Abstract
Background
The presence of medial tibial osteophytes on knee radiographs suggests cartilage wear, but may be associated with medial meniscus extrusion (MME). The joint space width of the medial compartment consists anatomically of cartilage and the medial meniscus, but which is most responsible for joint space narrowing remains unclear. Magnetic resonance imaging (MRI) reveals MME and cartilage thickness.
Purposes
To determine which radiographic medial tibial osteophyte width correlates better with cartilage thickness or MME distance and which radiographic medial joint space width correlates better with cartilage thickness or MME distance.
Study Type
Cross‐sectional.
Population
Total of 527 subjects, 253 females and 274 males, aged 30–79 years, included in the Kanagawa Knee Study.
Field Strength/Sequence
3 T/fat‐suppressed spoiled gradient echo and proton density weighted.
Assessment
The medial tibial osteophyte width and “the minimum joint space width at the medial compartment” (mJSW) were measured from plain radiographs. The cartilage region was automatically extracted from MRI data using software. The medial femoral and tibial cartilage regions were each divided into nine subregions, and the average thickness of the cartilage was determined in each region and subregion. MME was manually measured by two orthopedic surgeons using MRI coronal section images.
Statistical Tests
Pearson's correlation coefficient and their comparison, with P < 0.05 considered statistically significant.
Results
The absolute values of the correlation coefficients were 0.33 at maximum between osteophyte width and cartilage thickness and 0.76 between osteophyte width and MME; the value was significantly higher with MME than with cartilage thickness (P < 0.001). The absolute values of the correlation coefficients were 0.50 at maximum between mJSW and cartilage thickness and 0.16 between mJSW and MME; the value was significantly higher with cartilage thickness than with MME (P < 0.001).
Data Conclusion
The medial tibial osteophyte width strongly reflected MME and the medial joint space width moderately reflected cartilage thickness.
Level of Evidence
3
Technical Efficacy Stage
3
Keywords: knee, MRI, radiograph, osteophyte, joint space width, medial meniscus extrusion
Osteoarthritis (OA) in the knee is most commonly diagnosed by radiographic examination of the anteroposterior view of the knee in the standing extension position. 1 The majority of knee OA is medial knee OA, which requires the evaluation of osteophytes and joint space narrowing in the medial compartment of the femorotibial joint. 2 The presence of osteophytes may be associated with cartilage wear, 3 , 4 the most characteristic feature of OA‐based changes. However, a recent report has shown an association between the medial tibial osteophyte width measured in Magnetic resonance imaging (MRI) T2 mapping and medial meniscus extrusion (MME), 5 one of the key pathologies in medial knee OA. 6 Joint space width in the medial compartment is anatomically composed of the femoral cartilage, medial meniscus (MM), and tibial cartilage from proximal to distal, but which aspect is most responsible for the relationship between tibial osteophyte width and MME.
The Kellgren and Lawrence (KL) system is a representative method for classifying the severity of OA. 7 In general, the KL system classifies OA into five grades from 0 to 4. Grades 1 and 2 are defined by the presence osteophytes and joint space narrowing, while grades 3 and 4 are defined by additional sclerosis and deformity of the bone ends. Each KL grade also had independent findings of osteophytes and joint space narrowing. This can be seen in the Atlas of Individual Radiographic Features in Osteoarthritis, 8 where these two types of radiographic features are shown as separate figures. The same KL grade may differ in its pathology between a type with prominent osteophytes and a type with prominent joint space narrowing. KL originally intended their OA classification to be used for field studies and clinical trials, 9 and it is still widely used for those purposes in practice. 10 However, failure to distinguish cases with prominent osteophytes are not distinguished from those with prominent joint space narrowing can result in the overlooking of crucial factors.
Yuan et al 11 performed transcriptome analysis from tissues of OA patients and reported that collagen catabolism increased in the type with prominent osteophytes, whereas immune responses increased in the type with prominent joint space narrowing. Consequently, in terms of developing novel therapeutic approaches, the treatment required for these different types of cases may vary. For cases with increased collagen catabolism, the therapeutic goal may be providing an efficient supply of collagen, whereas for those with increased immune responses, anti‐inflammation may be the therapeutic target. 11 The slow development of disease‐modifying OA drugs (DMOADs) 12 may therefore reflect issues with subjects in clinical trials, as the focus is on matching KL grades, rather than on distinguishing between these two types.
The purpose of the present study was to determine whether the medial tibial osteophyte width, determined radiographically, was better correlated better with cartilage thickness or MME distance. A second aim was to determine whether the radiographic medial joint space width was better correlated with cartilage thickness or with MME distance.
Subjects and Methods
Kanagawa Knee Study and Subject Enrollment
This study was approved by our institutional review board (Medical Research Ethics Committee of Tokyo Medical and Dental University), and all subjects provided written informed consent.
Subjects were excluded if they had a history of knee OA, lower extremity trauma, previous surgery, rheumatoid arthritis, or consecutive visits to the hospital for more than 3 months. Knee radiographs and MRI scans were performed between September 1, 2018, and August 30, 2019. Height and weight were also obtained and body mass index (BMI) was evaluated.
Measurements of Osteophyte and Minimum Joint Space Widths in Radiographs
Radiographs were taken of the anteroposterior view of the knee with the patient in a standing position with knee full extension (Fig. 1a). DICOM data were imported into a dedicated viewer (RadiAnt DICOM viewer 2020.1.1, Medixant, Poznań, Poland) and enlarged to fit a 24‐inch display. A single orthopedic surgeon (S.S.) with 4 years of experience measured the medial tibial osteophyte width (Fig. 1b) in 527 subjects using the length measurement tool of the viewer. Another orthopedic surgeon (Y.M.) with 4 years of experience also measured the medial tibial osteophyte width in 50 subjects to provide inter‐rater reliability. “The minimum joint space width at the medial compartment” (mJSW; Fig. 1c) 13 in 527 subjects was measured by single orthopedic surgeon (Y.M.). 14 Another orthopedic surgeon (S.S.) also measured mJSW in 50 subjects to provide inter‐rater reliability.
