Summary
The primary aim of this review was to identify, analyse and codify the prominence and nature of human factors and ergonomics within difficult airway management algorithms. A directed search across OVID Medline and PubMed databases was performed. All articles were screened for relevance to the research aims and according to predetermined exclusion criteria. We identified 26 published airway management algorithms. A coding framework was iteratively developed identifying human factors and ergonomic specific words and phrases based on the Systems Engineering Initiative for Patient Safety model. This framework was applied to the papers to delineate qualitative and quantitative results. Our results show that human factors are well represented within recent airway management guidelines. Human factors associated with work systems and processes featured more prominently than user and patient outcome measurement and adaption. Human factors are an evolving area in airway management and our results highlight that further considerations are necessary in further guideline development.
Keywords: airway management, airway research, guidelines, human factors, non‐technical skills
Introduction
Clinical guidelines are tools for improving airway management [1, 2, 3, 4]. Theur purpose, along with cognitive aids, is to assist in streamlining clinical decision‐making and to minimise human error, ultimately improving patient safety [5]. Disasters in airway management often involve cognitive overload leading to poor decision‐making and/or analysis [6]. Human factors concepts such as perception, decision‐making and interpersonal communication are subject areas clinicians intuitively understand as important, yet it has taken time for these to be formalised. The first airway guideline was published in 1993 but it took a further 22 y for an airway guideline to include decision‐making prompts in an algorithm in the form of the Difficult Airway Society's ‘Stop and think’ [7, 8]. Since then, human factors in various forms have been included in other airway guidelines but the specific types of human factors included in recent guidelines have not yet been studied.
The concept of human factors comprises much more than individual cognition errors (e.g. perceptions and decision‐making) or interpersonal communication failures. Human factors permeate everything that affects how work is done, from the culture and regulations affecting an organisation to how equipment and tasks are designed within the complex systems of healthcare delivery. The concept of human factors may be defined as 'environmental, organisational and job factors together with human and individual characteristics, which influence behaviour at work in a way which can affect health and safety’ [9]. Organisational focus on human factor frameworks is thought to reduce patient harm through numerous checks and balances [10, 11]. Originally evaluated within the aviation industry, the importance of human factors has gained increased attention in healthcare (particularly in acute care) as a way to minimise omissions or errors during time‐critical situations [12, 13].
The Systems Engineering Initiative for Patient Safety (SEIPS) model was first published in 2006 by Carayon et al. and was based on data collected over 20 y [14]. The model describes the interaction between work systems, processes and outcomes, as well as people, tools and the environment (Fig. 1). It also attempts to analyse human factors in healthcare system performance by outlining overarching components that ‘can contribute to acceptable or unacceptable process’ and by identifying the specific human factor components in a ‘descriptive, not prescriptive’ manner [14].
Figure 1.
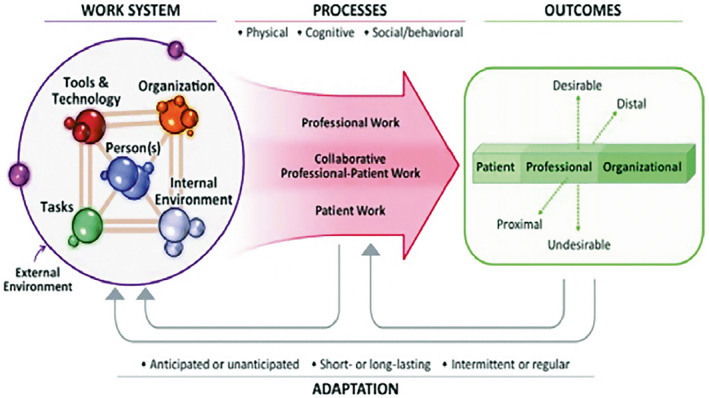
SEIPS 2.0 model reproduced from Holden et al. [15].
We used the SEIPS model framework to quantify the types of human factors included in airway guidelines that have been published within the last 5 y.
Methods
The search strategy is available in online Supporting Information (Appendix S1).
