Abstract
Introduction
The electronic dental model (e‐model) is an example of a digital 3‐dimensional technology to support inquiry‐based learning in undergraduate dental education. As student perceptions of and engagement with e‐models vary, it is uncertain whether these perceptions have implications for their learning processes and outcomes.
Materials and Methods
Third‐year dental students (N = 40) completed a questionnaire to identify their perceptions of and preferences for model modalities. They were divided into three groups based on their preference: Preferring plaster models (Group 1); Preferring e‐models (Group 2); No preference (Group 3). Students from three groups (N = 9) attended a hands‐on digital occlusion evaluation workshop, and then completed a case‐based diagnostic evaluation test using digital occlusion evaluation software. Camtasia Studio™ recorded real‐time and on‐screen data of the number of mouse‐clicks and time spent.
Results
Students reported positive feedbacks on the use of e‐models, and 72.5% of the students preferred combination use of e‐models and plaster models. After attending the hands‐on digital dental occlusion evaluation workshop, Group 2 scored higher on the diagnostic evaluation test (p < .05) and registered more mouse‐clicks than Group 1 when evaluating the arch symmetry (p < .05). Group 2 registered fewer mouse‐clicks than Group 3 during tooth size measurement (p < .05). There was no significant difference regarding the time used to answer the knowledge questions amongst the three groups.
Conclusion
Undergraduate dental students indicated a generally high acceptance of e‐models for their learning in orthodontics, and more prefer a blended approach. Students preferring e‐models presented higher performance outcomes, which supports cognitive load theory regarding prior exposure to simulation‐based environments.
Keywords: blended learning, case‐based learning, E‐learning, electronic dental models, orthodontic education, simulation
1. INTRODUCTION
The advancement of information technology in recent years has created opportunities to implement blended learning experiences in higher education. A “hybrid campus” model was suggested by Bleed 1 to incorporate the creative use of technology, architecture and people, through a combination of physical and virtual instruction. The integration of physical, face‐to‐face approaches and virtual online technologies aims to promote active, self‐directed learning opportunities for students with added flexibility. 2
Electronic 3‐D technology has been in extensive use in education across a range of disciplines such as physics, 3 medicine 4 and engineering. 5 In dental education, virtual reality simulators with haptic feedback were introduced in the 2000s as a 3‐D alternative to the traditional phantom head simulators. 6 , 7 , 8 More recently, 3‐D digital patient records, such as electronic dental study models (e‐models), have been introduced to undergraduate curricula as an innovative resource to support deep engagement in inquiry‐based learning processes in both problem‐based learning (PBL) and case‐based learning (CBL). 9 , 10 However, more research in this emerging field is needed so as to understand learning processes with 3‐D simulations. 11
In clinical practice, information technology has also shifted modern medicine and dentistry into an era of electronic patient records. The Institute of Medicine (IOM) of the United States has urged “a renewed national commitment to building an information infrastructure to support health care delivery, consumer health, quality measurement and improvement, public accountability, clinical and health services research, and clinical education”. 12 , 13 The IOM aims to replace handwritten clinical data by electronic records by the end of this decade. Electronic records are thought to be superior to paper/solid records for many reasons such as decreased handwriting errors and easy physical storage. 14 In the dental field, 2‐D digital radiographs and photos have been successfully integrated into record keeping in clinical dentistry. However, dental models, which are a type of unique but important 3‐D record in dentistry, are amongst the last type of record to be digitally converted in the dental field. 15 Dental models are an essential clinical record in orthodontic treatments. The American Association of Orthodontists regarded dental models as one of the recommended basic orthodontic records in the Clinical Practice Guidelines for Orthodontics and Dentofacial Orthopedics. 16 Dental models alone provide the critical information necessary for orthodontic treatment planning. 17 Joffe 18 noted an increasing popularity of e‐models in clinical education worldwide and predicted that e‐models would become the norm for dental models in the future. Studies had verified that the accuracy of e‐models is compatible to traditional plaster ones in terms of linear measurements, intra‐ and inter‐arch relationship. 19
In view of the various potentials and importance of e‐models in dental education and clinical dental practice, dental students should be equipped with the ability to utilise e‐models during their undergraduate studies. According to the technology acceptance model and its extensions such as unified theory of acceptance and use of technology (UTAUT), factors including performance expectancy, effort expectancy, social influence and facilitating conditions are all critical determinants of user adoption intention or behaviors. 20 A recent survey indicated that positive student perceptions towards e‐models may lead to improvement in learning motivation. 9 , 21 Despite their positive perceptions towards e‐models, their cognition in relationship to achievement of learning outcomes remains uncertain.
