Abstract
Background
Physical restraints are used in nursing homes (NHs) despite their negative consequences. Use of surveillance technologies as alternatives to physical forms of restraints and negative staff opinions about the appropriateness of restraint use have been postulated to reduce this practice; however, these have rarely been investigated alongside resident outcome data. This study aimed to measure physical restraint prevalence in Swiss NHs and its associations with (a) the use of surveillance technologies and (b) staff's opinion about the appropriateness of physical restraint use.
Methods
This cross‐sectional multicenter study analyzed data on 3,137 staff and 6,149 residents of 292 units in 86 Swiss NHs (2018–2019). Based on routine resident data, we measured the prevalence of two classes of physical restraint: (a) bedrails or (b) trunk fixation or seating option that prevents standing. To assess potential factors associated with restraint use, we applied a logistic multilevel model.
Results
A 11.1% of residents were restrained with at least one form of physical restraint. Against our hypothesis, surveillance technologies were not significantly associated with restraint use, and staff members' opinion that the use of physical restraints was appropriate on their unit was associated with decreased odds of residents being restrained (odds ratio (OR): 0.48; 95% confidence interval (CI) 0.29–0.80).
Conclusions
Although Swiss NHs have a low prevalence of physical restraint use, only a minority of NH units do not use any restraints with their residents. Surveillance technologies seem to be used concurrently with restraints and not as an alternative. Further research should investigate staff's current and intended uses of surveillance technologies in practice. Staff members' opinion that they use restraints inappropriately might correctly reflect overuse of restraints on their unit. If so, staff ratings of inappropriate restraint use may identify units that need improvement.
Keywords: attitude, nurses, nursing homes, physical, restraint, technology
Key points
Physical restraint use was not related to the use of surveillance technologies in Swiss nursing home units.
Staff opinion that their units' physical restraint use was inappropriate was associated with higher odds of residents being restrained.
Why does this paper matter?
Although surveillance technology is offered as an alternative to physical restraint use, our data show that its use is not associated with lower use of physical restraints. Further exploration is needed about the interplay of surveillance technology and physical restraint use. Staff opinions about the appropriateness of physical restraint use might be a helpful indicator of its overuse.
INTRODUCTION
Despite physical restraints' known lack of effectiveness and safety, 1 , 2 they are commonly used in nursing homes (NHs). Defined as “any action or procedure that prevents a person's free body movement to a position of choice and/or normal access to his/her body by the use of any method, attached or adjacent to a person's body that he/she cannot control or remove easily,” 3 physical restraints include measures such as wrist or ankle belts, bedrails, tightly tucked sheets, or (wheel)chairs with locked tray tables or brakes. 2 In addition to the risk of serious and harmful consequences, physical restraint use reduces residents' quality of life. 4 , 5 While restraint use raises ethical questions concerning residents' autonomy, self‐determination, and dignity, 6 many NHs still consider it a necessary safety measure, for example, against falls, or to deal with certain problem behaviors, for example, aggression and wandering. 7 , 8 , 9
Prevalence for physical restraint use ranges widely internationally. Beyond country‐specific differences, the heterogeneity of research methods and wide variations in conceptual and operational definitions impedes international comparisons. 1 , 2 , 10 A 2021 meta‐analysis reported a pooled prevalence of 37% in Europe and of 22% in North America,2 while a 2021 scoping review reported a median occurrence of 26.5% in European NHs, with substantial variability (range: 7.7%–60.5%). 10 Several factors have been investigated in relation to physical restraint use, such as public reporting policies, organizational characteristics (e.g., staffing), organizational culture, and resident characteristics. While resident characteristics—especially higher levels of cognitive deficiency and dependency—have been repeatedly significantly associated with increased restraint use, most other factors have produced mixed results. 11 , 12 , 13 , 14 , 15 , 16
The last two decades have seen many changes in the NH sector in relation to physical restraint use. On one hand, many countries, including Switzerland in 2013, have implemented least‐restraint policies or laws aiming to restrict restraint use, which have been hypothesized to have influenced prevalence rates, staff’ practices, and opinions. 1 In the United States, for instance, the passage of the Omnibus Budget Reconciliation Act of 1987 has been associated with a large reduction of the proportion of restrained residents. 17 On the other hand, technologies have developed and have been increasingly used in NHs. 18 Specifically, the use of surveillance technologies (e.g., sensor‐based, cameras, GPS tracking) has been hypothesized to lead to the reduction of physical restraint use as they could be used as a less restrictive alternative to physical restraints. For instance, residents can wear bracelets that allow them to go through some doors but not others, for example, ensuring they do not leave the facility’ premises but allowing them to walk freely within the facility. 18 , 19 , 20 , 21 However, despite its increased use, there is a striking lack of research on the use of such technologies in NHs and their effects on physical restraint use.
Staff attitudes about the use of physical restraints have been explored across many countries. A 2014 systematic review concluded that, despite a generally negative attitude toward restraint use, geriatric care staff often consider restraints necessary. 8 The main hypothesis in the literature is that staff who find the use of restraints inappropriate are less likely to use such restraints. However, few studies have linked staff opinions (i.e., their opinion about the appropriateness of restraint use) to resident‐level measurements of physical restraint use, and those studies date back from the early 2000s, before many least‐restraint policies were introduced. 8 , 22
In this article, we used a socio‐technical approach, which highlights how interactions between social and technical elements contribute to organizational achievements, to recognize the interactions between staff and technology and their influence on restraint use. 23 , 24
To address the knowledge gaps highlighted before, the study has two aims: (1) to describe the prevalence of physical restraint use in Swiss NHs and (2) to explore the association between physical restraint use and (a) surveillance technology use, hypothesizing less restraint use with more surveillance technology use, and (b) staff opinion toward the appropriateness of restraint use, hypothesizing more restraint use with more positive opinion regarding its appropriateness.
METHODS
Study design and sample
This study is based on data collected during the Swiss Nursing Home Human Resources Project 2018 (SHURP 2018), a cross‐sectional, multicenter study in Swiss NHs. Data were collected from a convenience sample of NHs recruited either (1) by inviting facilities that had participated in the first edition of the SHURP study 25 to participate again, (2) by inviting randomly‐selected NHs, and (3) by accepting any other facility willing to participate. Recruitment took place between November 2017 and March 2019. NHs unable to provide physical restraint use data for their resident populations were excluded from the subsample used in this study. We included staff of all educational levels who had been working in their current NHs and on their current units a minimum of 20% (i.e., 8.4 h/week) for a minimum of 1 month. Residents were included in the sample if their available records included data on physical restraint use.
