Abstract
Introduction
There is a growing drive to improve the heterogeneity of medical school cohorts. However, those from lower socio‐economic groups remain under‐represented. Understanding the methods used by applicants to prepare for medical school selection, and the challenges they face with respect to opportunities and access, may provide important insights to this lack of diversity. This research considered the influence of socio‐demographic background on preparation for medical school selection and on the successful offer of a place.
Methods
All eligible applicants to a large UK medical school were invited to complete an anonymous online survey (international and mature applicants excluded), detailing demographic data and experiences of preparing for selection and challenges faced (n = 1885). Selection outcomes across all UK medical schools were examined for consenting students (n = 955). Univariate and multivariate analyses explored the associations of preparatory activities and demographic data with subsequent offer of a place at a UK medical school.
Results
The survey response rate was 66.4%. Clinical work experience (hospital or general practice), fee‐based courses for admissions tests and school preparation courses for interview were activities significantly associated with the offer of a place (P < .05). Those attending independent (private) schools most frequently reported school support and fee‐based courses to support preparation (P < .01). Applicants from state non‐selective (SNS) schools and lower socio‐economic groups more frequently reported challenges in accessing fee‐based support, school interview courses and clinical work experience (P ≤ .02).
Discussion
Clinical work experience, commercial courses for admissions tests and school‐based support for interview represent areas of preparation that are associated with success. However, they also represent areas that are more challenging to access for demographic groups traditionally under‐represented in medicine. Addressing complex issues of fairness in highly selective higher education settings can appear an insurmountable task. These preparatory activities represent key areas for applicants, schools and institutions to explore and address.
Short abstract
The authors evidence preparation strategies associated with success in medical school selection while highlighting how challenging they are to access for socio‐demographic groups underrepresented in medicine.
1. INTRODUCTION
There is a growing drive to improve the demographic diversity of medical schools, to better represent the heterogeneous populations served by healthcare and to change the tide of disadvantage for those groups under‐represented in medicine. 1 Although medical schools have become increasingly diverse in terms of gender and ethnicity, the same cannot be said about the socio‐economic background of medical students. Students from lower socio‐economic classes are less likely to succeed when they apply for medicine and are less widely represented. 2 , 3 Changes to selection processes themselves, and the provision of targeted support to under‐represented groups (through the widening participation [WP] agenda), have been outlined as possible solutions. 2 , 4 However, there is not compelling evidence that the modification of selection processes has led to significant change in the demographic mix of medical schools. 3 In addition, such modification of selection processes to improve socio‐demographic representation may have unintended consequences for equitable participation. For example, admissions tests (such as aptitude tests) were introduced with a purpose to improve socio‐demographic inequality. However applicants have since described language barriers and a financial burden associated with preparing for, and sitting, these tests. 5 , 6
The WP agenda aims to address some of these inequalities for a small proportion of qualifying candidates. 7 However, it has been suggested that the implementation of such policy is varied in scope and commitment, depending on various contextual factors of the university. 2 Placing the onus on medical schools to ‘solve’ nuanced and complex issues of inequality through WP or selection methods alone seems to be a superficial solution, a view held by a number of admissions tutors. 2
From a perspective committed to improving diversity in medical schools, it has been suggested that attention to the preparation phase (‘getting ready’ to apply) is required, over and above modification of selection processes. 3 Although university admissions teams are explicit and transparent regarding the methods of selection, the means by which an applicant should prepare are typically not prescribed in detail. Similarly, the literature is unclear as to the preparatory activities most likely to lead to success. Courses run by private companies, or simply undertaking a greater number of preparatory activities, have been shown to be associated with the offer of a place at medical school in one Australian study. 8 However, some studies have questioned the benefits of commercial coaching on selection test performance and its predictive validity. 9 , 10 Extracurricular activities appear to be commonly undertaken, and significant effort made by applicants, but one study suggested this made little impact on outcomes at selection. 11 Studies that do explore applicant preparation and associations with success frequently examine outcomes from a single medical school. 8 , 11 , 12
What is also unclear from the literature is whether there are socio‐demographic disparities in opportunity and access to preparatory activities associated with success in medical school selection. In a highly competitive environment, those who wish to succeed must demonstrate cognitive ability, alongside the personal attributes expected of a student doctor. 13 Preparation for selection occurs largely outside the hegemony of medical school: in schools, colleges, homes and families. It is frequently shaped over the preceding months or years before application. Those who cannot afford or access particular opportunities may risk disadvantage, and this has been suggested in the literature on coaching support and arrangement of work experience placements. 14 , 15 , 16
2. CONCEPTUAL FRAMEWORK
The literature on inequality in education frequently draws on the work of Bourdieu, where it is suggested that education systems can ‘reproduce social inequality by exalting or enacting certain cultural practices associated with the dominant classes’. 17 Citing cultural capital, Bourdieu suggests that there are taken for granted forms and practice of knowledge within the predominant culture, which, if lacking, can limit educational success for individuals outside of that culture (or, in this case, socio‐demographic background). 18 Linked to this concept is a student's ‘habitus’. 17 , 19 Defined as ‘long lasting dispositions of the mind’, the legacies of family and childhood socialisation (the past) bring about a set of complex predispositions, which render those students from outside the predominant culture as unable to decode the implicit ‘rules of the game’. 17 , 20 , 21 Habitus has been considered in research relating to ‘first in family’ students and ‘working class’ medical students, where distinct disadvantages were suggested arising from disparities in secondary education, family income and support, education expectations, academic preparation 19 and school support. 22 These concepts provide an impetus to consider socio‐demographic differences in the preparation opportunities that applicants are afforded and the ways in which the preparation phase is navigated. Furthermore, if such opportunities are lacking in the preparatory journey of particular socio‐demographic groups, this becomes of additional importance if educational success is also limited.
This research explored the influence of socio‐demographic background on preparation for medical school selection, considering opportunities and challenges to preparation and associations with the successful offer of a place. The following research questions were investigated:
What are the common activities that applicants will undertake in their preparation to secure a place at medical school?
To what extent are difficulties experienced in accessing or arranging preparatory activities?
To what extent do particular preparatory activities, and difficulties, influence outcome at selection?
Does socio‐demographic background influence these preparatory activities or challenges?
