Abstract
Background
Perinatal quality improvement lacks valid tools to measure adverse hospital experiences disproportionately impacting Black mothers and birthing people. Measuring and mitigating harm requires using a framework that centers the lived experiences of Black birthing people in evaluating inequitable care, namely, obstetric racism. We sought to develop a valid patient‐reported experience measure (PREM) of Obstetric Racism© in hospital‐based intrapartum care designed for, by, and with Black women as patient, community, and content experts.
Methods
PROMIS© instrument development standards adapted with cultural rigor methodology. Phase 1 included item pool generation, modified Delphi method, and cognitive interviews. Phase 2 evaluated the item pool using factor analysis and item response theory.
Results
Items were identified or written to cover 7 previously identified theoretical domains. 806 Black mothers and birthing people completed the pilot test. Factor analysis concluded a 3 factor structure with good fit indices (CFI = 0.931‐0.977, RMSEA = 0.087‐0.10, R 2 > .3, residual correlation < 0.15). All items in each factor fit the IRT model and were able to be calibrated. Factor 1, “Humanity,” had 31 items measuring experiences of safety and accountability, autonomy, communication, and empathy. A 12‐item short form was created to ease respondent burden. Factor 2, “Racism,” had 12 items measuring experiences of neglect and mistreatment. Factor 3, “Kinship,” had 7 items measuring hospital denial and disruption of relationships between Black mothers and their child or support system.
Conclusions
The PREM‐OB Scale™ suite is a valid tool to characterize and quantify obstetric racism for use in perinatal improvement initiatives.
Keywords: black mothers, obstetric racism, psychometrics, quality improvement
1. INTRODUCTION
Perinatal quality improvement (PQI) and implementation studies tend to focus on the disparate rates of adverse pregnancy‐related outcomes between Black mothers and birthing people and non‐Black mothers and birthing populations, namely, differences in outcomes whereby race, and not racism, is the risk factor. 1 In contrast, a growing body of knowledge, particularly generated and disseminated by Black women scholars, continues to illuminate the association between perinatal health inequities and historical and contemporary racism. 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 Unfortunately, translating this knowledge into meaningful change is challenging. A growing body of work highlights the failure of leading scholars and journals, 1 , 17 , 18 funders, 7 and large‐scale quality improvement organizations 19 , 20 to earnestly interrogate racism as a critical driver of health inequities. The consequences of this failure can lead to research with statistically significant findings without culturally relevant or translatable utility to the research priorities identified by the impacted community. 7 , 21 This gap between expressed intentions and actual change in the practice of knowledge generation highlights a need for new methods and tools to undertake quality improvement science, specifically, using theories, frameworks, and methodologies from the social sciences and public health focused on advancing race and gender equity and social justice, specifically for, by, and with Black mothers and birthing people.
Using cultural rigor during knowledge generation is one method to combat inequities in health services provision, evaluation, and training (Figure 1). When applied as a body of standard practices for research (ie, a research praxis), cultural rigor mandates that each step of the process operationalize (1) Black feminism, (2) reproductive justice, (3) research justice, and (4) use participatory data development and dissemination methods. 7 For clarity, a glossary of important terms has been included in Appendix S1. As applied to this study, achieving cultural rigor included naming obstetric racism as the explanatory framework to illuminate experiences of reproductive and perinatal care of Black women and people within the health care system. 18 Davis’ explanatory framework of obstetric racism is based on decades of ethnographic work and is defined as the demonstration of medical racism and obstetric violence in hospital‐based service provision. 22 Applying cultural rigor catalyzes a transfer of power from the researchers to those being studied, by naming the phenomenon under examination through the lived experiences, intellectual thoughts and political activism of Black women as patient, community, and content experts. 19 Consequently, cultural rigor acknowledges, accepts, and amplifies Black women as knowledge guardians, generators, incubators, accelerators, and disseminators. 19 To address the gaps in current PQI methodology that contribute to the dissemination of problematic stereotypes, stories, and scripts about Blackness, Black bodies, and Black people, we illustrate and argue for the application of cultural rigor in each step of survey design and validation as a means to ensure the quality, applicability, and relevance of the resulting product.
FIGURE 1.
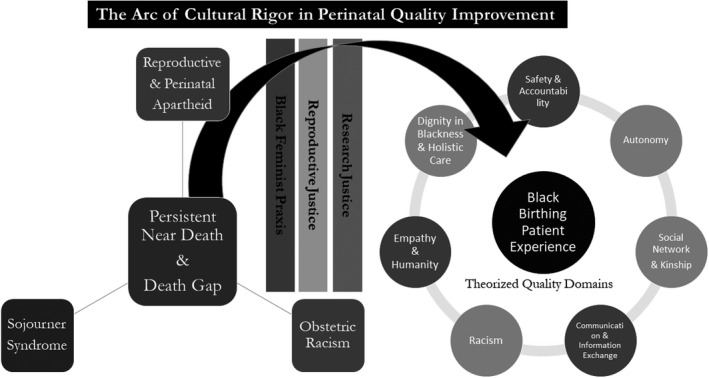
The arc of cultural rigor in perinatal quality improvement and theorized domains of SACRED birth
Measurement tools in PQI have typically relied upon outcomes data obtainable from large administrative databases, birth certificate data, or medical record abstraction 23 ; reinforcing individual‐level characteristics as the drivers of inequitable care, outcomes, and experiences during and after childbirth 18 , 24 ; and perpetuating mother blame narratives, particularly among Black mothers and birthing communities. 25 Maintaining fidelity to cultural rigor in PQI requires nuanced knowledge and insight into the power relations, differentials, and dynamics among hospitals, Black mothers and birthing people, and Black communities during service provision and evaluation. Measurement tools developed without first forming dignified and sustainable partnerships with Black women as patient, community, and content experts in driving innovation and transformation in measure development and data analytics fail to meet existing calls for accountability in research. 17
To fill this void, this study aimed to develop a psychometrically sound, culturally rigorous measure of patient‐reported experiences of obstetric racism during hospital labor, birth, and postpartum. Particularly, this measure would translate Davis' explanatory framework of obstetric racism 22 into examples of harmful clinical practices and policies using cultural rigor methodology, as defined and refined for, by, and with Black women as patient, community, and content experts.
