Abstract
Introduction
The major stressors associated with the COVID‐19 pandemic provide an opportunity to understand the extent to which protective factors against depression may exhibit gender‐specificity.
Method
This study examined responses from multiple waves of a 50 states non‐probability internet survey conducted between May 2020 and January 2021. Participants completed the PHQ‐9 as a measure of depression, as well as items characterizing social supports. We used logistic regression models with population reweighting to examine association between absence of even mild depressive symptoms and sociodemographic features and social supports, with interaction terms and stratification used to investigate sex‐specificity.
Results
Among 73,917 survey respondents, 31,199 (42.2%) reported absence of mild or greater depression—11,011/23,682 males (46.5%) and 20,188/50,235 (40.2%) females. In a regression model, features associated with greater likelihood of depression‐resistance included at least weekly attendance of religious services (odds ratio [OR]: 1.10, 95% confidence interval [CI]: 1.04–1.16) and greater trust in others (OR: 1.04 for a 2‐unit increase, 95% CI: 1.02–1.06), along with level of social support measured as number of social ties available who could provide care (OR: 1.05, 95% CI: 1.02–1.07), talk to them (OR: 1.10, 95% CI: 1.07–1.12), and help with employment (OR: 1.06, 95% CI: 1.04–1.08). The first two features showed significant interaction with gender (p < .0001), with markedly greater protective effects among women.
Conclusion
Aspects of social support are associated with diminished risk of major depressive symptoms, with greater effects of religious service attendance and trust in others observed among women than men.
Keywords: depression, major depressive disorder, resilience, resilient, SARS‐CoV2, survey
1. INTRODUCTION
A substantial proportion of the risk for most mood and anxiety disorders is environmental, with acute stressors among the best‐understood risk factors (Gilman et al., 2015; Smoller, 2016). On the contrary, a subset of individuals with such stressors will not develop mood or anxiety symptoms. Understanding the characteristics of these individuals—namely, the features that confer resilience in the face of stress (Schetter & Dolbier, 2011)—may facilitate the development of interventions aimed at enhancing resilience for primary or secondary prevention.
Social supports are well‐understood to confer resilience to the effects of stress, using a variety of study designs (Ozbay et al., 2007; Southwick et al., 2016). What is less clearly defined is whether these protective factors exhibit sex‐specificity—that is, are there differences in the extent to which women are protected compared to men. Two lines of evidence suggest that sex‐specificity is likely. First, major depressive disorder, and multiple other mood and anxiety disorders, exhibit differential prevalence among women (Bebbington et al., 1998). Second, social behavior on average differs by sex, from mouse models through primates as well as in human psychological studies (Dudek et al., 2021; Ma et al., 2019).
The COVID‐19 pandemic presents an opportunity to better understand resilience effects, particularly as they may inform efforts to enhance resilience (Kunzler et al., 2020). In addition to chronic stress, the financial consequences of the pandemic as acute stressors have become apparent. In the present study, we utilized data from a multi‐wave US survey that included questions about COVID‐19 encompassing 50 states and the District of Columbia. As respondents did not know the survey topic before opting in, the design is less susceptible to selection bias than many alternate designs. We sought to understand, first, whether individual characteristics of social interaction and supports were associated with diminished likelihood of depression during the COVID‐19 pandemic—that is, enhanced resilience against depression—and second, whether such effects might exhibit gender‐specificity.
2. METHOD
2.1. Study design
We utilized 10 waves of an online survey between May 2020 and January 2021 across 50 states and the District of Columbia, applying nonprobability sampling using representative quotas to balance age, gender, and race/ethnicity. Survey results were weighted to balance on age, gender, race/ethnicity, education, region, and rural/urban area of residence, based on US Census data. The study was reviewed by the Institutional Review Board of Harvard University and determined to be exempt. Participants signed consent online before survey access. We followed AAPOR reporting guidelines for survey studies, as described at https://www.aapor.org/Standards-Ethics/AAPOR-Code-of-Ethics/Survey-Disclosure-Checklist.aspx; response rates are not calculable as multiple web‐based survey panels could opt‐in to complete the survey.