Measurements and data collection
Data on residents, staff, unit, and facility characteristics were collected between September 2018 and October 2019. Residents' data came from routinely collected data while staff, unit, and facility data were collected with questionnaires.
Our outcome of interest was physical restraint use measured at resident level. In this study, it is operationalized to cover: (1) use of bedrails and (2) use of trunk fixation or any seating option that prevents residents from standing up. A resident is considered restrained if one or both types of restraints have been applied on six of the seven last days. 26 Examples of the measures are provided in Table 1. In Switzerland, physical restraint is defined in a similar way as in the United States (i.e., with MDS 3.0.), although there are differences: e.g., the United States is more restrictive in the definition of the frequency used (i.e., daily use vs 6 of the last 7 days in Switzerland). 27
TABLE 1.
Variables' descriptions and measurements
| Variables | Description and measurement |
|---|---|
| Facility level | |
| Ownership status | Publicly‐owned, that is, owned by a government body versus privately‐owned, that is, either for profit or not for profit |
| Unit level | |
| Size of the unit/ward | Size of the unit based on the number of beds, categorized as: small: ≤ 20 beds; medium: 21–30 beds; large: ≥ 31 beds |
| Number of FTE/100 beds | Number of FTE staff positions divided by the number of beds on the unit, multiplied by 100 |
| Dementia‐focus unit | Unit offers dementia care: yes/no answer |
|
Use of surveillance technologies Use of pressure‐detection mats Use of cameras Use of an electronic system to control the ability to open doors Use of electronic bracelets |
Each item covers a type of surveillance technology either used on the unit or not: yes/no answer |
| Individual level | |
| Staff | |
| MAQ subscale on the staff's opinion regarding the appropriateness of physical restraint use on their unit | The MAQ tool uses a 5‐point Likert‐type scale from 1 (strongly disagree) to 5 (strongly agree). Three items are inversely recoded. A score of 1 indicates a negative attitude towards restraint, that is, finding restraints use inappropriate and a score of 5 indicates a positive attitude, that is, finding restraint use appropriate. Cronbach's α: 0.74. The unit‐mean was calculated based on individual scale scores. Items are as follow: (A) My ward/unit uses physical restraints far too often; (B) If we use physical restraints, it is always necessary; (C) Physical restraints are used too quickly; (D) Physical restraints are applied as a result of convenience to nursing staff. |
| Residents | |
| Age | Age in years |
| Sex | Female or male |
| Care level | Based on the national reimbursement system, each resident is allocated to one of twelve levels of care demand, where each increase of one level represents an additional 20 min of care time needed by the resident per day. |
| Cognitive Performance Scale (CPS) | The CPS measures cognitive impairment and is calculated on a scale from 0 (intact) to 6 (very severe impairment). The scale has fine internal consistency, inter‐rater reliability and validity. |
| Physical restraint status |
Resident is restrained by either bedrails or by trunk fixation/seating option that prevents from rising or by both, in the last 7 days: yes/no In accordance with the definitions of the national quality indicators concerning physical restraint used in Switzerland, residents who were competent to make decisions and capable to provide informed consent, and who had either requested or agreed to physical restraint measures were excluded. |
| Bedrails | Resident is restrained by daily use of bedrails or other devices on all open sides of the bed that did not allow the resident to leave the bed independently in the last 7 days: yes/no. These include full‐enclosure bedrails or unilateral bedrail at one side of the bed with the wall on the other side. |
| Trunk fixation or seating option that prevents residents from standing up | Resident is restrained by daily fixation of the trunk or with seating that prevented the resident from rising in the last 7 days): yes/no. These include a large number of restraints such as belt restraints, chair with a locked tray table, geri‐chair, wheelchair locked in front of table, deep chairs, tight sheet, vests, etc. |
Abbreviations: CPS, Cognitive Performance Scale; FTE, full‐time equivalent; MAQ, Maastricht Attitude Questionnaire.
Resident data (i.e., characteristics, including cognitive performance scale (CPS), 28 and physical restraint status) were collected by NHs using an updated version of their resident assessment instrument—either (1) the Resident Assessment Instrument–Nursing Home (RAI–NH) or (2) the BewohnerInnen‐Einstufungs‐und Abrechnungssystem (BESA) (i.e., resident classification and billing system). With these instruments, NHs collect routine data at regular intervals to evaluate residents' needs, to plan residents' care, and to make health insurance claims. Such assessments must be performed for each resident upon admission, then at least once every 6 months. 29 NH staff is trained and supervised in collecting these data. A pilot study assessed how Swiss NH staff collected physical restraint data and concluded that it was collected reliably, reducing the risk of bias. 30
Facility, unit and staff data were collected using paper questionnaires. Facility‐level data covered NH's ownership status, while unit‐level data covered each unit's size, type, and staffing level, as well as which types of surveillance technologies were in use. Staff‐level data covered staff opinions on how appropriately physical restraint is applied on their unit, according to them. This was measured using 4 items from the appropriateness subscale of the validated Maastricht Attitude Questionnaire (MAQ). 31 Definitions and measurement of the variables are presented in Table 1.
Data analysis
We examined the data for completeness, plausibility, and missing values. Missing values (all <5.0%) are displayed in Table 2. Missing data were deleted listwise. We computed descriptive statistics for basic characteristics (frequencies, percentages, means, standard deviations [SDs]). The outcome variable—physical restraint—is binary, that is, it differentiates residents who were restrained from those who were not. We performed a 3‐level logistic multilevel analysis to examine factors associated with physical restraint use at resident level (level 1), modeling unit‐level data and staff data aggregated at unit level on level 2, and facility‐level data on level 3. This approach was based on a calculation of interclass correlation 1 (ICC1), which indicates the proportions of between‐units and between‐facilities variance attributable to the group level. 32 Because ICC1 yielded a value of 0.09 (CI: 0.06–0.12) on the unit level and 0.08 (CI: 0.04–0.11) on the facility level, both unit and facility IDs were used as random effects in the model. Along with resident care level and cognitive status, facility ownership status, number of FTE/100 beds, and the unit's focus on dementia were used as control variables. p‐values <0.05 were considered significant. Two additional multilevel logistic regression models were also computed separately for each class of physical restraint (bedrails or trunk fixation/seating that prevents standing).
TABLE 2.
