Abstract
Health systems rely on the unpaid work of family caregivers. Nevertheless, demographic changes suggest a shortage of caregivers in the near future, which can constrain the long‐term care policy in many countries. In order to find ways to support family caregivers, a primary effort would be to estimate how much their work is worth. This paper estimates the economic value of long‐term family caregivers and how these costs would be shared by the health system, the social insurances and the cared‐for person in the absence of informal caregivers. We use data of 717 family caregivers of persons with spinal cord injury (SCI) in Switzerland. We implemented the proxy‐good method and estimated the market value of their work if performed by professional caregivers. Our results show that family caregivers in the sample spent an average of 27 hr per week caring for a relative for almost 12 years. This work, if undertaken by professional home care, has a market value of CHF 62,732 (EUR 56,455) per year. In the absence of family caregivers, these costs should be financed by the health insurances (47%), by the cared‐for person (24%) and by the social insurances (29%). It is in the best interest of the cared‐for person and of the healthcare and social systems to keep a sustained supply of family caregivers. One option is finding ways to recognise and compensate them for their work and make it less cumbersome.
Keywords: chronic illness and disability, family caregivers, health economics, health systems, long‐term care, social care
What is known about this topic?
Demographic dynamics forecast a sharp increase in the care needs of the population.
A big part of care is undertaken by family caregivers, whose work is mostly unpaid and unrecognised.
Existing studies have limited data on the caregiving process. Thus, estimates of the economic value are a simplification of the work performed by family caregivers.
What this paper adds?
We use data of persons with spinal cord injury (SCI), which is a long‐term, multimorbid condition that requires frequent care. Our results can serve as an upper bound estimated for the needs of care in other long‐term health conditions, and even in the ageing population.
We use detailed data of the caregiving process, which includes the time of care, and the complexity of tasks family caregivers perform on a regular basis.
Following the Swiss long‐term care policy, this study estimates what it would cost to the Swiss health and social systems to replace the work undertaken by family caregivers.
1. INTRODUCTION
Demographic changes together with the prevalence of chronic illnesses forecast a sharp increase in the need of long‐term care, which is generally undertaken by unpaid family caregivers (Nowossadeck, 2013). Parallelly, single‐person households are more common (Snell, 2017), women are participating more in the labour market (Hirst, 2001; Jensen, 2012; Ortiz‐Ospina & Sandra, 2017), and the fertility rate is falling (Roser, 2014), which forecast a steady decline in the supply of family caregivers (Broese van Groenou & De Boer, 2016). In their absence, the healthcare system has to rethink its long‐term care policy and transition to the provision of professional home care.
The objective of this paper is to estimate the economic value of family caregivers of persons with spinal cord injury (SCI) in Switzerland. We estimated the economic value as how much it would cost to the health and social systems to replace the work undertaken by family caregivers. SCI is of special interest to the study of health systems and long‐term care policy as it is an irreversible multimorbid condition that requires frequent, specialised and non‐specialised medical care. Even though the incidence of SCI is quite low, the associated health and social costs are among the highest (Kang et al., 2017; Yoon et al., 2018). This group suffers from a series of comorbidities, which makes their main medical contact general physician or primary care providers (Gemperli et al., 2017). Compared to ageing population, the most common secondary health conditions this group faces include urinary tract infections, spasticity, constipation, chronic pain, sexual disfunction, fatigue, mental health disorders, among others (Brinkhof et al., 2016). Thus, the work undertaken by family caregivers of persons with SCI can be seen as an upper bound for other health conditions. Caregivers of persons with SCI not only look after persons with a high level of physical impairment (paraplegia/tetraplegia), but they also undertake a broad range of caring tasks on a regular basis. The tasks family caregivers perform go from support with eating and drinking, to more complex tasks like bowel management (Huang et al., 2019; Smith et al., 2016). Compared to other long‐term caregivers, family caregivers of persons with SCI spend several years as caregivers, and devote more hours in caregiving tasks. (Gemperli et al., 2020).
The advantage of this study is that it has comprehensive information about the caregiving process. We use disaggregated data on the type of tasks and on the time family members devote in a week to caregiving duties. This information put together with the long‐term care policy in Switzerland, which regulates the caregiving tasks covered by the insurances, as well as the hourly pricing when the tasks are performed by professional caregivers, made it possible to estimate the costs to replace the work undertaken by family caregivers. Thus, our estimates can serve as a good proxy to forecast caring needs in other long‐term health conditions, and even among the ageing population.
Related literature has estimated the economic value of family caregivers of older adults (Arno et al., 1999; van den Berg et al., 2005; Longacre et al., 2016; Paraponaris et al., 2012), and of caregivers of people with specific health conditions like cancer (Li et al., 2013), or schizophrenia (Pletscher et al., 2014). The study that is closest to ours, estimated the economic value of family caregivers of persons with dementia in CHF 55,300 per year (EUR 49,800), value that accounted for about 90% of the total costs for dementia in Switzerland (Kraft et al., 2010). Due to the lack of detailed data on the caregiving process, there are few studies on highly burdened long‐term family caregivers that take into account the number of caregiving hours per type of tasks. The existing evidence on the economic value of family caregivers show a high variation, which is related to the country of analysis, the existing long‐term care policy, and the valuation method (van den Berg et al., 2005; de Meijer et al., 2010; Oliva‐Moreno et al., 2017). Some studies estimated the work undertaken by family caregivers by using the hourly wage of nurses or external housekeepers. This method, however, is an underestimation of the work family caregivers undertake, as it reduces caregiving to a number of hours of care and disregards the complexity of the caregiving tasks.
It is important for the health and social system to estimate how much the work of family caregivers is worth in the market in order to forecast how many resources are needed in cases where there is no family caregiver. By knowing their economic value, it is possible to design policies to better support family caregivers and guarantee their lasting involvement in the caregiving process when desirable. Supporting family caregivers will provide recognition to their work, and it will also encourage the system to reform its long‐term care policy in order to adapt to the fast demographic changes (Donelan et al., 2002; Gibson & Houser, 2007). Otherwise, the growing health expenditure will be unable to catch up with the population needs, which might have detrimental effects on the health of the cared‐for person, but also on the financial sustainability of the system (Pletscher et al., 2014; Rabarison et al., 2018; Rose et al., 2015).