2.2. Measures
Survey participants completed the PHQ‐9, a well‐validated screen for major depressive disorder that measures frequency of individual symptoms in the preceding 2 weeks (Kroenke & Spitzer, 2002). Participants were also asked about social support as putative protective factors (represented as number of people who could provide a particular form of support, from 0 to 11 or more). Specifically, they were asked to identify the number of people who could care for them if they became ill, lend them money, serve as someone to talk to if they felt down or depressed, or help them find employment; these validated questions were drawn from a prior examination of social networks (Lubbers et al., 2019). Additional questions asked about frequency of religious service attendance (from never to more than once a week) and degree of trust in others on a Likert scale ranging from 1 (you can't be too careful) to 10 (most people can be trusted). A further question asked about number of face‐to‐face meetings with individuals outside of the household over the past 24 h.
2.3. Analysis
In primary analysis, we defined resilient individuals as those with no evidence of even mild depression, defined as PHQ‐9 score less than 5. Survey results were reweighted using interlocking national weights for age, sex, race/ethnicity, education, and region. We used logistic regression in R 4.0 (R Core Team, 2019) with the “survey” package to examine the association between resilience (again, absence of depressive symptoms despite stressors) and individual features of social network, including response to the 10‐point trust Likert scale, frequency of religious service attendance of any sort, and extent of social supports. All analyses were also adjusted for age, self‐reported gender, self‐reported race/ethnicity indicated on a 5‐item questionnaire, income, and rural/suburban/urban area of residence. In sensitivity analysis to examine the extent to which current social interaction might modify or confound these effects, we added a term for current social interaction to these models; to examine the extent to which effects could be impacted by COVID‐19 illness, we added a term capturing prior clinician diagnosis and/or positive SARS‐CoV2 test. For any social network characteristics exhibiting main effects, we then examined gender specificity in two ways: by incorporating a feature‐by‐gender interaction term, and by estimating effects stratified by gender. Missing data (Table 1) reflecting the fact that only a randomly‐selected subset of respondents received all questions were addressed using case‐wise deletion; multiple imputation did not yield meaningfully different results.
Table 1.
Social features among male and female survey respondents
| Male (N = 23,682) | Female (N = 50,235) | Total (N = 73,917) | p value | |
|---|---|---|---|---|
| No depressive symptoms | 11,011 (46.5%) | 20,188 (40.2%) | 31,199 (42.2%) | <.001 |
| Trust score (1–10) | <.001 | |||
| (missing) | 4857 | 11,100 | 15,957 | |
| Mean (SD) | 5.493 (2.515) | 4.870 (2.363) | 5.072 (2.431) | <.001 |
| Service attendance | ||||
| (missing) | 4180 | 8928 | 13,108 | <.001 |
| Weekly or more frequent | 5848 (30.0%) | 8802 (21.3%) | 14,650 (24.1%) | |
| Someone to care for | ||||
| Mean (SD) | 2.84 (2.62) | 3.02 (2.62) | 2.96 (2.62) | |
| Someone to lend money | <.001 | |||
| (missing) | 213 | 465 | 678 | |
| Mean (SD) | 2.35 (2.36) | 2.28 (2.21) | 2.30 (2.26) | |
| Someone to talk to | <.001 | |||
| (missing) | 295 | 583 | 878 | |
| Mean (SD) | 3.37 (3.10) | 3.72 (3.10) | 3.61 (3.10) | |
| Someone to find a job | <.001 | |||
| (missing) | 403 | 953 | 1356 | |
| Mean (SD) | 2.72 (3.08) | 2.64 (2.95) | 2.66 (3.00) | |
| Face‐to‐face meetings | <.001 | |||
| (missing) | 89 | 187 | 276 | |
| Mean (SD) | 5.48 (12.70) | 6.10 (14.34) | 5.90 (13.84) |
3. RESULTS
The full cohort included 73,917 survey respondents with PHQ‐9 results, of whom 31,199 (42.2%) reported absence of mild or greater depression—11,011/23,682 males (46.5%) and 20,188/50,235 (40.2%) females. The cohort had a mean age of 40.94 years (SD 16.06), who were 68.0% female, 71.4% white, 10.9% Black, 7.9% Hispanic, and 5.8% Asian. In univariate analyses, those with and without depression differed statistically in all sociodemographic features (Table 2). Social features also differed significantly by gender, as summarized in Table 2.
Table 2.
