7° to 7.7°. The variations of U1-NA (°) and U1-SN (°) with Invisalign® ranged from 33.6° to 7.2°and 35.2° to 6.0°.
3.2. Subgroup comparisons between Damon Q and Invisalign® group
The individual change for the 5 tested angular and linear variables was showed in Figure 3 and Table 3. In subgroup Ⅲ, more retractions were obtained with Invisalign® compared to Damon Q (P ≤ .001, Table 3), and more labial root deviations were found with Invisalign® than Damon Q in subgroup Ⅲ (P = .04, Table 3). However, maxillary Lip to E-plane (mm) distance did not show significant differences among 3 subgroups between Damon Q and Invisalign® groups (Table 3).
Figure 3.
Angular and linear variations over treatment in different subgroups for individual patient. Invisalign® resulted in more lingual crown inclinations (A, U1-NA (°) and U1-SN (°)) and buccal root deviations (B, U1R-NA (mm)) compared with Damon Q in subgroup Ⅲ (P ≤ .04). Independent t test (Mann–Whitney U test) and ANOVA (Kruskal–Wallis test) were applied. ***P < 0.001.
Table 3.
Descriptive statistics of 3 subgroups T0-T1.
| Damon Q (Mean ± SD) | Invisalign® (Mean ± SD) |
Significance between | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Subgroup I ① (n = 7) |
Subgroup II ② (n = 14) |
Subgroup III ③ (n = 12) |
Subgroup I ④ (n = 7) |
Subgroup II ⑤ (n = 9) |
Subgroup III ⑥ (n = 10) |
①②③ | ④⑤⑥ | ①④ | ②⑤ | ③⑥ | |
| U1-NA (°) | 14.80 ± 4.61 | 16.43 ± 6.27 | 17.56 ± 3.88 | 17.23 ± 6.96 | 18.53 ± 8.73 | 24.55 ± 6.47 | 0.63 | 0.11 | 0.46 | 0.51 | 0.01 |
| U1-NA (mm) | 5.60 ± 0.59 | 5.40 ± 1.83 | 5.07 ± 3.27 | 5.51 ± 2.37 | 6.48 ± 2.61 | 7.77 ± 2.00 | 0.84* | 0.16 | 0.93 | 0.26 | 0.09† |
| U1R-NA (mm) | 0.51 ± 0.59 | -0.44 ± 1.76 | -0.74 ± 0.90 | -0.82 ± 1.83 | 0.11 ± 1.93 | -2.06 ± 1.79 | 0.14 | 0.06 | 0.09 | 0.49 | 0.04 |
| U1-SN (°) | 15.59 ± 5.21 | 16.83 ± 6.27 | 17.98 ± 3.92 | 17.71 ± 9.10 | 18.78 ± 8.98 | 25.35 ± 6.72 | 0.73 | 0.12 | 0.60 | 0.55 | 0.00 |
| Maxillary Lip to E-plane (mm) | 1.80 ± 12.04 | 2.01 ± 1.37 | 2.23 ± 1.52 | 2.87 ± 3.05 | 1.70 ± 1.76 | 2.60 ± 1.65 | 0.90 | 0.51 | 0.46 | 0.64 | 0.51 |
Similar retraction effect among the 3 subgroups were obtained in both Damon Q and Invisalign® groups (P ≥ .06). More retractions and more labial root deviations were also obtained with Invisalign® in subgroup Ⅲ (P ≤ .04). Maxillary Lip to E-plane (mm) distance did not show significant differences among 3 subgroups between Damon Q and Invisalign® groups.
Multiple comparisons of 3 subgroups for Damon Q or Invisalign® were tested with ANOVA or Kruskal–Wallis test.
Comparisons between Damon Q and Invisalign® in different subgroups were tested with Independent t test or Mann–Whitney U test.