2. METHODS
2.1. Data
This study employed cross‐sectional data of informal caregivers of persons with SCI living in Switzerland. Data were collected through the Swiss Spinal Cohort Study (SwiSCI). (Post et al., 2011) Persons with SCI, independently of their participation in SwiSCI, who were not living in a residential home, received a letter asking them to forward the attached questionnaire to their primary family caregiver (n = 4,502). Otherwise, they were asked to send a reply letter indicating they did not have a family caregiver (n = 1,259). The survey targeted family caregiver aged 18 years and older, who could answer the questionnaire in one of the three Swiss official languages: German, French, or Italian. From the total, 864 were identified as not eligible, and 717 participants return the questionnaire, a 35% response rate.
The questionnaire asked about demographic information, living situation and quality of life, working status, financial needs, health services utilisation, interpersonal relations, social life, leisure activities and caregiving situation. Participates had the option to fill the questionnaire in paper form, an online version, or, if necessary, they had the option to get support from the study team to fill in the survey during a face‐to‐face interview, or by a phone call. (Gemperli et al., 2020).
As for caregiving tasks, besides asking their weekly time commitment (in hours) to caregiving, family caregivers were also asked about the type of tasks and time commitment for each task. More specifically, family caregivers were asked:
In which of the following activities you support the person with SCI in a weekly basis. Indicate the number of hours per week you spend on each activity
‐ Indicate “not applicable” in case you do not support the person in that specific activity.
In total, family caregivers indicated their commitment in 22 caregiving tasks, where the last one was labelled as ‘other’. In an initial data cleaning, many of the reports in the ‘other’ were recategorised and included in one of the other 21 activities. This resulted in few reports in the ‘other’ category. When a caregiver reported as ‘not applicable’, meaning they did not perform the task, the caregiving hours were coded as 0. Finally, to account for overreporting, we searched for outliers, that is total reported hours of care above 168 hr per week (24 hr/7 days), where we only had three participants reporting above 200 hr. These observations were eliminated from the estimation.
2.2. Statistical analysis
2.2.1. Proxy‐good method
The proxy‐good method uses a substitute to estimate the market value of the work undertaken by family caregivers. In the case of Switzerland, the closest substitute is professional home care, also known as Spitex (Spital = hospital + external). The services provided by Spitex are defined in the Swiss Ordinance on the Provision of Care, which also fixes and regulates the services' prices and include:
| 1. Evaluation, advice and coordination of care | CHF 79.80 per hour |
| 2. Tests & treatment | CHF 65.40 per hour |
| 3. Basic care | CHF 54.60 per hour |
| 4. Household & support | CHF 38.00 per hour |
The indicated prices are standard in the country for the first three categories. For household & support services, the prices vary by canton and provider. For this category, we simplified our estimates by using the price (CHF 38 per hour) reported by one public professional care provider in the Canton of Zurich. This price was found to vary close around the mean amongst the several consulted providers (Debrunner Zora, 2015; Hauswirtschaftliche Spitex‐Leistungen, 2018).
To monetise the work undertaken by family caregivers, we classified the 22 reported caregiving tasks in the questionnaire into the four categories defined in the Ordinance. Once classified, it was possible to estimate the economic value (EV) of family caregivers in a year:
where the EV stands for the economic value of family caregiver that equal to the price for the task times the hours per week caregiver spent on task . To get yearly estimates, EV was multiplied by the 52 weeks.
As we used the reported caregiving hours, we adjusted the estimated values by the age of the family caregiver in order to avoid overestimating the EV. In general, older caregivers reported more time in caregiving duties not because they performed more complex tasks than younger caregivers, but because they required more time to perform a task. We adjusted the estimates using a locally weighted regression, which smoothed the estimated EV around its mean value by caregiver's age. We did not use a standard regression as it would have adjusted the estimates to the sample mean, which would not have been optimal as the caregivers age was also correlated to the cared‐for person age. We tested the sensitivity of these results across five different adjustments models (Table 4).
TABLE 4.
Sensitivity analysis: Economic value of family caregivers (values in CHF per year)
| Unadjusted model | Adjusted 1 | Adjusted 2 | Adjusted 3 | Locally weighted | |
|---|---|---|---|---|---|
| Total economic value | 63,613.04 | 63,674.45 | 63,544.95 | 63,668.89 | 62,731.46 |
| Std. Dev. | 63,893.00 | 1,605.45 | 13,079.29 | 13,192.03 | 23,946.43 |
| Male caregivers | 59,154.70 | 63,466.45 | 64,792.67 | 64,830.37 | 63,844.34 |
| Std. Dev. | 66,942.59 | 1,424.10 | 13,820.90 | 13,785.74 | 23,659.46 |
| Female caregivers | 65,422.60 | 63,755.82 | 63,063.07 | 63,221.55 | 62,368.85 |
| Std. Dev. | 62,712.36 | 1,664.01 | 12,783.94 | 12,962.29 | 24,065.77 |
| By age‐group | |||||
| 18–35 years old | 36,202.73 | 62,501.18 | 59,516.71 | 58,622.93 | 36,004.52 |
| Std. Dev. | 40,403.98 | 633.75 | 11,696.38 | 12,091.04 | 11,979.86 |
| 36–54 years old | 46,277.29 | 63,080.72 | 62,122.35 | 61,893.96 | 47,695.19 |
| Std. Dev. | 51,450.30 | 1,095.29 | 12,542.16 | 12,550.00 | 18,259.71 |
| 55–65 years old | 63,021.81 | 63,655.46 | 63,072.29 | 63,226.41 | 61,201.04 |
| Std. Dev. | 65,274.33 | 1,426.86 | 13,452.65 | 13,613.14 | 21,839.15 |
| +65 years old | 75,992.94 | 64,152.03 | 64,544.43 | 64,922.42 | 73,819.11 |
| Std. Dev. | 67,318.57 | 1,871.41 | 12,441.05 | 12,379.69 | 22,433.72 |
| By type of injury | |||||
| Paraplegia | 51,051.76 | 63,787.54 | 62,952.75 | 63,083.71 | 58,649.01 |
| Std. Dev. | 52,957.04 | 1,624.63 | 12,999.62 | 13,126.00 | 24,329.79 |
| Tetraplegia | 90,885.11 | 63,497.09 | 64,427.01 | 64,448.84 | 71,929.72 |
| Std. Dev. | 77,937.36 | 1,548.15 | 12,775.38 | 12,945.41 | 21,542.05 |
| By level of dependency | |||||
| Wheelchair dependent | 68,192.87 | 63,809.73 | 63,109.85 | 63,299.60 | 65,574.74 |
| Std. Dev. | 66,531.66 | 1,623.15 | 12,775.78 | 12,888.17 | 23,894.23 |
| Able to stand | 56,224.71 | 63,428.55 | 67,746.98 | 67,581.37 | 63,649.84 |
| Std. Dev. | 51,223.07 | 1,435.66 | 14,966.39 | 14,881.14 | 21,571.48 |
| Partially able to walk | 52,520.82 | 63,305.78 | 64,078.82 | 63,977.41 | 54,285.62 |
| Std. Dev. | 59,347.96 | 1,474.59 | 13,425.36 | 13,735.05 | 22,700.51 |
Values in Swiss Francs (CHF).
