Abstract
Objectives
Meditation interventions typically show small to moderate effects on health and well‐being, but we know little about how these effects vary across individuals. This meta‐analytic study investigates the relationship between baseline participant characteristics and the outcomes of meditation.
Methods
A systematic search yielded 51 eligible studies with 7782 participants. A combination of subgroup analyses and meta‐regression based on the random‐effects model were used.
Results
We found that a higher baseline level of psychopathology or depression was associated with deterioration in mental health after a meditation intervention. On the other hand, participants with higher scores on interpersonal variables, motivation, medical conditions, and mindfulness showed higher levels of positive meditation outcomes. Higher well‐being and stress were simultaneously associated with moderate increases in negative and positive meditation outcomes. Participant demographics, psychological traits, self‐concept, and length of meditation practice did not significantly influence the response to meditation.
Conclusions
Overall, we found that meditation interventions affect participants differently, and identified some of the individual characteristics that should be considered when using meditation interventions.
Keywords: meditation, mindfulness, individual differences, meta‐analysis, participant characteristics
Statement of contribution.
The effects of participant characteristics on meditation intervention outcomes: A meta‐analysis
What is already known on this subject?
There is an universalist assumption that has been guiding studies on meditation techniques, which can be simply be stated as ‘meditation works in the same way for everyone’. This assumption explains why, thus far, participant characteristics as sources of variability in the response to meditation have not been examined directly through a meta‐analysis, but only briefly explored as moderating factors in meta‐analyses that examine the effects of meditation on specific dependent variable in a specific population (e.g., age as a moderator of the effect of meditation on reducing trait anxiety in adults, see Khoury, Sharma, Rush, & Fournier, 2015; Orme‐Johnson & Barnes, 2013; Zoogman, Goldberg, Hoyt, & Miller, 2015).
Based on these previous meta‐analyses it appears that age, gender and ethnicity do not to moderate outcomes of meditation in clinical and non‐clinical samples (Khoury et al., 2015; Orme‐Johnson & Barnes, 2013; Zoogman et al., 2015); that the reduction in trait anxiety following meditation appears to be greater in people with high anxiety levels (Orme‐Johnson & Barnes, 2013); and that people with three or more episodes of major depression responded better to Mindfulness‐Based Cognitive Therapy (MBCT) than those with one or two episodes (Piet & Hougaard, 2011). However, a comprehensive analysis of participant factors in relation to the efficacy of meditation‐based interventions has not been conducted before.
What does this study add?
People with higher psychopathology are more likely to show worsening of mental health following meditation.
People with interpersonal problems or with medical conditions are more likely to experience benefits of meditation.
Demographics, psychological traits and self‐concept do not influence the response to meditation.
Background
Meditation is generally practiced with the aim of achieving positive changes, whether physical, mental health, or of a moral‐spiritual character. In reality, the effectiveness of meditation practices varies among individuals; while many reap benefits and become dedicated long‐term practitioners, others sense no noticeable effects or might even experience unwanted, unpleasant, or adverse effects (Cebolla, Demarzo, Martins, Soler, & Garcia‐Campayo, 2017; Van Dam et al., 2018; Farias, Maraldi, Wallenkampf, & Lucchetti, 2020; Lindahl, Fisher, Cooper, Rosen, & Britton, 2017; Schlosser, Sparby, Vörös, Jones, & Marchant, 2019). In 1977, the American Psychiatric Association issued a statement on meditation strongly recommending the need to undertake research that evaluates the possible usefulness, indications, and contraindications of meditation (American Psychiatric Association, 1977). Over 40 years have passed, and we still have not achieved a body of research allowing us to tell which type of individuals may benefit the most and the least from meditation interventions.
One example of the wide‐reaching problems driven by the lack of insight into individual differences in meditation research concerns its clinical implications. Meta‐analyses focusing on mindfulness‐based interventions (MBIs) have shown that patients with some psychiatric conditions using these techniques experience a level of symptom reduction equivalent to that of other evidence‐based treatments, such as psychotherapy or biomedical treatment (Goldberg et al., 2018; Hofmann & Gómez, 2017; Veehof, Trompetter, Bohlmeijer, & Schreurs, 2016). Despite this evidence, the British National Institute for Health and Care Excellence recommends MBIs in only two specific cases: for individuals with a history of three or more episodes of depression (Pilling et al., 2009), and for treating fatigue in patients with multiple sclerosis (Perry et al., 2014). This rather restrictive recommendation is understandable as the majority of current evidence is based on reports of mean group changes, but it pays no attention to how individuals might react differently to MBIs or other meditation‐based practices. For instance, even if high‐quality randomized controlled trials with anxious samples show moderate effect sizes of meditation on anxiety, there would still be many participants within each trial that show no reductions in anxiety where we would not be aware of why that is so. If there is variability in the valence and intensity of meditation effects across individuals, the task at hand is to assess this variability so clinicians and therapists know when and with whom to use these techniques and when to avoid them.
As it happens with other types of psychological interventions, there are three groups of characteristics that are likely to lead to variability in responses to meditation interventions: participant, intervention, and teacher characteristics (Baer, Crane, Miller, & Kuyken, 2019). The focus of this paper is on participant characteristics because there has been no comprehensive analysis of participant factors in relation to the efficacy of meditation‐based interventions. Participant characteristics as sources of variability in the response to meditation have not been examined directly through a meta‐analysis, but only briefly explored as moderating factors in meta‐analyses that examine the effects of meditation on the specific dependent variable in a specific population (e.g., age as a moderator of the effect of meditation on reducing trait anxiety in adults, see Khoury et al., 2015; Orme‐Johnson & Barnes, 2013; Zoogman et al., 2015) or in a non‐quantitative form as a narrative review of 26 studies (Buric, Brazil, & van Mulukom, 2021). These previous studies provide limited conclusions regarding variability in meditation responses. For instance, the meta‐analyses suggest that age, gender, and ethnicity did not moderate various outcomes of meditation in clinical and non‐clinical samples (Khoury et al., 2015; Orme‐Johnson & Barnes, 2013; Zoogman et al., 2015). This is partially in congruence with a narrative review that found the females respond better to meditation interventions, but there is no relationship between other demographic variables and meditation outcomes (Buric et al., 2021). Another meta‐analysis found that the reduction in trait anxiety following meditation was greater in people with high anxiety levels (Orme‐Johnson & Barnes, 2013), similar to a review that found that people who are more anxious generally tend to respond better to meditation interventions (Buric et al., 2021). Finally, a meta‐analysis found that people with three or more episodes of major depression responded better to mindfulness‐based cognitive therapy than those with one or two episodes (Piet & Hougaard, 2011). Buric et al. (2021) reached a similar conclusion and also identified several other sources of variability in meditation responses. More specifically, Buric et al. (2021) suggested that people with higher expectations of meditation tend to respond better to meditation interventions and that people with more severe medical conditions also tend to respond better. Finally, they also found indications that there might be some genetic predispositions that make some people more prone to experience better responses to meditation interventions. While these previous studies are certainly noteworthy, they do not provide numerical comparisons of different participant characteristics that could aid in predicting how a person might respond to meditation. The topic is quickly becoming of greater relevance as clinical practice recognizes the importance and urgency of developing interventions that are tailored to the individual’s needs (i.e., are personalized) (Cuthbert & Insel, 2013), particularly in populations that tend to be less responsive to the established interventions (Brazil, van Dongen, Maes, Mars, & Baskin‐Sommers, 2018). The central idea behind personalized medicine is to move beyond the one‐size‐fits‐all principle. One way in which we can move meditation research in the direction of individualized treatment is to first explore carefully how participant characteristics might affect meditation interventions.
Aims of the study
Our first aim was to examine the relationship between participant characteristics and responses to meditation through a series of meta‐analyses. Thus, our focus is different from previous meta‐analyses that have examined whether meditation works as an intervention across different populations (e.g., Khoury et al., 2015; Orme‐Johnson & Barnes, 2013; Sedlmeier et al., 2012; Zoogman et al., 2015) or from non‐quantitative reviews (Buric et al., 2021). To carry out these meta‐analyses, we identified studies of meditation‐based interventions that measured at least one variable pertaining to participant characteristics and reported how these characteristics were linked to meditation outcomes. As there is a lack of theory that would guide the selection of outcomes in meditation studies, this leads to wide variability in the selection of outcome variables. To run such meta‐analyses, all outcome variables have to be split into positive and negative (i.e., as having a positive or negative impact on mental health) because any participant characteristic could have one kind of association with negative outcomes, and a different association with positive outcomes. For instance, participants’ baseline depression levels could be highly associated with a change in stress scores following meditation intervention, but less associated with a change in sleep quality scores.
Based on previous studies described above, we expected to find that demographic variable had no effect on positive or negative outcomes of meditation. Furthermore, we expected that participants with higher trait anxiety or with higher depression levels would experience a more positive impact from meditation. We did not have further specific hypotheses about other participant characteristics and their effect on meditation outcomes, as many of these characteristics were still unknown and the present study was the first to systematically explore the literature to uncover them.
Our second aim was to test for moderators of the relationship between participant characteristics and meditation outcomes. We included six moderators: sample size, sample type, research design, study quality, meditation type, and length of meditation. The first four moderators were chosen based on the results of previous meta‐analyses focusing on meditation, which often show smaller effect sizes in studies with larger samples, in non‐clinical samples, in randomized controlled trials, and in studies of high methodological quality (Sedlmeier et al., 2012). The remaining two moderators were chosen because the effect sizes often vary for different types of meditation and different lengths of meditation interventions (Kok & Singer, 2017), thus we wanted to test these moderators in the context of participant characteristics and meditation. We also examined the methodological rigor of the studies included in our analyses given that concerns have been raised about the methodological quality of meditation studies (Chiesa & Serretti, 2009; Goyal et al., 2014).
Methods and materials
Selection of studies
We searched the databases Psych INFO, MEDLINE, PsycARTICLES until March 2019 using the following search terms: (meditation OR mindfulness) AND (moderator OR predictor OR individual differences OR interaction). The search was limited to titles and abstracts. To locate studies that were not detected with the initial database search, we contacted 58 experts to enquire if they were familiar with additional studies that met our eligibility criteria, and we hand‐searched references of the 79 articles that met our eligibility criteria (Figure 1). Following the removal of duplicates, 2000 records were screened. A total of 51 articles met the following inclusion criteria:
The sample contained participants that were 18 years of age or older.
Both clinical and non‐clinical samples were allowed.
There should be at least 10 participants per group (Hedges, 1985).
Studies had to include a meditation intervention, baseline measures of participants’ characteristics, and at least one meditation outcome.
All types of meditation or meditation‐based interventions that included meditation as a core component were eligible.
Research designs could be experimental or quasi‐experimental.
Articles should have been published in English in peer‐reviewed journals.
Figure 1.
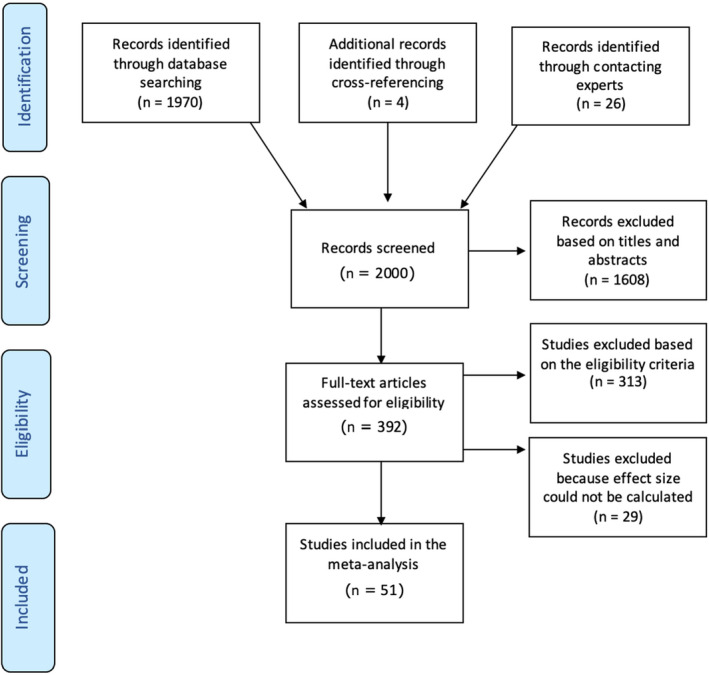
PRISMA flowchart.