Descriptive results for the overall sample are stratified for units with average use of physical restraints and for units with above‐average use of physical restraints
| Overall sample values | Units with average or under average use of physical restraint | Units with above‐average use of physical restraint | SMD | |
|---|---|---|---|---|
| Facilities (n = 86) | ||||
| Ownership status, public, % | 50.0 (43) | N/A | N/A | |
| Units (n = 287 units) a | ||||
| FTE/100 beds, mean a ± SD | 49.1 (15.8) | 49.4 (15.8) | 45.3 (15.5) | |
| Unit size | ||||
| Small (up to 20 beds), % (n) | 28.6 (82) | 29.8 (79) | 13.6 (3) | |
| Medium (21–30 beds), % (n) | 48.1 (138) | 47.5 (126) | 54.5 (12) | |
| Large (31 beds and more), % (n) | 23.3 (67) | 22.6 (60) | 31.8 (7) | |
| Unit offers dementia‐focused services, % yes (n) | 72.8 (209) | 72.1 (191) | 81.8 (18) | |
| Unit leaders (n = 265 units) a | ||||
| Use of surveillance technologies, % yes (n) | ||||
| Unit uses pressure‐sensitive detection mats | 93.6 (248) | 94.3 (232) | 84.2 (16) | |
| Unit uses electronic bracelets | 67.5 (179) | 68.7 (169) | 52.6 (10) | |
| Unit uses electronic system to control the ability to open doors | 30.6 (81) | 31.3 (77) | 21.0 (4) | |
| Unit uses cameras | 5.7 (15) | 5.7 (14) | 5.3 (1) | |
| Staff (n = 291 units) a | ||||
| Appropriateness of physical restraint use (MAQ, range: 1–5), mean ± SD | 4.1 (0.34) | 4.1 (0.35) | 3.9 (0.27) | 0.54 |
| Item A c : My ward/unit uses physical restraints far too often, mean ± SD | 3.9 (0.47) | 4.0 (0.46) | 3.6 (0.42) | 0.80 |
| Item B: If we use physical restraints, it is always necessary, mean ± SD | 4.0 (0.41) | 4.0 (0.42) | 3.9 (0.31) | 0.22 |
| Item C c : Physical restraints are used too quickly, mean ± SD | 3.9 (0.39) | 3.9 (0.44) | 3.7 (0.35) | 0.53 |
| Item D c : Physical restraints are applied as a result of convenience of nursing staff, mean ± SD | 4.4 (0.39) | 4.4 (0.39) | 4.4 (0.33) | 0.10 |
| Residents (n = 6,149) b | ||||
| Gender, female, % (n) | 70.6 (4341) | 71.1 (3900) | 66.4 (441) | |
| Age in years, mean ± SD | 84.8 (10.0) | 85.1 (9.3) | 81.8 (14.3) | |
| Care level, 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 mean ± SD | 5.8 (2.7) | 5.8 (2.7) | 6.2 (2.7) | |
| CPS score, 1 , 2 , 3 , 4 , 5 , 6 mean ± SD | 2.5 (1.6) | 2.5 (1.6) | 2.6 (1.7) | |
| Physically restrained, % (n) | 11.1 (682) | 8.8 | 29.7 | |
| Physically restrained by bedrails, % (n) | 10.9 (642) | 8.7 | 29.1 | |
| Physically restrained by trunk fixation/seating option, % (n) | 2.4 (149) | 1.8 | 7.8 | |
Abbreviations: CPS, Cognitive Performance Scale; FTE, Full‐time equivalent; MAQ, Maastricht Attitude Questionnaire; SMD, Standardized mean difference.
Total number of units with residents with quality indicator information in the overall sample: 292. The group of units with average use of physical restraints consists of n = 268; the group of units with above‐average use of physical restraints consist of n = 24. We did not receive unit information for 5 units (questionnaires not sent back); unit leaders: we did not receive unit leaders information for 27 units (questionnaires not sent back); staff: we did not receive any information from 1 unit (no questionnaires were sent back).
Missing values for the use of bedrails were of 4.6% (n = 284).
These variables have been recoded according to the MAQ manual.
To confirm our regression results regarding the relationship between staff opinion and restraint use, we categorized NH units in two groups: units with high use of restraints versus units with average or low use of restraints. Units were categorized based on a random effect caterpillar plot using a logistic mixed model adjusted for resident characteristics (i.e., care level and cognitive status), with unit as a random effect. This approach allowed us to discern differences between units beyond chance and resident characteristics. 26 Based on this model, units applying significantly more restraints than the sample mean were categorized as “above‐average” units and units using average as well as under‐average use of restraints were included in the “average” group (i.e., because the under‐average group, n = 4, was too small to be its own group). To indicate effect sizes, we have calculated standardized mean differences (SMD), equivalent to Cohens' D. Values of 0.2–0.5 are considered small, >0.5–0.8 medium, and >0.8 large. 33
We used boxplots to illustrate the differences in staff opinion levels between the “above‐average” units and the “average” units. Boxplots were computed for the MAQ “appropriateness” subscale and for each of the subscale's items. Data analyses were performed using R version 4.0.4. 32 ICCs were computed using the rptR package, 34 logistic mixed models using the lme4 package,35 and boxplots using the ggplot2 package. 36
Ethical aspects
This study received an ethics waiver from the appropriate Swiss ethics committee, as it was observational and individuals' data were collected anonymously (Northwest and Central Switzerland ethics committee, BASEC Nr Req‐2018‐00420). Each NH participated voluntarily, with the relevant administrators providing written consent before the study's start. Individual respondents were informed about the study; participation was voluntary; and returning the filled questionnaire was considered as informed consent. All resident data were anonymized before being transferred to the study team.
RESULTS
Sample description
Of the 118 NHs initially recruited, 86 had collected physical restraint data, making them eligible for inclusion. The final sample consisted of 3,137 staff and 6,149 residents from 292 units in 86 NHs (see flowchart in Figure S1). Half (n = 43) of the participating facilities were publicly owned (i.e., government‐owned). The mean number of residents per unit was 21.1 (SD: 10.0). Of all included staff, 88.2% were female, 25.6% 30 years and younger, 38.4% between 31 and 50 years old, and 36.0% 51 years and older. Most were licensed practical nurses (31.3%), followed by registered nurses (29.5%), nurse aides (21.4%), and certified assistant nurses (15.5%) (other qualifications: 2.3%). The staff's mean response rate was 67.2%.
