Abstract
Autism spectrum disorder (ASD) is characterized by significant social functioning impairments, including (but not limited to) emotion recognition, mentalizing, and joint attention. Despite extensive investigation into the correlates of social functioning in ASD, only recently has there been focus on the role of low‐level sensory input, particularly visual processing. Extensive gaze deficits have been described in ASD, from basic saccadic function through to social attention and the processing of complex biological motion. Given that social functioning often relies on accurately processing visual information, inefficient visual processing may contribute to the emergence and sustainment of social functioning difficulties in ASD. To explore the association between measures of gaze and social functioning in ASD, a systematic review and meta‐analysis was conducted. A total of 95 studies were identified from a search of CINAHL Plus, Embase, OVID Medline, and psycINFO databases in July 2021. Findings support associations between increased gaze to the face/head and eye regions with improved social functioning and reduced autism symptom severity. However, gaze allocation to the mouth appears dependent on social and emotional content of scenes and the cognitive profile of participants. This review supports the investigation of gaze variables as potential biomarkers of ASD, although future longitudinal studies are required to investigate the developmental progression of this relationship and to explore the influence of heterogeneity in ASD clinical characteristics.
Lay Summary
This review explored how eye gaze (e.g., where a person looks when watching a movie) is associated with social functioning in autism spectrum disorder (ASD). We found evidence that better social functioning in ASD was associated with increased eye gaze toward faces/head and eye regions. Individual characteristics (e.g., intelligence) and the complexity of the social scene also influenced eye gaze. Future research including large longitudinal studies and studies investigating the influence of differing presentations of ASD are recommended.
Keywords: attention, autism spectrum disorder, cognition, eye gaze, motivation, social functioning, visual processing
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that involves lifelong difficulties, spanning cognitive, behavioral, and emotional domains. Social cognitive and social communicative difficulties are core features of ASD, and broadly encompass the skills required to engage with the social world (Pallathra et al., 2018; Pallathra et al., 2019). Social difficulties have been extensively mapped across the autism spectrum, resulting in a set of common, albeit not universal, impairments in the following areas: the ability to infer the mental states and intentions of others (i.e., theory of mind [ToM]; Leppanen et al., 2018), the direction of attention to shared social experiences (i.e., joint attention; Franchini et al., 2019; Mundy, 2018), face and emotion recognition (Tang et al., 2015; Uljarevic & Hamilton, 2013), empathy (Song et al., 2019), language (Eigsti et al., 2011), and the “global” processing of visual stimuli (Van der Hallen et al., 2015). Collectively, these features can result in difficulties engaging in one's social environment.
These social functioning difficulties cannot be ascribed to an isolated deficit in a specific neural region. Rather, such widespread difficulties are often characteristic of disruptions within the “social brain”, referring to a network of interconnected neural structures involved in social information processing. Relevant nodes include the medial prefrontal cortex (mentalizing ability; Schurz et al., 2014), temporoparietal junction (prosocial decision‐making; Zanon et al., 2014), posterior superior temporal sulcus (biological motion processing; Deen et al., 2015; Pelphrey & Carter, 2008), and fusiform gyrus (face processing; Furl et al., 2011).
Despite extensive examination of social brain regions and their associated behavioral, cognitive, and emotional disturbances in ASD, these studies often fail to examine the sensory inputs required to initially examine and process social information. Of particular interest is visual information processing, given that adequate processing of social information requires that relevant environmental social stimuli are attended to, perceived, and processed in an accurate manner (Griffin & Scherf, 2020). The disruption of visual processing early in development may lead to differences in how socio‐communicative interactions are perceived and acted upon, resulting in potentially inaccurate perceptions and interactions with the social environment (Hellendoorn et al., 2013; Thye et al., 2018).
Dysfunction across multiple levels of the visual processing pathway has been reported in ASD, from basic saccadic eye movements (Mosconi et al., 2013; Schmitt et al., 2014; Stanley‐Cary et al., 2011) to biological motion processing (part of the aforementioned “social brain” network; Annaz et al., 2010; Klin et al., 2009). Additionally, differences in the way in which social gaze is allocated has been demonstrated in ASD. For example, two meta‐analyses conducted by Chita‐Tegmark found that participants with ASD look less at the eyes, mouth, face, and the entire screen on which stimuli are presented, and more time toward the body and nonsocial regions (Chita‐Tegmark, 2016a), and that greater group differences in attending to social stimuli between ASD and neurotypical groups is seen with social stimuli containing more than one person (Chita‐Tegmark, 2016b). However, Frazier et al. (2017) conducted a more comprehensive meta‐analysis, exploring the contributions of stimulus and methodological factors (including participant characteristics, eyetracking parameters, and stimulus features) on the gaze difficulties experienced in ASD. Although results were consistent with previous findings in that those with ASD had reductions in gaze toward eye and mouth regions and greater gaze allocation toward nonsocial regions, meta‐regression analyses revealed the influence of stimulus and methodological factors (e.g., points of calibration, number of stimuli presented). The analysis further revealed ASD‐specific gaze differences in comparison to other developmental delay conditions, indicating the potential clinical utility of assessing gaze toward social and nonsocial stimuli to aid differential diagnosis. Overall, ASD is associated with a pattern of visual exploration in which attending to aspects of the social environment critical to social understanding is affected. This is likely also underpinned, at least in part, by disrupted saccadic functioning given the role it plays in driving the allocation of gaze toward environmental regions of interest (Ibbotson & Krekelberg, 2011; Wollenberg et al., 2020).
The above findings suggest that it is crucial to consider gaze and visual attention when attempting to understand social difficulties in ASD. To date, empirical studies and meta‐analyses have focused on profiling the gaze differences toward social and nonsocial stimuli between ASD and neurotypical controls. These differences, however, may not necessarily translate into difficulties with social functioning. For example, although increased gaze toward the mouth has been associated with declines in social functioning in ASD (e.g., Hanley et al., 2015), Klin et al. (2002) found that gaze toward the mouth was instead associated with improvements in social functioning in ASD. This was considered to be a possible compensatory strategy whereby focusing on the mouth facilitated a literal understanding of speech, and in turn, social situations. Examining how the allocation of gaze across social and nonsocial scenes is associated with social functioning would provide a novel understanding of how gaze is used by individuals with ASD to engage in their social world.
Therefore, the primary purpose of this systematic review was to clarify the nature of social dysfunction in ASD by examining the relationships between gaze allocation and measures of social functioning in ASD, and to identify the factors that contribute to variation in this relationship. This is important to consider as the development of targeted interventions training the allocation of gaze in the social environment may need to be tailored to specific ASD profiles.
METHOD
Search strategy
Selected databases (CINAHL Plus, Embase, OVID Medline, and psycINFO) were searched for articles in July 2021 using the following search terms: [(autis* OR ASD OR Asperger*) AND (eyetracking OR eye‐tracking OR eye tracking OR gaze OR sacc*) AND (social* OR theory of mind OR ToM OR mentali* OR empath* OR imitati* OR face recog* OR emotion recog*)], where “*” represented truncations.
Study selection and eligibility
In order to be eligible, articles needed to (a) contain an ASD group with or without a comparison control group, (b) use either standardized clinical measures or clinical assessment for the ASD diagnosis, (c) examine the link between gaze and social function, (d) include at least one eyetracking measure or coded measure of gaze and one objective/validated measure of social functioning, (e) contain peer reviewed, empirical data, (f) include a sample size of at least 10 in each group, and (g) be written in English. No limits were placed on the age or gender of the participants. Additionally, results were included that also incorporated other participant groups within analyses (e.g., neurotypical). Cross‐sectional and longitudinal designs were included, in addition to studies that included a baseline measure of the relationship between gaze and social functioning in the context of intervention research.
Studies were initially screened by JR for inclusion based on review of titles and abstracts. Selected studies then proceeded to full‐text review for final inclusion. Reference lists were further reviewed for the inclusion of additional studies. Any uncertainties were resolved via consultation with CG and PE.
Quantitative analysis
To provide a quantitative estimate of the correlation between gaze and social functioning/autism symptom severity, separate meta‐analyses were performed for three core gaze regions (i.e., face, eyes, and mouth). Subgroup analyses and, for eligible regions, meta regressions were performed to identify potential modifiers of the overall combined correlation effect estimate. All analyses were performed in R 4.1.0 (R Core Team, 2017) using rma.mv and metafor functionalities.
Study inclusion/exclusion criteria
A combination approach was employed for all meta‐analyses to (1) minimize and (2) accommodate heterogeneity among studies (e.g., different measures of broad social functioning/autism symptom severity, subgroup versus global measurement of ASD, operationalizations of gaze measure, type of reported summary effect estimate, task conditions, such as emotional images vs. non‐emotional images) and dependence of effect estimates within studies (e.g., one study contributing > 1 estimate to the meta‐analysis).
To minimize heterogeneity, inclusion/exclusion criteria were further applied to studies included in the systematic review. In terms of exclusion for gaze measure, studies were retained that examined fixation duration/looking time (both percentages and absolute values), given that this remains the most commonly reported gaze index consistent with Chita‐Tegmark (2016a). Additionally, studies were limited to those that reported a global autism symptom severity score (e.g., Autism Diagnostic Observation Schedule [ADOS] Global score, Social Responsiveness Scale [SRS] Total score). In the case that a study reported a global estimate and subgroup estimate(s), only the global estimate was used in the meta‐analysis. As there were no studies that included global measures of social functioning (i.e., not including restricted/repetitive behavior as part of the total score), analysis was limited to measures of global autism symptom severity. To minimize dependence among effect estimates, for studies that reported > 1 effect estimate of the association between gaze and autism symptom severity due to the use of > 1 different global measure of autism symptom severity (but the same fixation duration/looking time gaze index), only one estimate was retained. Notably, each of the applicable studies included the ADOS Global score, and therefore, given its status as a gold standard approach in the assessment and diagnosis of ASD (Harstad et al., 2015; Kamp‐Becker et al., 2018), this was selected for the meta‐analysis. With respect to inclusion/exclusion criteria associated with the type of effect estimate, statistics listed in Supplementary Materials 1 in Data S1 were retained, with the understanding that some summary statistic types would require conversion into a correlational form (i.e., point biserial correlation or Pearson r) prior to meta‐analysis. Additionally, studies were retained if they examined the relationship between gaze and global measures of autism symptom severity in an ASD only group, in line with the overarching study goal of exploring this association within an ASD population. Remaining inclusion/exclusion criteria and further detail can be seen in Supplementary Materials 1 in Data S1.
The application of inclusion/exclusion criteria meant that studies only contributed more than one effect estimate of interest as a result of differing task conditions (e.g., White et al., 2015 examined the association separately for happy, disgust, and angry faces). After study level inclusion/exclusion criteria were applied, regions were deemed eligible for meta‐analysis if they had at least 10 estimates (not studies) available. This resulted in three eligible regions: face, eyes, and mouth.
Meta‐analysis: Data preparation and model specification
Prior to performing the meta‐analysis, correlations reported in studies (i.e., partial, Spearman, Pearson, bivariate standardized beta coefficient) were directly converted to Fisher z scores and corresponding sampling variances (escalc function in R). Cohen's d associated with between subjects t tests were converted to point biserial correlation prior to conversion to Fisher z (sampling variance uniquely computed in such case). When studies failed to report group size, equal size was assumed. A square root transformation for partial R 2 or R 2 reported in studies was applied to obtain Pearson r before conversion to Fisher z.
To accommodate dependence of study effect estimates, a multivariate/multilevel, random effects meta‐analysis was performed for each region, with a random effect for each level of the study variable (i.e., for each study). Models were fit using restricted maximum likelihood. A single study reporting R 2 failed to report indication of r directionality (Murias et al., 2018) across the three regions. In lieu of excluding the study, meta‐analyses were conducted for both a positive and negative direction for this study's Pearson r value for each region. Additionally for the face region, given the lack of indication of whether samples used in the two Riby and Hancock studies were the same, our analyses assumed, and thus modeled them, as different samples (Riby & Hancock, 2009a; Riby & Hancock, 2009b). The final combined Fisher z correlation effect estimate and confidence interval produced for each meta‐analysis was then converted to a Pearson correlation coefficient estimate using the following formula:
Cochran's Q test based on the chi‐square distribution was used to evaluate the presence of heterogeneity. Funnel plots provide a means of assessing the presence of publication bias by modeling effect size estimates relative to precision of the estimate. The present study did not employ this method of evaluation given plots do not take into account dependence among multiple effects from the same study and thus papers that provide multiple effects would unduly impact symmetry, negating the value of interpreting symmetry.
Meta‐regression: Participant and task characteristics
If significant heterogeneity was detected for a region in the meta‐analysis model (Cochran's Q test p < 0.05), bivariate meta‐regressions were performed for that region to identify study characteristics that explain heterogeneity in the overall effect size estimate. A total of 10 continuous (*) and categorical (**) explanatory variables (autism symptom severity measure rater**, % females in the sample*, emotional vs. non‐emotional task condition**, number of people in the scene**, points of calibration**, whether the task was static or dynamic**, eyetracker sampling rate**, unique regions of interest in stimuli**, total number of trials**, and age* [in years]) were meta‐regressed for eligible regions, provided that there were 10 or more non‐missing values in the region‐specific predictor (Cochrane Training, n.d.). These counts can be found in Supplementary Table 1 in Data S1. Definitions and region‐level summary statistics for predictors can be found in Supplementary Materials 2 and Supplementary Table 1 in Data S1, respectively. Multiple predictors could not be investigated simultaneously in a model (i.e., multiple meta‐regression) due to an inadequate number of estimates per region (Cochrane Training, n.d.). For bivariate meta‐regression models, a single explanatory variable was added to the basic intercept model with no fixed effect predictors used to perform the meta‐analysis. Only statistics linked to significant predictors are reported (p < 0.05) in main body results.
Sensitivity and subgroup analyses
A risk of bias assessment was conducted using the Newcastle‐Ottawa Scale, adapted for cross‐sectional studies (Modesti et al., 2016). A detailed overview of the risk of bias assessment tailored for the current analysis is in Supplementary Table 2 in Data S1, and an estimate‐level summary of risk of bias levels per region of interest (ROI) is included in Supplementary Table 1 in Data S1. Effect statistics from studies evaluated as possessing different levels of risk of bias were all included in the calculation of the combined effect estimate for each region. Additionally, combined estimates were derived based on a range of different correlation types, in place of restricting to Pearson correlation coefficient. These decisions were made in the interest of maximizing sample size of the meta‐analysis. Analysis results may be impacted by the assumption of comparability among correlation type. Partial correlations which control for covariate(s) are often attenuated relative to Pearson correlations and Spearman correlations are considered a good approximation of Pearson under specific conditions (e.g., large sample size; de Winter et al., 2016). In turn, sensitivity analyses were performed to investigate how conclusions may be impacted when only considering Pearson correlation coefficients. Subgroup analyses were performed to compare the overall effect estimate derived from studies with unsatisfactory levels of bias to studies with satisfactory levels of bias.
RESULTS
From a total of 2991 articles initially identified, 95 met inclusion criteria and were included (refer to Figure 1 for PRISMA flowchart; Page et al., 2021). To achieve our aim of understanding how gaze allocation is related to social functioning in ASD, results were initially grouped and examined by gaze measure. Gaze measures were coded by the type of eyetracking paradigm employed: free viewing (where participants were not instructed to allocate gaze toward predetermined regions of interest), visual search (where participants were instructed to locate a predetermined target of interest), and saccadic paradigms (where participants were required to shift their gaze in response to visual stimuli). An overview of gaze measures used across studies can be seen in Table 1. For free viewing measures, results were further classified by the ROI in which gaze was allocated (see Table 2), including single ROIs (face, eyes, mouth, nose, hand, head, body, people, object, background, overall stimulus) and multiple ROIs (dual social/nonsocial stimuli, face vs. non‐face, eyes vs. mouth). Studies were further defined by the type of visual stimulus used to assess visual processing function (i.e., dynamic vs. static, social vs. nonsocial). Dynamic stimuli involved a moving sequence of events, while static stimuli involved still images. Social stimuli reflected the presence of at least one human, while nonsocial stimuli involved the presence of nonhuman related activities and images.
FIGURE 1.
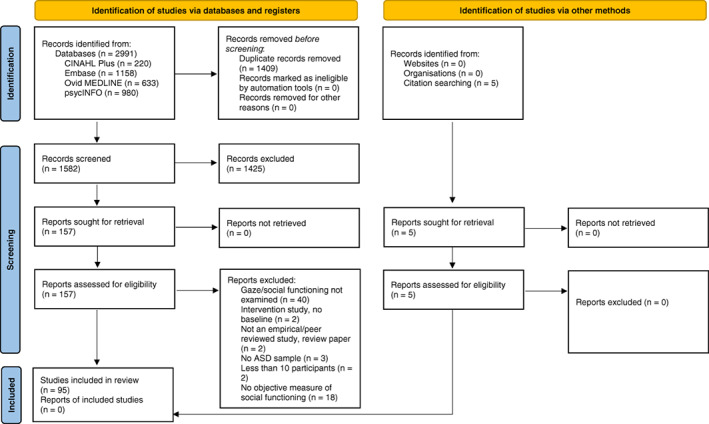
PRISMA flow diagram
TABLE 1.
List of gaze measures employed across studies by task
| Gaze measure | Studies |
|---|---|
| Free viewing | |
| Eye contact | |
| Duration | Jones et al. (2017). |
| Frequency | Jones et al. (2017). |
| Dwell/looking time | Bacon et al. (2020), Campbell et al. (2014), Chawarska and Shic (2009), Chawarska et al. (2012), Chawarska et al. (2016), Crawford et al. (2015), Crehan and Althoff (2021), Crehan et al. (2020), Cuve et al. (2021), Frazier et al. (2016), Frazier et al. (2018), Groen et al. (2012), Kaliukhovich et al. (2020), Macari et al. (2021), Murias et al. (2018), Nadig et al. (2010), Plesa‐Skwerer et al. (2019), Sasson et al. (2007), Sawyer et al. (2012), Shic et al. (2011), Shic et al. (2020). |
| Dynamic scanning index | Wilson et al. (2012). |
| Entropy | |
| Gaze transition entropy | Cuve et al. (2021). |
| Stationary gaze entropy | Cuve et al. (2021). |
| Eye fixation points | Ohya et al. (2014). |
| Gaze allocation | Amso et al. (2014). |
| Gaze following | Sumner et al. (2018). |
| Gaze shifts (no. correct) | Franchini et al. (2017). |
| Gaze similarity | Avni et al. (2020), Tenenbaum et al. (2021), Wang et al. (2018). |
| Fixation | |
| Change | Kliemann et al. (2010). |
| Count/number/percentage/proportion | Bast et al. (2021), Corden et al. (2008), Crehan and Althoff (2021), Cuve et al. (2021), Fedor et al. (2018), Hanley et al. (2015), Kou et al. (2019), McPartland et al. (2011), Rigby et al. (2016), Snow et al. (2011), Unruh et al. (2016), Vivanti et al. (2014). |
| Duration/time | Amestoy et al. (2015), Asberg Johnels et al. (2017), Avni et al. (2020), Bast et al. (2021), Bird et al. (2011), Bradshaw et al. (2019), Chawarska and Shic (2009), Cole et al. (2017), Crehan and Althoff (2021), Crehan et al. (2020), Cuve et al. (2021), Del Valle Rubido et al. (2018), Fedor et al. (2018), Franchini et al. (2016), Frost‐Karlsson et al. (2019), Fujioka et al. (2016), Fujioka et al. (2020), Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Gillespie‐Smith, Riby, et al. (2014), Greene et al. (2020), Griffin and Scherf (2020), Grynszpan and Nadel (2014), Hanley et al. (2014), Jones et al. (2008), Jones and Klin (2013), Kirchner et al. (2011), Klin et al. (2002), Kou et al. (2019), Moore et al. (2018), Muller et al. (2016), Norbury et al. (2009), Parish‐Morris et al. (2013), Pierce et al. (2011), Pierce et al. (2016), Riby and Hancock (2009a), Riby and Hancock (2009b), Riby et al. (2013), Rice et al. (2012), Rigby et al. (2016), Sasson et al. (2016), Shaffer et al. (2017), Speer et al. (2007), Sumner et al. (2018), Swanson and Siller (2013), Thorup et al. (2017), Unruh et al. (2016), White et al. (2015), Wieckowski and White (2016), Xavier et al. (2015), Zamzow et al. (2014), Zantinge et al. (2017). |
| Latency | Crawford et al. (2015), Frost‐Karlsson et al. (2019), Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Gillespie‐Smith, Riby, et al. (2014), Hanley et al. (2014), Sumner et al. (2018), Unruh et al. (2016). |
| Likelihood | Del Bianco et al. (2021). |
| Responsive search score | Ohya et al. (2014). |
| Saccadic indices | |
| Amplitude | Cuve et al. (2021). |
| Amplitude, duration, peak velocity, velocity main sequence | Bast et al. (2021). |
| Number | Xavier et al. (2015). |
| Total eye scanning length | Ohya et al. (2014). |
| Visual exploration | Sasson et al. (2008). |
| Visual search | |
| Fixation duration | Wang et al. (2020). |
| Latency | Glennon et al. (2020). |
| Looking time (target) | Bavin et al. (2014). |
| Saccadic error | Keehn and Joseph (2016). |
| Search asymmetry | Keehn and Joseph (2016). |
| Search intercept | Joseph et al. (2009). |
| Search slope | Joseph et al. (2009). |
| Saccadic paradigms | |
| Antisaccade | |
| Error rate | DiCriscio et al. (2016). |
| Latency | DiCriscio et al. (2016). |
| Distractor task | |
| Accuracy | Lindor et al. (2019). |
| Predictive saccades | |
| Visit count (violation trials) | Greene et al. (2019). |
| Prosaccade | |
| Accuracy | Zalla et al. (2016). |
| Disengagement, gap effect | Keehn et al. (2019), McLaughlin et al. (2021). |
| Facilitation (gap‐baseline) | Glennon et al. (2020). |
| Gaze cueing | Kuhn et al. (2010). |
| Latency | DiCriscio et al. (2016), Zalla et al. (2016). |
| Variability | Zalla et al. (2016). |
| Velocity | Zalla et al. (2016). |
TABLE 2.
List of regions of interest employed by free viewing studies
| Region of interest | Studies |
|---|---|
| Face/head (N = 33) | Avni et al. (2020), Chawarska and Shic (2009), Chawarska et al. (2012), Cole et al. (2017), Del Bianco et al. (2021), Del Valle Rubido et al. (2018), Gillespie‐Smith, Riby, et al. (2014), Greene et al. (2020), Griffin and Scherf (2020), Grynszpan and Nadel (2014), Hanley et al. (2014), Kaliukhovich et al. (2020), Kirchner et al. (2011), Macari et al. (2021), Murias et al. (2018), Nadig et al. (2010), Parish‐Morris et al. (2013), Plesa‐Skwerer et al. (2019), Riby and Hancock (2009a), Riby and Hancock (2009b), Rigby et al. (2016), Sasson et al. (2007), Sasson et al. (2016), Shic et al. (2011), Shic et al. (2020), Snow et al. (2011), Sumner et al. (2018), Swanson and Siller (2013), Vivanti et al. (2014), White et al. (2015), Wilson et al. (2012), Xavier et al. (2015), Zantinge et al. (2017). |
| Eyes (N = 32) | Amestoy et al. (2015), Asberg Johnels et al. (2017), Avni et al. (2020), Chawarska and Shic (2009), Corden et al. (2008), Crawford et al. (2015), Crehan and Althoff (2021), Crehan et al. (2020), Cuve et al. (2021), Del Valle Rubido et al. (2018), Fedor et al. (2018), Fujioka et al. (2016), Fujioka et al. (2020), Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Hanley et al. (2014), Hanley et al. (2015), Jones et al. (2008), Jones and Klin (2013), Jones et al. (2017), Kirchner et al. (2011), Klin et al. (2002), McPartland et al. (2011), Muller et al. (2016), Murias et al. (2018), Norbury et al. (2009), Plesa‐Skwerer et al. (2019), Rice et al. (2012), Sawyer et al. (2012), Speer et al. (2007), White et al. (2015), Wieckowski and White (2016), Zamzow et al. (2014). |
| Mouth (N = 23) | Amestoy et al. (2015), Asberg Johnels et al. (2017), Chawarska and Shic (2009), Chawarska et al. (2012), Corden et al. (2008), Cuve et al. (2021), Del Valle Rubido et al. (2018), Fedor et al. (2018), Fujioka et al. (2016), Fujioka et al. (2020), Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Hanley et al. (2015), Jones et al. (2008), Kirchner et al. (2011), Klin et al. (2002), Muller et al. (2016), Murias et al. (2018), Norbury et al. (2009), Plesa‐Skwerer et al. (2019), Rice et al. (2012), Sawyer et al. (2012), Wieckowski and White (2016), Zamzow et al. (2014). |
| Nose (N = 4) | Chawarska and Shic (2009), Cuve et al. (2021), Del Valle Rubido et al. (2018), Zamzow et al. (2014). |
| Hand (N = 2) | |
| Body (N = 7) | Del Valle Rubido et al. (2018), Jones et al. (2008), Kaliukhovich et al. (2020), Klin et al. (2002), Muller et al. (2016), Sasson et al. (2007), Speer et al. (2007). |
| People (N = 4) | Del Valle Rubido et al. (2018), Frost‐Karlsson et al. (2019), Murias et al. (2018), Shic et al. (2011). |
| Global scene (N = 10) | Avni et al. (2020), Bast et al. (2021), Chawarska et al. (2012), Chawarska et al. (2016), Cuve et al. (2021), Griffin and Scherf (2020), Murias et al. (2018), Shic et al. (2011), Tenenbaum et al. (2021), Wang et al. (2018). |
| Object and nonbiological targets (N = 22) | Cole et al. (2017), Del Valle Rubido et al. (2018), Franchini et al. (2017), Fujioka et al. (2020), Gillespie‐Smith, Riby, et al. (2014), Greene et al. (2020), Griffin and Scherf (2020), Jones et al. (2008), Kaliukhovich et al. (2020), Klin et al. (2002), Muller et al. (2016), Murias et al. (2018), Ohya et al. (2014), Plesa‐Skwerer et al. (2019), Riby et al. (2013), Rice et al. (2012), Sasson et al. (2008), Shic et al. (2011), Snow et al. (2011), Swanson and Siller (2013), Thorup et al. (2017), Vivanti et al. (2014). |
| Background (N = 3) | Del Valle Rubido et al. (2018), Kaliukhovich et al. (2020), Shic et al. (2011). |
| Face versus non‐face (N = 4) | Amso et al. (2014), Bird et al. (2011), Chawarska et al. (2016), Greene et al. (2020). |
| Eyes versus mouth (N = 6) |
Bird et al. (2011), Bradshaw et al. (2019), Chawarska and Shic (2009), Chawarska et al. (2016), Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Kliemann et al. (2010). |
| Dual social and nonsocial stimuli (N = 18) | Bacon et al. (2020), Bradshaw et al. (2019), Campbell et al. (2014), Chawarska and Shic (2009), Chawarska et al. (2016), Del Valle Rubido et al. (2018), Franchini et al. (2016), Frazier et al. (2016), Frazier et al. (2018), Fujioka et al. (2016), Fujioka et al. (2020), Groen et al. (2012), Kou et al. (2019), Moore et al. (2018), Pierce et al. (2011), Pierce et al. (2016), Shaffer et al. (2017), Unruh et al. (2016). |
| Biological motion displays (N = 4) | Del Valle Rubido et al. (2018), Fujioka et al. (2016), Fujioka et al. (2020), Kou et al. (2019). |
Social functioning measures included clinical autism measures (social domain and total scores), behavioral functioning (social subscales), social impairment, and performance on social functioning tasks (including emotion recognition, face recognition, gender identification, joint attention, and ToM). Additionally, three studies created composite measures of social functioning from individual tasks/scales. An overview of these can be found in Table 3.
TABLE 3.
List of social functioning and autism symptom severity measures used across studies
| Social functioning/autism symptom severity measure | Studies |
|---|---|
| Autism symptom scales | |
| Autism Behavior Checklist (Volkmar et al., 1988) | |
| Total | Wang et al. (2020). |
| Autism Behavior Inventory (Bangerter et al., 2017, 2019) | |
| Social communication | Kaliukhovich et al. (2020). |
| Core ASD symptom scale | Kaliukhovich et al. (2020). |
| Autism Diagnostic Interview—Revised (ADI‐R; Lord et al., 1994; Rutter et al., 2003) | |
| Reciprocal social interaction | Amestoy et al. (2015), Grynszpan and Nadel (2014), Plesa‐Skwerer et al. (2019), Tenenbaum et al. (2021), Zalla et al. (2016). |
| Social affect | Bast et al. (2021). |
| Social interaction | Keehn and Joseph (2016). |
| Social score | Kirchner et al. (2011), Kliemann et al. (2010), Speer et al. (2007), Zamzow et al. (2014), Zantinge et al. (2017). |
| Total | Kliemann et al. (2010). |
| Autism Diagnostic Observation Schedule (ADOS, ADOS‐2, ADOS‐G, ADOS‐T; Hus et al., 2011; Lord et al., 1989; Lord et al., 1999; Lord et al., 2000; Lord et al., 2002; Lord, Luyster, et al., 2012; Lord, Rutter, et al., 2012; Luyster et al., 2009) | |
| Communication and social interaction | Del Valle Rubido et al. (2018). |
| Comparison score | Avni et al. (2020). |
| Reciprocal social interaction | Corden et al. (2008), Del Valle Rubido et al. (2018), DiCriscio et al. (2016), Groen et al. (2012), Zalla et al. (2016). |
| Severity score | Rice et al. (2012), Zantinge et al. (2017). |
| Severity score (calibrated) | Bast et al. (2021), Fedor et al. (2018), Keehn et al. (2019), Plesa‐Skwerer et al. (2019), Tenenbaum et al. (2021). |
| Social | Joseph et al. (2009), Norbury et al. (2009), Speer et al. (2007). |
| Social affect | Amso et al. (2014), Bast et al. (2021), Frazier et al. (2016), Jones and Klin (2013), Kaliukhovich et al. (2020), Kou et al. (2019), Macari et al. (2021), Moore et al. (2018), Pierce et al. (2011), Plesa‐Skwerer et al. (2019), Shic et al. (2011), Wang et al. (2018). |
| Social affect (calibrated severity score) | Bast et al. (2021), Jones et al. (2017). |
| Social affect/communication | Pierce et al. (2016). |
| Social algorithm | Jones et al. (2008), Klin et al. (2002). |
| Social communication | McLaughlin et al. (2021), Unruh et al. (2016), Vivanti et al. (2014). |
| Social interaction | Keehn and Joseph (2016). |
| Symptom severity | Bird et al. (2011), Franchini et al. (2016), Frazier et al. (2016), Frazier et al. (2018), Murias et al. (2018), Unruh et al. (2016). |
| Total algorithm score | Shic et al. (2020). |
| Total score (calibrated severity score) | Bast et al. (2021), Bradshaw et al. (2019), Griffin and Scherf (2020), Shic et al. (2020). |
| Total score (module 1) | Campbell et al. (2014). |
| Global/total score | Amestoy et al. (2015), Avni et al. (2020), Bacon et al. (2020), Chawarska et al. (2012), Chawarska et al. (2016), Corden et al. (2008), Del Valle Rubido et al. (2018); Kaliukhovich et al. (2020), Kou et al. (2019), McLaughlin et al. (2021), Moore et al. (2018), Nadig et al. (2010), Pierce et al. (2011), Pierce et al. (2016), Thorup et al. (2017). |
| Autism Spectrum Screening Questionnaire (ASSQ; Ehlers et al., 1999) | |
| Total score (caregiver rated, teacher rated) | Ohya et al. (2014). |
| Autism Spectrum Quotient (AQ, AQ28; Baron‐Cohen, Wheelwright, Skinner, et al., 2001; Baron‐Cohen et al., 2006; Hoekstra et al., 2011) | |
| Total score | Asberg Johnels et al. (2017), Corden et al. (2008), Cuve et al. (2021), Kuhn et al. (2010), Rigby et al. (2016). |
| Childhood Autism Rating Scale (CARS; Schopler et al., 1998) | |
| Total | Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Gillespie‐Smith, Riby, et al. (2014), Grynszpan and Nadel (2014), Riby and Hancock (2009a), Riby and Hancock (2009b), Riby et al. (2013). |
| Pervasive Developmental Disorder Behavior Inventory (PDD‐BI; Cohen et al., 2003) | |
| Expressive/receptive social communication | Murias et al. (2018), Tenenbaum et al. (2021). |
| Autism composite | Murias et al. (2018), Tenenbaum et al. (2021). |
| Social Communication Questionnaire (SCQ; Rutter et al., 2003) | |
| Social subscale | Sasson et al. (2008). |
| Total score | Bavin et al. (2014), Crawford et al. (2015), Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), Gillespie‐Smith, Riby, et al. (2014), Greene et al. (2019), Parish‐Morris et al. (2013), Shaffer et al. (2017), Sumner et al. (2018), Vivanti et al. (2014). |
| Behavioral scales | |
| Aberrant Behavior Checklist (ABC; Aman et al., 1985) | |
| Lethargy/social withdrawal subscale | Del Valle Rubido et al. (2018), Kaliukhovich et al. (2020), Shaffer et al. (2017), Tenenbaum et al. (2021). |
| Behavior Assessment System for Children, 2nd Edition (BASC‐2; Goldin et al., 2014) | |
| Social skills | Murias et al. (2018). |
| Five to Fifteen (FTF; Kadesjo et al., 2004) | |
|
Social competence subscale |
Frost‐Karlsson et al. (2019). |
| Composite measures | |
| Autism traits | |
| Principal components analysis of Autism Diagnostic Observation Schedule (ADOS‐2; Lord et al., 2000), Social Responsiveness Scale (SRS; Constantino et al., 2003 ), The Awareness of Social Inference Test (TASIT; McDonald et al., 2006 ), and Autism Spectrum Quotient (AQ; Baron‐Cohen, Wheelwright, Skinner, et al., 2001 ). | Cole et al. (2017). |
| Face processing accuracy | |
| Composite of Let us Face It! Matching Identity Across Expression and Matchmaker Expression Subtests (Tanaka et al., 2012; Wolf et al., 2008 ) | Parish‐Morris et al. (2013). |
| Theory of Mind Battery | |
| Unexpected contents first‐order false‐belief task (Smarties Task; Wimmer & Hartl, 1991 ), unexpected location first‐order false belief task (Sally and Andy Task; Wimmer & Perner, 1983 ), belief desire reasoning task (Nice Surprise Task; Harris et al., 1989 ), unexpected location second‐order false‐belief task (Grandad Story; Perner & Wimmer, 1985 ) | Hanley et al. (2014). |
| Emotion Recognition Tasks | |
| Dynamic emotional face paradigm | Cuve et al. (2021). |
| Ekman‐Friesen test of facial affect recognition (Ekman & Friesen, 1976) | |
| Happy, sad, angry, surprised, disgusted, fear recognition | Corden et al. (2008). |
| Emotion classification task | |
| Total | Kliemann et al. (2010). |
| Emotions in context task | |
| Accuracy | Sasson et al. (2016). |
| Emotion recognition task/s | |
| Accuracy | Wieckowski and White (2016), Xavier et al. (2015). |
| Accuracy (basic expression, complex expression) | Sawyer et al. (2012). |
| Free choice response expression task | |
| Accuracy | Wieckowski and White (2016). |
| Penn Emotion Recognition Task (ER‐40; Gur et al., 2002) | |
| Composite score | Greene et al. (2020). |
| Social scenes task (emotion recognition) | |
| Accuracy | Sasson et al. (2007). |
| Face recognition tasks | |
| Cambridge Face Memory Test (CFMT; Duchaine & Nakayama, 2006) | |
| Immediate recognition, delayed recognition | Fedor et al. (2018). |
| Total | Kirchner et al. (2011). |
| Face‐fan memory task | |
| Recognition accuracy | Snow et al. (2011). |
| Face recognition test | |
| Accuracy | Wilson et al. (2012). |
| Visual Paired Comparison paradigm (VPC; Fantz, 1964) | |
| Familiar, novel, novelty preference ratio | Chawarska and Shic (2009). |
| Gender identification | |
| Mind in the Eyes: Gender task (Baron‐Cohen, Wheelwright, Scahill, et al., 2001) | |
| Total correct | McPartland et al. (2011). |
| Joint attention tasks | |
| Early Social Communication Scale (ESCS; Mundy et al., 2003) | |
| Total correct | Franchini et al. (2017). |
| Social functioning scales | |
| Movie for the Assessment of Social Cognition (MASC; Dziobek et al., 2006) | |
| Total | Muller et al. (2016). |
| Social Skills Improvement System (SSIS; Gresham & Elliott, 2008) | |
| Social skills (parent report) | Griffin and Scherf (2020). |
| Social Responsiveness Scale (SRS, SRS‐2; Constantino & Gruber, 2002, 2005, 2012; Constantino et al., 2003) | |
| Parent/caregiver rated | Bacon et al. (2020). |
| Autistic mannerisms subscale | Hanley et al. (2015), Shaffer et al. (2017). |
| Social awareness subscale | Hanley et al. (2015), Shaffer et al. (2017), Swanson and Siller (2013). |
| Social cognition subscale | Hanley et al. (2015), Kaliukhovich et al. (2020), Shaffer et al. (2017). |
| Social communication subscale | Hanley et al. (2015), Kaliukhovich et al. (2020), Shaffer et al. (2017). |
| Social communication and interaction | Kaliukhovich et al. (2020). |
| Social motivation subscale | Hanley et al. (2015), Kaliukhovich et al. (2020), Shaffer et al. (2017). |
| Total | Bast et al. (2021), Crehan and Althoff (2021), Del Bianco et al. (2021), Frazier et al. (2016), Frazier et al. (2018), Fujioka et al. (2020), Glennon et al. (2020), Greene et al. (2020), Griffin and Scherf (2020), Hanley et al. (2015), Jones et al. (2017), Kaliukhovich et al. (2020), Keehn et al. (2019), Lindor et al. (2019), McLaughlin et al. (2021), Shaffer et al. (2017), Speer et al. (2007), Thorup et al. (2017), Unruh et al. (2016), White et al. (2015). |
| Self‐rated | |
| Total | Bast et al. (2021), Fujioka et al. (2016), Greene et al. (2019), Greene et al. (2020). |
| Theory of mind tasks | |
| Hinting Task (Corcoran et al., 1995) | |
| Total | Greene et al. (2020). |
| Reading the Mind in the Eyes Test (RMET; Baron‐Cohen, Wheelwright, Hill, et al., 2001) | |
| Total | Kirchner et al. (2011). |
| Theory of Mind Inventory—Second Edition, self‐report (ToMI‐2‐SR; Hutchins et al., 2014) | |
| Early, basic, advanced | Crehan and Althoff (2021), Crehan et al. (2020). |
| Total | Crehan and Althoff (2021). |
Results are presented by the type of eyetracking paradigm employed, with the free viewing studies further classified by ROI.