Adjusted 1: estimates adjusted by the caregiving years.
Adjusted 2: estimates adjusted by the self‐reported health status of the family caregiver.
Adjusted 3: estimates adjusted by the caregiving years and the self‐reported health status of the caregiver.
Locally weighted: estimates locally weighted by the age of the family caregivers.
Finally, to account for the complexity of care needs, the results of were disaggregated by the level of impairment: paraplegia and tetraplegia. People with paraplegia, in general, require less care and support as they have a paralysis in both legs but keep mobility in the arms. In contrast, people with tetraplegia, also known as quadriplegia, cannot move neither their legs, nor their arms.
2.2.2. Financial burden: Who pays what?
In Switzerland, close relatives keep legal obligation to care and support for family members in need of regular care (van den Berg et al., 2005; Longacre et al., 2016). In the absence of informal caregivers, however, the system has to guarantee and finance the care of the persons in need, which include (a) the insurances covering the person in need (i.e. health and accident insurance), and (b) the cared‐for person (i.e. out‐of pocket expenditure). Nevertheless, the cared‐for person can finance the financial needs by getting support from available social insurances and the Canton and/or municipality of residence to pay for the needs of care.
Health and accident insurance
Professional home care services included in items 1 to 3 (i.e. evaluation, advice and coordination of care, tests and treatment and basic care) are reimbursed by the health or accident insurance as long as the need of the services is assessed and prescribed by a physician, and the services are provided by registered staff. Tasks related to support with households chores (item 4) are never reimbursed (Ordonnance du DFI sur les prestations dans l’assurance obligatoire des soins en cas de maladie, 2019), but can be purchased in demand. The prices of the latter vary by canton of residence, service provider and, in many cases, by the household income of the cared‐for person.
Cared‐for person
For tasks 1–3, the care‐for person has a copayment of care. The copayment is capped at CHF 15.95 per day, or CHF 5,821.75 per year and can vary by the canton of residence. The Canton of Vaud, for example, does not require a copayment; other cantons limit the patient participation to CHF 8 per day (Aide et soins à domicile, 2018). To finance the remaining costs, the cared‐for person can get support from two allowances designed to cover the costs of care and/or assistance (helplessness allowance, and assistance allowance), and the Canton or municipality of residence.
Helplessness allowance
Persons in need of regular care and support from a third person are eligible to receive a helplessness allowance. The allowance is granted per month, and the amount depends on the insurance covering the case (i.e. health or accident insurances), and on the level of disability (i.e. low, middle and high level of disability). When a person is covered through health insurance, the helplessness allowance is paid out from the disability insurance, which is funded by the national social support system through taxes. Otherwise, the allowance is paid by the accident insurance:
| Health insurance | Accident insurance | |
|---|---|---|
| Low disability level | CHF 474 | CHF 692 |
| Middle disability level | CHF 1,185 | CHF 1,384 |
| High disability level | CHF 1,896 | CHF 2,076 |
The level of disability is determined by an initial assessment and depends on the number of activities of daily living that the cared‐for person needs support with. People with a low level of disability require support with at least two daily activities, people with a middle level of disability require support with most of daily activities, and people with a high level of disability require support in all daily activities.
Assistance allowance
People covered by health insurance, receive helplessness allowance, and who live on their own place are eligible for an assistance allowance. The amount of the allowance depends on how much assistance is required, and it pays CHF 39.20 per hour, but it can go up to CHF 49.80 if the support task requires some specific skills. The allowance can only be used to pay for services undertaken by persons who are not directly related to the cared‐for person, that is spouses, or cohabiting partners cannot be paid with the assistance allowance. People covered by the accident insurance are not eligible for this allowance.
Cantons and municipalities
In cases where the existing allowances do not cover the needs of care, the cantons of residence of the person in need of care, together with the municipalities, can support to pay for care services. The financial support depends on the cantons’ regulation and the financial situation of the cared‐for person. In general, the municipalities evaluate the financial situation (income + wealth) of the cared‐for person and of the close family members to decide how much support to grant. As this type of support is case‐specific, and we do not have data to estimate the share of the municipalities financing the costs, we will exclude it from the estimation.
3. RESULTS
3.1. Descriptive statistics
Family caregivers are mostly female (73%), 57 years old on average, living in households without children (87%), with a high quality of life (i.e. 78% reported to have a good/very good quality of life), and with a high health satisfaction (7.4 out of 10). A third of the sample reported to have higher education, and about half of the sample lived in households with an income above the population median. (Household Income & Expenditure, 2018) More than half of caregivers (52%) were in gainful employment; where, most of them worked in part‐time jobs. Few caregivers (7%) reported to be unemployed. On average, respondents have been caregivers for about 12 years, caring for a person with traumatic SCI, who was completely dependent (73%). Family caregivers spent 27 hr per week on caring tasks, and 46% of them received professional home care support. We only found three outliers in the sample, who reported to care for more than 200 hr per week. To avoid an overestimation, we dropped them from the estimation (Table 1).
TABLE 1.