FIGURE 1.
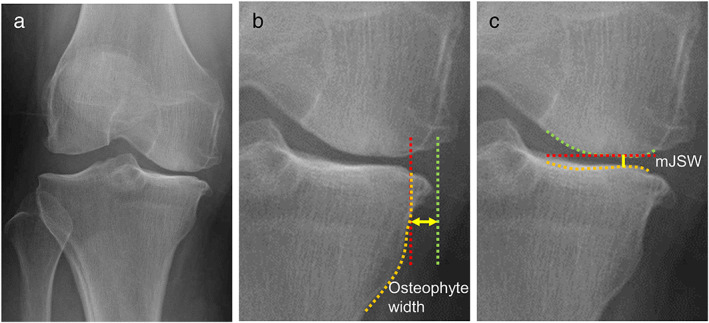
Measurement methods used with radiographs. (a) Representative radiograph—anteroposterior view of a subject standing with the knee extended. (b) Measurement of osteophyte width. A line along the medial edge of the tibia (orange line) is drawn. A vertical line (red line) is then drawn from the point of the intersection of that line and the articular surface. A third line (green line) is drawn from the inner edge of the osteophyte of the medial tibia. The distance between the red and green lines is defined as the osteophyte width (yellow arrow). (c) Measurement of the mJSW. A bright radio‐dense zone (orange line), defined at the anterior edge of the medial tibia, was drawn. A horizontal straight line (red line) was also drawn at the lowest end of the medial femoral condyle (green line). The minimum distance between these two lines was defined as mJSW (yellow line). mJSW, minimum joint space width at the medial compartment.
MRI Scanning
MRI was performed at 3.0 T (Achieva 3.0TX, Philips, Amsterdam, Netherlands) with a 16‐channel coil. Images in the sagittal plane of the knee joint were acquired with both a fat‐suppressed spoiled gradient echo sequence image (SPGR) and a proton density weighted (PDW) image (Table 1).
TABLE 1.
Imaging Parameters for the MRI Sequences
| SPGR | PDW | |
|---|---|---|
| Repetition time (msec) | 20 | 1000 |
| Echo time (msec) | 1st: 7 | 35 |
| 2nd: 13.8 | ||
| Flip angles (°) | 35 | 90 |
| Echo train length | (−) | 32 |
| Acquisition voxel size (mm) | 0.6 × 0.6 × 0.6 | 0.6 × 0.6 × 0.6 |
| Reconstruction matrix size (mm) | 0.3 × 0.3 × 0.3 | 0.3 × 0.3 × 0.3 |
| No. of sections | 320 | 320 |
| Slice thickness (mm) | 0.3 | 0.3 |
| Slice gap (mm) | 0 | 0 |
| Field of view (mm × mm) | 150 × 150 | 150 × 150 |
| WFS/BW (pix/Hz) | 2.002/217.0 | 0.836/519.4 |
| Number of excitations | 1 | 1 |
| Total examination time | 7 min 30 sec | 7 min 10 sec |
SPGR = fat‐suppressed spoiled gradient echo; PDW = proton density weighted; WFS/BW = actual waterfat shift/bandwidth; MRI = magnetic resonance imaging.
Measurements of Cartilage Thickness
The software for MRI analyses was a three‐dimensional image analysis system volume analyzer (SYNAPSE 3D (Japanese product name: SYNAPSE VINCENT), collaborative version, FUJIFILM Corporation, Tokyo, Japan). A three‐dimensional convolutional neural network (3D‐CNN) algorithm for segmentation of bone, cartilage, and region of interest (ROI) was constructed based on U‐Net containing an encoder and a decoder. The outputs were probability maps of the target regions, including the background region. Each pixel in the image was assigned a number as the region label for that pixel, and segmentation of the image was obtained. 15
The PDW images, bone region, and ROI were automatically segmented. The SPGR images were used for automatic segmentation of the cartilage region, and then the 3D image with ROI was reconstructed. The femoral cartilage was projected radially around the intercondylar axis. The center of the condyle was determined by approximating the condyle to an ellipse from a lateral view. The software provided cartilage thickness mapping by displaying cartilage thickness as a color scale; thick areas were represented in white and thin areas in red (Fig. 2a). The thickness of the cartilage was defined as the unit volume of the cartilage and included a vertical line drawn across the subchondral surface divided by the unit area of the subchondral surface. The software automatically divided the ROI of femoral cartilage into three regions (medial femoral, lateral femoral, and trochlear femoral) based on the shape of the ROI and then further divided each region into nine subregions based on the shape of each region. The software also showed a three‐dimensional view of the femoral cartilage from below along the long axis of the femur (Fig. 2b). The tibial cartilage was divided into two regions (medial tibial and lateral tibial), and each region was divided into nine subregions by dividing the ROI into three equal parts horizontally and vertically. 15 In this study, only the medial compartment was analyzed (Fig. 2c). The average cartilage thicknesses at two regions and 18 subregions were obtained, and the correlation with the medial tibial osteophyte width and mJSW in the radiographic analysis was examined for each of them.
FIGURE 2.