Hence, the aim of this study is first to further identify dental students' perceptions of e‐models and their preferences amongst model modalities, and besides, to investigate students' learning performance and achievement using e‐models as well as the effects of students' perceptions towards e‐models on their learning outcomes.
2. METHODS
The study was approved by the Institutional Review Board, Hong Kong West Cluster (UW 12–098). It adopted a mixed method approach with a pre‐workshop questionnaire and post‐workshop focus group discussion providing student perception data and an experimental design examining student learning processes and outcomes.
2.1. Pre‐workshop questionnaire
Forty third‐year dental students (BDS III) who have had 1 year's experience in using e‐models (O3DM, Aarhus C, Denmark) were invited to complete a self‐administered questionnaire to evaluate their perceptions of using dental e‐models for learning orthodontic diagnostic skills. 19 Student preferences regarding dental model modalities were also examined.
The 23‐item questionnaire was, therefore, structured to collect information on the following aspects of students' perception of e‐models (see Appendix 1):
Characteristics of e‐models;
Usefulness of e‐models in PBL and CBL tutorials;
Past utilization experience of e‐models in PBL and CBL tutorials;
e‐models as a resource to introduce students to electronic patient records;
Willingness to use e‐models in future PBL and CBL curricula;
Preference of model modalities.
Questions from category 1 to category 5 were rated in a 5‐point Likert scale (1 as strongly disagree; 5 as strongly agree). For the last category, students stated if traditional plaster models, e‐models or both were their dental study models of choice.
2.2. Hands‐on occlusion evaluation workshop
Based on the questionnaire results, students were divided into three groups according to their preference: Group 1 (preferring traditional plaster models); Group 2 (preferring e‐models); Group 3 (no preference of either type). Since only three students indicated a preference for e‐models (Group 2), all three were invited to participate in a hands‐on occlusion evaluation workshop. The same number of students in Groups 1 and 3 were randomly selected to participate in the workshop. Thus, a total number of nine students, three from each group, participated in a hands‐on, case‐based, occlusion (dental bite) evaluation workshop facilitated by a full‐time academic staff in orthodontics to teach the students about the use of e‐models. The contents taught in the workshop were brand new for all the students. Students were instructed to use the O3DM software in their own personal computers to manipulate the e‐models and perform various measurements while completing six diagnostic evaluation questions related to the occlusion of the e‐models at the end of the workshop to evaluate their performance. The performance in the hands‐on occlusion evaluation workshop was assessed aiming to test the students' orthodontic diagnostic ability and their skills in manipulating the e‐models. The diagnostic test contained six questions related to orthodontic evaluation (see Appendix 2):
Sagittal relationship
Transverse relationship
Vertical relationship
Arch symmetry
Tooth number and alignment
Tooth size measurement
The model answers were documented in a written format by the full‐time academic staff in orthodontics based on both solid and e‐models (same answers were drawn from the solid and e‐models). The orthodontic diagnostic evaluation test was marked by this full‐time academic staff and checked by a second marker afterwards. Inter‐rater agreement was 100%.
Camtasia Studio™ was pre‐installed in the students' personal computers to record their on‐screen activities and real‐time learning processes while applying the O3DM e‐model software to complete the orthodontic diagnostic evaluation test at the end of the workshop. Camtasia Studio™ was designed to create screencasts, that is digital recordings of computer screen output, which could be integrated with audio or other multimedia recordings. It consists of two components: 1) Camtasia Studio Recorder for capturing screen videos and audios; 2) Camtasia Studio Editor for editing the videos and audios in a timeline interface. Camtasia Studio Recorder logged all screen movements and actions and created a video clip for post‐workshop review by the researchers. The Camtasia Studio Editor allowed the video clip to be displayed as tracks by using the timeline interface with an integrated preview window. The number of mouse‐clicks and the time used to answer each of the six questions were counted from tracks of the timeline interface as a means of gauging functional interaction with the software.
2.3. Post‐workshop focus group discussion
After the workshop, all the nine BDSIII students were invited to join a focus group discussion with the full‐time academic staff in orthodontics. Using a basic SWOT analysis structure, they were invited to share their feedback on:
Their general impressions of using e‐models;
The pros and cons of e‐models as an e‐learning resource for inquiry‐based learning;
The potential utility of electronic patient records in dentistry.
The discussions were videotaped and transcribed.