Prevalence of physical restraint use in Swiss nursing home units
A total of 11.1% (n = 682) of residents were physically restrained with at least one form of restraint (unit‐level range: 0.0%–63.6%). Looking at the two broad classes of restraints used, 10.9% involved bedrails (n = 642 of 5,865 with valid information, unit‐level range: 0.0%–61.1%), and 2.4% involved trunk fixations or seating options that prevented standing up (n = 149 of 6,149 with valid information, unit‐level range: 0.0%–60.0%). Both types of restraints were used on 109 residents. A total of 88 units (30.1%) spread across 41 NHs used no physical restraints. In Table 2, we present descriptive facility, unit, staff, and resident characteristics for the overall sample. There were no missing facility, unit, and staff data except for FTE/100 beds (n = 3, 1.0%). Regarding resident characteristics, there were missing data for age (n = 1, 0.0%), CPS (n = 3, 0.0%), trunk fixation (n = 3, 0.0%), and bedrails (n = 284, 4.6%). We also compared characteristics of units with average use of restraint and units with significant above‐average use of physical restraint in order to illustrate differences between these two groups.
Association between physical restraint use and surveillance technology use
Contrary to our hypothesis, our regression analysis did not show any significant association between the use of surveillance technologies and physical restraint use (see Table 3). The descriptive results suggest that units which use technologies restrain their residents less, but this was not reflected in the regression model.
TABLE 3.
Unadjusted and adjusted multilevel logistic regression model to identify factors significantly associated with physical restraint use at resident level
| Unadjusted, n = 5,682 a | Adjusted, n = 5,682 | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p‐value | OR | 95% CI | p‐value | |
| Facilities | ||||||
| Ownership status: private b | 1.95 | 1.14–3.36 | 0.015 | |||
| Units | ||||||
| Unit size: medium c | 1.12 | 0.77–1.62 | 0.560 | 0.94 | 0.60–1.47 | 0.777 |
| Unit size: large c | 0.66 | 0.41–1.04 | 0.073 | 0.58 | 0.33–1.02 | 0.058 |
| FTE/100 beds d | 1.02 | 1.00–1.03 | 0.006 | 0.98 | 0.97–1.00 | 0.024 |
| Unit offers dementia‐focus services | 1.80 | 1.30–2.51 | <0.001 | 1.20 | 0.80–1.78 | 0.378 |
| Unit uses pressure‐sensitive detection mat | 1.74 | 0.88–3.45 | 0.111 | 1.71 | 0.76–3.84 | 0.192 |
| Unit uses electronic bracelets | 0.99 | 0.72–1.35 | 0.930 | 1.04 | 0.71–1.52 | 0.851 |
| Unit uses electronic system to control the ability to open doors | 0.97 | 0.73–1.29 | 0.826 | 0.94 | 0.67–1.33 | 0.733 |
| Unit uses cameras | 1.29 | 0.70–2.39 | 0.417 | 0.92 | 0.44–1.92 | 0.815 |
| Staff | ||||||
| Opinions on appropriateness of restraint use from staff (MAQ) | 0.54 | 0.35–0.82 | 0.004 | 0.48 | 0.29–0.80 | 0.005 |
| Residents | ||||||
| Care level b | 2.05 | 1.91–2.20 | <0.001 | |||
| CPS b | 1.67 | 1.53–1.83 | <0.001 | |||
| AIC | 3533.9 | 2352.1 | ||||
Abbreviations: OR, Odds ratio; CI, Confidence interval; FTE, Full‐time equivalent; MAQ, Maastricht Attitudes Questionnaire; CPS, Cognitive Performance Scale; AIC, Akaike's information criterion.
The model included 262 units from 85 nursing homes.
Given the inclusion of 12 variables, n = 5,682 had complete cases and a total n of 467 (7.6%) residents were excluded. Significant factors in the table are in bold.
Unit size: small ≤20 beds; medium 21–30 beds; large: ≥31 beds.
The upper bound for the adjusted model is 0.9991.
Association between physical restraint use and staff opinions
Contrary to our hypothesis, residents had significantly lower odds to be restrained in units where staff perceived that they were using physical restraints appropriately (OR: 0.48; 95% CI 0.29–0.80). The boxplots illustrated this conclusion: in units with lower prevalence of restraint use, staff found the use of restraints more appropriate (MAQ median score: 4.10) than their counterparts in units with higher restraint prevalence (MAQ median score: 3.99), which perceived the use of restraints as less appropriate (see Figure 1). There is a medium effect size between the two groups (SMD: 0.54), see Table 2. We also produced boxplots for each of the MAQ subscale's individual items (see Figure 2). Compared to the main model, separate models for bedrails and for trunk fixation/seating options that prevent standing showed no major differences (see Table S2).
FIGURE 1.
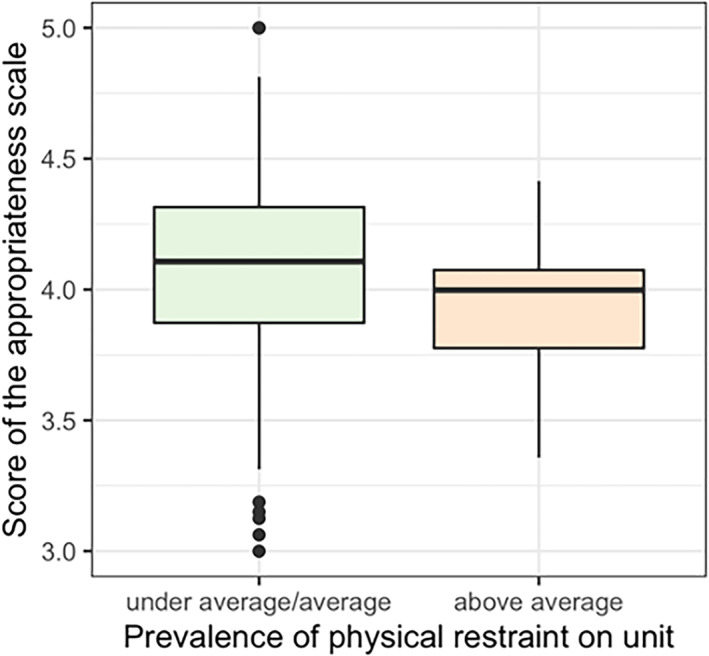
Boxplot of the “appropriateness of restraint use” subscale scoring in relation to the prevalence of physical restraint use on the unit. The units are stratified into two groups: units with under‐average as well as average use of restraints versus units with above‐average use of physical restraints compared to the sample mean. Maastricht Attitude Questionnaire (MAQ) subscale scores range from 1–5. Lower scores (towards 1) indicate more negative attitudes, that is, finding the use of restraints inappropriate, while higher scores (towards 5) indicate more positive attitudes towards restraints, that is, finding the use of restraints appropriate. The average group included n = 268 units; the above‐average group included n = 23 units
FIGURE 2.