3. METHODS
This research was conducted as part of a mixed methods programme of work at the University of Birmingham (UoB) to explore the preparatory activities of medical school applicants. The electronic survey design of this element of the research had the benefit of capturing the experiences of a broad range of respondents, across the UK applicant pool, and was particularly attractive with respect to our interest in socio‐demographic diversity. 23
3.1. Context of study
The UoB is the one of the largest in the United Kingdom, with over 2000 applicants annually for around 360 places. 24 Across the United Kingdom, medical schools have different approaches to the selection process, placing different emphases on interviews, aptitude tests and school academic achievement. The selection process at UoB requires applicants to attain threshold scores on aptitude tests and General Certificate of Secondary Education (GCSE; an academic qualification undertaken nationally at aged 15–16) to be offered an interview. The second step (independent from scores needed for an interview offer) is a Multiple‐Mini Interview, where those scoring highest are offered a place. As part of the university's WP agenda, a proportion of applicants meeting particular socio‐economic criteria receive adjustments to lower qualifying criteria, and some are also eligible to participate in the university's WP programme, which provides mentorship and additional support for application preparation. 25 , 26
When considering markers of socio‐economic status in the United Kingdom, there is no ideal measure. UK applicants typically attend state non‐selective (SNS) schools, state selective (SS) schools (SS) or independent (IND) (private) schools. 3 Participation in IND or SS education is linked with higher rates of acceptance to highly selective universities, and private education is concentrated at the very top of family income distribution. 27 , 28 School background therefore offers a rudimentary marker for socio‐economic status in the UK setting. 3 POLAR4 data classifies local geographical areas (in quintiles) across the United Kingdom according to young persons' participation rate in higher education. The 20% of areas with lowest participation in higher education are designated as ‘Quintile 1’, with the top 20% ‘Quintile 5’. 29 UoB uses both school background and Participation of Local Areas (POLAR4) data as markers of socio‐economic status, and this information was also used in our survey analysis.
3.2. Survey design
The questionnaire design was based on the results from previous narrative interviews with applicants and on focus groups with medical students. 30 , 31 All UoB UK school applicants in the 2017–2018 admissions cycle were invited to register their interest to participate in an interview and provided baseline demographic data, which was used to purposively sample participants based on school background, gender and ethnicity. Of the 687 applicants registering interest, 23 telephone interviews were undertaken. Three focus groups were also undertaken with 17 Year 1 medical students. All preparatory activities outlined by applicants (in both interviews and focus groups) were coded and used to inform the areas of preparation included within the survey. Themes from these early stages of the research also identified particular difficulties or opportunities that were experienced in accessing or arranging these activities. These findings prompted a development of questions that would explore preparatory activities undertaken and the relative ease (or difficulty) in accessing and arranging these activities. An option for free‐text responses was included. 32 The survey was piloted initially with academic clinical fellows (speciality doctors in training, involved in regular medical student teaching), and discussion with this group developed a Likert‐type scale to explore the relative ease or difficulty experienced in accessing each activity (considering the ‘obstacles’, if any, in arranging or accessing each activity). In light of our considerations around habitus and cultural capital, we included an option for respondents to indicate activities that they were not aware of, and questions were included to explore sources of support (such as help from school or family) and demographic details. A final draft of the survey was later piloted with medical student volunteers and amendments made based on feedback on question structure, additional preparatory activities and readability. Participants could consent to link their responses to Universities and Colleges Admissions Service (UCAS) outcomes, indicating offers of a place at any UK medical school. Box 1 outlines the particular domains explored within the electronic survey, and the survey itself is outlined in Appendix 1.
Box 1. Domains included within the electronic questionnaire.
□ General preparation
□ Admissions test preparation
□ Work experience
□ Interview preparation
□ Difficulties encountered
□ Demographic details
All applicants to the 5‐year MBChB programme (n = 2281; 2018–19 applicant cycle) were invited to complete a Jisc Online Survey (an electronic survey tool provided to higher education environments in the United Kingdom). Mature (already completed an undergraduate degree programme) and overseas applicants were excluded. Figure 1 outlines the approach taken.
FIGURE 1.
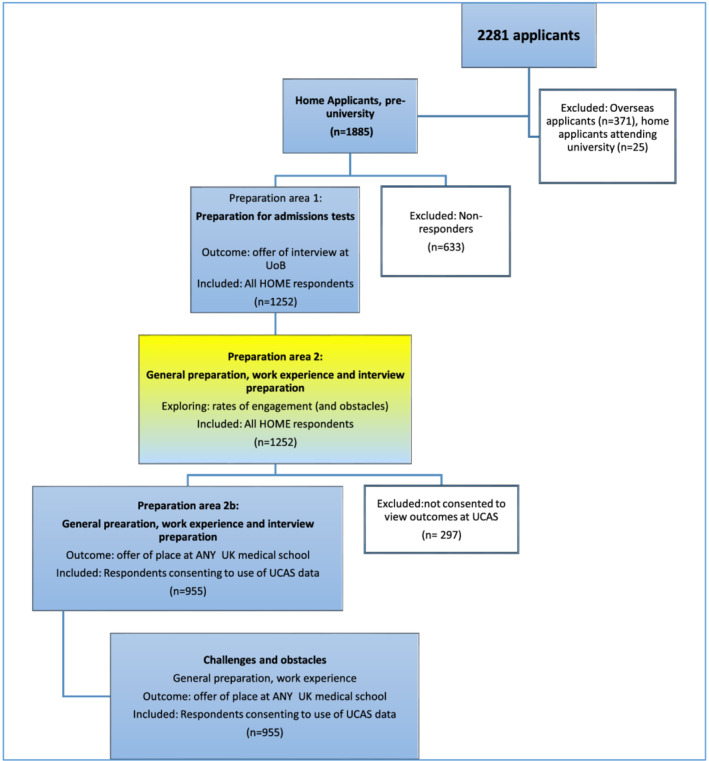
Approach to survey inclusions and exclusions [Color figure can be viewed at wileyonlinelibrary.com]
3.3. Statistical analysis
Survey data were uploaded into Microsoft Excel and IBM SPSS ‘Statistics 24’ databases for analysis. Descriptive analysis of demographic characteristics, work experience, preparatory activities and challenges was undertaken, and associations explored using chi‐squared testing. Univariate logistic regression analysis of these variables was performed to evaluate unadjusted relationships between demographic characteristics, preparatory activities and the offer of a place at any UK medical school. Informed by the results, multivariable logistic regression models were constructed to evaluate adjusted relationships. The offer of a place at any UK medical school as the outcome was initially constructed.