Characteristics of survey respondents who reported minimal depressive symptoms, compared to mild or greater depressive symptoms
| Mild or greater symptoms (N = 42,718) | No depression (N = 31,199) | Total (N = 73,917) | p value | |
|---|---|---|---|---|
| Age | <.001 | |||
| Mean (SD) | 37.07 (14.42) | 46.24 (16.67) | 40.94 (16.06) | |
| Female gender (%) | 30,047 (70.3%) | 20,188 (64.7%) | 50,235 (68.0%) | <.001 |
| Household income | <.001 | |||
| (missing) | 3122 | 1722 | 4844 | |
| Mean ($1000) (SD) | 61.46 (71.34) | 71.13 (73.72) | 65.59 (72.52) | |
| Race/ethnicity | <.001 | |||
| White | 30,144 (70.6%) | 22,635 (72.6%) | 52,779 (71.4%) | |
| Hispanic | 3710 (8.7%) | 2111 (6.8%) | 5821 (7.9%) | |
| Black | 4506 (10.5%) | 3578 (11.5%) | 8084 (10.9%) | |
| Asian | 2551 (6.0%) | 1741 (5.6%) | 4292 (5.8%) | |
| Other | 1807 (4.2%) | 1134 (3.6%) | 2941 (4.0%) | |
| Location | <.001 | |||
| Rural | 7400 (17.3%) | 5207 (16.7%) | 12,607 (17.1%) | |
| Suburban | 24,535 (57.4%) | 18,443 (59.1%) | 42,978 (58.1%) | |
| Urban | 10,783 (25.2%) | 7549 (24.2%) | 18,332 (24.8%) | |
| Trust score | <.001 | |||
| (missing) | 7916 | 8041 | 15,957 | |
| Mean (SD) | 4.92 (2.44) | 5.30 (2.41) | 5.07 (2.43) | |
| Service attendance | <.001 | |||
| (missing) | 5954 | 7154 | 13,108 | |
| Weekly or more frequent | 8038 (21.9%) | 6612 (27.5%) | 14,650 (24.1%) | |
| Someone to care for | <.001 | |||
| Mean (SD) | 2.80 (2.53) | 3.18 (2.74) | 2.962 (2.62) | |
| Someone to lend money | <.001 | |||
| (missing) | 406 | 272 | 678 | |
| Mean (SD) | 2.20 (2.15) | 2.44 (2.40) | 2.30 (2.26) | |
| Someone to talk to | <.001 | |||
| (missing) | 522 | 356 | 878 | |
| Mean (SD) | 3.31 (2.98) | 4.01 (3.22) | 3.61 (3.10) | |
| Someone to find a job | <.001 | |||
| (missing) | 798 | 558 | 1356 | |
| Mean (SD) | 2.51 (2.83) | 2.87 (3.20) | 2.66 (3.00) | |
| Face‐to‐face meetings interactions/24 h | .001 | |||
| (missing) | 166 | 110 | 276 | |
| Mean (SD) | 6.04 (14.28) | 5.70 (13.21) | 5.90 (13.84) |
In a multiple regression model (Figure 1), features associated with greater likelihood of depression‐resistance included at least weekly attendance of religious services (odds ratio [OR]: 1.10, 95% confidence interval [CI] 1.04–1.16) and greater trust in others (OR: 1.04 for a 2‐unit increase, 95% CI: 1.02–1.06), along with level of social support measured as number of social ties available who could provide care (OR: 1.05 for every two additional supports, 95% CI: 1.02–1.07), talk to them (OR: 1.10, 95% CI: 1.07–1.12), and help with employment (OR: 1.06, 95% CI: 1.04–1.08). Results were not meaningfully changed (i.e., coefficients changed by <10% in all cases) with addition of a term for frequency of face‐to‐face interactions in the past 24 h. Likewise, in secondary analysis incorporating a term for prior symptomatic COVID‐19 diagnosis (4044/73,275 or 5.5%), coefficients changed by <10% with the exception of impact of weekly attendance of religious services (OR: 1.15, 95% CI: 1.09–1.22).
Figure 1.