Exclusion criteria:
Meta‐analyses, review papers, commentaries, doctoral theses, and conference proceedings.
Studies that only used non‐standardized tasks and/or questionnaires.
Studies with outcomes that cannot be categorized as having a positive or negative impact on mental health.
Quality assessment
We assessed the methodological quality of the studies using the National Institutes of Health Study Quality Assessment Tools: Quality Assessment of Controlled Intervention Studies and Quality Assessment Tool for Before–After (Pre–Post) Studies with No Control Group (National Heart, Lung and Blood Institute, 2014). Each tool consists of 8–14 questions that are answered with yes, no, or not reported/cannot determine/not applicable, where the latter two suggest a potential flaw in the study design or implementation. The questions examine components of internal validity, such as if the study used random sequence generation, included blinding of outcome assessment, or showed selective reporting of statistical results. We had to modify two out of three quality assessment tools, as some items were not applicable to meditation research. Specifically, in the Quality Assessment of Pre–Post Studies with no Control Group, we excluded two items: Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (i.e., did they use an interrupted time‐series design)? and if the intervention was conducted at a group level (e.g., a whole hospital, a community, etc.) did the statistical analysis take into account the use of individual‐level data to determine effects at the group level? In the Quality Assessment of Controlled Intervention Studies, we excluded one item: Were study participants and providers blinded to treatment group assignment? because it is dubious whether one can truly blind participants to a meditation intervention (Davidson & Kaszniak, 2015). The responses were coded as 1 if the answer was yes or as 0 if the answer was no or not reported.
Study characteristics
There was a total of 7782 participants across 51 articles (full references of included articles can be found after the references cited in the text, and the extracted data can be found in Table 1). Studies showed moderate‐quality based on the National Institutes of Health study quality assessment tools (see Table 2). The median length of meditation interventions was 56 days. Out of the 51 included studies, mindfulness meditation was used in 68% of the studies, while 14% of the studies employed transcendental meditation, and other techniques (mainly compassion or breathing meditations) were used in 18% of studies. Furthermore, 56% of the studies had pre–post design studies without a control group, while 44% were randomized controlled trials. Randomized controlled trials used active control groups in 58% of cases, which included psycho‐education or various forms of attention control, such as reading or listening to a story. Healthy adults were examined in 56% of the 51 eligible studies. The most common clinical populations were patients with chronic medical conditions, such as cancer, hypertension, or arthritis (24%). The most prevalent mental disorders were anxiety (18%) and depression (18%), followed by substance abuse (14%), and studies that targeted more than one mental disorder (14%). Studies were published between 1978 and 2018, though the majority (72%) was published in the past ten years, which suggests a growing interest in examining the effects of participant characteristics.
Table 1.
Summary of the results of all studies included in the meta‐analysis showing authors of each study, examined participant characteristic and outcomes of meditation, effect size (ES) converted to Pearson’s r, sample size, research design type, sample type, meditation type and length, and study quality estimated with tools by National Institutes of Health (ranging from 0 to 1)
| Authors | Participant characteristics | Outcomes | ES | Sample size | Design type | Sample type | Meditation type | Meditation length (days) | Study quality |
|---|---|---|---|---|---|---|---|---|---|
| Azam et al. (2016) | Having headache | Heart‐rate variability | .37 | 77 | RCT | Healthy adults | Loving‐kindness meditation | 1 | .83 |
| Brotto et al. (2015) | Trait anxiety | Change score in pain | .02 | 63 | Non‐RCT | Women with vulvodynia | Group training that includes mindfulness, cognitive‐behavioural therapy, and pain education | 56 | .70 |
| Depression | Change score in pain | .13 | 60 | Non‐RCT | Women with vulvodynia | Group training that includes mindfulness, cognitive‐behavioural therapy, and pain education | 56 | .70 | |
| Number of comorbid conditions | Pain induced by a cotton swab at 6 mo follow‐up | −.18 | 69 | Non‐RCT | Women with vulvodynia | Group training that includes mindfulness, cognitive‐behavioural therapy, and pain education | 56 | .70 | |
| Sexual distress | Change score in pain | .05 | 63 | Non‐RCT | Women with vulvodynia | Group training that includes mindfulness, cognitive‐behavioural therapy, and pain education | 56 | .70 | |
| Cohn & Fredrickson (2010) | Social support received | Continued meditation practice at 8 weeks | .19 | 95 | RCT | Healthy adults | Loving‐kindness | 365 | .69 |
| Daily positive emotions during the week before learning meditation | Continued meditation practice at 8 weeks | .24 | 95 | RCT | Healthy adults | Loving‐kindness | 365 | .69 | |
| Cordon Brown & Gibson (2009) | Insecure attachment | Drop‐out rate | .29 | 131 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 75 | .90 |
| Crandall et al. (2019) | Intentions to practice mindfulness and subjective norms | Practicing mindfulness | .30 | 85 | Non‐RCT | Healthy adults | Provisional selection among many mindfulness exercises within an app (The Smiling mind app) | 14 | .90 |
| Perceived behavioural control | Practicing mindfulness | .06 | 85 | Non‐RCT | Healthy adults | Provisional selection among many mindfulness exercises within an app (The Smiling mind app) | 14 | .90 | |
| Age, gender, employment status | Practicing mindfulness | .02 | 85 | Non‐RCT | Healthy adults | Provisional selection among many mindfulness exercises within an app (The Smiling mind app) | 14 | .90 | |
| Crescentini et al. (2014) | Implicit religiousness/spirituality | Implicit religiousness/spirituality | .40 | 30 | Non‐RCT | Healthy adults | Mindfulness group training based on Theravada traditions and mindfulness‐based stress reduction | 70 | .50 |
| Day et al. (2016) | Expectations/motivation | Pain interference | .34 | 21 | RCT | Chronic headache pain | Mindfulness‐based cognitive therapy | 56 | .54 |
| Expectations/motivation | Home practice | .15 | 21 | RCT | Chronic headache pain | Mindfulness‐based cognitive therapy | 56 | .54 | |
| Delmonte (1981) | Age | Deciding to learn meditation after tm lecture | .25 | 94 | Non‐RCT | Healthy adults | Transcendental meditation | 16 | .60 |
| Expectations | Deciding to learn meditation after tm lecture | .33 | 64 | Non‐RCT | Healthy adults | Transcendental meditation | 16 | .60 | |
| Perceived self | Deciding to learn meditation after tm lecture | .32 | 70 | Non‐RCT | Healthy adults | Transcendental meditation | 16 | .60 | |
| Delmonte (1985) | Expectations (positive rationale group) | Skin conductance | .42 | 40 | Non‐RCT | Healthy adults | Transcendental meditation | 1 | .70 |
| Delmonte (1988) | Extraversion | Becoming a regular meditator at 12mo | .02 | 37 | Non‐RCT | Outpatients with psychosomatic and neurotic symptoms | Transcendental meditation | 104 | .70 |
| Dobkin et al. (2017) | Not depressed | Stress | .30 | 63 | Non‐RCT | Patients with various chronic illnesses | Mindfulness‐based stress reduction | 56 | .70 |
| Not depressed | Coherence (average comprehensibility, manageability, meaningfulness, | .10 | 63 | nNon‐RCT | Patients with various chronic illnesses | Mindfulness‐based stress reduction | 56 | .70 | |
| Felleman et al. (2016) | Gender | PTSD severity | .16 | 116 | Non‐RCT | PTSD veterans | Mindfulness‐based stress reduction | 56 | .80 |
| PTSD severity | PTSD severity | .19 | 116 | Non‐RCT | PTSD veterans | Mindfulness‐based stress reduction | 56 | .80 | |
| Gawrysiak et al. (2016) | Distress tolerance | Perceived stress | .32 | 327 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .90 |
| Greenberg et al. (2018) | Self‐compassion | Change in depression symptoms | −.02 | 13 | RCT | Patients with depression | Mindfulness‐based cognitive therapy | 56 | .62 |
| Greeson et al. (2011) | Having a religious affiliation | Change in depression symptoms | −.04 | 279 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .90 |
| Greeson et al. (2015) | Having a religious affiliation | Change in depression symptoms | .01 | 322 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .90 |
| Age | Change in depression symptoms | −.04 | 322 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .90 | |
| Mindfulness | Change in depression symptoms | .19 | 322 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .90 | |
| Mental functioning | Change in depression symptoms | .19 | 119 | Non‐RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .90 | |
| Geschwind et al. (2012) | Number of depressive episodes | Depression symptoms HSRD scale | .21 | 260 | RCT | Adults with history of depression | Mindfulness‐based cognitive therapy | 56 | .77 |
| Heide et al. (1980) | Hypnotic responsivity | Trait anxiety | .20 | 58 | RCT | Healthy adults | Mantra meditation | 7 | .77 |
| Hypnotic responsivity | Perceived benefit from meditation | .19 | 58 | RCT | Healthy adults | Mantra meditation | 7 | .77 | |
| Herdt et al. (2012) | Therapist's assessment of the patients’ motivation | Number of attended sessions | .43 | 51 | Non‐RCT | Psychiatric patients | Mindfulness‐based cognitive therapy | 63 | .80 |
| Having participated in group therapies earlier | Completed sessions 1–3 | .21 | 74 | Non‐RCT | Psychiatric patients | Mindfulness‐based cognitive therapy | 63 | .80 | |
| Hülsheger et al. (2015) | Age | Work hours | −.13 | 140 | RCT | Healthy adults | Self‐trained mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 10 | .46 |
| Age | Sleep duration | .00 | 140 | RCT | Healthy adults | Self‐trained mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 10 | .46 | |
| Age | Mindfulness | −.06 | 140 | RCT | Healthy adults | Self‐trained mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 10 | .46 | |
| Trait mindfulness | Mindfulness | .19 | 140 | RCT | Healthy adults | Self‐trained mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 10 | .46 | |
| Sleep duration | Sleep duration | .23 | 140 | RCT | Healthy adults | Self‐trained mindfulness based on mindfulness‐based stress reduction andmindfulness‐based cognitive therapy | 10 | .46 | |
| Jazaieri et al. (2016) | Low social anxiety | Social anxiety during MBSR | .30 | 47 | RCT | Patients with social anxiety disorder | Mindfulness‐based stress reduction | 56 | .54 |
| Kabat‐Zinn & Chapman‐Waldrop (1988) | Gender in pain cohort | Completing the program | .12 | 500 | Non‐RCT | Patients with stress or pain‐related conditions | Mindfulness‐based stress reduction | 56 | .60 |
| Type of pain/stress diagnosis | Completing the program | .14 | 784 | Non‐RCT | Patients with stress or pain‐related conditions | Mindfulness‐based stress reduction | 56 | .60 | |
| Gender (total population) | Being a no‐show vs being a drop‐out | .06 | 784 | Non‐RCT | Patients with stress or pain‐related conditions | Mindfulness‐based stress reduction | 56 | .60 | |
| Kharlas & Frewen (2016) | Mindfulness | Distress during meditation | −.12 | 508 | Non‐RCT | Healthy adults | A single session of mindfulness imagery practice | 1 | .60 |
| Mindfulness | Visual imagery during meditation | .13 | 508 | Non‐RCT | Healthy adults | A single session of mindfulness imagery practice | 1 | .60 | |
| Sensory imagery | Distress during meditation | .01 | 508 | Non‐RCT | Healthy adults | A single session of mindfulness imagery practice | 1 | .60 | |
| Sensory imagery | Pleasantness during meditation | .25 | 508 | Non‐RCT | Healthy adults | A single session of mindfulness imagery practice | 1 | .60 | |
| Lee & Bowen (2015) | Conscientiousness | Curiosity | .01 | 63 | Non‐RCT | Prisoners with addiction disorders | Mindfulness group training based on mindfulness‐based stress reduction | 56 | .70 |