2.4. Analysis
Statistical data retrieved from the questionnaires, the scores on the orthodontic diagnostic evaluation test and the on‐screen activities in the workshop were analysed using SPSS 19.0. Descriptive analysis was performed on the different aspects of students' perception on e‐models mentioned above. Inferential analysis with analysis of variance (ANOVA) tests was performed to evaluate the association between students' preference for e‐models and the scores of the orthodontic diagnostic evaluation test and on‐screen activities in the hands‐on occlusion evaluation workshop. Focus group transcripts were analysed according to the interview schema and the four priori elements of SWOT analysis. 22
3. RESULTS
3.1. Pre‐workshop student perceptions (Table 1)
Forty of fifty‐four third‐year dental students of HKU completed the pre‐workshop questionnaire (5‐point Likert scale), with a 74% response rate Table 1. The mean score for questions relating to the characteristics of e‐models was 3.58 and ≥95% of students were neutral, agreed or strongly agreed with the questions. The mean score for questions relating to the usefulness of e‐models in PBL and CBL tutorials was 3.24 and at least 87.5% of students were neutral, agreed or strongly agreed. Ninety‐five per cent of students were neutral, agreed or strongly agreed that introduction of e‐models into BDS curriculum is useful preparation for the era of the “electronic patient record” and the mean score of this question was 3.43. The mean score for questions relating to the willingness to use e‐models in future problem‐ and case‐based learning was 3.36 and >97.5% of students were neutral, agreed or strongly agreed. In terms of prior experience with e‐models, students reported limited exposure with a mean score of 2.65 and only 60% of students were neutral, agreed or strongly agreed. Overall, the results indicated that students were generally positively disposed towards e‐models in terms of their learning and future clinical practice but had had limited exposure to date.
TABLE 1.
Mean scores and standard deviations of individual items in the pre‐workshop questionnaire
| Items | Mean scores (Standard deviation) |
|---|---|
| 1) Characteristics of e‐models | |
| The e‐models are interesting. | 3.50 (0.55) |
| The e‐models are user‐friendly. | 3.38 (0.59) |
| The e‐models show teeth and adjacent structures clearly. | 3.65 (0.66) |
| The e‐models can be rotated and moved easily. | 3.68 (0.62) |
| Measurement can be easily done on e‐models. | 3.70 (0.61) |
| 2) Usefulness of e‐models in PBL and CBL tutorials | |
| Introduction of e‐models into PBL will make/makes PBL more interactive and interesting. | 3.18 (0.68) |
| Introduction of e‐models into CBL makes CBL more interactive and interesting. | 3.13 (0.61) |
| E‐models are useful in PBL tutorial 1. | 3.23 (0.70) |
| E‐models are useful in PBL self‐learning. | 3.43 (0.64) |
| E‐models are useful in PBL tutorial 2. | 3.3 (0.69) |
| E‐models are useful for the group to share the models together during PBL and CBL group discussion. | 3.25 (0.67) |
| E‐models are useful for me to go over the PBL and CBL problems after tutorials. | 3.18 (0.68) |
| 3) The actual utilization of e‐models in PBL and CBL tutorials | |
| I used e‐models in PBL. | 2.60 (0.59) |
| I used e‐models in PBL tutorial 1. | 2.60 (0.55) |
| I used e‐models in PBL self‐learning. | 2.68 (0.62) |
| I used e‐models in PBL tutorial 2. | 2.68 (0.62) |
| I used e‐models in CBL. | 2.68 (0.57) |
| I used e‐models during PBL and CBL group discussion. | 2.68 (0.57) |
| I used e‐models to go over the PBL and CBL problems after tutorials. | 2.68 (0.53) |
| 4) e‐models as a resource to introduce students to electronic patient record | |
| Introduction of e‐models into BDS curriculum is useful for me to approach the era of patient record. | 3.43 (0.68) |
| 5) Willingness to use e‐models in future PBL and CBL curricula | |
| I will use e‐models in future PBL curriculum. | 3.35 (0.53) |
| I will use e‐models in future CBL curriculum. | 3.38 (0.54) |
For students' preference of the types of e‐models, 20% (n = 8, Group 1) preferred traditional plaster models, 7.5% (n = 3, Group 2) preferred e‐models and 72.5% (n = 29, Group 3) had no preference. The same numbers of students from the above three groups were invited to join the e‐model workshop. Since only three students indicated a clear preference for e‐models (Group 2), all the three were invited to participate in the hands‐on occlusion evaluation workshop. The same number of students in each of the other two groups (Groups 1 and 3) were randomly selected to participate in the workshop.