3.3. Comparisons of dental measurement pre- and post-treatment for Damon Q and Invisalign® group
The changes of molar relationship and anterior overjet and overbite were showed in Table 4. 69.2% patients (18/26) in Invisalign® group obtained a Class I molar relationship, which was less than 87.8% (29/33) in Damon Q group (P = .012). Damon Q also displayed higher capacity to improve anterior overbite than Invisalign® (P = .047). The percentage of normal overbite in patients was increased from 36.3% to 90.9% in Damon Q group after treatment, while from 42.3% to 61.5% in Invisalign® group. The difference of overjet improvement was no significant between Damon Q and Invisalign® group.
Table 4.
Malocclusion improvements in Damon Q and Invisalign® group.
| Damon Q (n = 33) | Invisalign® (n = 26) | P value | ||||
|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | |||
| Angle classification | ||||||
| Class I | 13 | 29 | 17 | 18 | .012 | |
| Class II | 19 | 4 | 8 | 8 | ||
| Class III | 1 | 0 | 1 | 0 | ||
| Anterior overjet | ||||||
| Normal | 5 | 31 | 3 | 24 | .373 | |
| Deep overjet | I° | 6 | 2 | 8 | 2 | |
| II° | 10 | 0 | 9 | 0 | ||
| III° | 12 | 0 | 6 | 0 | ||
| Anterior overbite | ||||||
| Normal | 12 | 30 | 11 | 16 | .047 | |
| Deep overbite | I° | 8 | 2 | 8 | 7 | |
| II° | 9 | 1 | 3 | 3 | ||
| III° | 4 | 0 | 4 | 0 | ||
Damon Q achieved more improvements on molar relationship and overbite than Invisalign® (P ≤ .047). The percentage of Class I molar relationship and normal overbite in patients was increased from 39.4% to 87.8% and 36.3% to 90.9% in Damon Q group after treatment. The percentage of Class I molar relationship and normal overbite in patients was slightly increased from 65.4% to 69.2% and 42.3% to 61.5% in Invisalign® after treatment. The difference of overjet improvement was no significant between two groups after treatment. Angle classification, Overjet and Overbite were ranked orthodontic data. The calculated rank of data (T0-T1) was analyzed with Mann–Whitney U test.
4. Discussion
The retraction of the maxillary incisors is crucial for the acquisition of a favorable profile in orthodontic treatment. Fixed appliances such as Damon Q SLBs have been demonstrated as effective tools to retract protruded incisors. In recent years, clear aligners have become an alternative option for fixed appliances but their management for maxillary incisors case has not been explored very clearly, especially in extraction cases. The retrospective study was performed to investigate the maxillary incisors retraction effect of Invisalign® and Damon Q systems for patients with first premolars extraction.
We found that Invisalign® was not sufficiently effective in retracting maxillary incisors compared with Damon Q appliances. This was similar to the previous studies.[14,15] Although the SmartTrack® material and G6 protocol were proposed in Invisalign®, the torque control of maxillary incisors still be a challenge for Invisalign®. Compared with Damon Q, more maxillary incisors lingual inclination changes were recorded from T0-T1, and especially apparent in the subgroup Ⅲ, indicating more tipping movements for severely protruded maxillary incisors. The previous report[17–19] also have the similar findings, as more labial root deviation and insufficient torque expression with Invisalign® when applied in extraction cases. Meanwhile, the more labial root deviation with Invisalign® also indicated a higher risk of creating or exacerbating bone fenestration during orthodontic treatment[20] although Invisalign® used to be considered good for periodontal health.[21] The last thing we need pay attention to the longer treatment duration in the Invisalign® group, which may explain by the higher cooperation requirement with removable clear aligner.
According to the improvement of molar relationship and anterior overjet and overbite, Damon Q group displayed larger portion of patients with Class I molar relationship and normal overbite than Invisalign® group after treatment. This suggested Invisalign® was not sufficiently in retracting the maxillary incisors, which showed limited ability to correct sagittal and anterior vertical discrepancies.[22] Systemic review and clinical study also reported the intrusion of maxillary incisors and correction of deep overbite with Invisalign® were insufficient,[23–25] which may resulting from the poor expression of prescribed overbite reduction (no more than 39.2%) of Invisalign® as reported by Blundell et al.[25]
There are still several limitations in this study. The sample size of this study was not very large. The parameters obtained by 2D radiographs for measuring the inclinations of the maxillary incisors may not be very precise. Further studies by three-dimensional analysis are needed in the future.