Free viewing studies
Individual interest areas
Biological interest areas
Face/head
A total of 33 studies examined the face/head ROI, with 20 identifying significant relationships between gaze toward the face and social functioning/autism symptom severity. Of these, 13 demonstrated significant relationships where reductions in looking time toward the face ROI was associated with decreased social functioning/increased autism symptom severity (refer to Table 4). Three studies found the opposite relationship. Sasson et al. (2007) found that increased gaze duration to the face was associated with reductions in emotion accuracy in ASD. Results indicated that the level of engagement with the face/head stimuli was also relevant to the association between gaze and social functioning/autism symptom severity. Chawarska and Shic (2009) found that increased gaze allocation to the face was associated with poorer face recognition performance (on the Visual Paired Comparison paradigm; Fantz, 1964) in participants with ASD, reflective of restricted scanning of internal facial features, while Del Valle Rubido et al. (2018) found that increased gaze toward the face during a gender discrimination task was associated with higher scores on the ADOS Reciprocal and Social Interaction and ADOS Communication and Social Interaction domains.
TABLE 4.
Summary of findings—Face/head region (N = 33)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Avni et al. (2020) | Fixation duration | Dynamic, social | Face |
ADOS‐2 (Total score) |
71 | ASD | 59 Males, 12 Females |
5.1 years (1.8 years) |
‐ | ‐ | No | ns |
| Chawarska and Shic (2009) | Looking time (familiar, novel preference), fixation duration (novelty preference ratio) | Static, social |
Face (inner) |
VPC (familiar preference) |
14 Age Group 1, 30 Age Group 2 | 27 Autism, 17 PDD‐NOS | 84% Males |
Age Group 1 26.9 months (6.2 months) Age Group 2 46.4 months (6.4 months) |
Age Group 1 VDQ: 61 (37), NVDQ: 85 (24) Age Group 2 VDQ: 66 (36), NVDQ: 76 (25) |
‐ | No |
Positive correlation (controlling for CA, VDQ, NVDQ) |
| VPC (novel preference, novelty preference ratio) |
ns (controlling for CA, VDQ, NVDQ) |
|||||||||||
| Face (outer) |
VPC (familar preference, novel preference, novelty preference ratio) |
ns (controlling for CA, VDQ, NVDQ) |
||||||||||
| Chawarska et al. (2012) | Looking time | Dynamic, social | Face | ADOS‐G (Total score) | 54 | Autism | 85% Males | 21.6 months (2.9 months) |
VMA: 9.1 months (5.8 months) NVMA: 16.6 months (4.5 months) |
EL‐RL Split: 8.1 (23.4) |
No | ns |
| Cole et al. (2017) | Fixation duration | Dynamic, social (implicit mentalizing: mentalizing‐action, mentalizing‐either; explicit mentalizing: mentalizing vs. non‐mentalizing) | Head | Autism Traits (principal components analysis of ADOS‐2, AQ, SRS, TASIT) | 17 ASD, 17 NT | ASD (14 Asperger's, 3 ASD), NT |
ASD 10 Males 7 Females NT 10 Males, 7 Females |
ASD 23.71 years (9.24 years) NT 23.71 years (9.07 years) |
ASD WASI IQ: 120.12 (9.32) WASI Verbal Score: 62.88 (6.66) NT WASI IQ: 120.00 (10.09) WASI Verbal Score: 61.61 (7.52) |
‐ | Yes (NT) |
ns |
| Del Bianco et al. (2021) | Fixation likelihood | Static, social | Head | SRS‐2 (T‐score, time 1) |
Cluster 1 294 AUT Cluster 2 25 AUT |
AUT |
Cluster 1 2.87 (Male: Female) Cluster 2 2.00 (Male: Female) |
Cluster 1 16.43 years (5.84 years) Cluster 2 16.03 years (6.43 years) |
Cluster 1 FSIQ: 103.33 (15.92) Cluster 2 FSIQ: 104.14 (10.51) |
‐ | No |
Cluster 1 ns (intercept, slope, quadratic, cubic) Cluster 2 Positive correlation (quadratic component), ns (intercept, slope, cubic) (age corrected correlations) |
| Del Valle Rubido et al. (2018) | Fixation duration |
Static, social (gaze discrimination) Static, social (gender discrimination) |
Inside the face |
ADOS (Total, RSI, CSI), ABC (L/SW) ADOS (RSI, CSI) ADOS (Total), ABC (L/SW) |
38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | ns |
| Positive correlation | ||||||||||||
| ns | ||||||||||||
| Gillespie‐Smith, Riby, et al. (2014) | Fixation duration, first fixation latency | Static social/nonsocial | Face | CARS, SCQ | 21 | ASD | 20 Males, 1 Female | 13 years, 7 months (30 months) |
BPVS‐II VA: 74 (27) RCPM NVA: 27 (7) |
‐ | No | ns |
| Greene et al. (2020) | Fixation duration | Dynamic, social | Face | Hinting Task, ER‐40, SRS‐2 (caregiver/self) |
SCIT‐A: 20 TAU: 21 |
ASD |
SCIT‐A 15 Males, 5 Females TAU 19 Males, 2 Females |
SCIT‐A 17.25 years (3.58 years) TAU 17.90 years (4.1 years) |
SCIT‐A FSIQ: 95.85 (16.53) TAU FSIQ: 114.90 (12.83) |
‐ | No | ns |
| Griffin and Scherf (2020) | Fixation duration |
Dynamic, social (gaze following task) Static, social (gaze perception task) |
Face | ADOS‐2 (Total CSS), SRS‐2 (Total), SSIS‐p (Social Skills). | 35 | ASD | 29 Males, 6 Females | 13.5 years (2.7 years) | VIQ: 96.8 (17.7); PIQ: 102.4 (14.2); FSIQ: 100.1 (15.7) | ‐ | No | ns |
| Grynszpan and Nadel (2014) | Fixation duration | Dynamic, social | Face (gaze contingent) |
ADI‐R (RSI), CARS |
11 | Autism | 9 Males, 2 Females | 21.36 years (4.41 years) |
VIQ: 88.91 (15.33) RPM: 47.03 (10.01) |
‐ | No | Negative correlation |
| Hanley et al. (2014) | Fixation duration | Dynamic, social | Face | ToM composite |
ASD: 17 SLI: 14 NT: 16 |
ASD, SLI, NT |
ASD 11 Males, 6 Females SLI 12 Males, 2 Females NT 6 Males, 10 Females |
ASD 121 months (25 months) SLI 115.2 months (10 months) NT 119.6 months (8 months) |
ASD VA: 84.5 (12.1) NVA: 92.9 (13.764) SLI VA: 84.4 (5.8) NVA: 93.79 (6.852) NT VA: 94.06 (8.621) NVA: 95.56 (7.174) |
‐ | Yes (SLI, NT) |
ns (first order correlation) |
| Fixation latency (anticipatory gaze) |
Negative correlation (controlling for age, verbal ability) |
|||||||||||
| Kaliukhovich et al. (2020) | Looking time | Dynamic, social | Heads (mutual gaze) | ADOS‐2 (Social Affect, Total) | 107 | ASD | 80 Males, 27 Females | 14.6 years (8.0 years) | KBIT‐2 IQ composite: 98.4 (19.9) | ‐ | No |
Negative correlation (controlling for age, sex, IQ) |
| ABC (L/SW), ABI (Symptom Scale, Social Communication), SRS‐2 (Total) |
ns (controlling for age, sex, IQ) |
|||||||||||
| Heads (shared focus) |
ABI, ABC (L/SW), ADOS‐2, SRS‐2 (Total) |
120 | ASD | 91 Males, 29 Females | 14.6 years (8.0 years) | KBIT‐2 IQ Composite: 98.9 (19.9) | ‐ |
ns (controlling for age, sex, IQ) |
||||
| Kirchner et al. (2011) | Fixation duration |
Static, social (MET: emotion recognition and face identity average) |
Face | ADI‐R (Social Score), CFMT, RMET | 20 | ASC | 15 Males, 5 Females | 31.9 years (7.6 years) | W‐IQ: 112.6 (11.6) | ‐ | No | ns |
| Macari et al. (2021) | Looking time | Dynamic, social (dyadic bid/tickle conditions, 6 months) | Face | ADOS‐T SA (18 months, 24 months) |
176 (21 HR‐ASD, 74 HR‐C, 32 HR‐TD, 49 LR‐TD) |
HR‐ASD, HR‐C, HR‐TD, LR‐TD | 81% Males (HR‐ASD), 70.3% Males (HR‐C), 50.0% Males (HR‐TD), 40.8% Males (LR‐TD) | a Age by group/timepoint |
bMSEL VDQ cMSEL NVDQ |
‐ | Yes (HR‐C, HR‐TD, LR‐TD) | ns (controlling for sex) |
| Dynamic, social (dyadic bid condition, 9 months) | ADOS‐T SA (18 months, 24 months) | Negative correlation (controlling for sex) | ||||||||||
| Dynamic, social (tickle condition, 9 months) | ADOS‐T SA (18 months, 24 months) | ns (controlling for sex) | ||||||||||
| Dynamic, social (dyadic bid condition, 12 months) | ADOS‐T SA (18 months) | Negative correlation (controlling for sex) | ||||||||||
| ADOS‐T SA (24 months) | ns (controlling for sex) | |||||||||||
| Dynamic, social (tickle condition, 12 months) | ADOS‐T SA (18 months, 24 months) | Negative correlation (controlling for sex) | ||||||||||
| Murias et al. (2018) | Looking time | Dynamic, social (dyadic bid) | Face | BASC‐2 (Social Skills); PDD‐BI (Expressive/Receptive Social Communication) | 23 | ASD | 19 Males, 4 Females | 53.6 months (13.5 months) | NVIQ: 64.7 (25.2) | ‐ | No | ns (controlling for age and NVIQ, otherwise positive predictive relationship) |
| PDD‐BI (Autism Composite); ADOS‐2 (Severity) |
ns (controlling/not controlling for age, NVIQ) |
|||||||||||
| Nadig et al. (2010) | Looking time | Dynamic, social (generic) | Face | ADOS (Total score, corrected for item B1) | 12 | HFA | 10 Males, 2 Females | 11 years, 4 months | ‐ | ‐ | No | Negative correlation |
| Dynamic, social (interest) | ns | |||||||||||
| Parish‐Morris et al. (2013) | Fixation duration | Dynamic, social | Face | Face processing accuracy (composite of Let's Face It! Matching Identity Across Expression and Matchmaker Expression subtests) | 60 ASD, 50 NT | ASD, NT |
ASD 53 Males, 7 Females NT 38 Males, 12 Females |
ASD 11.28 years (2.89 years) NT 11.34 years (3.04 years) |
ASD GCA: 111.63 (14.61) NT GCA: 113.70 (14.58) |
ASD Verbal: 110.12 (16.61), Nonverbal: 111.07 (15.48) NT Verbal: 116.42 (16.70), Nonverbal: 108.26 (13.71) |
Yes (NT) |
Positive predictive relationship (gaze > face processing skill) (controlling for age) |
|
SCQ |
ns |
|||||||||||
| Plesa‐Skwerer et al. (2019) | Looking time | Dynamic, social | Face (collapsed across episodes) |
ADI‐R (RSI), ADOS (overall CSS, Social Affect) |
37 MV‐ASD; 34 V‐ASD | ASD |
MV‐ASD 29 Males, 8 Females V‐ASD 26 Males, 8 Females |
MV‐ASD 13.56 years (3.5 years); V‐ASD 14.97 years (3.4 years) |
Nonverbal Reasoning MV‐ASD Leiter‐3: 62.14 (14.7) V‐ASD WASI‐PR: 104.15 (23.2) |
EL MV‐ASD 20.61 (10.8) V‐ASD 109.24 (81.3) RL MV‐ASD 26.88 (14.5) V‐ASD 102.58 (71.6) |
No |
ns (controlling for NVIQ) |
| Face (expected gaze) |
ADI‐R (RSI) |
Negative correlation (controlling for NVIQ) |
||||||||||
| ADOS (overall CSS, Social Affect CSS) |
ns (controlling for NVIQ) |
|||||||||||
| Face (unexpected gaze) | ADI‐R (RSI), ADOS (overall CSS, Social Affect CSS) |
ns (controlling for NVIQ) |
||||||||||
| Riby and Hancock (2009a) | Fixation duration |
Static, social (cartoons); dynamic, social (human actors); dynamic, social (cartoons) |
Face | CARS (Total score) | 20 | Autism | 15 Males, 5 Females | 13 years, 4 months (48 months) | RCPM: 13 (4) | ‐ | No | Negative correlation |
| Riby and Hancock (2009b) | Fixation duration |
Static, social (embedded picture, scrambled picture) |
Face | CARS (Total score) | 24 | Autism | 18 Males, 6 Females | 12 years, 4 months | RCPM: 12 | ‐ | No | Negative correlation |
| Rigby et al. (2016) | Fixation duration |
Static/dynamic, social (single, multiple characters) |
Faces | AQ | 16 ASD, 16 NT | ASD, NT |
ASD 11 Males, 5 Females NT 11 Males, 5 Females |
ASD 27.8 years (7.8 years) NT 27.3 years (7.5 years) |
ASD FSIQ: 106.3 (10.8), VIQ: 107.8 (13.9), PIQ: 103.9 (15.7) NT FSIQ: 113.4 (8.7), VIQ: 110.7 (9.5), PIQ: 113.3 (11.4) |
‐ | Yes (NT) | Negative correlation |
| Fixation duration, no. fixations (per trial) | Static/dynamic, social (multiple characters) | Individual faces | ||||||||||
| Sasson et al. (2007) | Looking time |
Static, social (face present) |
Face | Social scenes task (emotion recognition) | 10 | Autism | 10 Males |
23.0 years (5.27 years) |
IQ: 107.8 (17.15) | ‐ | No | Negative correlation |
| Static, social (face absent) | ns | |||||||||||
| Sasson et al. (2016) | Fixation duration |
Static, social (congruent, incongruent, scene) |
Face | ECT | 21 | ASD | 18 Males, 3 Females |
23.43 years (4.36 years) |
101.48 (16.97) | ‐ | No | ns |
| Shic et al. (2011) | Looking time | Dynamic, social | Heads | ADOS‐G (Social Affect) | 28 | ASD (20 autistic disorder, 8 PDD‐NOS) | 22 Males, 6 Females | 20.7 months (3.0 months) |
VDQ: 59.7 (28.5); NVDQ: 89.9 (17.3); VMA: 12.1 months (5.9 months); NVMA: 18.4 months (4.1 months). |
‐ | No | Negative correlation |
| Shic et al. (2020) | Looking time | Dynamic, social |
△%Face (%Face DG+SP+ minus %Face DG‐SP‐) |
ADOS‐2 (Total algorithm/CSS score, concurrent/prospective measures) | 50 ASD, 47 NT | ASD, NT |
ASD 88% Males NT 51% Males |
ASD 22.6 months (3.1 months) NT 22.1 months (3.2 months) |
ASD VDQ: 51.7 (21.5), NVDQ: 82.8 (15.8) NT VDQ: 117.2 (17.1), NVDQ: 113.0 (14.8) |
‐ | Yes (NT) |
Negative correlation (controlling/not controlling for VDQ/NVDQ) |
| Snow et al. (2011) | No. fixations | Static, social | Face |
Face recognition accuracy (face‐fan task) |
22 | ASD | 21 Males, 1 Female |
15.96 years (2.44 years) |
FSIQ: 111.50 (17.57) | ‐ | No | Positive correlation |
| Sumner et al. (2018) | Fixation duration | Static, social (combined individual and social conditions) | Face | SCQ | 28 ASD, 25 NT, 28 DCD | ASD, DCD, NT |
ASD 24 Males, 4 Females NT 22 Males, 3 Females DCD 21 Males, 7 Females |
ASD 8.58 years (1.18 years) NT 9.10 years (1.07 years) DCD 8.53 years (1.16 years) |
FSIQ: ASD 101.32 (14.32) NT 110.64 (10.07) DCD 95.93 (12.47) |
‐ | Yes (DCD, NT) | Negative correlation (combined ASD, NT, DCD), ns (separate groups) |
| First fixation latency, gaze following | Static, social | nr | ns | |||||||||
| Swanson and Siller (2013) | Fixation duration | Dynamic, social | Face (congruent vs. incongruent) | SRS (Social Awareness) | 21 ASD, 24 NT | ASD, NT |
ASD 18 Males, 3 Females NT 20 Males, 4 Females |
ASD 87.24 months (18.39 months) NT 81.67 months (19.21 months) |
ASD NVMA: 84.67 months (20.28 months), NVDQ: 98.78 (19.08) NT NVMA: 87.29 months (25.15 months), NVDQ: 107.75 (22.18) |
ASD RL standard (PPVT‐4): 97.81 (21.58); EL standard (EOWPVT‐4): 98.43 (18.76) NT RL standard (PPVT‐4): 103.63 (9.15); EL standard (EOWPVT‐4): 99.63 (10.72) |
Yes (NT) | Significant SRS (social awareness) x condition interaction (controlling for EL). Differences in gaze allocation between conditions when SRS < 70.25. |
| Vivanti et al. (2014) | Fixation proportion | Dynamic, social | Face | ADOS (Social Communication), SCQ | 24 | ASD | 21 Males, 3 Females | 46.54 months (10.55 months) | MSEL composite age equivalent score: 30.39 (12.15) |
MSEL RL age equivalent: 26.75 (14.78) MSEL EL age equivalent: 29.75 (35.22) |
No | ns |
| White et al. (2015) | Fixation duration | Static, social | Face (happy, disgust, angry) | SRS (Total, parent‐rated) | 15 | ASD | 8 Males, 7 Females |
14.88 years (1.552 years) |
‐ | ‐ | No | ns |
| Wilson et al. (2012) | Dynamic scanning index | Static, social | Face regions (left/right eye, nose, mouth) | Face recognition | 11 | ASD | 7 Males, 4 Females | 10.21 years (2.00 years) | WASI matrices: 45.72 (11.60) | TROG‐2: 82.55 (20.09) | No |
Positive correlation (controlling for nonverbal IQ, receptive grammar, and social communication, average percentage of time viewing face) |
| Xavier et al. (2015) | Fixation duration | Static, social | Face | Emotion recognition (combined and individual visual unimodal/bimodal) | 19 | ASD | 14 Males, 5 Females | 9.95 years (1.75 years) |
IQ: 78.5 (21.02) Mental age: 7.74 years (2.51 years) |
‐ | Yes (NT) | ns |
| No. saccades | ||||||||||||
| Zantinge et al. (2017) | Fixation duration | Dynamic, social (anger clip) | Face | ADI‐R (Social), ADOS (Severity score) | 28 | ASD | 26 Males, 2 Females | 57.96 months (10.06 months) | FSIQ: 83.71 (22.32) | ‐ | No | Negative predictive relationship |
Abbreviations: ABC, Aberrant Behavior Checklist; ABI, Autism Behavior Inventory; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; ADOS‐T, Autism Diagnostic Observation Schedule, toddler module; AQ, Autism Spectrum Quotient; ASC, autism spectrum conditions; ASD, autism spectrum disorder; AUT, autistic; BASC‐2, Behavior Assessment System for Children, Second Edition; BPVS‐2, British Picture Vocabulary Scale, Second Edition; CA, chronological age; CARS, Childhood Autism Rating Scale; CFMT, Cambridge Face Memory Test; CSI, communication and social interaction; CSS, calibrated severity score; DCD, developmental coordination disorder; DG+SP+, direct gaze and speech; DG+SP+, no direct gaze and no speech; ECT, emotions in context task; EL, expressive language; EOWPVT‐4, Expressive One‐Word Picture Vocabulary Test, Fourth Edition; ER‐40, Penn Emotion Recognition Task; FSIQ, full scale intelligence quotient; GCA, general conceptual ability; HFA, high functioning autism; HR‐ASD, high risk autism spectrum disorder; HR‐C, high risk complex; HR‐TD, high risk typically developing; IQ, intelligence quotient; KBIT‐2, Kaufmann Brief Intelligence Test, Second Edition; L/SW, lethargy/social withdrawal; LR‐TD, low risk typically developing; MET, Multifaceted Empathy Test; MSEL, Mullen Scales of Early Learning; MV‐ASD, minimally verbal children and adolescents with autism spectrum disorder; nr, not reported; ns, not significant; NT, neurotypical; NVA, nonverbal age; NVDQ, nonverbal developmental quotient; NVIQ, nonverbal intelligence quotient; NVMA, nonverbal mental age; PDD‐BI, Pervasive Developmental Disorder – Behavior Inventory; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; PPVT‐4, Peabody Picture Vocabulary Test, Fourth Edition; RCPM, Raven's Colored Progressive Matrices; RL, receptive language; RMET, Reading the Mind in the Eyes Test; RPM, Raven's Progressive Matrices; RSI, reciprocal social interaction; SCIT‐A, Social Cognition and Interaction Training for Autism; SCQ, Social Communication Questionnaire; SLI, specific language impairment; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; SSIS‐p, Social Skills Improvement System, parent report; TASIT, The Awareness of Social Inference Test; TAU, treatment as usual; ToM, theory of mind; TROG‐2, Test for Reception of Grammar, Second Edition; VA, verbal age; V‐ASD, verbally fluent children and adolescents with autism spectrum disorder; VDQ, verbal developmental quotient; VIQ, verbal intelligence quotient; VMA, verbal mental age; VPC, Visual Paired Comparison paradigm; WASI, Wechsler Abbreviated Scale of Intelligence; WASI‐PR, Wechsler Abbreviated Scale of Intelligence, perceptual reasoning scale; W‐IQ, Wortschatztest Intelligence Quotient.
6 months: HR‐ASD: 6.4 months (0.6 months); HR‐C: 6.5 months (1.0 months); HR‐TD: 6.4 months (0.6 months); LR‐TD: 6.2 months (0.3 months); 12 months: HR‐ASD: 12.5 months (0.5 months); HR‐C: 12.4 months (0.7 months); HR‐TD: 12.5 months (0.6 months); LR‐TD: 12.3 months (0.6 months); 18 months: HR‐ASD: 18.2 months (0.5 months); HR‐C: 18.5 months (0.8 months); HR‐TD: 18.4 months (0.8 months); LR‐TD: 18.6 months (0.9 months); 24 months: HR‐ASD: 24.5 months (1.1 months); HR‐C: 24.8 months (1.3 months); HR‐TD: 24.7 months (1.6 months); LR‐TD: 24.5 months (1.0 months).
6 months: HR‐ASD: 78.7 (12.2); HR‐C: 77.5 (17.1); HR‐TD: 79.1 (13.2); LR‐TD: 84.3 (13.2); 12 months: HR‐ASD: 75.0 (20.3); HR‐C: 82.3 (16.9); HR‐TD: 96.7 (16.5); LR‐TD: 95.6 (19.1); 18 months: HR‐ASD: 78.8 (30.4); HR‐C: 85.6 (23.6); HR‐TD: 114.2 (19.4); LR‐TD: 115.5 (18.3); 24 months: HR‐ASD: 92.6 (25.7); HR‐C: 103.6 (20.9); HR‐TD: 120.2 (16.5); LR‐TD: 127.1 (18.6).
6 months: HR‐ASD: 94.1 (13.7); HR‐C: 93.1 (23.8); HR‐TD97.9 (23.8); LR‐TD: 97.8 (16.5); 12 months: HR‐ASD: 103.3 (12.0); HR‐C: 112.9 (13.7); HR‐TD: 113.4 (12.0); LR‐TD: 118.9 (11.7); 18 months: HR‐ASD: 97.2 (11.2); HR‐C: 100.9 (10.9); HR‐TD: 109.3 (10.7); LR‐TD: 110.8 (11.7); 24 months: HR‐ASD: 94.7 (17.2); HR‐C: 103.1 (13.4); HR‐TD: 113.8 (14.1); LR‐TD: 116.6 (13.2).
Three studies used joint attention paradigms exploring congruent/expected (where a model's gaze is directed toward a target) and incongruent/unexpected (where a model's gaze is directed away from a target) gaze. Across a combined sample of participants with ASD and neurotypical controls, Swanson and Siller (2013) found a significant moderating effect of social functioning ability. Specifically, differences in fixation duration toward the face between congruent and incongruent conditions were only evident in participants with high levels of social awareness (using the Social Awareness subscale of the SRS). In participants with ASD, Plesa‐Skwerer et al. (2019) found that reduced looking time to the face was associated with higher scores on the Autism Diagnostic Interview‐Revised (ADI‐R) Reciprocal Social Interaction subscale during the expected gaze shift condition, with no relationship identified for the unexpected gaze shift condition. No significant relationships with the ADOS Overall and Social Affect calibrated severity scores were identified. In participants with ASD, Kaliukhovich et al. (2020) demonstrated that increased looking time to the heads of actors was associated with increased social functioning (ADOS‐2 Social Affect) and reduced autism symptom severity (ADOS‐2 Total) only when actors were gazing at each other, but not when actors' gaze was focused on a shared activity. However, no associations were identified for social domains of the Autism Behavior Inventory or Aberrant Behavior Checklist, and the authors urged caution in interpretation of the results given the number of multiple comparisons performed.
Further evidence linking difficulties prioritizing attention to socially pertinent information with ToM was demonstrated by Hanley et al. (2014). Across participants with ASD, specific language impairment and neurotypical controls, there was an association between longer anticipatory gaze (defined as the delay in gaze toward a social actor to determine their awareness of an unexpected event occurring) and reduced ToM performance (a composite of four false‐belief tasks).
There is also evidence to suggest that gaze allocation to the face in ASD is associated with autism symptom severity in tasks requiring higher levels of social exchange. Nadig et al. (2010) examined gaze duration to the face of the researcher while they engaged in a brief face‐to‐face conversation with participants with ASD relating to either a pre‐identified specific circumscribed interest or a more generic topic (e.g., pets). A significant negative relationship between ADOS Total score (excluding item B1 “unusual eye contact”) and fixations on the face was identified during conversation about the generic topic, although a trend level negative relationship was identified for the circumscribed interest topic.
Overall, there is an indication that the relationship between gaze toward the face and social functioning/autism symptom severity is dependent on the social context relating to the face. Research remains limited and future directions might include further investigation to determine how allocation of gaze toward the face is used to support social functioning.
Eyes
A total of 32 studies investigated gaze directed toward the eyes, with 15 of these identifying significant positive associations between gaze allocation to the eyes and social functioning and inverse associations with autism symptom severity (refer to Table 5). Contrastingly, one study, Chawarska and Shic (2009) found that increased gaze allocation to the eyes was associated with poorer face recognition performance (on the Visual Paired Comparison paradigm; Fantz, 1964) in participants with ASD, reflective of limited scanning of internal facial features.
TABLE 5.