2. MATERIALS AND METHODS
This study operationalized Black feminist praxis, reproductive justice, and research justice through the four modalities of cultural rigor: social movement, analytic framework, praxis, and vision. 7 , 26 , 27 (Figures 1 and 2) Typical survey development processes were adapted by a Black women‐led transdisciplinary and transgenerational team of Black women scholars, Black women‐led community organizations, non‐Black health services researchers, and Black mothers and birthing people.
FIGURE 2.
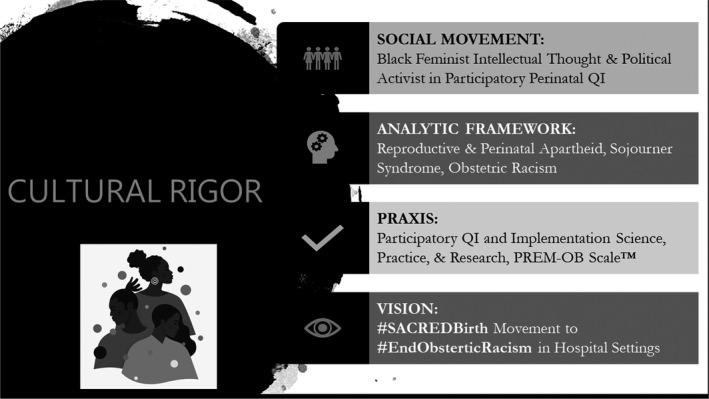
The four modalities of cultural rigor
Our measure was developed following the Patient‐Reported Outcome Measurement Information System (PROMIS®) instrument development and validation scientific standards, 28 in which rigorous mixed‐methods approaches are recommended to develop person‐centered instruments. Specifically, qualitative approaches were used to define the priority concept and conceptual model; compile and/or compose individual items; and subsequently construct an (or more) item pool(s). 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 Quantitative approaches were then used to evaluate psychometric properties of the item bank(s).
2.1. Qualitative methods—item pool generation
2.1.1. Definition of the key concept and conceptual model
The study team provided significant content expertise DD and KS, whereas multiple research librarians were consulted to conduct a comprehensive literature search using keywords relevant to reproductive justice, birth equity, Black feminism, Obstetric Racism, and patient‐reported birth experiences. (Appendix S2) We then applied a Birthing Cultural Rigor™ screening protocol (Appendix S3) consisting of a 20‐item checklist to determine whether the study or instrument maintained fidelity to the four modalities of cultural rigor.
The conceptual model and theoretical domains were further developed based on qualitative analysis of focus groups with Black mothers and birthing people from Oakland and Los Angeles, California, with a prior live hospital birth. Details of these methods and analyses have been previously described. 20 The focus groups and analysis were approved under expedited IRB review, by the Stanford University Institutional Review Board (IRB) March 2019.
Key concept and theoretical domains
The resulting key concept, entitled SACRED birth, was based on the scholarship of three Black feminist scholars: (1) Mullings' Sojourner syndrome 44 which characterizes the oppression, resistance, and resilience of Black women and people within various structures, sectors, and systems in society before and during pregnancy and childbirth; (2) Davis' existing explanatory framework of Obstetric Racism, which is the demonstration of medical racism and obstetric violence in hospital‐based service provision 22 , 27 ; and (3) Scott's adaptation of Medical Apartheid, 45 called Reproductive & Perinatal Apartheid, 15 which describes a system of unequal but separate experiences and outcomes in health care service provision and policies rooted in a hierarchy of power and human value on both skin color and anatomy. The theoretical patient‐identified quality care domains included: (1) Safety & Accountability, (2) Autonomy, (3) Communication & Information Exchange, (4) Racism, (5) Empathy & Humanity, (6) Dignity in Blackness & Holistic Care, and (7) Kinship (SACRED). 18 , 20 , 46 (Figure 1) Details of key concept and theoretical domain development have been previously described.
2.1.2. Construction of an item pool
Draft an item pool. Existing measures of patient‐reported birth experiences were identified during the above step a. These measures were evaluated for face validity, use among Black birthing people in the United States, and scholarly involvement of Black women. Items were considered for inclusion if they addressed any of the seven theorized SACRED domains. Permission from authors of existing items was obtained. New items were written to cover domains with a paucity of mapped existing items.
Modified Delphi Process: A list of subject matter experts in reproductive health, rights, and justice, birth justice, health services, disparities, and equity research was generated by the study team for focused recruitment via individual emails. Snowball technique was used to identify additional experts. Three rounds of iterative review and prioritization were completed:
First, subjects were asked to review each item and indicate if that item should be kept as is, altered, or eliminated. Items that received a simple majority to keep were kept in for the next round. Items marked for alteration were revised by the study team and included in the next round.
The second round asked participants to prioritize items from most to least important to include in domain‐specific groupings.
The final round was a live virtual meeting to review the highest‐ranked items by the study team to determine adequate coverage of each domain and make revisions where indicated by subject matter experts.
This part of the study was approved by the NorthShore University HealthSystem IRB on November 27, 2019.
Community checking: Focus groups were conducted with 11 Black mothers from Oakland who participated in the 2019 focus group. Participants were identified in partnership with a Black women‐led community research partner who facilitated the focus groups in 2019. Participants reviewed and revised domain names, meanings, and measures to ensure alignment and accuracy between lived experiences and theorized domains.
Cognitive interviews were conducted with 25 postpartum Black patients in 2020. Participants were identified using social media and in partnership with fifteen Black women‐led community accountability research partners. An interview guide was developed based on Cognitive Interviewing 47 , 48 standards and elicited feedback from participants using think aloud and verbal prompts to comment on item length, wording, relevance, clarity, and their thought processes as they reviewed up to 10 items each. In addition, participants commented on any content deficiencies in the draft item pool for their reviewed domain.