Free‐text responses were analysed using thematic analysis. 33 , 34 The responses were uploaded verbatim to Microsoft Excel and coded using phrases as the units of analysis. 35 , 36 DJ performed the initial analysis, and DJ, AS and JCA worked together through analytical cycles, resolving disagreement through discussion and consensus. AS and JCA helped refine the themes. Frequently occurring or novel themes were presented.
3.4. Ethical approval
This study, as part of the larger programme of research, was approved by the UoB ethics committee (ERN_17‐0964_A). Explicit consent was requested to link applicants' survey responses to national selection outcomes using data made available by the UCAS. Two invites were sent to potential participants, and survey completion was voluntary, without compensation.
4. RESULTS
Following exclusions, 1252 surveys were available for analysis (Figure 1), representing a response rate of 66.4% of all eligible UK‐schooled applicants (n = 1885). Of those who completed the survey, 955 (76.3%) also gave consent to link their responses to UCAS records reporting the offer of a place at any UK medical school.
4.1. Demographics of participants
Over two‐thirds of respondents were reportedly female, approximately half described their ethnic group as White, and a further third described their ethnic group as Asian/Asian British. 7.6% described their ethnicity as Black (any) (Table 1). When comparing survey responders and non‐responders, there were significant differences, with higher response rates from females, those attending SNS or SS schools, those on WP programmes and those from POLAR4 Quintile 5 (Table 1). There were no statistically significant differences in the demographic characteristics of those responders who gave consent to link their responses to UCAS and those who did not (Table 1).
TABLE 1.
School background, gender and ethnicity data
| Respondent characteristics | All UK school respondents (n = 1252) | All consenting to UCAS linkage (n = 955) | P‐value (chi squared) consenting to UCAS link and not consenting to UCAS link | Non‐responders (n‐633) | P‐value (chi squared) responders and non‐responders | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | % | ||||
| Gender | Male | 374 | 29.87% | 287 | 30.05% | 48.28% | ||
| Female | 862 | 68.85% | 661 | 69.21% | 57.72% | |||
| Prefer not to say | 6 | 0.48% | 1 | 0.10% | ||||
| Not reported | 10 | 0.80% | 6 | 0.63% | .45 | .00 | ||
| Ethnicity | White_any | 602 | 48.08% | 473 | 49.53% | |||
| Mixed_any | 69 | 5.51% | 56 | 5.86% | ||||
| Asian_any | 419 | 33.47% | 312 | 32.67% | ||||
| Black_any | 95 | 7.59% | 74 | 7.75% | ||||
| Other | 31 | 2.48% | 26 | 2.72% | ||||
| Prefer not to say | 26 | 2.08% | 10 | 1.05% | ||||
| Not reported | 10 | 0.80% | 4 | 0.42% | .50 | |||
| School type | State non‐sel | 599 | 47.84% | 479 | 50.16% | 36.26% | ||
| State sel | 298 | 23.80% | 214 | 22.41% | 16.30% | |||
| Independent | 334 | 26.68% | 249 | 26.07% | 30.01% | |||
| Other | 11 | 0.88% | 8 | 0.84% | ||||
| Not reported | 10 | 0.80% | 5 | 0.52% | .28 | .00 | ||
| Any WP | No | 1043 | 83.31% | 796 | 83.35% | 93% | ||
| Yes | 207 | 16.53% | 158 | 16.54% | 7% | |||
| Not reported | 2 | 0.16% | 1 | 0.10% | .94 | .92 | ||
| POLAR4 | 1 | 85 | 6.79% | 62 | 6.49% | 6.24% | ||
| 2 | 122 | 9.74% | 91 | 9.53% | 11.07% | |||
| 3 | 230 | 18.37% | 187 | 19.58% | 16.53% | |||
| 4 | 230 | 18.37% | 182 | 19.06% | 17.47% | |||
| 5 | 530 | 42.33% | 389 | 40.73% | 34.17% | |||
| Not reported | 55 | 4.39% | 44 | 4.61% | .96 | .00 | ||
4.2. What are the common activities that applicants will undertake in their preparation to secure a place at medical school?
4.2.1. General preparatory activities
Review of general news media and websites (>90%) and the use of online free forums (74%) were common preparatory activities for applicants (see Figure 2). Over 50% of applicants were also engaged in reading medical journals, participation in a school‐based medical society, discussing experiences with previous applicants, paid online courses and reading preparation books (Figure 2).
FIGURE 2.
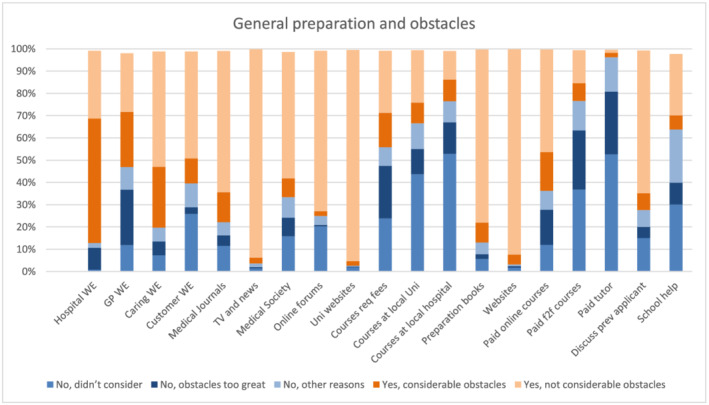
Preparation activities and obstacles [Color figure can be viewed at wileyonlinelibrary.com]
4.2.2. Work experience
The most commonly reported work experience activity was volunteering in a non‐hospital caring environment (88%). Shadowing in a hospital environment was more frequently reported compared with shadowing in a GP setting (84% compared with 54%) (Table 2). In general, shadowing experiences were usually shorter in duration (modal response 3–5 days for hospital and GP shadowing), compared with the typically reported >10 days for volunteering and paid experiences.
TABLE 2.