Descriptive statistics
| %/mean | SD | |
|---|---|---|
| Female | 73.0% | |
| Age (average years) | 57.2 | 13.9 |
| Swiss nationality | 90.0% | |
| In partnership | 80.0% | |
| Household size (average number) | 1.7 | 1.1 |
| Household with children | 13.0% | |
| Satisfaction with health (average) | 7.4 | 2.1 |
| Financial satisfaction | 6.9 | 2.5 |
| Quality of life | ||
| Very good | 23.0% | |
| Good | 55.0% | |
| Not good nor bad | 20.0% | |
| Bad & very bad | 2.0% | |
| Education | ||
| No mandatory | 4.0% | |
| Mandatory school | 24.0% | |
| Secondary school | 45.0% | |
| Higher education | 28.0% | |
| Household income | ||
| 1500–3000 CHF | 7.0% | |
| 3000–4500 CHF | 15.0% | |
| 4500–6000 CHF | 21.0% | |
| 6000–7500 CHF | 19.0% | |
| 7500–9000 CHF | 15.0% | |
| >9000 CHF | 23.0% | |
| Working status | ||
| Has gainful employment | 52.0% | |
| Working pensum | 59.50% | |
| Unemployed | 7.0% | |
| Caregiving characteristics | ||
| Caregiving hours per week | 27.1 | 25.6 |
| Years as caregiver | 12.0 | 10.7 |
| Use of professional home support | 46.5% | |
| Characteristics cared‐for person | ||
| Traumatic SCI | 73.1% | |
| Completely dependent | 73.0% | |
| Paraplegic | 66.0% | |
| Has gainful employment | 32.6% | |
| N | 611 | |
Satisfaction with health and financial satisfaction goes from 0 (not satisfied) to 10 (very satisfied).
Among the caring tasks reported in the questionnaire, 13 were related to basic care, three to tests and treatment and six to household & support activities. Tasks in basic care were related to eating and drinking, personal care and mobility and transfers. Tasks in tests and treatment included respiratory care, bladder and bowel management. Tasks in household chores and support included housekeeping, company to therapy and shopping. Most caregivers (85%) reported doing housekeeping chores for 11 hr per week, on average. The least reported task was support with climbing stairs, 2 hr per week (Table 2).
TABLE 2.
Caregiving tasks by type of service
| % caregivers | Mean (hours per‐week) | SD | |
|---|---|---|---|
| Basic care | |||
| Eating and drinking | 24.2% | 8.5 | 6.9 |
| Washing face and hands | 18.8% | 3.7 | 4.6 |
| Washing upper body and head | 23.4% | 2.1 | 1.8 |
| Washing feet | 30.1% | 1.9 | 1.9 |
| Washing lower body | 26.2% | 2.5 | 2.1 |
| Dressing upper body | 29.8% | 2.4 | 2.2 |
| Dressing lower body | 37.5% | 2.5 | 2.2 |
| Transfer to bed | 29.8% | 2.8 | 5.6 |
| Transfer bathtub | 18.6% | 2.0 | 1.6 |
| Climbing stairs | 6.6% | 1.9 | 1.7 |
| Moving in the house | 10.4% | 2.7 | 2.2 |
| Transfer to the car | 32.2% | 1.8 | 1.6 |
| Moving outdoors moderate distances | 22.7% | 2.0 | 1.8 |
| Tests & treatment | |||
| Respiratory care | 8.2% | 2.9 | 3.2 |
| Bladder management | 24.3% | 3.0 | 3.3 |
| Bowel management | 23.4% | 3.3 | 2.8 |
| Household & support | |||
| Moving outdoors long distances | 34.9% | 3.0 | 4.0 |
| Company to therapy or others | 44.9% | 2.3 | 2.7 |
| Housekeeping | 85.5% | 11.6 | 11.0 |
| Shopping | 82.1% | 3.2 | 3.1 |
| Paperwork | 43.1% | 2.2 | 2.7 |
| Other assistance | 19.6% | 5.8 | 7.7 |
| N | 608 | ||
% of caregivers: percentage of caregivers who reported to perform such task in a week.
3.2. The economic value of informal caregivers
The estimated market value of the average family caregiver was CHF 62,732 per year (EUR 56,455). See Table 3.
TABLE 3.
Results: Economic value of family caregivers (values in CHF per year)
| Mean | SD | Median | Minimum | Maxium | N | |
|---|---|---|---|---|---|---|
| Total economic value | 62,731.5 | 23,946.4 | 68,094.7 | 20,116.5 | 100,105.7 | 608 |
| Male caregivers | 63,844.3 | 23,659.5 | 71,602.5 | 20,146.6 | 99,796.1 | 166 |
| Female caregivers | 62,368.9 | 24,065.8 | 67,456.2 | 20,116.5 | 100,105.7 | 441 |
| By age‐group | ||||||
| 18–35 years old | 39,603.7 | 13,727.9 | 42,005.8 | 20,116.5 | 62,564.6 | 50 |
| 36–54 years old | 52,850.0 | 21,049.0 | 57,367.6 | 24,587.6 | 83,159.3 | 191 |
| 55–65 years old | 66,856.9 | 22,050.5 | 72,925.7 | 32,337.4 | 93,876.0 | 171 |
| +65 years old | 74,661.5 | 22,164.7 | 79,051.2 | 37,215.0 | 100,105.7 | 196 |
| By type of injury | ||||||
| Paraplegia | 58,649.0 | 24,329.8 | 61,453.7 | 20,116.5 | 100,000.3 | 373 |
| Tetraplegia | 71,929.7 | 21,542.1 | 78,320.8 | 20,146.6 | 99,796.1 | 193 |
| By level of dependency | ||||||
| Wheelchair dependent | 65,574.7 | 23,894.2 | 72,230.5 | 20,116.5 | 100,000.3 | 424 |
| Able to stand | 63,649.8 | 21,571.5 | 70,354.9 | 28,228.3 | 93,705.5 | 18 |
| Partially able to walk | 54,285.6 | 22,700.5 | 47,435.8 | 20,146.6 | 99,555.6 | 140 |
values were estimated using a locally adjusted regression by the age of the family caregiver.
Exchange rate (2017): CHF 1 = EUR 0.90 = USD 1.01.
The value for male caregivers was similar to that of female caregivers (CHF 63,844 versus. CHF 62,369). In contrast, older caregivers spent significantly more hours on caring tasks than younger caregivers, which made their economic value twice as expensive (CHF 74,662 vs. CHF 39,604 for caregivers older than 65 years as compared to those 35 years of age or younger).