| Logie & Frewen (2015) | Curiosity | Negative affect during referential processes | .15 | 70 | RCT | Healthy adults | A single session of mindfulness via an audio recording (focused attention) | 1 | .69 |
| Curiosity | Positive affect during referential processes | .14 | 70 | RCT | Healthy adults | A single session of mindfulness via an audio recording (focused attention) | 1 | .69 | |
| Ly et al. (2014) | Low depression symptoms | Depression symptoms | .40 | 37 | RCT | Patients with major depressive disorder | Mindfulness training via an app (focused attention) | 56 | .92 |
| Mak et al. (2018) | Discomfort with emotion | Well‐being | .04 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 |
| Ambiguity tolerance | Well‐being | .03 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Gender | Well‐being | .04 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Religion | Well‐being | .00 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Discomfort with emotion | Distress | .05 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Ambiguity tolerance | Distress | .03 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Gender | Distress | .00 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Religion | Distress | .00 | 2161 | RCT | Healthy adults | Mindfulness training via an app (focused attention) | 28 | .85 | |
| Michalak et al. (2016) | Childhood abuse | Depression change in meditation group (observer rated) | −.29 | 26 | RCT | Patients with chronic depression | Mindfulness‐based cognitive therapy | 56 | .61 |
| Nguyen‐Feng et al. (2016) | History of interpersonal violence | Worry | −.33 | 314 | RCT | Healthy adults | Three 20‐minute pre‐recorded mindfulness exercises via a web (focused attention) | 1 | .61 |
| Nguyen‐Feng et al. (2017) | History of interpersonal violence | Depression, anxiety, stress | −.11 | 147 | RCT | Healthy adults | Pre‐recorded mindfulness training via a web (focused attention) | 28 | .77 |
| Oken et al. (2018) | Gender Age Education | Health‐related quality of life | .01 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 |
| Depression | Health‐related quality of life | −.08 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based Ccognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Mental health, affect, sleep quality | Health‐related quality of life | .00 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Life stressors | Health‐related quality of life | .14 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Perceived stress | Health‐related quality of life | .01 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Neuroticism | Health‐related quality of life | .18 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Expectancy | Health‐related quality of life | −.09 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Self‐efficacy | Health‐related quality of life | −.09 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Mindfulness | Health‐related quality of life | .00 | 121 | Non‐RCT | Stressed adults | Mindfulness based on mindfulness‐based cognitive therapy, one‐on‐one with a trained instructor | 42 | .69 | |
| Pace et al. (2010) | Affect | Amount of practice (high vs low) | .36 | 30 | Non‐RCT | Healthy adults | Compassion meditation | 42 | .80 |
| Affect | Amount of practice (high vs low) | .50 | 30 | Non‐RCT | Healthy adults | Compassion meditation | 42 | .80 | |
| Pace et al. (2009) | IL‐6 | Amount of practice (high vs low) | .14 | 30 | Non‐RCT | Healthy adults | Compassion meditation | 42 | .80 |
| Gender | Amount of practice (high vs low) | .12 | 61 | RCT | Healthy adults | Compassion meditation | 42 | .85 | |
| Depressive symptoms | Amount of practice (high vs low) | .07 | 61 | RCT | Healthy adults | Compassion meditation | 42 | .85 | |
| Park & Park (2012) | Self‐directedness | Heart‐rate variability | −.10 | 58 | Non‐RCT | Healthy adults | Paced breathing | 1 | .80 |
| Harm avoidance | Heart‐rate variability | −.08 | 58 | Non‐RCT | Healthy adults | Paced breathing | 1 | .80 | |
| Prins et al. (2014) | Pain catastrophizing | Rating pain during painful stimuli | .26 | 51 | RCT | Healthy adults | A single session of pre‐recorded mindfulness (focused attention and open monitoring) | 1 | .62 |
| Reich et al. (2014) | Lymphocyte subsets | Fatigue | .32 | 17 | RCT | Breast cancer patients | Mindfulness‐based cognitive therapy | 42 | .77 |
| Rohsenow Smith et al. (1985) | Anxiety | Anxiety difference | .58 | 36 | RCT | Adults with heavy drinking problems | Cognitive‐affective stress management | 1 | .23 |
| Irrational beliefs | Anger difference | .52 | 36 | RCT | Adults with heavy drinking | Cognitive‐affective stress management | 1 | .23 | |
| Social support | Anxiety difference | .13 | 36 | RCT | Adults with heavy drinking | Cognitive‐affective stress management | 1 | .23 | |
| Alcohol consumption | Anxiety difference | .52 | 36 | RCT | Adults with heavy drinking | Cognitive‐affective stress management | 1 | .23 | |
| Locus of control | Anxiety difference | .32 | 36 | RCT | Adults with heavy drinking | Cognitive‐affective stress management | 1 | .23 | |
| Mood | Anxiety difference | .67 | 36 | RCT | Adults with heavy drinking | Cognitive‐affective stress management | 1 | .23 | |
| Rojiani et al., 2017 | Women | Negative affect | .31 | 77 | Non‐RCT | Healthy adults | Mindfulness from Buddhist or Daoist traditions (focused attention and open monitoring) | 84 | .70 |
| Men | Mindfulness | .67 | 77 | Non‐RCT | Healthy adults | Mindfulness from Buddhist or Daoist traditions (focused attention and open monitoring) | 84 | .70 | |
| Roos et al. (2017) | Substance use severity | Number of substance use days | .10 | 80 | Non‐RCT | Substance use disorders | Mindfulness‐based relapse prevention | 56 | .92 |
| Depression | Number of substance use days | .05 | 80 | Non‐RCT | Substance use disorders | Mindfulness‐based relapse prevention | 56 | .92 | |
| Anxiety | Number of substance use days | −.07 | 80 | Non‐RCT | Substance use disorders | Mindfulness‐based relapse prevention | 56 | .92 | |
| Rosenzweig et al. (2010) | Type of pain diagnosis | Psychological distress | .33 | 133 | Non‐RCT | Patients with chronic pain | Mindfulness‐based stress reduction | 56 | .70 |
| Type of pain diagnosis | Quality of life | .26 | 133 | Non‐RCT | Patients with chronic pain | Mindfulness‐based stress reduction | 56 | .70 | |
| Sass et al. (2013) | Low discomfort with emotion | Psychological distress | .58 | 24 | Non‐RCT | Healthy adults | Mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 56 | .70 |
| Seer & Raeburn (1980) | Diastolic blood pressure | Responding to treatment | .40 | 41 | RCT | Patients with hypertension | Transcendental meditation | 5 | .61 |
| Feeling relaxed | Responding to treatment | .44 | 41 | RCT | Patients with hypertension | Transcendental meditation | 5 | .61 | |
| Shapiro et al. (2011) | Mindfulness | Rumination | −.50 | 30 | RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .69 |
| Mindfulness | Mindfulness | .29 | 30 | RCT | Healthy adults | Mindfulness‐based stress reduction | 56 | .69 | |
| Smith (1978) | Trait anxiety | Trait anxiety | .22 | 19 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 |
| Trait anxiety | Continued practice of meditation for 6 months | .10 | 22 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Age | Trait anxiety | .09 | 19 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Gender | Continued practice of meditation for 6 months | .16 | 22 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Considered therapy | Trait anxiety | −.24 | 19 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Considered therapy | Continued practice of meditation for 6 months | .30 | 22 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Self‐concept (averaged) | Trait anxiety | −.13 | 19 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Self‐concept (averaged) | Continued practice of meditation for 6 months | .06 | 22 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Social desirability | Trait anxiety | .10 | 19 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Social desirability | Trait anxiety | −.01 | 19 | RCT | Adults with anxiety | Transcendental meditation | 180 | .85 | |
| Takahashi et al. (2005) | Novelty seeking | Heart‐rate variability | −.06 | 20 | Non‐RCT | Healthy adults | Other types of meditation | 1 | .50 |
| Tamagawa et al. (2015) | Anxiety | Class attendance | .26 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 |
| Married/cohabitating vs single | Home practice | .20 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based Ccancer recovery | 56 | .80 | |
| Depression | Meditation home practice | .09 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 | |
| Social support | Meditation home practice | .10 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 | |
| Months since cancer diagnosis | Meditation home practice | −.05 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 | |
| Low self‐esteem | Class attendance | .03 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 | |
| Repressive/defensiveness | Class attendance | −.02 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 | |
| Low well‐being | Class attendance | .05 | 38 | Non‐RCT | Distressed breast cancer patients | Mindfulness‐based cancer recovery | 56 | .80 | |
| Watier & Dubois (2016) | Low mindfulness | Executive attention | .19 | 78 | RCT | Healthy adults | One‐session pre‐recorded mindfulness (focused attention) | 1 | .62 |
| Weinstein & Smith (1992) | Absorption | Somatic anxiety difference | .55 | 52 | Non‐RCT | Adults with anxiety | Focused attention meditation | 1 | .80 |
| Absorption | Focusing difference | −.53 | 52 | Non‐RCT | Adults with anxiety | Focused attention meditation | 1 | .80 | |
| Zalta et al. (2018) | Combat or military sexual trauma | PTSD severity | .41 | 191 | Non‐RCT | PTSD patients | Cognitive processing, mindfulness, yoga, and psychoeducation | 31 | .90 |
| Combat or military sexual trauma | Health | .22 | 191 | Non‐RCT | PTSD patients | Cognitive processing, mindfulness, yoga, and psychoeducation | 31 | .90 | |
| Gender | PTSD severity | .10 | 191 | Non‐RCT | PTSD patients | Cognitive processing, mindfulness, yoga, and psychoeducation | 31 | .90 | |
| Zautra et al. (2008) | History of recurrent depression | Catastrophizing | .24 | 144 | RCT | Patients with rheumatoid arthritis | Mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 56 | .54 |
| History of recurrent depression | Pain control | .15 | 144 | RCT | Patients with rheumatoid arthritis | mindfulness based on mindfulness‐based stress reduction and mindfulness‐based cognitive therapy | 56 | .54 | |
| Zuroff & Schwarz (1978) | Expectancy | Anxiety difference | −.26 | 60 | RCT | Healthy adults | Transcendental meditation | 63 | .62 |
| Psychological maladjustment | Anxiety difference | .06 | 60 | RCT | Healthy adults | Transcendental meditation | 63 | .62 | |
| Locus of control | Anxiety difference | .53 | 60 | RCT | Healthy adults | Transcendental meditation | 63 | .62 | |
| Social desirability | Anxiety difference | −.20 | 60 | RCT | Healthy adults | Transcendental meditation | 63 | .62 |
Table 2.
Characteristics of the studies included in the meta‐analysis (N = 51)
| Average | Median | Range | SD | Sum | |
|---|---|---|---|---|---|
| Number of participants a | 155.64 | 63 | 17–2161 | 510.25 | 7782 |
| Length of meditation (days) | 47.14 | 56 | |||
| Study quality | 0.72 | 0.7 | |||
| RCT | Non‐RCT | ||||
| Research design | 44% | 56% | |||
| Clinical sample | Non‐clinical Sample | ||||
| Sample type | 44% | 56% | |||
| Mindfulness | Transcendental meditation | Other | |||
| Meditation type | 68% | 14% | 18% |
RCT: randomized controlled trial. Other types of meditation mainly included self‐compassion or breathing meditation.
Sample sizes varied from 17 (minimum) to 2161 (maximum), while the standard deviation was 510.25.
Procedure for data extraction and categorization
The lead author (IBu) reviewed titles, abstracts, and full texts. An extraction sheet was used to specify relevant information for each study: sample size, meditation type, meditation length, type of research design, quality assessment, examined participant characteristics, outcomes, and the relationship between participant characteristics and outcomes. Two authors (IBu and JMAD) independently extracted data on participant characteristics and meditation outcomes. Inter‐rater agreement was high (r =.89) and disagreements were discussed until consensus was reached.