Summary of findings—Eyes (N = 32)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Amestoy et al. (2015) | Fixation time (total) | Static, social | Eyes | ADI‐R (RSI) |
Adults: 13 Children: 14 |
ASD |
Adults: 12 Males, 1 Female Children: 11 Males, 3 Females |
Adults: 23.8 years (3.6 years) Children: 11.3 years (2.1 years) |
Adults: VIQ: 107.2 (18); NVIQ: 102.1 (15) Children: VIQ: 94.5 (17); NVIQ: 89.8 (11) |
‐ | No | Negative correlation |
| Asberg‐Johnels et al. (2017) | Fixation duration | Dynamic, social (neutral, fearful, happy, angry) | Eyes | AQ |
ASD Adults: 27 Adolescents: 30 NT Adults: 27 Adolescents: 31 |
ASD Adults: 9 AD, 17 AS, 1 PDD‐NOS Adolescents: 17 AD, 12 AS, 1 PDD‐NOS NT Adults: 27, Adolescents: 27 |
‐ |
ASD Adults: 29.0 years (8.0 years) Adolescents: 15.0 years (2.2 years) NT Adults: 27.0 years (6.4 years) Adolescents: 14.8 years (2.2 years) |
ASD Adults: PIQ: 109.2 (16.5) Adolescents: PIQ: 102.3 (15.8) NT Adults: PIQ: 112.9 (8.6) Adolescents: PIQ: 113.6 (14.8) |
‐ | Yes (NT) |
ns (ASD‐Adult and ASD‐Adolescent separately, full sample, collapsed across diagnosis and age) |
| Avni et al. (2020) | Fixation duration | Dynamic, social | Eyes |
ADOS‐2 (Total score) |
71 | ASD | 59 Males, 12 Females | 5.1 years (1.8 years) | ‐ | ‐ | No | ns |
| Chawarska and Shic (2009) | Looking time (familiar, novel preference), fixation duration (novelty preference ratio) | Static, social | Eyes | VPC (familiar preference) | 14 Age Group 1, 30 Age Group 2 | 27 autism, 17 PDD‐NOS | 84% Males |
Age Group 1 26.9 months (6.2 months) Age Group 2 46.4 months (6.4 months) |
Age Group 1 VDQ: 61 (37), NVDQ: 85 (24) Age Group 2 VDQ: 66 (36), NVDQ: 76 (25) |
‐ | No |
Positive correlation (controlling for CA, VDQ, NVDQ) |
| VPC (novelty preference, novelty preference ratio) |
ns (controlling for CA, VDQ, NVDQ) |
|||||||||||
| Corden et al. (2008) | Percentage total fixations | Static, social | Eyes |
Ekman‐Friesen test of facial affect recognition (fear recognition) |
18 | AS | 13 Males, 5 Females | 32.9 years (13.35 years) | VIQ: 116.3 (9.14), NVIQ: 117.1 (14.56), FSIQ: 119.9 (11.10) | ‐ | No |
Positive correlation Positive prediction |
| Ekman‐Friesen test of facial affect recognition (happy, sad, angry, surprised, disgusted recognition), ADOS, AQ. | ns | |||||||||||
| Eyes (sad, fear, angry, surprised, disgusted) | Ekman‐Friesen test of facial affect recognition (fear recognition) | Positive prediction | ||||||||||
| Eyes (happy) | ns | |||||||||||
| Crawford et al. (2015) | Looking time, fixation latency | Static, social (neutral faces) | Eyes | SCQ | 15 ASD, 13 FXS | ASD (8 autistic disorder, 2 asperger syndrome, 5 PDD‐NOS), FXS |
ASD 80% Males FXS 92.31% Males |
ASD 11.00 years (3.48 years) FXS 19.70 years (9.00 years) |
‐ | ‐ | Yes (FXS) | ns |
|
Crehan and Althoff (2021) |
Dwell time, fixation count, second fixation duration |
Dynamic, static (stable vs. dynamic) | Eyes |
SRS‐A, ToMI‐2‐SR (early, basic, advanced, total) |
15 ASD, 21 NT | ASD, NT |
ASD 33% Females NT 48% Females |
ASD 21.20 years (3.10 years) NT 20.05 years (1.16 years) |
ASD IQ: 117.00 (11.73) NT IQ: 109.71 (14.05) |
‐ | Yes (NT) | ns |
| Dynamic, static (more eye contact vs. less eye contact) | SRS‐A | Negative correlation, ns (regression model, controlling for age, sex and IQ) | ||||||||||
| Dwell time, fixation count | Dynamic, static (more eye contact vs. less eye contact) | ToMI‐2‐SR (early, advanced, total) | Positive correlation, positive prediction (advanced only), ns (regression model—total scale only). Regressions controlling for age, sex, and IQ. | |||||||||
| ToMI‐2‐SR (basic) | ns | |||||||||||
| Second fixation duration | Dynamic, static (more eye contact vs. less eye contact) | ToMI‐2‐SR (advanced) | Positive correlation, ns (regression model, controlling for age, sex, and IQ). | |||||||||
| ToMI‐2‐SR (basic, early, total) | ns | |||||||||||
| Crehan et al. (2020) | Dwell time |
Dynamic, social (catching another staring) |
Eyes | ToMI‐2‐SR (advanced) | 15 ASD, 17 NT | ASD, NT |
ASD 67% Males NT 52% Males |
ASD 21.20 years (3.10 years) NT 20.05 years (1.16 years) |
ASD IQ: 117.00 (11.73) NT IQ: 109.71 (14.05) |
‐ | Yes (NT) | Positive correlation |
| Dynamic, social (getting caught staring); static, social (mutual) | ToMI‐2‐SR (advanced) | Positive correlation | ||||||||||
| ToMI‐2‐SR (early, basic) | ns | |||||||||||
| Static, social (averted) | ToMI‐2‐SR (advanced) | ns | ||||||||||
| Fixation duration (second fixation) | Dynamic, social (getting caught staring) | ToMI‐2‐SR (advanced) | Positive correlation | |||||||||
| Static, social (mutual) | Negative correlation | |||||||||||
| Dynamic, social (catching another staring); static, social (averted) | ToMI‐2‐SR (early, basic, advanced) |
ns |
||||||||||
| Cuve et al. (2021) | Fixation duration, fixation count | Dynamic, social | Eyes | AQ28, emotion recognition | 25 ASD, 45 NT | ASD, NT |
ASD 13 Males, 11 Females NT 16 Males, 29 Females |
ASD 37.68 years (11.86 years) NT 26.13 years (6.66 years) |
ASD IQ: 121.68 (16.49) NT IQ: 117.76 (13.52) |
‐ | nr | ns |
| Del Valle Rubido et al. (2018) | Fixation duration | Dynamic, social (complex movies), static, social (gender discrimination) | Eyes | ADOS (Total, RSI, CSI); ABC (L/SW) | 38 | ASD | 38 Males | 24.2 years (5.8 years) |
FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) |
‐ | No | ns |
| Fedor et al. (2018) | Fixation duration, fixation count | Static, social (immediate recognition, delayed recognition) | Eyes | ADOS CSS, CFMT | 24 children, 23 adolescents, 19 adults | Autism |
Children: 21 Males, 3 Females Adolescents: 19 Males, 4 Females Adults: 18 Males, 1 Female |
Children: 11.2 years (1.7 years), Adolescents: 15.3 years (1.5 years), Adults: 24.2 years (4.9 years) |
Children VIQ: 108.7 (13.0), PIQ: 114.4 (13.3), FSIQ: 112.8 (12.9) Adolescents VIQ: 106.3 (13.2), PIQ: 107.1 (13.1), FSIQ: 107.7 (13.3) Adults VIQ: 109.8 (13.0), PIQ: 110.3 (15.9), FSIQ: 111.3 (14.6) |
‐ | No |
ns (controlling for FSIQ, age) |
| Fujioka et al. (2016) | Fixation duration |
Dynamic, social (human face, blinking) Static, social (still human face); dynamic, social (human face, mouth moving; human face, silent; human face, talking) |
Eyes | SRS | 21 | ASD | 21 Males | 27.6 years (7.7 years) |
FSIQ: 99.8 (13.5) VIQ: 103.3 (13.3) PIQ: 96.4 (16.0) Note, N = 20 |
‐ | No | ns |
| Fujioka et al. (2020) | Fixation duration | Dynamic/social (face with mouth motion, face without mouth motion) | Eyes | SRS‐2 |
ASD 0–5 years 19 6–11 years 34 12–18 years 30 NT 0–5 years 120 6–11 years 150 12–18 years 37 |
ASD, NT |
ASD 0–5 years 14 Males, 5 Females 6–11 years 28 Males, 6 Females 12–18 years 22 Males, 8 Females NT 0–5 years 58 Males, 62 Females 6–11 years 69 Males, 81 Females 12–18 years 14 Males, 23 Females |
ASD 0–5 years 4.7 years (0.9 years) 6–11 years 9.2 years (1.6 years) 12–18 years 14.5 years (1.6 years) NT 0–5 years 4.6 years (1.0 years) 6–11 years 8.7 years (1.7 years) 12–18 years 14.2 years (1.5 years) |
ASD IQ/DQ > 70 |
‐ | Yes (NT) |
ns (whole group and ASD only, controlling for age, sex) |
| Gillespie‐Smith, Doherty‐Sneddon, et al. (2014) | Fixation duration | Static, social (familiar face) | Eyes | CARS, SCQ | 21 | ASD | 20 Males, 1 Female | 13 years, 7 months (30 months) |
BPVS‐II VA: 74 (27) RCPM NVA: 27 (7) |
‐ | No | ns |
| Static, social (unfamiliar face) | Eyes | CARS | ns | |||||||||
| SCQ | Negative correlation, HSF = LSF | |||||||||||
| Static, social (self‐face) | Eyes |
CARS |
ns | |||||||||
| SCQ | Negative correlation, HSF > LSF | |||||||||||
| First fixation latency | Static, social (familiar, unfamiliar, self‐face) | Eyes | CARS, SCQ | ns | ||||||||
| Hanley et al. (2014) | Fixation duration | Dynamic, social | Eyes | ToM composite |
17 ASD, 14 SLI, 16 NT |
ASD, SLI, NT |
ASD 11 Males, 6 Females SLI 12 Males, 2 Females NT 6 Males, 10 Females |
ASD 121 months (25 months) SLI 115.2 months (10 months) NT 119.6 months (8 months) |
ASD VA: 84.5 (12.1) NVA: 92.9 (13.764) SLI VA: 84.4 (5.8) NVA: 93.79 (6.852) NT VA: 94.06 (8.621) NVA: 95.56 (7.174) |
‐ | Yes (SLI, NT) |
Positive correlation (controlling for age, verbal ability) |
| Hanley et al. (2015) | Percentage fixations | Dynamic, social | Eyes | SRS (Social Awareness domain) | 11 | ASD | 7 Males, 4 Females | 26 years (8.1 years) | VIQ: 120 (14); PIQ: 111 (9) | ‐ | No | Negative correlation |
| SRS (Total score, Social Cognition domain, Social Communication domain, Social Motivation domain, Autistic Mannerisms domain) | ns | |||||||||||
| Jones et al. (2008) | Fixation duration | Dynamic, social | Eyes | ADOS (Social Algorithm total score) | 15 | ASD | 11 Males, 4 Females | 2.28 years (0.58 years) | VF AE (MSEL R/E): 1.17 years (0.66 years); NVF (MSEL VR): 1.77 years (0.47 years). |
‐ |
No | Negative correlation |
| Jones and Klin (2013) | Fixation duration | Dynamic, social | Eyes | ADOS (Social Affect)—24 months | 11 | ASD | 11 Males |
2–24 months |
Mullen NV AE: 23.36 (6.20) |
Mullen RL AE: 22.45 (7.59), Mullen ELV AE: 22.18 (7.56) |
No | Negative correlation |
| 2–6 months, 2–9 months |
ns |
|||||||||||
| 2–12 months, 2–15 months, 2–18 months | Negative correlation | |||||||||||
| Jones et al. (2017) | Eye contact duration | Dynamic, social (conversation) | Eyes | ADOS (CSS Social Affect); SRS‐2 (total T score) |
ASD (Sample 1) 20 ASD (Sample 2) 20 |
ASD |
ASD (Sample 1) 16 Males, 4 Females ASD (Sample 2) 12 Males, 3 Females |
ASD (Sample 1) 7.0 years (2.1 years) ASD (Sample 2) 8 years (2.8 years) |
ASD (Sample 1) VIQ: 105.55 (18), NVIQ: 109.75 (25). ASD (Sample 2) VIQ: 95.07 (26), NVIQ: 99.40 (29). |
‐ | Yes (NT, SRS only) | Negative correlation |
| Dynamic, social (interactive play) | ADOS (CSS Social Affect); SRS‐2 (total T score) | ns | ||||||||||
| Eye contact frequency | Dynamic, social (conversation, interactive play) |
ADOS (CSS Social Affect) |
||||||||||
| Kirchner et al. (2011) | Fixation duration | Static, social (MET: emotion recognition and face identity average) | Eyes |
RMET |
20 | ASC | 15 Males, 5 Females | 31.9 years (7.6 years) | W‐IQ: 112.6 (11.6) | ‐ | No | Positive correlation |
| ADI‐R (Social score), CFMT |
ns |
|||||||||||
| Klin et al. (2002) | Fixation duration |
Dynamic, social |
Eyes |
ADOS (Social Algorithm) |
15 | Autism | 15 Males | 15.4 years (7.3 years) | VIQ: 101.3 (24.9) | ‐ | No | ns |
| McPartland et al. (2011) | Fixations (proportion) | Static, social (upright face stimuli) | Eyes |
Mind in the Eyes: Gender task |
15 | ASD | 13 Males, 2 Females | 14.5 years (1.7 years) | PIQ: 115.1 (11.8) | ‐ | No | ns |
| Muller et al. (2016) | Fixation duration | Dynamic, social | Eyes | MASC |
33 ASD, 23 NT |
ASD, NT |
ASD 27 Males, 6 Females NT 14 Males, 9 Females |
ASD 15.6 years (1.9 years) NT 16.3 years (2.4 years) |
ASD GAI: 101.1 (14.4) NT GAI: 109.8 (15.1) |
‐ | Yes (NT) | Positive prediction |
| Murias et al. (2018) | Looking time | Dynamic, social (dyadic bid) | Eyes | BASC‐2 (Social Skills); PDD‐BI (Expressive/Receptive Social Communication), PDD‐BI (Autism Composite); ADOS‐2 (Severity) | 23 | ASD | 19 Males, 4 Females | 53.6 months (13.5 months) | NVIQ: 64.7 (25.2) | ‐ | No | ns |
| Norbury et al. (2009) | Fixation duration | Dynamic, social | Eyes | ADOS (Social) | 14 ALI, 14 ALN | ASD | 27 Males, 1 Females |
ALI 14.9 years (1.2 years) ALN 14.9 years (1.4 years) |
ALI Verbal: 81.9 (22.8) Nonverbal: 96.6 (15.7) ALN Verbal: 101.9 (16.3) Nonverbal: 99.7 (14.3) |
ALI CELF‐III, Sentence Repetition: 4.1 (1.4). ALN CELF‐III Sentence Repetition: 8.8 (1.8). |
No |
ns (ALI/ALN combined, ALI and ALN separately) |
| Plesa‐Skwerer et al. (2019) | Looking time | Dynamic, social | Eyes (collapsed across episodes) | ADI‐R (RSI), ADOS (overall CSS, Social Affect CSS) | 37 MV‐ASD; 34 V‐ASD | ASD |
MV‐ASD 29 Males, 8 Females V‐ASD 26 Males, 8 Females |
MV‐ASD 13.56 years (3.5 years) V‐ASD 14.97 years (3.4 years) |
MV‐ASD Leiter‐3: 62.14 (14.7) V‐ASD WASI‐PR: 104.15 (23.2) |
MV‐ASD RL: 26.88 (14.5), EL: 20.61 (10.8) V‐ASD RL: 102.58 (71.6), EL: 109.24 (81.3) |
No |
ns (controlling for NVIQ) |
| Eyes (unexpected gaze) |
ADOS (overall CSS) |
Negative correlation (controlling for NVIQ) |
||||||||||
| ADI‐R (RSI), ADOS (Social Affect CSS) |
ns (controlling for NVIQ) |
|||||||||||
| Eyes (expected gaze) |
ADI‐R (RSI), ADOS (overall CSS, Social Affect CSS) |
ns (controlling for NVIQ) |
||||||||||
| Rice et al. (2012) | Fixation duration | Dynamic, social | Eyes | ADOS (Severity) |
ASD (Additional) 72 ASD (Matched) 37 |
37.6% Autism, 12.8% Asperger Syndrome, 49.5% PDD‐NOS |
ASD (Additional) 53 Males, 19 Females ASD (Matched) 30 Males,7 Females |
ASD (Additional) 10.2 years (3.5 years) ASD (Matched) 10.0 years (2.3 years) |
ASD (Additional) FSIQ: 88.7 (19.8), VIQ: 88.5 (19.7), NVIQ: 92.3 (19.4) ASD (Matched) FSIQ: 112.0 (15.2), VIQ: 111.4 (16.3), NVIQ: 111.4 (14.5) |
‐ | No |
Negative correlation (even FSIQ group, higher even FSIQ group) ns (total ASD, N = 109; VIQ split; NVIQ split, lower even FSIQ group, higher even FSIQ Group = lower even FSIQ Group) |
| Sawyer et al. (2012) | Looking time | Static, social |
Eyes |
Emotion recognition task (basic expression) Emotion recognition task (complex expression) |
29 Asperger's, 24 NT | Asperger's, NT | nr |
Asperger's 21.6 years (9.8 years) NT 24.0 years (9.2 years) |
Asperger's VIQ: 109.7 (19.1), NVIQ:104.3 (18.2), FSIQ: 108.1 (17.9) NT VIQ:113.4 (12.8), NVIQ: 111.4 (12.8), FSIQ: 108.1 (17.9) |
‐ | Yes (NT) |
ns (overall group, Asperger's group only) |
| Speer et al. (2007) | Fixation duration | Dynamic, social | Eyes | ADI‐R (Social), ADOS (Social) | 12 ASD, 12 NT | ASD, NT |
ASD 12 Males NT 12 Males |
ASD 13.60 years (2.70 years) NT 13.30 years (2.30 years) |
ASD VIQ: 96.3 (15.0) PIQ: 104.5 (17.66) NT VIQ: 100.3 (10.1) PIQ: 108.25 (14.52) |
‐ | Yes (NT, SRS only) | ns |
| SRS (Total) | Negative correlation | |||||||||||
| White et al. (2015) | Fixation duration | Static, social | Eyes (happy, disgust, angry) | SRS (parent‐rated) | 15 | ASD | 8 Males, 7 Females | 14.88 years (1.552 years) | ‐ | ‐ | No | ns |
| Wieckowski and White (2016) | Fixation duration | Dynamic, social | Eyes | Emotion recognition (accuracy), free choice response expression task | 20 | ASD (16 Asperger's, 4 autism) | 14 Males, 6 Females | 14.65 years (1.79 years) | ‐ | ‐ | No |
ns (Fixation duration, fixation duration x emotion type) |
| Zamzow et al. (2014) | Fixation duration | Dynamic, social | Eyes | ADI‐R (Social) | 12 | ASD | 9 Males, 3 Females | 18.25 years (2.66 years) | IQ: 103.50 (13.04) | ‐ | No | ns |
Abbreviations: ABC, Aberrant Behavior Checklist; AD, autistic disorder; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ALI, autism, language impaired; ALN, autism, language normal; AQ, Autism Spectrum Quotient; AS, Asperger syndrome; ASC, autism spectrum conditions; ASD, autism spectrum disorder; BPVS‐2, British Picture Vocabulary Scale, Second Edition; CA, chronological age; CARS, Childhood Autism Rating Scale; CELF‐III, Clinical Evaluation of Language Fundamentals, Third Edition; CFMT, Cambridge Face Memory Test; CSI, communication and social interaction; CSS, calibrated severity score; DQ, developmental quotient; FSIQ, full scale intelligence quotient; FXS, fragile X syndrome; GAI, general ability index; HSF, high social functioning; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; LSF, low social functioning; MASC, Movie for the Assessment of Social Cognition; MET, Multifaceted Empathy Test; MSEL ELV AE, Mullen Scales of Early Larning, expressive language age equivalent; MSEL NV AE, Mullen Scales of Early Learning, visual reception (nonverbal function) age equivalent; MSEL R/E, Mullen Scales of Early Learning, receptive and expressive language subtests; MSEL RL AE, Mullen Scales of Early Learning, receptive language age equivalent; MSEL VR, Mullen Scales of Early Learning, visual reception subtest; MV‐ASD, minimally verbal children and adolescents with autism spectrum disorder; nr, not reported; ns, not significant; NT, neurotypical; NVA, nonverbal age; NVDQ, nonverbal developmental quotient; NVF, nonverbal function; NVIQ, nonverbal intelligence quotient; PDD‐BI, Pervasive Developmental Disorder‐Behavior Inventory; PDD‐NOS, pervasive developmental disorder‐not otherwise specified; PIQ, performance intelligence quotient; RCPM, Raven's Colored Progressive Matrices; RSI, reciprocal social interaction; SCQ, Social Communication Questionnaire; SLI, specific language impairment; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; SRS‐A, Social Responsiveness Scale, adult self‐report; ToM, theory of mind; ToMI‐2‐SR, Theory of Mind Inventory, Second Edition‐self report; VA, verbal age; V‐ASD, verbally fluent children and adolescents with autism spectrum disorder; VDQ, verbal developmental quotient; VF, verbal function; VIQ, verbal intelligence quotient; VPC, Visual Paired Comparison paradigm; WASI‐PR, Wechsler Abbreviated Scale of Intelligence, perceptual reasoning scale; W‐IQ, Wortschatztest Intelligence Quotient.
There was further evidence to suggest that gaze allocation to the eyes was related to social functioning and autism symptom severity in situations requiring greater social engagement and understanding. In participants with ASD, Gillespie‐Smith, Doherty‐Sneddon, et al. (2014) found that reduced fixation duration to the eyes was associated with higher scores on the Social Communication Questionnaire (SCQ) when viewing self and unfamiliar faces, but not for familiar faces. No significant relationships were identified with the Childhood Autism Rating Scale (CARS). Jones et al. (2017) examined participants with ASD engaging in both interactive play and conversation segments with the researcher. A significant relationship only emerged during the conversational segment (requiring a greater level of reciprocal social interaction), where reductions in eye fixation was associated with higher ADOS Social Affect domain (calibrated severity score), and SRS‐2 Total scores (the latter including neurotypical participants in the analysis). Plesa‐Skwerer et al. (2019) found that reduced fixation duration to the eyes of an actor was associated with increased ADOS Overall calibrated severity scores in participants with ASD. However, this was only when the actors gaze unexpectedly shifted away from the target of interest, but not when gaze shifted toward the target of interest. No significant relationships were identified with the ADI‐R or ADOS social subscales.
Limited studies also suggest a potential influence of participant characteristics on this relationship. Rice et al. (2012) explored the impact of cognitive ability on the relationship between fixation duration to the eyes and ADOS severity scores. In ASD participants with a higher even full scale IQ profile (i.e., verbal IQ = nonverbal IQ, full scale IQ ≥ 98), increased percentage fixation duration to the eyes was associated with lower ADOS severity scores; a pattern not identified in participants with a lower even full scale IQ profile (i.e., verbal IQ = nonverbal IQ, full scale IQ < 98), a verbal advantage (i.e., verbal IQ > nonverbal IQ) or nonverbal advantage (i.e., nonverbal IQ > verbal IQ). In their longitudinal investigation of infants later diagnosed with ASD, Jones and Klin (2013) found that in infants later diagnosed with ASD, a decline in eye fixation from 2 to 24 months of age was associated with increased ADOS Social Affect subscale scores measured at 24 months. The decline in eye fixation from 2 to 24 months of age was further broken down into subsets (2–6 months, 2–9 months, 2–12 months, 2–15 months, 2–18 months), with a statistically significant relationship between eye fixation decline and increased ADOS Social Affect subscale scores emerging at the 2–12 month band (which remained significant for 2–15 month and 2–18 month bands).
The association between eye gaze and social functioning/autism symptom severity appears to be context‐dependent, similar to gaze allocation toward the face more broadly. Further investigation of mediating factors, such as IQ and neurodevelopment of gaze, will be of interest.
Mouth
Of the 23 studies investigating the relationship between gaze to the mouth and social functioning/autism symptom severity, 10 studies identified significant findings (refer to Table 6). The direction of these results, however, were mixed. Some studies found that increased gaze toward the mouth was associated with improved social functioning/autism symptom severity (e.g., Fedor et al., 2018; Klin et al., 2002), while others found that it was associated with deficits in social functioning/autism symptom severity (e.g., Amestoy et al., 2015; Hanley et al., 2015).
TABLE 6.
Summary of findings – Mouth (N = 23)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Amestoy et al. (2015) | Fixation time (total) | Static, social | Mouth | ADOS (Global) |
Adults: 13 Children: 14 |
ASD |
Adults: 12 Males, 1 Female Children: 11 Males, 3 Females |
Adults: 23.8 years (3.6 years) Children: 11.3 years (2.1 years) |
Adults: VIQ: 107.2 (18); NVIQ: 102.1 (15) Children: VIQ: 94.5 (17); NVIQ: 89.8 (11) |
‐ | No | Positive correlation |
| Asberg‐Johnels et al. (2017) | Fixation duration |
Dynamic, social (neutral, fearful, happy, angry) |
Mouth | AQ |
ASD Adults: 27 Adolescents: 30 NT Adults: 27 Adolescents: 31 |
ASD Adults: 9 AD, 17 AS, 1 PDD‐NOS Adolescents: 17 AD, 12 AS, 1 PDD‐NOS NT Adults: 27, Adolescents: 27 |
‐ |
ASD Adults: 29.0 years (8.0 years) Adolescents: 15.0 years (2.2 years) NT Adults: 27.0 years (6.4 years) Adolescents: 14.8 years (2.2 years) |
ASD Adults: PIQ: 109.2 (16.5) Adolescents: PIQ: 102.3 (15.8) NT Adults: PIQ: 112.9 (8.6) Adolescents: PIQ: 113.6 (14.8) |
‐ | Yes (NT) |
ns (ASD‐Adult and ASD‐Adolescent separately, full sample, collapsed across diagnosis and age) |
| Dynamic, social (happy vs. neutral) |
ns (ASD‐Adult and ASD‐Adolescent separately) Negative correlation (full sample, collapsed across diagnosis and age) |
|||||||||||
| Chawarska and Shic (2009) | Looking time (familiar, novel preference), fixation duration (novelty preference ratio) | Static, social | Mouth | VPC (familiar preference, novelty preference, novelty preference ratio) | 44 (14 Age Group 1, 30 Age Group 2) | ASD (27 Autism, 17 PDD‐NOS) | 84% Males |
Age Group 1 26.9 months (6.2 months) Age Group 2 46.4 months (6.4 months) |
Age Group 1 VDQ: 61 (37), NVDQ: 85 (24) Age Group 2 VDQ: 66 (36), NVDQ: 76 (25) |
‐ | No |
ns (controlling for CA, VDQ, NVDQ) |
| Chawarska et al. (2012) | Looking time | Dynamic, social | Mouth | ADOS‐G (Total score) | 54 | Autism | 85% Males | 21.6 months (2.9 months) |
Verbal MA: 9.1 months (5.8 months) Nonverbal MA: 16.6 months (4.5 months) |
EL‐RL Split: 8.1 (23.4) | No | ns |
| Corden et al. (2008) | Percentage total fixations | Static, social | Mouth | ADOS (RSI, Total scores), AQ | 18 | AS | 13 Males, 5 Females | 32.9 years (13.35 years) |
VIQ: 116.3 (9.14), NVIQ: 117.1 (14.56), FSIQ: 119.9 (11.10) |
‐ | No | ns |
| Cuve et al. (2021) | Fixation duration, fixation count | Dynamic, social | Mouth | AQ28, emotion recognition | 25 ASD, 45 NT | ASD, NT |
ASD 13 Males, 11 Females NT 16 Males, 29 Females |
ASD 37.68 years (11.86 years) NT 26.13 years (6.66 years) |
ASD IQ: 121.68 (16.49) NT IQ: 117.76 (13.52) |
‐ | Yes (NT) | ns |
| Del Valle Rubido et al. (2018) | Fixation duration |
Dynamic, social (complex social movies) |
Mouth |
ADOS (Total, RSI) |
38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | Negative correlation |
| ADOS (CSI), ABC (L/SW) | ns | |||||||||||
| Static, social (gender discrimination) | ADOS (Total, RSI, CSI), ABC (L/SW) | ns | ||||||||||
| Fedor et al. (2018) | Fixation duration |
Static, social (immediate recognition, delayed recognition) |
Mouth | ADOS CSS, CFMT | 24 Children, 23 Adolescents, 19 Adults | Autism |
Children: 21 Males, 3 Females Adolescents: 19 Males, 4 Females Adults: 18 Males, 1 Female |
Children: 11.2 years (1.7 years), Adolescents: 15.3 years (1.5 years), Adults: 24.2 years (4.9 years) |
Children VIQ: 108.7 (13.0), PIQ: 114.4 (13.3), FSIQ: 112.8 (12.9) Adolescents VIQ: 106.3 (13.2), PIQ: 107.1 (13.1), FSIQ: 107.7 (13.3) Adults VIQ: 109.8 (13.0), PIQ: 110.3 (15.9), FSIQ: 111.3 (14.6) |
‐ | No |
ns (controlling for age and FSIQ) |
| Fixation count |
Static, social (immediate recognition) |
ADOS CSS, CFMT |
ns (controlling for age and FSIQ) |
|||||||||
| Static, social (delayed recognition) | ADOS CSS |
ns (controlling for age and FSIQ) |
||||||||||
| CFMT |
Positive correlation (controlling for age and FSIQ) |
|||||||||||
| Fujioka et al. (2016) | Fixation duration |
Dynamic, social (human face, blinking) |
Mouth | SRS | 21 | ASD | 21 Males | 27.6 years (7.7 years) |
FSIQ: 99.8 (13.5) VIQ: 103.3 (13.3) PIQ: 96.4 (16.0) Note, N = 20 |
‐ | No | Positive correlation |
| Static, social (still human face); dynamic, social (human face, mouth moving); dynamic, social (human face, silent); dynamic, social (human face, talking) | ns | |||||||||||
| Fujioka et al. (2020) | Fixation duration | Dynamic/social (face with mouth motion, face without mouth motion) | Mouth | SRS‐2 |
ASD 0–5 years 19 6–11 years 34 12–18 years 30 NT 0–5 years 120 6–11 years 150 12–18 years 37 |
ASD |
ASD 0–5 years 14 Males, 5 Females 6–11 years 28 Males, 6 Females 12–18 years 22 Males, 8 Females NT 0–5 years 58 Males, 62 Females 6–11 years 69 Males, 81 Females 12–18 years 14 Males, 23 Females |
ASD 0–5 years 4.7 years (0.9 years) 6–11 years 9.2 years (1.6 years) 12–18 years 14.5 years (1.6 years) NT 0–5 years 4.6 years (1.0 years) 6–11 years 8.7 years (1.7 years) 12–18 years 14.2 years (1.5 years) |
IQ/DQ > 70 | ‐ | Yes (NT) |
ns (whole group and ASD only, controlling for age, sex) |
| Gillespie‐Smith, Doherty‐Sneddon, et al. (2014) | Fixation duration | Static, social (familiar face); static, social (unfamiliar face); static, social (self‐face) | Mouth | CARS | 21 | ASD | 20 Males, 1 Female | 13 years, 7 months (30 months) |
BPVS‐II VA: 74 (27) RCPM NVA: 27 (7) |
‐ | No |
ns |
| Static, social (unfamiliar face); static, social (self‐face) | SCQ |
ns (HSF = LSF) |
||||||||||
| First fixation latency | Static, social (familiar, unfamiliar, self‐face) | ns | ||||||||||
| Hanley et al. (2015) | Percentage fixations | Dynamic, social | Mouth | SRS (Social Awareness domain) | 11 | ASD | 7 Males, 4 Females | 26 years (8.1 years) | VIQ: 120 (14); PIQ: 111 (9) | ‐ | No | Positive correlation |
| SRS (Total score, Social Cognition domain, Social Communication domain, Social Motivation domain, Autistic Mannerisms domain) | ns | |||||||||||
| Jones et al. (2008) | Fixation duration | Dynamic, social | Mouth | ADOS (Social Algorithm) | 15 | ASD | 11 Males, 4 Females | 2.28 years (0.58 years) | VF age equivalence (MSEL R/E): 1.17 years (0.66 years); NVF (MSEL VR): 1.77 years (0.47 years). | ‐ | No | ns |
| Kirchner et al. (2011) | Fixation duration | Static, social (MET: emotion recognition and face identity average) | Mouth | RMET, CMFT | 20 | ASC | 15 Males, 5 Females | 31.9 years (7.6 years) | W‐IQ: 112.6 (11.6) | ‐ | No |
Negative correlation Negative prediction |
| ADI‐R (Social score) | ns | |||||||||||
| Klin et al. (2002) |
Fixation duration |
Dynamic, social | Mouth | ADOS (Social Algorithm) | 15 | Autism | 15 Males | 15.4 years (7.3 years) | VIQ: 101.3 (24.9) | ‐ | No | Negative correlation |
| Muller et al. (2016) | Fixation duration | Dynamic, social | Mouth | MASC |
33 ASD, 23 NT |
ASD, NT |
ASD 27 Males, 6 Females NT 14 Males, 9 Females |
ASD 15.6 years (1.9 years) NT 16.3 years (2.4 years) |
ASD GAI: 101.1 (14.4) NT GAI: 109.8 (15.1) |
‐ | Yes (NT) | ns |
| Murias et al. (2018) | Looking time | Dynamic, social (dyadic bid) | Mouth |
BASC‐2 (Social Skills); PDD‐BI (Expressive/Receptive Social Communication) |
23 | ASD | 19 Males, 4 Females | 53.6 months (13.5 months) | NVIQ: 64.7 (25.2) | ‐ | No |
ns (controlling for age and NVIQ, otherwise positive predictive relationship) |
| PDD‐BI (Autism Composite); ADOS‐2 (Severity) |
ns (controlling for age and NVIQ) |
|||||||||||
| Norbury et al. (2009) | Fixation duration | Dynamic, social | Mouth | ADOS (Social) | 28 (14 ALI, 14 ALN) | ASD | 27 Males, 1 Female |
ALI 14.9 years (1.2 years) ALN 14.9 years (1.4 years) |
ALI Verbal: 81.9 (22.8) Nonverbal: 96.6 (15.7) ALN Verbal: 101.9 (16.3) Nonverbal: 99.7 (14.3) |
ALI CELF‐III (Sentence Repetition): 4.1 (1.4). ALN CELF‐III (Sentence Repetition): 8.8 (1.8). |
No |
ns (ALI and ALN combined, ALI and ALN separately) |
| Plesa‐Skwerer et al. (2019) | Looking time | Dynamic, social | Mouth (collapsed across episodes) | ADI‐R (RSI), ADOS (overall CSS, Social Affect) | 37 MV‐ASD; 34 V‐ASD | ASD |
MV‐ASD 29 Males, 8 Females V‐ASD 26 Males, 8 Females |
MV‐ASD 13.56 years (3.5 years); V‐ASD 14.97 years (3.4 years) |
MV‐ASD Leiter‐3: 62.14 (14.7) V‐ASD WASI‐PR: 104.15 (23.2) |
MV‐ASD RL: 26.88 (14.5), EL: 20.61 (10.8) V‐ASD RL: 102.58 (71.6), EL: 109.24 (81.3) |
No |
ns (controlling for NVIQ) |
| Mouth (verbal greeting) | ||||||||||||
| Rice et al. (2012) | Fixation duration | Dynamic, social | Mouth | ADOS (Severity) |
ASD (Additional) 72 ASD (Matched) 37 |
37.6% Autism, 12.8% Asperger Syndrome, 49.5% PDD‐NOS |
ASD (Additional) 53 Males, 19 Females ASD (Matched) 30 Males, 7 Females |
ASD (Additional) 10.2 years (3.5 years) ASD (Matched) 10.0 years (2.3 years) |
ASD (Additional) FSIQ: 88.7 (19.8), VIQ: 88.5 (19.7), NVIQ: 92.3 (19.4) ASD (Matched) FSIQ: 112.0 (15.2), VIQ: 111.4 (16.3), NVIQ: 111.4 (14.5) |
‐ | No |
Negative correlation (VIQ Split), positive correlation (higher even FSIQ group), Higher even FSIQ correlation ≠ lower even FSIQ or VIQ Split correlation ns (Total ASD, N = 109; NVIQ Split, even FSIQ group; lower even FSIQ group) |
| Sawyer et al. (2012) | Looking time | Static, social | Mouth |
Emotion recognition task (basic expression) Emotion recognition task (complex expression) |
29 Asperger's, 24 NT | Asperger's, NT | nr |
Asperger's 21.6 years (9.8 years) NT 24.0 years (9.2 years) |
Asperger's VIQ: 109.7 (19.1), NVIQ:104.3 (18.2), FSIQ: 108.1 (17.9) NT VIQ:113.4 (12.8), NVIQ: 111.4 (12.8), FSIQ: 108.1 (17.9) |
‐ | Yes (NT) |
ns (overall group, Asperger's group only) |
| Wieckowski and White (2016) | Fixation duration | Dynamic, social | Mouth | Emotion recognition (accuracy) | 20 | ASD (16 Asperger's, 4 Autism) | 14 Males, 6 Females | 14.65 years (1.79 years) | FSIQ‐2: 94.90 (16.11) | ‐ | No |
Significant effect of fixation duration to the mouth on accuracy. Increased fixation duration toward mouth with correct identification of sadness versus incorrect identification of sadness. ns (happy, anger, disgust, fear, surprise expressions) |
| Free choice response expression task |
ns (effect of fixation duration on mouth and mirroring emotion). Significant fixation duration x emotion type interaction on mirroring emotion. Increased fixation duration toward mouth with correct versus incorrect mirroring of sadness Increased fixation duration toward mouth with incorrect mirroring versus correct mirroring of sadness. ns (anger, disgust, happy, surprise) |
|||||||||||
| Zamzow et al. (2014) | Fixation duration | Dynamic, social | Mouth | ADI‐R (Social) | 12 | ASD | 9 Males, 3 Females | 18.25 years (2.66 years) |
IQ: 103.50 (13.04) |
‐ | No | ns |
Abbreviations: ABC, Aberrant Behavior Checklist; AD, autistic disorder; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; ALI, autism, language impaired; ALN, autism, language normal; AQ, Autism Spectrum Quotient; AS, Asperger syndrome; ASC, autism spectrum conditions; ASD, autism spectrum disorder; BASC‐2, Behavior Assessment System for Children, Second Edition; BPVS‐2, British Picture Vocabulary Scale, Second Edition; CA, chronological age; CARS, Childhood Autism Rating Scale; CELF‐III, Clinical Evaluation of Language Fundamentals, Third Edition; CFMT, Cambridge Face Memory Test; CSI, communication and social interaction; CSS, calibrated severity score; DQ, developmental quotient; EL, expressive language; FSIQ, full scale intelligence quotient; GAI, general ability index; HSF, high social functioning; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; LSF, low social functioning; MA, mental age; MASC, Movie for the Assessment of Social Cognition; MET, multifaceted empathy test; MSEL R/E, Mullen Scales of Early Learning, receptive and expressive language subtests; MSEL VR, Mullen Scales of Early Learning, visual reception subtest; MV‐ASD, minimally verbal children and adolescents with autism spectrum disorder; nr, not reported; ns, not significant; NT, neurotypical; NVA, nonverbal age; NVDQ, nonverbal developmental quotient; NVF, nonverbal function; NVIQ, nonverbal intelligence quotient; PDD‐BI, Pervasive Developmental Disorder‐Behavior Inventory; PDD‐NOS, pervasive developmental disorder, not otherwise identified; PIQ, performance intelligence quotient; RCPM, Raven's Colored Progressive Matrices; RL, receptive language; RMET, Reading the Mind in the Eyes Test; RSI, reciprocal social interaction; SCQ, Social Communication Questionnaire; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; VA, verbal age; V‐ASD, verbally fluent children and adolescents with autism spectrum disorder; VDQ, verbal developmental quotient; VF, verbal function; VIQ, verbal intelligence quotient; VPC, Visual Paired Comparison paradigm; W‐IQ, Wortschatztest Intelligence Quotient.