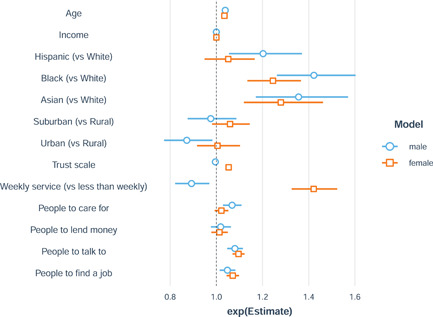
Logistic regression model of minimal depressive symptoms, stratified by gender Caption: Trust score effects are reported per unit increase on 1–10 scale; social support effects are reported per two‐person increase in supports identified
Among those social features demonstrating significant main effects, religious service attendance and trust showed significant interaction with gender (p < .0001), with positive associations with resilience among women (Figure 2)—for trust, OR: 1.11 (95% CI: 1.08–1.14), and for weekly religious service attendance, OR: 1.42 (95% CI: 1.33–1.52). Conversely, weekly or more frequent religious service among males was associated with greater risk (OR: 0.89, 95% CI: 0.82–0.97), while no association with trust was observed (OR: 0.99, 95% CI: 0.96–1.02). The number of identified supports were not associated with statistically significant differential effects—interaction‐by‐gender for caregiving, t = −1.90, p = .06; for someone to talk to, t = 0.81, p = .42; and for help with employment, t = 1.59, p = .11).
Figure 2.
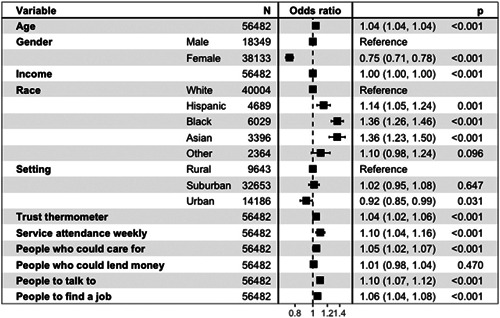
Logistic regression model of minimal depressive symptoms. Trust score effects are reported per unit increase on 1–10 scale; social support effects are reported per two‐person increase in supports identified
4. DISCUSSION
In this analysis of national survey data from 73,917 survey respondents, 31,199 (42.2%) reported absence of mild or greater depression, suggesting resilience in the face of chronic stressors. Greater age, male gender, and being non‐white were associated with lesser likelihood of reporting depression. In general, greater number of social supports were also associated with lesser likelihood of reporting depressive symptoms; these effects were modest in comparison with other effect sizes and did not exhibit gender‐specificity. In contrast, greater trust in others, and more frequent religious service attendance, exhibited significantly larger association with resilience among women.
As a cross‐sectional analysis, we cannot infer causation, and must acknowledge the possibility that depressive symptoms impact reporting of social network features, or contribute to reduction in social network size. We do note that incorporating face‐to‐face interaction in the past 24 h does not meaningfully change associations, as we might expect if depression was simply causing less social activity overall—that is, if the causal arrow were reversed. Longitudinal cohort studies, particularly those that include data preceding onset of widespread COVID‐19 infection, will be important to investigate causal effects of social behavior.
The psychiatric consequences of the COVID‐19 pandemic, in terms of mood and anxiety symptoms, became apparent early and have been well‐documented in a range of studies (Ettman et al., 2020; Rossi et al., 2020). The stressors associated with the pandemic are somewhat different from those of past disasters such as the 9/11 terrorist attack or the Fukushima nuclear power plant disaster, particularly in terms of their chronicity, but also in that they disrupt the very social supports that may represent important factors in resilience. As such, studies to understand what kind of social supports enhance resilience—and, if possible, how they can be maintained and augmented—are needed.
Despite recent enthusiasm for precision medicine in psychiatry, one of the most basic differences between individuals—that is, gender—is honored more in the abstract. A small number of studies suggest that, in general, psychological factors contributing to adverse outcomes may differ by gender or sex (Smaardijk et al., 2020). In this study, we sought to understand whether social effects differ in their capacity to confer resilience by gender. An abundant literature supports differences in depression and anxiety by gender, beginning with prevalence and onset age (Bebbington et al., 1998) and extending through phenomenology and putative neuroanatomy (Yang et al., 2017). Marked differences in stress response have been observed in animal models (Dudek et al., 2021; Ma et al., 2019). Likewise, phenomenology and neurobiology of social functioning also differs by gender (Masi et al., 2021). However, the capacity of social interaction to contribute to resilience by gender is less extensively studied, particularly for chronic stresses.