Work experience and obstacles
| All home respondents | Hospital (%) | GP (%) | Caring (%) | Customer (%) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1252 | ANY | Shadow | Volunteer | Paid | ANY | Shadow | Volunteer | Paid | ANY | Shadow | Volunteer | Paid | ANY | Shadow | Volunteer | Paid | ||||
| Amount undertaken | n | % | n | % | n | % | n | % | ||||||||||||
| Never | 125 | 10% | 16% | 59% | 99% | 575 | 46% | 48% | 88% | 98% | 92 | 7% | 53% | 12% | 91% | 320 | 27% | 76% | 56% | 58% |
| 1–2 days | 9% | 6% | 0% | 13% | 4% | 0% | 10% | 4% | 1% | 5% | 4% | 1% | ||||||||
| 3–5 days | 35% | 5% | 0% | 25% | 3% | 0% | 11% | 7% | 1% | 8% | 6% | 1% | ||||||||
| 6–10 days | 22% | 3% | 0% | 8% | 2% | 0% | 6% | 6% | 0% | 3% | 4% | 2% | ||||||||
| >10 days | 18% | 28% | 1% | 5% | 3% | 1% | 20% | 71% | 7% | 9% | 30% | 38% | ||||||||
| WE reported at all (ever) | ||||||||||||||||||||
| Ever (any) | 1127 | 90% | 84% | 41% | 1% | 677 | 54% | 52% | 12% | 2% | 1160 | 93% | 47% | 88% | 9% | 932 | 74% | 24% | 44% | 42% |
| Not reported | 0% | 0% | 0% | 0% | 0% | 0% | 0.1% | 0% | 0% | 0% | 0% | 0% | ||||||||
| Obstacles reported | n= | %= | n= | %= | n= | %= | n= | %= | ||||||||||||
| No, didn't consider | 11 | 1% | 149 | 12% | 92 | 7% | 324 | 26% | ||||||||||||
| No, obstacles too great | 123 | 10% | 312 | 25% | 76 | 6% | 37 | 3% | ||||||||||||
| No, other reasons | 26 | 2% | 126 | 10% | 79 | 6% | 135 | 11% | ||||||||||||
| Yes, considerable obstacles | 700 | 56% | 311 | 25% | 342 | 27% | 140 | 11% | ||||||||||||
| Yes, not considerable obstacles | 381 | 30% | 330 | 26% | 649 | 52% | 602 | 48% | ||||||||||||
| Other | 11 | 1% | 24 | 2% | 14 | 1% | 14 | 1% | ||||||||||||
4.3. To what extent are difficulties experienced in accessing or arranging preparatory activities?
4.3.1. Obstacles
Activities associated with a financial cost, such as tutors and fee‐based courses (particularly face to face courses), were most frequently not done because the obstacles were considered too great (24%) (Figure 2).
Twenty‐five per cent of respondents did not undertake work experience in a GP setting because the obstacles to arranging this were too great. Twenty‐five per cent of participants (who did undertake this experience) reported considerable obstacles in arranging it. Ninety per cent of participants undertook hospital‐based work experience (of various types) and considerable obstacles were reported by 56% of participants when arranging this. Obstacles to arrange work experience in a customer‐focused or caring environment setting were less commonly reported, and 52% and 48%, respectively, felt there were not considerable obstacles in arranging these experiences (Table 2).
Analysis of free‐text responses suggested that participants frequently found it challenging to juggle their time to prepare for selection alongside school examination preparation (n = 184), and the pressure of the process was highlighted (n = 56). Some respondents reported feeling isolated, lacking support from school or family (n = 81), and the financial cost of particular activities was an explicitly cited barrier by 77 participants (Table 3). Methods used by applicants to navigate the application process (n = 12) and a perceived lack of transparent guidance were also frequently discussed (n = 27).
TABLE 3.
Free‐text analysis of described challenges in preparation (code frequency)
| Code | Code frequency (count) |
|---|---|
| Admissions Tests | 321 |
| Work Experience | 196 |
| Challenge: Juggling Time | 184 |
| Interview Prep | 89 |
| Challenge: Feeling isolated/Unsupported | 81 |
| Challenge: Cost | 77 |
| Challenge: Pressure/Stress | 56 |
| Application Form | 38 |
| Challenge: Lack of Transparent Guidance | 27 |
| Navigating Approach to Uni Choice | 24 |
| Challenge: Age (too young for opportunities) | 13 |
| Navigating application process | 12 |
| Challenge: Negativity/Bad Advice from others | 8 |
| Challenge: Lack of Widening Participation support | 6 |
| Challenge: Late Starter | 4 |
| Challenge: Personal Health | 3 |
4.4. To what extent do particular preparatory activities, and difficulties, influence outcome at selection?
4.4.1. Outcomes at selection
Of the 955 applicants who consented to link their response to outcomes via UCAS, 769 (80.5%) received an offer of a place from at least one UK medical school (Table 4). WP programme participation was not statistically significantly associated with receiving an offer. Applicants who reported accessing general news media, participating in a school medical society, accessing admissions test preparation books and paid courses, receiving help from school (including mock interviews), paying for face‐to‐face interview courses and discussing with previous interviewees were all significantly more likely to receive an offer of a place (Table 4). Hospital shadowing, GP shadowing and caring volunteering were associated with an increased likelihood of receiving an offer of a place (P < .01) (Table 4).
TABLE 4.