Two studies found that gaze allocation to the mouth was associated with both increased and decreased social functioning/autism symptom severity with the direction of findings dependent on cognitive capacity (Rice et al., 2012) or emotion (Wieckowski & White, 2016). In relation to cognitive capacity, Rice et al. (2012) found that participants with ASD and a verbal IQ advantage (i.e., verbal IQ > nonverbal IQ) demonstrated a negative association between percentage fixation duration to the mouth and ADOS severity scores. Conversely, higher ADOS severity scores were related to increased percentage fixation duration to the mouth for participants with a higher even full scale IQ profile (i.e., verbal IQ = nonverbal IQ, full scale IQ ≥ 98). In relation to emotion, Wieckowski and White (2016) identified altered gaze toward the mouth region, where increased gaze was associated with increased performance in the identification and mirroring of sad expressions and with decreased performance in mirroring fear expressions.
Nose
Four studies explored gaze allocation to the nose with social functioning/autism symptom severity (refer to Table 7), with no significant relationships identified (Chawarska & Shic, 2009; Cuve et al., 2021; Del Valle Rubido et al., 2018; Zamzow et al., 2014).
TABLE 7.
Summary of findings—Nose (N = 4)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Chawarska and Shic (2009) | Looking time (familiar, novel preference), fixation duration (novelty preference ratio) | Static, social | Nose | VPC (familiar preference, novelty preference, novelty preference ratio) | 14 Age Group 1, 30 Age Group 2 | 27 autism, 17 PDD‐NOS | 84% Males |
Age Group 1 26.9 months (6.2 months) Age Group 2 46.4 months (6.4 months) |
Age Group 1 VDQ: 61 (37), NVDQ: 85 (24) Age Group 2 VDQ: 66 (36), NVDQ: 76 (25) |
‐ | No |
ns (controlling for CA, VDQ, NVDQ) |
| Cuve et al. (2021) | Looking time | Dynamic, social | Nose | Emotion recognition | 25 ASD, 45 NT | ASD |
ASD 13 Males, 11 Females NT 16 Males, 29 Females |
ASD 37.68 years (11.86 years) NT 26.13 years (6.66 years) |
ASD IQ: 121.68 (16.49) NT IQ: 117.76 (13.52) |
‐ | nr | ns |
| Del Valle Rubido et al. (2018) | Fixation duration | Static, social (gaze discrimination, gender discrimination) | Nose | ADOS (Total, RSI, CSI), ABC (L/SW) | 38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | ns |
| Zamzow et al. (2014) | Fixation duration | Dynamic, social | Nose |
ADI‐R (Social) |
12 | ASD | 9 Males, 3 Females | 18.25 years (2.66 years) | IQ: 103.50 (13.04) | ‐ | No | ns |
Abbreviations: ABC, Aberrant Behavior Checklist; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ASD, autism spectrum disorder; CA, chronological age; CSI, communication and social interaction; FSIQ, full scale intelligence quotient; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; nr, not reported; ns, not significant; NT, neurotypical; NVDQ, nonverbal developmental quotient; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; RSI, reciprocal social interaction; VDQ, verbal developmental quotient; VIQ, verbal intelligence quotient; VPC, Visual Paired Comparison paradigm.
Hand
Two studies explored fixation duration to the hand region with social functioning/autism symptom severity (refer to Table 8), with no significant results identified (Cole et al., 2017; Vivanti et al., 2014).
TABLE 8.
Summary of findings—Hand (N = 2)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Cole et al. (2017) | Fixation duration |
Dynamic, social (implicit mentalizing: mentalizing‐action, mentalizing‐either; explicit mentalizing: mentalizing vs. non‐mentalizing) |
Grasp release point |
Autism traits (principal components analysis of ADOS‐2, AQ, SRS, TASIT) | 17 ASD, 17 NT | ASD (14 Asperger's, 3 ASD), NT |
ASD 10 Males, 7 Females NT 10 Males, 7 Females |
ASD 23.71 years (9.24 years) NT 23.71 years (9.07 years) |
ASD WASI IQ: 120.12 (9.32) WASI verbal score: 62.88 (6.66) NT WASI IQ: 120.00 (10.09) WASI verbal score: 61.61 (7.52) |
‐ | Yes (NT) | ns |
| Vivanti et al. (2014) | Fixation proportion | Dynamic, social (head turning condition) | Grasping action | ADOS (Social Communication), SCQ | 24 | ASD | 21 Males, 3 Females | 46.54 months (10.55 months) | MSEL composite age equivalent score: 30.39 (12.15) |
MSEL RL age equivalent score: 26.75 (14.78) MSEL EL age equivalent score: 29.75 (35.22) |
No | ns |
Abbreviations: ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; AQ, Autism Spectrum Quotient; ASD, autism spectrum disorder; EL, expressive language; IQ, intelligence quotient; ns, not significant; NT, neurotypical; RL, receptive language; SCQ, Social Communication Questionnaire; SRS, Social Responsiveness Scale; TASIT, The Awareness of Social Inference Test; WASI, Wechsler Abbreviated Scale of Intelligence.
Body
Seven studies examined the relationship between fixation duration/looking time to the body and social functioning/autism symptom severity with the general pattern of findings indicating a lack of association between fixation duration to the body and social functioning/autism symptom severity (refer to Table 9). Six of the seven studies employed stimuli in which two or more people were interacting (Del Valle Rubido et al., 2018; Kaliukhovich et al., 2020; Klin et al., 2002; Muller et al., 2016; Sasson et al., 2007; Speer et al., 2007), Jones et al. (2008) included a video of a single actor looking directly into the camera, and Speer et al. (2007) employed stimuli with single and multiple social characters.
TABLE 9.
Summary of findings—Body (N = 7)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Del Valle Rubido et al. (2018) | Fixation duration | Dynamic, social (activity monitoring) | Body | ADOS (Total) | 38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | Negative correlation |
| ABC (L/SW), ADOS (RSI, CSI) | ns | |||||||||||
| Jones et al. (2008) | Fixation duration | Dynamic, social | Body | ADOS (Social Algorithm) | 15 | ASD | 11 Males, 4 Females | 2.28 years (0.58 years) | VF Age Equivalence (MSEL R/E): 1.17 years (0.66 years); NVF (MSEL VR): 1.77 years (0.47 years). | ‐ | No | ns |
| Kaliukhovich et al. (2020) | Looking time | Dynamic, social | Bodies (mutual) | ABI (Symptom Scale, Social Communication), ABC (L/SW), ADOS‐2 (Social Affect, Total), SRS‐2 (Total) | 107 | ASD | 80 Males, 27 Females | 14.6 years (8.0 years) | KBIT‐2 IQ Composite: 98.4 (19.9) |
‐ |
No |
ns (controlling for age, sex, IQ) |
| Bodies (shared focus) | 120 | ASD | 91 Males, 29 Females | 14.6 years (8.0 years) | KBIT‐2 IQ Composite: 98.9 (19.9) | |||||||
| Klin et al. (2002) | Fixation duration | Dynamic, social | Body | ADOS (Social Algorithm) | 15 | Autism | 15 Males | 15.4 years (7.3 years) | VIQ: 101.3 (24.9) | ‐ | No | ns |
| Muller et al. (2016) | Fixation duration | Dynamic, social | Body | MASC |
33 ASD, 23 NT |
ASD |
ASD 27 Males, 6 Females NT 14 Males, 9 Females |
ASD 15.6 years (1.9 years) NT 16.3 years (2.4 years) |
ASD GAI: 101.1 (14.4) NT GAI: 109.8 (15.1) |
‐ | Yes (NT) | ns |
| Sasson et al. (2007) | Looking time | Static, social (face present, face absent) | Body |
Social scenes task |
10 | ASD | 10 Males | 23.0 years (5.27 years) | IQ: 107.8 (17.15) | ‐ | No | ns |
| Speer et al. (2007) | Fixation duration | Dynamic, social | Body | ADI‐R (Social), ADOS (Social), SRS (Total) | 12 | ASD |
ASD 12 Males NT 12 Males |
ASD 13.60 years (2.70 years) NT 13.30 years (2.30 years) |
ASD VIQ: 96.3 (15.0) PIQ: 104.5 (17.66) NT VIQ: 100.3 (10.1) PIQ: 108.25 (14.52) |
‐ | Yes (NT, SRS only) | ns |
Abbreviations: ABC, Aberrant Behavior Checklist; ABI, Autism Behavior Inventory; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ASD, autism spectrum disorder; CSI, communication and social interaction; FSIQ, full scale intelligence quotient; GAI, general ability index; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; MASC, Movie for the Assessment of Social Cognition; MSEL R/E, Mullen Scales of Early Learning, receptive and expressive language subtests; MSEL VR, Mullen Scales of Early Learning, visual reception subtest; ns, not significant; NVF, nonverbal function; PIQ, performance intelligence quotient; RSI, reciprocal social interaction; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; VF, verbal function; VIQ, verbal intelligence quotient.
People
Four studies examined gaze allocation to people within a social scene, two employing stimuli with single people (Frost‐Karlsson et al., 2019; Murias et al., 2018) and two studies using stimuli with two people engaged in a shared activity (Del Valle Rubido et al., 2018; Shic et al., 2011). Refer to Table 10 for a summary. Overall, a clear pattern of results was lacking, with findings largely non‐significant.
TABLE 10.
Summary of findings—People (N = 4)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Del Valle Rubido et al. (2018) | Fixation duration | Dynamic, social (activity monitoring) | Person | ADOS (Total) | 38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | Negative correlation |
| ABC (L/SW), ADOS (RSI, CSI) | ns | |||||||||||
| Frost‐Karlsson et al. (2019) |
Fixation duration |
Static, social/nonsocial | Person (social scenes only) | FTF (5–15), Social Competence domain | 23 ASD, 13 non‐ASD | ASD, non‐ASD |
Total 27 Males, 9 Females |
Total 16.45 years (1.65 years) |
Total IQ (WISC‐IV/WAIS‐IV): 90.6 (12.5) |
‐ |
Yes (non‐ASD) | ns |
| Fixation latency | Positive correlation | |||||||||||
| Murias et al. (2018) | Looking time | Dynamic, social (dyadic bid) |
Actor |
BASC‐2 (Social Skills); PDD‐BI (Expressive/Receptive Social Communication) | 23 | ASD | 19 Males, 4 Females | 53.6 months (13.5 months) | NVIQ: 64.7 (25.2) | ‐ | No |
Positive predictive relationship (controlling/not controlling for age, NVIQ) |
| PDD‐BI (Autism Composite); ADOS‐2 (Severity) |
ns (controlling/not controlling for age, NVIQ) |
|||||||||||
| Shic et al. (2011) | Looking time | Dynamic, social | People | ADOS‐G (Social Affect) | 28 | ASD (20 autistic disorder, 8 PDD‐NOS) | 22 Males, 6 Females | 20.7 months (3.0 months) | VDQ: 59.7 (28.5); NVDQ: 89.9 (17.3); VMA: 12.1 months (5.9 months); NVMA: 18.4 months (4.1 months). | ‐ | No | ns |
Abbreviations: ABC, Aberrant Behavior Checklist; ADOS, Autism Diagnostic Observation Schedule; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; ASD, autism spectrum disorder; BASC‐2, Behavior Assessment System for Children, Second Edition; CSI, communication and social interaction; FSIQ, full scale intelligence quotient; FTF (5–15), Five to Fifteen Questionnaire; L/SW, lethargy/social withdrawal; ns, not significant; NVA, nonverbal age; NVDQ, nonverbal developmental quotient; NVIQ, nonverbal intelligence quotient; NVMA, nonverbal mental age; PDD‐BI, Pervasive Developmental Disorder‐Behavior Inventory; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; RSI, reciprocal social interaction; VDQ, verbal developmental quotient; VIQ, verbal intelligence quotient; VMA, verbal mental age; WAIS‐IV, Wechsler Adult Intelligence Scale, Fourth Edition; WISC‐IV, Wechsler Intelligence Scale for Children, Fourth Edition.
Global scene/stimulus
Ten studies examined the distribution of gaze across the entirety of the presented social scene (refer to Table 11). Of these, six studies explored fixation duration or dwell time directed to the presented social scene. Results were mixed, with two indicating that a reduction in attending to a social scene was associated with increased social functioning difficulties (ADOS‐Generic Social Affect; Shic et al., 2011) and autism symptom severity (ADOS‐Generic Total; Chawarska et al., 2016), and three failing to identify significant relationships (Bast et al., 2021; Griffin & Scherf, 2020; Murias et al., 2018). Additionally, although Chawarska et al. (2012) found a negative correlation between attention to the scene and ADOS‐Generic Total score, ADOS‐Generic Total score was not a significant predictor of attention to the social scene when entered into a stepwise regression alongside verbal and nonverbal IQ.
TABLE 11.
Summary of findings—Global scene/stimulus (N = 10)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Avni et al. (2020) | Gaze similarity (distance from control group gaze) | Dynamic, social | Scene | ADOS‐2 (Total score, comparison score) | 71 | ASD | 59 Males, 12 Females | 5.1 years (1.8 years) | ‐ | ‐ | No |
Positive correlation |
| Gaze similarity (inter‐subject correlation) | Negative correlation | |||||||||||
| Gaze similarity (intra‐subject correlation) | Negative correlation | |||||||||||
| Bast et al. (2021) |
Fixation duration, fixations per second, saccade duration, saccade amplitude, peak saccade velocity, velocity main sequence (Mean, SD) |
Dynamic, social/nonsocial | Scenes | ADI‐R SA, ADOS CSS (Total, SA), SRS (parent, self‐report) | 142 | ASD | 105 Males, 37 Females | 16.23 years (5.77 years) | IQ: 102.17 (15.59) | ‐ | No | ns |
| Chawarska et al. (2012) | Looking time | Dynamic, social | Scene | ADOS‐G (Total score) | 54 | Autism | 85% Males | 21.6 months (2.9 months) |
VMA: 9.1 months (5.8 months) NVMA: 16.6 months (4.5 months) |
EL‐RL Split: 8.1 (23.4) | No |
Negative correlation ns (predictor) |
| Chawarska et al. (2016) |
Looking time |
Dynamic, social |
Scene on–off PC |
ADOS‐G (Total) | 90 | ASD | 84% Males | 20.5 months (3.77 months) | VDQ: 49 (26), NVDQ: 80 (17) | ‐ | No | Negative correlation |
| Cuve et al. (2021) | GTE, SGE, saccade amplitude | Dynamic, social | Scene | AQ28, emotion recognition | 25 ASD, 45 NT | ASD, NT |
ASD 13 Males, 11 Females NT 16 Males, 29 Females |
ASD 37.68 years (11.86 years) NT 26.13 years (6.66 years) |
ASD IQ: 121.68 (16.49) NT IQ: 117.76 (13.52) |
‐ | nr | ns |
| Griffin and Scherf (2020) | Fixation duration |
Dynamic, social (gaze following), static, social (gaze perception) |
Stimuli | ADOS‐2 (Total CSS), SRS‐2 (Total), SSIS‐p (Social Skills). | 35 | ASD | 29 Males, 6 Females | 13.5 years (2.7 years) | VIQ: 96.8 (17.7); PIQ: 102.4 (14.2); FSIQ: 100.1 (15.7) | ‐ | No | ns |
| Murias et al. (2018) | Looking time | Dynamic, social (dyadic bid) | Media | BASC‐2 (Social Skills); PDD‐BI (Expressive/Receptive Social Communication) | 23 | ASD | 19 Males, 4 Females | 53.6 months (13.5 months) | NVIQ: 64.7 (25.2) | ‐ | No |
ns (controlling for age and NVIQ, otherwise positive predictive relationship) |
| PDD‐BI (Autism Composite); ADOS‐2 (Severity) |
ns (controlling for age and NVIQ) |
|||||||||||
| Shic et al. (2011) | Looking time | Dynamic, social | Total | ADOS‐G (Social Affect) | 28 | ASD (20 autistic disorder, 8 PDD‐NOS) | 22 Males, 6 Females | 20.7 months (3.0 months) |
VDQ: 59.7 (28.5); NVDQ: 89.9 (17.3); VMA: 12.1 months (5.9 months); NVMA: 18.4 months (4.1 months). |
‐ | No | Negative correlation |
| Tenenbaum et al. (2021) | Gaze similarity (distance from typical scan path) | Dynamic, social (overall distance) | Scene | PDD‐BI (Expressive Social Communication Composite) |
155 full sample ASD 93 age‐matched ASD 40 NT |
ASD, NT |
Full sample ASD 122 Males, 33 Females Age‐matched ASD 72 Males, 21 Females NT 23 Males, 17 Females |
Full sample ASD 65.65 months (19.73 months) Age‐matched ASD 51.88 months (11.92 months) NT 49.95 months (10.51 months) |
Full sample ASD NVDQ: 76.47 (21.03) Age‐matched ASD NVDQ: 73.25 (19.99) NT NVDQ: 118.47 (16.02) |
‐ | Yes (NT) |
Negative correlation (controlling for age, NVDQ) |
| ABC‐C L/SW, ADI‐R RSI |
Positive correlation (controlling for age, NVDQ) |
|||||||||||
| ADOS‐2 CSS, PDD‐BI (Autism Composite) |
ns (controlling for age, NVDQ) |
|||||||||||
| Dynamic, social (dyadic bid) | ADOS‐2 CSS, ABC‐C L/SW |
Positive correlation (controlling for age, NVDQ) |
||||||||||
| PDD‐BI (Expressive Social Communication Composite) |
Negative correlation (controlling for age, NVDQ) |
|||||||||||
| ADI‐R RSI, PDD‐BI (Autism Composite) |
ns (controlling for age, NVDQ) |
|||||||||||
| Dynamic, social (joint attention) | ADOS‐2 CSS, ABC‐C L/SW, ADI‐R RSI |
Positive correlation (controlling for age, NVDQ) |
||||||||||
| PDD‐BI (Autism Composite/Expressive Social Communication Composite) |
ns (controlling for age, NVDQ) |
|||||||||||
| Dynamic, social (sandwich, moving toys) | ABC‐C L/SW |
Positive correlation (controlling for age, NVDQ) |
||||||||||
| ADOS‐2 CSS, ADI‐R RSI, PDD‐BI (Autism Composite/Expressive Social Communication Composite) |
ns (controlling for age, NVDQ) |
|||||||||||
| Wang et al. (2018) | Gaze similarity (typicality score: sandwich condition, dyadic bid condition) | Dynamic, social | Scene | ADOS (Social Affect) | 112 | ASD | 85.7% Males | 22.39 months (3.02 months) | VDQ: 55.84 (30.97), NVDQ: 82.70 (16.67) | ‐ | No | Negative correlation |
| Gaze similarity (typicality score: animated toys condition) | ns | |||||||||||
Abbreviations: ABC‐C, Aberrant Behavior Checklist‐Community; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; ASD, autism spectrum disorder; BASC‐2, Behavior Assessment System for Children, Second Edition; CSS, calibrated severity score; EL, expressive language; FSIQ, full scale intelligence quotient; GTE, gaze transition entropy; L/SW, lethargy/social withdrawal; nr, not reported; ns, not significant; NT, neurotypical; NVDQ, nonverbal developmental quotient; NVIQ, nonverbal intelligence quotient; NVMA, nonverbal mental age; PC, principal component; PDD‐BI, Pervasive Developmental Disorder‐Behavior Inventory; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; RL, receptive language; RSI, reciprocal social interaction; SA, social affect; SGE, stationary gaze entropy; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; SSIS‐p, Social Skills Improvement System, parent report; VDQ, verbal developmental quotient; VIQ, verbal intelligence quotient; VMA, verbal mental age.
Three studies compared gaze patterns between ASD and neurotypical participants when viewing movie scenes with social based activities and interactions (Avni et al., 2020; Tenenbaum et al., 2021; Wang et al., 2018). Each study found that ASD participants had significantly more idiosyncratic/variable gaze patterns and that these were associated with poorer social functioning (e.g., ADI‐R Reciprocal Social Interaction; Tenenbaum et al., 2021; ADOS Social Affect; Wang et al., 2018) and increased autism symptom severity (e.g., ADOS‐2 calibrated severity score; Tenenbaum et al., 2021; ADOS‐2 Total; Avni et al., 2020).
Cuve et al. (2021) investigated predictability of gaze allocation across presentations of dynamic emotional facial expressions. This was achieved via the investigation of indices of entropy, where reduced entropy reflected structured patterns of gaze behavior. No significant associations were identified between measures of entropy and autism traits (Autism Spectrum Quotient [AQ] 28) or emotion recognition performance.
Finally, Bast et al. (2021) explored how additional ocular motor features (fixations per second, saccade duration, saccade amplitude, peak saccade velocity, velocity main sequence) were associated with social functioning and autism symptom severity (ADI‐R Social Affect, ADOS Social Affect/Total calibrated severity scores, parent and self‐rated SRS scores) during the visual exploration of naturalistic (social and nonsocial) scenes in participants with ASD. No significant associations were identified.
Overall, although there is inconsistency as to whether attention to presented stimuli is associated with social functioning/autism symptom severity, recent literature suggests this may instead be driven by how gaze is distributed across the social scene.
Summary of biological interest areas
Overall, existing literature supports clear associations between the face, eyes, and mouth with social functioning/autism symptom severity in ASD. Although decreased gaze toward the face and eyes is associated with decreased social functioning/higher autism symptom severity, the relationship between gaze toward the mouth and social functioning/autism symptom severity is less clear and likely dependent on emotional content of a social scene and cognitive profile.
Nonbiological interest areas
Objects and nonbiological targets
A total of 22 studies explored the relationship between gaze toward objects and nonbiological targets and social functioning/autism symptom severity (refer to Table 12). Of these studies, 10 employed gaze cued, joint attention, and activity monitoring paradigms (Del Valle Rubido et al., 2018; Franchini et al., 2017; Fujioka et al., 2020; Griffin & Scherf, 2020; Kaliukhovich et al., 2020; Plesa‐Skwerer et al., 2019; Riby et al., 2013; Shic et al., 2011; Swanson & Siller, 2013; Thorup et al., 2017) and the general pattern of findings (seven out of these 10 studies) indicated significant associations between gaze measures and social functioning/autism symptom severity.
TABLE 12.
Summary of findings—Objects and non‐biological targets (N = 22)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Cole et al. (2017) | Fixation duration | Dynamic, social |
Poker chip (implicit mentalizing: mentalizing‐action, mentalizing‐either; explicit mentalizing: mentalizing vs. non‐mentalizing) |
Autism traits (principal components analysis of ADOS‐2, AQ, SRS, TASIT) | 17 ASD, 17 NT | ASD (14 Asperger's, 3 ASD), NT |
ASD 10 Males, 7 Females NT 10 Males, 7 Females |
ASD 23.71 years (9.24 years) NT 23.71 years (9.07 years) |
ASD WASI IQ: 120.12 (9.32) WASI Verbal: 62.88 (6.66) NT WASI IQ: 120.00 (10.09) WASI Verbal: 61.61 (7.52) |
‐ | Yes (NT) | ns |
| Del Valle Rubido et al. (2018) | Fixation duration | Dynamic, social (activity monitoring) |
Activity |
ADOS (Total) |
38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | Positive correlation |
| ABC (L/SW), ADOS (RSI, CSI) |
ns |
|||||||||||
| Franchini et al. (2017) | RJA | Dynamic, social | Face/hand to object | ESCS | 25 | ASD | 23 Males, 2 Females |
34.2 years (9.6 years) |
‐ | ‐ | No | Positive correlation |
| Fujioka et al. (2020) | Fixation duration | Dynamic/social (finger pointing) | Social target | SRS‐2 |
ASD 0–5 years 19 6–11 years 34 12–18 years 30 NT 0–5 years 120 6–11 years 150 12–18 years 37 |
ASD |
ASD 0–5 years 14 Males, 5 Females 6–11 years 28 Males, 6 Females 12–18 years 22 Males, 8 Females NT 0–5 years 58 Males, 62 Females 6–11 years 69 Males, 81 Females 12–18 years 14 Males, 23 Females |
ASD 0–5 years 4.7 years (0.9 years) 6–11 years 9.2 years (1.6 years) 12–18 years 14.5 years (1.6 years) NT 0–5 years 4.6 years (1.0 years) 6–11 years 8.7 years (1.7 years) 12–18 years 14.2 years (1.5 years) |
ASD IQ/DQ > 70 |
‐ | Yes (NT) |
ns (whole group, ASD only; controlling for age, sex) |
| Geometry |
Positive correlation (ASD group: 0–18 years) (controlling for age, sex) ns (whole groups; ASD group: 0–5 years, 6–11 years, 12–18 years) (controlling for age, sex) |
|||||||||||
| Gillespie‐Smith, Riby, et al. (2014) | Fixation duration, first fixation latency | Static social/nonsocial | Objects | CARS, SCQ | 21 | ASD | 20 Males, 1 Female | 13 years, 7 months (30 months) |
BPVS‐II VA: 74 (27) RCPM NVA: 27 (7) |
‐ | No | ns |
| Greene et al. (2020) | Fixation duration | Dynamic, social | Background objects | Hinting Task, ER‐40, SRS‐2 (caregiver/self rated) |
SCIT‐A 20 TAU 21 |
ASD |
SCIT‐A 15 Males, 5 Females TAU 19 Males, 2 Females |
SCIT‐A 17.25 years (3.58 years) TAU 17.90 years (4.1 years) |
SCIT‐A FSIQ: 95.85 (16.53) TAU FSIQ: 114.90 (12.83) |
‐ | No | ns |
| Hands and manipulated objects | ||||||||||||
| Griffin and Scherf (2020) | Fixation duration, task performance (% correct) | Dynamic, social (gaze following task) | Target object | ADOS (Total CSS) | 35 | ASD | 29 Males, 6 Females | 13.5 years (2.7 years) | VIQ: 96.8 (17.7); PIQ: 102.4 (14.2); FSIQ: 100.1 (15.7) | ‐ | No | Negative prediction |
| SRS‐2 (Total), SSIS‐p (Social Skills) | ns | |||||||||||
| Dynamic, social (gaze perception task) | ADOS (Total CSS), SRS‐2 (Total), SSIS‐p (Social Skills) | ns | ||||||||||
| Jones et al. (2008) | Fixation duration | Dynamic, social | Object | ADOS (Social Algorithm) | 15 | ASD | 11 Males, 4 Females | 2.28 years (0.58 years) | VF Age Equivalence (MSEL R/E): 1.17 years (0.66 years); NVF (MSEL VR): 1.77 years (0.47 years). | ‐ | No | ns |
| Kaliukhovich et al. (2020) | Looking time | Dynamic, social | Activity (mutual gaze) |
ABI (Symptom Scale) |
107 | ASD | 80 Males, 27 Females | 14.6 years (8.0 years) | KBIT‐2 IQ Composite: 98.4 (19.9) | ‐ | No |
Negative correlation (controlling for age, sex, IQ) |
| ABI (Social Communication), ABC (L/SW) ADOS‐2 (Social Affect, Total), SRS‐2 (Total) |
ns |
|||||||||||
| Activity (shared focus) | ABI (Symptom Scale, Social Communication), ABC (L/SW) ADOS‐2 (Social Affect, Total), SRS‐2 (Total) | 120 | ASD | 91 Males, 29 Females | 14.6 years (8.0 years) | KBIT‐2 IQ composite: 98.9 (19.9) | ‐ |
ns |
||||
| Klin et al. (2002) | Fixation duration | Dynamic, social | Object | ADOS (Social Algorithm) | 15 | Autism | 15 Males | 15.4 years (7.3 years) | VIQ: 101.3 (24.9) | ‐ | No |
Positive correlation |
| Muller et al. (2016) | Fixation duration | Dynamic, social | Object | MASC |
33 ASD, 23 NT |
ASD |
ASD 27 Males, 6 Females NT 14 Males, 9 Females |
ASD 15.6 years (1.9 years) NT 16.3 years (2.4 years) |
ASD GAI: 101.1 (14.4) NT GAI: 109.8 (15.1) |
‐ | Yes (NT) | ns |
| Murias et al. (2018) | Looking time | Dynamic, social (dyadic bid) | Toys | BASC‐2 (Social Skills); PDD‐BI (Expressive/Receptive Social Communication), PDD‐BI (Autism Composite); ADOS‐2 (Severity) | 23 | ASD | 19 Males, 4 Females | 53.6 months (13.5 months) | NVIQ: 64.7 (25.2) | ‐ | No | ns |
| Ohya et al. (2014) | Eye fixation points | Static, nonsocial | Entire stimulus (repeat comparison, no protrusions) | ASSQ (caregiver, teacher) | 23 | Asperger syndrome | 20 Males, 3 Females | 12.1 years (2.6 years) | ‐ | ‐ | No | Negative correlation |
| Entire stimulus (total) | ASSQ (caregiver) | Negative correlation | ||||||||||
| ASSQ (teacher) | ns | |||||||||||
| Total eye scanning length | Entire stimulus (total) | ASSQ (caregiver) | Negative correlation | |||||||||
| ASSQ (teacher) | ns | |||||||||||
| Responsive search score | Entire stimulus (repeat comparison, single/no protrusion, total) | ASSQ (caregiver, teacher) | ns | |||||||||
| Plesa‐Skwerer et al. (2019) | Looking time | Dynamic, social | Toy Spider, iPad, Panda (collapsed across episodes) |
ADI‐R (RSI), ADOS (overall CSS, SA) |
37 MV‐ASD; 34 V‐ASD | ASD |
MV‐ASD 29 Males, 8 Females V‐ASD 26 Males, 8 Females |
MV‐ASD 13.56 years (3.5 years); V‐ASD 14.97 years (3.4 years) |
MV‐ASD Leiter‐3: 62.14 (14.7) V‐ASD WASI‐PR: 104.15 (23.2) |
MV‐ASD RL: 26.88 (14.5), EL: 20.61 (10.8) V‐ASD RL: 102.58 (71.6), EL: 109.24 (81.3) |
No |
ns (controlling for NVIQ) |
| Spider (expected gaze), Panda (unexpected gaze) | ADI‐R (RSI), ADOS (overall CSS, SA) |
ns (controlling for NVIQ) |
||||||||||
| Hands/activity (collapsed across episodes) | ADI‐R (RSI), ADOS (overall CSS, SA) |
ns (controlling for NVIQ) |
||||||||||
| Riby et al. (2013) | Fixation duration | Static, social (spontaneous condition, cued condition) | Target item | CARS (Total score) | 22 | Autism | 18 Males, 4 Females | 11 years, 3 months (62 months) |
RCPM: 12 (3.7) |
‐ | No | ns |
| Rice et al. (2012) | Fixation duration | Dynamic, social | Object | ADOS (Severity) |
ASD (Additional) 72 ASD (Matched) 37 |
37.6% Autism, 12.8% Asperger Syndrome, 49.5% PDD‐NOS |
ASD (Additional) 53 Males, 19 Females ASD (Matched) 30 Males, 7 Females |
ASD (Additional) 10.2 years (3.5 years) ASD (Matched) 10.0 years (2.3 years) |
ASD (Additional) FSIQ: 88.7 (19.8), VIQ: 88.5 (19.7), NVIQ: 92.3 (19.4) ASD (Matched) FSIQ: 112.0 (15.2), VIQ: 111.4 (16.3), NVIQ: 111.4 (14.5) |
‐ | No |
Positive correlation (total ASD, N = 109; Even FSIQ group) ns (VIQ Split; NVIQ split, higher even FSIQ, lower even FSIQ, higher even FSIQ = lower even FSIQ) |
| Sasson et al. (2008) | Visual exploration | Static, social/nonsocial (object images) | Entire stimulus | SCQ (Social subscale) | 29 | ASD (17 autism, 8 Asperger syndrome, 4 PDD‐NOS) | 93% Male | 114.83 months (29.28 months) | 99.48 (16.56) | ‐ | No | Positive correlation |
| Shic et al. (2011) | Looking time | Dynamic, social | Activity | ADOS‐G (Social Affect) | 28 | ASD (20 autistic disorder, 8 PDD‐NOS) | 22 Males, 6 Females | 20.7 months (3.0 months) |
VDQ: 59.7 (28.5); NVDQ: 89.9 (17.3); VMA: 12.1 months (5.9 months); NVMA: 18.4 months (4.1 months). |
‐ | No | Negative correlation, negative prediction |
| Snow et al. (2011) | No. fixations | Static, social | Fan | Face Recognition Accuracy | 22 | ASD | 21 Males, 1 Female |
15.96 years (2.44 years) |
111.50 (17.57) | ‐ | No | Positive correlation |
| Swanson and Siller (2013) | Fixation duration | Dynamic, social | Target (congruent vs. incongruent) | SRS (Social Awareness) | 21 ASD, 24 NT | ASD, NT |
ASD 18 Males, 3 Females NT 20 Males, 4 Females |
ASD 87.24 months (18.39 months) NT 81.67 months (19.21 months) |
ASD NVMA: 84.67 months (20.28 months), NVDQ: 98.78 (19.08) NT NVMA: 87.29 months (25.15 months), NVDQ: 107.75 (22.18) |
ASD RL Standard (PPVT‐4): 97.81 (21.58); EL Standard (EOWPVT‐4): 98.43 (18.76). NT RL standard (PPVT‐4): 103.63 (9.15); EL standard (EOWPVT‐4): 99.63 (10.72) |
Yes (NT) | Significant SRS (social awareness) x condition interaction. Differences in gaze allocation between conditions when SRS < 66.05. |
| First fixation duration | ns | |||||||||||
| Thorup et al. (2017) | First fixation duration (AUF index) | Dynamic, social (high interest condition, baseline condition) | Attended versus unattended object | ADOS‐2 (Total), SRS | 16 ASD, 17 NT | ASD, NT |
ASD 12 Males, 4 Females NT 12 Males, 5 Females |
ASD 81.56 months (15.42 months) NT 74.12 months (15.51 months) |
ASD NVIQ: 105.23 (19.20) NT NVIQ: 115.76 (11.01) |
‐ | No | ns |
| Vivanti et al. (2014) | Fixation proportion | Dynamic, social | Target object | ADOS (Social Communication), SCQ | 24 | ASD | 21 Males, 3 Females | 46.54 months (10.55 months) | MSEL composite age equivalent score: 30.39 (12.15) |
MSEL RL age equivalent score: 26.75 (14.78) MSEL EL age equivalent score: 29.75 (35.22) |
No | ns |
Abbreviations: ABC, Aberrant Behavior Checklist; ABI, Autism Behavior Inventory; ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; AQ, Autism Spectrum Quotient; ASD, autism spectrum disorder; ASSQ, Autism Spectrum Screening Questionnaire; AUF‐Index, attended‐unattended fixation index; BASC‐2, Behavior Assessment System for Children, Second Edition; BPVS‐2, British Picture Vocabulary Scale, Second Edition; CARS, Childhood Autism Rating Scale; CSI, communication and social interaction; CSS, calibrated severity score; DQ, developmental quotient; EL, expressive language; EOWPVT‐4, Expressive One‐Word Picture Vocabulary Test, Fourth Edition; ESCS, Early Social Communication Scale; FSIQ, full scale intelligence quotient; GAI, general ability index; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; MASC, Movie for the Assessment of Social Cognition; MSEL R/E, Mullen Scales of Early Learning, receptive and expressive language subtests; MSEL VR, Mullen Scales of Early Learning, visual reception subtest; MSEL, Mullen Scales of Early Learning, expressive language; MSEL, Mullen Scales of Early Learning, receptive language; MV‐ASD, minimally verbal children and adolescents with autism spectrum disorder; ns, not significant; NT, neurotypical; NVDQ, nonverbal developmental quotient; NVIQ, nonverbal intelligence quotient; NVMA, nonverbal mental age; PDD‐BI, Pervasive Developmental Disorder‐Behavior Inventory; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; PPVT‐4, Peabody Picture Vocabulary Test, Fourth Edition; RCPM, Raven's Colored Progressive Matrices; RJA, responding to joint attention; RL, receptive language; RSI, reciprocal social interaction; SCQ, Social Communication Questionnaire; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; SSIS‐p, Social Skills Improvement System, parent report; TASIT, The Awareness of Social Inference Test; V‐ASD, verbally fluent children and adolescents with autism spectrum disorder; VDQ, verbal developmental quotient; VF, verbal function; VIQ, verbal intelligence quotient; WASI, Wechsler Abbreviated Scale of Intelligence; WASI‐PR, Wechsler Abbreviated Scale of Intelligence, perceptual reasoning scale.