3.2. Results of the orthodontic diagnostic evaluation test and analysis of on‐screen activities
For the overall scores on the orthodontic diagnostic evaluation test, Group 2 (e‐models) achieved the highest mean score (17.67 ± 0.577), and was higher than that of Group 3 (no preference) (15.67 ± 0.577) with statistical significance (p < .05) (Figure 1). Group 2 registered the highest number of mouse‐clicks while evaluating the arch symmetry of e‐models (16.33 ± 1.528), and this was significantly more than that of Group 1 (plaster models) (9.33 ± 0.577) (p < .05) indicating that Group 2 had more utilization of the digital grid in evaluating the arch symmetry of the e‐models. Group 2 registered the lowest number of mouse‐clicks in measuring tooth size on e‐models (16.67 ± 3.512), which was significantly less than that of Group 3 (29 ± 2.646) (p < .05) (Figure 2). However, there was no statistically significant difference regarding the time spent on answering the questions in the orthodontic diagnostic evaluation test amongst the three groups (Figure 3).
FIGURE 1.
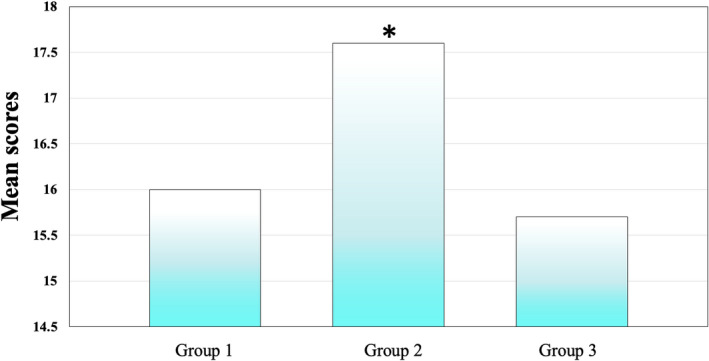
Overall scores on orthodontic diagnostic evaluation test in three groups (*p < .05) [Colour figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
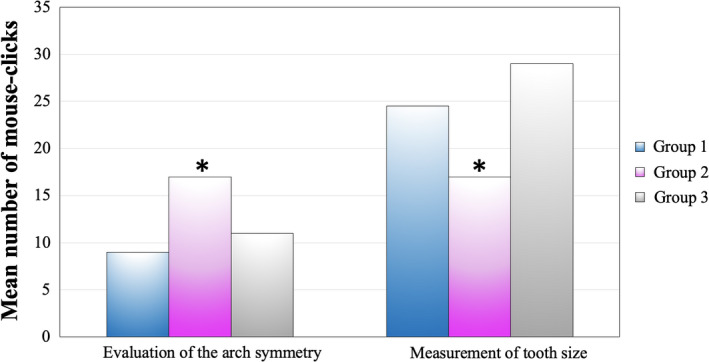
The number of mouse‐clicks of the 3 groups during the evaluation of arch symmetry and tooth size (*p < .05) [Colour figure can be viewed at wileyonlinelibrary.com]
FIGURE 3.
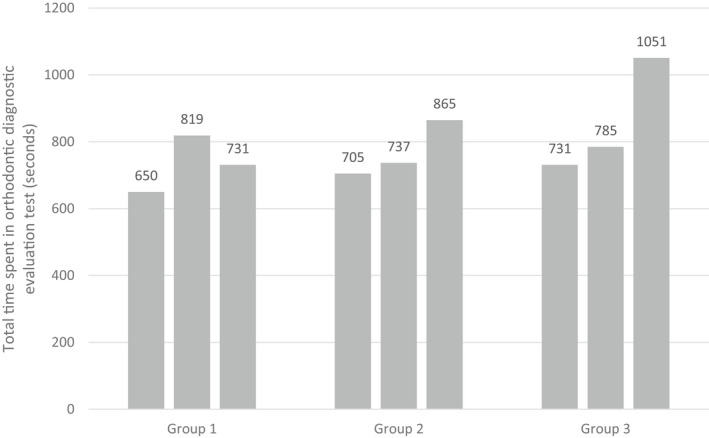
The total time spent in answering the questions in the orthodontic diagnostic evaluation test for each student in three groups
3.3. Focus group discussion feedback
The participants shared their feedback on the learning experience with the 3‐D simulations in case‐based workshop. They were also asked to give their opinions on the strength and weakness of e‐models, and on the future of e‐models as an essential electronic patient record in dentistry. Generally, for the experience of using e‐models, Group 1 (preferring plaster models) did not express much opinion on this, while Group 2 (preferring e‐models) reported enjoying using e‐models with descriptions of “convenient for measurement” and “ease of use.” Group 3 (no preference) members reflected that they had some difficulties in using the virtual platform, including “not easy to manipulate” and “more time consuming to get used to the software,” but felt that the workshop was useful for learning the techniques. Regarding the SWOT analysis, all three groups identified different aspects of strength for e‐models regarding convenience, accuracy and ease of operation. Group 2 (preferring e‐models) did not report any weaknesses on e‐models, and no student in Group 1 (preferring plaster models) described aspects of opportunity. Although all groups had some concerns as to the potential threats of e‐models, their concerns differed. Group 1 (preferring plaster models) and Group 2 (preferring e‐models) were focused on security issues, while Group 3 (no preference) thought the labour‐intensive scanning would be the major problem. The students' focus group discussion feedback is summarised in Tables 2 and 3.