Offer of a place and associations with demographic activity and preparatory activities
| All consenting to UCAS linkage (n = 955) | |||||||
|---|---|---|---|---|---|---|---|
| Demographics | Place offer | No place offer | |||||
| n | n | % | n | % | P | ||
| Gender | Male | 287 | 224 | 78% | 63 | 22% | |
| Female | 661 | 539 | 82% | 122 | 18% | ||
| Prefer not to say | 1 | 1 | 100% | 0 | 0% | .41 | |
| Ethnicity | White_any | 473 | 395 | 84% | 78 | 16% | |
| Mixed_any | 56 | 44 | 79% | 12 | 21% | ||
| Asian_any | 312 | 251 | 80% | 61 | 20% | ||
| Black_any | 74 | 48 | 65% | 26 | 35% | ||
| Other | 26 | 20 | 77% | 6 | 23% | ||
| Prefer not to say | 10 | 7 | 70% | 3 | 30% | ||
| Not reported | 4 | 4 | 100% | 0 | 0% | <.01 | |
| School type | State non‐sel | 479 | 375 | 78% | 104 | 22% | |
| State sel | 214 | 184 | 86% | 30 | 14% | ||
| Independent | 249 | 202 | 81% | 47 | 19% | ||
| Other | 8 | 3 | 38% | 5 | 63% | ||
| Not reported | 5 | 5 | 100% | 0 | 0% | .26 | |
| Any WP | Yes | 158 | 124 | 78% | 34 | 22% | |
| Not reported | 1 | 1 | 100% | 0 | 0% | .38 | |
| POLAR4 | 1 | 62 | 50 | 81% | 12 | 19% | |
| 2 | 91 | 67 | 74% | 24 | 26% | ||
| 3 | 187 | 149 | 80% | 38 | 20% | ||
| 4 | 182 | 149 | 82% | 33 | 18% | ||
| 5 | 389 | 334 | 86% | 55 | 14% | ||
| Not reported | 44 | 20 | 45% | 24 | 55% | <.01 | |
| Work experience | Number DID activity | Did Activity AND Place Offer | Did NOT do Activity AND Place Offer | ||||
|---|---|---|---|---|---|---|---|
| n | n | n | n | % | P | ||
| Hospital | Shadowing | 802 | 672 | 84% | 97 | 63% | <.01 |
| Volunteering | 395 | 325 | 82% | 444 | 79% | .25 | |
| Paid | 11 | 11 | 100% | 758 | 80% | .06 | |
| GP | Shadowing | 479 | 402 | 84% | 367 | 77% | <.01 |
| Volunteering | 111 | 78 | 70% | 691 | 82% | .01 | |
| Paid | 17 | 16 | 94% | 753 | 80% | .16 | |
| Caring | Shadowing | 449 | 359 | 80% | 410 | 81% | .71 |
| Volunteering | 838 | 688 | 82% | 81 | 69% | <.01 | |
| Paid | 84 | 72 | 86% | 697 | 80% | .54 | |
| Customer | Shadowing | 225 | 176 | 78% | 593 | 81% | .23 |
| Volunteering | 405 | 325 | 80% | 444 | 81% | .34 | |
| Paid | 408 | 331 | 81% | 438 | 80% | .21 | |
| General preparation | Number DID activity | Did Activity AND Place Offer | Did NOT do Activity AND Place Offer | ||||
|---|---|---|---|---|---|---|---|
| n | n | % | n | % | P | ||
| Medical journals | Yes | 731 | 530 | 81% | 172 | 80% | .61 |
| TV and news | Yes | 921 | 749 | 81% | 19 | 58% | <.01 |
| Medical society | Yes | 615 | 505 | 82% | 252 | 77% | <.01 |
| Online forums | Yes | 706 | 575 | 81% | 188 | 78% | .06 |
| Uni websites | Yes | 930 | 752 | 81% | 15 | 68% | .11 |
| Courses req fees | Yes | 406 | 342 | 84% | 424 | 78% | .01 |
| Course local uni | Yes | 301 | 241 | 80% | 524 | 81% | .55 |
| Admissions test preparation | Number DID activity | Did Activity AND Place Offer | Did NOT do Activity AND Place Offer | ||||
|---|---|---|---|---|---|---|---|
| n | n | % | n | % | P | ||
| Preparation books | Yes | 829 | 681 | 82% | 86 | 69% | <.01 |
| Websites | Yes | 919 | 743 | 81% | 25 | 71% | .37 |
| Paid online course | Yes | 603 | 510 | 85% | 259 | 74% | <.01 |
| Paid F2F course | Yes | 209 | 183 | 88% | 583 | 79% | <.01 |
| Paid tutor | Yes | 32 | 20 | 63% | 747 | 81% | <.01 |
| Discuss prev applicant | Yes | 684 | 560 | 82% | 208 | 78% | .06 |
| School help | Yes | 323 | 271 | 84% | 486 | 79% | .05 |
| Interview preparation | Number DID activity | Did Activity AND Place Offer | Did NOT do Activity AND Place Offer | ||||
|---|---|---|---|---|---|---|---|
| n | n | % | n | % | P | ||
| Prep books | Yes | 527 | 425 | 81% | 332 | 81% | .98 |
| Free online course | Yes | 564 | 451 | 80% | 303 | 81% | .30 |
| Paid online course | Yes | 132 | 101 | 77% | 656 | 81% | .22 |
| Paid F2F course | Yes | 155 | 137 | 88% | 620 | 79% | <.01 |
| Paid tutor | Yes | 25 | 15 | 60% | 742 | 81% | .03 |
| Prep course‐ school | Yes | 639 | 539 | 84% | 209 | 73% | <.01 |
| Prep course‐ uni/hospital | Yes | 180 | 149 | 83% | 600 | 80% | .36 |
| Discuss with previous applicant | Yes | 762 | 627 | 82% | 130 | 73% | <.01 |
| Practised interview | Yes | 777 | 637 | 82% | 120 | 74% | .04 |
| School help | Yes | 695 | 578 | 83% | 176 | 74% | <.01 |
4.5. Does socio‐demographic background influence these preparatory activities or challenges?
Univariate analysis demonstrated ethnic group and POLAR4 quintile as statistically significantly associated with receiving an offer, with those from White ethnic groups and POLAR4 Quintile 5 most likely to be successful and Black applicants least likely (65% compared with 84% White applicants) (Table 4). A multiple logistic regression model with the offer of a place at any UK medical school as the outcome was initially constructed using demographic characteristics only as explanatory variables (classification accuracy 81%; Table 5). The multivariate model suggested that White ethnic group and attendance at an SS school were most closely associated with receiving an offer of a place (Table 5).
TABLE 5.
Multiple log regression: Demographics, preparatory activities and offer of a place at any UK medical school
| Variable | B | SE | Sig. | OR | 95% confidence interval | |
|---|---|---|---|---|---|---|
| Constant | −1.124 | .478 | .02 | .325 | ||
| Ethnic group | ||||||
| Mixed_any | −.465 | .375 | .215 | .628 | .301 | 1.310 |
| Asian_any | −.099 | .208 | .635 | .906 | .602 | 1.362 |
| Black_any | −.940 | .306 | <.01 | .391 | .215 | .712 |
| Other | −.412 | .531 | .438 | .663 | .234 | 1.876 |
| Prefer not to say | −.698 | .745 | .348 | .497 | .116 | 2.140 |
| Reference group: White_any | ||||||
| School type | ||||||
| State selective | .190 | .242 | .433 | 1.209 | .752 | 1.943 |
| Independent | −.244 | .217 | .259 | .783 | .512 | 1.198 |
| Other | −2.270 | .833 | .01 | .103 | .020 | .528 |
| Reference group: State non‐selective | ||||||
| Preparation activities (Yes/No) | ||||||
| Hospital shadowing | .723 | .219 | <.01 | 2.060 | 1.340 | 3.167 |
| GP shadowing | .424 | .187 | .02 | 1.528 | 1.059 | 2.205 |
| GP volunteering | −.855 | .262 | <.01 | .425 | .254 | .711 |
| TV and news | .933 | .406 | .02 | 2.542 | 1.146 | 5.637 |
| Admissions Test prep books | .637 | .237 | .01 | 1.891 | 1.189 | 3.008 |
| Admissions Test paid online course | .526 | .182 | <.01 | 1.691 | 1.183 | 2.417 |
| Mock school interview | .568 | .186 | <.01 | 1.765 | 1.225 | 2.544 |
| −2 Log likelihood | 814.890 | |||||
| Chi square | 91.384 | df = 15 | P < .001 | |||
| Nagelkerke R Square | .151 | |||||
| Hosmer and Lemeshow Test | P = .673 | |||||
| Classification accuracy | 81.0% | |||||
Preparatory activities and work experience (previously shown to be associated with the outcome using univariate analyses) were then also included in the model (Table 5). When controlling for all other variables, accessing general news media, accessing admissions test preparation books and paid online courses, attending courses at school incorporating mock interviews and shadowing in a hospital and GP setting were all associated with an increased likelihood of an offer, whereas volunteering in a GP setting was associated with a reduced likelihood of an offer. However, no model was a good fit for these data (estimated using pseudo‐R 2 statistics), and further inclusion of interaction terms did not identify any significant associations, so these were not included.