Since there is no validated or accepted taxonomy for human factors, a coding framework was iteratively developed by three authors (SL, SM and MT). The mention of human factors and ergonomics was identified using specific words and phrases based on the SEIPS model. This coding framework was divided into three major domains: work system; processes; and outcomes/adaptation (Table 1). Specific human factors were separated into their most appropriate domain. The work system domain included equipment; tasks; team members; organisational; and internal/external environments. The processes domain included planning; recaps/situational reports; cognitive aids; communication; alarm use; and role allocation. The outcomes/adaptation domain included patient outcomes; user outcomes; and organisational issues.
Table 1.
Coding framework based on the Systems Engineering Initiative for Patient Safety (SEIPS) model.
| Work System | ||
|---|---|---|
| Element | Definition | Terms |
| Equipment |
Defines what equipment to use Ensures equipment is available and prepared (work surface/kit dump mat) Minimum monitoring equipment (capnography/oximetry) Suggested medications |
equipment; equipment select/selected/selecting/selection; equipment preparation; monitoring; work surface; kit dump; knoll; equipment check/checked/checking/checks; syringe size; syringe organisation/organisation; syringe ordering; syringe preparation; medication organisation/organisation; medication ordering; medication preparation; drug organisation/organisation; drug ordering; drug preparation; red‐barrelled syringe; red syringe; airway cart; airway trolley; difficult airway cart; difficult airway trolley; equipment availability; equipment storage |
| Tasks | Defines how tasks are done (CICO and otherwise), for example, where to stand, how to perform (scalpel/bougie cricothyrotomy technique for example) | ergonomics; physical ergonomics; physical space; design; lighting; noise; position/positioned/positioning; layout; location; where; scalpel type; scalpel size; bougie type; bougie size; coudé tip; finger; incision; technique |
| Team members |
Defines minimum number and type of team members Defines skill set of team member(s) |
skills; skill‐mix; skill‐set; training; education; team size; team composition; team member; skills matrix |
| Organisational |
Suggests rostering/organisational issues or team such as airway emergency teams Defines hospital/health service‐wide changes |
roster; teams; response team; difficult airway response team; DART; emergency team; facilities; purpose‐built; specialist; specialised/specialised; MET team; MERT team; organisation/organisation; health service; health district; code blue/red/black; service change/changed/changes; service alteration; service‐wide change; service‐wide alteration; schedule/scheduling/scheduled; emergency response |
| Internal environment |
Describes modification of internal environment – minimise noise, distraction Outlines engineering principles such as negative pressure/airflow characteristics |
internal environment; noise minimisation/minimization; distract/distraction; interrupt; airflow; negative pressure; below 10,000/10,000; sterile cockpit; sterile communication/s; alarms; temperature; light; lighting |
| External environment | Suggests broader legal/regulatory changes or systems larger than single health service | law; legal; regulatory; multi‐site; licence; licence; certify; board; regulation; legislative change; medical board |
| Processes | ||
|---|---|---|
| Planning |
Suggests pre‐case planning/huddle Checklist provided or suggested Written (explicit) protocols and plans made (e.g. via a whiteboard) How plans and protocols are agreed and communicated |
plan/planned/planning/plans; protocol/s; check‐list/checklist; whiteboard; strategy; huddle; pre‐brief; algorithm; preparation; time‐out; shared mental model; common understanding; airway assess/assessed/assessing/assessment; chart review |
| Recaps/situation reports |
Describes pauses for team situation awareness/team suggestions Provides a structure for these recaps Provides framework for team decision‐making |
awareness; recap; decision‐making; situational awareness; stop and think; pause; sitrep/sit‐rep; SNAPPI; callout/call‐out |
| Cognitive aids |
Provides or suggests a cognitive aid Defines who reads a cognitive aid Defines how the cognitive aid is used (e.g. challenge‐response) Advises physical/electronic properties of the cognitive aid |
cognitive aid; challenge‐response; call‐response; mnemonic; acronym; poster; algorithm; reader; verify; verification; display; displayed; screen‐based; electronic; aide‐memoire; memory aids; prompts |
| Communication |
Mentions closed‐loop communication Advises or promotes a Graded Assertiveness method to prevent fixation Defines what information requires explicit versus implicit coordination Promotes ‘sterile’ periods of communication Uses specific ‘critical language’ |
communication; closed‐loop/closed loop; sterile communication/s; implicit co‐ordination/coordination; explicit co‐ordination/coordination; explicit communication; speak up; escalation; assertiveness; critical language; non‐verbal communication; read out/readout/read‐out; readback/read back/read‐back; fixation |
| Alarm use |
Suggests methods to deal with alarms Suggests methods to maintain awareness of time elapsed |