The characteristics of the cared‐for person marked significant differences in the estimated values. Persons with tetraplegia required care with an economic value almost two times the economic value required for persons with paraplegia (CHF 71,930 vs. CHF 58,649). As expected, persons with SCI who were able to walk, required less care than persons who were wheelchair dependent (CHF 54,286 vs. 65,575 CHF).
From the total estimated economic value, 52% was for housekeeping and support tasks, 38% for basic care and 10% for medical care. This distribution changed when the results were disaggregated by level of impairment: caregivers of person with tetraplegia spent significantly more time on basic care and medical care duties than caregivers of persons with paraplegia (Figure 1).
FIGURE 1.
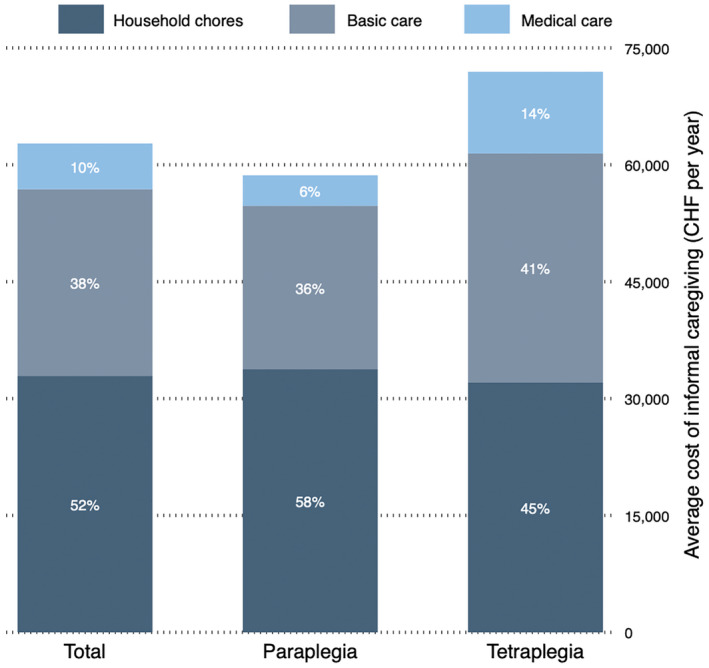
Economic value by type of caregiving task
3.2.1. Financial burden
In the absence of family caregivers, professional home care should take over the care of persons in need of regular care. On average, the financial burden of caregiving is shared between the health and accident insurances in 47%, and the cared‐for person in 53%. The share of the cared‐for person, however, can be financed by the helplessness allowance (18%) and the assistance allowance (11%). Yet, the cared‐for person has to finance almost 24% of the remaining costs with out‐of‐pocket payments.
When the financial burden is disaggregated by the hours of care, which is a proxy of the severity of the injury of the cared‐for person, the share borne by payers varies with a higher burden for the insurances (57%) in high‐severity situations (more than 100 hr of care per week) and a lower financial share burden for the cared‐for person (15%, Figure 2).
FIGURE 2.
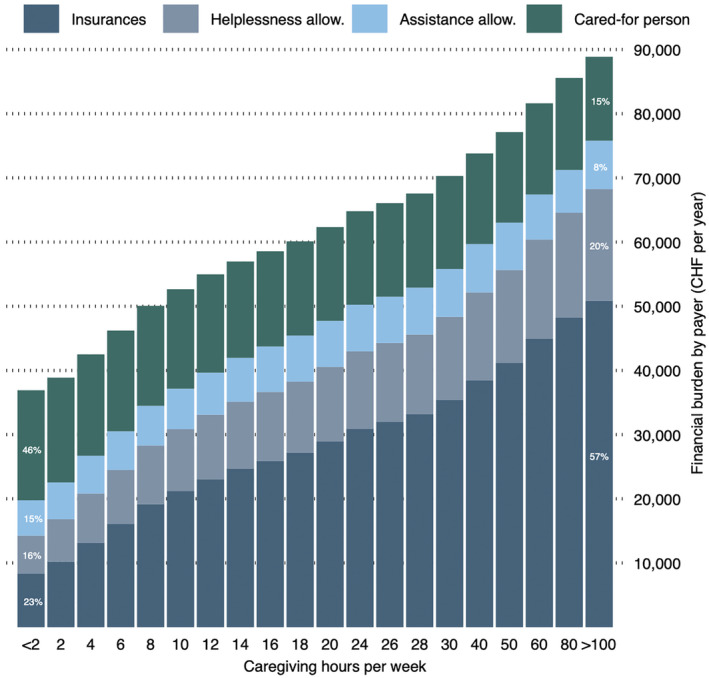
Financial burden by payer and by hours of care
4. DISCUSSION
Family caregivers of persons with SCI spent an average of 27 hr per week on a wide range of caring tasks. This work has an estimated market value of CHF 62,732 per years (EUR 56,455) if undertaken by professional home caregivers. More than half of the costs are due to housekeeping chores (52%), followed by basic care (38%), and to medical care (10%). This value, however, shows a significant variation explained by the characteristics of the caregiver and the cared‐for person. Surprisingly, there were no marked differences in the estimates by the caregivers’ sex. Even though female caregivers spent on average more time on caring tasks than male caregivers (28 vs. 25 hr/week), a big share of their time was destinated to housekeeping, task with a lower price in the market. Male caregivers, in contrast, spent relatively more time on basic care, that is personal care, or transportation, tasks that are more expensive to replace by a market substitute. Similarly, older caregivers had higher economic value than younger caregivers even after adjusting the results by the caregiver's age, which reflects that older caregivers also care for older persons with SCI.
In the case of the cared‐for person, the variation in the estimates is explained by the severity of the disability, where persons with complete tetraplegia, that is persons who do not have mobility of neither their arms nor legs, required support with most of the daily living activities. Thus, caregivers of this group not only invested more time on caring tasks, but they also performed more complex tasks. Compared to persons with paraplegia, that is persons who do not have mobility of the legs, this group designated relatively less time to household chores and more time to basic care and medical care.
Even though the Swiss health system is universal and provides professional home care services and financial support to persons in need of care, it does not have any direct support to family caregivers.