2.1.3. Quantitative components—evaluation of psychometric properties of item bank(s)
Participants
Black mothers and birthing people were recruited from across the United States using online social media, self‐referral, community‐based word‐of‐mouth and dissemination strategies situated within Black virtual and physical communities. The study team partnered with fifteen Black women‐led community‐based organizations to do population‐specific recruitment, whereas health care organization partners and individual providers were also leveraged to recruit potential participants. Potential participants completed an online self‐screen. Eligibility criteria included self‐identifying as a Black or African American woman or person, aged 18 years or older, who had given birth to a live newborn in a hospital in the United States from January 1, 2020 to December 31, 2020, with access to the Internet for participation in all study activities during mandatory social distancing, with abilities to read, speak, and write in English. Eligible candidates submitted the signed electronic consent to the study team if they agreed to participate. Upon receipt of the completed consent, research staff conducted a series of online and phone verification calls prefaced by texts as part of quality assurance. Upon online and phone verification, the study candidate completed the online enrollment and final survey. All participants who completed the survey received a $100 Visa gift card. This part of the study was approved by the University of California San Francisco IRB on July 13, 2020.
2.2. Statistical analysis
We first evaluated dimensionality of the item pool by using factor analyses. As the item pool was developed according to the hypothesized theoretical domains, confirmatory factor analysis (CFA), including the conceptual model‐driven bi‐factor analysis, was used. Item sets were considered unidimensional, with their items retained in the item pool when the following criteria were met: comparative fit index (CFI) >0.9; root mean square error of approximation (RMSEA) <0.1; R 2 > .3; residual correlations <.20. 49 Item inclusion/exclusion was determined using CFA, correlational analysis, and item content to ensure resulted measures were not only holding psychometric merit but also conceptually reasonable.
Unidimensional item sets were then analyzed by using item response theory (IRT). We modeled responses to candidate item sets using the graded response model (GRM). We defined item misfit as occurring when the item fit test ratio of chi‐squared to degrees of freedom was >3.0. Item parameters were used to estimate item information functions at both the level of individual items and the level of the entire measure, to characterize the precision of items and the overall scale across the measurement continuum, which was used as a reference to identify items to be included in the final brief version of the measure. For criterion validity, we examined the association between the IRT scaled scores and representative nonretained PQI items with strong face validity (categorized as 3—Strongly agree/Agree, 2—Neutral, 1—Disagree/Strongly disagree) using cumulative proportional odds (PO) logistic regression. For the variables violating proportional odds assumption, we used non‐PO logistic regression models to get separate parameter estimates for each response level. If the ORs from non‐PO model were within the 95% confidence interval of PO model, the cumulative OR provided by PO model were reported as an average estimate of the predictor effect. We employed Mplus v7.4 to conduct CFA modeling analyses, IRTPRO v3.1 (Vector Psychometric Group) for IRT‐related analysis, and SAS version 9.4 (SAS Institute Inc) for other statistical analyses.
3. RESULTS
3.1. Item pool generalization
A total of 1068 items were identified for consideration from existing sources. From these, 134 were selected and 21 were newly written to cover the 7 theoretical domains. After the modified Delphi process, 75 items remained. Cognitive interviews did not result in elimination of any items; however, several were revised for clarity and 6 new items were written to cover possible gaps raised during the cognitive interviews. The final item pool to be tested in the following phase contained 81 items.
3.2. Evaluation of the psychometric properties of the item pool
3.2.1. Participants
Eight hundred and fifteen Black‐identifying mothers and birthing people completed the item pool out of 1294 who completed the self‐screen and were deemed eligible. Nine individuals were excluded from analyses: 7 were found to be ineligible (ie, did not identify as Black or African American) and 2 completed <50% of the item pool. Participant characteristics are shown in Table 1. The sample was similar to the Black birthing population in the United States, with increased representation from individuals with a higher level of education. 50
TABLE 1.
Clinical and demographic characteristics of pilot test participants
| US Black Birthing Population (2019) a | Pilot Test Sample | Median IRT Scale Score | ||||||
|---|---|---|---|---|---|---|---|---|
| N = 3863 | N = 806 | Racism | P b | Kinship | P b | Humanity | P b | |
| Maternal age | n (%) | n (%) | .765 | 0.998 | .968 | |||
| 15‐19 years | 171 (4.4) | 20 (3.4) | −0.52 | −0.04 | 0.06 | |||
| 20‐34 years | 2796 (72.4) | 424 (73.1) | −0.03 | −0.04 | 0.08 | |||
| 35‐50 years | 896 (23.2) | 136 (23.4) | −0.03 | −0.04 | 0.11 | |||
| Missing | 226 | |||||||
| BMI | .591 | 0.366 | .775 | |||||
| <30 | NA | 478 (60.2) | −0.03 | −0.04 | 0.1 | |||
| ≥30 | NA | 316 (39.8) | 0.07 | 0.06 | 0.11 | |||
| Missing | 11 | |||||||
| Household income | <.0001 | 0.001 | .001 | |||||
| <$50 000 | 1783 (50.4) | 468 (61.9) | 0.16 | 0.16 | 0.24 | |||
| $50 000 to $75 000 | 582 (16.5) | 108 (14.3) | 0.2 | 0.16 | 0.12 | |||
| >$75 000 | 1171 (33.1) | 180 (23.8) | −0.28 | −0.14 | −0.09 | |||
| Missing | 50 | |||||||
| Educational attainment | .001 | 0.006 | .001 | |||||
| HS Diploma/GED or less | 1575 (40.8) | 172 (21.4) | −0.28 | −0.25 | −0.06 | |||
| Some college, associates | 1440 (37.3) | 289 (36.0) | 0.24 | 0.16 | 0.38 | |||
| Bachelor's degree | 541 (14.0) | 180 (22.4) | −0.14 | −0.09 | −0.08 | |||
| Master's/Doctorate/Professional | 307 (8.0) | 162 (20.2) | 0.02 | 0.06 | 0.12 | |||
| Missing | 3 | |||||||
| Relationship status | .133 | 0.917 | .497 | |||||
| Married | 1453 (37.6) | 318 (39.7) | −0.14 | −0.04 | 0.05 | |||
| Single | 2410 (62.4) | 483 (60.3) | 0.07 | 0.06 | 0.16 | |||
| Missing | 5 | |||||||
| Cohabitation status | .349 | 0.618 | .793 | |||||
| Yes | NA | 498 (62.2) | −0.03 | −0.04 | 0.08 | |||
| No | NA | 303 (37.8) | 0.07 | 0.06 | 0.16 | |||
| Missing | 5 | |||||||
| Birthing with partner/support person | .001 | 0.0001 | .007 | |||||
| Yes | NA | 720 (89.3) | −0.03 | −0.04 | 0.05 | |||
| No | NA | 86 (10.7) | 0.32 | 0.45 | 0.47 | |||
| Type of delivery | .303 | 0.246 | .474 | |||||
| Vaginal birth | NA | 499 (62.3) | −0.03 | −0.04 | 0.05 | |||
| Cesarean birth | NA | 302 (37.7) | 0.16 | 0.06 | 0.15 | |||
| Missing | 5 | |||||||
Abbreviations: GED, General Educational Development; HS, High School; IRT, Item Response Theory.