alarm/alarms; situational awareness; fixation; alarm fatigue; time dilation; time contraction; time awareness; elapsed; help; call for help; emergency button; red button |
| Role allocation |
Defines minimum roles Defines who allocates roles Defines how the leadership role is assigned and/or reassigned Defines followership roles |
role allocation; role assignment; role delegation; leader; follower; task management; task assignment; team dynamics; interpersonal/inter‐personal |
| Outcomes/adaptation | ||
|---|---|---|
| Patient outcomes |
Assesses morbidity and mortality of airway management episodes Advises a system for incident reporting and learning |
morbidity; mortality; incident report/reporting; review; learning; case conference; quality improvement; quality assurance |
| User outcomes |
System exists for collecting and incorporating feedback to future versions Assessing processes of airway management episodes in simulation |
feedback; safety; simulation; resilience; resilience engineering; feed forward; performance assessment |
| Organisational issues | Underpinned by a reputable body which is sustainable | sustain; review; review process; re‐engineer; re‐design; society; committee; consultation; medical college |
NVivo analysis software (Version 1.5.1; QSR International Pty Ltd., Chadstone, Victoria, Australia) was used to analyse the text. The coding framework (Table 1) along with the 26 airway guidelines was inputted for analysis. Each guideline was analysed for the presence and number of coded human factors terms. To ensure optimal capture of human factors data, each guideline was also evaluated by one of two authors (DE or DB) to extract any other human factors that may have not been extracted with the coding software.
The resulting coding matrices were exported and further analysed on Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) with tables and illustrative charts formulated. A comparative illustration of the distribution of the three major human factors components is shown along with other findings in online Supporting Information (Appendix S2).
Quantitative categoric analysis of the human factor types in the three domains was recorded, with prevalence of each subdomain also analysed. The results were tabulated to delineate if all, some or none of the subdomains were present for each paper.
Results
In the last five years (May 2016–May 2021), 26 airway guidelines were identified (Table 2). Of these, more than half were published after January 2020 (n = 18) and 13 were COVID specific.
Table 2.
Included guidelines.
| Year Published | Professional airway group and reference | Country | COVID‐19 specific |
|---|---|---|---|
| 2021 | Canadian Airway Focus Group [16] | Canada | N |
| 2021 | Society for Airway Management [17] | USA | N |
| 2021 | French Society of Anaesthesia and Intensive Care Medicine [18] | France | Y |
| 2021 | Society of Airway Management [19] | USA | Y |
| 2020 | Difficult Airway Society [1] | UK | N |
| 2020 | Canadian Anesthesiologists' Society [20] | Canada | N |
| 2020 | Catalan Society of Anesthesiology [21] | Spain | N |
| 2020 | Anaesthesia Patient Safety Foundation [22] | US | Y |
| 2020 | Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists [23] | China | Y |
| 2020 | Safe Airway Society [24] | Australia | Y |
| 2020 | Difficult Airway Society (DAS), Association of Anaesthetists, Intensive Care Society, Faculty of Intensive Care Medicine and the Royal College of Anaesthetists [25] | UK | Y |
| 2020 | Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva (SIAARTI) and the European Airway Management Society [26] | Italy | Y |
| 2020 | Indian Society of Anaesthesiologists [27] | India | Y |
| 2020 | Chinese Society of Anesthesiology [28] | China | Y |
| 2020 | All India Difficult Airway Association [29] | India | Y |
| 2020 | Korean Society of Anesthesiologists [30] | Korea | Y |
| 2020 | Taiwan Association of Anesthesiologists [31] | Taiwan | Y |
| 2020 | N/A [32] | International | Y |
| 2019 | French Society of Anaesthesia and Intensive Care Medicine and French‐speaking Intensive Care Society [33] | France | N |
| 2018 | Difficult Airway Society [3] | UK | N |
| 2018 | Société Française d'Anesthésie et de réanimation [34] | France | N |
| 2017 | French Society of Anaesthesia and Intensive Care Medicine [35] | France | N |
| 2017 | Chinese Collaboration Group for Emergency Airway Management [36] | China | N |
| 2017 | Association of Anaesthetists [37] | UK | N |
| 2016 | All India Difficult Airway Association [38] | India | N |
| 2016 | All India Difficult Airway Association [4] | India | N |
Overall, we found that items relating to human factors were well represented in the 26 included airway guidelines. Terms relating to work system were the most frequently mentioned; all six elements of the work system domain were present in all included guidelines. The other two major domains as defined by the SEIPS model, processes and outcomes/adaptations, were well represented. Within the processes domain, planning and role allocation were the prominent elements identified. Within outcomes/adaptations, organisational issues were shown to be the predominant element with user outcomes the least mentioned element. Table 3 illustrates the prevalence of each major domain among the papers.