Of particular interest was the finding of Rice et al. (2012), who found that the relationship between fixation duration to objects and social functioning was modulated by cognitive functioning. Specifically, increased fixation duration to objects was related to higher ADOS severity scores only in participants with a higher even full scale IQ profile (i.e., verbal IQ = nonverbal IQ, full scale IQ ≥ 98), with the relationship becoming nonsignificant in remaining cognitive profiles (i.e., verbal IQ = nonverbal IQ and full scale IQ < 98, verbal IQ > nonverbal IQ, nonverbal IQ > verbal IQ).
Background
Three studies examined fixation duration to background regions within social scenes in participants with ASD (refer to Table 13). Shic et al. (2011) found that increased fixation duration to the background region of a scene depicting an interaction between an adult and child was related to greater issues with social affect (ADOS‐Generic, Social Affect subscale). Contrastingly, two studies failed to identify significant relationships between gaze and fixation duration to the background of social scenes with social functioning and autism symptom severity (Del Valle Rubido et al., 2018; Kaliukhovich et al., 2020).
TABLE 13.
Summary of findings—Background (N = 3)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Del Valle Rubido et al. (2018) | Fixation duration | Dynamic, social (complex social movies) | Background | ADOS (Total, RSI, CSI); ABC (L/SW) | 38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | ns |
| Kaliukhovich et al. (2020) | Looking time | Dynamic, social | Background (mutual) | ABI (Symptom Scale, Social Communication), ABC (L/SW), ADOS‐2 (Social Affect, Total), SRS‐2 (Total) | 107 | ASD | 80 Males, 27 Females | 14.6 years (8.0 years) | KBIT‐2 IQ composite: 98.4 (19.9) | ‐ | No |
ns (controlling for age, sex, IQ). |
| Background (shared focus) | 120 | ASD | 91 Males, 29 Females | 14.6 years (8.0 years) | KBIT‐2 IQ composite: 98.9 (19.9) | |||||||
| Shic et al. (2011) | Looking time | Dynamic, social | Background | ADOS‐G (Social Affect) | 28 | ASD (20 autistic disorder, 8 PDD‐NOS) | 22 Males, 6 Females | 20.7 months (3.0 months) | VDQ: 59.7 (28.5); NVDQ: 89.9 (17.3); VMA: 12.1 months (5.9 months); NVMA: 18.4 months (4.1 months). | ‐ | No | Positive correlation |
Abbreviations: ABC, Aberrant Behavior Checklist; ABI, Autism Behavior Inventory; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; ASD, autism spectrum disorder; CSI, communication and social interaction; ER‐40, Penn Emotion Recognition task; FSIQ, full scale intelligence quotient; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; ns, not significant; NT, neurotypical; NVDQ, nonverbal developmental quotient; NVMA, nonverbal mental age; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; RSI, reciprocal social interaction; SCIT‐A, Social Cognition and Interaction Training for Autism; SRS‐2, Social Responsiveness Scale, Second Edition; TAU, treatment as usual; VDQ, verbal developmental quotient; VIQ, verbal intelligence quotient; VMA, verbal mental age.
Multiple interest areas
Face versus non‐face region
Four studies investigated the distribution of gaze between broader face and non‐face regions, returning mixed results in participants with ASD (refer to Table 14). Bird et al. (2011) explored the dispersion of gaze across face and non‐face stimuli while participants viewed four video clips. Greater preference for the face compared with non‐face regions was associated with decreased autism symptom severity (ADOS symptom severity). As part of their examination of the influence of low‐level visual features on driving visual attention across a social scene, Amso et al. (2014) found a relationship, controlling for age and average fixation counts, between decreases in looking at the primary face area of interest and more toward secondary areas of interest with increased Social Affect severity on the ADOS.
TABLE 14.
Summary of findings—Face versus non‐face region comparisons (N = 4)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Amso et al. (2014) | Gaze allocation | Static, social (congruent only) | Face versus non‐face regions | ADOS (Social Affect) | 15 |
ASD (14 AD, 1 PDD‐NOS) |
9 Males, 6 Females | 3.53 years (1.06 years) | IQ: 68.8 (12) |
PLS‐IV EL: 18.87 (10.77) PLS‐IV RL: 17.33 (12.60) |
No |
Negative correlation(controlling for age, average fixation counts in the 1 second interval) |
| Bird et al. (2011) | Fixation duration | Dynamic, social | Face:non‐face | ADOS (Symptom Severity) | 13 | 2 ASD, 9 AS, 1 autism, 1 atypical autism | 10 Males, 3 Females | 40.5 years (14.5 years) | FSIQ: 115 (14) | ‐ | No |
Negative correlation Significant prediction (stepwise regression, TAS score initial predictor) |
| Chawarska et al. (2016) |
Looking time |
Dynamic, social |
Face‐toys, activity‐face PC |
ADOS‐G (Total) | 90 | ASD | 84% Males | 20.5 months (3.77 months) | VDQ: 49 (26), NVDQ: 80 (17) | ‐ | No | ns |
| Greene et al. (2020) | Fixation duration | Dynamic, social | Social prioritization (face‐background) | Hinting Task, ER‐40, SRS‐2 (caregiver/self) |
SCIT‐A 20 TAU 21 |
ASD |
SCIT‐A 15 Males, 5 Females TAU 19 Males, 2 Females |
SCIT‐A 17.25 years (3.58 years) TAU 17.90 years (4.1 years) |
SCIT‐A FSIQ: 95.85 (16.53) TAU FSIQ: 114.90 (12.83) |
‐ | No | ns |
Abbreviations: AD, autistic disorder; ADOS, Autism Diagnostic Observation Schedule; AS, Asperger's syndrome; EL, expressive language; ER‐40, Penn Emotion Recognition Task; FSIQ, full scale intelligence quotient; IQ, intelligence quotient; NVDQ, nonverbal developmental quotient; PC, principal component; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PLS‐IV, Preschool Language Scales, Fourth Edition; RL, receptive language; SRS‐2, Social Responsiveness Scale, Second Edition; TAS, Toronto Alexithymia Scale; TAU, treatment as usual; VDQ, verbal developmental quotient.
Contrastingly, two studies failed to identify relationships in participants with ASD. Chawarska et al. (2016) examined the distribution of gaze across a short video of an actress surrounded by four toys and sandwich ingredients. Differences in the allocation of gaze between the face versus activity and in the face versus toys was not related to autism symptom severity (ADOS‐Generic Total). Greene et al. (2020) explored the utility of a social skills intervention, using performance on an eyetracking task (involving joint and parallel play) as a measure of treatment response. Social prioritization at baseline (the difference in fixation duration to social [faces] and object [background] ROIs) was not associated with social cognition and functioning (Hinting Task, Penn Emotion Recognition Task, SRS‐2).
Eyes versus mouth region
Six studies compared the allocation of gaze between the eye and mouth regions in participants with ASD, with mixed findings (refer to Table 15). Three of these identified significant results. Gillespie‐Smith, Doherty‐Sneddon, et al. (2014) found that longer fixation to the eyes compared with the mouth was associated with increased social functioning (SCQ) when viewing head and shoulder photographs of unfamiliar and self‐faces, but not for familiar faces. Kliemann et al. (2010) used an eye preference index, representing fixation changes upward from the mouth, and downward from the eyes of static facial images depicting different emotions. Greater preference for the eye region was related to improved social functioning (ADI‐R Social), higher emotion recognition performance (emotion classification task), but unrelated to global autism symptomatology (ADI‐R Total). Contrastingly, Chawarska and Shic (2009) found that increased gaze duration to the eyes was associated with poorer facial recognition performance (Visual Paired Comparison paradigm; Fantz, 1964), reflective of the limited scanning required to fully encode a face for later recognition.
TABLE 15.
Summary of findings—Eyes versus mouth comparisons (N = 6)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Bird et al. (2011) | Fixation duration | Dynamic, social | Eyes:mouth | ADOS (Symptom Severity) | 13 |
2 ASD, 9 AS, 1 autism, 1 atypical autism |
10 Males, 3 Females | 40.5 years (14.5 years) | FSIQ: 115 (14) | ‐ | No | ns |
| Bradshaw et al. (2019) | Fixation duration | Static, social | Eyes:mouth | ADOS CSS (Total) | 28 | ASD | 24 Males, 4 Females | 34.21 months (9.28 months) | ‐ |
PLS‐5 Total: 74.11 (18.9) |
No | ns |
| Chawarska and Shic (2009) | Looking time (familiar, novel preference), fixation duration (novelty preference ratio) | Static, social | Eye:mouth |
VPC (novelty preference ratio) |
14 Age Group 1, 30 Age Group 2 | 27 Autism, 17 PDD‐NOS | 84% Males |
Age Group 1 26.9 months (6.2 months) Age Group 2 46.4 months (6.4 months) |
Age Group 1 VDQ: 61 (37), NVDQ: 85 (24) Age Group 2 VDQ: 66 (36), NVDQ: 76 (25) |
‐ | No |
Negative correlation (controlling for CA, VDQ, NVDQ) |
| VPC (familiar preference, novel preference) |
ns (controlling for CA, VDQ, NVDQ) |
|||||||||||
| Chawarska et al. (2016) |
Looking time |
Dynamic, social | Mouth‐eyes PC | ADOS‐G (Total) | 90 | ASD | 84% male | 20.5 months (3.77 months) |
VDQ: 49 (26), NVDQ: 80 (17) |
‐ | No | ns |
| Gillespie‐Smith, Doherty‐Sneddon, et al. (2014) | Fixation duration | Static, social (familiar face) | Eyes versus mouth | SCQ | 21 | ASD | 20 Males, 1 Female | 13 years, 7 months (30 months) |
BPVS‐II VA: 74 (27) RCPM NVA: 27 (7) |
‐ | No | ns |
| Static, social (unfamiliar face); static, social (self‐face) | Negative correlation | |||||||||||
| Kliemann et al. (2010) | Fixation change | Static, social | Eye preference index (eyes vs. mouth) | Emotion classification task | 12 | ASD | 8 Males, 4 Females | 35.40 years (8.10 years) | MWT‐IQ: 102.6 (14.3) | ‐ | No | Positive correlation, positive predictive relationship |
| ADI‐R (Social score) | Negative correlation | |||||||||||
| ADI‐R (Total score) | ns | |||||||||||
Abbreviations: ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; AS, Asperger's syndrome; ASD, autism spectrum disorder; BPVS‐2, British Picture Vocabulary Scale, Second Edition; CA, chronological age; CSS, calibrated severity score; FSIQ, full scale intelligence quotient; MWT‐IQ, Multiple Choice Vocabulary Test‐Intelligence Quotient; ns, not significant; NVA, nonverbal age; NVDQ, nonverbal developmental quotient; PC, principal component; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PLS‐5, Preschool Language Scales, Fifth Edition; RCPM, Raven's Colored Progressive Matrices; SCQ, Social Communication Questionnaire; VA, verbal age; VDQ, verbal developmental quotient; VPC, Visual Paired Comparison paradigm.
Three studies, however, failed to find a relationship between the ratio of eye to mouth fixation duration with autism symptom severity using dynamic social stimuli (Bird et al., 2011) and static facial images (Bradshaw et al., 2019; Chawarska et al., 2016). Overall, findings suggest that gaze allocation across the eye and mouth regions is associated with social functioning specifically, rather than broader autism symptom severity.
Combined social and nonsocial regions
A total of 18 studies explored the distribution of gaze across combinations of social and nonsocial regions of interest (refer to Table 16). Of particular interest are the 11 studies that used variations of the preferential looking task initially developed by Pierce et al. (2011), involving the dual presentation of dynamic or static social and geometric images, with participants instructed to view the display naturally. There is evidence to suggest that a preference for viewing social stimuli is associated with higher social functioning ability (e.g., Fujioka et al., 2020; Kou et al., 2019; Moore et al., 2018; Pierce et al., 2016). Moreover, Franchini et al. (2016) found that fixation duration to biological motion in toddlers with ASD predicted improvement in autism symptom severity 1 year later (ADOS‐Generic severity score).
TABLE 16.
Summary of findings—Dual social and nonsocial stimuli (N = 18)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Bacon et al. (2020) | Looking time (young age, M = 23 months) | Dynamic, social/nonsocial | Geometric stimuli |
ADOS‐2 (Total score, school age) |
ASD (persistent) 45 ASD (previous) 4 |
ASD |
ASD (persistent) 36 Males, 9 Females ASD (previous) 3 Males, 1 Females |
ASD (persistent) 8.1 years (1.6 years) ASD (previous) 8.0 years (0.8 years) |
ASD (persistent) WISC‐V VC: 87.4 (25.1) VS: 92.4 (24.0) FSIQ: 83.8 (24.7) ASD (previous) WISC‐V VC: 101.0 (11.8) VS: 109.0 (14.6) FSIQ: 101.0 (15.0) |
‐ | No |
Positive correlation (persistent, persistent + previous) Positive prediction (persistent only) |
| SRS‐2 (parent rated, school age) |
ns (persistent only) |
|||||||||||
| Bradshaw et al. (2019) | Fixation duration | Dynamic, social/nonsocial | Social preference | ADOS CSS (Total) | 28 | ASD | 24 Males, 4 Females |
34.21 months (9.28 months) |
‐ |
PLS‐5 Total: 74.11 (18.9) |
No | ns |
| Campbell et al. (2014) | Looking time | Dynamic, social | Scene, face, toys, eyes, mouth, eyes versus mouth ratio | ADOS (module 1 total) |
Visit 1 65 Visit 2 48 |
Visit 1 50 Autism, 15 PDD‐NOS Visit 2 unknown |
80% Males |
Visit 1 21.4 months (2.9 months) Visit 2 36.2 months (4.2 months) |
Visit 1 Mullen VDQ: 48 (25), Mullen NVDQ: 81 (17) Visit 2 Mullen VDQ: 78 (36), Mullen NVDQ: 80 (22) |
‐ | No |
Cluster 1 > Cluster 2, 3 Cluster 2 = 3 |
| Chawarska and Shic (2009) | Looking time (familiar, novel preference), fixation duration (novelty preference ratio) | Static, social |
Non‐face |
VPC (familiar preference, novel preference) |
14 Age Group 1, 30 Age Group 2 | 27 Autism, 17 PDD‐NOS | 84% Males |
Age Group 1 26.9 months (6.2 months) Age Group 2 46.4 months (6.4 months) |
Age Group 1 VDQ: 61 (37), NVDQ: 85 (24) Age Group 2 VDQ: 66 (36), NVDQ: 76 (25) |
‐ | No | Positive correlation (controlling for CA, VDQ, NVDQ) |
| Chawarska et al. (2016) |
Looking time |
Dynamic, social | Toy‐person PC | ADOS‐G (Total) | 90 | ASD | 84% Male | 20.5 months (3.77 months) | VDQ: 49 (26), NVDQ: 80 (17) | ‐ | No | ns |
| Del Valle Rubido et al. (2018) | Fixation duration | Dynamic, social/nonsocial (human activity preference) | Human preference |
ADOS (Total, RSI, CSI), ABC (L/SW) |
38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No |
ns |
| Franchini et al. (2016) | Fixation duration | Dynamic, social/nonsocial | Biological motion preference | Time 1 ADOS‐G (Severity score) | 20 | ASD | 20 Males |
Time 1 35.00 months (9.47 months) Time 2 47.13 months (9.54 months) |
‐ |
‐ | No | ns |
| Time 1 to 2 ADOS‐G (Severity score) change | Significant prediction (positive) | |||||||||||
| Social responders (biological motion bias) versus geometric responders (geometric motion bias) | Time 1 ADOS‐G (Severity score) | ns | ||||||||||
|
Time 1 to 2
ADOS‐G (Severity score) change |
SR‐ASD > GR‐ASD | |||||||||||
| Frazier et al. (2016) | ARI | Dynamic/static, social/nonsocial | Social versus nonsocial | ADOS‐2 (Total severity) |
Initial Study 25 ASD, 20 NT Replication Study 15 ASD, 19 NT |
ASD |
Initial Study ASD (20 Males, 5 Females), NT (17 Males, 3 Females) Replication study ASD (11 Males, 4 Females), NT (15 Males, 4 Females) |
Initial Study ASD: 5.4 years (1.8 years), NT: 5.9 years (1.4 years) Replication study ASD: 4.9 years (1.6 years), NT: 5.8 years (1.3 years) |
‐ |
MSEL Total Initial Study ASD: 81.6 (21.1), NT: 101.3 (20.8) Replication study ASD: 81.9 (25.1), NT: 86.3 (20.6) |
Yes (NT) |
Positive correlation (initial + replication studies, ASD+ neurotypical sample, controlling for RL and CBCL) |
| ADOS‐2 (SA) |
Positive correlation (initial + replication studies) |
|||||||||||
| SRS‐2 (total T‐score) |
ns (initial + replication studies) |
|||||||||||
| Frazier et al. (2018) | ARI | Dynamic/static, social/nonsocial | Social versus nonsocial |
ADOS‐2 (Total severity); SRS‐2 (total T‐score) |
91 ASD, 110 NT | ASD, NT |
ASD 75 Males, 16 Females NT 86 Males, 24 Females |
ASD 5.7 years (3.6 years) NT 6.8 years (3.3 years) |
‐ |
MSEL, CELF‐IV, or PLS‐5 (N = 172) ASD 74.4 (23.5) NT 87.9 (23.8) |
No |
Positive correlation (also when controlling for RL, CBCL total problems in ADOS total severity) ns (controlling for nonverbal ability) |
| Fujioka et al. (2016) | Fixation duration | Dynamic, social/nonsocial | Same size (people and geometry), small window (geometry only) | SRS | 21 | ASD | 21 Males | 27.6 years (7.7 years) |
FSIQ: 99.8 (13.5) VIQ: 103.3 (13.3) PIQ: 96.4 (16.0) Note, N = 20 |
‐ | No | ns |
| Fujioka et al. (2020) | Fixation duration | Dynamic/social (the preference paradigm) | People | SRS‐2 |
ASD 0–5 years 19 6–11 years 34 12–18 years 30 NT 0–5 years 120 6–11 years 150 12–18 years 37 |
ASD |
ASD 0–5 years 14 Males, 5 Females 6–11 years 28 Males, 6 Females 12–18 years 22 Males, 8 Females NT 0–5 years 58 Males, 62 Females 6–11 years 69 Males, 81 Females 12–18 years 14 Males, 23 Females |
ASD 0–5 years 4.7 years (0.9 years) 6–11 years 9.2 years (1.6 years) 12–18 years 14.5 years (1.6 years) NT 0–5 years 4.6 years (1.0 years) 6–11 years 8.7 years (1.7 years) 12–18 years 14.2 years (1.5 years) |
ASD IQ/DQ > 70 |
‐ | Yes (NT) |
Negative correlation (whole group: 6–11 years) (controlling for age, sex) ns (whole group: 0–18, 0–5 years, 12–18 years; ASD groups) (controlling for age, sex) |
| Geometry |
ns (whole group, ASD only groups) (controlling for age, sex) |
|||||||||||
|
Groen et al. (2012) |
Looking time | Dynamic, social |
Combined ROIs (faces, window)—Relative time |
ADOS (RSI) | 23 | ASD | 16 Males, 7 Females | 3.1 years | ‐ | ‐ | No |
Negative correlation |
| Kou et al. (2019) | Fixation duration | Dynamic, social/nonsocial (task 1) | Dynamic social image | ADOS‐2 (SA) | 32 | ASD | 26 Males, 6 Females | 3.72 years (1.25 years) | ‐ | ‐ | No | Negative correlation |
| ADOS‐2 (Total) | ns | |||||||||||
| Static, social/nonsocial (task 3) | Boy with toy (1), boy's face, toy alone (1), toy alone (2) | ADOS‐2 (SA, Total) |
ns |
|||||||||
| Fixation counts (proportion) | Dynamic, social/nonsocial (task 1) | Dynamic social image | ADOS‐2 (SA) | Negative correlation | ||||||||
| ADOS‐2 (Total) | ns | |||||||||||
| Static, social/nonsocial (task 3) |
Boy with toy (1), boy's face, toy alone (1), toy alone (2) |
ADOS‐2 (SA, Total) |
ns |
|||||||||
| Moore et al. (2018) | Fixation duration | Dynamic, social/nonsocial | People versus geometry | ADOS (SA, Total) | Total: 76 (14 GeoPref subtype, 17 SocPref subtype) | ASD |
ASD Total 70 Males, 6 Females ASD GeoPref 13 Males, 1 Female ASD SocPref 15 Male, 2 Females |
ASD Total 30.0 months (8.8 months) ASD GeoPref 31.2 months (9.2 months) ASD SocPref 28.7 months (7.2 months) |
‐ |
ASD Total MSEL EL: 0.60 (0.26), MSEL RL: 0.58 (0.28) ASD GeoPref MSEL EL: 0.53 (0.26), MSEL RL: 0.46 (0.25) ASD SocPref MSEL EL: 0.67 (0.30), MSEL RL: 0.68 (0.26) |
No | ASD GeoPref > ASD SocPref |
| Geometry | ADOS (Total) |
Positive correlation (full sample) |
||||||||||
| Pierce et al. (2011) | Fixation duration | Dynamic, social/nonsocial | People versus geometry | ADOS (SA, Overall) | 37 | ASD | 30 Males, 7 Females | 26.7 months (7.7 months) |
MSEL VDQ: 63.5 (21.4), MSEL NVDQ: 78.4 (21.6) |
‐ | No | ns |
| Pierce et al. (2016) | Fixation duration | Dynamic, social/nonsocial | DGI | ADOS (SA/CoSo, Total score). | 115 | ASD | 88 Males, 27 Females | 28 months (8.4 months) | ‐ | MSEL (t‐scores) EL: 32.0 (13.0), RL: 32.3 (13.2) | No |
Positive prediction (controlling for age) |
| People versus geometry | DGI preference > DSI preference | |||||||||||
| Shaffer et al. (2017) | Fixation duration | Dynamic, social/nonsocial | SSPR | SCQ | 37 ASD, 26 NT | ASD, NT |
ASD 30 Males, 7 Females NT 14 Males, 12 Females |
ASD 9.5 years (3.3 years) NT 10.6 years (3.0 years) |
ASD 69.7 (20.3) NT ‐ |
‐ | Yes (NT) | Negative correlation |
| ABC (Lethargy); SRS (Social Awareness/Social Cognition/Social Communication, Autistic Mannerisms, total T‐Score) | ns | |||||||||||
| Unruh et al. (2016) | Preference | Static, social/nonsocial (social + high object interest) | Social, object | ADOS (Social and Communication, Total severity), SRS (Total) | 33 ASD, 31 NT | ASD |
ASD 29 Males, 4 Females NT 28 Males, 3 Females |
ASD 167.4 months (36.0 months) NT 165.8 months (32.4 months) |
ASD VIQ: 98.9 (21.3), NVIQ: 105.5 (16.7) NT VIQ: 112.5 (12.9), NVIQ: 111.4 (12.6) |
‐ | No | ns |
| Detail orientation, fixation duration, prioritization | Social | |||||||||||
Abbreviations: ABC, Aberrant Behavior Checklist; ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ADOS‐G, Autism Diagnostic Observation Schedule, Generic; ARI, autism risk index; ASD, autism spectrum disorder; CA, chronological age; CBCL, Child Behavior Checklist; CELF‐IV, Clinical Evaluation of Language Fundamentals, Fourth Edition; Co/So, communication social; CSI, communication and social interaction; CSS, calibrated severity score; DGI, dynamic geometric images; DQ, developmental quotient; DSI, dynamic social images; EL, expressive language; FSIQ, full scale intelligence quotient; GeoPref, geometric preference; GR‐ASD, geometric responders with autism spectrum disorder; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; MSEL, Mullen Scales of Early Learning; ns, not significant; NT, neurotypical; NVDQ, nonverbal developmental quotient; PC, principal component; PDD‐NOS, pervasive developmental disorder, not otherwise specified; PIQ, performance intelligence quotient; PLS‐5, Preschool Language Scales, Fifth Edition; RL, receptive language; ROI, region of interest; RSI, reciprocal social interaction; SA, social affect; SCQ, Social Communication Questionnaire; SocPref, social preference; SR‐ASD, social responders with autism spectrum disorder; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; SSPR, social interaction scene preference ratio; VC, verbal comprehension; VDQ, verbal developmental quotient; VIQ, verbal intelligence quotient; VPC, Visual Paired Comparison paradigm; VS, visual spatial; WISC‐V, Wechsler Intelligence Scale for Children, Fifth Edition.
Biological motion displays
Four studies examined gaze to point light displays of biological motion, with mixed findings (refer to Table 17). Del Valle Rubido et al. (2018) employed a biological motion task in participants with ASD, involving the simultaneous presentation of two dynamic point light displays—one depicting a human engaging in activities (e.g., walking, waving), and the other a series of moving dots. Preference for biological motion was negatively associated with the Aberrant Behavior Checklist Lethargy/Social Withdrawal subscale, but no relationships were identified for the ADOS social domains or total score. Fujioka et al. (2020) found that results differed depending on age, where increased fixation duration to inverted biological motion was associated with improved social functioning (SRS‐2) across ASD and neurotypical participants in the 0–18 year and 6–11 year age groups. No significant relationships were identified for upright biological motion.
TABLE 17.
Summary of findings—Biological motion displays (N = 4)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Del Valle Rubido et al. (2018) | Preference (fixation duration) | Dynamic, social/nonsocial (biomotion) | Biological motion |
ABC (L/SW) |
38 | ASD | 38 Males | 24.2 years (5.8 years) | FSIQ: 101.1 (14.3), VIQ: 100.5 (16.1), PIQ: 100.6 (12.7) | ‐ | No | Negative correlation |
| ADOS (RSI, CSI, Total) | ns | |||||||||||
| Fujioka et al. (2016) | Fixation duration | Dynamic, social (biological motion) | Upright, inverted | SRS | 21 | ASD | 21 Males | 27.6 years (7.7 years) |
FSIQ: 99.8 (13.5) VIQ: 103.3 (13.3) PIQ: 96.4 (16.0) Note, N = 20 |
‐ | No | ns |
| Fujioka et al. (2020) | Fixation duration | Dynamic, social (biological motion) | Upright | SRS‐2 |
ASD 0–5 years 19 6–11 years 34 12–18 years 30 NT 0–5 years 120 6–11 years 150 12–18 years 37 |
ASD |
ASD 0–5 years 14 Males, 5 Females 6–11 years 28 Males, 6 Females 12–18 years 22 Males, 8 Females NT 0–5 years 58 Males, 62 Females 6–11 years 69 Males, 81 Females 12–18 years 14 Males, 23 Females |
ASD 0–5 years 4.7 years (0.9 years) 6–11 years 9.2 years (1.6 years) 12–18 years 14.5 years (1.6 years) NT 0–5 years 4.6 years (1.0 years) 6–11 years 8.7 years (1.7 years) 12–18 years 14.2 years (1.5 years) |
ASD IQ/DQ > 70 |
‐ | Yes (NT) |
ns (controlling for age, sex) |
| Inverted |
Negative correlation (whole group: 0–18 years and 6–11 years) (controlling for age, sex) ns (whole group: 0–5 years, 12–18 years), ASD group (0–18 years, 0–5 years, 6–11 years, 12–18 years) (controlling for age, sex) |
|||||||||||
| Kou et al. (2019) | Fixation duration, fixation counts | Dynamic, social/nonsocial (task 2) | Human, Cat | ADOS‐2 (SA, Total) | 32 | ASD | 26 Males, 6 Females | 3.72 years (1.25 years) | ‐ | ‐ | No | ns |
Note: ABC, Aberrant Behavior Checklist; ADOS, Autism Diagnostic Observation Schedule; ASD, autism spectrum disorder; CSI, communication and social interaction; DQ, developmental quotient; FSIQ, full scale intelligence quotient; IQ, intelligence quotient; L/SW, lethargy/social withdrawal; ns, not significant; NT, neurotypical; PIQ, performance intelligence quotient; RSI, reciprocal social interaction; SA, social affect; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; VIQ, verbal intelligence quotient.
Two failed to identify significant relationships with social functioning or autism symptom severity. Fujioka et al. (2016) examined fixation duration to both upright and inverted representations of human biological motion, neither of which was related to social functioning (SRS). Kou et al. (2019) explored fixation counts and duration to animate (human, cat) and inanimate (random dots) point light displays. No significant relationships were identified with ADOS‐2 Total and Social domain scores.
Visual search
Five studies examined visual search paradigms, although tasks and measures of visual processing varied (refer to Table 18). Three studies employed visual search paradigms where participants were required to identify a target stimulus presented among distractor stimuli. In a sample of participants with ASD, Keehn and Joseph (2016) found a greater number of initial leftward saccades was associated with improved social functioning, while a greater number of initial rightward saccades was associated with reduced social functioning. Joseph et al. (2009) explored the factors underpinning superior visual search performance in ASD across static/dynamic and target absent/present arrays of a target presented among distractor letters. Although search slope (an indicator of search efficiency reflective of attentional shifting between array items and the ability to filter irrelevant items) was not associated with social functioning (ADOS Social domain), the intercept (reaction time if the visual search component was removed from the task) in the static/target present condition was negatively associated with the ADOS Social domain score. Participants in Glennon et al. (2020) were required to identify a red apple embedded within an array of blue apple and red rectangle distractor targets. Although faster target detection was identified in children (both ASD and Down syndrome) with higher scores on the SRS‐2, search latency did not predict SRS‐2 scores in children with ASD.
TABLE 18.