TABLE 2.
Post‐workshop feedback from the focus group discussion on students' experience in using e‐models
| Comments | Groups a |
|---|---|
| No specific comments on this point | Group 1 |
| Convenient for measurement | Group 2 |
| Ease of use (technical) | |
| Not easy to manipulate the e‐model (e.g. rotation) | Group 3 |
| More time‐consuming to get used to the software | |
| Workshop is useful for learning the e‐model software |
(Group 1) plaster model preference; (Group 2) e‐model preference; (Group 3) no preference.
TABLE 3.
The group conclusion on the strengths, weaknesses, opportunities and treats of e‐models
| Groupsa | Comments | |
|---|---|---|
| Group 1 | Better accuracy than manual measurement | Strengths |
| More accessible during PBL sessions | ||
| Easy to store | ||
| Cannot modify the e‐model (do build‐up or trimming, diagnostic wax‐up) | Weaknesses | |
| Privacy concerns regarding data security of patient's electronic records | Treats | |
| Group 2 | Convenient for measurement | Strengths |
| Easy to use | ||
| E‐models can be replicated easily | Opportunities | |
| Convenient for communication between colleagues | ||
| Privacy concerns regarding data security of patient's electronic records | Treats | |
| Group 3 | Workshop is useful for learning the e‐model software | Strengths |
| Data would not be distorted | ||
| Cannot be mounted on articulators | Weaknesses | |
| Time‐consuming to gain expertise in the software | ||
| Not easy to manipulate the e‐model (e.g. rotation) | ||
| Could not be used as working models for prosthodontics | ||
| As a supplement to plaster models when learning orthodontic principles | Opportunities | |
| Simple clinical record keeping | ||
| Labour‐intensive scanning of the stone dental models into electronic ones | Treats |
(Group 1) plaster model preference; (Group 2) e‐model preference; (Group 3) no preference.
4. DISCUSSION
4.1. Learning in simulated environments
In this study, the mean scores of the questions relating to 1) the characteristics of e‐models; 2) the usefulness of e‐models in PBL and CBL tutorials; 3) e‐models as a resource to introduce students to electronic patient record and 4) willingness to use e‐models in future PBL and CBL curriculums are all greater than 3, with more than 87.5% of students indicated neutral, agreed or strongly agreed. This reflects that the BDS III students were generally positively disposed towards simulations using e‐models for their learning. Most of them appreciated the different characteristics of e‐models, and agreed that e‐models were useful tools in PBL/CBL tutorials as well as helping to introduce them to electronic patient records. They were positively disposed to using e‐models for learning in PBL/CBL tutorials in the future. The acceptance of an e‐learning resource by students is essential in the successful implementation of blended learning approach in the inquiry‐based learning. 23 It also sets a baseline from which the change of students' perception of e‐models over time and experience can be evaluated.
The 40 surveyed third‐year students (in a 6‐year undergraduate programme) indicated limited prior exposure to e‐models (mean score is 2.65 ± 0.58) and the majority (72.5%) preferred to use both plaster models and e‐models as dental study models. This may reflect that the students were in a transitional stage between solid and electronic dental study models as learning resources and they regarded both types of dental study models as useful for them in learning. The positive response from the workshop participants indicates potential future acceptance. 23 This also supports a blended learning approach in dentistry, which combines traditional clinical records (e.g. plaster models) with virtual records (e.g. e‐models). Use of plaster models is particularly important in such an operative discipline as dentistry requiring the acquisition of haptic sensibility in order to treat real‐life patients. 6 , 7 , 8
4.2. Learning outcomes and early adopters
To objectively assess students' ability to learn with a new e‐learning resource, that is e‐models in our study, an evaluation task was used to assess students' ability to manipulate e‐models and extract useful information from them. Since the dental students might have different levels of dental/orthodontic knowledge prior to the study which might affect the results, the instructor explained the meaning of each question and provided the necessary orthodontic knowledge to the students before asking them to complete the orthodontic diagnostic evaluation test. The students were also given unlimited time to complete each of the questions and amend the answers, in order to minimise errors due to time constrains. We believe that the results and scores of the test could reflect the learning outcomes of students using e‐models software for diagnostic occlusal evaluation. The higher overall scores achieved by students preferring e‐models (Group 2) suggested that students who have more positive perception of e‐models showed better cognition.