Data extraction yielded 99 variables for participant characteristics and 76 outcome variables (see Tables 3 and 4). Given that many sources of individual differences in mediation outcomes still remained to be uncovered, we first explored whether ‘themes’ could be found within the pool of extracted participant characteristic variables by clustering these variables into thematic categories. Each category consisted of at least four studies. First, we searched for broad themes that were present across most studies and were therefore relatively easy to identify, such as well‐being, psychopathology, psychological traits, and medical conditions. Next, studies were added to each of these clusters until thematically different sub‐clusters emerged that consisted of four or more studies each, which led to the conversion of the sub‐clusters into separate thematic categories. For example, studies categorized under anxiety were initially part of the psychopathology category until, from the classification process, 4 or more studies assessing anxiety emerged. We found thirteen conceptually distinct categories of participant characteristics (Table 3). A second researcher (JMAD) also conducted the clustering independently to control for subjectivity bias. Inter‐rater agreement was high (r = 0.93) and all discrepancies were settled before proceeding with the analyses.
Table 3.
Participant characteristics that were measured in the 51 eligible study, categorized across 13 categories
| Category | Number of studies | Measured baseline participant characteristics |
|---|---|---|
| Psychological traits | 11 | Absorption, social desirability, cooperativeness, persistence, novelty‐seeking, harm avoidance, reward dependence, repressive/defensiveness, hypnotic responsivity, Big Five (extraversion, neuroticism, openness to experience, conscientiousness, agreeableness), sensory imagery |
| Anxiety | 7 | State anxiety, social anxiety, trait anxiety, bodily symptoms of anxiety |
| Self‐concept | 9 | Locus of control, low self‐esteem, perceived self, self‐concept, self‐transcendence, self‐directedness, self‐efficacy, self‐compassion, perceived behavioural control |
| Interpersonal | 9 | Positive life experiences, social support received, social support given insecure attachment, history of interpersonal violence, childhood abuse, life experience stressors, sexual trauma, combat‐related trauma |
| Demographics | 13 | Age, gender, marital status, employment, education |
| Depression | 9 | Depression symptoms, history of recurrent depression, number of depression episodes, fatigue |
| Motivation | 8 | Therapist's assessment of patient's motivation, therapist's prediction of leaving preterm, expectancy, motivation for spiritual growth, considered meditation, considered therapy, attitudes about meditation, intentions to practice meditation, subjective norms |
| Psychopathology | 4 | Obsessive–compulsive behaviour, alcohol consumption, posttraumatic stress disorder severity, psychological maladjustment, severity of substance use |
| Mindfulness | 7 | Trait mindfulness, curiosity, decentering, non‐judgement |
| Belief system | 4 | Irrational beliefs, spirituality, religiosity, implicit religiousness/spirituality, religious affiliation |
| Medical conditions | 6 | Headaches, length of time since cancer diagnosis, pain/stress diagnosis, diastolic blood pressure, hypertension history, number of comorbid pain conditions, baseline pain |
| Stress‐related factors | 7 | Cortisol, IL‐6, lymphocyte subsets, mitogen‐stimulated subsets, pain catastrophizing, discomfort with emotion, sexual distress |
| Well‐being | 12 | Psychological detachment from work, sleep quality, sleep duration, well‐being, pain self‐efficacy, minutes of physical activity per day, distress tolerance, relaxation level, mood, positive and negative affect, positive emotions, experience in group therapy, psychological functioning, physical functioning, mental health |
The second column represents the number of studies per category and its sum is bigger than the total number of included studies (N = 51) as almost all studies had outcomes that were included in more than one category.
Table 4.
Outcomes of meditation interventions that were measured in the 51 eligible study, categorized as positive or negative
| Category | Number of studies | Measured baseline participant characteristics |
|---|---|---|
| Positive outcomes | 68 | Heart‐rate variability, meditation practice frequency at home, meditation session attendance, implicit religiousness/spirituality, religion, coherence, sleep duration, mindfulness, visual imagery (during meditation), pleasantness (during meditation), curiosity, positive affect, well‐being, ambiguity tolerance, quality of life, responding to hypertension treatment, executive attention, focusing, health, pain control |
| Negative outcomes | 62 | Skin conductance, perceived pain, pain interference, drop‐out rate, perceived stress, PTSD severity, depression, trait anxiety, social anxiety, somatic anxiety, work hours, distress (during meditation), distress, negative affect, discomfort with emotion, worry, fatigue, anger, frequency of substance abuse, rumination, catastrophizing, |
The second column represents the number of studies per category and its sum is bigger than the total number of included studies (N = 51) as almost all studies had multiple outcomes. An outcome is categorized as positive if its increase has a positive impact on mental health or as negative if its increase meant a deterioration in mental heal.
Following this, we classified all meditation outcomes into two types: positive or negative (Table 4). They were classified as positive when an increase in scores reflected a positive impact on mental health (e.g., improved emotion regulation), and as negative when an increase in scores meant a deterioration in mental health (e.g., increased stress). Studies with outcomes that could not be classified as positive or negative were excluded from the analyses; this led to the exclusion of two studies with EEG measures.
Finally, we considered the moderators. As three out of our six moderators were categorical, they were coded as follows: sample type was coded as ‘non‐clinical’ or ‘clinical’ (samples that included only participants with a psychiatric or other medical diagnosis were considered clinical, while samples with healthy adults were considered non‐clinical); meditation type was coded as ‘mindfulness’, ‘transcendental meditation’, or ‘other type of meditation’; type of research design was coded as ‘RCT’ if the study was a randomized controlled trial or as ‘non‐RCT’ if another experimental design was employed.
Data handling and statistical analysis
A summary of data extraction and analysis can be found in Figure 2. Following data extraction and categorization of variables, effect sizes were calculated as Pearson’s r using Meta‐Calc (Rosenberg, Adams, & Gurevitch, 2000). If there were insufficient data to calculate effect sizes in the published studies, we contacted the authors. Similarly, for studies that included statistical corrections that reduced comparability across studies (e.g., including age as a covariate in all analyses), authors were contacted to obtain original data to calculate the uncorrected effect sizes. There were 79 studies that met our eligibility criteria, but we had to exclude 28 studies because the data could not be retrieved from its authors, leaving a total of 51 studies.
Figure 2.
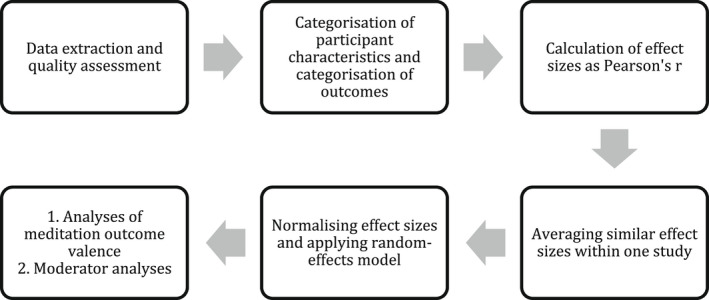
Schema for conducting data extraction and analysis. First, the relevant data were extracted from the 51 eligible studies and the quality of each study was rated. Second, we categorized all independent variables (i.e., participant characteristics) and dependent variables (i.e., outcome measure of meditation intervention), which resulted in thirteen categories of independent variables and two categories of dependent variables. Third, all extracted effect sizes were converted into Pearson’s r. Fourth, multiple effect sizes within one study were averaged when they were related to the same construct or the same category, when the effect sizes represented two or more follow‐ups, or when studies included three or more groups. Fifth, effect sizes were normalized through Fisher’s z transformation and a random‐effects model was applied in all analyses. Subgroup analyses were used to show the effect for each category of participant characteristics on two types of outcomes (i.e., positive and negative), and to test categorical moderators: sample type, research design, and meditation type. Finally, a meta‐regression was conducted to test for continuous moderators: sample size, study quality, and length of meditation.
When studies used different measures of the same construct (e.g., two pain scales) or of the same category (e.g., several measures within well‐being; see Table 3), the effects were averaged across measures. Similarly, in studies that had several follow‐ups, the effects were averaged across all post‐intervention time‐points. When studies included three or more groups, the meditation intervention group was compared against the combination of other groups (for a similar procedure see (Hoppenbrouwers, Bulten, & Brazil, 2016)).
Effect sizes were first imported into MetaWin, normalized through Fisher’s z‐transformation (Rosenberg et al., 2000). Publication bias was evaluated using funnel plots combined with Rosenthal’s fail‐safe N approach (Orwin, 1983). A funnel plot shows the mean effect size of eligible studies converted to Fisher’s z on the X‐axis and standard errors on the Y‐axis, along with the expected distribution of studies in the absence of bias (Sterne, Becker, & Egger, 2006). If studies were symmetrically distributed around the mean effect size, this shows there is no publication bias. Conversely, the fail‐safe N indicates the number of unpublished studies with non‐significant results that would be required to make the mean effect size non‐significant (Egger, Smith, Schneider, & Minder, 1997). As a rule of thumb, if the fail‐safe N is larger or equal to 5n + 10, where n is the number of studies, then the results are considered to be robust (Rosenberg, 2005). As this meta‐analysis includes 51 studies, the fail‐safe N had to be larger than 260 for the results to be considered robust. Note that a category was included in analysis only if it included a minimum of four studies.
The effects of participant characteristics on meditation outcomes were first examined with a univariate meta‐analysis using a random‐effects model (Rosenberg et al., 2000). Heterogeneity of scores between and within studies was assessed with the Q statistic (Cochran, 1954). The main downside of the univariate analysis is that it includes studies with multiple effect sizes, which violates the assumption of independence of effect sizes. When the effect sizes in a meta‐analysis are not independent, the estimated standard errors (SEs) on the average effect are generally under‐estimated (López‐López, Van den Noortgate, Tanner‐Smith, Wilson, & Lipsey, 2017). To ensure the robustness of our results, we ran an additional analysis based on a three‐level meta‐analysis model using metafor package in R (Cheung, 2019). The three‐level meta‐analysis provides more information on how the heterogeneity can be decomposed into 2 levels: level 2 represents the variance of effect sizes that stem from the same study, and level 3 represents the variance of effect sizes between studies (Table S3).
In addition to testing the effects of participant characteristics on meditation outcomes, we conducted moderator analyses. Three categorical moderators were examined with subgroup analyses, while three continuous moderators were examined with meta‐regression. The interpretation of the effect sizes is based on established guidelines by which the effects were considered small if r = .1, medium if r = .3, and large if r = .5 (Cohen, 2013). Significance was determined based on bootstrapped 95% confidence intervals (with 999 replications).
Results
Analyses based on thematic categories
Outcome valence: Do the effects of participant characteristics vary depending on whether mental health outcomes are negative or positive?
We tested whether each of the identified categories was linked to negative and/or positive effects on mental health after mediation. The mean effect size for participant characteristics on the negative effects of meditation was r = .12. The largest effect sizes were for stress‐related factors (r = .25), well‐being (r = .24), depression (r = .22), and psychopathology (r = .21), while the smallest were for demographics (r = .03), interpersonal (r = .03), and mindfulness (r = −.04) variables. Only four categories out of 12 had statistically significant effect sizes: psychopathology, well‐being, depression, and stress‐related factors. There were less than four studies available for medical conditions for this particular analysis, thus this variable was not examined (see Table 5).
Table 5.
The results of the meta‐analysis showing effect size (ES) of each category of participant characteristics on positive and negative outcomes, with corresponding 95% confidence intervals (CI)
| Participant characteristics category | Negative outcomes | Positive outcomes | ||||
|---|---|---|---|---|---|---|
| Number of ES | Mean ES | CI | Number of ES | Mean ES | CI | |
| Psychological traits | 5 | .14 | −.08, .37 | 10 | .02 | −.15, .15 |
| Anxiety | 5 | .20 | .00, .44 | N/A | N/A | N/A |
| Self‐concept | 4 | .29 | −.08, .52 | 6 | .05 | −.06, .17 |
| Interpersonal | 6 | .04 | −.21, .30 | 4 | .17 | .11, .21 |
| Psychopathology | 4 | .21 | .07, .42 | N/A | N/A | N/A |
| Belief system | 4 | .08 | −.03, .35 | N/A | N/A | N/A |
| Well‐being | 5 | .24 | .09, .50 | 8 | .19 | .09, .30 |
| Motivation | 4 | .06 | −.26, .41 | 6 | .23 | .05, .38 |
| Depression | 6 | .22 | .14.30 | 5 | .06 | −.03, .13 |
| Stress‐related factors | 4 | .25 | .09, .60 | 4 | .10 | .03, .26 |
| Demographics | 7 | .03 | −.04, .11 | 11 | .00 | −.19, .11 |
| Mindfulness | 5 | −.04 | −.25, .13 | 6 | .15 | .08, .21 |
| Medical conditions | N/A | N/A | N/A | 5 | .23 | .11, .34 |
| Overall | 65 | .13 | .06, .19 | 63 | .11 | .06, .15 |
N/A: analysis is not possible because less than four studies were available. Mean ES reported as Pearson’s r with significant results marked in bold. The number of effect sizes exceeds the number of samples because more than one participant characteristic from the same category was used in some studies (e.g., gender and age belong to the demographics category). Confidence intervals are 95% and bootstrapped.