While multiple surveys of mood in COVID‐19 have been reported, few have sought to examine social features contributing to resilience. A recent systematic review of studies among healthcare workers noted the role of social support (both individual, and organizational) but did not characterize gender‐specificity (Sirois & Owens, 2020). A survey of healthcare workers suggested that the need for social support was associated with poorer outcomes (Hennein et al., 2021), but also did not investigate gender‐specific effects.
Among non‐healthcare populations, there are fewer reports of resilience factors related to social networks. Unsurprisingly, a Norwegian survey of ~10,000 individuals identified loneliness during social distancing as associated with greater levels of depression (Hoffart et al., 2020). Our findings regarding religious service attendance also extend prior work. In the largest study to date (Chen et al., 2021), drawing on three prospective cohorts, religious service attendance was associated with diminished risk for depression and greater well‐being. Investigations in particular subgroups have yielded similar results, including diminished suicidality among college students (Kim et al., 2021) and reduced hopelessness among middle‐aged Black individuals (Mitchell et al., 2020). Notably, however, none of these studies examined sex‐specificity of these associations. As with other elements of social functioning, our work highlights the importance of considering sex differences in future work.
A parallel line of evidence (Grossoehme et al., 2020) suggests that religiosity or spirituality itself, with a variety of definitions, may be associated with diminished risk for depressive and anxious symptoms. For example, in a study of 400 Palestinians, coping strategies involving religion were associated with diminished depressive symptoms and lower levels of perceived stress, although the authors did not report gender‐specific effects (Mahamid & Bdier, 2021). The relationship between religiosity and religious service attendance is complex, and may change across the lifespan (see, e.g., Dew et al., 2020). The present study cannot distinguish the possibility that the association observed with resilience or risk reflects religiosity rather than religious activity.
We note multiple limitations in our work beyond the cross‐sectional nature of the survey. First, we apply a non‐probability design with web‐based panels, so cannot report a survey response rate, which would aid in understanding generalizability and bias. We emphasize that, because the survey as a whole is not focused solely on COVID‐19, and does not recruit by mentioning COVID‐19, selection bias should be diminished compared to more focused surveys that might attract individuals with a greater interest in the pandemic. Moreover, large‐scale non‐probability designs have tended to yield results consistent with the far costlier probability samples (Czeisler, 2020). A further limitation is that our characterization of social functioning is opportunistic—that is, we can characterize only a subset of features of social support and interaction. Here too, prospective cohort studies applying validated instruments will be critical to extend and refine our work. We also emphasize that absence of depression is only one element of resilience; positive affect and well‐being reflect more than simply being free from depressive symptoms. Finally, the collection of data during a pandemic represents both a strength and a limitation of this study: the increase in ambient stress levels may make effects on resilience easier to identify, but the extent to which these effects will generalize to other sources of stress, and following the pandemic, will require further investigation as well.
Nonetheless, as a large‐scale investigation of gender‐specificity of social effects, our study adds to the literature regarding resilience in mood disorders. Consistent with abundant animal modeling work, our results suggest that males and females are quite different in how they respond to chronic stress, particularly in terms of how social characteristics modify the risk of developing depressive symptoms. In light of the profound impact of COVID‐19 on mental health, strategies to develop more targeted means of improving resilience (Kunzler et al., 2020) will be needed to diminish risk for depression, anxiety, and related disorders.
CONFLICT OF INTERESTS
Perlis has received consulting fees from Burrage Capital, Genomind, RID Ventures, and Takeda. He holds equity in Outermost Therapeutics and Psy Therapeutics. The other authors report no disclosures.
AUTHOR CONTRIBUTIONS
Analyzed data, drafted and revised manuscript: Roy H. Perlis, MD, MSc. Cleaned and analyzed data: Jon Green, PhD. Revised manuscript: Mauricio Santillana, PhD. Secured funding, oversaw study, revised manuscript: David Lazer, PhD. Oversaw data collection, revised manuscript: Katherine Ognyanova, PhD. Revised manuscript, oversaw data collection: Matthew Simonson. Secured funding, revised manuscript: Matthew A. Baum, PhD. Cleaned data, revised manuscript: Alexi Quintana. Contributed to data collection, revised manuscript: Hanyu Chwe. Revised manuscript: James Druckman, PhD. Revised manuscript: Jennifer Lin.