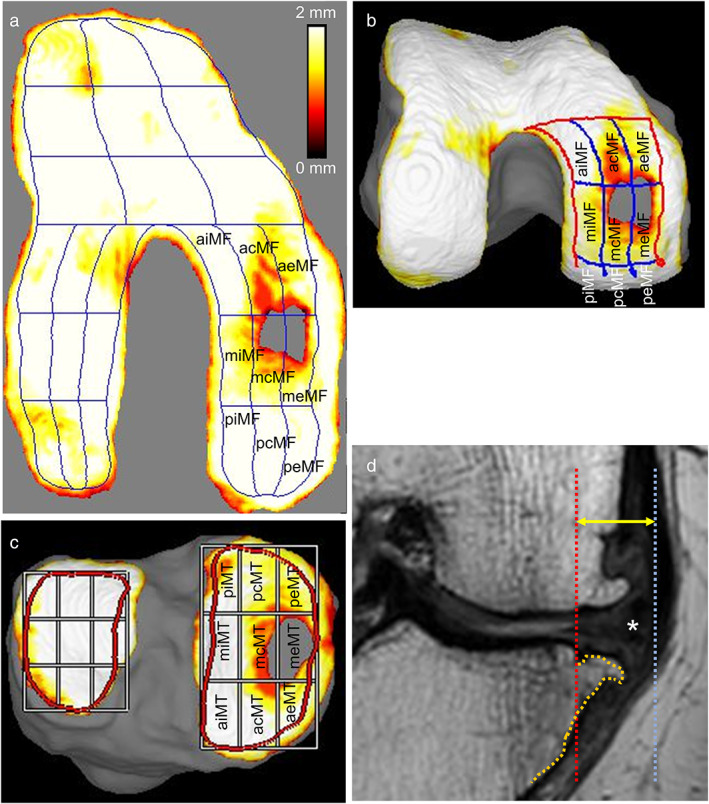
Subregions and MME measurement methods in MRI. The knee shown in Fig. 1 is further examined. (a) Radially projected cartilage thickness mapping of the femoral cartilage and subregions of the medial femoral cartilage. The MF region is the combined area of the nine MF subregions. Cartilage thickness is shown with a color bar. (b) Three‐dimensional femoral cartilage viewed from below along the long axis of the femur. Subregions of the medial femoral cartilage are also shown. (c) Three‐dimensional tibial cartilage and subregions of the medial tibial cartilage. The MT region is the combined area of the nine MT subregions. (d) Measurement of MME. A line along the medial edge of the tibia (orange line) is drawn using a coronal plane MR. A vertical line (red line) is then drawn from the point of the intersection of that line, excluding the osteophytes, and the articular surface. A third line (blue line) is drawn from the outer edge of the MM (asterisk). The distance between the red and blue lines is defined as the MME distance (yellow arrow). acMF, anterior central MF; acMT, anterior central MT; aeMF, anterior external MF; aeMT, anterior external MT; aiMF, anterior internal MF; aiMT, anterior internal MT; mcMF, middle central MF; mcMT, middle central MT; meMF, middle external MF; meMT, middle external MT; MF, medial femoral; miMF, middle internal MF; miMT, middle internal MT; MME, medial meniscus extrusion; MRI, magnetic resonance imaging; MT, medial tibial; pcMF, posterior central MF; pcMT, posterior central MT; peMF, posterior external MF; peMT, posterior external MT; piMF, posterior internal MF; piMT, posterior internal MT.
Measurements of MME by MRI
The MRI DICOM data were analyzed independently by two orthopedic surgeons (S.S. and Y.M.) using the software. The MRI measurements by S.S. were used for comparison with radiographic measurements, and the MRI measurements by Y.M. were used for inter‐rater reliability. Coronal cross‐section images were reconstructed from MRI data of PDW sagittal cross‐section images. The slice showing the maximum transverse diameter of the tibia was selected. A perpendicular line was drawn from the inner edge of the tibia, excluding the osteophyte. A perpendicular line was also drawn from the outer edge of MM. The distance between these two perpendicular lines was defined as the MME 16 (Fig. 2d).
Anatomical Relationship Between the Tibial Osteophyte and MME in a Surgical Case
The subject was an 84‐year‐old female who was not enrolled in the Kanagawa Knee Study and who underwent total knee arthroplasty for advanced OA of the right knee. The medial tibial osteophyte was exposed intraoperatively and photographed. The MM was then returned to its original position and photographed again.
Statistical Analysis
Pearson's correlation coefficient was used to evaluate the association between the osteophyte and each cartilage thickness and between the osteophyte and MME. A P value <0.05 was considered statistically significant. Correction for multiple comparisons was performed for cartilage thickness, and the P value was set at 0.0025 (=0.05/20) because the analysis was performed for a total of 20 areas in the region and subregion.
Inter‐rater reliability was assessed with the intraclass correlation coefficient (ICC) and was shown with its 95% confidence interval. For the osteophyte width and mJSW, 50 subjects (five females and five males in their 30s, 40s, 50s, 60s, and 70s) were randomly selected and measured independently by two examiners (S.S. and Y.M.) from blinded radiographic data. If the reliability of this partial selection was low, we planned to have all 527 subjects measured by multiple examiners. For the MME, 527 subjects were selected and independently measured by two examiners (S.S. and Y.M.).
All statistical analyses including correlation analysis, ICC, comparison of correlation coefficients, and outlier analysis were performed using the BellCurve software for Excel (Social Survey Research Information Co., Ltd., Tokyo, Japan).
Correlation coefficients of 0.00–0.19 were considered “very weak,” 0.20–0.39 as “weak,” 0.40–0.59 as “moderate,” 0.60–0.79 as “strong,” and 0.80–1.0 as “very strong.” 17
Results
Characteristics of Subjects
In total, 573 subjects were enrolled, but 11 withdrew, and one had ineligible data, leaving 561 participants for the study. Six subjects with lateral knee OA were subsequently excluded, and a further 28 subjects with inappropriate radiographs were also excluded, leaving a total of 527 subjects who were included in the current analysis (Fig. 3). The decision for inclusion was first made visually and independently by two orthopedic surgeons (S.S. and Y.M.) and then finalized by one (I.S.) with 30 years of experience. The 527 subjects included 254 (48%) females and 273 (52%) males; the average age was 54 ± 14 years (average ± standard deviation [SD]) and the average BMI was 23 ± 3 kg/m2. The KL grading scale in the extension view identified 508 (96.4%) subjects with grade 0 or 1 knee OA; nine (1.7%) with grade 2; seven (1.3%) with grade 3; and three (0.6%) with grade 4.