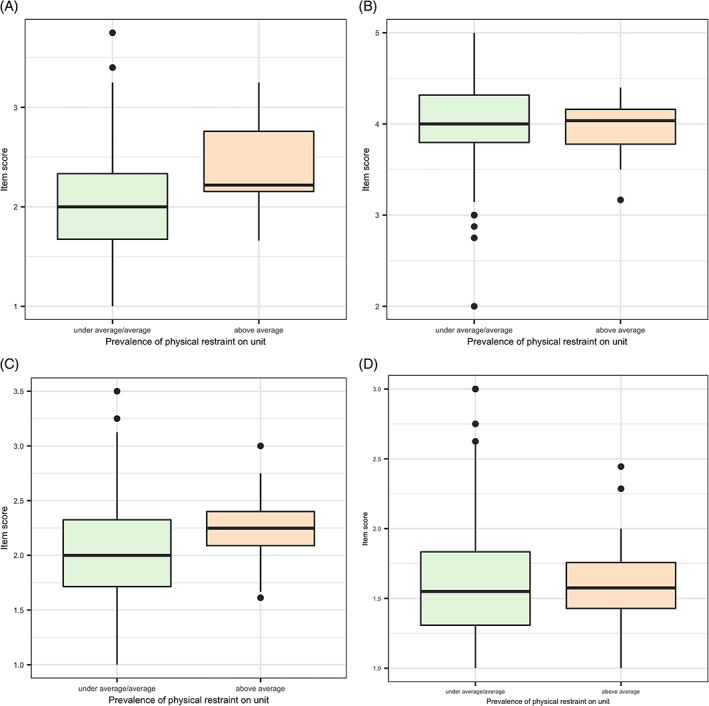
Boxplots of the mean ratings of each of the four items from the Maastricht Attitude Questionnaire “appropriateness” subscale stratified in two groups: units with under‐average as well as average use of restraints versus units with above‐average use of restraints. 5 means “strongly agree” and 1 means “strongly disagree” for the four items. (A) My ward/unit uses physical restraints far too often. (B) If we use physical restraints, it is always necessary. (C) Physical restraints are used too quickly. (D) Physical restraints are applied as a result of convenience of nursing staff
DISCUSSION
In our sample of 292 units across 86 Swiss NHs, 11.1% of residents were physically restrained. Although our descriptive results suggested that units using surveillance technologies had a lower number of restrained residents, we did not find any significant association in our regression model between surveillance technology use and restraint use. However, staff's opinion that their units used physical restraints inappropriately was associated with higher odds of residents being restrained, suggesting that team members are aware when their unit is overusing restraints.
Our results show that Switzerland has a relatively low prevalence of physical restraint use in international comparison. Studies measuring restraints in a similar way reported rates of 26% in Germany 37 and of 85% in Spain. 38 In the United States, studies have reported rates between 2.7% and 7.4%. 39 , 40 A recent meta‐analysis reported an overall pooled prevalence of 33% 1 but noted that the use of administrative data to measure restrains use (as this study did) yielded the lowest prevalence (20%) of any method used. This low prevalence might additionnally be explained by the fact that Switzerland does not count physical restraint use in residents who request it and are capable to give their informed consent, a differentiation not made in other countries.
A 2009 study focusing on uses of seating options and fixations as restraints reported that 31% of residents were restrained in Canada, 20% in Hong Kong, 9% in the United States, and 6% in Switzerland, 41 in contrast to 2.4% in our sample. Reported pooled prevalence figures range from 8% for chair restraints to 7% for trunk restraints to 3% for bed belts, and 44% was reported for the use of bedrails. 1 Our results are similar to those of an earlier (2016) Swiss study that measured the prevalence of bedrail use (13.0%) and that of trunk fixation/seating options that prevent standing up (3.4%). 26 Staff generally assess bedrails as less restrictive than belts, which partly explains the differences in prevalence between the two general types of restraints. 42 A recent scoping review concluded that reported rates of restraint use decreased (nonsignificantly) over the last decade, which is to take into account when comparing our findings to results from earlier studies. 10 While the current study's data indicate a relatively low prevalence (11.1%) of restraint use, there is high variability between units (range: 0.0%–63.6%), and despite research findings suggesting that restraint‐free nursing is an achievable goal in NHs, only 30.1% of our sample's units were providing such care. 43
We also investigated the relationship between the use of surveillance technologies and rates of physical restraint use. To the best of our knowledge, this is the first study investigating the use of these devices with data on physical restraint outcomes. On the basis of the literature, we hypothesized that surveillance technologies could be used to reduce and replace more restrictive forms of restraints (e.g., belts) allowing residents more bodily autonomy while maintaining their safety. 19 , 20 , 21 In our study, this hypothesis was not supported. This lack of association is in line with the results from a 2012 qualitative study, which concluded that Dutch staff tended to consider surveillance technology as an auxiliary measure to physical restraint use rather than as an alternative. 19 Still, our descriptive results show that units relying less on physical restraint were using surveillance technologies more (e.g., bracelets: 68.7%) than units with above‐average use of restraints (bracelets: 52.6%). As such, surveillance technologies might reduce the use of physical restraints in some cases. However, as we did not measure surveillance technology use at the resident level, our data cannot show whether these technologies were focused on already‐restrained residents or on others.
Our study brings much‐needed evidence to a current topic. Previous research suggested that attitudes toward surveillance technologies were less skeptical in North America than in Europe. 18 In the United States, for instance, the use of surveillance technologies such as cameras is already allowed in several states and increasing. 44 Cameras are used mainly to monitor staff's behaviors, but their use has also been hypothesized to potentially decrease physical restraint use too. 19 However, these developments are not evidence‐based, and this study does not support the use of such technology to reduce restraints. Further and particularly experimental research is warranted to examine ways in which surveillance technologies can be or are used, along with associated staff behaviors and impacts on residents.