Source: United States Census Bureau, Beta. Custom Table, 2019.https://data.census.gov/mdat/#/search?ds=ACSPUMS1Y2019&vv=*AGEP(16:50)&cv=FER(1),RACBLK(1)&wt=PWGTP
P‐values to compare median IRT scaled scores are derived from Wilcoxon rank sum test (for dichotomous variables) or Kruskal–Wallis test (for variables with >2 categories). P‐values <.05 were considered statistically significant.
3.2.2. Analysis results
A series of descriptive and factor analyses led to removing 24 items because of low Spearman's rho with the rest of the item pool, low R 2, high residual correlations, or inappropriate content. The remaining 57 items formed three unidimensional measures (0 existing items as‐is, 34 significantly modified existing items, 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 and 9 de novo items). Results of a bi‐factor analysis support the sufficient unidimensionality of the “Humanity” measure, in which the general factor was defined as “humanity” and four local factors (or subdomains) were as follows: safety and accountability, autonomy, communication and information exchange, and empathy. All fit indices met the criteria: CFI = 0.952, RMSEA = 0.085, all R 2 > .3, and residual correlations <.2. All items had higher loadings to the general factor (ie, Humanity) than to the associated local factor, supporting sufficient unidimensionality of all 31 items. All 31 items fit the IRT model and were calibrated together to the same measurement continuum. Cronbach's Alpha of the Humanity measure was 0.96. A 14‐item short‐form was then created to ease respondent burden. End‐users can construct customized short‐forms to meet their specific needs and scores from these forms, including the original long‐form, which are comparable since all items are from the same IRT‐calibrated measure. Factor 2, “Racism,” had 12 items measuring experiences of neglect and mistreatment based on anti‐Black racism and anti‐Black gendered racism. All fit indices met the criteria: CFI = 0.977, RMSEA = 0.087, all R 2 > .3 and residual correlations <.2. All 12 items fit the IRT model and were calibrated together to the same measurement continuum. Cronbach's Alpha of Racism was 0.93. Factor 3, “Kinship,” had 9 items measuring hospital recognition and involvement of social relationships between birthing people and their child or support system in service provision. All fit indices met the criteria: CFI = 0.975, RMSEA = 0.081, all R 2 > .3 and residual correlations <.2. All 9 items fit the IRT model and were calibrated together to the same measurement continuum. Cronbach's Alpha of the Kinship was 0.86. (Table 2) Each of the resulting scales was evaluated for fit with the original concepts identified by focus groups, and a refined scale definition was created.
TABLE 2.
Individual scale properties of the PREM‐OB Scale™ Suite
| Scale | Number of items | Cronbach alpha | Raw score | IRT scaled scores | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | |||
| Racism | 12 | 0.93 | 21.9 | 10.3 | 12 | 60 | 0 | 0.92 | −1.37 | 3.06 |
| Kinship | 9 | 0.86 | 23.4 | 8.1 | 9 | 45 | 0 | 0.92 | −2.15 | 2.71 |
| Humanity | 31 | 0.96 | 74.2 | 27.4 | 31 | 155 | 0 | 0.94 | −2.52 | 3.24 |
Abbreviations: IRT, item response theory; Max, maximum; Min, minimum; SD, standard deviation.
3.2.3. Criterion validity
Median IRT scores for each of the three scales varied significantly by socioeconomic factors previously shown to be associated with experiences of racism including income and education levels. 51 In addition, the scales did not vary by reported clinical characteristics (including maternal BMI, gestational age, and mode of delivery), demonstrating that the measure is independent of clinical risk. (Table 1) All three measures (Humanity, Racism, and Kinship) were significantly associated with separate items with strong face validity as measures of safety, mistreatment, or inequity. 52 (Table 3) Higher agreement on items representing optimum care and minimally acceptable care showed inverse association with all three IRT scaled scores, whereas higher agreement on items representing patient dissatisfaction with care (E66, D74, and R56) showed direct association with each IRT scaled scores. (Table 3).
TABLE 3.
Cumulative proportional odds logistic regression of scale scores on representative perinatal quality improvement items
| IRT scaled scores | Alignment between experience and expectation |
I felt hospital staff were available and paid attention to me when I needed help. (S10) |
I would seek out a Black physician, midwife, doula, lactation educator, or nurse to be part of my hospital birth team, If I could re‐do my 2020 hospital birth. (E66) |
The hospital made me feel that because my baby and I survived birth, my experiences in labor, birth, and postpartum did not matter. (D74) |
I wished I had more information and support about lactation, breastfeeding, or chest feeding that was specific to Black mothers and birthing people. (R56) |
||
|---|---|---|---|---|---|---|---|
| During labor | At birth | Postpartum care | |||||
| OR (95% CI) a , b | OR (95% CI) a , b | OR (95% CI) a , b | OR (95% CI) a , b | OR (95% CI) a , b | OR (95% CI) a , b | OR (95% CI) a , b | |
| Racism | 0.22 (0.18‐0.27) | 0.28 (0.23‐0.34) | 0.27 (0.22‐0.33) c | 0.13 (0.10‐0.17) | 2.84 (2.36‐3.42) | 6.43 (5.02‐8.24) c | 2.07 (1.73‐2.47) |
| Kinship | 0.13 (0.10‐0.17) | 0.16 (0.12‐0.21) | 0.17 (0.13‐0.22) | 0.10 (0.08‐0.13) | 3.03 (2.51‐3.66) | 5.60 (4.38‐7.15) | 2.59 (2.15‐3.12) c |
| Humanity | 0.11 (0.08‐0.14) | 0.16 (0.13‐0.21) | 0.16 (0.13‐0.21) c | 0.03 (0.02‐0.04) | 2.89 (2.42‐3.46) | 8.36 (6.24‐11.21) | 2.33 (1.96‐2.77) |
All P‐values were statistically significant (<.0001).