5. Conclusion
In patients with bilateral maxillary first premolar extractions, Invisalign® was not sufficiently effective in retracting maxillary incisors compared with Damon Q appliances.
Invisalign® caused more lingual inclination of maxillary incisors in patients with bilateral maxillary first premolar extraction, especially those with severely protruded maxillary incisors.
Acknowledgments
We would like to thank Miss Chongchong Zhou from Department of Research Management, Nanjing Stomatological Hospital, Medical School of Nanjing University, for the statistical consultation of this study.
Author contributions
Conceptualization: Huang Li.
Data curation: Jiping Chen. Juan Wen, Ling Huang, Lu Zhang, Lei Han.
Formal analysis: Jiping Chen.
Supervision: Huang Li.
Writing – original draft: Jiping Chen.
Writing – review & editing: Jiping Chen, Juan Wen, Huang Li.
Abbreviations:
- ICC =
- intraclass correlation coefficient
- SLBs =
- self-ligating brackets
The data collection was supported by National Natural Science Foundation of China [81670960], Jiangsu Provincial Medical Youth Talent [QNRC2016115], and Nanjing Clinical Research Center for Oral Diseases [2019060009].
The retrospective study was approved by the Institutional Ethics Committee of Nanjing Stomatological Hospital, Medical School of Nanjing University with the registration number NJSH-2021NL-87. Informed consent was obtained from each participant.
The authors have no conflicts of interest to disclose.
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Chen J, Wen J, Huang L, Zhang L, Han L, Li H. Comparisons of maxillary incisor retraction effects for patients with first premolar extractions between Damon Q and Invisalign®: A retrospective study. Medicine 2022;101:40(e30919).
Contributor Information
Jiping Chen, Email: njumedcjp@163.com.
Juan Wen, Email: puredark_wen@126.com.
Ling Huang, Email: huangling0107@qq.com.
Lu Zhang, Email: 18725514287@163.com.
Lei Han, Email: pinedream@163.com.
References
- [1].Pace M, Cioffi I, D’Antò V, et al. Facial attractiveness of skeletal class I and class II malocclusion as perceived by laypeople, patients and clinicians. Minerva Stomatol. 2018;67:77–85. [DOI] [PubMed] [Google Scholar]
- [2].Sundareswaran S, Vijayan R. Profile changes following orthodontic treatment of class I bimaxillary protrusion in adult patients of Dravidian ethnicity: a prospective study. Indian J Dent Res. 2017;28:530–7. [DOI] [PubMed] [Google Scholar]
- [3].Lee R, Hwang S, Lim H, et al. Treatment satisfaction and its influencing factors among adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2018;153:808–17. [DOI] [PubMed] [Google Scholar]
- [4].Alqahtani N, Alqasir A, Al-Jewair T, et al. Dental and soft tissue changes following extraction of second premolars in females with bimaxillary protrusion: a retrospective study. Original Article. Niger J Clin Pract. 2020;23:1110–9. [DOI] [PubMed] [Google Scholar]
- [5].Alkadhi RM, Finkelman MD, Trotman CA, et al. The role of lip thickness in upper lip response to sagittal change of incisor position. Orthod Craniofac Res. 2019;22:53–7. [DOI] [PubMed] [Google Scholar]
- [6].Al-Thomali Y, Mohamed RN, Basha S. Torque expression in self-ligating orthodontic brackets and conventionally ligated brackets: a systematic review. J Clin Exp Dent. 2017;9:e123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Archambault A, Lacoursiere R, Badawi H, et al. Torque expression in stainless steel orthodontic brackets. A systematic review. Angle Orthod. 2010;80:201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Monteiro MR, Silva LE, Elias CN, et al. Frictional resistance of self-ligating versus conventional brackets in different bracket-archwire-angle combinations. J Appl Oral Sci. 2014;22:228–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pandis N, Polychronopoulou A, Eliades T. Self-ligating vs conventional brackets in the treatment of mandibular crowding: a prospective clinical trial of treatment duration and dental effects. Am J Orthod Dentofacial Orthop. 2007;132:208–15. [DOI] [PubMed] [Google Scholar]