The mean effect size for participant characteristics on the positive effects of meditation was r = .11 (CI 0.06, 0.15). Six out of 10 categories were significant: motivation (r = .23), medical conditions (r = .19), well‐being (r = .19), interpersonal (r = .17), mindfulness (r = .15), and stress‐related factors (r = .10), (see Table 5). The results were not carried out for three categories – anxiety, psychopathology, and belief system – because there were less than four studies available.
The analyses also revealed that the diversity in outcome measures was a large source of heterogeneity, as the Q statistic decreased when the data were split into studies with positive and negative outcomes (see Table 6). Therefore, although the overall analysis indicated that there was heterogeneity of effect sizes across studies, this was not the case once the total sample was divided into sub‐classes based on the different types of outcomes of meditation. Rosenthal’s fail‐safe N was large for both positive and negative outcomes (510 and 457, respectively), suggesting that the results are robust. When we compared the outcomes of this univariate analysis with a three‐level meta‐analysis, this confirmed the original effect sizes and provided more insight into heterogeneity. We found that 85% of the variation in effect sizes across studies is due to heterogeneity rather than chance, which supports the choice of the random‐effects model. Furthermore, we were able to identify the types of studies that have the largest percentage of variation between studies due to heterogeneity: RCTs (88%) and studies that examine positive health outcomes (85%). On the other hand, studies with non‐clinical samples (59%), non‐RCTs (57%), and studies that include types of meditation other than mindfulness or transcendental meditation (40%) have the largest percentage of variation within studies.
Table 6.
The results of the meta‐analysis showing effect sizes (ES), confidence intervals (CI), overall heterogeneity (Q), heterogeneity within studies (Qw), heterogeneity between studies (Qb), and fail‐safe Ns for the overall analysis, subgroup analyses, and moderator analyses
| ES | 95% CI | Q | Qw | Qb | Fail‐safe N | |
|---|---|---|---|---|---|---|
| Overall analysis | .11 | .08, .15 | 197.51 | 180.53 | 16.99 | 2568.1 |
| Negative outcome analysis | .13 | .06, .19 | 77.85 | 67.08 | 10.77 | 417.7 |
| Positive outcomes analysis | .11 | .06, .15 | 78.39 | 64.83 | 13.56 | 493.1 |
| Moderator analysis 1: research design | 220.02 | 219.96 | 0.06 | 2873.7 | ||
| RCT | .11 | .06, .17 | 124.71 | 111.20 | 13.52 | 780.4 |
| non‐RCT | .11 | .06, .15 | 88.80 | 88.62 | 0.18 | 514.6 |
| Moderator analysis 2: sample type | 225.48 | 221.15 | 4.33 | 2947.6 | ||
| clinical | .14 | .10, .19 | 86.51 | 75.85 | 10.66 | 909.3 |
| non‐clinical | .08 | .03, .13 | 127.59 | 127.47 | 0.12 | 434.7 |
| Moderator analysis 3: meditation type | 219.90 | 215.08 | 4.82 | 2872.0 | ||
| mindfulness | .09 | .06, .13 | 121.83 | 121.07 | 0.75 | 1215.9 |
| transcendental | .18 | .05, .27 | 18.15 | 16.80 | 1.36 | 43.8 |
| other | .16 | −.02., .32 | 23.31 | 18.52 | 4.78 | 25.4 |
| Moderator analysis 4: length of meditation | .11 | .08, .14 | 216.42 | 216.13 | 0.07 | 2822.0 |
| Moderator analysis 5: sample size | .11 | .08, .14 | 225.31 | 219.24 | 6.07 | 2945.3 |
| Moderator analysis 6: study quality | .11 | .08, .14 | 217.95 | 212.35 | 5.59 | 2845.5 |
Q statistic represents a composite measure of heterogeneity between (Qb) and heterogeneity within studies (Qw). Rosenthal’s fail‐safe N represents the required number of unpublished studies with non‐significant results that would make the mean effect size non‐significant, which should be over 260 in the case of a meta‐analysis of 51 studies. Confidence intervals (CI) are 95% and bootstrapped. Mean ES reported as Pearson’s r with significant results marked in bold.
Moderator analyses: Categorical moderators
Research design: Do participant characteristics have a larger effect in randomized controlled trials?
Types of research designs were coded as categorical variables to differentiate between randomized controlled trials and other research designs. The effect size in RCTs (r = .11, CI 0.06, 0.77) was almost identical to other study types (r = .11, CI 0.06, 0.15). The Q statistic was significant, indicating a large amount of heterogeneity based on study design. More specifically, there was a high amount of heterogeneity within and between the samples in RCTs, which suggests that included RCTs showed more diverse effect sizes, while studies employing a non‐RCT design had less variability in the effects of participant characteristics (see Table 6). Large fail‐safe numbers support the robustness of these results.
Sample type: Do participant characteristics have a larger effect in clinical or non‐clinical samples?
To test if participant type moderated the relationship between participant characteristics and meditation outcomes, we differentiated between clinical and non‐clinical samples. Although the effect size was larger for studies with clinical (r = .14, CI 0.10, 0.19) than non‐clinical samples (r = .08, CI 0.03, 0.13), both types showed significant effects of participant characteristics on meditation outcomes. The heterogeneity statistic was significant when studies were split based on the sample type, which suggests that the sample type was a source of heterogeneity (Table 6). The effect sizes of participant characteristics in studies with non‐clinical samples varied significantly, while the effect sizes of studies with diverse clinical samples were consistent. Large fail‐safe numbers support the robustness of these results.
Meditation type: Do participant characteristics have a larger effect in mindfulness meditation in comparison with other types of meditation?
Types of meditation were coded as categorical variables to differentiate between mindfulness, transcendental meditation, and other types of meditation. The lowest effect size was for mindfulness (r = .09, CI 0.06, 0.13), followed by other types of meditation (r = .16, CI −0.02, 0.32), and the largest for transcendental meditation (r = .18, CI 0.05, 0.28). However, participant characteristics had a significant effect on outcomes in studies that employed mindfulness or transcendental meditation, while this was not found for other types of meditation. Heterogeneity was significant only in studies that used mindfulness, while studies of transcendental meditation and other types of meditation show more consistent effect sizes, but also low fail‐safe numbers, which suggests that these results are not robust (see Table 6). Additionally, the funnel plot is symmetrical (Figure 3), which suggests the absence of bias and systematic heterogeneity.
Figure 3.
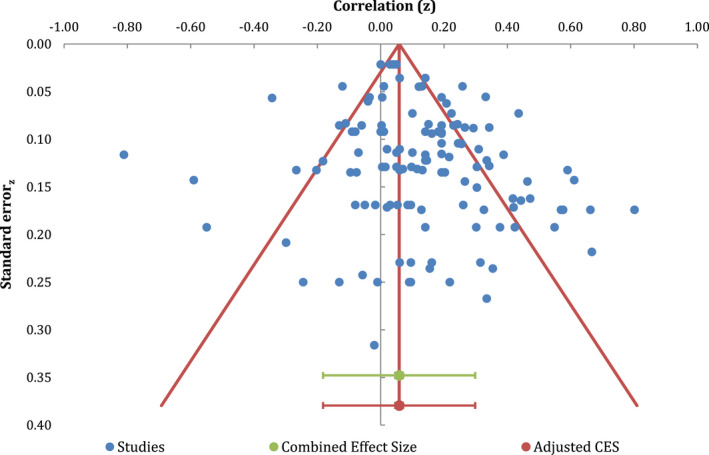
The funnel plot shows the overall mean effect size of eligible studies converted to Fisher’s z on the X‐axis and standard errors on the Y‐axis, along with the expected distribution of studies in the absence of bias.
Moderator analyses: Continuous moderators
Meta‐regression was conducted to examine three continuous moderators: sample size, length of meditation intervention, and study quality. We first tested whether sample size moderated the effect size of participant characteristics. Meta‐regression confirmed that participant characteristics had a smaller effect on meditation outcomes when studies had larger samples (p = .01). Next, we investigated whether the frequency of meditation intervention or practice moderated the effect size of participant characteristics. Meta‐regression results showed that the effect size of participant characteristics was not affected by the frequency of meditation practice (p = .79), which varied from 1 to 365 days. The third question concerned the moderating effect of the methodological quality of the study (for quality scores see Tables 1 and 2). Meta‐regression showed that the quality of the study moderated the effects of participant characteristics on meditation response so that studies with higher quality had lower effect sizes (p = .02). Fail‐safe N confirmed that the results are rigorous for all three meta‐regressions, but Q statistics point to significant heterogeneity, which indicates large variability in effect sizes (see Table 6).
Discussion
The present study shows that participant characteristics play a significant role in shaping responses to meditation. Here, we focused on participant characteristics as sources of variability in responses to meditation, though we acknowledge that contextual factors, such as characteristics of the meditation teacher or group processes, can also play a role.
Our results confirmed the impact of participant characteristics on negative and positive health outcomes with two robust data analyses: a univariate and three‐level meta‐analysis. Psychological traits, self‐concept, and demographics were the only non‐significant categories in all analyses. This suggests that the response to meditation is not significantly impacted by participants’ personality traits as operationalized in, for example, the Big Five theory of personality, nor to self‐concept variables such as self‐esteem or locus of control. In line with our findings, demographic variables have previously been found to not have a significant effect on the effect of meditation on health in clinical and non‐clinical populations (Goldberg et al., 2018; Khoury et al., 2015; Sedlmeier et al., 2012).
In contrast, two categories were significantly related to meditation outcomes in all analyses: well‐being and stress‐related factors. We found that participants with higher baseline levels of well‐being showed moderate increases for both negative and positive meditation outcomes. Similarly, participants with higher baseline levels of stress showed moderate increases in negative outcomes and small increases in positive outcomes. These results suggest that meditation has contrasting, even opposing effects for individuals with higher well‐being and higher stress levels. Some authors have argued that meditation, by making one acutely aware of certain thoughts and emotions, can be a difficult process for some (Creswell, Pacilio, Lindsay, & Brown, 2014; Farias & Wikholm, 2015).
There was another unexpected and somewhat counter‐intuitive result. Baseline levels of depression were only significantly related to negative outcomes. In other words, meditation practice or intervention is more likely to lead to negative outcomes for an individual reporting a higher level of depression. We need to qualify this result by looking at the individual studies that led to this result. Three out of the nine included studies in this category were conducted with participants with a diagnosis of current major depression episode (Ly et al., 2014) or a history of major depression (Geschwind, Peeters, Huibers, van Os, & Wichers, 2012; Zautra et al., 2008), while the six remaining studies included different clinical populations that often exhibit symptoms of depression, such as chronic pain conditions (Brotto, Basson, Smith, Driscoll, & Sadownik, 2015), breast cancer survivors (Tamagawa et al., 2015), or substance use disorders (Roos, Bowen, & Witkiewitz, 2017). This suggests that it is not depression per se, but depression as a comorbid factor that might interact negatively with meditation. This claim seemingly contradicts prior meta‐analytic findings showing that individuals with a current episode of depression can benefit from a meditation‐based intervention (Strauss, Cavanagh, Oliver, & Pettman, 2014). However, Strauss et al. (2014) did not directly examine if there was a relationship between the extent of depression symptoms that are present before the meditation intervention and the outcomes after the intervention, thus there remains a possibility that their data would show results similar to ours if the same research question was examined. However, it is important to emphasize that we cannot conclude that the symptoms of depression necessarily get worse because only two out of the nine studies measured that, while others measured negative outcomes such as stress or substance use. Another possible explanation of the association between baseline depression levels and negative outcomes is that participants with symptoms of depression experience an initial worsening of their mental health in the early stages of meditation practice, but then experience improvements in later stages if they manage to develop high acceptance. As none of the included studies that measured depression as a participant characteristic provided data for more than 8 weeks of practice nor examined acceptance as a mediator, we currently cannot examine this.