Probabilities modeled are accumulated over the lower Ordered Values (3‐Strongly agree/Agree, 2‐Neutral, 1‐Disagree/Strongly disagree).
Proportional Odds Assumption does not hold. For the 4 variables violating proportionality assumption, if the ORs from nonproportional odds model were within the 95% confidence interval of proportional odds model, the OR (95% CI) from proportional odds model were used.
In calculating the important difference in IRT scale score for each scale in the suite, we chose four nonretained items consistent with national PQI goals as anchors to estimate important differences. These items represented both optimal care (eg, “I feel the hospital supported the experience I wanted [during labor][during birth][during postpartum]”) and minimally acceptable care (eg, “I felt the hospital staff were available and paid attention to me when I needed help”). They all displayed medium to large effect sizes when moving from strongly disagree/disagree to neutral or from neutral to agree/strongly agree (Cohen's d mean with range: Racism 0.79, 0.58‐1.24; Kinship 0.88, 0.65‐1.35; Humanity 0.98, 0.69‐0.76). Calculated important differences for each scale are expressed in IRT scale score (range): 0.59 (0.45‐0.90) for Racism; 0.64 (0.46‐0.96) for Kinship; and 0.67 (0.49‐1.04) for Humanity.
4. DISCUSSION
The PREM‐OB Scale™ suite offers a tool to quantitatively measure and monitor the lived experiences of birthing while Black in hospital settings in the United States as characterized by Black mothers and birthing people in partnership with Black women community leaders, a Black women‐led research team in the social sciences, humanities, legal studies, social justice, nursing, midwifery, medicine, and public health, and non‐Black women scholars. 4 , 10 , 11 , 12 , 13 , 22 , 27 , 44 , 51 , 52 , 53 , 54 The PREM‐OB Scale™ suite is the first and only intrapartum metric of hospital‐based care informed by the explanatory frameworks of Sojourner syndrome, obstetric racism, and reproductive and perinatal apartheid, which revealed and validated items unique to the experiences of Black birthing people using methodologies grounded in cultural rigor. 7 , 20
The PREM‐OB Scale™ suite consists of 3 independent scales that measure both harmful and protective patient experiences during childbirth hospitalization, which can be leveraged as actionable benchmarks during PQI initiatives. Scale definitions include:
4.1. Racism
The Racism scale measures anti‐Black racism and misogynoir 55 as demonstrated by the hospital enacting acts of degradation and humiliation against Black mothers and birthing people by inappropriate and persistent inquiry about the presence or involvement of the father of the baby; justifying race, and not racism, as the reason for clinical challenges or cultivating a culture of warfare 56 , 57 whereby Black mothers and birthing people feel they must physically, emotionally, mentally, and spiritually activate particular types of mechanisms to mitigate the onset, frequency, duration, and repetition of violence and abuse during hospital childbirth.
4.2. Kinship
The Kinship scale measures disruption and interruption of biological and social ties by hospital policies and practices manifested as acts of obstetric racism enacted against Black mothers and birthing people and their infants, partners, family members, or support persons.
4.3. Humanity
The Humanity scale measures violations of safety and accountability during service provision as demonstrated by perpetuation of physical, emotional, and mental harm; delayed, dismissive, or neglectful care; or inappropriate or rushed care. 27 , 38 , 52 Violations of autonomy are demonstrated by exclusion of patient from decision making; acts of retaliation toward patient or support person when either expressed disagreement with plan of care; limited or constraining of time for appropriate discussion and shared decision making; denial of full range of care options during misalignment between the patient and partner and hospital team, 58 and abrupt interruption of bonding between the patient and family or support person without explanation. 59 , 60 The Humanity scale also includes an evaluation of empathy, from hospital to patient, by assessing whether the hospital clinicians and staff demonstrated capacity to consider life as a Black pregnant, laboring, birthing, and parenting mother or person outside the hospital, particularly during times of disagreement, hurt, and mistrust. Violations of communication and information exchange are demonstrated by denying patient's right to culturally and clinically relevant, accurate, and comprehensive information because of provider packaging of information 54 ; hospital inability to practice reflexive listening without coercion, judgment, or patience 38 ; or cultivating a culture of fear, deception, or mistrust whereby Black mothers modify their language or behavior to appease hospital staff, at the expense of their patient needs, to avoid actual or anticipated retaliation such as not asking for care or help, known as racial reconnaissance. 22 , 27 , 61
To our knowledge, the PREM‐OB Scale™ suite is the only perinatal instrument to include a valid measure of demonstrated empathy, which is significant given existing literature shows that empathy declines during clinical training, 62 and may adversely impact health care quality. 63 In addition, the Kinship and Humanity scales reflect active disruptions of protective and possibly harm‐mitigating mechanisms, whereby Black mothers and birthing people use kinship networks and humanizing strategies to shield themselves and their babies during the birthing process. 64 Existing literature demonstrates the expressed desires of Black mothers and fathers to experience support, rather than barriers, to be involved in pregnancy and childbirth as both partners and parents. 65 Unfortunately, hospital nurses, physicians, and staff may undermine the humanity and autonomy of Black mothers and fathers as parents and caretakers. Research covering the past several decades has demonstrated the disproportionate utilization of child protective services, hospital security, and law enforcement in the practice of parent–child separation, which has been characterized as a form of retaliation against Black mothers and fathers during disagreement with or misunderstanding during health services provision. 66 , 67 , 68 , 69 , 70 , 71 , 72 It is incumbent upon hospital clinicians and staff to accept responsibility for actively facilitating traumatic parent‐child separations, and work with social agencies to reduce harm and promote patient safety and the preservation of Black kinship.