Summary of findings—Visual search (N = 5)
| Reference | Visual processing index | Visual stimuli | Interest area | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | |||||||
| Bavin et al. (2014) | Looking time | Static, social/nonsocial | Target item (800–1000, 1000–1200,1200–1400 intervals) | SCQ (parent report) |
ASD (Moderate) 21 ASD (Severe) 16 NT 48 |
ASD (100% HFA), NT |
ASD (Moderate) 17 Males, 4 Females ASD (Severe) 14 Males, 2 Females NT 36 Males, 12 Females |
ASD (Moderate) 6.35 years (0.77 years) ASD (Severe) 6.48 years (0.67 years) NT 6.33 years (0.72 years) |
ASD (Moderate) FSIQ: 96.06 (11.18) ASD (Severe) FSIQ: 99.00 (11.05) NT FSIQ: 99.87 (10.28) |
CELF‐IV ASD (Moderate) Total: 99.50 (16.54) ASD (Severe) Total: 91.13 (18.68) NT Total: 103.79 (11.77) |
Yes (NT) | Negative association (adjusting for RL, EL, VIQ, NVIQ, and attention) |
| Glennon et al. (2020) | Target detection latency | Static, nonsocial | Target object | SRS‐2 | 16 iASD, 7 DS + ASD, 8 DS‐ASD | iASD |
iASD 16 Males DS ± ASD 4 Males, 3 Females DS‐ASD 4 Males, 4 Females |
iASD 8.5 years (1.6 years) DS ± ASD 8.7 years (1.8 years) DS‐ASD 9.1 years (2.2 years) |
Leiter‐3 iASD 56 (22) DS ± ASD 30 (18) DS‐ASD 49 (15) |
‐ | Yes (iASD, DS + ASD, DS‐ASD) |
Main effect of search latency (higher SRS‐2 scores associated with faster target detection) |
| iASD only |
ns (regression model with facilitation in gap‐overlap task) |
|||||||||||
| Joseph et al. (2009) | Search slope | Static, nonsocial; dynamic, nonsocial |
Target (present), Target (absent) |
ADOS (Social) | 21 | ASD | 17 Males, 4 Females | 14 years, 7 months (2 years, 8 months) | VIQ: 99 (19); NVIQ: 107 (10) | ‐ | No | ns |
| Search intercept | Static, nonsocial |
Target (present) |
Negative correlation (controlling for age, VIQ, NVIQ, independently) |
|||||||||
| Target (absent) | ns | |||||||||||
| Dynamic, nonsocial |
Target (present), target (absent) |
ns | ||||||||||
| Keehn and Joseph (2016) | Left versus right difference score (saccade, absent saccade) | Static, nonsocial (target absent) | Entire stimulus | ADI‐R (Social) | 22 | ASD | 16 Males, 6 Females | 13.7 years (3 years) | VIQ: 104 (20), NVIQ: 114 (12) | ‐ | No |
Negative correlation (controlling for VIQ) |
| Saccade error | ADI‐R (Social) |
ns (controlling for VIQ) |
||||||||||
| Left versus right difference score (saccade, absent saccade), saccade error | ADOS (Social) | ns | ||||||||||
| Wang et al. (2020) | First fixation duration, fixation duration | Dynamic, social | Social (people) | Autism Behavior Checklist | 35 | ASD | 33 Males, 2 Females | 16.51 years (7.02 years) | GDS Verbal: 16.51 (7.02) | ‐ | No | Negative correlation |
Abbreviations: ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ASD, autism spectrum disorder; CARS, Childhood Autism Rating Scale; CELF‐IV, Clinical Evaluation of Language Fundamentals, Fourth Edition; DS + ASD, Down syndrome with autism spectrum disorder; DS‐ASD, Down syndrome without autism spectrum disorder; EL, expressive language; FSIQ, full scale intelligence quotient; GDS, Gesell Development Schedules; HFA, high functioning autism; iASD, idiopathic autism spectrum disorder; ns, not significant; NT, neurotypical; NVIQ, nonverbal intelligence quotient; RCPM, Raven's Colored Progressive Matrices; RL, receptive language; SCQ, Social Communication Questionnaire; SRS‐2, Social Responsiveness Scale, Second Edition; VIQ, verbal intelligence quotient.
Two studies required participants to detect targets without distractor stimuli. Bavin et al. (2014) employed a target detection task and reported that reduced looking time at the target was associated with higher SCQ scores in a combined group of participants with ASD and neurotypical controls. Wang et al. (2020) presented participants with ASD with photographs of natural scenes (e.g., oceans, trees) in which either a social (i.e., children) or nonsocial (e.g., bowl) incongruent image was embedded. Participants were required to search for children in each scene. First fixation duration and total fixation duration to embedded social stimuli was negatively associated with scores on the Autism Behavior Checklist.
Overall, although there is an indication of some visual processing measures being associated with social functioning/autism symptom severity in ASD, methodological heterogeneity makes it difficult to draw conclusions.
Saccadic function
Saccadic functioning was examined by eight studies across multiple paradigms (refer to Table 19). DiCriscio et al. (2016) explored antisaccade errors and antisaccade/prosaccade latency, using social (i.e., open‐mouth happy faces), high autism interest (e.g., vehicles, construction equipment, books) and low autism interest (e.g., office supplies, furniture, musical instruments) images as peripheral stimuli. Although increased antisaccade error rates were associated with increased social impairment across all three stimulus categories, no significant relationships were identified when considering each stimulus category independently. Saccade latency was not related to measures of social functioning. Lindor et al. (2019) explored the influence of distractors and motor proficiency on saccadic functioning. Autism symptomatology (SRS‐2 Total score) significantly predicted final saccade accuracy, but only in the context of low motor proficiency.
TABLE 19.
Summary of findings—Saccadic paradigms (N = 8)
| Reference | Visual processing index | Visual stimuli | Social function/autism trait measure | Participant characteristics | Other clinical groups in analysis? | Results | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Diagnosis | Sex | Age M(SD) | IQ/DQ/mental age | Language | ||||||
| DiCriscio et al. (2016) | Antisaccade (error rate) |
Static, social/nonsocial (HAI, LAI) |
ADOS (RSI) | 19 | ASD | 16 Males, 3 Females | 13.35 years (4.38 years) |
VIQ: 101.11 (18.78) NVIQ: 103.84 (14.57) IQ Composite: 103.05 (14.29) |
‐ | No |
Positive correlation (across all stimulus categories) ns (within stimulus categories) |
| Antisaccade (latency), prosaccade (latency) |
ns |
||||||||||
| Glennon et al. (2020) | Facilitation (target object, gap/overlap task) | Static, nonsocial | SRS‐2 | 16 iASD, 7 DS + ASD, 8 DS‐ASD | iASD |
iASD 16 Males DS ± ASD 4 Males, 3 Females DS‐ASD 4 Males, 4 Females |
iASD 8.5 years (1.6 years) DS ± ASD 8.7 years (1.8 years) DS‐ASD 9.1 years (2.2 years) |
Leiter‐3 iASD 56 (22) DS ± ASD 30 (18) DS‐ASD 49 (15) |
‐ | Yes (iASD, DS + ASD, DS‐ASD) |
Main effect of group, group x facilitation interaction (higher SRS‐2 scores associated with smaller facilitation in iASD, not DS) |
| iASD only |
Negative prediction (regression model with mean search latency in gap‐overlap task) |
||||||||||
| Greene et al. (2019) | Visit count (cue predicted location, violation trials) | Static, social | SCQ, SRS | 25 ASD, 18 NT | ASD, NT |
ASD 22 Males, 3 Females NT 17 Males, 11 Females |
ASD 14.78 years (1.62 years) NT 14.81 years (2.08 years) |
ASD VIQ: 105.24 (16.98); PIQ: 101.80 (18.02); FSIQ: 104.40 (18.22) NT VIQ: 110.78 (11.97); PIQ: 104.83 (14.98); FSIQ: 109.28 (14.88) |
‐ | Yes (NT) |
Negative correlation (full sample, only SRS survived Bonferroni correction) ns (ASD, NT individually) |
| Keehn et al. (2019) | Disengagement (auditory gap/overlap) | Dynamic, social | ADOS‐2 (CSS – ASD only), SRS‐2 (Total) | 21 ASD, 20 NT | ASD, NT |
ASD 17 Males, 4 Females NT 15 Males, 5 Females |
ASD 11.5 years (1.3 years) NT 11.2 years (1.5 years) |
ASD VIQ: 102 (19), NVIQ: 101 (20) NT VIQ: 110 (11), NVIQ: 111 (13) |
‐ | Yes (NT, SRS only) | ns |
| Kuhn et al. (2010) | Gaze cueing (difference in interference between arrow and gaze cues) | Static, social | AQ | 12 ASD, 12 NT | ASD, NT | ‐ |
ASD 26.0 years (10.5 years) NT: 22.4 years (9.7 years) |
ASD VIQ: 109 (24.9); PIQ: 105 (17.6) FSIQ: 108 (22.9) NT VIQ: 108 (14.5), PIQ: 107 (10.9) FSIQ: 109 (12.5) |
‐ | Yes (NT) | ns |
| Lindor et al. (2019) | Final saccade accuracy (distractor task) | Dynamic, nonsocial | SRS‐2 (Total) | 19 ASD, 26 NT | ASD, NT |
ASD 10 Males, 9 Females NT 12 Males, 14 Females |
ASD 9.48 years (1.94 years) NT 10.11 years (2.43 years) |
ASD FSIQ: 104.89 (16.66) NT FSIQ: 108.62 (13.25) |
‐ | Yes (NT) |
Significant Interaction (SRS‐2 x MABC‐2) ns (SRS‐2, SRS‐2 x Conners‐3 Global T‐score; SRS‐2, SRS‐2 x Conners‐3 Inattention T‐score; SRS‐2, SRS‐2 x Conners‐3 Hyperactivity/Impulsivity T‐score; SRS‐2, SRS‐2 x age; SRS‐2, SRS‐2 x gender |
| McLaughlin et al. (2021) | Gap effect | Static, social/nonsocial | ADOS‐2 Social Communication, Total; SRS‐2 parent report | 35 | ASD | 27 Males, 8 Females | 10.96 years (2.72 years) | IQ: 90.82 (24.09) | ‐ | No | ns |
| Zalla et al. (2016) |
Visually guided saccade (step, gap, overlap): latency, accuracy, mean velocity, variability |
Green filled square | ADI‐R (RSI); ADOS (Social) | 20 | ASD | 19 Males, 1 Female | 31.5 years (10.7 years) | FSIQ: 108.6 (15.6), VIQ: 111.7 (14.7), PIQ: 105.7 (16.8) | ‐ | No | ns |
Abbreviations: ADI‐R, Autism Diagnostic Inventory, Revised; ADOS, Autism Diagnostic Observation Schedule; ADOS‐2, Autism Diagnostic Observation Schedule, Second Edition; ASD, autism spectrum disorder; CSS, calibrated severity score; DS + ASD, Down syndrome with autism spectrum disorder; DS‐ASD, Down syndrome without autism spectrum disorder; FSIQ, full scale intelligence quotient; HAI, high autism interest; iASD, idiopathic autism spectrum disorder; IQ, intelligence quotient; LAI, low autism interest; MABC‐2, Movement Assessment Battery for Children, Second Edition; ns, not significant; NT, neurotypical; NVIQ, nonverbal intelligence quotient; RSI, reciprocal social interaction; SCQ, Social Communication Questionnaire; SRS, Social Responsiveness Scale; SRS‐2, Social Responsiveness Scale, Second Edition; VIQ, verbal intelligence quotient.
Four studies used gap‐overlap paradigms, involving the presentation of a central target stimulus that disappears prior to the onset of a peripheral stimulus (gap condition), or remains on the screen with the presentation of a peripheral stimulus (overlap condition). Additionally, a baseline (or step) condition was included where the central stimulus offset is simultaneous with peripheral stimulus onset. Results were mixed. Glennon et al. (2020) found that reduced facilitation (the difference in saccadic reaction time between gap and baseline trials) was associated with higher scores on the SRS‐2 in ASD. However, using auditory (rather than visual) central and peripheral stimuli, Keehn et al. (2019) found that disengagement efficiency (saccadic reaction time divided by the number of trials in which a gaze shift occurred) across gap/overlap/baseline conditions was not associated with scores on the ADOS‐2 (calibrated severity score) or SRS‐2 (Total score). Zalla et al. (2016) found that saccadic latency, accuracy, velocity, and variability were not associated with the social subscales of the ADI‐R and ADOS across gap, overlap, and step conditions. Finally, McLaughlin et al. (2021) did not identify an association between the gap effect (difference in latency between the gap and overlap conditions) and autism symptom severity (ADOS‐2 Total score) or social functioning (ADOS‐2 Social Communication score, SRS‐2 Total score [parent report]) across combinations of social and nonsocial central and peripheral stimuli.
Finally, two studies examined cued and predictive gaze paradigms with similarly mixed findings. Participants in Greene et al. (2019) undertook an eyetracking task where the presentation of a circle or a square on a computer screen was indicative of the target (social and nonsocial images) appearing on the left and right side of the screen, respectively. Target locations were correctly cued 80% of the time. During trials in which the target was incorrectly cued, the number of times in which the cued location was attended to was negatively related to both SCQ and SRS scores (although only the SRS survived corrections for multiple comparisons) across ASD and neurotypical participants. These, however, were not significant within the ASD group alone. Kuhn et al. (2010) required participants to direct their gaze to a peripheral target with either an eye‐gaze distractor (a centrally positioned face looking at one of the two peripheral targets) or arrow distractor (directional arrow pointing toward one of the two peripheral targets) across both congruent and incongruent trials (distractors looking/pointing toward or away from the peripheral target, respectively). An efficiency score incorporating saccadic reaction time was not associated with AQ scores.
Overall, although there is an indication of associations between oculomotor indices with social functioning/autism symptom severity, studies are few with further investigation required.
Quantitative analysis
Sample size and descriptive statistics
A total of 16, 17, and 13 correlation effect estimates generated from nine, eight, and seven studies were included in the meta‐analysis for the face, eye, and mouth region, respectively. Names of studies included in the meta‐analysis for each region can be found in Supplementary Materials 3–8 in Data S1. After exclusion criteria were applied, no odds ratios or unstandardized beta estimates were present and studies only contributed more than one effect size due to different task conditions. Count and proportion of statistic type included in the meta‐analyses for each region are summarized in Supplementary Table 1 in Data S1.
Meta‐analysis: Overall effect estimate and key results
According to Cohen's effect size guidelines of Pearson correlation (Cohen, 1988), a multilevel, random effects meta‐analysis model revealed a medium sized and negative combined correlation effect estimate for the face region, Murias et al. (2018) negative value: Fisher's z = −0.49, p < 0.001, 95% CI [−0.74, −0.23]; Pearson r = −0.45, 95% CI [−0.63, −0.23]. This indicated that more looking at the face region was associated with reduced autism symptom severity. The confidence interval was wide, implying that aggregated data support values for the true unknown population association that correspond to a negative correlation of either small, medium or large magnitude.
For the eye region, a small and negative overall correlation effect size estimate was obtained, Murias et al. (2018) negative value: Fisher's z = −0.24, p < 0.001, 95% CI [−0.35, −0.13]; Pearson r = −0.24, 95% CI [−0.33, −0.13]. This similarly indicated that more looking at the eye region was associated with reduced autism symptom severity. The confidence interval was wide and indicates that aggregated data support values for the true unknown population association that correspond to a negative correlation of either small or medium magnitude.
For the mouth region, a positive relationship of negligible effect size (i.e., very small) was identified, Murias et al. (2018) negative value: Fisher's z = 0.03, p = 0.79, 95% CI [−0.21, 0.27]; Pearson r = 0.03, 95% CI [−0.21, 0.27]. The confidence interval was wide and suggests that aggregated data support values for the true unknown population association that correspond to either a positive or negative correlation of very small to small magnitude. Thus, much uncertainty exists around the true nature of this association (i.e., positive or negative). For each region, weighted Fisher z transformed units and Pearson correlation forest plots are in Supplementary Materials 3–8 in Data S1. Plots reflect an imputed negative value for the Murias study across regions (face r: −0.37, eyes r: −0.39, mouth r: −0.39). For Pearson forest plots, the x‐axis was transformed (non‐linear x‐axis) to obtain symmetric 95% confidence intervals.
For all regions, minimal change in the overall effect estimate and precision of the estimate (i.e., width of 95% CI) was observed by changing the valence of the Murias et al. (2018) statistic from negative to positive; faces Murias et al. (2018) positive value: Fisher's z = −0.42, 95% CI [−0.69, −0.14]; Pearson r = −0.40, 95% CI [−0.60, −0.14], eyes Murias et al. (2018) positive value: Fisher's z = −0.19, 95% CI [−0.33, −0.06]; Pearson r = −0.19, 95% CI [−0.32, −0.05], mouth Murias et al. (2018) positive value: Fisher's z = 0.12, 95% CI [−0.10, 0.35]; Pearson r = 0.12, 95% CI [−0.10, 0.34]. The slight adjustments to the estimate incurred by changing the valence made no, or very minor, difference to interpretation of findings in terms of strength and direction of association. As a result, for subsequent meta‐regression and subgroup analyses, a negative value was assigned to results from this study for the face, eyes, and mouth regions.
Meta‐regression
Cochran's Q tests revealed significant heterogeneity in the meta‐analysis for the face and mouth regions (p < 0.001 and 0.001, respectively). No significant heterogeneity was identified for the meta‐analysis with respect to the eye region (p > 0.05). Therefore, for the face and mouth regions, explanatory variables were assessed to determine whether they significantly contributed to the heterogeneity identified in their respective meta‐analyses.
For the face and mouth regions, the rater of the autism symptom severity measure (categories: clinician/researcher rated, parent/caregiver rated, self‐rated [eyes, mouth only], teacher rated) was found to be a significant predictor of the effect estimate in both meta‐analyses, face: Qm(df = 2) = 10.69, p = 0.005, mouth: Qm(df = 3) = 19.59, p < 0.001. Qm is the omnibus test of whether there is a difference in size of the correlation estimate between at least two levels of a categorical variable. For the face region, results revealed that compared to clinician/researcher rated measures, a stronger negative relationship between looking time at the face and autism symptom severity was identified for teacher rated measures (Fisher's z: b = −0.62, 95% CI [−1.03, −0.22], p = 0.003). For the mouth region, results revealed that compared to clinician/researcher rated measures (in which a negative correlation was estimated), a more positive relationship between looking time at the face and autism symptom severity was identified for parent/caregiver rated measures (Fisher's z outcome: b = +0.32, 95% CI [0.044, 0.59], p = 0.023), self‐rated measures (Fisher's z outcome: b = +0.63, 95% CI [0.34, 0.92], p < 0.001), and teacher rated measures (Fisher's z outcome: b = +0.48, 95% CI [0.052, 0.90], p = 0.028). The change in correlation from reference category, clinician/researcher rated, to comparator group is represented by b (present and subsequent paragraph).
Two additional significant predictors of the effect estimate were also identified. For the face region, points of calibration was a significant predictor, Qm(df = 1) = 42.77, p < 0.001. In comparison to studies using five points of calibration during eyetracking, a stronger negative relationship was identified between looking time at the face and autism symptom severity using more than five points of calibration during eyetracking (Fisher's z: b = −0.76, 95% CI [−0.99, −0.53], p < 0.001). For the mouth region, the number of unique ROIs was a significant predictor, Qm(df = 3) = 13.21, p < 0.001. In comparison to studies with two unique ROIs, a more negative association was identified between looking time at the face and autism symptom severity with four unique ROIs (Fisher's z: b = −0.44, 95% CI [−0.75, −0.12], p = 0.006).
Full omnibus meta‐regression results for all predictors investigated for the face and mouth regions in addition to correlational estimates of the association between gaze and ASD symptom severity for each level of categorical predictors can be found in Supplementary Materials 9 and 10 in Data S1, respectively.
Sensitivity and subgroup analyses
Correlation type
For each region, we judged that minimal change in the effect size estimate was observed when a meta‐analysis was conducted only using Pearson's correlation coefficients. The overall combined estimate for Pearson's correlation coefficients were (1) face (Fisher's z: b = −0.54, 95% CI [−0.82, −0.27]; Pearson's r = −0.50, 95% CI [−0.67, −0.27]), (2) eyes (Fisher's z: b = −0.19, 95% CI [−0.36, −0.03]; Pearson's r = −0.19, 95% CI [−0.35, −0.03]), and (3) mouth (Fisher's z: b = 0.08, 95% CI [−0.32, −0.47]; Pearson's r = 0.08, 95% CI [−0.44, −0.31]).
Risk of bias
The influence of level of study bias on overall effect size estimates was only investigated for the eye and mouth regions, as all studies included in the face region were evaluated as “satisfactory” based on the Newcastle‐Ottawa scale.
For mouth and eye regions, studies were categorized as either “unsatisfactory” or “satisfactory” and no studies were classified as “good” or “very good.” For the eye region, no significant difference in the combined correlation effect estimate was identified when comparing studies considered “unsatisfactory” and those considered “satisfactory” (Fisher's z: b = 0.086, 95% CI [−0.16, 0.33], p = 0.49). Similarly, for the mouth region, no significant difference in the combined correlation effect estimate was identified when comparing studies considered “unsatisfactory” and those considered “satisfactory” (Fisher's z: b = −0.188, 95% CI [−0.712, 0.337], p = 0.48). The magnitude and direction of change in correlation from reference category, “unsatisfactory,” to comparator group, “satisfactory,” is indicated by b.
DISCUSSION
Much research has been dedicated to exploring the relationship between visual processing and social functioning in ASD, particularly in recent years. Despite the reviewed literature supporting some longstanding assertions as to the gaze correlates of social functioning/autism symptom severity (e.g., reduced face and eye fixation), findings are generally negative or inconsistent, and there is evidence to suggest that relationships are context‐dependent and reflective of the heterogeneous nature of ASD. Moreover, although increased gaze toward the face/head and eye regions is largely linked to better social functioning and reduced autism symptom severity, gaze allocation to the mouth appears dependent on social and emotional content of scenes and cognitive profiles of participants. Our research also highlights that variation in social functioning measurements, ASD heterogeneity, a lack of research design consistency, and the exploratory/underpowered nature of many studies makes further conclusions difficult to draw at this stage. Each of these will be considered in turn.
Social motivation
Individuals with ASD have been described as assigning less reward value to social situations, reflective of the social motivation hypothesis of ASD (Chevallier et al., 2012). This theory posits that less reward value is assigned to engagement with social stimuli, leading to a reduction in attending to and engaging with social stimuli. Therefore, rather than a consequence of poor social functioning, reduced social motivation instead leads to social functioning difficulties. Indeed, there is evidence in the literature to suggest that social functioning ability of individuals can only be appraised in relation to visual processing when social stimuli are used that reduce the likelihood of an individual with ASD to regress into independent, nonsocial activity. Nadig et al. (2010) and Jones et al. (2017) identified that greater ASD symptomatology and reductions in social functioning was related to reduced fixations toward the face and eyes, respectively, during tasks in which there was a greater need for engagement with a social partner. The process of discussing a circumscribed interest for the ASD group in Nadig et al.'s study was described as a well‐rehearsed and mechanistic process. Therefore, the reciprocal nature of the conversation is reduced, with the authors suggesting that face fixation serves to orient the individual toward their social partner rather than being utilized to share a social experience. Additionally, although Jones et al. (2017) suggested that a lack of variability may account for the nonsignificant findings with respect to the interactive play segment, it may be that this activity was analogous to the circumscribed interest topic, where individuals with ASD were more likely to regress into independent activity. Significant results were instead obtained with conversational (Jones et al., 2017) and generic (Nadig et al., 2010) topics, both reflective of a shared social experience in which social functioning can be more adequately assessed.
This finding could also be extended to Gillespie‐Smith, Doherty‐Sneddon, et al. (2014), who explored the influence of facial familiarity on the allocation of gaze and social functioning. Increased percentage fixation duration to the eyes was significantly associated with greater social functioning ability only with respect to unfamiliar and self‐faces, but not familiar faces. It has been proposed that attending to familiar faces may result in more cognitively efficient face processing, with less time directed toward examining specific facial components (i.e., eyes, mouth; Sterling et al., 2008). It may be that this leads to a similar regression into nonsocial activity in that there is a lack of direction of visual attention toward facial components that convey social meaning. Instead, the use of unfamiliar and self‐faces may require individuals with ASD to interpret social cues from infrequent sources, requiring the increased allocation of social attention from which the allocation of gaze (and in turn, social functioning) can be assessed.
Moreover, disruption to early social learning processes may then lead to difficulties in later modulating gaze in response to unexpected social actions. Across a combined group of ASD and neurotypical participants, Swanson and Siller (2013) found that participants with higher social functioning ability were able to modulate their gaze between conditions where a model directed their gaze toward (congruent) or away from (incongruent) a target of interest. Fixation duration to the face was significantly higher for the incongruent condition, suggesting an orientation of gaze toward the model's face is made in an effort to search for joint attention cues to explain a violation of the model in acting in a socially consistent manner (i.e., looking at the target). Such modulation was not seen for participants with poorer social functioning ability, reflecting a lack of understanding the use of shared social cues to act in a socially consistent manner. Similarly, Hanley et al. (2014) found that participants with ASD took longer to redirect their gaze toward the face of the magician as a means of inferring their social awareness when there was overt interference in their performance.
Overall, there is an indication that direction of visual attention toward social stimuli in individuals with ASD is not necessarily reflective of increased motivation to fully immerse oneself in a shared social experience. In this case, increased motivation to attend to less threatening and well‐rehearsed social stimuli may instead result in regression into nonsocial activity, despite outwardly appearing social. Contrastingly, a lack of motivation to attend to social stimuli and interactions of increased complexity and novelty in turn has detrimental effects on social cognitive processing. This may also be bidirectional, with poor social cognitive processing contributing to the maintenance of poor social gaze. The use of eyetracking to identify gaze allocation across social stimuli and interactions that are spontaneous and novel (increasing the likelihood of actively engaging with a social partner) may not only be a useful supplementary diagnostic tool in identifying ASD, but also in serving as an indicator of improvement following social motivational interventions.
Cognitive function
The clinical heterogeneity in the cognitive profile of ASD is well documented, so it is not surprising to see emerging evidence of its influence on the relationship between allocation of gaze and social functioning. Although increased allocation of gaze toward the eyes has long been associated with increased social functioning, there is evidence to suggest that optimal social functioning in ASD is not necessarily constrained to looking at this facial region.
This is particularly evident when it comes to allocating gaze toward the mouth. In participants with a higher verbal than nonverbal cognitive profile, Rice et al. (2012) found that increased fixation duration to the mouth was related to improved social functioning. This result was ascribed to this population directing gaze toward the mouth in an effort to achieve social understanding by way of interpreting literal linguistic cues. This was further supportive of their previous study (Klin et al., 2002), although only a verbal IQ in the average range was reported in this sample. Another two studies similarly identified improved social functioning with increased fixation of the mouth, however, participants demonstrated a relatively even verbal versus nonverbal profile (Del Valle Rubido et al., 2018; Fedor et al., 2018), while Wieckowski and White (2016) did not provide this cognitive detail.
Contrastingly, Rice et al. (2012) noted that decreased social functioning was instead identified for participants with a higher full scale IQ (i.e., ≥ 98) when gazing at the mouth (with an even verbal/nonverbal profile). For this group, optimal social functioning was instead related to increased fixation duration to the eyes. This is also consistent with Fujioka et al. (2016) who also identified that increased duration of looking at the mouth of a blinking human face was associated with decreased social functioning/increased autism symptom severity in ASD participants with a mean full scale IQ ≥ 98 (with an even verbal/nonverbal profile). The direction of gaze toward specific facial regions may vary according to the cognitive profile of ASD and the associated capacity to successfully engage in social interactions. More research in this field could yield social training interventions that incorporate cognitive profiles and are accordingly tailored to increasing attention to facial regions that will likely lead to improvements in social function.
Limitations and future research directions
Age
There are a broad range of ages covered across each of the 95 studies reviewed, including infants later diagnosed with autism through to adults. Despite this range, only three studies have examined age‐related implications. Jones and Klin (2013) explored eye fixations in infants later diagnosed with autism across 2–6 month, 2–9 month, 2–12 month, 2–15 month, and 2–18 month developmental periods. Emerging at trend level from the 2–9 month developmental period, a significant decline in eye fixation was associated with reduced social functioning (ADOS Social Affect score) thereafter. Bacon et al. (2020) found that a preference for geometric figures in children aged 1–3 years with ASD positively predicted ADOS total scores at 6–12 years. Contrastingly, Asberg Johnels et al. (2017) found no relationship between either fixation duration to the eye and mouth regions across face depicting different emotions (i.e., happy, fearful, angry, neutral) or the difference between fixation duration to the eye and mouth regions with autism traits (as measured by the AQ) across either adolescent or adult ASD groups. Although Frazier et al. (2017) and Chita‐Tegmark (2016b) found that age did not moderate group differences in social/nonsocial attention between ASD and neurotypical participants in their meta‐analysis of eyetracking studies, Chita‐Tegmark (2016b) noted that the average age of included studies were generated across a broad age range and at best only offered a cross‐sectional representation of the influence of age. A longitudinal investigation would not only offer a detailed examination of the natural progression of gaze allocation in ASD, but also highlight the potential effectiveness of remediative programs aiming to train gaze to improve social functioning and symptom severity.
Biological sex
Males were by far most represented across studies, ranging from 53% males (Lindor et al., 2019; White et al., 2015) to male only samples (Del Valle Rubido et al., 2018; Franchini et al., 2016; Fujioka et al., 2016; Jones & Klin, 2013; Klin et al., 2002; Sasson et al., 2007; Speer et al., 2007). Not only is this consistent with a greater incidence of ASD in males (Loomes et al., 2017), but also with the broader literature that has been biased toward predominantly male samples (Kirkovski et al., 2013). None of the reviewed studies, however, have examined the relationship between gaze and social cognition as a function of biological sex. This is particularly important given the suggestion that females with ASD engage in social camouflaging, being better able to disguise their social functioning difficulties (Tubio‐Fungueirino et al., 2020). Specifically, as the female social dynamic tends to reflect more intimate styles of social behavior, ASD‐related symptomatology is easier to conceal compared to the large group‐based activities within which males usually engage (Dean et al., 2017). Emerging evidence supports more normative social attention in females with ASD, with increased attention to faces compared to males with ASD (Harrop et al., 2019; Harrop et al., 2020). Accordingly, there is a strong need to consider the female presentation of ASD when understanding the complex dynamics between visual processing and social function in this population.
Social functioning measurement
A wide variety of social functioning measures have been employed across studies, from specific measures of social functioning (e.g., SRS subscales), social functioning subscales of global autism measures (e.g., ADOS Social Algorithm), and global autism measures (e.g., ADI‐R Total score, AQ). Additionally, these have reflected parent, close other, and self‐report versions. Although 20 studies included in this review identified relationships between visual processing and social functioning that were dependent on the social functioning measure used, no clear patterns were identified.
This heterogeneity in approach has clear implications for the assessment of social functioning in ASD. For example, research has indicated that measurement tools used to screen for ASD symptomatology may not adequately assess all presentations across the autism spectrum (e.g., Cederberg et al., 2018). Global measures of ASD symptomatology (including the assessment of other ASD core domains, such as restricted/repetitive behavior) have also been used as a means of assessing social functioning in ASD (e.g., SRS; Fujioka et al., 2016; White et al., 2015), meaning that associations between these measures and gaze indices would likely not be different to investigating group differences in gaze between ASD and neurotypical participants. Moreover, Pallathra et al. (2018) noted that social functioning can be considered an overarching term encompassing difficulties in domains such as social motivation, social anxiety, social cognition, and social skills. In turn, it was suggested that individuals with ASD may demonstrate different profiles of deficits depending on these subcategories of social functioning, and that tailored social functioning treatments depending on individual profiles would likely be more effective than universal treatment approaches in ASD. Therefore, future research should look to investigate not only the different domains comprising social functioning, but also the specific social functioning measurements that best correlate with these domains.
Additionally, an issue in formally assessing social functioning in ASD is the widespread heterogeneity in presentation. The categorical framework of current diagnostic methods (e.g., DSM‐5) fail to capture the variability in presenting symptoms and the influence of comorbid conditions which can have significant implications for treatment approach (Hennessey et al., 2018; Mandy, 2018). Current diagnostic approaches to ASD are also reliant on self/close‐other reports and behavioral observations (Hennessey et al., 2018), with categorical approaches neglecting the consideration of neurobiological and genomic advances in our understanding of mental health conditions (Insel et al., 2010).
The limitations associated with categorical approaches in diagnosing mental health conditions, and the heterogeneity in ASD presentations identified in the current review (e.g., age, IQ), supports the continued investigation into the use of the research domain criteria (RDoC) in the context of social functioning in ASD. This approach to the investigation and conceptualization of mental health disorders assesses psychological functioning dimensionally from nonclinical to clinical, with a focus on identifying underlying pathophysiology (Cuthbert & Insel, 2013). The RdoC matrix considers a range of functional domains (e.g., cognitive systems, arousal and regulatory systems) against multiple units of analysis (from genes through to self‐report). Currently, ASD symptomatology can be represented across each of the functional domains of the RdoC (Harrison et al., 2021). As a functional domain of the RdoC, systems for social processes explores interpersonal functioning across four constructs (affiliation and attachment, social communication, perception and understanding of self, perception, and understanding of others). Investigating social functioning from this perspective acknowledges the diversity in ASD via a consideration of the complex interaction between biological and behavioral determinants, allowing for the development of targeted treatment approaches depending on individual pathophysiological profiles (Ibrahim & Sukhodolsky, 2018; Mandy, 2018). Eye gaze detection and scanning patterns have been included as behavioral units of analysis for the social communication construct of the systems for social processes domain, and their inclusion would not only account for the heterogeneity identified across the autism spectrum with respect to gaze, but as potential diagnostic biomarkers. Indeed, there are recent studies that have explored the use of eyetracking variables as potential biomarkers for ASD (Bradshaw et al., 2019; Del Valle Rubido et al., 2018; McPartland et al., 2020).
Despite RdoC criteria holding promise as a means of characterizing the diversity in ASD, it is important to recognize that it is still in its infancy. There are few studies that have empirically examined the veracity of RdoC with respect to ASD, with studies continuing to offer refinements and additions to this framework (e.g., Harrison et al., 2021; Tschida & Yerys, 2020). Additionally, RdoC is not intended to fully replace current diagnostic criteria, but provides a translational and transdiagnostic approach to researching and understanding mental health conditions, including ASD (Cuthbert & Insel, 2013; Mandy, 2018). Nonetheless, this is a promising area of research in becoming inclusive of the diagnostic variability in ASD.