Based on previous studies, we had a clear hypothesis that people with higher trait anxiety would be more likely to experience a more positive response to meditation. However, there were fewer than four studies available that included these data, so we were not able to confirm nor dismiss this hypothesis. Instead, we were able to find that the association between anxiety and negative outcomes was non‐significant. Furthermore, there were several other categories of participant characteristics where we were not able to obtain results due to a lack of studies: interpersonal participants characteristics (regarding both positive and negative outcomes), psychopathology (and positive outcomes), belief systems (and positive outcomes), and medical conditions (and negative outcomes; see Table 5). It remains unknown how different the results of this study would be if we were able to include the additional 28 studies that met our eligibility criteria, but that failed to provide the necessary data to calculate effect sizes.
Overall, these results highlight the possibility that some individuals can react negatively to meditation. The negative effects of mind‐body interventions have been an uncomfortable and neglected topic within meditation research, though recently some studies have suggested that adverse experiences in meditators have a prevalence of about 8%, which is similar to that reported for psychotherapy practice (Farias et al., 2020). The prevalence and relevance of these negative effects are potentially underestimated. Two recent meta‐analyses of mindfulness‐based therapeutic interventions found that only 9 trials out of 47 (19%) (Goyal et al., 2014) and 36 trials out of 231 (16%) (Wong, Chan, Zhang, Lee, & Tsoi, 2018) reported adverse effects. There are also criticisms concerning the use of unreliable methods to address these negative effects (Lindahl, Britton, Cooper, & Kirmayer, 2021), and a tendency to frame these effects as difficulties during meditation which will eventually transform themselves into positive experiences (e.g., Chen, Qi, Hood, & Watson, 2011).
Looking at the other side of the spectrum, motivation, medical conditions, and interpersonal characteristics were significantly related to only positive outcomes. These results point at various interesting possibilities. First, it indicates that people with medical problems may particularly benefit from meditation. It would be interesting for future studies to look at the processes that potentially mediate this relationship, such as self‐regulation, or detachment from anxiety related to the medical condition. Second, it shows that interpersonal characteristics play a significant role in shaping meditation outcomes. A closer look at the studies involved shows that most of them focused on negative interpersonal factors, such as abuse, violence, and sexual trauma. This is in line with some research suggesting that individuals with a history of childhood trauma are more likely to benefit from a meditation‐based intervention when being treated for recurrent depression (Williams et al., 2014). Thirdly, motivational factors, such as positive attitudes and expectations of meditation, were associated with positive outcomes. This is an expected finding as it can be assumed that individuals who begin learning meditation with higher motivation and expectations of achieving benefits do actually show greater benefits. Nevertheless, this is an important result to consider, as few meditation studies have controlled for this variable. Those who have, though, have found that positive expectations of meditation outcomes play a significant role in the results of studies (Creswell et al., 2014).
We took a deeper look into the data by examining several moderators: research design, sample type, meditation type, length of meditation intervention, sample size, and study quality. The effects of participant characteristics on meditation outcomes were statistically significant concerning the type of research designs (RCTs or non‐RCTs), the types of samples (clinical or non‐clinical), and whether a study employed transcendental meditation or mindfulness.
The results of meta‐regression showed that participant characteristics have the same effect on the outcomes of meditation regardless of the length of meditation intervention, which ranged from 1 day to 1 year. This suggests that future studies could successfully study the effects of participant characteristics using brief meditations interventions because predictors of short‐term and long‐term outcomes of meditation are similar. On the other hand, participant characteristics had a smaller effect on meditation outcomes when studies had larger samples and higher methodological quality.
We found that, overall, the quality of studies was moderate. The most consistent flaw across studies was the lack of transparent reporting that would enable the assessment of all aspects of study quality. It is generally recommended to adhere to the Consolidated Standards of Reporting Trials (CONSORT) that has an extension for social and psychological interventions (Montgomery et al., 2018). Developing a reporting guideline that is specific to MBIs could improve the quality of research in the field and, in turn, contribute to estimating the effectiveness of MBIs more accurately.
One critical consideration is a large amount of variation in measures of individual differences in meditation research. To deal with this, we created categories based on previous research. There are inherent ambiguities in this process; for example, some could argue that ‘experience in group therapy’ should not belong to the category ‘well‐being’, but in the interpersonal category. We have dealt with this problem following standard protocols of inter‐rater reliability and discussion. Further variation in meditation literature was observed while examining different types of meditation, where the majority (68%) of eligible studies used mindfulness interventions. Notably, although 70% of those studies that used mindfulness interventions were following standardized 8‐week programs that are delivered in a group format (e.g., mindfulness‐based stress reduction or mindfulness‐based cognitive therapy), some studies used apps or other forms of self‐training via pre‐recorded mindfulness instructions that lasted less than 8 weeks. It is possible that different participant characteristics would be significant across different formats of mindfulness interventions, thus this remains to be examined by future studies.
Finally, we acknowledge that this meta‐analysis is the first one of its kind, which means that further work is required to validate its results and develop clear and precise clinical recommendations. One suggestion for a future meta‐analysis is to include individual‐level data, instead of group averages that were used here.
Conclusions
This meta‐analysis has shown that participant baseline characteristics significantly influence the response to mindfulness and transcendental meditation interventions. Although more work is needed to validate these results and develop clinical recommendations, our results suggest the importance of actively monitoring the experiences of individuals undertaking meditation interventions, particularly individuals with high levels of psychopathology and depression who are more likely to experience negative outcomes of meditation.
Conflict of interest
The authors declare that they have no conflict of interest.
Author contribution
Ivana Buric: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Software; Visualization; Writing – original draft; Writing – review & editing. Miguel Farias: Conceptualization; Supervision; Writing – review & editing. Josi Driessen: Data curation; Formal analysis; Methodology; Validation; Writing – review & editing. Inti Brazil: Conceptualization; Methodology; Software; Supervision; Writing – review & editing.
Ethical approval
The manuscript does not contain clinical studies or patient data.
Open research badges
This article has earned an Open Data Badge for making publicly available the digitally‐shareable data necessary to reproduce the reported results. The data is available at https://osf.io/nquwa/?view_only=53d1a09611c945cf8e115386e6898741.
Supporting information
Table S1. Summary of the results of all studies included in the meta‐analysis showing authors of each study, examined participant characteristic and outcomes of meditation, effect size (ES) converted to Pearson’s r, sample size, research design type, sample type, meditation type and length, and study quality estimated with tools by National Institutes of Health (ranging from 0 to 1).
Table S2. Characteristics of the studies included in the meta‐analysis (N = 50).
Table S3. Comparison of univariate and multivariate analysis showing mean effect sizes as Pearson’s r, estimated heterogeneity variance (EHV) and the relative heterogeneity statistic I 2.
Figure S1. Graphical representation of the subgroup analyses results showing categories of participant baseline that are associated with negative or positive outcomes of meditation.
Figure S2. The overall effects of participant characteristics by type of outcome measures, study design, sample type, and type of meditation.
Acknowledgements
Financial or material support was not received for this study.
Data availability statement
The data are available at the Open Science Framework website: https://osf.io/nquwa/?view_only=53d1a09611c945cf8e115386e6898741
References
References for all studies that were included in the meta‐analysis
- American Psychiatric Association . (1977). Position statement on meditation. American Journal of Psychiatry, 134(6), 720–720. 10.1176/ajp.134.6.720 [DOI] [Google Scholar]
- Baer, R. , Crane, C. , Miller, E. , & Kuyken, W. (2019). Doing no harm in mindfulness‐based programs: Conceptual issues and empirical findings. Clinical Psychology Review, 71, 101–114. 10.1016/j.cpr.2019.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazil, I. A. , van Dongen, J. D. M. , Maes, J. H. R. , Mars, R. B. , & Baskin‐Sommers, A. R. (2018). Classification and treatment of antisocial individuals: From behavior to biocognition. Neuroscience & Biobehavioral Reviews, 91, 259–277. 10.1016/j.neubiorev.2016.10.010 [DOI] [PubMed] [Google Scholar]
- Brotto, L. A. , Basson, R. , Smith, K. B. , Driscoll, M. , & Sadownik, L. (2015). Mindfulness‐based group therapy for women with provoked vestibulodynia. Mindfulness, 6, 417–432. 10.1007/s12671-013-0273-z [DOI] [Google Scholar]
- Buric, I. , Brazil, I. A. , & van Mulukom, V. (2021). Individual differences in meditation outcomes. In Farias M., Brazier D. & Lalljee M. (Eds.), The Oxford Handbook of Meditation (pp. 503–524). Oxford, UK: Oxford University Press. https://doi/org/10.1093/oxfordhb/9780198808640.013.26 [Google Scholar]
- Cebolla, A. , Demarzo, M. , Martins, P. , Soler, J. , & Garcia‐Campayo, J. (2017). Unwanted effects: Is there a negative side of meditation? A multicentre survey. PLoS One, 12(9), e0183137. 10.1371/journal.pone.0183137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Z. , Qi, W. , Hood, R. W. , & Watson, P. J. (2011). Common core thesis and qualitative and quantitative analysis of mysticism in Chinese Buddhist monks and nuns. Journal for the Scientific Study of Religion, 50(4), 654–670. 10.1111/j.1468-5906.2011.01606.x [DOI] [Google Scholar]
- Cheung, M. W.‐L. (2019). A guide to conducting a meta‐analysis with non‐independent effect sizes. Neuropsychology Review, 29(4), 387–396. 10.1007/s11065-019-09415-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa, A. , & Serretti, A. (2009). Mindfulness‐based stress reduction for stress management in healthy people: A review and meta‐analysis. The Journal of Alternative and Complementary Medicine, 15(5), 593–600. 10.1089/acm.2008.0495 [DOI] [PubMed] [Google Scholar]
- Cochran, W. G. (1954). The combination of estimates from different experiments. Biometrics, 10(1), 101. 10.2307/3001666 [DOI] [Google Scholar]
- Cohen, J. (2013). Statistical power analysis for the behavioral sciences. New York, NY: Routledge. 10.4324/9780203771587 [DOI] [Google Scholar]