FIGURE 3.
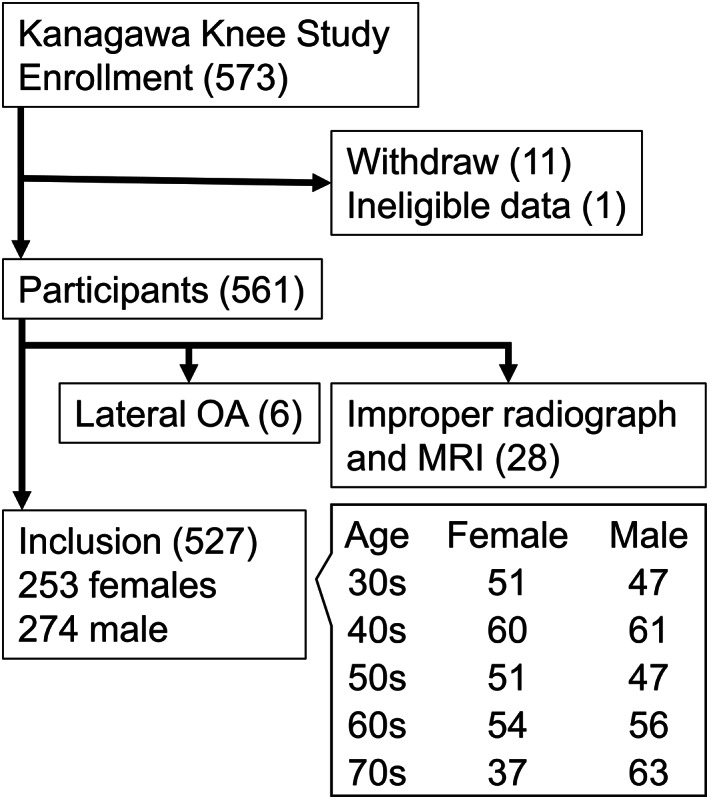
Flow chart for the study enrollment and age breakdown. Initially, 573 subjects were enrolled, but 11 withdrew, and one had ineligible data, leaving 561 participated in the study. A further 34 subjects were excluded, leaving a total of 527 subjects aged 30–79 years that were included in the current analysis. MRI, magnetic resonance imaging; OA, osteoarthritis.
Inter‐rater Reliability of Osteophyte and MME Measurements
The inter‐rater reliability (ICC 2, 1) was 0.85 (95% confidence interval [CI], 0.75–0.91) for osteophyte width, 0.89 (95% CI, 0.81–0.94) for mJSW, and 0.90 (95% CI, 0.87–0.92) for MME distance. These results indicated strong reliability. 18
Correlation of Osteophyte Width With Cartilage Thickness and With MME Distance
Osteophyte width and cartilage thickness showed significantly negative correlations in the following subregions: middle central medial femoral (mcMF; r = −0.13) and anterior central MF (acMF; r = −0.18) in the medial femur, and middle external medial tibial (meMT; r = −0.33), middle central MT (mcMT; r = −0.26), and anterior internal MT (aiMT; r = 0.03) in the medial tibia (Table 2). Among these, the lowest correlation coefficient was found for meMT (Fig. 4a). Osteophyte width and MME distance were significantly positively correlated, with a correlation coefficient of 0.76 (Fig. 4a).
TABLE 2.
Correlations Between the Osteophyte Width (mm) and Cartilage Thickness (mm) at Regions and Subregions in the Medial Compartment (n = 527)
| r | P Value | ||
|---|---|---|---|
| MF | Region | −0.05 | 2.2E‐01 |
| peMF | Subregion | 0.14* | 1.1E‐03 |
| meMF | Subregion | 0.09 | 4.3E‐02 |
| aeMF | Subregion | 0.00 | 9.2E‐01 |
| pcMF | Subregion | −0.02 | 6.3E‐01 |
| mcMF | Subregion | −0.13* | 2.4E‐03 |
| acMF | Subregion | −0.18* | 3.9E‐05 |
| piMF | Subregion | 0.07 | 9.5E‐02 |
| miMF | Subregion | −0.13 | 2.8E‐03 |
| aiMF | Subregion | −0.07 | 1.1E‐01 |
| MT | Region | −0.05 | 2.2E‐01 |
| peMT | Subregion | −0.10 | 2.1E‐02 |
| meMT | Subregion | −0.33 * | 5.1E‐15 |
| aeMT | Subregion | −0.09 | 4.8E‐02 |
| pcMT | Subregion | 0.02 | 6.0E‐01 |
| mcMT | Subregion | −0.26* | 1.3E‐09 |
| acMT | Subregion | 0.01 | 7.9E‐01 |
| piMT | Subregion | 0.17* | 8.5E‐05 |
| miMT | Subregion | 0.03 | 5.1E‐01 |
| aiMT | Subregion | 0.22* | 2.8E‐07 |
The set with the largest absolute value of the correlation coefficient is shown in bold.
r = correlation coefficient; MF = medial femoral; aiMF = anterior internal MF; acMF = anterior central MF; aeMF = anterior external MF; miMF = middle internal MF; mcMF = middle central MF; meMF = middle external MF; piMF = posterior internal MF; pcMF = posterior central MF; peMF = posterior external MF; MT = medial tibial; piMT = posterior internal MT; pcMT = posterior central MT; peMT = posterior external MT; miMT = middle internal MT; mcMT = middle central MT; meMT = middle external MT; aiMT = anterior internal MT; acMT = anterior central MT; aeMT = anterior external MT.
P < 0.0025.
FIGURE 4.