This situation pushes family caregivers to find their own ways to reconcile their life with caregiving, which requires many sacrifices (Exel et al., 2008). Depending on the financial situation of the household, family caregivers constrain their professional career, limit their family life, and reduce their leisure time to perform their role as caregiver (Bayen et al., 2017; Gibson & Houser, 2007; Nguyen & Connelly, 2014). This situation translates in overly burdened caregivers, which is not desirable for neither the caregiver's health, nor for the cared‐for person nor from a health system's perspective (Al‐Janabi et al., 2018; Peetoom et al., 2016).
Compared to other groups in need of care, a trade‐off between formal and informal care does not really take place for persons with SCI. In our sample, on average, professional home care acts more as a complement to the work undertaken by family caregivers rather than a substitute. This is explained by the characteristics of SCI that is a high‐needs group that requires long‐term frequent care that includes a series of caring tasks, many of which are complex. (Huang et al., 2020) Nevertheless, a trade‐off happens at higher income groups, where families in richer households can afford services that are not reimbursed by the insurances, like housekeeping, which free time that could be spent on other activities.
In the absence of family caregivers, the health system together with the social system and the persons in need of care have to finance long‐term care and assistance services. How much of the costs of care is borne by the insurances, the cash allowances and out‐of pocket expenditure depends on the severity of the case. Therefore, from a societal perspective, replacing family caregivers might not be optimal neither for the persons in need of care, nor financial sustainable for taxpayers (Plichta, 2018), except in those cases where the health and labour market effects outweighs the cost of caregiving. In our sample, however, more than 50% of family caregivers reported to also have a paid activity (13.5% work full time, and 35% work part‐time), and close to 40% of the sample reported to be retired. Only 7% reported to be actively searching for a job. (Gemperli et al., 2020).
One way to support this group would be to recognise their work through compensation measures like direct payments (cash grants), provisions of respite services, or relief with domestic chores putting more attention on caregivers dealing with more severe cases (Donelan et al., 2002; Household Income & Expenditure, 2018; Tamiya et al., 2011). These kind of measures are not only cheaper for the system by keeping family caregivers, but they are also in the best interest of the cared‐for person.
4.1. Limitations
One limitation of this study is about the time caregivers reported for every caring task. Even though the questionnaire asked caregivers to report the time they spent on caring tasks, it was difficult to declare precise hours with minutes. In fact, the questionnaire listed tasks that could be performed simultaneously, so splitting the time was not always optimal. In addition, in the day‐to‐day activities, there were tasks that caregivers performed for themselves, such as cleaning or cooking. Therefore, there could exist some overlap in the reported time spend on caregiving tasks (van den Berg et al., 2006). Also, depending on the relationship to the person with SCI, what is reported as a caregiving task might differ. For caregivers that are also the partner of the person with SCI, cooking and cleaning might be underreported; however, for a caregiver that is a daughter or a friend, this task is more likely to be counted as an additional duty. Similar situation for caregivers living in different households’ compositions. For caregivers that also take care of young children, differentiating caring time for children and caring time for the person with SCI might not be simple. Nevertheless, how to address this issue is not yet clear in the literature. A possibility is to compare the reported hours of care of the caregiver with the reported hours of need of care by the person with SCI, and check the reasons for discrepancies (Urwin et al., 2021).
Also, the results show that even when the Swiss health system, together with the social system have several means of support, the financial burden for the cared‐for person is significant, especially for severe cases. Nevertheless, depending on the place of residence, and the financial situation of the household, the cared‐for person might get additional support from the local authorities. As this kind of support is case specific, there are no data that allow us to quantify how much the municipalities support persons in need. Therefore, our estimates on the financial burden might be inflated.
Finally, the proxy‐good method estimates the economic value of family caregivers by assuming there is a ‘perfect’ market substitute of their work. Nevertheless, this method disregards other monetary and non‐monetary costs/benefits of family caregiving, like the income loss caregivers incur when caring for a relative, the increasing healthcare costs due to a reduced health status, and other effects of caregiving related to the family dynamics (Bauer & Sousa‐Poza, 2015). Even when professional home care is of good quality, assuming they can fully replace family caregivers is unrealistic (van den Berg et al., 2005). Therefore, the estimates presented in this study should be taken as an underestimation of the total economic value of family caregivers.
5. CONCLUSIONS
This study estimated what it would cost to the Swiss health and social system to substitute the work undertaken by long‐term family caregivers. We analysed the case of family caregivers of persons with SCI, which is an irreversible health condition that combines physical impairment with a series of chronic illness. We found that replacing the work performed by family caregivers is extremely expensive. Thus, it is in the best interest of the society to keep a sustained supply of family caregivers by making their work less cumbersome. Aside from a proper recognition of their work, it would be important to establish instruments to compensate family caregivers for their work to assure their lasting involvement when desirable.
CONFLICT OF INTERESTS
The authors declare to have no conflicts of interest.
AUTHORS CONTRIBUTION
Diana Pacheco Barzallo: Conceptualisation, methodology, formal analysis, writing original draft, writing ‐review & editing, visualisation. Rina Hernandez: Data management, formal analysis, writing original draft. Mirjam Brach: Data management, writing original draft, project administration. Armin Gemperli: Conceptualisation, writing original draft, supervision, validation, project administration.
ACKNOWLEDGEMENT
Open Access Funding provided by Universitat Luzern.
Pacheco Barzallo, D. , Hernandez, R. , Brach, M. , & Gemperli, A. (2022). The economic value of long‐term family caregiving. The situation of caregivers of persons with spinal cord injury in Switzerland. Health & Social Care in the Community, 30, e2297–e2307. 10.1111/hsc.13668
Funding information
This research was funded by Swiss National Science Foundation grant 160158 and Swiss Paraplegic Research.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author.