The socio‐technical approach highlights the interconnected influence of both technologies and people on quality of care. The literature has suggested that attitudes play an important part in the decision to use physical restraints. 8 , 9 For the current study, we assessed one aspect of staff members' attitude toward restraint use by measuring the degree to which staff considered physical restraint appropriate in their daily clinical practice. Overall, the staff in our sample rated their units' restraint use as rather appropriate, with a mean MAQ subscale score of 4.1 (SD: 0.34) (range of 1: inappropriate—5: appropriate). This aligns with previous European NH findings, where scores ranged from 3.71 in Portugal to 4.37 in Austria, with Swiss staff scoring 4.02 (SD: 0.75). 42 , 45 , 46 , 47
Few recent studies have investigated staff attitudes in relation to their own units' use of restraints in practice, but none have used a validated scale to do so. 22 , 48 Myers et al. 48 found that staff attitudes were not predictive of their self‐reported restraint use. In 1999, Karlsson et al. showed that, despite an overall negative staff attitude regarding restraint use, almost a third of residents were restrained,49 and in 2001, they found staff less prone to use restraints in restraint‐free units than in others. 22
Two decades later, our analyses show that the odds of residents being restrained were lower in units where staff reported that they use restraints appropriately. Our further analysis confirmed this by showing that staff members working in units restraining higher‐than‐average proportions of residents tend to feel that restraints are used too often or too quickly. While there are statistically significant differences (medium effect size with SMD: 0.54), we do not know whether they reflect differences in staff's practices. This result does not support our hypothesis, which was that staff members finding restraints use appropriate were more likely to use them. Our explanation for this result is that staff finds restraints use inappropriate when they use it a lot because they are aware of the overuse of such measures in their unit. Likewise, on units where physical restraints are used sparingly, if at all, staff are more likely to consider that they use it appropriately.
Changes in policies and laws mandating the restriction of restraint use have been implemented in several countries over the last decades. In Switzerland, a 2013 federal law introduced a principle of restraint‐free care, allowing for exceptions, by laying out a procedure to be followed before physical restraint measures can be applied. 50 Furthermore, physical restraint use started to be measured in all Swiss NHs in 2019. Both developments have led to many practice changes in Swiss NHs through leadership and staff sensitization, which we might see reflected in our results.
This study's strengths include its large sample size and the relatively high participant response rate. It also has limitations. First, its cross‐sectional design does not allow causal inferences. Second, the included facilities were not randomly selected, which might have created a bias, especially regarding the (over‐)representation of higher‐performing NHs. This may limit the generalizability of the results. Furthermore, because of large variations of physical restraint definitions used in the literature, prevalence comparisons should be made with caution. Finally, we used self‐reported survey data to explore factors associated to physical restraint use, which might have introduced some bias (e.g., social desirability).
CONCLUSION
In conclusion, despite a low overall prevalence of physical restraint use, a majority of Swiss NH units still currently use restraints on their residents. Our findings do not show a significant relationship between the use of surveillance technologies and physical restraint use. As surveillance technologies are being increasingly used in NHs, its use as an alternative to restraints warrants further investigations. Our findings also show that staff members of units using a lot of restraints perceive that they are using restraints in an inappropriate way. Future research should explore the possibility of using staff opinions as an indicator to target units where physical restraint is routinely overused.
AUTHOR CONTRIBUTIONS
Study concept and design: Lauriane Favez, Michael Simon, Franziska Zúñiga, and Christine Serdaly. Acquisition of data: Lauriane Favez and Franziska Zúñiga. Analysis and interpretation of data: Lauriane Favez, Michael Simon, Franziska Zúñiga, and Michel Bleijlevens. Preparation of Manuscript: all authors.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
SPONSOR'S ROLE
None.
Supporting information
Figure S1 Flowchart of included participants in the sample.
Table S2. Separate unadjusted and adjusted multilevel logistic regression models to identify factors significantly associated with (1) the use of bedrails and (2) the use of trunk fixation or seating options that prevents standing up.
ACKNOWLEDGMENTS
Everyone who contributed significantly to this manuscript's production has been listed. We thank the NHs that participated in this study and Chris Shultis for the English editing of this manuscript. Open access funding provided by Universitat Basel.
Favez L, Simon M, Bleijlevens MHC, Serdaly C, Zúñiga F. Association of surveillance technology and staff opinions with physical restraint use in nursing homes: Cross‐sectional study. J Am Geriatr Soc. 2022;70(8):2298‐2309. doi: 10.1111/jgs.17798
Funding information The Swiss Nursing Home Human Resources Project 2018 (SHURP 2018) study was funded via participation fees paid by the participating nursing homes.
[Correction added on 9 May 2022, after first online publication: Funding statement has been corrected.]
Contributor Information
Lauriane Favez, Email: lauriane.favez@unibas.ch.
Franziska Zúñiga, Email: franziska.zuniga@unibas.ch.