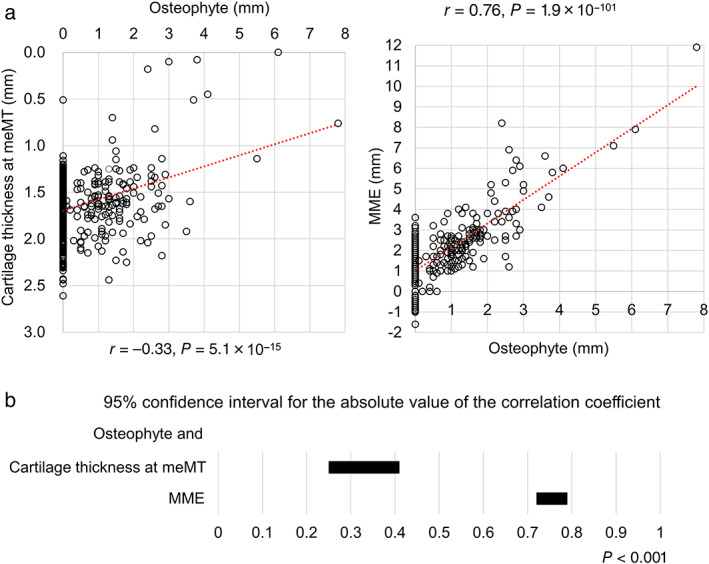
Correlation between the osteophyte width and cartilage thickness and between the osteophyte width and MME distance. (a) Scatterplots between osteophyte thickness and cartilage thickness at the meMT subregion and between the osteophyte width and MME distance. The correlation coefficient (r) and P values are shown. (b) 95% confidence interval for the absolute value of the correlation coefficient. meMT, middle external medial tibial; MME, medial meniscus extrusion.
The 95% CI for the absolute value of the correlation coefficient between the osteophyte width and cartilage thickness was 0.25–0.41 at meMT (the area with the highest correlation out of a total of 20 areas in the region and subregion). On the other hand, the 95% CI for the absolute value of the correlation coefficient between the osteophyte width and MME distance was 0.72–0.79. The correlation coefficient was significantly higher for the MME than for cartilage thickness (P < 0.001; Fig. 4b).
Anatomical Relationship Between the Tibial Osteophyte Width and MME in a Surgical Case
We observed the medial tibial osteophyte and the MM in an advanced OA knee during total knee arthroplasty to determine the anatomical relationship between the tibial osteophyte width and MME. Osteophytes are observed after detachment of the periosteum of the proximal medial tibia and peeling off the joint capsule along with the MM (Fig. 5a). Subsequently, when the outer 1/3 of the MM is cut circumferentially from the anterior to the middle segment and returned to its original position, the MM could be seen to be located above the medial tibial osteophyte (Fig. 5b).
FIGURE 5.
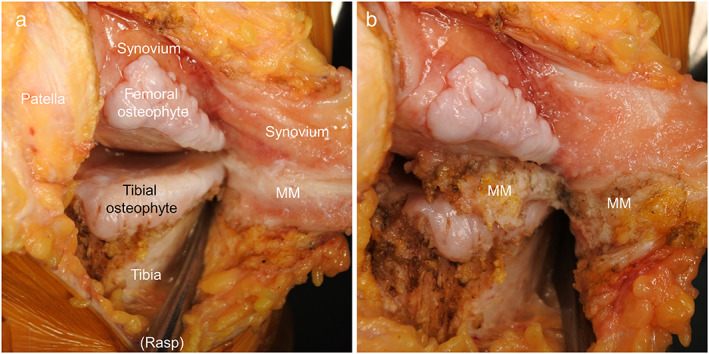
Anatomical relationship between the tibial osteophyte width and the MM in severe OA knees observed during total knee arthroplasty. (a) Medial tibial osteophyte. The medial periosteum of the tibia was detached from anterior to medial using a rasp. (b) Position of MM in relation to osteophytes. MM was returned to its original position before exposing the medial tibial osteophyte by cutting the outer 1/3 of the MM from the anterior to the middle segment to remove the tension applied to the MM. MM, medial meniscus; OA, osteoarthritis.
Correlation of the mJSW With Cartilage Thickness and With the MME Distance
The mJSW and cartilage thickness were significantly positively correlated in the MF region (r = 0.38) and in seven subregions in the medial femur (r = 0.29–0.46), as well as in the MT region (r = 0.49) and in all nine subregions in the medial tibia (r = 0.14–0.50) (Table 3). The highest correlation coefficient was found for meMT (r = 0.50) (Fig. 6a). The mJSW and MME distance were significantly negatively correlated (r = −0.16; Fig. 6a).
TABLE 3.
Correlations Between the mJSW (mm) and Cartilage Thickness (mm) at Regions and Subregions in the Medial Compartment (n = 527)
| r | P Value | ||
|---|---|---|---|
| MF | Region | 0.38* | 4.2E‐19 |
| peMF | Subregion | −0.04 | 3.7E‐01 |
| meMF | Subregion | 0.29* | 1.1E‐11 |
| aeMF | Subregion | 0.39* | 2.9E‐20 |
| pcMF | Subregion | 0.11 | 1.3E‐02 |
| mcMF | Subregion | 0.35* | 1.5E‐16 |
| acMF | Subregion | 0.46* | 1.2E‐28 |
| piMF | Subregion | 0.11 | 1.5E‐02 |
| miMF | Subregion | 0.34* | 6.0E‐16 |
| aiMF | Subregion | 0.38* | 1.4E‐19 |
| MT | Region | 0.49* | 1.5E‐32 |
| peMT | Subregion | 0.32* | 1.2E‐13 |
| meMT | Subregion | 0.50 * | 5.9E‐34 |
| aeMT | Subregion | 0.46* | 3.1E‐29 |
| pcMT | Subregion | 0.29* | 1.3E‐11 |
| mcMT | Subregion | 0.47* | 6.4E‐30 |
| acMT | Subregion | 0.44* | 2.4E‐26 |
| piMT | Subregion | 0.14* | 1.3E‐03 |
| miMT | Subregion | 0.37* | 5.8E‐19 |
| aiMT | Subregion | 0.27* | 2.5E‐10 |
The set with the largest absolute value of the correlation coefficient is shown in bold.
mJSW = minimum joint space width at the medial compartment; r = correlation coefficient; MF = medial femoral; aiMF = anterior internal MF; acMF = anterior central MF; aeMF = anterior external MF; miMF = middle internal MF; mcMF = middle central MF; meMF = middle external MF; piMF = posterior internal MF; pcMF = posterior central MF; peMF = posterior external MF; MT = medial tibial; piMT = posterior internal MT; pcMT = posterior central MT; peMT = posterior external MT; miMT = middle internal MT; mcMT = middle central MT; meMT = middle external MT; aiMT = anterior internal MT; acMT = anterior central MT; aeMT = anterior external MT.