REFERENCES
- Aide et soins à domicile . (2018). Participation du patient en 2018. Spitex.Ch. https://www.spitex.ch/files/942CAR1/Financement‐des‐soins‐Liste‐participation‐patients‐2018.pdf [Google Scholar]
- Al‐Janabi, H. , Carmichael, F. , & Oyebode, J. (2018). Informal care: Choice or constraint? Scandinavian Journal of Caring Sciences, 32(1), 157–167. 10.1111/scs.12441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arno, P. S. , Levine, C. , & Memmott, M. M. (1999). The economic value of informal caregiving. Health Affairs, 18(2), 182–188. 10.1377/hlthaff.18.2.182 [DOI] [PubMed] [Google Scholar]
- Bauer, J. M. , & Sousa‐Poza, A. (2015). Impacts of informal caregiving on caregiver employment, health, and family. Journal of Population Ageing, 8(3), 113–145. 10.1007/s12062-015-9116-0 [DOI] [Google Scholar]
- Bayen, E. , Laigle‐Donadey, F. , Prouté, M. , Hoang‐Xuan, K. , Joël, M.‐E. , & Delattre, J.‐Y. (2017). The multidimensional burden of informal caregivers in primary malignant brain tumor. Supportive Care in Cancer, 25(1), 245–253. 10.1007/s00520-016-3397-6 [DOI] [PubMed] [Google Scholar]
- Brinkhof, M. W. G. , Al‐Khodairy, A. , Eriks‐Hoogland, I. , Fekete, C. , Hinrichs, T. , Hund‐Georgiadis, M. , Meier, S. , Scheel‐Sailer, A. , Schubert, M. , & Reinhardt, J. D. & SwiSCI Study Group . (2016). Health conditions in people with spinal cord injury: Contemporary evidence from a population‐based community survey in Switzerland. Journal of Rehabilitation Medicine, 48(2), 197–209. 10.2340/16501977-2039 [DOI] [PubMed] [Google Scholar]
- Broese van Groenou, M. I. , & De Boer, A. (2016). Providing informal care in a changing society. European Journal of Ageing, 13(3), 271–279. 10.1007/s10433-016-0370-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Meijer, C. , Brouwer, W. , Koopmanschap, M. , van den Berg, B. , & van Exel, J. (2010). The value of informal care–a further investigation of the feasibility of contingent valuation in informal caregivers. Health Economics, 19(7), 755–771. 10.1002/hec.1513 [DOI] [PubMed] [Google Scholar]
- Debrunner Zora . (2015). Senso—Das Gesundheitsmagazin von Helsana. https://epaper.helsana.ch/senso/2015‐02/de/files/assets/basic‐html/page‐11.html
- Donelan, K. , Hill, C. A. , Hoffman, C. , Scoles, K. , Feldman, P. H. , Levine, C. , & Gould, D. (2002). Challenged to care: Informal caregivers in a changing health system. Health Affairs, 21(4), 222–231. 10.1377/hlthaff.21.4.222 [DOI] [PubMed] [Google Scholar]
- Gemperli, A. , Ronca, E. , Scheel‐Sailer, A. , Koch, H. G. , Brach, M. , & Trezzini, B. (2017). Health care utilization in persons with spinal cord injury: Part 1—outpatient services. Spinal Cord, 55(9), 823–827. 10.1038/sc.2017.44 [DOI] [PubMed] [Google Scholar]
- Gemperli, A. , Rubinelli, S. , Zanini, C. , Huang, J. , Brach, M. , & Pacheco Barzallo, D. (2020). Living situation of family caregivers of persons with spinal cord injury. Journal of Rehabilitation Medicine, 52(11), jrm00124. 10.2340/16501977-2762 [DOI] [PubMed] [Google Scholar]
- Gibson, M. J. , & Houser, A. (2007). Valuing the invaluable: A new look at the economic value of family caregiving. Issue Brief (Public Policy Institute (American Association of Retired Persons)), IB82, 1–12. [PubMed] [Google Scholar]
- Hauswirtschaftliche Spitex‐Leistungen. (2018). http://www.spitex‐zuerich.ch/tarife‐2014/hauswirtschaftliche‐leistungen/ [Google Scholar]
- Hirst, M. (2001). Trends in informal care in Great Britain during the 1990s. Health & Social Care in the Community, 9(6), 348–357. 10.1046/j.0966-0410.2001.00313.x [DOI] [PubMed] [Google Scholar]
- Household income and Expenditure . (2018). Federal statistical office. https://www.bfs.admin.ch/bfs/en/home/statistics/economic‐social‐situation‐population/income‐consumption‐wealth/household‐budget.html [Google Scholar]
- Huang, J. , Pacheco Barzallo, D. , Rubinelli, S. , Münzel, N. , Brach, M. , & Gemperli, A. (2019). What influences the use of professional home care for individuals with spinal cord injury? A cross‐sectional study on family caregivers. Spinal Cord, 57(11), 924–932. 10.1038/s41393-019-0296-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, J. , Pacheco Barzallo, D. , Rubinelli, S. , Münzel, N. , Brach, M. , & Gemperli, A. (2020). Professional home care and the objective care burden for family caregivers of persons with spinal cord injury: Cross sectional survey. International Journal of Nursing Studies Advances, 3, 100014. 10.1016/j.ijnsa.2020.100014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen, R. (2012). Do labor market opportunities affect young women's work and family decisions? Experimental evidence from India. The Quarterly Journal of Economics, 127(2), 753–792. 10.1093/qje/qjs002 [DOI] [Google Scholar]
- Kang, Y. , Ding, H. , Zhou, H. , Wei, Z. , Liu, L. , Pan, D. , & Feng, S. (2017, December 29). Epidemiology of worldwide spinal cord injury: A literature review. Journal of Neurorestoratology. 10.2147/JN.S143236 [DOI] [Google Scholar]
- Kraft, E. , Marti, M. , Werner, S. , & Sommer, H. (2010). Cost of dementia in Switzerland. Swiss Medical Weekly, 140(3536), 10.4414/smw.2010.13093 [DOI] [PubMed] [Google Scholar]
- Li, C. , Zeliadt, S. B. , Hall, I. J. , Smith, J. L. , Ekwueme, D. U. , Moinpour, C. M. , Penson, D. F. , Thompson, I. M. , Keane, T. E. , & Ramsey, S. D. (2013). Burden among partner caregivers of patients diagnosed with localized prostate cancer within 1 year after diagnosis: An economic perspective. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 21(12), 3461–3469. 10.1007/s00520-013-1931-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longacre, M. L. , Valdmanis, V. G. , Handorf, E. A. , & Fang, C. Y. (2016). Work impact and emotional stress among informal caregivers for older adults. The Journals of Gerontology: Series B, 72(3), 522–531. 10.1093/geronb/gbw027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, H. T. , & Connelly, L. B. (2014). The effect of unpaid caregiving intensity on labour force participation: Results from a multinomial endogenous treatment model. Social Science & Medicine, 100, 115–122. 10.1016/j.socscimed.2013.10.031 [DOI] [PubMed] [Google Scholar]