We successfully demonstrated the application of methods (tools and procedures used to conduct research) and methodologies (justification and rationalization about why these methods were appropriate for adaptation) grounded in cultural rigor in our survey validation. The ethical and theoretical approaches in the validation of the PREM‐OB Scale™ suite demonstrate accountability to the call for community‐driven research by Black women patient, content, and community experts. 20 , 54 , 73 The original sample was diverse and reasonably representative of the United States birthing population as a whole, and thus, there is good reason to believe it can be used across settings within the United States. Study limitations include our use of a convenience sample and online written survey format, which likely decreased representation from participants with lower reading comprehension or with greater structural barriers to technology access and utilization. Our cross‐sectional single test format did not allow for test–retest reliability, which will be addressed in future work. Furthermore, research in diverse birth settings and over time is needed to establish reliability. Finally, adaptations across the broader perinatal and reproductive life course may be considered.
Used in conjunction with existing PQI measures and initiatives, the PREM‐OB Scale™ suite facilitates empirical analyses of the associations between process, outcome, and structural measures and patient experiences of obstetric racism enacted exclusively against Black mothers and birthing people. Likewise, data from the PREM‐OB Scale™ suite can be used to benchmark hospitals’ performance and track impact of PQI initiatives on patient, community, and systems level outcomes. Integration of geospatial data and the PREM‐OB Scale™ suite data can identify “hot spots” of racism, disrupted kinship, and dehumanization within hospitals across the US and facilitate customization of place‐based mitigations against obstetric racism. Payers may be able to use these data to better examine and address the dual burden of obstetric racism and any other quantifiable phenomenon in the design, implementation, and evaluation of value‐based reimbursement models for maternity and perinatal care.
Supporting information
Appendix S1‐S3
ACKNOWLEDGMENTS
The authors would like to thank the Black women reproductive health, rights, and justice experts that participated in the modified Delphi process; California Black Women's Health Project who hosted our town hall meeting and supported community referrals, and Catherine Xu for her contribution to this study. The authors additionally thank Black mothers and birthing people who participated in the focus groups, cognitive interviews, and survey testing and gave birth in hospital settings during the 2020 pandemic.
White VanGompel E, Lai J‐S , Davis D‐A, et al. Psychometric validation of a patient‐reported experience measure of obstetric racism© (The PREM‐OB Scale™ suite). Birth. 2022;49:514–525. doi: 10.1111/birt.12622
Funding information
Financial support for this study was provided by the California Health Care Foundation, the Tara Health Foundation, the Grove Foundation, Dwight and Dr Taya Scott, EdD. Funders had no input or influence on data collection, study design or interpretation, reporting, or decision to submit for publication
Contributor Information
Emily White VanGompel, Email: ewhitevangompel@northshore.org.
Karen A. Scott, Email: scotty@birthingculturalrigor.org.
DATA AVAILABILITY STATEMENT
Due to the sensitive nature of this research, participants of this study did not agree for their data to be shared publicly. In an effort to protect the privacy and confidentiality of the participants and to prevent any acts of retaliation or stigmatization, supporting data is not available.
REFERENCES
- 1. Prussing E. Contextualizing racial disparities in preterm delivery: A rhetorical analysis of U.S. epidemiological research at the turn of the 21st century. Soc Sci Med. 2014;4(115):82‐93. [DOI] [PubMed] [Google Scholar]
- 2. Chambers BD, Araga H, Spellen S, et al. Pregnant Black women's experiences of racial discrimination. Am J Obstet Gynecol. 2018;218(1):S569. [Google Scholar]
- 3. Chan AL, Guo N, Popat R, et al. Racial and ethnic disparities in hospital‐based care associated with postpartum depression. J Racial Ethn Health Disparities. 2020;30(8):220‐229. [DOI] [PubMed] [Google Scholar]
- 4. Nuru‐Jeter A, Dominguez TP, Hammond WP, et al. 'It’s The Skin You’re In’: African‐ American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J. 2009;13(1):29‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ekeke PM, Yanowitz DD, Catov JM. Racial differences in the biochemical effects of stress in pregnancy. Int J Environ Res Public Health. 2020;17(19):6941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mendez DD, Vijaya K, Culhane JF. Stress during pregnancy: the role of Institutional racism. Stress & Health. 2013;29(4):266‐274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Scott KA, Bray S, McLemore MR. First, do no harm: why philanthropy needs to re‐examine its role in reproductive equity and racial justice. Health Equity. 2020;4(1):17‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jefferson SS, Mustafaa FN, Misra DP. Early‐life neighborhood context, perceived stress, and preterm birth in African American Women. SSM Popul Health. 2019;28:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Black Mamas Matter Alliance Research Working Group . Black Maternal Health Research Re‐Envisioned: Best Practices for the Conduct of Research With, For, and By Black Mamas [Internet]. Cambridge: Harvard Law and Policy Review; 2020. [cited September 20, 2021]. 23. https://harvardlpr.com/wp‐content/uploads/sites/20/2020/11/BMMA‐Research‐Working‐Group.pdf
- 10. Bridges K. Racial disparities in maternal mortality. NYUL Rev. 2020;95(5):1229. [Google Scholar]
- 11. Chambers BD, Arabia SE, Arega H, et al. Exposures to structural racism and racial discrimination among pregnant and early post‐partum Black women living in Oakland, California. Stress Health. 2020;36(2):213‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chambers BD, Arega H, Arabia SE, et al. Black women's perspectives on structural racism across the reproductive lifespan: a conceptual framework for measurement development. Matern Child Health J. 2021;25(3):402‐413. [DOI] [PubMed] [Google Scholar]