ACKNOWLEDGMENTS
This study was supported by the National Institute of Mental Health (R01MH116270 and 1R56MH115187; Perlis) and the National Science Foundation (SES‐2029292 and SES‐2029792; Baum and Ognyanova). The sponsors did not contribute to any aspect of study design, data collection, data analysis, or data interpretation. The authors had the final responsibility for the decision to submit for publication.
Perlis, R. H. , Ognyanova, K. , Quintana, A. , Green, J. , Santillana, M. , Lin, J. , Druckman, J. , Lazer, D. , Simonson, M. , Baum, M. A. , & Chwe, H. (2021). Gender‐specificity of resilience in major depressive disorder. Depression Anxiety, 38, 1026–1033. 10.1002/da.23203
ENDNOTES
The link will be made available after submission.
REFERENCES
- Bebbington, P. E. , Dunn, G. , Jenkins, R. , Lewis, G. , Brugha, T. , Farrell, M. , & Meltzer, H. (1998). The influence of age and sex on the prevalence of depressive conditions: Report from the National Survey of Psychiatric Morbidity. Psychological Medicine, 28(1), 9–19. 10.1017/s0033291797006077 [DOI] [PubMed] [Google Scholar]
- Chen, Y. , Kim, E. S. , & VanderWeele, T. J. (2021). Religious‐service attendance and subsequent health and well‐being throughout adulthood: Evidence from three prospective cohorts. International Journal of Epidemiology, 49(6), 2030–2040. 10.1093/ije/dyaa120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler, M. É. (2020). Mental health, substance use, and suicidal ideation during the COVID‐19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69, 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dew, R. E. , Fuemmeler, B. , & Koenig, H. G. (2020). Trajectories of religious change from adolescence to adulthood, and demographic, environmental, and psychiatric correlates. The Journal of Nervous and Mental Disease, 208(6), 466–475. 10.1097/NMD.0000000000001154 [DOI] [PubMed] [Google Scholar]
- Dudek, K. A. , Dion‐Albert, L. , Kaufmann, F. N. , Tuck, E. , Lebel, M. , & Menard, C. (2021). Neurobiology of resilience in depression: Immune and vascular insights from human and animal studies. The European Journal of Neuroscience, 53(1), 183–221. 10.1111/ejn.14547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman, C. K. , Abdalla, S. M. , Cohen, G. H. , Sampson, L. , Vivier, P. M. , & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID‐19 pandemic. JAMA Network Open, 3(9), e2019686. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman, S. E. , Ni, M. Y. , Dunn, E. C. , Breslau, J. , McLaughlin, K. A. , Smoller, J. W. , & Perlis, R. H. (2015). Contributions of the social environment to first‐onset and recurrent mania. Molecular Psychiatry, 20(3), 329–336. 10.1038/mp.2014.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossoehme, D. H. , Friebert, S. , Baker, J. N. , Tweddle, M. , Needle, J. , Chrastek, J. , Thompkins, J. , Wang, J. , Cheng, Y. I. , & Lyon, M. E. (2020). Association of religious and spiritual factors with patient‐reported outcomes of anxiety, depressive symptoms, fatigue, and pain interference among adolescents and young adults with cancer. JAMA Network Open, 3(6), e206696. 10.1001/jamanetworkopen.2020.6696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennein, R. , Mew, E. J. , & Lowe, S. R. (2021). Socio‐ecological predictors of mental health outcomes among healthcare workers during the COVID‐19 pandemic in the United States. PLOS One, 16(2), e0246602. 10.1371/journal.pone.0246602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffart, A. , Johnson, S. U. , & Ebrahimi, O. V. (2020). Loneliness and social distancing during the COVID‐19 pandemic: Risk factors and associations with psychopathology. Frontiers in Psychiatry, 11, 589127. 10.3389/fpsyt.2020.589127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, Y. J. , Crutchfield, J. , & Kim, Y. K. (2021). Effects of church attendance Vs. private religious activities on suicidal ideation: A study of rural US College students. Journal of Religion and Health, 60, 2560–2572. 10.1007/s10943-021-01224-7 [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , & Spitzer, R. L. (2002). The PHQ‐9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515. 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kunzler, A. M. , Helmreich, I. , Chmitorz, A. , König, J. , Binder, H. , Wessa, M. , & Lieb, K. (2020). Psychological interventions to foster resilience in healthcare professionals. The Cochrane Database of Systematic Reviews, 7, CD012527. 10.1002/14651858.CD012527.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubbers, M. J. , Molina, J. L. , & Valenzuela‐García, H. (2019). When networks speak volumes: Variation in the size of broader acquaintanceship networks. Social Networks, 56, 55–69. 10.1016/j.socnet.2018.08.004 [DOI] [Google Scholar]