Amongst the six questions in the orthodontic diagnostic evaluation test, questions 1–3 asked for the classification of malocclusion of the e‐models from different views. This required rotation and movement of the e‐models in the software, which were relatively simple and easy to perform. However, to assess the arch symmetry, one had to utilise the digital grid function, which was a build‐in tool hidden in the menu bar of the e‐model software. By superimposing the digital grid with the occlusal surface of the e‐models, arch symmetry could be better evaluated. The software allowed the manipulation of the grid orientation, and the scale of the grid could be changed as needed. The students needed to click a number of buttons so as to activate the digital grid and position it appropriately to help analyse the arch symmetry of the e‐models. With better computer self‐efficacy and skills, one could better utilise the digital grid as an adjunct to arch symmetry analysis.
On the contrary, to measure individual tooth size from the e‐model, the digital ruler function had to be employed. It was also a built‐in tool hidden in the menu bar of the e‐model software. The user defined two points by manipulating the two ends of the digital ruler; then the distance between the two points would be automatically calculated. With better computer self‐efficacy and skills, one could accomplish the task with just a few numbers of mouse‐click. With similar time spent in answering the questions in the orthodontic diagnostic evaluation test, Group 2 students manipulated the e‐models more skilfully by utilising more of the digital assistant tool and employing fewer mouse‐clicks to measure tooth size.
Cognitive load theory was proposed based on assumptions regarding the characteristics of human cognitive architecture with primary knowledge and evolutionary secondary knowledge composed. 24 In the context of 3D orthodontic learning, information or instructional activity, that is digital occlusion evaluation workshop, is crucial in the learning outcome, but it also dependent on the intrinsic cognitive load of electronic formats. 25 For those unfamiliar with digital simulations, the interface may have been a distracting factor limiting their ability to apply the principles. Another explanation is ascribable to interactions between motivation and cognition that are emergent amongst processes of knowing, learning and emotions. 26 Student preferring plaster models (Group 1) and with no preference (Group 3) may not be as engaged and motivated as those in Group 2 for completion of the orthodontic diagnostic evaluation test, which then possibly reflected on the their learning performance.
The findings were also supported by students' feedback in the post‐workshop group discussion. Students preferring e‐models (Group 2) perceived that the e‐model software was convenient for the measurement of tooth size. On the contrary, students with no preference (Group 3) perceived that it was difficult to manipulate the e‐model software and it was time‐consuming to get used to the software. However, they thought that the hands‐on occlusion evaluation workshop was useful for them to learn the e‐model software. The performance in the cognition test and the students' feedback in the group discussion suggested that students who have more positive perception on e‐models have better functionality in using e‐models.
In a blended e‐learning system, learning satisfaction depends on factors such as computer self‐efficacy, performance expectations, system functionality and content feature. 27 Our study shows that students preferring e‐models performed better in evaluation test, had better computer self‐efficacy and skills, better functionality in using e‐models, and they thought that the e‐model software was easy to use. The level of digital literacy or digital competence of individual dental students might contribute to their preference to e‐models. A recent European Commission report 28 defined five core areas of digital competence as:
“1. Information: identify, locate, retrieve, store, organise and analyse digital information, judging its relevance and purpose.
2. Communication: communicate in digital environments, share resources through online tools, link with others and collaborate through digital tools, interact with and participate in communities and networks, cross‐cultural awareness;
3. Content‐creation: Create and edit new content (from word processing to images and video); integrate and re‐elaborate previous knowledge and content; produce creative expressions, media outputs and programming; deal with and apply intellectual property rights and licences;
4. Safety: personal protection, data protection, digital identity protection, security measures, safe and sustainable use.
5. Problem‐solving: identify digital needs and resources, make informed decisions as to which are the most appropriate digital tools according to the purpose or need, solve conceptual problems through digital means, creatively use technologies, solve technical problems, update one's own and others' competences.”
It may be the case that students with high levels of digital competence have better skills and confidence in manipulating the e‐model software, and hence tended to prefer e‐models to traditional plaster counterparts. However, the digital competence of the dental students against established frameworks was not investigated. Although university students may be familiar with information technologies such as web surfing and social networking in their daily lives, it does not mean that have a high level of digital competence, especially in navigating and manipulating new, sophisticated computer software for analysis of simulated 3‐D objects such as in this study. Further investigations may be required into the relationship between extraneous cognitive load, digital competence and students' perceptions towards, processes with and learning outcomes from the incorporation of simulations in dental curricula.