- [10].Paduano S, Cioffi I, Iodice G, et al. Time efficiency of self-ligating vs conventional brackets in orthodontics: effect of appliances and ligating systems. Prog Orthod. 2008;9:74–80. [PubMed] [Google Scholar]
- [11].Krishnan M, Kalathil S, Abraham KM. Comparative evaluation of frictional forces in active and passive self-ligating brackets with various archwire alloys. Am J Orthod Dentofacial Orthop. 2009;136:675–82. [DOI] [PubMed] [Google Scholar]
- [12].Alobeid A, El-Bialy T, Reimann S, et al. Comparison of the efficacy of tooth alignment among lingual and labial brackets: an in vitro study. Eur J Orthod. 2018;40:660–5. [DOI] [PubMed] [Google Scholar]
- [13].Caruso S, Nota A, Ehsani S, et al. Impact of molar teeth distalization with clear aligners on occlusal vertical dimension: a retrospective study. BMC Oral Health. 2019;19:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Rossini G, Parrini S, Castroflorio T, et al. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85:881–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Li W, Wang S, Zhang Y. The effectiveness of the Invisalign appliance in extraction cases using the ABO model grading system: a multicenter randomized controlled trial. Int J Clin Exp Med. 2015;8:8276–82. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [16].Sfondrini MF, Gandini P, Castroflorio T, et al. Buccolingual inclination control of upper central incisors of aligners: a comparison with conventional and self-ligating brackets. Biomed Res Int. 2018;2018:9341821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Dai F-F, Xu T-M, Shu G. Comparison of achieved and predicted tooth movement of maxillary first molars and central incisors: first premolar extraction treatment with Invisalign. Angle Orthod. 2019;89:679–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Guan X, Chang DT, Yan Y, et al. [Clinical efficacy of clear aligners in treating bimaxillary protrusion]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2017;52:549–53. [DOI] [PubMed] [Google Scholar]
- [19].Jiang T, Jiang YN, Chu FT, et al. A cone-beam computed tomographic study evaluating the efficacy of incisor movement with clear aligners: assessment of incisor pure tipping, controlled tipping, translation, and torque. Am J Orthod Dentofacial Orthop. 2021;159:635–43. [DOI] [PubMed] [Google Scholar]
- [20].Jing W-D, Xu L, Li X-T, et al. Prevalence of and risk factors for alveolar fenestration and dehiscence in the anterior teeth of Chinese patients with skeletal Class III malocclusion. Am J Orthod Dentofacial Orthop. 2021;159:312–20. [DOI] [PubMed] [Google Scholar]
- [21].Jiang Q, Li J, Mei L, et al. Periodontal health during orthodontic treatment with clear aligners and fixed appliances: a meta-analysis. J Am Dent Assoc. 2018;149:712–20.e12. [DOI] [PubMed] [Google Scholar]
- [22].Patterson BD, Foley PF, Ueno H, et al. Class II malocclusion correction with Invisalign: is it possible? Am J Orthod Dentofacial Orthop. 2021;159:e41–8. [DOI] [PubMed] [Google Scholar]
- [23].Dai FF, Xu TM, Shu G. Comparison of achieved and predicted crown movement in adults after 4 first premolar extraction treatment with Invisalign. Am J Orthod Dentofacial Orthop. 2021;160:805–13. [DOI] [PubMed] [Google Scholar]
- [24].Papadimitriou A, Mousoulea S, Gkantidis N, et al. Clinical effectiveness of Invisalign® orthodontic treatment: a systematic review. Prog Orthod. 2018;19:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Blundell HLD, Weir TD, Kerr BD, et al. Predictability of overbite control with the Invisalign appliance. Am J Orthod Dentofacial Orthop. 2021;160:725–31. [DOI] [PubMed] [Google Scholar]