Table 3.
Prevalence of human factors of each included paper as per the three Systems Engineering Initiative for Patient Safety (SEIPS) domains.
| Work systems | Processes | Outcomes/adaptation | |
|---|---|---|---|
| Law et al. [16] | X | X | X |
| Kornas et al. [17] | X | Z | Z |
| Velly et al. [18] | X | Z | X |
| Foley et al. [19] | X | Z | Z |
| Ahmad et al. [1] | X | X | Z |
| Dobson et al. [20] | X | X | X |
| Lopez et al. [21] | X | X | Z |
| Zucco et al. [22] | X | Z | Z |
| Chen et al. [23] | X | Z | O |
| Brewster et al. [24] | X | X | X |
| Cook et al. [25] | X | Z | Z |
| Sorbello et al. [26] | X | Z | Z |
| Malhotra et al. [27] | X | Z | O |
| Zuo et al. [28] | X | Z | O |
| Patwa et al. [29] | X | Z | Z |
| Kim et al. [30] | X | Z | Z |
| Ting et al. [31] | X | Z | Z |
| Yao et al. [32] | X | Z | Z |
| Quintard et al. [33] | X | Z | X |
| Higgs et al. [3] | X | X | X |
| Langeron et al. [34] | X | Z | Z |
| Quintard et al. [35] | X | Z | Z |
| Sun et al. [36] | X | Z | O |
| Lockey et al. [37] | X | Z | X |
| Myatra et al. [38] | X | Z | X |
| Myatra et al. [4] | X | Z | X |
X, all subdomains present; Z = some of the subdomains present; O, no subdomains present.
Discussion
In this review, we aimed to explore how human factors appear within airway management guidelines. We describe the domains and elements and quantify the nature of the recommendations included in these 26 published airway guidelines in relation to an accepted healthcare system safety framework, SEIPS.
The concept of an ‘airway time‐out’ has gained more traction in the recent literature and is commonly included in guidelines. By contrast, there are newly developed process and communication interventions which are generally not yet included. These emergent ideas include ‘sterile communication’, a concept where all non‐essential communication/activity is banned at critical phases of airway management, stating of glottic view by the airway operator and confirmation of exhaled carbon dioxide to the team. The authors believe that if these new interventions prove effective, they should be included in future guidelines as a means to improve communication at critical event intervals and reduce cognitive workload.
Collectively, human factors recommendations were well represented in the 26 airway guidelines. However, some subcategories were less well represented. For example, within the cognitive aids element, analysis distinguishing between algorithms and cognitive aids revealed less than half of the guidelines illustrated or demonstrated a cognitive aid. Of the 22 guidelines which included coding terms associated with cognitive aids, 15 simply referred to their importance in the management of the airway or referenced articles discussing cognitive aids but failed to mention or detail a specific cognitive aid in the guideline.
Research involving simulation supports the use of cognitive aids in anaesthesia, as well as in other fields of medicine [39, 40, 41, 42]. Despite the increased focus on human factors in anaesthesia, and the known evidence supporting the use of cognitive aids to reduce slips, lapses and mistakes, cognitive aids were not included in four guidelines, and mentioned but not presented in an additional 15, totalling 19 of 26 (73%) [43]. Cognitive aids can and should be adapted to fit the local context with variations in protocols, availability of equipment and training across hospitals [41]. The process of adaptation of cognitive aids has been shown to be associated with improved implementation, with lack of local adaptation and unsatisfactory design being associated with poor implementation and adoption of cognitive aids across hospital networks [44].