4.3. Methodological implications
In this study, screen‐recording software, Camtasia Studio™, was used to collect data on students' on‐screen behaviour during the e‐model workshop by logging the number of mouse‐clicks and the time spent in answering each question in the orthodontic diagnostic evaluation test. Similar methodology has been used in the investigation of human cognition in other disciplines. 29 , 30 , 31 , 32 The screen‐recording software provides access to the real‐time learning process of an individual. Researchers can trace the user's activity by studying the recordings and logging the parameters for describing the user's behaviour (such as mouse‐clicks and time). One major deficiency identified with this method was that the interpretation of the performances in the orthodontic diagnostic evaluation test associated with the on‐screen activities of an individual was largely based on the researcher's speculation. 32 This might not directly reflect the individual's own perceptions; hence, there was no direct relationship between the on‐screen activities and the individual's cognitive processes, as the analysis of these data relies on researchers' interpretation. 29 By combining the screen‐recording software with a post‐workshop group discussion, which collected the retrospective feedbacks of the learning experience from the students, participants could share their own personal opinions and perceptions of the learning experience, and explaining the rationale behind their on‐screen actions recorded by the screen‐recording software. The post‐workshop group discussion provided Supplementary information which helped connect the participants' on‐screen activities to their own perceptions, thus reflecting their cognition in manipulating e‐models in the workshop.
As demonstrated in this study, screen‐recording software is an innovative research tool in examining student learning from simulations in dental education. The on‐screen navigations and manipulations and the timing of these in relation to learning tasks as captured by the screen‐recording software provide invaluable information about the subjects' cognitive process.
4.4. Limitations
In our study, the sample size for the experimental phase was relatively small (n = 9) as only 3 amongst the whole class (n = 40) indicated preference for e‐models (Group 2) and, according to standard experimental study designs, 33 the two other groups (Groups 1 and 3) needed to have the same numbers of participants. Despite this, the novel application of screen recording software (Camtasia Studio™) generated a rich dataset. We hope this may inform new directions in future studies in e‐learning in dental education. As noted in the discussion above, the level of digital competence of the dental students was not assessed and this may be an area worthy of future research.
5. CONCLUSION
Dental students were generally accepting of 3‐Dimensional simulations in the form of e‐models and evaluation software; however, the majority indicated a preference for learning from both traditional solid and e‐models for case‐based learning in orthodontics. This supports the application of a blended approach in dentistry, which requires engagement with multiple modalities for the acquisition of haptic sensibility and development of critical analysis in order to treat real‐life patients.
Students' preference of e‐models may be associated with better skills in manipulating and analysing the orthodontic features of e‐models. More direct instruction on technical skills and platform navigation could enhance motivation when using 3‐D virtual tools. Overall, the study reinforces the role of attitude in students' adoption of new modalities in dental education.
CONFLICT OF INTEREST
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us. We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
ACKNOWLEDGEMENTS
We would like to thank O3DM for its support in this project by providing free use of the software for teaching purposes. The project was supported by a Teaching Development Grant of the University of Hong Kong.
APPENDIX 1.
Pre‐workshop questionnaire.
| Categories | Question items |
|---|---|
| Characteristics of e‐models |
1. The e‐models are interesting. 2. The e‐models are user‐friendly. 3. The e‐models show teeth and adjacent structures clearly. 4. The e‐models can be rotated and moved easily. 5. Measurement can be easily done on e‐models. |
| Use of e‐models in PBL and CBL |
6. Introduction of e‐models into PBL will make/makes PBL more interactive and interesting. 7. E‐models are useful in PBL tutorial 1. 8. E‐models are useful in PBL self‐learning. 9. E‐models are useful in PBL tutorial 2. 10. I used e‐models in PBL. 11. I used e‐models in PBL tutorial 1. 12. I used e‐models in PBL self‐learning. 13. I used e‐models in PBL tutorial 2. 14. Introduction of e‐models into CBL makes CBL more interactive and interesting. 15. I used e‐models in CBL. 16. E‐models are useful for the group to share the models together during PBL and CBL group discussion. 17. I used e‐models during PBL and CBL group discussion. 18. E‐models are useful for me to go over the PBL and CBL problems after tutorials. 19. I used e‐models to go over the PBL and CBL problems after tutorials. 20. Introduction of e‐models into BDS curriculum is useful for me to approach the era of ‘electronic patient record’. 21. I will use e‐models in future PBL curriculum. 22. I will use e‐models in future CBL curriculum. |
| Preference of the type of models | 23. Preference of study cast is traditional plaster models, e‐models or both. |
APPENDIX 2.
Orthodontic diagnostic evaluation test of the hands‐on occlusion evaluation workshop.