For the activities associated with the offer of a place (on univariate and multivariate analyses), socio‐demographic associations were considered in relation to reported participation and to reported obstacles (Appendix 2, Tables S1 and S2). Watching TV and engaging with news media were widely considered and generally considered easy to access, with no significant socio‐demographic difference in uptake (Appendix 2, Tables S1 and S2).
Participation in school‐based medical societies (school support) and attending fee‐based interview or admissions test courses were more commonly reported by those attending SS and IND schools, as well as those from POLAR4 Quintile 5 (P < .01) (Appendix 2, Table S1). Those from SNS schools and participating in WP programmes and from POLAR4 Quintiles 1 and 2 were most likely to report obstacles too great to access courses requiring fees or participate in a school‐based medical society (P < .01).
Participation in hospital and GP shadowing was reported more frequently by those from SS and IND schools when compared with SNS schools (P < .01) and those in higher POLAR4 quintile groups (P < .01 and P = .03, respectively). There were significant ethnicity differences in participation in hospital and GP shadowing. Hospital shadowing was reported by 72% of Black applicants (compared with 88% of White applicants) and GP shadowing reported by 445 of Black applicants (compared with 51% white applicants and 56% Asian applicants) (Appendix 2, Table S1).
Those from SNS schools and participating in WP programmes and from POLAR4 Quintile 1 were most likely to report that the obstacles to arranging hospital‐based work experience were too great. Those from SNS schools and POLAR4 Quintile 1 also more commonly reported the obstacles too great to arrange experience in a GP setting (Appendix 2, Table S2).
5. DISCUSSION
This research aimed to explore the influence of socio‐demographic background on preparation for medical school selection through the consideration of the opportunities and challenges to preparation activities and their association with the successful offer of a place.
Firstly, when exploring the range and types of activity undertaken, many applicants appear to be engaged in a range of multiple sources of extracurricular activity. This spans books, websites, online forums, discussion with peers and engagement with media and journals.
An exploration of the obstacles and challenges faced by applicants in preparation was a key consideration in our research, as we felt this may offer important insights for medical schools when planning selection processes and support for applicants. The data suggest that applicants continue to remain committed to arranging clinical work experience, with 90% undertaking hospital‐based placements (mainly shadowing), despite 56% reporting considerable challenge in arranging these placements. This pursuit of hospital‐based experience has continued notwithstanding guidance released by the UK Medical Schools Council to reassure applicants that clinical settings for work experience were not necessary. 37 Work experience in general practice, a key objective to primary care workforce recruitment, was more challenging to arrange, with 25% of applicants reporting that the challenges were too great. 38 , 39 The Royal College of Practitioners has developed an online platform to provide ‘virtual’ work experience in the GP setting (launched in 2020), and this may go some way to address this. 40
Free‐text responses alluding to stress, pressure, the juggle of time and feelings of isolation may offer some explanation for why particular obstacles were reported and highlight additional scope for exploration. The free‐text comments related to the navigation of the application process and perceived lack of transparency in preparation guidance also suggest that preparing for selection is more than simply having access to particular activities. It may also require applicants to have the ‘know how’ to navigate the options available and prioritise those activities most likely to be associated with success. This relates to cultural capital. 17 , 18 Although a focus for this study is in the opportunities available (or inaccessible) to applicants, it is important to recognise this complexity. Attempts to make preparatory activities more ‘accessible’ may also require an exploration of how activities are chosen, prioritised and navigated by applicants to begin to bring about meaningful change.
With applicants engaged in significant range and scope of preparatory activity, and a sense that some may be experiencing stress, pressure or difficulty in prioritising their time and effort, we also aimed to explore those activities most likely to be associated with success. Our multivariate analysis suggested that activities significantly associated with the offer of a place at a UK medical school were engagement with health‐related news, undertaking clinical shadowing (hospital or GP), using books or paying fees for admissions test preparation and participating in interview practice at school. The literature is equivocal as to the benefits of commercial coaching for admissions tests (face‐to‐face or online). 9 , 10 Our results add to this discussion by suggesting that online fee‐paying courses may contribute to success at selection, although this did not appear to apply (on multivariate analysis) to commercial coaching for interviews, the use of tutors or face‐to‐face admissions test coaching. This finding does require some caution with its interpretation, as the particular facets of the admissions tests are not explored within our study, nor is the predictive validity. In studies where these have been explored, the impact of coaching has been less convincing. 9 , 10
The main focus of this research was to explore whether socio‐demographic background influenced preparatory activity or obstacles, particularly those associated with success. The results indicate significant demographic differences in the types of activities associated with success that were undertaken by applicants, particularly when considering their school type, ethnicity and POLAR4 status. Applicants from IND schools were more likely to report school‐based support when compared with those from SNS schools. This group of applicants also more frequently reported paying for courses to support their application. In contrast, applicants from the lowest POLAR4 quintile more frequently reported challenges in accessing some types of school‐based support, such as a medical society and interview practice, and in accessing courses requiring a fee.
Those from SNS schools and lowest POLAR4 quintiles were less likely to undertake GP and hospital‐based work experiences and more frequently reported obstacles in arranging them, which echoes similar findings from elsewhere in the literature. 39
Although the influence of ethnicity has been explored in various studies of medicine admissions, ‘White’ and ‘non‐White’ categorisation of participants may have failed to granulate the challenges faced by particular ethnic groups. 41 , 42 Our results suggested that Black (any) applicants less frequently reported participation in interview practice and hospital shadowing when compared with White, Asian or mixed ethnicity applicants. These were preparatory activities in our results that were associated with the offer of a place. Further research is required to fully appreciate the nuanced challenges faced by particular ethnicities within medical school admissions, but our results suggest that ethnicity (explored at a more granular level) is an important socio‐demographic consideration, alongside POLAR4 and school background data.