- 13. Goode KL. Birthing Blackness, and the Body: Black Midwives and Experiential Continuities of Institutional Racism. New York: CUNY Academic Works; 2014 [cited September 20, 2021]. 215. Available from: https://academicworks.cuny.edu/cgi/viewcontent.cgi?article=1422&context=gc_etds
- 14. Goode K, Katz‐Rothman B. African‐American Midwifery, a History and a Lament. Am J Econ Sociol. 2017;76(1):65‐94. [Google Scholar]
- 15. Julian Z, Robles D, Whetstone S, et al. Community‐informed models of perinatal and reproductive health services provision: a justice‐centered paradigm toward equity among Black birthing communities. Semin Perinatol. 2020;44(5):151267. [DOI] [PubMed] [Google Scholar]
- 16. Chan AL, Guo N, Popat R, et al. Racial and ethnic disparities in hospital‐based care associated with postpartum depression. J Racial Ethn Health Disparities. 2021;8(1):220‐229. doi: 10.1007/s40615-020-00774-y [DOI] [PubMed] [Google Scholar]
- 17. Boyd RW, Lindo EG, Weeks L, McLemore MR. Health Affairs Blog [Internet]. On Racism: A New Standard For Publishing On Racial Health Inequities; 2020. Available from: https://www.geneticsandsociety.org/article/racism‐new‐standard‐publishing‐racial‐health‐inequities
- 18. Scott KA, Davis DA. Obstetric racism: naming and identifying a way out of black women's adverse medical experiences. Am Anthropol. 2021;123(3):681‐684. [Google Scholar]
- 19. Scott KA. The rise of black feminist intellectual thought and political activism in perinatal quality improvement: a righteous rage about racism, resistance, resilience, and rigor. Am Anthrop. 2021;2(1):155‐160. [Google Scholar]
- 20. Scott KA. Prioritizing patient narratives & community wisdom in quality improvement andimplementation science. Section: Birthing experiences in care settings. In Alper J, Martinez RM, McHugh K eds. Advancing Maternal Health Equity & Reducing Maternal Mortality: Proceedings of a Workshop. The National Academies of Science, Engineering, and Medicine. National Academy Press; 2021:31‐34. [Google Scholar]
- 21. Bowleg L. "The Master's Tools Will Never Dismantle the Master's House": ten critical lessons for black and other health equity researchers of color. Health Educ Behav. 2021;48(3):237‐249. [DOI] [PubMed] [Google Scholar]
- 22. Davis DA. Obstetric racism: the racial politics of pregnancy, labor, and birthing. Med Anthropol. 2019;38(7):560‐573. [DOI] [PubMed] [Google Scholar]
- 23. National Quality Forum . Perinatal and Reproductive Healthcare Endorsement Maintenance 2011‐ National Quality Forum 2011. [cited September 20, 2021]. Available from https://www.qualityforum.org/Projects/n‐r/Perinatal_Care_Endorsement_Maintenance_2011/Perinatal_and_Reproductive_Healthcare_Endorsement_Maintenance_2011.aspx
- 24. Morton CH. The problem of increasing maternal morbidity: integrating normality and risk in maternity care in the United States. Birth. 2014;41(2):119‐121. [DOI] [PubMed] [Google Scholar]
- 25. Scott KA, Britton L, McLemore MR. The ethics of perinatal care for black women. J Perinat Neonatal Nurs. 2019;33(2):108–115. [DOI] [PubMed] [Google Scholar]
- 26. Collins PH. The social construction of black feminist thought. Signs. 1989;14(4):745‐773. [Google Scholar]
- 27. Davis DA. Reproductive Injustice: Racism, Pregnancy, and Premature Birth. In: Brodwin P, Rivkin‐Fish M, Shaw S, eds. Anthropologies of American Medicine: Culture, Power, and Practice. NYU Press; 2019:272. [Google Scholar]
- 28. National Institute on Aging . Patient‐Reported Outcomes Measurement Information System (PROMIS) [Internet]. 2021. Available from https://www.healthmeasures.net/explore‐measurement‐systems/promis
- 29. Uludağ E, Mete S. Development and testing of women's perception for the scale of supportive care given during labor. Pain Manag Nurs. 2015;16(5):751‐758. doi: 10.1016/j.pmn.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 30. Martin CR, Hollins Martin CJ, Burduli E, Barbosa‐Leiker C, Donovan‐Batson C, Fleming SE. The Birth Satisfaction Scale ‐ Revised (BSS‐R): should the subscale scores or the total score be used? J Reprod Infant Psychol. 2018;36(5):530‐535. [DOI] [PubMed] [Google Scholar]
- 31. Afulani PA, Feeser K, Sudhinaraset M, Aborigo R, Montagu D, Chakraborty N. Toward the development of a short multi‐country person‐centered maternity care scale. Int J Gynaecol Obstet. 2019;146(1):80‐87. [DOI] [PubMed] [Google Scholar]
- 32. Shulman H, D’Angelo DV, Harrison L, Smith RA, Warner L. The Pregnancy Risk Assessment Monitoring System (PRAMS): overview of design and methodology. Am J Public Health. 2018;108(10):1305‐1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vedam S, Stoll K, Khemet Taiwo T, et al. The Giving Voice to Mothers study: inequity and mistreatment during pregnancy and childbirth in the United States. Reprod Health. 2019;16(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Duff LA, Lamping DL, Ahmed LB. Evaluating satisfaction with maternity care in women from minority ethnic communities: development and validation of a Sylheti questionnaire. Int J Qual Health Care. 2001;13(3):215‐230. [DOI] [PubMed] [Google Scholar]
- 35. Lewis JA, Neville HA. Construction and initial validation of the Gendered Racial Microaggressions Scale for Black women. J Couns Psychol. 2015;62(2):289‐302. [DOI] [PubMed] [Google Scholar]
- 36. Scheerhagen M, van Stel HF, Franx A, Birnie E, Bonsel GJ. The discriminative power of the ReproQ: a client experience questionnaire in maternity care. PeerJ. 2019;27(7):e7575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vedam S, Stoll K, Martin K, et al. The Mother's Autonomy in Decision Making (MADM) scale: patient‐led development and psychometric testing of a new instrument to evlauate experience of maternity care. PLoS One. 2017;12(2):e0171804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vedam S, Stoll K, Rubashkin N, et al. The Mothers on Respect (MOR) index: measuring quality, safety, and human rights in childbirth. SSM Popul Health. 2017;19(3):201‐210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ford E, Ayers S, Wright DB. Measurement of maternal perceptions of support and control in birth (SCIB). J Womens Health (Larchmt). 2009;18(2):245‐252. [DOI] [PubMed] [Google Scholar]
- 40. Gungor I, Beji NK. Development and psychometric testing of the scales for measuring maternal satisfaction in normal and caesarean birth. Midwifery. 2012;28(3):348‐357. [DOI] [PubMed] [Google Scholar]
- 41. Gaumer Erickson AS, Soukup JH, Noonan PM & McGurn L Empathy formative questionnaire [Measurement instrument]. 2015. Available from http://www.researchcollaboration.org/uploads/EmpathyQuestionnaireInfo.pdf. Accessed February 17, 2022.