- Creswell, J. D. , Pacilio, L. E. , Lindsay, E. K. , & Brown, K. W. (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12. 10.1016/j.psyneuen.2014.02.007 [DOI] [PubMed] [Google Scholar]
- Cuthbert, B. N. , & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126. 10.1186/1741-7015-11-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, R. J. , & Kaszniak, A. W. (2015). Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist, 70, 581–592. 10.1037/a0039512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger, M. , Smith, G. D. , Schneider, M. , & Minder, C. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ, 315, 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias, M. , Maraldi, E. , Wallenkampf, K. , & Lucchetti, G. (2020). Adverse events in meditation practices and meditation‐based therapies: a systematic review. Acta Psychiatrica Scandinavica, 142, 374–393. 10.1111/acps.13225 [DOI] [PubMed] [Google Scholar]
- Farias, M. , & Wikholm, C. (2015). The Buddha pill: Can meditation change you? London, UK: Watkins Publishing. ISBN: 9781780287188 [Google Scholar]
- Geschwind, N. , Peeters, F. , Huibers, M. , van Os, J. , & Wichers, M. (2012). Efficacy of mindfulness‐based cognitive therapy in relation to prior history of depression: Randomised controlled trial. British Journal of Psychiatry, 201, 320–325. 10.1192/bjp.bp.111.104851 [DOI] [PubMed] [Google Scholar]
- Goldberg, S. B. , Tucker, R. P. , Greene, P. A. , Davidson, R. J. , Wampold, B. E. , Kearney, D. J. , & Simpson, T. L. (2018). Mindfulness‐based interventions for psychiatric disorders: A systematic review and meta‐analysis. Clinical Psychology Review, 59, 52–60. 10.1016/j.cpr.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal, M. , Singh, S. , Sibinga, E. M. S. , Gould, N. F. , Rowland‐Seymour, A. , Sharma, R. , … Haythornthwaite, J. A. (2014). Meditation programs for psychological stress and well‐being: A systematic review and meta‐analysis. JAMA Internal Medicine, 174, 357. 10.1001/jamainternmed.2013.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges, L. V. , & Olkin, I. (1985). Statistical methodology in meta‐analysis. Orlando, Florida: Academic Press, INC. 10.1016/C2009-0-03396-0 [DOI] [Google Scholar]
- Hofmann, S. G. , & Gómez, A. F. (2017). Mindfulness‐based interventions for anxiety and depression. Psychiatric Clinics of North America, 40, 739–749. 10.1016/j.psc.2017.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppenbrouwers, S. S. , Bulten, B. H. , & Brazil, I. A. (2016). Parsing fear: A reassessment of the evidence for fear deficits in psychopathy. Psychological Bulletin, 142, 573–600. 10.1037/bul0000040 [DOI] [PubMed] [Google Scholar]
- Khoury, B. , Sharma, M. , Rush, S. E. , & Fournier, C. (2015). Mindfulness‐based stress reduction for healthy individuals: A meta‐analysis. Journal of Psychosomatic Research, 78, 519–528. 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Kok, B. E. , & Singer, T. (2017). Phenomenological fingerprints of four meditations: Differential state changes in affect, mind‐wandering, meta‐cognition, and interoception before and after daily practice across 9 months of training. Mindfulness, 8(1), 218–231. 10.1007/s12671-016-0594-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl, J. R. , Britton, W. B. , Cooper, D. J. , & Kirmayer, L. J. (2021). Challenging and adverse meditation experiences: Toward a person‐centered approach. In Farias M., Lalljee M. & Brazier D. (Eds.), The Oxford Handbook of Meditation, 841–865. Oxford, UK: Oxford University Press. [Google Scholar]
- Lindahl, J. R. , Fisher, N. E. , Cooper, D. J. , Rosen, R. K. , & Britton, W. B. (2017). The varieties of contemplative experience: A mixed‐methods study of meditation‐related challenges in Western Buddhists. PLoS One, 12, e0176239. 10.1371/journal.pone.0176239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López‐López, J. A. , Van den Noortgate, W. , Tanner‐Smith, E. E. , Wilson, S. J. , & Lipsey, M. W. (2017). Assessing meta‐regression methods for examining moderator relationships with dependent effect sizes: A Monte Carlo simulation. Research Synthesis Methods, 8, 435–450. 10.1002/jrsm.1245 [DOI] [PubMed] [Google Scholar]
- Ly, K. H. , Trüschel, A. , Jarl, L. , Magnusson, S. , Windahl, T. , Johansson, R. , … Andersson, G. (2014). Behavioural activation versus mindfulness‐based guided self‐help treatment administered through a smartphone application: A randomised controlled trial. British Medical Journal Open, 4(1), e003440. 10.1136/bmjopen-2013-003440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery, P. , Grant, S. , Mayo‐Wilson, E. , Macdonald, G. , Michie, S. , Hopewell, S. , & Moher, D. (2018). Reporting randomised trials of social and psychological interventions: The CONSORT‐SPI 2018 Extension. Trials, 19(1), 407. 10.1186/s13063-018-2733-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orme‐Johnson, D. W. , & Barnes, V. A. (2013). Effects of the transcendental meditation technique on trait anxiety: A meta‐analysis of randomized controlled trials. The Journal of Alternative and Complementary Medicine, 20, 330–341. 10.1089/acm.2013.0204 [DOI] [PubMed] [Google Scholar]
- Orwin, R. G. (1983). A fail‐safe N for effect size in meta‐analysis. Journal of Educational Statistics, 8(2), 157–159. 10.3102/10769986008002157 [DOI] [Google Scholar]
- Perry, M. , Swain, S. , Kemmis‐Betty, S. , Cooper, P. & on behalf of the Guideline Development Group (2014). Multiple sclerosis: summary of NICE guidance. BMJ, 349, g5701. 10.1136/bmj.g5701 [DOI] [PubMed] [Google Scholar]
- Piet, J. , & Hougaard, E. (2011). The effect of mindfulness‐based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta‐analysis. Clinical Psychology Review, 31, 1032–1040. 10.1016/j.cpr.2011.05.002 [DOI] [PubMed] [Google Scholar]
- Pilling, S. , Anderson, I. , Goldberg, D. , Meader, N. , & Taylor, C. & On behalf of the two guideline development groups (2009). Depression in adults, including those with a chronic physical health problem: summary of NICE guidance. BMJ, 339, b4108. 10.1136/bmj.b4108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos, C. R. , Bowen, S. , & Witkiewitz, K. (2017). Baseline patterns of substance use disorder severity and depression and anxiety symptoms moderate the efficacy of mindfulness‐based relapse prevention. Journal of Consulting and Clinical Psychology, 85, 1041–1051. 10.1037/ccp0000249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg, M. S. (2005). The file‐drawer problem revisited: a general weighted method for calculating fail‐safe numbers in meta‐analysis. Evolution, 59(2), 464–468. 10.1111/j.0014-3820.2005.tb01004.x [DOI] [PubMed] [Google Scholar]
- Rosenberg, M. S. , Adams, D. C. , & Gurevitch, J. (2000). MetaWin: Statistical software for meta‐analysis. Sunderland, England: Sinauer Associates. ISBN: 0878937609 [Google Scholar]
- Schlosser, M. , Sparby, T. , Vörös, S. , Jones, R. , & Marchant, N. L. (2019). Unpleasant meditation‐related experiences in regular meditators: Prevalence, predictors, and conceptual considerations. PLoS One, 14, e0216643. 10.1371/journal.pone.0216643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlmeier, P. , Eberth, J. , Schwarz, M. , Zimmermann, D. , Haarig, F. , Jaeger, S. , & Kunze, S. (2012). The psychological effects of meditation: A meta‐analysis. Psychological Bulletin, 138, 1139–1171. 10.1037/a0028168 [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. C. , Becker, B. J. , & Egger, M. (2006). The funnel plot. In Rothstein H. R., Sutton A. J. & Borenstein M. (Eds.), Publication bias in meta‐analysis (pp. 73–98). Chichester, England: John Wiley & Sons, Ltd. 10.1002/0470870168.ch5 [DOI] [Google Scholar]
- Strauss, C. , Cavanagh, K. , Oliver, A. , & Pettman, D. (2014). Mindfulness‐based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta‐analysis of randomised controlled trials. PLoS One, 9, e96110. 10.1371/journal.pone.0096110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamagawa, R. , Speca, M. , Stephen, J. , Pickering, B. , Lawlor‐Savage, L. , & Carlson, L. E. (2015). Predictors and effects of class attendance and home practice of yoga and meditation among breast cancer survivors in a mindfulness‐based cancer recovery (MBCR) program. Mindfulness, 6, 1201–1210. 10.1007/s12671-014-0381-4 [DOI] [Google Scholar]
- Van Dam, N. T. , van Vugt, M. K. , Vago, D. R. , Schmalzl, L. , Saron, C. D. , Olendzki, A. , … Meyer, D. E. (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 13(1), 36–61. 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veehof, M. M. , Trompetter, H. R. , Bohlmeijer, E. T. , & Schreurs, K. M. G. (2016). Acceptance‐ and mindfulness‐based interventions for the treatment of chronic pain: A meta‐analytic review. Cognitive Behaviour Therapy, 45(1), 5–31. 10.1080/16506073.2015.1098724 [DOI] [PubMed] [Google Scholar]
- Williams, J. M. G. , Crane, C. , Barnhofer, T. , Brennan, K. , Duggan, D. S. , Fennell, M. J. V. , … Russell, I. T. (2014). Mindfulness‐based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82, 275–286. 10.1037/a0035036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, S. Y. S. , Chan, J. Y. C. , Zhang, D. , Lee, E. K. P. , & Tsoi, K. K. F. (2018). The safety of mindfulness‐based interventions: A systematic review of randomized controlled trials. Mindfulness, 9, 1344–1357. 10.1007/s12671-018-0897-0 [DOI] [Google Scholar]
- Zautra, A. J. , Davis, M. C. , Reich, J. W. , Nicassario, P. , Tennen, H. , Finan, P. , … Irwin, M. R. (2008). Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology, 76, 408–421. 10.1037/0022-006X.76.3.408 [DOI] [PubMed] [Google Scholar]
- Zoogman, S. , Goldberg, S. B. , Hoyt, W. T. , & Miller, L. (2015). Mindfulness Interventions with Youth: A Meta‐Analysis. Mindfulness, 6, 290–302. 10.1007/s12671-013-0260-4 [DOI] [Google Scholar]
- Azam, M. A. , Katz, J. , Mohabir, V. , & Ritvo, P. (2016). Individuals with tension and migraine headaches exhibit increased heart rate variability during post‐stress mindfulness meditation practice but a decrease during a post‐stress control condition – A randomized, controlled experiment. International Journal of Psychophysiology, 110, 66–74. 10.1016/j.ijpsycho.2016.10.011 [DOI] [PubMed] [Google Scholar]
- Cohn, M. A. , & Fredrickson, B. L. (2010). In search of durable positive psychology interventions: Predictors and consequences of long‐term positive behavior change. The Journal of Positive Psychology, 5, 355–366. 10.1080/17439760.2010.508883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordon, S. L. , Brown, K. W. , & Gibson, P. R. (2009). The role of mindfulness‐based stress reduction on perceived stress: Preliminary evidence for the moderating role of attachment style. Journal of Cognitive Psychotherapy, 23(3), 258–269. 10.1891/0889-8391.23.3.258 [DOI] [Google Scholar]
- Crandall, A. , Cheung, A. , Young, A. , & Hooper, A. P. (2019). Theory‐based predictors of mindfulness meditation mobile app usage: A survey and cohort study. JMIR MHealth and UHealth, 7(3), e10794. 10.2196/10794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crescentini, C. , Urgesi, C. , Campanella, F. , Eleopra, R. , & Fabbro, F. (2014). Effects of an 8‐week meditation program on the implicit and explicit attitudes toward religious/spiritual self‐representations. Consciousness and Cognition, 30, 266–280. 10.1016/j.concog.2014.09.013 [DOI] [PubMed] [Google Scholar]
- Day, M. A. , Halpin, J. , & Thorn, B. E. (2016). An empirical examination of the role of common factors of therapy during a mindfulness‐based cognitive therapy intervention for headache pain. the Clinical Journal of Pain, 32, 420–427. 10.1097/AJP.0000000000000277 [DOI] [PubMed] [Google Scholar]
- Delmonte, M. M. (1985). Effects of expectancy on physiological responsivity in novice meditators. Biological Psychology, 21, 107–121. 10.1016/0301-0511(85)90009-2 [DOI] [PubMed] [Google Scholar]
- Delmonte, M. M. (1988). Personality correlates of meditation practice frequency and dropout in an outpatient population. Journal of Behavioral Medicine, 11, 593–597. 10.1007/BF00844908 [DOI] [PubMed] [Google Scholar]