REFERENCES
- 1. Lee D‐CA, Robins LM, Bell JS, et al. Prevalence and variability in use of physical and chemical restraints in residential aged care facilities: a systematic review and meta‐analysis. Int J Nurs Stud. 2021;117:103856. doi: 10.1016/j.ijnurstu.2020.103856 [DOI] [PubMed] [Google Scholar]
- 2. Robins LM, Lee D‐CA, Bell JS, et al. Definition and measurement of physical and chemical restraint in long‐term care: a systematic review. Int J Environ Res Public Health. 2021;18(7):3639. doi: 10.3390/ijerph18073639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bleijlevens MH, Wagner LM, Capezuti E, Hamers JP. International physical restraint W. physical restraints: consensus of a research definition using a modified Delphi technique. J Am Geriatr Soc. 2016;64(11):2307‐2310. doi: 10.1111/jgs.14435 [DOI] [PubMed] [Google Scholar]
- 4. Bellenger EN, Ibrahim JE, Lovell JJ. The nature and extent of physical restraint–related deaths in nursing homes: a systematic review. J Aging Health. 2018;30(7):1042‐1061. doi: 10.1177/0898264317704541 [DOI] [PubMed] [Google Scholar]
- 5. Castle N, Engberg J. The health consequences of using physical restraints in nursing homes. Med Care. 2009;47(11):1164‐1173. [DOI] [PubMed] [Google Scholar]
- 6. Gastmans C, Milisen K. Use of physical restraint in nursing homes: clinical‐ethical considerations. J Med Ethics. 2006;32(3):148‐152. doi: 10.1136/jme.2005.012708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leahy‐Warren P, Varghese V, Day MR, Curtin M. Physical restraint: perceptions of nurse managers, registered nurses and healthcare assistants. Int Nurs Rev. 2018;65:327‐335. doi: 10.1111/inr.12434 [DOI] [PubMed] [Google Scholar]
- 8. Mohler R, Meyer G. Attitudes of nurses towards the use of physical restraints in geriatric care: a systematic review of qualitative and quantitative studies. Int J Nurs Stud. 2014;51(2):274‐288. doi: 10.1016/j.ijnurstu.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 9. Goethals S, Dierckx de Casterle B, Gastmans C. Nurses' decision‐making in cases of physical restraint: a synthesis of qualitative evidence. J Adv Nurs. 2012;68(6):1198‐1210. doi: 10.1111/j.1365-2648.2011.05909.x [DOI] [PubMed] [Google Scholar]
- 10. Ambrosi E, Debiasi M, Longhini J, et al. Variation of the occurrence of physical restraint use in the long‐term care: a scoping review. Int J Environ Res Public Health. 2021;18(22):1‐11. doi: 10.3390/ijerph182211918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heinze C, Dassen T, Grittner U. Use of physical restraints in nursing homes and hospitals and related factors: a cross‐sectional study. J Clin Nurs. 2012;21(7–8):1033‐1040. doi: 10.1111/j.1365-2702.2011.03931.x [DOI] [PubMed] [Google Scholar]
- 12. Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JPH. Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies. J Am Med Dir Assoc. 2014;15(6):383‐393. doi: 10.1016/j.jamda.2013.12.080 [DOI] [PubMed] [Google Scholar]
- 13. Huizing AR, Hamers JP, de Jonge J, Candel M, Berger MP. Organisational determinants of the use of physical restraints: a multilevel approach. Soc Sci Med. 2007;65(5):924‐933. doi: 10.1016/j.socscimed.2007.04.030 [DOI] [PubMed] [Google Scholar]
- 14. Hofmann H, Hahn S. Characteristics of nursing home residents and physical restraint: a systematic literature review. J Clin Nurs. 2014;23(21–22):3012‐3024. doi: 10.1111/jocn.12384 [DOI] [PubMed] [Google Scholar]
- 15. Thomas KS, Hyer K, Castle NG, Branch LG, Andel R, Weech‐Maldonado R. Patient safety culture and the association with safe resident care in nursing homes. Gerontologist. 2012;52(6):802‐811. doi: 10.1093/geront/gns007 [DOI] [PubMed] [Google Scholar]
- 16. Konetzka RT, Brauner DJ, Shega J, Werner RM. The effects of public reporting on physical restraints and antipsychotic use in nursing home residents with severe cognitive impairment. J Am Geriatr Soc. 2014;62(3):454‐461. doi: 10.1111/jgs.12711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fashaw SA, Thomas KS, McCreedy E, Mor V. Thirty‐year trends in nursing home composition and quality since the passage of the Omnibus Reconciliation Act. J Am Med Dir Assoc. 2020;21(2):233‐239, 239. doi: 10.1016/j.jamda.2019.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Niemeijer AR, Frederiks BJM, Riphagen II, Legemaate J, Eefsting JA, Hertogh CMPM. Ethical and practical concerns of surveillance technologies in residential care for people with dementia or intellectual disabilities: an overview of the literature. Int Psychogeriatr. 2010;22(7):1129‐1142. doi: 10.1017/S1041610210000037 [DOI] [PubMed] [Google Scholar]
- 19. Zwijsen SA, Depla MFIA, Niemeijer AR, Francke AL, Hertogh CMPM. Surveillance technology: an alternative to physical restraints? A qualitative study among professionals working in nursing homes for people with dementia. Int J Nurs Stud. 2012;49(2):212‐219. doi: 10.1016/j.ijnurstu.2011.09.002 [DOI] [PubMed] [Google Scholar]
- 20. Te Boekhorst S, Depla MF, Francke AL, Twisk JW, Zwijsen SA, Hertogh CM. Quality of life of nursing‐home residents with dementia subject to surveillance technology versus physical restraints: an explorative study. Int J Geriatr Psychiatry. 2013;28(4):356‐363. doi: 10.1002/gps.3831 [DOI] [PubMed] [Google Scholar]
- 21. Freeman MA. Motion device: an alternative to physical restraints. Geriatr Nurs. 2004;25(3):175. doi: 10.1016/j.gerinurse.2004.04.012 [DOI] [PubMed] [Google Scholar]
- 22. Karlsson S, Bucht G, Eriksson S, Sandman P‐O. Factors relating to the use of physical restraints in geriatric care settings. J Am Geriatr Soc. 2001;49(12):1722‐1728. doi: 10.1046/j.1532-5415.2001.49286.x [DOI] [PubMed] [Google Scholar]
- 23. Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19(Suppl 3):i68‐i74. doi: 10.1136/qshc.2010.042085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Or C, Dohan M, Tan J. Understanding critical barriers to implementing a clinical information system in a nursing home through the lens of a socio‐technical perspective. J Med Syst. 2014;38(9):99. doi: 10.1007/s10916-014-0099-9 [DOI] [PubMed] [Google Scholar]
- 25. Schwendimann R, Zúñiga F, Ausserhofer D, Schubert M, Engberg S, de Geest S. Swiss Nursing Homes Human Resources Project (SHURP): protocol of an observational study. J Adv Nurs. 2014;70(4):915‐926. doi: 10.1111/jan.12253 [DOI] [PubMed] [Google Scholar]