P < 0.0025.
FIGURE 6.
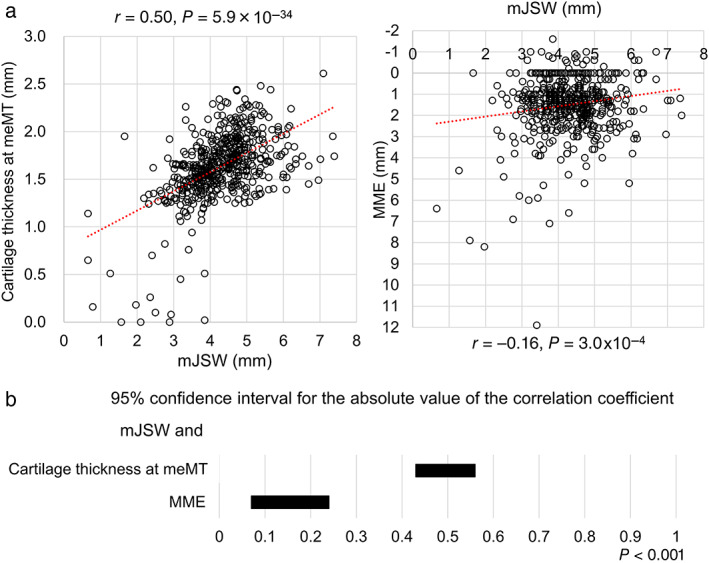
Correlation between the mJSW and cartilage thickness and between the mJSW and MME distance. (a) Scatterplots between mJSW and cartilage thickness at meMT subregion and between mJSW and MME distance. The correlation coefficient (r) and P values are shown. (b) 95% confidence interval for the absolute value of the correlation coefficient. meMT, middle external medial tibial; mJSW, minimum joint space width at the medial compartment; MME, medial meniscus extrusion.
The 95% CI for the absolute value of the correlation coefficient between mJSW and cartilage thickness at meMT (the area with the highest correlation out of a total of 20 areas in the region and subregion) was 0.43–0.56. On the other hand, the 95% CI for the absolute value of the correlation coefficient between mJSW and MME distance was 0.07–0.24. The correlation coefficient was significantly higher for the cartilage thickness than for MME (P < 0.001; Fig. 6b).
Discussion
The observation of medial tibial osteophytes is considered indicative of cartilage wear in OA, but it has also been reported to be associated with MME. 3 , 4 Joint space narrowing at the medial compartment is another important radiographic feature of medial OA, but whether the femoral cartilage, MM, or tibial cartilage is most responsible for its occurrence is unclear. This study examined whether the medial tibial osteophyte width had a greater correlation with cartilage thickness or MME distance, and whether the medial joint space width had a greater correlation with cartilage thickness or with MME distance. The results showed that the medial tibial osteophyte width was better correlated with MME and, conversely, that mJSW was better correlated better with cartilage thickness.
Medial Tibial Osteophyte and MME
Osteophytes are a representative feature of OA in the knee and can be identified in plain radiographs. 19 Osteophyte formation is generally considered to represent a repair process of the degenerated articular cartilage in knee OA. 3 , 4 However, many clinical studies have shown that radiographs are not always sufficiently specific to predict the presence of cartilage lesions in the same compartment of the knee joint. 20 , 21 , 22 , 23 The findings presented here showed that cartilage thickness was only weakly correlated with osteophyte width in seven of the 18 subregions. The lowest value of the correlation coefficient was at the meMT subregion, where a negative correlation was found between osteophyte width and cartilage thickness. The medial tibial osteophytes observed on radiographs taken in the anteroposterior direction of the knee should be continuous from the aeMT, meMT, or peMT. This study did not consider which of the three subregions had the largest osteophytes; however, the osteophytes connected to the meMT subregion are presumed to have the greatest involvement since they are perpendicular to the irradiation line. These results suggest that cartilage loss and osteophyte formation could be associated, although not strongly.
MME is one of the most critical pathologies of medial knee OA. 6 MRI‐based studies were the first to generate the concept of MME, which denotes a medial shift of the MM 24 , 25 and a subsequent dysfunction of load distribution, which is one of the most important functions of the meniscus. 26 Since Adams et al 24 first reported in 1999 that meniscus extrusion and cartilage loss contribute to the narrowing of the joint space in knee OA, the association between MME and OA has been attracting attention. However, we were unable to find any studies that examined the relationship between radiographic osteophyte width and MME using scatter plots. Hada et al 5 divided the medial tibial osteophyte into a bone and cartilage portion using T2 mapping in 50 patients with medial knee OA of KL grade 0–2 and showed that both osteochondrophyte width and chondrophyte width were correlated with MME, whereas the osteophyte width was not. Conversely, we demonstrated that MME had a strong correlation with the medial tibial osteophyte width measured on radiographs. The difference between these results may reflect the difference in the assessment of osteophytes between MRI and radiographs, differences between the patient and volunteer populations, and differences in sample size (50 and 527).