A key feature of the SEIPS model of healthcare system safety is that analysis of patient and user outcomes data allows organisations and individuals to redesign the work system via a feedback loop. Our study has demonstrated that patient and user outcomes were the least represented human factors recommendations overall, making up less than one‐fifth of all coding terms identified. More strikingly, we found that the author's perceived experience of increased focus of user outcomes as a result of the COVID‐19 pandemic appears not to be reflected in the corresponding COVID‐19‐specific airway guidelines. This was evidenced by user and patient outcomes elements making up a smaller proportion of mentions in non‐COVID‐19‐specific guidelines compared with COVID‐19‐specific guidelines. It may be appropriate that the scale is still tipped towards content heavier work system recommendations but the comparative lack of outcome measurement and adaption is a key finding from our study which should be addressed. The authors believe that future guideline development (or updates) should allow for feedback from both user and patient outcomes following the implementation of an airway guideline. By facilitating this feedback, appropriate adaptation could potentially form part of a much‐needed improvement in the evidence basis from which airway guidelines are designed. The key recommendations of this paper are found in Table 4.
Table 4.
Key recommendation for guideline development.
|
‐ Future research and guideline development should consider a systems‐based approach to airway management ‐ Guideline development should maintain human‐centred design ‐ Cognitive aids, simulation programs and outcomes should be included ‐ Systems for review processes which allow for local adaptation of guidelines integrating both patient and user should be implemented ‐ Following the implementation of an airway guideline, feedback from both user and patient outcomes should be allowed for further development and updates |
This is a novel narrative review detailing the prevalence of human factors terms and recommendations within airway management guidelines. It is also the first review that stratifies specific human factor themes as per the SEIPS model and details within current airway management guidelines which human factor themes are most commonly included and, perhaps more importantly, which remain absent.
The primary limitation of this paper is the narrow scope of airway guidelines limited to the last five years. This recent snapshot allowed the authors to examine and analyse the tone of human factors in airway guidelines related to current practice; however, it limited the ability to examine trends over a longer period of time.
In conclusion, human factors are generally well represented within current airway management guidelines. Many clinicians have an intuitive understanding of the importance of communication, insight into their cognitive biases and the need for efficient and effective workspaces. How we address human factors systematically during guideline development remains an area in development. By assessing which human factors have been emphasised in airway management guidelines, this may perhaps guide us to which human factors are well represented, and which are yet to be fully addressed.
Supporting information
Appendix S1. Search strategy.
Appendix S2. Results of coded human factor term search.
Acknowledgements
LD is an Editor and SM is an Associate Editor of Anaesthesia. MT is an Editor of Anaesthesia Reports. No other competing interests declared. Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Contributor Information