- 26. Favez L, Zúñiga F, Sharma N, Blatter C, Simon M. Assessing nursing homes quality Indicators' between‐provider variability and reliability: a cross‐sectional study using ICCs and Rankability. Int J Environ Res Public Health. 2020;17(24):1‐15. doi: 10.3390/ijerph17249249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Morris JN, Moore T, Jones R, et al. Validation of Long‐Term and Post‐Acute Care Quality Indicators, Final Report. Abt Associates Inc, Brown University; 2003. [Google Scholar]
- 28. Paquay L, De Lepeleire J, Schoenmakers B, Ylieff M, Fontaine O, Buntinx F. Comparison of the diagnostic accuracy of the cognitive performance scale (minimum data set) and the mini‐mental state exam for the detection of cognitive impairment in nursing home residents. Int J Geriatr Psychiatry. 2007;22(4):286‐293. doi: 10.1002/gps.1671 [DOI] [PubMed] [Google Scholar]
- 29. Vettori A, von Stokar T, Petry C, Britt D, Gattinger H, Saxer S. Mindestanforderungen für Pflegebedarfserfassungssysteme (Schlussbericht) [Minimum Requirements for Care Needs Assessment Systems (Final Report)]. Bundesamt für Gesundheit (BAG); 2017. [Google Scholar]
- 30. Zúñiga F, Blatter C, Wicki R, Simon M. Fragebogenerhebung zur Zuverlässigkeit der Daten und Nützlichkeit aus Sicht der Anwender [national quality indicators in Swiss nursing homes: questionnaire survey on data reliability and users' view on the usefulness]. Z Gerontol Geriatr. 2019;52(8):730‐736. doi: 10.1007/s00391-019-01583-7 [DOI] [PubMed] [Google Scholar]
- 31. Bleijlevens MHC, Wagner LM, Capezuti L, Hamers JPH. Maastricht Attitude Questionnaire, English Version. Maastricht University; 2012. [Google Scholar]
- 32. van Dishoeck AM, Lingsma HF, Mackenbach JP, Steyerberg EW. Random variation and rankability of hospitals using outcome indicators. BMJ Qual Saf. 2011;20(10):869‐874. doi: 10.1136/bmjqs.2010.048058 [DOI] [PubMed] [Google Scholar]
- 33. Andrade C. Mean difference, standardized mean difference (SMD), and their use in meta‐analysis: as simple as it gets. J Clin Psychiatry. 2020;81(5):e1‐e4. doi: 10.4088/JCP.20f13681 [DOI] [PubMed] [Google Scholar]
- 34. Stoffel MA, Nakagawa S, Schielzeth H, Goslee S. rptR: repeatability estimation and variance decomposition by generalized linear mixed‐effects models. Methods Ecol Evol. 2017;8(11):1639‐1644. doi: 10.1111/2041-210x.12797 [DOI] [Google Scholar]
- 35. Bates D, Maechler M, Bolker B, Walker S. Fitting linear mixed‐effects models using lme4. J Stat Softw. 2015;67:1‐48. doi: 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- 36. Wickham H. ggplot2: Elegant Graphics for Data Analysis. Springer‐Verlag; 2016. [Google Scholar]
- 37. Meyer G, Kopke S, Haastert B, Muhlhauser I. Restraint use among nursing home residents: cross‐sectional study and prospective cohort study. J Clin Nurs. 2009;18(7):981‐990. doi: 10.1111/j.1365-2702.2008.02460.x [DOI] [PubMed] [Google Scholar]
- 38. Estevez‐Guerra GJ, Farina‐Lopez E, Nunez‐Gonzalez E, Gandoy‐Crego M, Calvo‐Frances F, Capezuti EA. The use of physical restraints in long‐term care in Spain: a multi‐center cross‐sectional study. BMC Geriatr. 2017;17(1):29. doi: 10.1186/s12877-017-0421-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gordon SE, Dufour AB, Monti SM, et al. Impact of a videoconference educational intervention on physical restraint and antipsychotic use in nursing homes: results from the ECHO‐AGE pilot study. J Am Med Dir Assoc. 2016;17(6):553‐556. doi: 10.1016/j.jamda.2016.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Decker FH, Castle NG. Relationship of the job tenure of nursing home top management to the prevalence of pressure ulcers, pain, and physical restraint use. J Appl Gerontol. 2011;30(5):539‐561. doi: 10.1177/0733464810375801 [DOI] [Google Scholar]
- 41. Feng Z, Hirdes JP, Smith TF, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross‐national study. Int J Geriatr Psychiatry. 2009;24(10):1110‐1118. doi: 10.1002/gps.2232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hamers JP, Meyer G, Köpke S, Lindenmann R, Groven R, Huizing AR. Attitudes of Dutch, German and Swiss nursing staff towards physical restraint use in nursing home residents, a cross‐sectional study. Int J Nurs Stud. 2009;46(2):248‐255. doi: 10.1016/j.ijnurstu.2008.06.007 [DOI] [PubMed] [Google Scholar]
- 43. Flaherty JH. Zero tolerance for physical restraints: difficult but not impossible. J Gerontol A Biol Sci Med Sci. 2004;59(9):919‐920. doi: 10.1093/gerona/59.9.m919 [DOI] [PubMed] [Google Scholar]
- 44. Carlesso J. Bill permitting use of cameras in nursing homes wins final passage. Connectitcut Mirror. 2021;3(6):2021. [Google Scholar]
- 45. Haut A, Kolbe N, Strupeit S, Mayer H, Meyer G. Attitudes of relatives of nursing home residents toward physical restraints. J Nurs Scholarsh. 2010;42(4):448‐456. doi: 10.1111/j.1547-5069.2010.01341.x [DOI] [PubMed] [Google Scholar]
- 46. Mayerl H, Trummer T, Stolz E, Rasky E, Freidl W. Nursing professionals' attitudes toward use of physical restraints in Styrian nursing homes Austria. Pflege. 2019;32(1):57‐63. doi: 10.1024/1012-5302/a000649 [DOI] [PubMed] [Google Scholar]
- 47. Ferrão SADS, Bleijlevens MHC, Nogueira PJ, Henriques MAP. A cross‐sectional study on nurses' attitudes towards physical restraints use in nursing homes in Portugal. Nurs Open. 2021;8(4):1571‐1577. doi: 10.1002/nop2.769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Myers H, Nikoletti S, Hill A. Nurses' use of restraints and their attitudes toward restraint use and the elderly in an acute care setting. Nurs Health Sci. 2001;3(1):29‐34. doi: 10.1046/j.1442-2018.2001.00068.x [DOI] [PubMed] [Google Scholar]
- 49. Karlsson S, Bucht G, Sandman PO. Physical restraints in geriatric care. Knowledge, attitudes and use. Scand J Caring Sci. 1998;12(1):48‐56. [PubMed] [Google Scholar]
- 50. CURAVIVA . Droit de la protection de l'adulte & mesures restreignant la liberté de mouvement [Adult protection law & measures restricting freedom of movement]. Date accessed: 21.09.2021. Available from: https://www.curaviva.ch/Infos‐specialisees/Dossiers‐thematiques/Droit‐de‐la‐protection‐de‐ladulte‐mesures‐restreignant‐la‐liberte‐de‐mouvement/PZUX3/?lang=fr.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Flowchart of included participants in the sample.
Table S2. Separate unadjusted and adjusted multilevel logistic regression models to identify factors significantly associated with (1) the use of bedrails and (2) the use of trunk fixation or seating options that prevents standing up.