The scatter plots between osteophyte width and cartilage thickness, and between osteophyte width and MME distance contained some osteophyte widths that appeared to be outliers. A Smirnov‐Grubbs analysis was used to evaluate eight points with an osteophyte width greater than 3.5 mm as outliers. Exclusion of those eight values decreased the correlation coefficient between osteophyte width and cartilage to −0.17 (n = 519, P = 8.6 × 10−5) and between osteophyte width and MME distance to 0.66 (n = 519, P = 1.1 × 10−65). However, the correlation coefficient between osteophyte width and MME distance still remained greater than the correlation coefficient between osteophyte width and cartilage thickness. However, since these eight outliers are not abnormal values due to errors in measurement, recording, or data input, we have retained them in the present analysis.
The association between osteophyte width and MME can be confirmed by the intraoperative findings of total knee arthroplasty. The MM can be found above the medial tibial osteophyte in advanced knee OA, and this supports the correlation between osteophyte width and MME.
Medial Joint Space Narrowing and Cartilage Thickness
The mJSW is composed of femoral cartilage, the MM, and tibial cartilage based on anatomy, but which component is the most important cannot yet be determined. Some reports have indicated an involvement of cartilage thickness, 27 , 28 while others have indicated an involvement of MME in the mJSW. 24 , 29 Buckland‐Wright et al 27 measured the mJSW from weight bearing plain radiographs taken from the tunnel view and compared them with the sum of the femoral and tibial cartilage thicknesses measured from double contrast arthrograms obtained in the nonweight bearing position in 54 subjects. The mJSW was highly correlated with the sum of the tibial and femoral cartilage thicknesses but the potential contribution of the MM was not mentioned. Khury et al 28 measured the mJSW on posteroanterior standardized‐flexion radiographs and cartilage thickness at 16 subregions of the femorotibial compartment in MRIs. The mJSW was significantly associated with cartilage thickness in the medial femorotibial compartments of 345 neutral‐alignment knees, but the potential contribution of the MM was again ignored. Conversely, Adams et al 24 assessed the mJSW on conventional radiographs and the degree of MME on two‐dimensional MRIs. Statistically significant differences were found in the degree of MMEs graded as 1–3 in the nine patients with joint space narrowing of KL grades 1–2 and the 23 patients with joint space narrowing of KL grades 3–4. However, their study did not assess cartilage thickness in the MRIs. Hunter et al 29 measured the mJSW using the Lyon Schuss knee radiograph (taken in flexion) and cartilage thickness at several subregions obtained via MRI using custom software in 62 obese females with knee OA and in 99 nonobese female controls. They showed that both the articular cartilage morphometry and meniscus position were related to the mJSW in knee radiographs. They mentioned that both the cartilage thickness and MME contributed to the mJSW, but their report differs from our study in terms of both the knee flexion angle during radiography and the number of cases.
Clinical Relevance
MME can be detected by evaluating the medial tibial osteophyte width on plain radiographic images. MRI and ultrasound can directly evaluate MME, but these methods are not usually the first choice for imaging of the knee. Plain radiographs remain a mainstay in the primary evaluation of OA because of their accessibility and relatively low cost, 30 meaning that the ability to assess the abnormalities of MME using only routine diagnostic imaging of the knee would be very beneficial in clinical practice.
Distinguishing between structural changes in the cartilage and the meniscus is important in the diagnosis of OA because the pathophysiology of the two tissues is different, as is the treatment. DMOADs 31 primarily target the improvement of cartilage metabolism; their development has been long expected, but delayed. This may reflect the fact that the patients have been included in clinical trials based only on their KL grades or joint space widths, and not strictly on osteophyte width. For example, for the Sprifermin (rhFGF18) trial, the inclusion criteria were KL grades of 2 or 3 with an mJSW of 2.5 mm or greater in the medial compartment, but no specific description of the osteophytes was given. 32 Making the range of osteophyte widths similar in the subject population indicates that the range of MME distance will also be similar, allowing for a stricter comparison. The treatment for improving MME does not involve the administration of DMOADs and centralization surgery is generally required to reposition and stabilize the extruded MM. 33 In addition, meniscus injury and meniscectomy are risk factors for MME, 34 and meniscus repair surgery is important to prevent it.
Limitations
One limitation of this study is the presence of selection bias because the study subjects were not randomly selected from the general population. The volunteers were recruited from desk workers but excluded those with a history of lower extremity trauma, surgery, or hospital visits for knee disease for more than three months. This resulted in a high proportion of KL grades 0 or 1. A second limitation was that the osteophyte width measurements on the radiographs and MME on MRIs were performed manually. The inter‐rater reliability of each measurement is reliable, but the potential for measurement errors cannot be ignored. Another limitation is that the measurements of osteophyte width, cartilage thickness, and MME were not corrected for patient height or BMI. According to our previous report, in which we analyzed data from the Kanagawa Knee Study, the thickness of the medial tibial cartilage was correlated with height, but only weakly, with a correlation coefficient of 0.2. 15
Conclusion
The medial tibial osteophyte width was strongly correlated with MME, but not with cartilage thickness. Conversely, the medial joint space width was moderately correlated with cartilage thickness, but only very weakly with MME. These results clarify the importance of determining both osteophyte width and joint space width in plain radiographs. They also provide an opportunity to develop a more detailed radiographic classification of OA according to pathological conditions, and can assist in finding suitable treatments for OA in a more homogeneous patient population, as classified by radiographs.
Acknowledgments
We thank Kimiko Takanashi for managing our laboratory and Ellen Roider for English editing.
I.S. has received research funding and MRI analysis software from Fujifilm.