- Delmonte, M. M. (1981). Expectation and meditation. Psychological Reports, 49, 699–709. 10.2466/pr0.1981.49.3.699 [DOI] [Google Scholar]
- Dobkin, P. L. , Zhao, Q. , & Monshat, K. (2017). Who experiences depressive symptoms following mindfulness‐based stress reduction and why? International Journal of Whole Person Care, 4(1), 13–31. 10.26443/ijwpc.v4i1.123 [DOI] [Google Scholar]
- Felleman, B. I. , Stewart, D. G. , Simpson, T. L. , Heppner, P. S. , & Kearney, D. J. (2016). Predictors of depression and PTSD treatment response among veterans participating in mindfulness‐based stress reduction. Mindfulness, 7, 886–895. 10.1007/s12671-016-0527-7 [DOI] [Google Scholar]
- Gawrysiak, M. J. , Leong, S. H. , Grassetti, S. N. , Wai, M. , Shorey, R. C. , & Baime, M. J. (2016). Dimensions of distress tolerance and the moderating effects on mindfulness‐based stress reduction. Anxiety, Stress, & Coping, 29, 552–560. 10.1080/10615806.2015.1085513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg, J. , Datta, T. , Shapero, B. G. , Sevinc, G. , Mischoulon, D. , & Lazar, S. W. (2018). Compassionate hearts protect against wandering minds: Self‐compassion moderates the effect of mind‐wandering on depression. Spirituality in Clinical Practice, 5, 155–169. 10.1037/scp0000168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeson, J. M. , Smoski, M. J. , Suarez, E. C. , Brantley, J. G. , Ekblad, A. G. , Lynch, T. R. , & Wolever, R. Q. (2015). Decreased symptoms of depression after mindfulness‐based stress reduction: Potential moderating effects of religiosity, spirituality, trait mindfulness, sex, and age. The Journal of Alternative and Complementary Medicine, 21, 166–174. 10.1089/acm.2014.0285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeson, J. M. , Webber, D. M. , Smoski, M. J. , Brantley, J. G. , Ekblad, A. G. , Suarez, E. C. , & Wolever, R. Q. (2011). Changes in spirituality partly explain health‐related quality of life outcomes after Mindfulness‐Based Stress Reduction. Journal of Behavioral Medicine, 34, 508–518. 10.1007/s10865-011-9332-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heide, F. J. , Wadlington, W. L. , & Lundy, R. M. (1980). Hypnotic responsivity as a predictor of outcome in meditation. International Journal of Clinical and Experimental Hypnosis, 28, 358–366. 10.1080/00207148008409864 [DOI] [PubMed] [Google Scholar]
- Herdt, J. , Bührlen, B. , Bader, K. , & Hänny, C. (2012). Participation in an adapted version of MBCT in psychiatric care. Mindfulness, 3, 218–226. 10.1007/s12671-012-0120-7 [DOI] [Google Scholar]
- Hülsheger, U. R. , Feinholdt, A. , & Nübold, A. (2015). A low‐dose mindfulness intervention and recovery from work: Effects on psychological detachment, sleep quality, and sleep duration. Journal of Occupational and Organizational Psychology, 88(3), 464–489. 10.1111/joop.12115 [DOI] [Google Scholar]
- Jazaieri, H. , Lee, I. A. , Goldin, P. R. , & Gross, J. J. (2016). Pre‐treatment social anxiety severity moderates the impact of mindfulness‐based stress reduction and aerobic exercise. Psychology and Psychotherapy: Theory, Research and Practice, 89(2), 229–234. 10.1111/papt.12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat‐Zinn, J. , & Chapman‐Waldrop, A. (1988). Compliance with an outpatient stress reduction program: Rates and predictors of program completion. Journal of Behavioral Medicine, 11(4), 333–352. 10.1007/bf00844934 [DOI] [PubMed] [Google Scholar]
- Kharlas, D. A. , & Frewen, P. (2016). Trait mindfulness correlates with individual differences in multisensory imagery vividness. Personality and Individual Differences, 93, 44–50. 10.1016/j.paid.2015.09.027 [DOI] [Google Scholar]
- Lee, K. H. , & Bowen, S. (2015). Relation between personality traits and mindfulness following mindfulness‐based training: A study of incarcerated individuals with drug abuse disorders in Taiwan. International Journal of Mental Health and Addiction, 13(3), 413–421. 10.1007/s11469-014-9533-y [DOI] [Google Scholar]
- Logie, K. , & Frewen, P. (2015). Self/other referential processing following mindfulness and loving‐kindness meditation. Mindfulness, 6(4), 778–787. 10.1007/s12671-014-0317-z [DOI] [Google Scholar]
- Mak, W. W. , Tong, A. C. , Yip, S. Y. , Lui, W. W. , Chio, F. H. , Chan, A. T. , & Wong, C. C. (2018). Efficacy and moderation of mobile app‐based programs for mindfulness‐based training, self‐compassion training, and cognitive behavioral psychoeducation on mental health: Randomized controlled noninferiority trial. JMIR Mental Health, 5(4), e8597. 10.2196/mental.8597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak, J. , Probst, T. , Heidenreich, T. , Bissantz, N. , & Schramm, E. (2016). Mindfulness‐based cognitive therapy and a group version of the cognitive behavioral analysis system of psychotherapy for chronic depression: Follow‐up data of a randomized controlled trial and the moderating role of childhood adversities. Psychotherapy and Psychosomatics, 85, 378–380. 10.1159/000447014 [DOI] [PubMed] [Google Scholar]
- National Institutes of Health . (2014). Study quality assessment tools. https://www.nhlbi.nih.gov/health‐topics/study‐quality‐assessment‐tools
- Nguyen‐Feng, V. N. , Greer, C. S. , & Frazier, P. (2017). Using online interventions to deliver college student mental health resources: Evidence from randomized clinical trials. Psychological Services, 14, 481–489. 10.1037/ser0000154 [DOI] [PubMed] [Google Scholar]
- Nguyen‐Feng, V. N. , Frazier, P. A. , Greer, C. S. , Meredith, L. , Howard, K. , & Paulsen, J. (2016). Testing the efficacy of three brief web‐based interventions for reducing distress among interpersonal violence survivors. Translational Issues in Psychological Science, 2(4), 439–448. 10.1037/tps0000099 [DOI] [Google Scholar]
- Oken, B. S. , Goodrich, E. , Klee, D. , Memmott, T. , & Proulx, J. (2018). Predictors of improvements in mental health from mindfulness meditation in stressed older adults. Alternative Therapies in Health and Medicine, 24(1), 48–55. [PMC free article] [PubMed] [Google Scholar]
- Pace, T. W. W. , Negi, L. T. , Adame, D. D. , Cole, S. P. , Sivilli, T. I. , Brown, T. D. , … Raison, C. L. (2009). Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology, 34(1), 87–98. 10.1016/j.psyneuen.2008.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace, T. W. W. , Negi, L. T. , Sivilli, T. I. , Issa, M. J. , Cole, S. P. , Adame, D. D. , & Raison, C. L. (2010). Innate immune, neuroendocrine and behavioral responses to psychosocial stress do not predict subsequent compassion meditation practice time. Psychoneuroendocrinology, 35, 310–315. 10.1016/j.psyneuen.2009.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, Y.‐J. , & Park, Y.‐B. (2012). Clinical utility of paced breathing as a concentration meditation practice. Complementary Therapies in Medicine, 20, 393–399. 10.1016/j.ctim.2012.07.008 [DOI] [PubMed] [Google Scholar]
- Prins, B. , Decuypere, A. , & Van Damme, S. (2014). Effects of mindfulness and distraction on pain depend upon individual differences in pain catastrophizing: An experimental study: Effects of mindfulness versus distraction on pain. European Journal of Pain, 18, 1307–1315. 10.1002/j.1532-2149.2014.491.x [DOI] [PubMed] [Google Scholar]
- Reich, R. R. , Lengacher, C. A. , Kip, K. E. , Shivers, S. C. , Schell, M. J. , Shelton, M. M. , Widen, R. H. , Newton, C. , Barta, M. K. , Paterson, C. L. , & Farias, J. R. (2014). Baseline immune biomarkers as predictors of MBSR (BC) treatment success in off‐treatment breast cancer patients. Biological Research for Nursing, 16(4), 429–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich, J. , Yates, W. , & Nduaguba, M. (1989). Prevalence of DSM‐III personality disorders in the community. Social Psychiatry and Psychiatric Epidemiology, 24(1), 12–16. 10.1007/BF01788194 [DOI] [PubMed] [Google Scholar]
- Rohsenow, D. J. , Smith, R. E. , & Johnson, S. (1985). Stress management training as a prevention program for heavy social drinkers: Cognitions, affect, drinking, and individual differences. Addictive Behaviors, 10(1), 45–54. 10.1016/0306-4603(85)90052-8 [DOI] [PubMed] [Google Scholar]
- Rojiani, R. , Santoyo, J. F. , Rahrig, H. , Roth, H. D. , & Britton, W. B. (2017). Women benefit more than men in response to college‐based meditation training. Frontiers in Psychology, 8. 10.3389/fpsyg.2017.00551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig, S. , Greeson, J. M. , Reibel, D. K. , Green, J. S. , Jasser, S. A. , & Beasley, D. (2010). Mindfulness‐based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research, 68(1), 29–36. 10.1016/j.jpsychores.2009.03.010 [DOI] [PubMed] [Google Scholar]
- Sass, S. M. , Berenbaum, H. , & Abrams, E. M. (2013). Discomfort with emotion moderates distress reduction in a brief mindfulness intervention. International Journal of Behavioral Consultation and Therapy, 7, 24–27. 10.1037/h0100962 [DOI] [Google Scholar]
- Seer, P. , & Raeburn, J. M. (1980). Meditation training and essential hypertension: A methodological study. Journal of Behavioral Medicine, 3(1), 59–71. 10.1007/BF00844914 [DOI] [PubMed] [Google Scholar]
- Shapiro, S. L. , Brown, K. W. , Thoresen, C. , & Plante, T. G. (2011). The moderation of Mindfulness‐based stress reduction effects by trait mindfulness: Results from a randomized controlled trial. Journal of Clinical Psychology, 67, 267–277. 10.1002/jclp.20761 [DOI] [PubMed] [Google Scholar]
- Smith, J. C. (1978). Personality correlates of continuation and outcome in meditation and erect sitting control treatments. Journal of Consulting and Clinical Psychology, 46(2), 272–279. 10.1037/0022-006X.46.2.272 [DOI] [PubMed] [Google Scholar]
- Takahashi, T. , Murata, T. , Hamada, T. , Omori, M. , Kosaka, H. , Kikuchi, M. , … Wada, Y. (2005). Changes in EEG and autonomic nervous activity during meditation and their association with personality traits. International Journal of Psychophysiology, 55(2), 199–220. 10.1016/j.ijpsycho.2004.07.004 [DOI] [PubMed] [Google Scholar]
- Watier, N. , & Dubois, M. (2016). The effects of a brief mindfulness exercise on executive attention and recognition memory. Mindfulness, 7, 745–753. 10.1007/s12671-016-0514-z [DOI] [Google Scholar]
- Weinstein, M. , & Smith, J. C. (1992). Isometric squeeze relaxation (Progressive Relaxation) Vs meditation: Absorption and focusing as predictors of state effects. Perceptual and Motor Skills, 75(3_suppl), 1263–1271. 10.2466/pms.1992.75.3f.1263 [DOI] [PubMed] [Google Scholar]
- Zalta, A. K. , Held, P. , Smith, D. L. , Klassen, B. J. , Lofgreen, A. M. , Normand, P. S. , … Karnik, N. S. (2018). Evaluating patterns and predictors of symptom change during a three‐week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18(1). 10.1186/s12888-018-1816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuroff, D. C. , & Schwarz, J. C. (1978). Effects of transcendental meditation and muscle relaxation on trait anxiety, maladjustment, locus of control, and drug use. Journal of Consulting and Clinical Psychology, 46, 264–271. 10.1037/0022-006X.46.2.264 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary of the results of all studies included in the meta‐analysis showing authors of each study, examined participant characteristic and outcomes of meditation, effect size (ES) converted to Pearson’s r, sample size, research design type, sample type, meditation type and length, and study quality estimated with tools by National Institutes of Health (ranging from 0 to 1).
Table S2. Characteristics of the studies included in the meta‐analysis (N = 50).
Table S3. Comparison of univariate and multivariate analysis showing mean effect sizes as Pearson’s r, estimated heterogeneity variance (EHV) and the relative heterogeneity statistic I 2.
Figure S1. Graphical representation of the subgroup analyses results showing categories of participant baseline that are associated with negative or positive outcomes of meditation.
Figure S2. The overall effects of participant characteristics by type of outcome measures, study design, sample type, and type of meditation.
Data Availability Statement
The data are available at the Open Science Framework website: https://osf.io/nquwa/?view_only=53d1a09611c945cf8e115386e6898741