- Ma, L. , Xu, Y. , Wang, G. , & Li, R. (2019). What do we know about sex differences in depression: A review of animal models and potential mechanisms. Progress in Neuro‐Psychopharmacology & Biological Psychiatry, 89, 48–56. 10.1016/j.pnpbp.2018.08.026 [DOI] [PubMed] [Google Scholar]
- Mahamid, F. A. , & Bdier, D. (2021). The association between positive religious coping, perceived stress, and depressive symptoms during the spread of coronavirus (COVID‐19) among a sample of adults in palestine: Across sectional study. Journal of Religion and Health, 60(1), 34–49. 10.1007/s10943-020-01121-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi, G. , Berloffa, S. , Milone, A. , & Brovedani, P. (2021). Social withdrawal and gender differences: Clinical phenotypes and biological bases. Journal of Neuroscience Research, 1–13. 10.1002/jnr.24802 [DOI] [PubMed] [Google Scholar]
- Mitchell, U. A. , Gutierrez‐Kapheim, M. , Nguyen, A. W. , & Al‐Amin, N. (2020). Hopelessness among middle‐aged and older blacks: The negative impact of discrimination and protecting power of social and religious resources. Innovation in Aging, 4(5), igaa044. 10.1093/geroni/igaa044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozbay, F. , Johnson, D. C. , Dimoulas, E. , Morgan, C. A. , Charney, D. , & Southwick, S. (2007). Social support and resilience to stress. Psychiatry (Edgmont), 4(5), 35–40. [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2019). R: A language and environment for statistical computing (3.6.0) [Computer software]. R Foundation for Statistical Computing. www.R-project.org
- Rossi, R. , Socci, V. , Pacitti, F. , Di Lorenzo, G. , Di Marco, A. , Siracusano, A. , & Rossi, A. (2020). Mental health outcomes among frontline and second‐line health care workers during the coronavirus disease 2019 (COVID‐19) pandemic in Italy. JAMA Network Open, 3(5), e2010185. 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schetter, C. D. , & Dolbier, C. (2011). Resilience in the context of chronic stress and health in adults. Social and Personality Psychology Compass, 5(9), 634–652. 10.1111/j.1751-9004.2011.00379.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirois, F. M. , & Owens, J. (2020). Factors associated with psychological distress in health‐care workers during an infectious disease outbreak: A rapid systematic review of the evidence. Frontiers in Psychiatry, 11, 589545. 10.3389/fpsyt.2020.589545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smaardijk, V. R. , Maas, A. H. E. M. , Lodder, P. , Kop, W. J. , & Mommersteeg, P. M. C. (2020). Sex and gender‐stratified risks of psychological factors for adverse clinical outcomes in patients with ischemic heart disease: A systematic review and meta‐analysis. International Journal of Cardiology, 302, 21–29. 10.1016/j.ijcard.2019.12.014 [DOI] [PubMed] [Google Scholar]
- Smoller, J. W. (2016). The genetics of stress‐related disorders: PTSD, depression, and anxiety disorders. Neuropsychopharmacology, 41(1), 297–319. 10.1038/npp.2015.266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick, S. M. , Sippel, L. , Krystal, J. , Charney, D. , Mayes, L. , & Pietrzak, R. (2016). Why are some individuals more resilient than others: The role of social support. World Psychiatry, 15(1), 77–79. 10.1002/wps.20282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, X. , Peng, Z. , Ma, X. , Meng, Y. , Li, M. , Zhang, J. , Song, X. , Liu, Y. , Fan, H. , Zhao, L. , Deng, W. , Li, T. , & Ma, X. (2017). Sex differences in the clinical characteristics and brain gray matter volume alterations in unmedicated patients with major depressive disorder. Scientific Reports, 7(1), 2515. 10.1038/s41598-017-02828-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