D. A. Edelman, @Daniel_edelman.
L. V. Duggan, @drlauraduggan.
S. L. Lockhart, @Shannonlockhart.
S. D. Marshall, @hypoxicchicken.
M. C. Turner, @MaryannCTurner.
D. J. Brewster, Email: dbrewster@cabrini.com.au, @drdavidbrewster.
References
- 1. Ahmad I, El‐Boghdadly K, Bhagrath R, et al. Difficult airway society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 2020; 75: 509–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Edelman DA, Perkins EJ, Brewster DJ. Difficult airway management algorithms: a directed review. Anaesthesia 2019; 74: 1175–85. [DOI] [PubMed] [Google Scholar]
- 3. Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. British Journal of Anaesthesia 2018; 120: 323–52. [DOI] [PubMed] [Google Scholar]
- 4. Myatra SN, Shah A, Kundra P, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian Journal of Anaesthesia 2016; 60: 885–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Marshall S. The use of cognitive aids during emergencies in anesthesia. Anesthesia and Analgesia 2013; 117: 1162–71. [DOI] [PubMed] [Google Scholar]
- 6. Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the 4th National Audit Project of the Royal College of Anaesthetists and the difficult airway society. Part 1 Anaesthesia. British Journal of Anaesthesia 2011; 106: 617–31. [DOI] [PubMed] [Google Scholar]
- 7. Caplan RA, Benumof JI, Berry FA, et al. Ovassapian: guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology 1993; 78: 597–602. [PubMed] [Google Scholar]
- 8. Frerk C, Mitchell VS, McNarry AF, et al.; Difficult Airway Society Intubation Guidelines Working Group . Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults. British Journal of Anaesthesia 2015; 115: 827–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Health and Safety Executive . Reducing Error and Influencing Behaviour [HSG48]. 2nd ed., 1999. TSO. https://www.tso.co.uk (accessed 23/06/2022). [Google Scholar]
- 10. Reason J. Human error: models and management. British Medical Journal 2000; 320: 768–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aaberg OR, Hall‐Lord ML, Husebø SIE, et al. A human factors intervention in a hospital ‐ evaluating the outcome of a TeamSTEPPS program in a surgical ward. BMC Health Services Research 2021; 21: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jones C, Fawker‐Corbett J, Groom P, Morton B, Lister C, Mercer S. Human factors in preventing complications in anaesthesia: a systematic review. Anaesthesia 2018; 73: 12–24. [DOI] [PubMed] [Google Scholar]
- 13. Marshall SD, Touzell A. Human factors and the safety of surgical and anaesthetic care. Anaesthesia 2020; 75: e34–e38. [DOI] [PubMed] [Google Scholar]
- 14. Carayon P, Schoofs Hundt A, Karsh B‐T, et al. Work system design for patient safety: the SEIPS model. Quality and Safety in Health Care 2006; 15: i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013; 56: 1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Law JA, Duggan LV, Asselin M, et al. Canadian airway focus group updated consensus‐based recommendations for management of the difficult airway: part 1. Difficult airway management encountered in an unconscious patient. Canadian Journal of Anesthesia 2021; 68: 1373–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kornas R, Owyang C, Sakles J, Foley L, Mosier J. Evaluation and management of the physiologically difficult airway: consensus recommendations from Society for Airway Management. Anesthesia and Analgesia 2020; 132: 395–405. [DOI] [PubMed] [Google Scholar]
- 18. Velly L, Gayat E, Quintard H, et al. Guidelines: Anaesthesia in the context of COVID‐19 pandemic. Anaesthesia, Critical Care and Pain Medicine 2020; 39: 395–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Foley LJ, Urdaneta F, Berkow L, et al. Difficult airway management in adult coronavirus disease 2019 patients: statement by the Society of Airway Management. Anesthesia and Analgesia 2021; 133: 876–90. [DOI] [PubMed] [Google Scholar]
- 20. Dobson G, Chow L, Filteau L, et al. Guidelines to the practice of anesthesia ‐ revised edition 2020. Canadian Journal of Anaesthesia 2020; 67: 64–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. López AM, Belda I, Bermejo S, et al. Recommendations for the evaluation and management of the anticipated and non‐anticipated difficult airway of the Societat Catalana d'Anestesiologia, Reanimació i Terapèutica del dolor, based on the adaptation of clinical practice guidelines and expert consensus. Revista Espanola de Anestesiologia y Reanimacion 2020; 67: 325–42. [DOI] [PubMed] [Google Scholar]
- 22. Zucco L, Levy N, Ketchandji D, Aziz M, Ramachandran SK. An update on the perioperative considerations for COVID‐19 severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2). https://www.apsf.org/article/an-update-on-the-perioperative-considerations-for-covid-19-severe-acute-respiratory-syndrome-coronavirus-2-sars-cov-2 (accessed 21/01/2022).