- Nowossadeck, S. (2013). Demographic change, people needing long‐term care, and the future need for carers. An overview. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 56(8), 1040–1047. 10.1007/s00103-013-1742-1 [DOI] [PubMed] [Google Scholar]
- Oliva‐Moreno, J. , Trapero‐Bertran, M. , Peña‐Longobardo, L. M. , & Del Pozo‐Rubio, R. (2017). The valuation of informal care in cost‐of‐illness studies: A systematic review. Pharmacoeconomics, 35(3), 331–345. 10.1007/s40273-016-0468-y [DOI] [PubMed] [Google Scholar]
- Ordonnance Du DFI Sur Les Prestations Dans L’assurance Obligatoire Des Soins En Cas De Maladie, 832.112.31. (2019). https://fedlex.data.admin.ch/filestore/fedlex.data.admin.ch/eli/cc/1995/4964_4964_4964/20190101/fr/pdf‐a/fedlex‐data‐admin‐ch‐eli‐cc‐1995‐4964_4964_4964‐20190101‐fr‐pdf‐a.pdf [Google Scholar]
- Ortiz‐Ospina, E. , & Sandra, T. (2017). Working women: Key facts and trends in female labor force participation. Our World in Data. https://ourworldindata.org/female‐labor‐force‐participation‐key‐facts [Google Scholar]
- Paraponaris, A. , Davin, B. , & Verger, P. (2012). Formal and informal care for disabled elderly living in the community: An appraisal of French care composition and costs. The European Journal of Health Economics, 13(3), 327–336. 10.1007/s10198-011-0305-3 [DOI] [PubMed] [Google Scholar]
- Peetoom, K. K. B. , Lexis, M. A. S. , Joore, M. , Dirksen, C. D. , & De Witte, L. P. (2016). The perceived burden of informal caregivers of independently living elderly and their ideas about possible solutions. A mixed methods approach. Technology and Disability, 28(1,2), 19–29. 10.3233/TAD-160441 [DOI] [Google Scholar]
- Pletscher, M. , Mattli, R. , Reich, O. , Von Wyl, A. , & Wieser, S. (2014). The societal costs of schizophrenia in Switzerland. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 17(7), A457. 10.1016/j.jval.2014.08.1253 [DOI] [PubMed] [Google Scholar]
- Plichta, S. B. (2018). Paying the hidden bill: How public health can support older adults and informal caregivers. American Journal of Public Health, 108(10), 1282–1284. 10.2105/AJPH.2018.304670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post, M. W. M. , Brinkhof, M. W. G. , von Elm, E. , Boldt, C. , Brach, M. , Fekete, C. , Eriks‐Hoogland, I. , Curt, A. , Stucki, G. , & SwiSCI Study Group . (2011). Design of the swiss spinal cord injury cohort study. American Journal of Physical Medicine & Rehabilitation, 90(11 Suppl 2), S5–S16. 10.1097/PHM.0b013e318230fd41 [DOI] [PubMed] [Google Scholar]
- Rabarison, K. M. , Bouldin, E. D. , Bish, C. L. , McGuire, L. C. , Taylor, C. A. , & Greenlund, K. J. (2018). The economic value of informal caregiving for persons with dementia: Results from 38 States, the District of Columbia, and Puerto Rico, 2015 and 2016 BRFSS. American Journal of Public Health, 108, 1370–1377. 10.2105/AJPH.2018.304573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose, M. S. , Noelker, L. S. , & Kagan, J. (2015). Improving policies for caregiver respite services. The Gerontologist, 55(2), 302–308. 10.1093/geront/gnu120 [DOI] [PubMed] [Google Scholar]
- Roser, M. (2014). Fertility rate. Our World in Data, https://ourworldindata.org/fertility‐rate [Google Scholar]
- Smith, E. M. , Boucher, N. , & Miller, W. C. (2016). Caregiving services in spinal cord injury: A systematic review of the literature. Spinal Cord, 54(8), 562–569. 10.1038/sc.2016.8 [DOI] [PubMed] [Google Scholar]
- Snell, K. D. M. (2017). The rise of living alone and loneliness in history. Social History, 42(1), 2–28. 10.1080/03071022.2017.1256093 [DOI] [Google Scholar]
- Tamiya, N. , Noguchi, H. , Nishi, A. , Reich, M. R. , Ikegami, N. , Hashimoto, H. , Shibuya, K. , Kawachi, I. , & Campbell, J. C. (2011). Population ageing and wellbeing: Lessons from Japan’s long‐term care insurance policy. The Lancet, 378(9797), 1183–1192. 10.1016/S0140-6736(11)61176-8 [DOI] [PubMed] [Google Scholar]
- Urwin, S. , Lau, Y.‐S. , Grande, G. , & Sutton, M. (2021). The challenges of measuring informal care time: A review of the literature. Pharmacoeconomics, 39(11), 1209–1223. 10.1007/s40273-021-01053-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg, B. , Bleichrodt, H. , & Eeckhoudt, L. (2005). The economic value of informal care: A study of informal caregivers’ and patients’ willingness to pay and willingness to accept for informal care. Health Economics, 14(4), 363–376. 10.1002/hec.980 [DOI] [PubMed] [Google Scholar]
- van den Berg, B. , Brouwer, W. , van Exel, J. , Koopmanschap, M. , van den Bos, G. A. M. , & Rutten, F. (2006). Economic valuation of informal care: Lessons from the application of the opportunity costs and proxy good methods. Social Science & Medicine, 62(4), 835–845. 10.1016/j.socscimed.2005.06.046 [DOI] [PubMed] [Google Scholar]
- van Exel, J. , Bobinac, A. , Koopmanschap, M. , & Brouwer, W. (2008). The invisible hands made visible: Recognizing the value of informal care in healthcare decision‐making. Expert Review of Pharmacoeconomics & Outcomes Research, 8(6), 557–561. 10.1586/14737167.8.6.557 [DOI] [PubMed] [Google Scholar]
- Yoon, J. , Chee, C. P. , Su, P. , Almenoff, P. , Zulman, D. M. , & Wagner, T. H. (2018). Persistence of high health care costs among VA patients. Health Services Research, 53(5), 3898–3916. 10.1111/1475-6773.12989 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author.