Eye movement recordings
The majority of studies (N = 70) included indices of how long participants directed their gaze toward aspects of a visual scene (e.g., interest areas). While gaze duration to specific interest areas is important to consider, it may not necessarily reflect the use of social cues to guide the allocation of gaze to regions of a social scene that are most conducive to social understanding.
This is particularly the case in the context of goal directed action, which has been described in the context of the direct matching hypothesis—where visual features of an observed action are mapped onto one's own motor system to facilitate action understanding (Rizzolatti et al., 2001). However, this has been found to be dependent on the use of predictive gaze—where gaze is allocated to the goal of an observed motor action prior to the completion of the observed motor action (Flanagan & Johansson, 2003). This has also been noted to be consistent with the mirror neuron system (MNS), a group of frontoparietal neurons that fire during both action observation and execution (Iacoboni & Mazziotta, 2007) and are believed to facilitate social understanding (Jeon & Lee, 2018). There are, in turn, associated implications for ASD, of which there has been notable debate regarding the integrity of the MNS. An examination of predictive rather than reactive gaze would further an understanding of how social gaze is used, particularly with respect to goal directed action, in ASD.
Methodological considerations
Many of the reviewed studies explored the relationship between gaze and social functioning variables in an exploratory manner (35 of the 95 studies cited the investigation of the social functioning/autism symptom severity association as a supplementary goal), often employing small sample sizes, and in a cross‐sectional manner. Additionally, the group composition in which this relationship was examined differed across studies (e.g., ASD only, ASD combined with neurotypical and/or other neurodevelopmental disorder groups), which may alter the strength of the relationship identified. This methodological heterogeneity makes it difficult to draw firm conclusions about the nature of the relationship between gaze and autism symptom severity and more specifically, whether any there are any distinct associations between gaze and social functioning in ASD.
This was also supported by the results of the meta‐analysis and meta‐regression. The meta‐analysis revealed a stronger effect size estimate for the face ROI compared with the eyes ROI, with negligible results for the mouth. This was consistent with Chita‐Tegmark (2016a) who found a larger effect size estimate for the face compared with the eyes and mouth when examining differences in gaze allocation to these regions between participants with ASD and neurotypical controls. The greater strength in the relationship observed for faces, however, might be explained by the larger relative size of the face ROI, which may offer a greater opportunity to capture gaze in order to assess the relationship with social functioning/autism symptom severity. Therefore, researchers seeking to validly investigate the relationship and compare this relationship dependent on ROI need to keep in mind equivalence of ROI size, which may act as a confounding variable. Additionally, the face ROI is comprised of both the eyes and mouth, with optimal social functioning dependent on being able to holistically integrate these features (Vrancken et al., 2017). Global/local processing difficulties are a longstanding feature of ASD (Happe & Frith, 2006; Koldewyn et al., 2013; Van Eylen et al., 2018), suggesting that future research should consider simultaneously examining local (i.e., mouth, eyes) and global (i.e., face) ROIs to shed further light as to the nature of the gaze‐social functioning/autism symptom severity relationship.
Additionally, the results of the meta‐regressions conducted for the face and mouth ROIs tentatively suggest that rater of the autism symptom severity measure may moderate the magnitude of the meta‐analysis effect estimates. For the face ROI, a substantially more negative correlation was observed in the teacher rating category relative to clinician/researcher, whereas a significantly more positive correlation was observed for parent/caregiver, self, and teacher‐rated measures relative to clinician/researcher for the mouth ROI. Notably, there were directional inconsistencies between region domains, which at face value, point to the hard to reason possibility that rater perception (e.g., clinician/researcher, teacher) is contingent on ROI domain. A factor which may underly directional differences and limit interpretability of such findings that requires acknowledgement, however, is that meta regressions were conducted in a bivariate context. Therefore, they do not control for other factors that may confound the relationship if unbalanced across rater levels. Furthermore, all individual effect estimates in the teacher rating category were either from the same study/studies with the same authors (and likely thus the same teacher raters), in turn reducing generalizability. Overall, these preliminary findings suggest that future research should consider the rater of the measurement tool in analyses as a means of further elucidating the nature (i.e., strength and magnitude) of the gaze‐social functioning/autism symptom severity relationship.
The investigation of variables that are postulated to contribute to this heterogeneity, including best measures of gaze and social functioning (e.g., reactive vs. predictive gaze), in addition to the paradigms and task parameters employed that best capture the nature of this relationship (e.g., basic vs. increasing social complexity, ROI size) would strengthen our understanding of this relationship in ASD. Moreover, large longitudinal studies would additionally account for any heterogeneity and would be able to track the developmental progression of this relationship. Such efforts are currently underway, with the Autism Biomarkers Consortium for Clinical Trials (McPartland et al., 2020) investigating potential biomarkers for ASD (including eyetracking indices).
Recommendations for future studies
Based on the systematic review and quantitative analysis, the following are recommended for future studies in assessing the relationship between gaze and social functioning in ASD:
Given indications that social functioning is comprised of specific domains (e.g., social cognition, social anxiety), incorporating more than one measure of social functioning targeting these domains would assist in further profiling social functioning difficulties in ASD and how they relate to social visual engagement.
Examining the impact of participant characteristics (including IQ, age, biological sex) on the gaze‐social functioning relationship in large samples of ASD groups.
Including comparisons to non‐ASD neurodevelopmental disorders to further assist in the specific characterization of deficits in ASD.
Inclusion of multiple gaze indices (e.g., predictive gaze, cued conditions, gaze similarity with neurotypical, and other non‐ASD neurodevelopmental disorders).
Consideration of the stimuli used to assess the relationship (e.g., complexity of social scenes) and employing task parameters to ensure quality of measurement (e.g., eyetracker points of calibration, size of ROI). This would facilitate the development of protocols that best capture the nature of the relationship between gaze and social functioning.
CONCLUSION
Despite a recent increase in studies examining the relationship between gaze and social functioning in ASD, ASD heterogeneity, a lack of research design consistency, and the exploratory/underpowered nature of the studies makes conclusions difficult to draw at this stage. Findings suggest increased gaze toward the face/head and eyes are generally associated with better social functioning. Moreover, there is emerging evidence that the gaze‐social functioning/autism symptom severity relationship in ASD differs depending on individual clinical characteristics (e.g., social motivation, cognitive ability). Given the recent interest in the use of eyetracking measures as a potential biomarker of ASD, further exploration of the associations between eyetracking and gaze with social functioning/autism symptom severity will be important. Coupled with appropriately powered designs, this would allow for the development of early interventions that would be best positioned to mitigate the downstream effect of aberrant gaze processing in disrupting social learning opportunities in those with ASD.
CONFLICT OF INTEREST
There are no conflicts of interest to declare.
ETHICS STATEMENT
This study was a review and meta‐analysis of existing, published literature not requiring ethics committee approval.
Supporting information
Appendix S1. Supporting Information
ACKNOWLEDGEMENTS
Peter Enticott is supported by a Future Fellowship from the Australian Research Council (FT160100077). Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Riddiford, J. A. , Enticott, P. G. , Lavale, A. , & Gurvich, C. (2022). Gaze and social functioning associations in autism spectrum disorder: A systematic review and meta‐analysis . Autism Research, 15(8), 1380–1446. 10.1002/aur.2729
Funding informationPeter G. Enticott is funded by a Future Fellowship from the Australian Research Council (FT160100077).
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Aman, M. G. , Singh, N. N. , Stewart, A. W. , & Field, C. J. (1985). The Aberrant Behavior Checklist: A behavior rating scale for the assessment of treatment effects. American Journal of Mental Deficiency, 89, 485–491. [PubMed] [Google Scholar]
- Amestoy, A. , Guillaud, E. , Bouvard, M. P. , & Cazalets, J. (2015). Developmental changes in face visual scanning in autism spectrum disorder as assessed by data‐based analysis. Frontiers in Psychology, 6, 989. 10.3389/fpsyg.2015.00989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amso, D. , Haas, S. , Tenenbaum, E. , Markant, J. , & Sheinkopf, S. J. (2014). Bottom‐up attention orienting in young children with autism. Journal of Autism and Developmental Disorders, 44, 664–673. 10.1007/s10803-013-1925-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annaz, D. , Remington, A. , Milne, E. , Coleman, M. , Campbell, R. , Thomas, M. S. , & Swettenham, J. (2010). Development of motion processing in children with autism. Developmental Science, 13(6), 826–838. 10.1111/j.1467-7687.2009.00939.x [DOI] [PubMed] [Google Scholar]
- Asberg Johnels, J. , Hovey, D. , Zurcher, N. , Hippolyte, L. , Lemonnier, E. , Gillberg, C. , & Hadjikhani, N. (2017). Autism and emotional face‐viewing. Autism Research, 10(5), 901–910. 10.1002/aur.1730 [DOI] [PubMed] [Google Scholar]
- Avni, I. , Meiri, G. , Bar‐Sinai, A. , Reboh, D. , Manelis, L. , Flusser, H. , Michaelovski, A. , Menashe, I. , & Dinstein, I. (2020). Children with autism observe social interactions in an idiosyncratic manner. Autism Research, 13, 935–946. 10.1002/aur.2234 [DOI] [PubMed] [Google Scholar]
- Bacon, E. C. , Moore, A. , Lee, Q. , Barnes, C. C. , Courchesne, E. , & Pierce, K. (2020). Identifying prognostic markers in autism spectrum disorder using eye tracking. Autism, 24(3), 658–669. 10.1177/1362361319878578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangerter, A. , Ness, S. , Aman, M. G. , Esbensen, A. J. , Goodwin, M. S. , Dawson, G. , Hendren, R. , Leventhal, B. , Khan, A. , Opler, M. , Harris, A. , & Pandina, G. (2017). Autism Behavior Inventory: A novel tool for assessing core and associated symptoms of autism spectrum disorder. Journal of Child and Adolescent Psychopharmacology, 27(9), 814–822. 10.1089/cap.2017.0018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangerter, A. , Ness, S. , Lewin, D. , Aman, M. G. , Esbensen, A. J. , Goodwin, M. S. , Dawson, G. , Hendren, R. , Leventhal, B. , Shic, F. , Opler, M. , Ho, K. F. , & Pandina, G. G. (2019). Clinical validation of the Autism Behavior Inventory: Caregiver‐rated assessment of core and associated symptoms of autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(6), 2090–2101. 10.1007/s10803-019-03965-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron‐Cohen, S. , Hoekstra, R. A. , Knickmeyer, R. , & Wheelwright, S. (2006). The Autism Spectrum Quotient (AQ) – Adolescent version. Journal of Autism and Developmental Disorders, 36(3), 343–350. 10.1007/s10803-006-0073-6 [DOI] [PubMed] [Google Scholar]
- Baron‐Cohen, S. , Wheelwright, S. , Hill, J. , Raste, Y. , & Plumb, I. (2001). The “Reading the Mind in the Eyes” Test revised version: A study with normal adults, and adults with Asperger syndrome or high‐functioning autism. Journal of Child Psychology and Psychiatry, 42(2), 241–251. 10.1111/1469-7610.00715 [DOI] [PubMed] [Google Scholar]
- Baron‐Cohen, S. , Wheelwright, S. , Scahill, V. , Lawson, J. , & Spong, A. (2001). Are intuitive physics and intuitive psychology independent? A test with children with Asperger syndrome. Journal of Developmental and Learning Disorders, 5, 47–78. [Google Scholar]
- Baron‐Cohen, S. , Wheelwright, S. , Skinner, R. , Martin, J. , & Clubley, E. (2001). The Autism‐Spectrum Quotient (AQ): Evidence from Asperger syndrome/high‐functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders, 31(1), 5–17. 10.1023/a:1005653411471 [DOI] [PubMed] [Google Scholar]
- Bast, N. , Mason, L. , Freitag, C. M. , Smith, T. , Portugal, A. M. , Poustka, L. , Banaschewski, T. , Johnson, M. , & The EU‐AIMS LEAP Group . (2021). Saccade dysmetria indicates attenuated visual exploration in autism spectrum disorder. Journal of Child Psychology and Psychiatry, 62(2), 149–159. 10.1111/jcpp.13267 [DOI] [PubMed] [Google Scholar]
- Bavin, E. L. , Kidd, E. , Prendergast, L. , Baker, E. , Dissanayake, C. , & Prior, M. (2014). Severity of autism is related to children's language processing. Autism Research, 7(6), 687–694. 10.1002/aur.1410 [DOI] [PubMed] [Google Scholar]
- Bird, G. , Press, C. , & Richardson, D. C. (2011). The role of alexithymia in reduced eye‐fixation in autism spectrum conditions. Journal of Autism and Developmental Disorders, 41, 1556–1564. 10.1007/s10803-011-1183-3 [DOI] [PubMed] [Google Scholar]
- Bradshaw, J. , Shic, F. , Holden, A. N. , Horowitz, E. J. , Barrett, A. C. , German, T. C. , & Vernon, T. W. (2019). The use of eye tracking as a biomarker of treatment outcome in a pilot randomized clinical trial for young children with autism. Autism Research, 12(5), 779–793. 10.1002/aur.2093 [DOI] [PubMed] [Google Scholar]
- Campbell, D. J. , Shic, F. , Macari, S. , & Chawarska, K. (2014). Gaze response to dyadic bids at 2 years related to outcomes at 3 years in autism spectrum disorders: A subtyping analysis. Journal of Autism and Developmental Disorders, 44(2), 431–442. 10.1007/s10803-013-1885-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cederberg, C. D. , Gann, L. C. , Foley‐Nicpon, M. , & Sussman, Z. (2018). ASD screening measures for high‐ability youth with ASD: Examining the ASSQ and SRS. The Gifted Child Quarterly, 62(2), 220–229. 10.1177/0016986217752098 [DOI] [Google Scholar]
- Chawarska, K. , Macari, S. , & Shic, F. (2012). Context modulates attention to social scenes in toddlers with autism. Journal of Child Psychology and Psychiatry, 53(8), 903–913. 10.1111/j.1469-7610.2012.02538.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawarska, K. , & Shic, F. (2009). Looking but not seeing: Atypical visual scanning and recognition of faces in 2 and 4‐year‐old children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 39(12), 1663–1672. 10.1007/s10803-009-0803-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawarska, K. , Ye, S. , Shic, F. , & Chen, L. (2016). Multilevel differences in spontaneous social attention in toddlers with autism spectrum disorder. Child Development, 87(2), 543–557. 10.1111/cdev.12473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevallier, C. , Kohls, G. , Troiani, V. , Brodkin, E. S. , & Schultz, R. T. (2012). The social motivation theory of autism. Trends in Cognitive Sciences, 16(4), 231–239. 10.1016/j.tics.2012.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chita‐Tegmark, M. (2016a). Attention allocation in ASD: A review and meta‐analysis of eye‐tracking studies. Review Journal of Autism and Developmental Disorders, 3(3), 209–223. 10.1007/s40489-016-0077-x [DOI] [PubMed] [Google Scholar]
- Chita‐Tegmark, M. (2016b). Social attention in ASD: A review and meta‐analysis of eye‐tracking studies. Research in Developmental Disabilities, 48, 79–93. 10.1016/j.ridd.2015.10.011 [DOI] [PubMed] [Google Scholar]
- Cochrane Training . (n.d.). Meta‐regression . https://handbook-5-1.cochrane.org/chapter_9/9_6_4_meta_regression.htm
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Academic Press. [Google Scholar]
- Cohen, I. L. , Schmidt‐Lackner, S. , Romanczyk, R. , & Sudhalter, V. (2003). The PDD Behavior Inventory: A rating scale for assessing response to intervention in children with pervasive developmental disorder. Journal of Autism and Developmental Disorders, 33(1), 31–45. [DOI] [PubMed] [Google Scholar]
- Cole, E. J. , Slocombe, K. E. , & Barraclough, N. E. (2017). Abilities to explicitly and implicitly infer intentions from actions in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(5), 1712–1726. 10.1007/s10803-017-3425-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino, J. N. , Davis, S. A. , Todd, R. D. , Schindler, M. K. , Gross, M. M. , Brophy, S. L. , Metzger, L. M. , Shoushtari, C. S. , Splinter, R. , & Reich, W. (2003). Validation of a brief quantitative measure of autistic traits: Comparison of the Social Responsiveness Scale with the Autism Diagnostic Interview‐Revised. Journal of Autism and Developmental Disorders, 33(4), 427–433. [DOI] [PubMed] [Google Scholar]
- Constantino, J. N. , & Gruber, C. P. (2002). Social Responsiveness Scale. Western Psychological Services. [Google Scholar]
- Constantino, J. N. , & Gruber, C. P. (2005). Social Responsiveness Scale. Western Psychological Services. [Google Scholar]
- Constantino, J. N. , & Gruber, C. P. (2012). Social Responsiveness Scale (2nd ed.). Western Psychological Services. [Google Scholar]
- Corcoran, R. , Mercer, G. , & Frith, C. D. (1995). Schizophrenia, symptomatology and social inference: Investigating “theory of mind” in people with schizophrenia. Schizophrenia Research, 17, 5–13. 10.1016/0920-9964(95)00024-g [DOI] [PubMed] [Google Scholar]
- Corden, B. , Chilvers, R. , & Skuse, D. (2008). Avoidance of emotionally arousing stimuli predicts social‐perceptual impairment in Asperger's syndrome. Neuropsychologia, 46(1), 137–147. 10.1016/j.neuropsychologia.2007.08.005 [DOI] [PubMed] [Google Scholar]
- Crawford, H. , Moss, J. , Anderson, G. M. , Oliver, C. , & McCleery, J. P. (2015). Implicit discrimination of basic facial expressions of positive/negative emotion in fragile X syndrome and autism spectrum disorder. American Journal on Intellectual and Developmental Disabilities, 120(4), 328–345. 10.1352/1944-7558-120.4.328 [DOI] [PubMed] [Google Scholar]
- Crehan, E. T. , & Althoff, R. R. (2021). Me looking at you, looking at me: The stare‐in the‐crowd effect and autism spectrum disorder. Journal of Psychiatric Research, 140, 101–109. 10.1016/j.jpsychires.2021.05.050 [DOI] [PubMed] [Google Scholar]
- Crehan, E. T. , Althoff, R. R. , Riehl, H. , Prelock, P. A. , & Hutchins, T. (2020). Brief report: Me, reporting on myself: Preliminary evaluation of the criterion‐related validity of the Theory of Mind Inventory‐2 when completed by autistic young adults. Journal of Autism and Developmental Disorders, 50(2), 659–664. 10.1007/s10803-019-04278-5 [DOI] [PubMed] [Google Scholar]
- Cuthbert, B. N. , & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(126), 1–8. 10.1186/1741-7015-11-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuve, H. C. , Castiello, S. , Shiferaw, B. , Ichijo, E. , Catmur, C. , & Bird, G. (2021). Alexithymia explains atypical spatiotemporal dynamics of eye gaze in autism. Cognition, 212, 104710. 10.1016/j.cognition.2021.104710 [DOI] [PubMed] [Google Scholar]
- de Winter, J. C. , Gosling, S. D. , & Potter, J. (2016). Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: A tutorial using simulations and empirical data. Psychological Methods, 21(3), 273–290. 10.1037/met0000079 [DOI] [PubMed] [Google Scholar]
- Dean, M. , Harwood, R. , & Kasari, C. (2017). The art of camouflage: Gender differences in the social behaviors of girls and boys with autism spectrum disorder. Autism, 21(6), 678–689. 10.1177/1362361316671845 [DOI] [PubMed] [Google Scholar]
- Deen, B. , Koldewyn, K. , Kanwisher, N. , & Saxe, R. (2015). Functional organization of social perception and cognition in the superior temporal sulcus. Cerebral Cortex, 25(11), 4596–4609. 10.1093/cercor/bhv111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Bianco, T. , Mason, L. , Charman, T. , Tillman, J. , Loth, E. , Hayward, H. , Shic, F. , Buitelaar, J. , Johnson, M. H. , Jones, E. J. H. , & the EU‐AIMS LEAP Group . (2021). Temporal profiles of social attention are different across development in autistic and neurotypical people. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 6(8), 813–824. 10.1016/j.bpsc.2020.09.004 [DOI] [PubMed] [Google Scholar]
- Del Valle Rubido, M. , McCracken, J. T. , Hollander, E. , Shic, F. , Noeldeke, J. , Boak, L. , Khwaja, O. , Sadikhov, S. , Fontoura, P. , & Umbricht, D. (2018). In search of biomarkers for autism spectrum disorder. Autism Research, 11(11), 1567–1579. 10.1002/aur.2026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiCriscio, A. S. , Miller, S. J. , Hanna, E. K. , Kovac, M. , Turner‐Brown, L. , Sasson, N. J. , Sapyta, J. , Troiani, V. , & Dichter, G. S. (2016). Brief report: Cognitive control of social and nonsocial visual attention in autism. Journal of Autism and Developmental Disorders, 46(8), 2797–2805. 10.1007/s10803-016-2804-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duchaine, B. , & Nakayama, K. (2006). The Cambridge Face Memory Test: Results for neurologically intact individuals and an investigation of its validity using inverted face stimuli and prosopagnosic participants. Neuropsychologia, 44(4), 576–585. 10.1016/j.neuropsychologia.2005.07.001 [DOI] [PubMed] [Google Scholar]
- Dziobek, I. , Fleck, S. , Kalbe, E. , Rogers, K. , Hassenstab, J. , Brand, M. , Kessler, J. , Woike, J. K. , Wolf, O. T. , & Convit, A. (2006). Introducing MASC: A movie for the assessment of social cognition. Journal of Autism and Developmental Disorders, 36(5), 623–636. 10.1007/s10803-006-0107-0 [DOI] [PubMed] [Google Scholar]
- Eigsti, I. M. , de Marchena, A. B. , Schuh, J. M. , & Kelley, E. (2011). Language acquisition in autism spectrum disorders: A developmental review. Research in Autism Spectrum Disorders, 5(2), 681–691. 10.1016/j.rasd.2010.09.001 [DOI] [Google Scholar]
- Ehlers, S. , Gillberg, C. , & Wing, L. (1999). A screening questionnaire for Asperger syndrome and other high‐functioning autism spectrum disorders in school age children. Journal of Autism and Developmental Disorders, 29(2), 129–141. 10.1023/a:1023040610384 [DOI] [PubMed] [Google Scholar]
- Ekman, P. , & Friesen, W. (1976). Pictures of facial affect. Consulting Psychologists Press. [Google Scholar]
- Fantz, R. L. (1964). Visual experience in infants: Decreased attention to familiar patterns relative to normal ones. Science, 146, 668–670. 10.1126/science.146.3644.668 [DOI] [PubMed] [Google Scholar]
- Fedor, J. , Lynn, A. , Foran, W. , DiCicco‐Bloom, J. , Luna, B. , & O'Hearn, K. (2018). Patterns of fixation during face recognition: Differences in autism across age. Autism, 22(7), 866–880. 10.1177/1362361317714989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan, J. R. , & Johansson, R. S. (2003). Action plans used in action observation. Nature, 424, 769–771. 10.1038/nature01861 [DOI] [PubMed] [Google Scholar]
- Franchini, M. , Armstrong, V. L. , Schaer, M. , & Smith, I. M. (2019). Initiation of joint attention and related visual attention processes in infants with autism spectrum disorder: Literature review. Child Neuropsychology, 25(3), 287–317. 10.1080/09297049.2018.1490706 [DOI] [PubMed] [Google Scholar]
- Franchini, M. , Glaser, B. , Gentaz, E. , Wood, H. , Eliez, S. , & Schaer, M. (2017). The effect of emotional intensity on responses to joint attention in preschoolers with an autism spectrum disorder. Research in Autism Spectrum Disorders, 35, 13–24. 10.1016/j.rasd.2016.11.010 [DOI] [Google Scholar]
- Franchini, M. , Wood de Wilde, H. , Glaser, B. , Gentaz, E. , Eliez, S. , & Schaer, M. (2016). Brief report: A preference for biological motion predicts a reduction in symptom severity 1 year later in preschoolers with autism spectrum disorders. Frontiers in Psychiatry, 7, 143. 10.3389/fpsyt.2016.00143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier, T. W. , Klingemier, E. W. , Beukemann, M. , Speer, L. , Markowitz, L. , Parikh, S. , Wexberg, S. , Giuliano, K. , Schulte, E. , Delahunty, C. , Ahuja, V. , Eng, C. , Manos, M. J. , Hardan, A. Y. , Youngstrom, E. A. , & Strauss, M. S. (2016). Development of an objective autism risk index using remote eye tracking. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 301–309. 10.1016/j.jaac.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier, T. W. , Klingemier, E. W. , Parikh, S. , Speer, L. , Strauss, M. S. , Eng, C. , Hardan, A. Y. , & Youngstrom, E. A. (2018). Development and validation of objective and quantitative eye tracking−based measures of autism risk and symptom levels. Journal of the American Academy of Child & Adolescent Psychiatry, 57(11), 858–866. 10.1016/j.jaac.2018.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier, T. W. , Strauss, M. , Klingemier, E. W. , Zetzer, E. E. , Hardan, A. Y. , Eng, C. , & Youngstrom, E. A. (2017). A meta‐analysis of gaze differences to social and nonsocial information between individuals with and without autism. Journal of the American Academy of Child & Adolescent Psychiatry, 56(7), 546–555. 10.1016/j.jaac.2017.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost‐Karlsson, M. , Galazka, M. A. , Gillberg, C. , Gillberg, C. , Miniscalco, C. , Billstedt, E. , Hadjikhani, N. , & Asberg Johnels, J. (2019). Social scene perception in autism spectrum disorder: An eye‐tracking and pupillometric study. Journal of Clinical and Experimental Neuropsychology, 41(10), 1024–1032. 10.1080/13803395.2019.1646214 [DOI] [PubMed] [Google Scholar]
- Fujioka, T. , Inohara, K. , Okamoto, Y. , Masuya, Y. , Ishitobi, M. , Saito, D. N. , Jung, M. , Arai, S. , Matsumura, Y. , Fujisawa, T. X. , Narita, K. , Suzuki, K. , Tsuchiya, K. J. , Mori, N. , Katayama, T. , Sato, M. , Munesue, T. , Okazawa, H. , Tomoda, A. , … Kosaka, H. (2016). Gazefinder as a clinical supplementary tool for discriminating between autism spectrum disorder and typical development in male adolescents and adults. Molecular Autism, 7, 19. 10.1186/s13229-016-0083-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujioka, T. , Tsuchiya, K. J. , Saito, M. , Hirano, Y. , Matsuo, M. , Kikuchi, M. , Maegaki, Y. , Choi, D. , Kato, S. , Yoshida, T. , Yoshimura, Y. , Ooba, S. , Mizuno, Y. , Takiguchi, S. , Matsuzaki, H. , Tomoda, A. , Shudo, K. , Ninomiya, M. , Katayama, T. , & Kosaka, H. (2020). Developmental changes in attention to social information from childhood to adolescence in autism spectrum disorders: A comparative study. Molecular Autism, 11(1), 24. 10.1186/s13229-020-00321-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furl, N. , Garrido, L. , Dolan, R. J. , Driver, J. , & Duchaine, B. (2011). Fusiform gyrus face selectivity relates to individual differences in facial recognition ability. Journal of Cognitive Neuroscience, 23(7), 1723–1740. 10.1162/jocn.2010.21545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie‐Smith, K. , Doherty‐Sneddon, G. , Hancock, P. J. , & Riby, D. M. (2014). That looks familiar: Attention allocation to familiar and unfamiliar faces in children with autism spectrum disorder. Cognitive Neuropsychiatry, 19(6), 554–569. 10.1080/13546805.2014.943365 [DOI] [PubMed] [Google Scholar]
- Gillespie‐Smith, K. , Riby, D. M. , Hancock, P. J. , & Doherty‐Sneddon, G. (2014). Children with autism spectrum disorder (ASD) attend typically to faces and objects presented within their picture communication systems. Journal of Intellectual Disability Research, 58(5), 459–470. 10.1111/jir.12043 [DOI] [PubMed] [Google Scholar]
- Glennon, J. M. , D'Souza, H. , Mason, L. , Karmiloff‐Smith, A. , & Thomas, M. S. C. (2020). Visuo‐attentional correlates of autism spectrum disorder (ASD) in children with Down syndrome: A comparative study with children with idiopathic ASD. Research in Developmental Disabilities, 104, 103678. 10.1016/j.ridd.2020.103678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin, R. L. , Matson, J. L. , Konst, M. J. , & Adams, H. L. (2014). A comparison of children and adolescents with ASD, atypical development, and typical development on the Behavioral Assessment System for Children, Second Edition (BASC‐2). Research in Autism Spectrum Disorders, 8(8), 951–957. 10.1016/j.rasd.2014.04.005 [DOI] [Google Scholar]
- Greene, R. K. , Parish‐Morris, J. , Sullivan, M. , Kinard, J. L. , Mosner, M. G. , Turner‐Brown, L. M. , Penn, D. L. , Wiesen, C. A. , Pallathra, A. A. , Brodkin, E. S. , Schultz, R. T. , & Dichter, G. S. (2020). Dynamic eye tracking as a predictor and outcome measure of social skills intervention in adolescents and adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 51, 1173–1187. 10.1007/s10803-020-04594-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene, R. K. , Zheng, S. , Kinard, J. L. , Mosner, M. G. , Wiesen, C. A. , Kennedy, D. P. , & Dichter, G. S. (2019). Social and nonsocial visual prediction errors in autism spectrum disorder. Autism Research, 12(6), 878–883. 10.1002/aur.2090 [DOI] [PubMed] [Google Scholar]
- Gresham, F. M. , & Elliott, S. N. (2008). Social Skills Improvement System: Rating Scales. Pearson Assessments. [Google Scholar]
- Griffin, J. W. , & Scherf, K. S. (2020). Does decreased visual attention to faces underlie difficulties interpreting eye gaze cues in autism? Molecular Autism, 11(1), 60. 10.1186/s13229-020-00361-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groen, W. B. , Rommelse, B. , de Wit, T. , Zwiers, M. P. , van Meerendonck, D. , van der Gaag, R. J. , & Buitelaar, J. K. (2012). Visual scanning in very young children with autism and their unaffected parents. Autism Research and Treatment, 2012, 748467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grynszpan, O. , & Nadel, J. (2014). An eye‐tracking method to reveal the link between gazing patterns and pragmatic abilities in high functioning autism spectrum disorders. Frontiers in Human Neuroscience, 8, 1067. 10.3389/fnhum.2014.01067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gur, R. C. , Sara, R. , Hagendoorn, M. , Marom, O. , Hughett, P. , Macy, L. , Turner, T. , Bajcsy, R. , Posner, A. , & Gur, R. E. (2002). A method for obtaining 3‐dimensional facial expression and its standardization for use in neurocognitive studies. Journal of Neuroscience Methods, 115, 137–143. 10.1016/s0165-0270(02)00006-7 [DOI] [PubMed] [Google Scholar]
- Hanley, M. , Riby, D. M. , Carty, C. , Melaugh McAteer, A. , Kennedy, A. , & McPhillips, M. (2015). The use of eye‐tracking to explore social difficulties in cognitively able students with autism spectrum disorder: A pilot investigation. Autism, 19(7), 868–873. 10.1177/1362361315580767 [DOI] [PubMed] [Google Scholar]
- Hanley, M. , Riby, D. M. , McCormack, T. , Carty, C. , Coyle, L. , Crozier, N. , Robinson, J. , & McPhillips, M. (2014). Attention during social interaction in children with autism: Comparison to specific language impairment, typical development, and links to social cognition. Research in Autism Spectrum Disorders, 8(7), 908–924. 10.1016/j.rasd.2014.03.020 [DOI] [Google Scholar]
- Happe, F. , & Frith, U. (2006). The weak coherence account: Detail‐focused cognitive style in autism spectrum disorders. Journal of Autism and Developmental Disorders, 36(1), 5–25. 10.1007/s10803-005-0039-0 [DOI] [PubMed] [Google Scholar]
- Harris, P. L. , Johnson, C. N. , Hutton, D. , Andrews, G. , & Cooke, T. (1989). Young children's theory of mind and emotion. Cognition and Emotion, 3(4), 379–400. 10.1080/02699938908412713 [DOI] [Google Scholar]
- Harrison, L. A. , Kats, A. , Kilroy, E. , Butera, C. , Jayashankar, A. , Keles, U. , & Aziz‐Zadeh, L. (2021). Motor and sensory features successfully decode autism spectrum disorder and combine with the original RDoC framework to boost diagnostic classification. Scientific Reports, 11(1), 7839. 10.1038/s41598-021-87455-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrop, C. , Jones, D. , Zheng, S. , Nowell, S. , Schultz, R. , & Parish‐Morris, J. (2019). Visual attention to faces in children with autism spectrum disorder: Are there sex differences? Molecular Autism, 10, 28. 10.1186/s13229-019-0276-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrop, C. , Jones, D. R. , Sasson, N. J. , Zheng, S. , Nowell, S. W. , & Parish‐Morris, J. (2020). Social and object attention is influenced by biological sex and toy gender‐congruence in children with and without autism. Autism Research, 13(5), 763–776. 10.1002/aur.2245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harstad, E. B. , Fogler, J. , Sideridis, G. , Weas, S. , Mauras, C. , & Barbaresi, W. J. (2015). Comparing diagnostic outcomes of autism spectrum disorder using DSM‐IV‐TR and DSM‐5 criteria. Journal of Autism and Developmental Disorders, 45(5), 1437–1450. 10.1007/s10803-014-2306-4 [DOI] [PubMed] [Google Scholar]
- Hellendoorn, A. , Langstraat, I. , Wijnroks, L. , Buitelaar, J. K. , van Daalen, E. , & Leseman, P. P. (2013). The relationship between atypical visual processing and social skills in young children with autism. Research in Developmental Disabilities, 35(2), 423–428. 10.1016/j.ridd.2013.11.012 [DOI] [PubMed] [Google Scholar]
- Hennessey, T. , Andari, E. , & Rainnie, D. G. (2018). RDoC‐based categorization of amygdala functions and its implications in autism. Neuroscience and Biobehavioral Reviews, 90, 115–129. 10.1016/j.neubiorev.2018.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoekstra, R. A. , Vinkhuyzen, A. A. , Wheelwright, S. , Bartels, M. , Boomsma, D. I. , Baron‐Cohen, S. , Posthuma, D. , & van der Sluis, S. (2011). The construction and validation of an abridged version of the Autism‐Spectrum Quotient (AQ‐Short). Journal of Autism and Developmental Disorders, 41(5), 589–596. 10.1007/s10803-010-1073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hus, V. , Maye, M. , Harvey, L. , Guthrie, W. , Liang, J. , & Lord, C. The adapted ADOS: Preliminary findings using a modified version of the ADOS for adults who are non‐verbal or have limited language [Poster Presentation]. International Meeting for Autism Research, San Diego. CA .