References
- 1. Hellio Le Graverand MP, Mazzuca S, Duryea J, Brett A. Radiographic‐based grading methods and radiographic measurement of joint space width in osteoarthritis. Radiol Clin North Am 2009;47:567‐579. [DOI] [PubMed] [Google Scholar]
- 2. McCormack DJ, Puttock D, Godsiff SP. Medial compartment osteoarthritis of the knee: A review of surgical options. EFORT Open Rev 2021;6:113‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Abramson SB, Attur M. Developments in the scientific understanding of osteoarthritis. Arthritis Res Ther 2009;11:227‐235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van der Kraan PM, van den Berg WB. Osteophytes: Relevance and biology. Osteoarthr Cartil 2007;15:237‐244. [DOI] [PubMed] [Google Scholar]
- 5. Hada S, Ishijima M, Kaneko H, et al. Association of medial meniscal extrusion with medial tibial osteophyte distance detected by T2 mapping MRI in patients with early‐stage knee osteoarthritis. Arthritis Res Ther 2017;19:201‐212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Berthiaume MJ, Raynauld JP, Martel‐Pelletier J, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 2005;64:556‐563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren‐Lawrence classification of osteoarthritis. Clin Orthop Relat Res 2016;474:1886‐1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthr Cartil 2007;15(Suppl 1):A1‐A56. [DOI] [PubMed] [Google Scholar]
- 9. Kellgren JH, Lawrence JS. Radiological assessment of osteo‐arthrosis. Ann Rheum Dis 1957;16:494‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Palmer JS, Monk AP, Hopewell S, et al. Surgical interventions for symptomatic mild to moderate knee osteoarthritis. Cochrane Database Syst Rev 2019;7:Cd012128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yuan C, Pan Z, Zhao K, et al. Classification of four distinct osteoarthritis subtypes with a knee joint tissue transcriptome atlas. Bone Res 2020;8:38‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Oo WM, Liu X, Hunter DJ. Pharmacodynamics, efficacy, safety and administration of intra‐articular therapies for knee osteoarthritis. Expert Opin Drug Metab Toxicol 2019;15:1021‐1032. [DOI] [PubMed] [Google Scholar]
- 13. Roth M, Emmanuel K, Wirth W, Kwoh CK, Hunter DJ, Eckstein F. Sensitivity to change and association of three‐dimensional meniscal measures with radiographic joint space width loss in rapid clinical progression of knee osteoarthritis. Eur Radiol 2018;28:1844‐1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Miura Y, Ozeki N, Katano H, et al. Difference in the joint space of the medial knee compartment between full extension and Rosenberg weight‐bearing radiographs. Eur Radiol 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aoki H, Ozeki N, Katano H, et al. Relationship between medial meniscus extrusion and cartilage measurements in the knee by fully automatic three‐dimensional MRI analysis. BMC Musculoskelet Disord 2020;21:742‐750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: Detection, evaluation and clinical implications. Eur J Radiol 2018;102:115‐124. [DOI] [PubMed] [Google Scholar]
- 17. Evans JD. Straightforward statistics for the behavioral sciences. Belmont: Thomson Brooks/Cole Publishing Co; 1996. [Google Scholar]
- 18. Koo TK, Li MY. A guideline of selecting and reporting Intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155‐163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA 2021;325:568‐578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Boegård T, Rudling O, Petersson IF, Jonsson K. Correlation between radiographically diagnosed osteophytes and magnetic resonance detected cartilage defects in the patellofemoral joint. Ann Rheum Dis 1998;57:395‐400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brandt KD, Fife RS, Braunstein EM, Katz B. Radiographic grading of the severity of knee osteoarthritis: Relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum 1991;34:1381‐1386. [DOI] [PubMed] [Google Scholar]
- 22. Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, De Smet AA. Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology 2006;239:818‐824. [DOI] [PubMed] [Google Scholar]
- 23. Markhardt BK, Li G, Kijowski R. The clinical significance of osteophytes in compartments of the knee joint with normal articular cartilage. AJR Am J Roentgenol 2018;210:W164‐W171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 1999;54:502‐506. [DOI] [PubMed] [Google Scholar]
- 25. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: Is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol 2004;183:17‐23. [DOI] [PubMed] [Google Scholar]
- 26. Wenger A, Wirth W, Hudelmaier M, et al. Meniscus body position, size, and shape in persons with and persons without radiographic knee osteoarthritis: Quantitative analyses of knee magnetic resonance images from the osteoarthritis initiative. Arthritis Rheum 2013;65:1804‐1811. [DOI] [PubMed] [Google Scholar]
- 27. Buckland‐Wright JC, Macfarlane DG, Lynch JA, Jasani MK, Bradshaw CR. Joint space width measures cartilage thickness in osteoarthritis of the knee: High resolution plain film and double contrast macroradiographic investigation. Ann Rheum Dis 1995;54:263‐268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Khury F, Fuchs M, Awan Malik H, Leiprecht J, Reichel H, Faschingbauer M. Validation of joint space narrowing on plain radiographs and its relevance to partial knee arthroplasty. Bone Joint Res 2021;10:173‐187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hunter DJ, Buck R, Vignon E, et al. Relation of regional articular cartilage morphometry and meniscal position by MRI to joint space width in knee radiographs. Osteoarthr Cartil 2009;17:1170‐1176. [DOI] [PubMed] [Google Scholar]
- 30. Braun HJ, Gold GE. Diagnosis of osteoarthritis: Imaging. Bone 2012;51:278‐288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mehta S, He T, Bajpayee AG. Recent advances in targeted drug delivery for treatment of osteoarthritis. Curr Opin Rheumatol 2021;33:94‐109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hochberg MC, Guermazi A, Guehring H, et al. Effect of intra‐articular sprifermin vs placebo on femorotibial joint cartilage thickness in patients with osteoarthritis: The FORWARD randomized clinical trial. JAMA 2019;322:1360‐1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Katagiri H, Nakagawa Y, Miyatake K, et al. Short‐term outcomes after high tibial osteotomy aimed at neutral alignment combined with arthroscopic centralization of medial meniscus in osteoarthritis patients. J Knee Surg 2021. [DOI] [PubMed] [Google Scholar]
- 34. Crema MD, Roemer FW, Felson DT, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: The multicenter osteoarthritis study. Radiology 2012;264:494‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]