It has been argued that a focus on selection processes alone is unlikely to make significant inroads in changing the landscape of higher education. 43 Bourdieu's concepts of habitus and cultural capital are important provocations for those involved in admissions, highlighting the complex and embedded nature of disadvantage, which starts long before the application process is commenced, influencing not just the opportunities for preparation for selection, but also applicant perceptions and navigation of the process. For admissions teams committed to improving diversity, we would suggest that this requires an appreciation of socio‐cultural complexity, and also of applicant activity, endeavour and challenge in the years preceding medical school admissions tests.
It is our aim to outline recommendations for those who wish to improve socio‐demographic disadvantage in medical school admissions with this complexity in mind, encouraging exploration and consideration of sociocultural influence, habitus, language and perception. It may be useful for admissions teams to review the content and format of guidance given to applicants, exploring how information is provided and communicated and considering whether there has been sufficient consideration of socio‐demographic variation in obstacles and opportunity for preparation. This may also require consideration of when and where such information is disseminated. Many of the activities associated with success in our study (such as work experience) are typically undertaken months to years before application, suggesting early engagement with schools and applicants. The least represented socio‐demographic groups in our study most commonly engaged with university websites and online media (rather than school‐based support), and these may represent important forums for communication.
Due to the complex considerations related to disadvantage, it can be difficult for admissions teams to know where to start when aiming to target research or support to improve diversity. Our results highlight activities that both appear to yield a greater chance of success, yet also are associated with higher risk of inequality. Applicants from less represented socio‐demographic backgrounds appear to have less school‐based support for interview preparation, and this may be important when considering interview design and programmes to provide additional support for applicants. Although work experience in clinical environments is not a ‘requirement’ for success at interview at a UK medical school, it continues to appear to be frequently undertaken by applicants, associated with success and linked with inequality. This suggests a case to understand why such experiences remain important for applicants despite explicit instruction to the contrary and to consider whether selection processes may continue to favour these activities. Although somewhat equivocal, fee‐based support for application may continue to confer advantage for those who can afford it, and this finding warrants further study.
6. LIMITATIONS
This study has explored the participation of applicants in each activity, rather than an assessment of the quality of each activity. Respondent bias (both recall and subjectivity) is also a limitation. 35 The multivariate modelling correctly classified 81% of cases. However, the complex and heterogeneous approaches to selection assessment used across UK medical schools may explain why the modelling is less able to identify those who do not receive an offer. Our dataset represents proportionally greater female, SS/SNS school and higher POLAR4 quintiles than our applicant pool and ultimately represents data from those applicants who have chosen to apply to the UoB (among others) based on their perception of likelihood of success according to our published processes. Further study is required across various institutional and international settings.
7. CONCLUSION
Clinical work experience, commercial courses for admissions tests and school‐based support for interview represent areas of preparation that are associated with success. However, they also represent areas that are more challenging to access for demographic groups traditionally underrepresented in medicine. These findings suggest that the lack of heterogeneity observed in medical schools relates to the applicant preparation phase, despite efforts from universities to address inequalities related to clinical work experience connections, financial cost and school background. Addressing complex issues of fairness in highly selective higher education settings can appear an insurmountable task. The results from this study identify some key areas, which appear to correlate with success, while perpetuating inequality. These represent important areas for applicants, schools and institutions to explore and address.
FUNDING INFORMATION
Not applicable.
CONFLICTS OF INTEREST
DJ, AS and JCA were employed as members of the university MBChB (Medicine) admissions team during the research design and implementation.
ETHICS STATEMENT
This study, as part of the larger programme of research, was approved by the University of Birmingham ethics committee (ERN_17‐0964_A). Explicit consent was requested to link applicants' survey responses to national selection outcomes using data made available by the Universities and Colleges Admissions Service (UCAS).
AUTHOR CONTRIBUTIONS
All authors (DJ, DW, AS and JCA) provided substantial contributions to the conception and design of the work, drafting the work, final approval of the version to be published and agreement to be accountable for all the aspects of the work. DJ and DW provided substantial contributions to the analysis and interpretation of data for the work.
Supporting information
Data S1.Supporting information
Table S1:Activities associated with the offer of a place: Demographic associations and reported participation
Table S2. Activities associated with the offer of a place: Demographic associations and reported obstacles
ACKNOWLEDGEMENTS
None.
Jackson D, Ward D, Agwu JC, Spruce A. Preparing for selection success: Socio‐demographic differences in opportunities and obstacles. Med Educ. 2022;56(9):922‐935. doi: 10.1111/medu.14811
REFERENCES
- 1. Mathers J, Sitch A, Marsh J, Parry J. Widening access to medical education for under‐represented socioeconomic groups: population based cross sectional analysis of UK data, 2002‐2006. BMJ. 2011;342:d918‐d925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cleland JA, Nicholson S, Kelly N, Moffat M. Taking context seriously: explaining widening access policy enactments in UK medical schools. Med Educ. 2015;49(1):25‐35. [DOI] [PubMed] [Google Scholar]
- 3. Steven K, Dowell J, Jackson C, Guthrie. Fair access to medicine? Retrospective analysis of UK medical schools application data 2009‐2012 using three measures of socioeconomic status. BMC Med Educ. 2016;16(1):11‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kelly ME, Gallagher N, Dunne FP, Murphy AW. Views of doctors of varying disciplines on HPAT‐Ireland as a selection tool for medicine. Med Teach. 2014;36(9):775‐782. [DOI] [PubMed] [Google Scholar]
- 5. Kumar K, Roberts C, Bartle E, Eley DS. Testing for medical school selection: What are prospective doctors' experiences and perceptions of the GAMSAT and what are the consequences of testing? Adv Health Sci Educ Theory Pract. 2018;23(3):533‐546. [DOI] [PubMed] [Google Scholar]
- 6. Dhar D, Perry W, Poole P. Students perceptions of the undergraduate medicine and health sciences admissions test (UMAT). NZ Med J. 2012;125‐136. [PubMed] [Google Scholar]
- 7. Kennedy H. Learning works: widening participation in further education. Further Education Funding Council (FEFC), corp creator; 1997.