- Hutchins, T. L. , Prelock, P. A. , & Bouyea, L. B. (2014). Technical manual for the Theory of Mind Inventory and Theory of Mind Task Battery .
- Iacoboni, M. , & Mazziotta, J. C. (2007). Mirror neuron system: Basic findings and clinical applications. Annals of Neurology, 62(3), 213–218. 10.1002/ana.21198 [DOI] [PubMed] [Google Scholar]
- Ibbotson, M. , & Krekelberg, B. (2011). Visual perception and saccadic eye movements. Current Opinion in Neurobiology, 21(4), 553–558. 10.1016/j.conb.2011.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim, K. , & Sukhodolsky, D. G. (2018). RDoC and autism. In Volkmar F. (Ed.), Encyclopedia of autism spectrum disorders. Springer. 10.1007/978-1-4614-6435-8_102261-1 [DOI] [Google Scholar]
- Insel, T. , Cuthbert, B. , Garvey, M. , Heinssen, R. , Pine, D. , Quinn, K. , Sanislow, C. , & Wang, P. (2010). Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. The American Journal of Psychiatry, 167(7), 748–751. 10.1176/appi.ajp.2010.09091379 [DOI] [PubMed] [Google Scholar]
- Jeon, H. , & Lee, S. H. (2018). From neurons to social beings: Short review of the mirror neuron system research and its socio‐psychological and psychiatric implications. Clinical Psychopharmacology and Neuroscience, 16(1), 18–31. 10.9758/cpn.2018.16.1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, R. M. , Southerland, A. , Hamo, A. , Carberry, C. , Bridges, C. , Nay, S. , Stubbs, E. , Komarow, E. , Washington, C. , Rehg, J. M. , Lord, C. , & Rozga, A. (2017). Increased eye contact during conversation compared to play in children with autism. Journal of Autism and Developmental Disorders, 47(3), 607–614. 10.1007/s10803-016-2981-4 [DOI] [PubMed] [Google Scholar]
- Jones, W. , Carr, K. , & Klin, A. (2008). Absence of preferential looking to the eyes of approaching adults predicts level of social disability in 2‐year‐old toddlers with autism spectrum disorder. Archives of General Psychiatry, 65(8), 946–954. 10.1001/archpsyc.65.8.946 [DOI] [PubMed] [Google Scholar]
- Jones, W. , & Klin, A. (2013). Attention to eyes is present but in decline in 2‐6‐month‐old infants later diagnosed with autism. Nature, 504(7480), 427–431. 10.1038/nature12715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph, R. M. , Keehn, B. , Connolly, C. , Wolfe, J. M. , & Horowitz, T. S. (2009). Why is visual search superior in autism spectrum disorder? Developmental Science, 12(6), 1083–1096. 10.1111/j.1467-7687.2009.00855.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadesjo, B. , Janols, L. O. , Korkman, M. , Mickelsson, K. , Strand, G. , Trillingsgaard, A. , & Gillberg, C. (2004). The FTF (Five to Fifteen): The development of a parent questionnaire for the assessment of ADHD and comorbid conditions. European Child and Adolescent Psychiatry, 13, 3–13. 10.1007/s00787-004-3002-2 [DOI] [PubMed] [Google Scholar]
- Kaliukhovich, D. A. , Manyakov, N. V. , Bangerter, A. , Ness, S. , Skalkin, A. , Goodwin, M. S. , Dawson, G. , Hendren, R. L. , Leventhal, B. , Hudac, C. M. , Bradshaw, J. , Shic, F. , & Pandina, G. (2020). Social attention to activities in children and adults with autism spectrum disorder: Effects of context and age. Molecular Autism, 11(1), 79. 10.1186/s13229-020-00388-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamp‐Becker, I. , Albertowski, K. , Becker, J. , Ghahreman, M. , Langmann, A. , Mingebach, T. , Poustka, L. , Weber, L. , Schmidt, H. , Smidt, J. , Stehr, T. , Roessner, V. , Kucharczyk, K. , Wolff, N. , & Stroth, S. (2018). Diagnostic accuracy of the ADOS and ADOS‐2 in clinical practice. European Child and Adolescent Psychiatry, 27(9), 1193–1207. 10.1007/s00787-018-1143-y [DOI] [PubMed] [Google Scholar]
- Keehn, B. , & Joseph, R. M. (2016). Exploring what's missing: What do target absent trials reveal about autism search superiority? Journal of Autism and Developmental Disorders, 46(5), 1686–1698. 10.1007/s10803-016-2700-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keehn, B. , Kadlaskar, G. , McNally Keehn, R. , & Francis, A. L. (2019). Auditory attentional disengagement in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 49(10), 3999–4008. 10.1007/s10803-019-04111-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner, J. C. , Hatri, A. , Heekeren, H. R. , & Dziobek, I. (2011). Autistic symptomatology, face processing abilities, and eye fixation patterns. Journal of Autism and Developmental Disorders, 41(2), 158–167. 10.1007/s10803-010-1032-9 [DOI] [PubMed] [Google Scholar]
- Kirkovski, M. , Enticott, P. G. , & Fitzgerald, P. B. (2013). A review of the role of female gender in autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(11), 2584–2603. 10.1007/s10803-013-1811-1 [DOI] [PubMed] [Google Scholar]
- Kliemann, D. , Dziobek, I. , Hatri, A. , Steimke, R. , & Heekeren, H. R. (2010). Atypical reflexive gaze patterns on emotional faces in autism spectrum disorders. The Journal of Neuroscience, 30(37), 12281–12287. 10.1523/JNEUROSCI.0688-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klin, A. , Jones, W. , Schultz, R. , Volkmar, F. , & Cohen, D. (2002). Visual fixation patterns during viewing of naturalistic social situations as predictors of social competence in individuals with autism. Archives of General Psychiatry, 59, 809–816. 10.1001/archpsyc.59.9.809 [DOI] [PubMed] [Google Scholar]
- Klin, A. , Lin, D. J. , Gorrindo, P. , Ramsay, G. , & Jones, W. (2009). Two‐year‐olds with autism orient to non‐social contingencies rather than biological motion. Nature, 459(7244), 257–261. 10.1038/nature07868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koldewyn, K. , Jiang, Y. V. , Weigelt, S. , & Kanwisher, N. (2013). Global/local processing in autism: Not a disability, but a disinclination. Journal of Autism and Developmental Disorders, 43(10), 2329–2340. 10.1007/s10803-013-1777-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kou, J. , Le, J. , Fu, M. , Lan, C. , Chen, Z. , Li, Q. , Zhao, W. , Xu, L. , Becker, B. , & Kendrick, K. M. (2019). Comparison of three different eye‐tracking tasks for distinguishing autistic from typically developing children and autistic symptom severity. Autism Research, 12(10), 1529–1540. 10.1002/aur.2174 [DOI] [PubMed] [Google Scholar]
- Kuhn, G. , Benson, V. , Fletcher‐Watson, S. , Kovshoff, H. , McCormick, C. A. , Kirkby, J. , & Leekam, S. R. (2010). Eye movements affirm: Automatic overt gaze and arrow cueing for typical asults with autism spectrum disorder. Experimental Brain Research, 201, 155–165. 10.1007/s00221-009-2019-7 [DOI] [PubMed] [Google Scholar]
- Leppanen, J. , Sedgewick, F. , Treasure, J. , & Tchanturia, K. (2018). Differences in the theory of mind profiles of patients with anorexia nervosa and individuals on the autism spectrum: A meta‐analytic review. Neuroscience and Biobehavioral Reviews, 90, 146–163. 10.1016/j.neubiorev.2018.04.009 [DOI] [PubMed] [Google Scholar]
- Lindor, E. , Rinehart, N. , & Fielding, J. (2019). Distractor inhibition in autism spectrum disorder: Evidence of a selective impairment for individuals with co‐occurring motor difficulties. Journal of Autism and Developmental Disorders, 49(2), 669–682. 10.1007/s10803-018-3744-1 [DOI] [PubMed] [Google Scholar]
- Loomes, R. , Hull, L. , & Mandy, W. P. L. (2017). What is the male‐to‐female ratio in autism spectrum disorder? A systematic review and meta‐analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(6), 466–474. 10.1016/j.jaac.2017.03.013 [DOI] [PubMed] [Google Scholar]
- Lord, C. , Luyster, R. , Gotham, K. , & Guthrie, W. W. (2012). Autism Diagnostic Observation Schedule (2nd ed.). Western Psychological Services. [Google Scholar]
- Lord, C. , Risi, S. , Lambrecht, L. , Cook, E. H. , Leventhal, B. , DiLavore, P. C. , Pickles, A. , & Rutter, M. (2000). The Autism Diagnostic Observation Schedule‐Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. [PubMed] [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P. C. , & Risi, S. (1999). Autism Diagnostic Observation Schedule‐WPS (ADOS‐WPS). Western Psychological Services. [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P. C. , & Risi, S. (2002). Autism Diagnostic Observation Schedule: ADOS. Western Psychological Services. [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P. C. , & Risi, S. (2008). Autism Diagnostic Observation Schedule (2nd ed.). Western Psychological Services. [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P. C. , Risi, S. , Gotham, K. , & Bishop, S. L. (2012). Autism Diagnostic Observation Schedule (2nd ed.). Western Psychological Services. [Google Scholar]
- Lord, C. , Rutter, M. , Goode, S. , Heemsbergen, J. , Jordan, H. , Mawhood, L. , & Schopler, E. (1989). Autism Diagnostic Observation Schedule: A standardised observation of communicative and social behavior. Journal of Autism and Developmental Disorders, 19(2), 185–212. 10.1007/BF02211841 [DOI] [PubMed] [Google Scholar]
- Lord, C. , Rutter, M. , & Le Couteur, A. (1994). Autism Diagnostic Interview‐Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. 10.1007/BF02172145 [DOI] [PubMed] [Google Scholar]
- Luyster, R. , Gotham, K. , Guthrie, W. , Coffing, M. , Petrak, R. , Pierce, K. , Bishop, S. , Esler, A. , Hus, V. , Oti, R. , Richler, J. , Risi, S. , & Lord, C. (2009). The Autism Diagnostic Observation Schedule‐toddler module: A new module of a standardized diagnostic measure for autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(9), 1305–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macari, S. , Milgramm, A. , Reed, J. , Shic, F. , Powell, K. K. , Macris, D. , & Chawarska, K. (2021). Context‐specific dyadic attention vulnerabilities during the first year in infants later developing autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 166–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandy, W. (2018). The research domain criteria: A new dawn for neurodiversity research? Autism, 22(6), 642–644. 10.1177/1362361318782586 [DOI] [PubMed] [Google Scholar]
- McDonald, S. , Bornhofen, C. , Shum, D. , Long, E. , Saunders, C. , & Neulinger, K. (2006). Reliability and validity of The Awareness of Social Inference Test (TASIT): A clinical test of social perception. Disability and Rehabilitation, 28(24), 1529–1542. 10.1080/09638280600646185 [DOI] [PubMed] [Google Scholar]
- McLaughlin, C. S. , Grosman, H. E. , Guillory, S. B. , Isenstein, E. L. , Wilkinson, E. , del Pilar Trelles, M. , Halpern, D. B. , Siper, P. M. , Kolevzon, A. , Buxbaum, J. D. , Wang, A. T. , & Foss‐Feig, J. H. (2021). Reduced engagement of visual attention in children with autism spectrum disorder. Autism, 1‐10, 2064–2073. 10.1177/13623613211010072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPartland, J. , Webb, S. J. , Keehn, B. , & Dawson, G. (2011). Patterns of visual attention to faces and objects in autism spectrum disorder. Journal of Autism and Developmental Disorders, 41, 148–157. 10.1007/s10803-010-1033-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPartland, J. C. , Bernier, R. A. , Jeste, S. S. , Dawson, G. , Nelson, C. A. , Chawarska, K. , Earl, R. , Faja, S. , Johnson, S. P. , Sikich, L. , Brandt, C. A. , Dziura, J. D. , Rozenblit, L. , Hellemann, G. , Levin, A. R. , Murias, M. , Naples, A. J. , Platt, M. L. , Sabatos‐DeVito, M. , the Autism Biomarkers Consortium for Clinical Trials (2020). The autism biomarkers consortium for clinical trials (ABC‐CT): Scientific context, study design, and progress toward biomarker qualification. Frontiers in Integrative Neuroscience, 14, 16. 10.3389/fnint.2020.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modesti, P. A. , Reboldi, G. , Cappuccio, F. P. , Agyemang, C. , Remuzzi, G. , Rapi, S. , Perruolo, E. , Parati, G. , & ESH Working Group on CV Risk in Low Resource Settings . (2016). Panethnic differences in blood pressure in Europe: A systematic review and meta‐analysis. PLoS One, 11(1), e0147601. 10.1371/journal.pone.0147601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, A. , Wozniak, M. , Yousef, A. , Barnes, C. C. , Cha, D. , Courchesne, E. , & Pierce, K. (2018). The geometric preference subtype in ASD: Identifying a consistent, early‐emerging phenomenon through eye tracking. Molecular Autism, 9, 19. 10.1186/s13229-018-0202-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosconi, M. W. , Luna, B. , Kay‐Stacey, M. , Nowinski, C. V. , Rubin, L. H. , Scudder, C. , Minshew, N. , & Sweeney, J. A. (2013). Saccade adaptation abnormalities implicate dysfunction of cerebellar‐dependent learning mechanisms in autism spectrum disorders (ASD). PLoS One, 8(5), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller, N. , Baumeister, S. , Dziobek, I. , Banaschewski, T. , & Poustka, L. (2016). Validation of the Movie for the Assessment of Social Cognition in adolescents with ASD: Fixation duration and pupil dilation as predictors of performance. Journal of Autism and Developmental Disorders, 46(9), 2831–2844. 10.1007/s10803-016-2828-z [DOI] [PubMed] [Google Scholar]
- Mundy, P. (2018). A review of joint attention and social‐cognitive brain systems in typical development and autism spectrum disorder. European Journal of Neuroscience, 47(6), 497–514. 10.1111/ejn.13720 [DOI] [PubMed] [Google Scholar]
- Mundy, P. , Delgado, C. , Block, J. , & Venezia, M. (2003). Early Social Communication Scales (ESCS) .
- Murias, M. , Major, S. , Davlantis, K. , Franz, L. , Harris, A. , Rardin, B. , Sabatos‐DeVito, M. , & Dawson, G. (2018). Validation of eye‐tracking measures of social attention as a potential biomarker for autism clinical trials. Autism Research, 11(1), 166–174. 10.1002/aur.1894 [DOI] [PubMed] [Google Scholar]
- Nadig, A. , Lee, I. , Singh, L. , Bosshart, K. , & Ozonoff, S. (2010). How does the topic of conversation affect verbal exchange and eye gaze? A comparison between typical development and high‐functioning autism. Neuropsychologia, 48(9), 2730–2739. 10.1016/j.neuropsychologia.2010.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norbury, C. F. , Brock, J. , Cragg, L. , Einav, S. , Griffiths, H. , & Nation, K. (2009). Eye movement patterns are associated with communicative competence in autistic spectrum disorders. Journal of Child Psychology and Psychiatry, 50(7), 834–842. 10.1111/j.1469-7610.2009.02073.x [DOI] [PubMed] [Google Scholar]
- Ohya, T. , Morita, K. , Yamashita, Y. , Egami, C. , Ishii, Y. , Nagamitsu, S. , & Matsuishi, T. (2014). Impaired exploratory eye movements in children with Asperger's syndrome. Brain and Development, 36(3), 241–247. 10.1016/j.braindev.2013.04.005 [DOI] [PubMed] [Google Scholar]
- Parish‐Morris, J. , Chevallier, C. , Tonge, N. , Letzen, J. , Pandey, J. , & Schultz, R. T. (2013). Visual attention to dynamic faces and objects is linked to face processing skills: A combined study of children with autism and controls. Frontiers in Psychology, 4, 185. 10.3389/fpsyg.2013.00185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hrobjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallathra, A. A. , Calkins, M. E. , Parish‐Morris, J. , Maddox, B. B. , Perez, L. S. , Miller, J. , Gur, R. C. , Mandell, D. S. , Schultz, R. T. , & Brodkin, E. S. (2018). Defining behavioral components of social functioning in adults with autism spectrum disorder as targets for treatment. Autism Research, 11(3), 488–502. 10.1002/aur.1910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallathra, A. A. , Cordero, L. , Wong, K. , & Brodkin, E. S. (2019). Psychosocial interventions targeting social functioning in adults on the autism spectrum: A literature review. Current Psychiatry Reports, 21(1), 5. 10.1007/s11920-019-0989-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelphrey, K. A. , & Carter, E. J. (2008). Charting the typical and atypical development of the social brain. Development and Psychopathology, 20(4), 1081–1102. 10.1017/S0954579408000515 [DOI] [PubMed] [Google Scholar]
- Perner, J. , & Wimmer, H. (1985). “John thinks that Mary thinks that…” Attribution of second‐order beliefs by 5‐ to 10‐year old children. Journal of Experimental Child Psychology, 39, 437–471. 10.1016/0022-0965(85)90051-7 [DOI] [Google Scholar]
- Pierce, K. , Conant, D. , Hazin, R. , Stoner, R. , & Desmond, J. (2011). Preference for geometric patterns early in life as a risk factor for autism. Archives of General Psychiatry, 68(1), 101–109. 10.1001/archgenpsychiatry.2010.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, K. , Marinero, S. , Hazin, R. , McKenna, B. , Barnes, C. C. , & Malige, A. (2016). Eye tracking reveals abnormal visual preference for geometric images as an early biomarker of an autism spectrum disorder subtype associated with increased symptom severity. Biological Psychiatry, 79(8), 657–666. 10.1016/j.biopsych.2015.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plesa‐Skwerer, D. , Brukilacchio, B. , Chu, A. , Eggleston, B. , Meyer, S. , & Tager‐Flusberg, H. (2019). Do minimally verbal and verbally fluent individuals with autism spectrum disorder differ in their viewing patterns of dynamic social scenes? Autism, 23, 2131–2144. 10.1177/1362361319845563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2017). R: A language and environment for statistical computing, Vienna, Austria. https://www.R-project.org/.
- Riby, D. , Hancock, P. J. B. , Jones, N. , & Hanley, M. (2013). Spontaneous and cued gaze‐following in autism and Williams syndrome. Journal of Neurodevelopmental Disorders, 5, 13. 10.1186/1866-1955-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riby, D. , & Hancock, P. J. B. (2009a). Looking at movies and cartoons: Eye‐tracking evidence from Williams syndrome and autism. Journal of Intellectual Disability Research, 53(2), 169–181. [DOI] [PubMed] [Google Scholar]
- Riby, D. M. , & Hancock, P. J. B. (2009b). Do faces capture the attention of individuals with Williams syndrome or autism? Evidence from tracking eye movements. Journal of Autism and Developmental Disorders, 39(3), 421–431. 10.1007/s10803-008-0641-z [DOI] [PubMed] [Google Scholar]
- Rigby, S. N. , Stoesz, B. M. , & Jakobson, L. S. (2016). Gaze patterns during scene processing in typical adults and adults with autism spectrum disorders. Research in Autism Spectrum Disorders, 25, 24–36. 10.1016/j.rasd.2016.01.012 [DOI] [Google Scholar]
- Rice, K. , Moriuchi, J. M. , Jones, W. , & Klin, A. (2012). Parsing heterogeneity in autism spectrum disorders: Visual scanning of dynamic social scenes in school‐aged children. Journal of the American Academy of Child & Adolescent Psychiatry, 51(3), 238–248. 10.1016/j.jaac.2011.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzolatti, G. , Fogassi, L. , & Gallese, V. (2001). Neurophysiological mechanisms underlying the understanding and imitation of action. Nature Reviews Neuroscience, 2, 661–670. 10.1038/35090060 [DOI] [PubMed] [Google Scholar]
- Rutter, M. , Bailey, A. , & Lord, C. (2003). SCQ: Social Communication Questionnaire. Western Psychological Services; Manual for the SCQ. [Google Scholar]
- Rutter, M. , Le Couteur, A. , & Lord, C. (2003). Autism Diagnostic Interview‐Revised. Western Psychological Services. [Google Scholar]
- Sasson, N. , Tsuchiya, N. , Hurley, R. , Couture, S. M. , Penn, D. L. , Adolphs, R. , & Piven, J. (2007). Orienting to social stimuli differentiates social cognitive impairment in autism and schizophrenia. Neuropsychologia, 45(11), 2580–2588. 10.1016/j.neuropsychologia.2007.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasson, N. J. , Pinkham, A. E. , Weittenhiller, L. P. , Faso, D. J. , & Simpson, C. (2016). Context effects on facial affect recognition in schizophrenia and autism: Behavioral and eye‐tracking evidence. Schizophrenia Bulletin, 42(3), 675–683. 10.1093/schbul/sbv176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasson, N. J. , Turner‐Brown, L. M. , Holtzclaw, T. N. , Lam, K. S. , & Bodfish, J. W. (2008). Children with autism demonstrate circumscribed attention during passive viewing of complex social and nonsocial picture arrays. Autism Research, 1(1), 31–42. 10.1002/aur.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer, A. C. , Williamson, P. , & Young, R. L. (2012). Can gaze avoidance explain why individuals with Asperger's syndrome can't recognise emotions from facial expressions? Journal of Autism and Developmental Disorders, 42(4), 606–618. 10.1007/s10803-011-1283-0 [DOI] [PubMed] [Google Scholar]
- Schmitt, L. M. , Cook, E. H. , Sweeney, J. A. , & Mosconi, M. W. (2014). Saccadic eye movement abnormalities in autism spectrum disorder indicate dysfunctions in cerebellum and brainstem. Molecular Autism, 5(1), 47. 10.1186/2040-2392-5-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schopler, E. , Reichler, R. , & Rocher‐Renner, B. (1998). Childhood Autism Rating Scale. Western Psychological Services. [Google Scholar]
- Schurz, M. , Radua, J. , Aichhorn, M. , Richlan, F. , & Perner, J. (2014). Fractionating theory of mind: A meta‐analysis of functional brain imaging studies. Neuroscience and Biobehavioral Reviews, 42, 9–34. 10.1016/j.neubiorev.2014.01.009 [DOI] [PubMed] [Google Scholar]
- Shaffer, R. C. , Pedapati, E. V. , Shic, F. , Gaietto, K. , Bowers, K. , Wink, L. K. , & Erickson, C. A. (2017). Brief report: Diminished gaze preference for dynamic social interaction scenes in youth with autism spectrum disorders. Journal of Autism and Developmental Disorders, 47(2), 506–513. 10.1007/s10803-016-2975-2 [DOI] [PubMed] [Google Scholar]
- Shic, F. , Bradshaw, J. , Klin, A. , Scassellati, B. , & Chawarska, K. (2011). Limited activity monitoring in toddlers with autism spectrum disorder. Brain Research, 1380, 246–254. 10.1016/j.brainres.2010.11.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shic, F. , Wang, Q. , Macari, S. L. , & Chawarska, K. (2020). The role of limited salience of speech in selective attention to faces in toddlers with autism spectrum disorders. Journal of Child Psychology and Psychiatry, 61(4), 459–469. 10.1111/jcpp.13118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow, J. , Ingeholm, J. E. , Levy, I. F. , Caravella, R. A. , Case, L. K. , Wallace, G. L. , & Martin, A. (2011). Impaired visual scanning and memory for faces in high‐functioning autism spectrum disorders: It's not just the eyes. Journal of the International Neuropsychological Society, 17(6), 1021–1029. 10.1017/S1355617711000981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, Y. , Nie, T. , Shi, W. , Zhao, X. , & Yang, Y. (2019). Empathy impairment in individuals with autism spectrum conditions from a multidimensional perspective: A meta‐analysis. Frontiers in Psychology, 10, 1902. 10.3389/fpsyg.2019.01902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speer, L. L. , Cook, A. E. , McMahon, W. M. , & Clark, E. (2007). Face processing in children with autism: Effects of stimulus contents and type. Autism, 11(3), 265–277. 10.1177/1362361307076925 [DOI] [PubMed] [Google Scholar]
- Stanley‐Cary, C. , Rinehart, N. , Tonge, B. , White, O. , & Fielding, J. (2011). Greater disruption to control of voluntary saccades in autistic disorder than Asperger's disorder: Evidence for greater cerebellar involvement in autism? Cerebellum, 10(1), 70–80. 10.1007/s12311-010-0229-y [DOI] [PubMed] [Google Scholar]
- Sterling, L. , Dawson, G. , Webb, S. , Murias, M. , Munson, J. , Panagiotides, H. , & Aylward, E. (2008). The role of face familiarity in eye tracking of faces by individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38(9), 1666–1675. 10.1007/s10803-008-0550-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner, E. , Leonard, H. C. , & Hill, E. L. (2018). Comparing attention to socially relevant stimuli in autism spectrum disorder and developmental coordination disorder. Journal of Abnormal Child Psychology, 46(8), 1717–1729. 10.1007/s10802-017-0393-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson, M. R. , & Siller, M. (2013). Patterns of gaze behavior during an eye‐tracking measure of joint attention in typically developing children and children with autism spectrum disorder. Research in Autism Spectrum Disorders, 7(9), 1087–1096. 10.1016/j.rasd.2013.05.007 [DOI] [Google Scholar]
- Tanaka, J. W. , Wolf, J. M. , Klaiman, C. , Koenig, K. , Cockburn, J. , Herlihy, L. , Brown, C. , Stahl, S. S. , South, M. , McPartland, J. C. , Kaiser, M. D. , & Schultz, R. T. (2012). The perception and identification of facial emotions in individuals with autism spectrum disorders using the Let's Face It! Emotion Skills Battery. Journal of Child Psychology and Psychiatry, 53(12), 1259–1267. 10.1111/j.1469-7610.2012.02571.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, J. , Falkmer, M. , Horlin, C. , Tan, T. , Vaz, S. , Falkmer, T. , & Falkmer, T. (2015). Face recognition and visual search strategies in autism spectrum disorders: Amending and extending a recent review by Weigelt et al. PLoS One, 10(8), e0134439. 10.1371/journal.pone.0134439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenenbaum, E. J. , Major, S. , Carpenter, K. L. H. , Howard, J. , Murias, M. , & Dawson, G. (2021). Distance from typical scan path when viewing complex stimuli in children with autism spectrum disorder and its association with behavior. Journal of Autism and Developmental Disorders, 51, 3492–3505. 10.1007/s10803-020-04812-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorup, E. , Kleberg, J. L. , & Falck‐Ytter, T. (2017). Gaze following in children with autism: Do high interest objects boost performance? Journal of Autism and Developmental Disorders, 47(3), 626–635. 10.1007/s10803-016-2955-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thye, M. D. , Bednarz, H. M. , Herringshaw, A. J. , Sartin, E. B. , & Kana, R. K. (2018). The impact of atypical sensory processing on social impairments in autism spectrum disorder. Developmental Cognitive Neuroscience, 29, 151–167. 10.1016/j.dcn.2017.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschida, J. E. , & Yerys, B. E. (2020). A systematic review of the positive valence system in autism spectrum disorder. Neuropsychology Review, 31(1), 58–88. 10.1007/s11065-020-09459-z [DOI] [PubMed] [Google Scholar]
- Tubio‐Fungueirino, M. , Cruz, S. , Sampaio, A. , Carracedo, A. , & Fernandez‐Prieto, M. (2020). Social camouflaging in females with autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders, 51, 2190–2199. 10.1007/s10803-020-04695-x [DOI] [PubMed] [Google Scholar]
- Uljarevic, M. , & Hamilton, A. (2013). Recognition of emotions in autism: A formal meta‐analysis. Journal of Autism and Developmental Disorders, 43(7), 1517–1526. 10.1007/s10803-012-1695-5 [DOI] [PubMed] [Google Scholar]
- Unruh, K. E. , Sasson, N. J. , Shafer, R. L. , Whitten, A. , Miller, S. J. , Turner‐Brown, L. , & Bodfish, J. W. (2016). Social orienting and attention is influenced by the presence of competing nonsocial information in adolescents with autism. Frontiers in Neuroscience, 10, 586. 10.3389/fnins.2016.00586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Hallen, R. , Evers, K. , Brewaeys, K. , Van den Noortgate, W. , & Wagemans, J. (2015). Global processing takes time: A meta‐analysis on local‐global visual processing in ASD. Psychological Bulletin, 141(3), 549–573. 10.1037/bul0000004 [DOI] [PubMed] [Google Scholar]
- Van Eylen, L. , Boets, B. , Steyaert, J. , Wagemans, J. , & Noens, I. (2018). Local and global visual processing in autism spectrum disorders: Influence of task and sample characteristics and relation to symptom severity. Journal of Autism and Developmental Disorders, 48(4), 1359–1381. 10.1007/s10803-015-2526-2 [DOI] [PubMed] [Google Scholar]
- Vivanti, G. , Trembath, D. , & Dissanayake, C. (2014). Atypical monitoring and responsiveness to goal‐directed gaze in autism spectrum disorder. Experimental Brain Research, 232(2), 695–701. 10.1007/s00221-013-3777-9 [DOI] [PubMed] [Google Scholar]
- Volkmar, F. R. , Cicchetti, D. V. , Dykens, E. , Sparrow, S. S. , Leckman, J. F. , & Cohen, D. J. (1988). An evaluation of the Autism Behaviour Checklist. Journal of Autism and Developmental Disorders, 18(1), 81–97. 10.1007/BF02211820 [DOI] [PubMed] [Google Scholar]
- Vrancken, L. , Germeys, F. , & Verfaillie, K. (2017). Holistic integration of gaze cues in visual face and body perception: Evidence from the composite design. Journal of Vision, 17(1), 24. 10.1167/17.1.24 [DOI] [PubMed] [Google Scholar]
- Wang, Q. , Campbell, D. J. , Macari, S. L. , Chawarska, K. , & Shic, F. (2018). Operationalizing atypical gaze in toddlers with autism spectrum disorders: A cohesion‐based approach. Molecular Autism, 9, 25. 10.1186/s13229-018-0211-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X. , Chen, L. , Liu, P. , Polk, R. J. , & Feng, T. (2020). Orientation to and processing of social stimuli under normal and competitive conditions in children with autism spectrum disorder. Research in Autism Spectrum Disorders, 78, 101614. 10.1016/j.rasd.2020.101614 [DOI] [Google Scholar]
- White, S. W. , Maddox, B. B. , & Panneton, R. K. (2015). Fear of negative evaluation influences eye gaze in adolescents with autism spectrum disorder: A pilot study. Journal of Autism and Developmental Disorders, 45(11), 3446–3457. 10.1007/s10803-014-2349-6 [DOI] [PubMed] [Google Scholar]
- Wieckowski, A. T. , & White, S. W. (2016). Eye‐gaze analysis of facial emotion recognition and expression in adolescents with ASD. Journal of Clinical Child & Adolescent Psychology, 46(1), 110–124. 10.1080/15374416.2016.1204924 [DOI] [PubMed] [Google Scholar]
- Wilson, C. E. , Palermo, R. , & Brock, J. (2012). Visual scan paths and recognition of facial identity in autism spectrum disorder and typical development. PLoS One, 7(5), e37681. 10.1371/journal.pone.0037681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wimmer, H. , & Hartl, M. (1991). Against the Cartesian view on mind: Young children's difficulty with false beliefs. British Journal of Developmental Psychology, 9, 125–138. 10.1111/j.2044-835X.1991.tb00866.x [DOI] [Google Scholar]
- Wimmer, H. , & Perner, J. (1983). Beliefs about beliefs: Representation and constraining function of wrong beliefs in young children's understanding of deception. Cognition, 13, 103–128. 10.1016/0010-0277(83)90004-5 [DOI] [PubMed] [Google Scholar]
- Wolf, J. M. , Tanaka, J. W. , Klaiman, C. , Cockburn, J. , Herlihy, L. , Brown, C. , South, M. , McPartland, J. , Kaiser, M. D. , Phillips, R. , & Schultz, R. T. (2008). Specific impairment of face‐processing abilities in children with autism spectrum disorder using the Let's Face It! Skills Battery. Autism Research, 1(6), 329–340. 10.1002/aur.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wollenberg, L. , Hanning, N. M. , & Deubel, H. (2020). Visual attention and eye movement control during oculomotor competition. Journal of Vision, 20(9), 16. 10.1167/jov.20.9.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xavier, J. , Vignaud, V. , Ruggiero, R. , Bodeau, N. , Cohen, D. , & Chaby, L. (2015). A multidimensional approach to the study of emotion recognition in autism spectrum disorders. Frontiers in Psychology, 6, 1954. 10.3389/fpsyg.2015.01954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalla, T. , Seassau, M. , Cazalis, F. , Gras, D. , & Leboyer, M. (2016). Saccadic eye movements in adults with high‐functioning autism spectrum disorder. Autism, 22, 195–204. 10.1177/1362361316667057 [DOI] [PubMed] [Google Scholar]
- Zamzow, R. M. , Christ, S. E. , Saklayen, S. S. , Moffitt, A. J. , Bodner, K. E. , Higgins, K. F. , & Beversdorf, D. Q. (2014). Effect of propranolol on facial scanning in autism spectrum disorder: A preliminary investigation. Journal of Clinical and Experimental Neuropsychology, 36(4), 431–445. 10.1080/13803395.2014.904844 [DOI] [PubMed] [Google Scholar]
- Zanon, M. , Novembre, G. , Zangrando, N. , Chittaro, L. , & Silani, G. (2014). Brain activity and prosocial behavior in a simulated life‐threatening situation. NeuroImage, 98, 134–146. 10.1016/j.neuroimage.2014.04.053 [DOI] [PubMed] [Google Scholar]
- Zantinge, G. , van Rijn, S. , Stockmann, L. , & Swaab, H. (2017). Psychophysiological responses to emotions of others in young children with autism spectrum disorders: Correlates of social functioning. Autism Research, 10(9), 1499–1509. 10.1002/aur.1794 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