- 42. Angeby K, Sandin‐Bojo AK, Persenius M, Wilde‐Larsson B. Early Labour Experience Questionnaire: psychometric testing and women's experiences in a Swedish setting. Midwifery. 2018;64:77‐84. [DOI] [PubMed] [Google Scholar]
- 43. Asefa A, Bekele D. Status of respectful and non‐abusive care during facility‐based childbirth in a hospital and health centers in Addis Ababa, Ethiopa. Reprod Health. 2015;12:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mullings L. Resistance and resilience: The Sojourner Syndrome and the social context of reproduction in Central Harlem. Transform Anthropol. 2005;13::79. [Google Scholar]
- 45. Washington HA. Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present. Doubleday Books; 2006:528. [Google Scholar]
- 46. Scott KA, Davis DA. Translating Obstetric Racism into a Patient‐Reported Experience Measure. Paper presented at: Social Science Grand Rounds. 2020 July 24; virtual event.
- 47. Casper RA, Lessler JT, Willis GB, editors. Cognitive Interviewing: A "How To" Guide. 1999 Meeting of the American Statistical Association; Rockville MD. North Carolina: Research Triangle Institute; 1999:41.
- 48. Peterson CH, Peterson NA, Powell KG. Cognitive interviewing for item development: validity evidence based on content and response processes. Meas Eval Couns Dev. 2017;50(4):217‐223. [Google Scholar]
- 49. L‐tB HU, Peter M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 2009;6(1):1‐55. [Google Scholar]
- 50. National Vital Statistics System [Internet]. Cited September 1, 2021. 2019. Available from: https://www.cdc.gov/nchs/nvss/index.htm
- 51. Vines AI, Baird DD, McNeilly M, Hertz‐Picciotto I, Light KC, Stevens J. Social correlates of the chronic stress of perceived racism among Black women. Ethn Dis. 2006;16(1):101‐107. [PMC free article] [PubMed] [Google Scholar]
- 52. Vedam S, Stoll K, Taiwo TK, et al. The Giving Voice to Mothers study: inequity and mistreatment during pregnancy and childbirth in the United States. Reprod Health. 2019;16(77):1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bridges KM. Reproducing Race: An ethnography of pregnancy as a site of racialization. University of California Press; 2011:306. [Google Scholar]
- 54. Cooper Owens D. Medical Bondage: Race, Gender, and the Origins of American Gynecology. University of Georgia Press; 2017:165. [Google Scholar]
- 55. Jackson FM, James SA, Owens TC, Bryan AF. Anticipated negative police‐youth encounters and depressive symptoms among pregnant African American women: a brief report. J Urban Health. 2017;94(2):250‐265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Altman MR, McLemore MR, Oseguera T, Lyndon A, Franck LS. Listening to women: recommendations from women of color to improve experiences in pregnancy and birth care. J Midwifery Womens Health. 2020;65(4):466‐473. [DOI] [PubMed] [Google Scholar]
- 57. Bailey M. Misogynoir Transformed: Black Women's Digital Resistance. NYU Press; 2021:248. [Google Scholar]
- 58. Oparah JC, Bonaparte AD. Birthing justice: black women, pregnancy, and childbirth. Paradigm Publishers; 2015:246. [Google Scholar]
- 59. Oparah JC, Arega H, Hudson D, Oseguera T. Battling over birth: black women and the maternal health care crisis. Praeclarus; 2018:24. [Google Scholar]
- 60. Attanasio LB, Hardeman RR. Declined care and discrimination during the childbirth hospitalization. Soc Sci Med. 2019;232:270‐277. [DOI] [PubMed] [Google Scholar]
- 61. Metzl JM, Roberts DE. Structural competency meets structural racism: race, politics, and the structure of medical knowledge. Virtual Mentor. 2014;16(9):674‐690. [DOI] [PubMed] [Google Scholar]
- 62. Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126‐133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Davis DA. Reproducing while Black: The crisis of Black maternal health, obstetric racism and assisted reproductive technology. Reprod Biomed Soc Online. 2020;1(11):56‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Chen D, Lew R, Hershman W, Orlander J. A cross‐sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434‐1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071‐1078. [DOI] [PubMed] [Google Scholar]
- 66. Gibney S, Deus V. New Visions in Birth, Intimacy, Kinship, and Sisterly Partnerships. In: Oparah JS, Bonaparte AD, eds. Changing Lives, One Birth at a Time. Routledge, Taylor & Francis; 2016:15. Chapter 3. [Google Scholar]
- 67. Edwards BN, McLemore MR, Baltzell K, Hodgkin A, Nunez O, Franck LS. What about the men? Perinatal experiences of men of color whose partners were at risk for preterm birth, a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Roberts DE. Prison, foster care, and the systemic punishment of black mothers. UCLA L Rev [Internet]. 2012 [cited September 20. 2021]; 59:1474. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2184329
- 69. Alexander M. The new jim crow. Ohio St J Crim L. 2011;9(1):7‐26. [cited 2021 Sept 20]. https://kb.osu.edu/bitstream/handle/1811/73367/OSJCL_V9N1_007.pdf?sequence=1&isAllowed=y [Google Scholar]
- 70. Roberts DE. The Color of Child Welfare. Basic Civitas Books; 2002:352. [cited 2021 Sept 20]. [Google Scholar]
- 71. Alexander M. The new jim crow: Mass incarceration in the age of color blindness. The New Press; 2020:290. [Google Scholar]
- 72. Briggs L. Somebody's Children: The politics of transracial and transnational adoption. Duke University Press; 2012:376. [Google Scholar]
- 73. Scott KA, Chambers BD, McKenzie‐Sampson S, et al. The Virtual Perinatal Quality Improvement Prioritization By Affected Communities (V‐QPAC) Protocol. Health Serv Res. 2021;56:56‐57. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1‐S3
Data Availability Statement
Due to the sensitive nature of this research, participants of this study did not agree for their data to be shared publicly. In an effort to protect the privacy and confidentiality of the participants and to prevent any acts of retaliation or stigmatization, supporting data is not available.