- 8. Laurence CO, Zajac IT, Lorimer M, Turnbull DA, Sumner KE. The impact of preparatory activities on medical school selection outcomes: a cross‐sectional survey of applicants to the university of Adelaide medical school in 2007. BMC Med Educ. 2013;13(1):159‐168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Griffin B, Carless S, Wilson I. The effect of commercial coaching on selection test performance. Med Teach. 2013;35(4):295‐300. [DOI] [PubMed] [Google Scholar]
- 10. Griffin B, Yeomans ND, Wilson IG. Students coached for an admission test perform less well throughout a medical course. Intern Med J. 2013;43(8):927‐932. [DOI] [PubMed] [Google Scholar]
- 11. Kim SH. Extracurricular activities of medical school applicants. Korean J Med Educ. 2016;28(2):201‐207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shankar N, Singh S, Gautam S, Dhaliwal U. Motivation and preparedness of first semester medical students for a career in medicine. Indian J Physiol Pharmacol. 2013;57(4):432‐438. [PubMed] [Google Scholar]
- 13. Rees, Hawarden AW, Dent G, Hays R, Bates J, Hassell AB. Evidence regarding the utility of multiple mini‐interview (MMI) for selection to undergraduate health programs: A BEME systematic review: BEME Guide No. 37. Med Teach. 2016;38(5):443‐455. [DOI] [PubMed] [Google Scholar]
- 14. Lambe P, Greatrix R, Milburn K, Dowell J, Bristow D. Do differentials in access to advice and support at UK schools on preparation for the UK clinical aptitude test disadvantage some candidate groups? University Clinical Aptitude Test; 2012.
- 15. Bligh ER, Courtney E, Stirling R, et al. Impact of the COVID‐19 pandemic on UK medical school widening access schemes: disruption, support and a virtual student led initiative. BMC Med Educ. 2021;21(1):344‐351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park J, Philipp R, Hughes A. Do we value work experience before medical school? Br J Gen Pract. 2005;55(512):242‐243. [PMC free article] [PubMed] [Google Scholar]
- 17. O'Shea. Avoiding the manufacture of ‘sameness’: first‐in‐family students, cultural capital and the higher education environment. High Educ. 2016;72(1):59‐78. [Google Scholar]
- 18. Bourdieu P. The Logic of Practice. Cambridge Polity Press; 1990. [Google Scholar]
- 19. Pascarella ET, Pierson CT, Wolniak GC, Terenzini PT. First‐Generation College Students. J High Educ. 2004;75(3):249‐284. [Google Scholar]
- 20. Aschaffenburg K, Maas. Cultural and educational careers: the dynamics of social reproduction. Am Sociol Rev. 1997;62(4):573‐587. [Google Scholar]
- 21. Reay D. ‘Always knowing’ and ‘never being sure’: familial and institutional habituses and higher education choice. J Educ Policy. 1998;13(4):519‐529. [Google Scholar]
- 22. Mathers J, Parry J. Why are there so few working‐class applicants to medical schools? Learning from the success stories. Med Educ. 2009;43(3):219‐228. [DOI] [PubMed] [Google Scholar]
- 23. Wilson N, McLean S. Questionnaire Design: A Practical Introduction. Newtownabbey Ulster University Press; 1994. [Google Scholar]
- 24. Spruce A. Medicine application statistics. University of Birmingham; 2020.
- 25. Outreach Office . Our activities for post 16 school and college pupils. University of Birmingham; 2021.
- 26. University of Birmingham . Widening participation and access. University of Birmingham; 2021.
- 27. Montacute R, Cullinane C. Access to advantage: the influence of schools and place on admissions to top universities. The Sutton Trust, London, UK; 2018.
- 28. Green F, Anders J, Henderson M, Henseke G. Who chooses private schooling in Britain and why? Centre for Learning and Life Chances in Knowledge Economies and Societies; 2017.
- 29. Higher Education Statistics Agency . Definitions and benchmark factors. HESA; 2021.
- 30. Jackson D, Spruce A, Whalley N, Seyan G, Agwu C (Eds). Medical Application Preparation Study (MAPS): Exploring culture and perceptions through applicant stories. In: Proceedings of the ASM 2019: Sustainability, Transformation and Innovation in Medical Education. Association for the Study of Medical Education; 2019. [Google Scholar]
- 31. Gavin J, Kelly R, Jackson D (Eds). Preparation for medical school application: is it all just a game? In: Proceedings of the Birmingham Conference. University of Birmingham; 2018. [Google Scholar]
- 32. Bailey KD. Methods of Social Research. 4thed. Basingstoke Collier‐Macmillan; 1994. [Google Scholar]
- 33. Braun V, Clarke. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77‐101. [Google Scholar]
- 34. Braun V, Clarke V. Thematic Analysis: A Practical Guide. London Sage; 2021. [Google Scholar]
- 35. Cohen L, Manion L, Morrison K. Research Methods in Education. 6thed. Routledge; 2007. [Google Scholar]
- 36. Krippendorff K. Content Analysis: An Introduction to its Methodology. Sage; 2004. [Google Scholar]
- 37. Council MS . Guidance on relevant experience for applying to medical school. 2017 update; 2017.
- 38. Wass V, Gregory S, Petty‐Saphon K. By choice—not by chance: supporting medical students towards future careers in general practice. London: Health Education England and the Medical Schools Council; 2016.
- 39. Agravat P, Ahmed T, Goudie E, et al. Medical applicant general practice experience and career aspirations: a questionnaire study. BJGP Open. 2021;5(3):BJGPO.2021.0023‐0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Royal College of General Practitioners . Observe GP. Royal College of General Practitioners, United Kingdom; 2020.
- 41. Fielding S, Tiffin PA, Greatrix R, et al. Do changing medical admissions practices in the UK impact on who is admitted? An interrupted time series analysis. BMJ Open. 2018;8(10):e023274‐023285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tiffin PA, Dowell JS, McLachlan JC. Widening access to UK medical education for under‐represented socioeconomic groups: modelling the impact of the UKCAT in the 2009 cohort. BMJ‐Brit Med J. 2012;344:e1805‐1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Archer L, Hutchings M, Ross A. Higher Education and Social Class: issues of exclusion and inclusion. RoutledgeFalmer; 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1.Supporting information
Table S1:Activities associated with the offer of a place: Demographic associations and reported participation
Table S2. Activities associated with the offer of a place: Demographic associations and reported obstacles