- 23. Chen X, Liu Y, Gong Y, et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the joint task force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology 2020; 132: 1307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brewster DJ, Chrimes N, Do TB, et al. Consensus statement: safe airway society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group. Medical Journal of Australia 2020; 212: 472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cook TM, El‐Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID‐19: guidelines from the difficult airway society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020; 75: 785–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sorbello M, El‐Boghdadly K, Di Giacinto I, et al. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia 2020; 75: 724–32. [DOI] [PubMed] [Google Scholar]
- 27. Malhotra N, Joshi M, Datta R, Bajwa S, Mehdiratta L. Indian Society of Anaesthesiologists (ISA national) advisory and position statement regarding COVID‐19. Indian Journal of Anaesthesia 2020; 64: 259–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zuo MZ, Huang YG, Ma WH, et al. Expert recommendations for tracheal intubation in critically ill patients with novel coronavirus disease 2019. Chinese Medical Sciences Journal 2020; 35: 105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Patwa A, Shah A, Garg R, et al. All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID‐19 pandemic. Indian Journal of Anaesthesia 2020; 64: S107–S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kim HJ, Ko JS, Kim TY. Recommendations for anesthesia in patients suspected of COVID‐19 coronavirus infection. Korean Journal of Anesthesiology 2020; 73: 89–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ting CK, Chen CW, Liu SK, et al. Endotracheal intubation in patients with COVID‐19 infection: expert panel‐based consensus recommendations. Asian Journal of Anesthesiology 2020; 58: 61–3. [DOI] [PubMed] [Google Scholar]
- 32. Yao W, Wang T, Jiang B, et al. Emergency tracheal intubation in 202 patients with COVID‐19 in Wuhan, China: lessons learnt and international expert recommendations. British Journal of Anaesthesia 2020; 125: e28–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Quintard H, l'Her E, Pottecher J, et al. Experts' guidelines of intubation and extubation of the ICU patient of French Society of Anaesthesia and Intensive Care Medicine (SFAR) and French‐speaking Intensive Care Society (SRLF). Annals of Intensive Care 2019; 9: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Langeron O, Bourgain JL, Francon D, et al. Intubation and extubation in adult anaesthesia. Anaesthesia, Critical Care and Pain Medicine 2018; 37: 639–51. [DOI] [PubMed] [Google Scholar]
- 35. Quintard H, l'Her E, Pottecher J, et al. Intubation and extubation of the ICU patient. Anaesthesia Critical Care and Pain Medicine 2017; 36: 327–41. [DOI] [PubMed] [Google Scholar]
- 36. Sun F, Wang Y, Ma S, et al. Clinical consensus of emergency airway management. Journal of Thoracic Disease 2017; 9: 4599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lockey DJ, Crewdson K, Davies G, et al. AAGBI: safer pre‐hospital anaesthesia 2017. Anaesthesia 2017; 72: 379–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Myatra SN, Ahmed SM, Kundra P, et al. The all India difficult airway association 2016 guidelines for tracheal intubation in the intensive care unit. Indian Journal of Anaesthesia 2016; 60: 922–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Koers L, van Haperen M, Meijer CGF, et al. Effect of cognitive aids on adherence to best practice in the treatment of deteriorating surgical patients: a randomized clinical trial in a simulation setting. Journal of the American Medical Association Surgery 2020; 155: e194704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Harvey R, Foulds L, Housden T, et al. The impact of didactic read‐aloud action cards on the performance of cannula cricothyroidotomy in a simulated ‘can't intubate can't oxygenate’ scenario. Anaesthesia 2017; 72: 343–9. [DOI] [PubMed] [Google Scholar]
- 41. Marshall S, Mehra R. The effects of a displayed cognitive aid on non‐technical skills in a simulated ‘can't intubate, can't oxygenate’ crisis. Anaesthesia 2014; 69: 669–77. [DOI] [PubMed] [Google Scholar]
- 42. Marshall S, Sanderson P, McIntosh CA, Kolawole H. The effect of two cognitive aid designs on team functioning during intra‐operative anaphylaxis emergencies: a multi‐centre simulation study. Anaesthesia 2016; 71: 389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Arriaga AF, Bader AM, Wong JM, et al. Simulation‐based trial of surgical‐crisis checklists. New England Journal of Medicine 2013; 368: 246–53. [DOI] [PubMed] [Google Scholar]
- 44. Alidina S, Goldhaber‐Fiebert SN, Hannenberg AA, et al. Factors associated with the use of cognitive aids in operating room crises: a cross‐sectional study of US hospitals and ambulatory surgical centers. Implementation Science 2018; 13: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Search strategy.
Appendix S2. Results of coded human factor term search.