Task 1: sagittal relationship
| Molar relationship: | ||||
| Right side: | Class I | Class II | Class III | |
| Left side: | Class I | Class II | Class III | |
| Canine relationship: | ||||
| Right side: | Class I | Class II | Class III | Unclassified |
| Left side: | Class I | Class II | Class III | Unclassified |
| Incisor relationship: | ||||
| Class I | Class II1 | Class II2 | Class III | |
| Overjet: | ||||
| Negative | Reduced | Normal | Increased | |
Task 2: vertical relationship
| Overbite: | |||||
| Openbite | Shallow | Normal | Deep | Complete | Incomplete |
Task 3: transverse relationship
| Midline | ||
| Coincide | Not coincide | |
| Posterior overjet: | ||
| Right side: | ||
| Normal | Buccal crossbite | Lingual crossbite (scissorbite) |
| Left side: | ||
| Normal | Buccal crossbite | Lingual crossbite (scissorbite) |
Task 4: arch
| Arch symmetry | ||
| Upper arch: | Symmetric | Asymmetric |
| Lower arch: | Symmetric | Asymmetric |
Task 5: tooth number and alignment
Clinical missing teeth.
| 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Upper arch: | |
| Spacing | Crowding |
| Lower arch: | |
| Spacing | Crowding |
Task 6: tooth size
Ho ACH, Liao C, Lu J, et al. 3‐Dimensional simulations and student learning in orthodontic education. Eur J Dent Educ. 2022;26:435–445. doi: 10.1111/eje.12718
The department and institution to which the work should be attributed: Faculty of Dentistry, The University of Hong Kong, Hong Kong, China
Contributor Information
Susan M. Bridges, Email: sbridges@hku.hk.
Yanqi Yang, Email: yangyanq@hku.hk.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analysed during the current study are not publicly available due to ethical issues but are available from the corresponding author on reasonable request.
REFERENCES
- 1. Bleed R. A hybrid campus for the new millennium. EDUCAUSE Rev. 2001;36(1):16‐22. [Google Scholar]
- 2. Garnham C, Kaleta R. Introduction to hybrid courses. Teach Technol Today. 2002;8(6).5. [Google Scholar]
- 3. Smithenry DW. Teaching with crystal structures: helping students recognize and classify the smallest repeating particle in a given substance. Sci Teach. 2009;76(6):52. [Google Scholar]
- 4. Jang S. From Vesalius to Virtual Reality: How Embodied Cognition Facilitates the Visualization of Anatomy. ProQuest LLC; 2010. [Google Scholar]
- 5. Krueger TJ, Barr RE. The concurrent engineering design paradigm is now fully functional for graphics education. Eng Des Graph J. 2009;71(1).22–28. [Google Scholar]
- 6. Perry S, Bridges SM, Burrow MF. A review of the use of simulation in dental education. Simul Healthc. 2015;10(1):31‐37. [DOI] [PubMed] [Google Scholar]
- 7. Perry S, Burrow MF, Leung WK, Bridges SM. Simulation and curriculum design: a global survey in dental education. Aust Dent J. 2017;62(4):453‐463. [DOI] [PubMed] [Google Scholar]
- 8. Perry S, Bridges SM, Zhu F, et al. Getting to the root of fine motor skill performance in dentistry: brain activity during dental tasks in a virtual reality haptic simulation. J Med Int Res. 2017;19(12):e371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yang Y, Zhang L, Bridges S. Blended learning in dentistry: 3‐D resources for inquiry‐based learning. Knowl Manag E‐Learn. 2012;4(2):217‐230. [Google Scholar]
- 10. Bridges S. An emic lens into online learning environments in PBL in undergraduate dentistry. Pedagog. 2015;10(1):22‐37. [Google Scholar]
- 11. Higgins D, Hayes M, Taylor J, Wallace J. A scoping review of simulation‐based dental education. MedEdPub. 2020;9(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Committee on Quality of Health Care in America . Crossing the quality chasm: a new health system for the 21st century. National Academy Press, Institute of Medicine (US); 2001:15, 166. [Google Scholar]
- 13. Gunter TD, Terry NP. The emergence of national electronic health record architectures in the United States and Australia: models, costs, and questions. J Med Internet Res. 2005;7(1):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hippisley‐Cox J, Pringle M, Cater R, et al. The electronic patient record in primary care—regression or progression? A cross sectional study. Br Med J. 2003;326(7404):1439‐1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Redmond WR. Digital models: a new diagnostic tool. J Clin Orthod. 2001;35(6):386‐387. [PubMed] [Google Scholar]
- 16. AAO O . Clinical Practice Guidelines for Orthodontics and Dentofacial Orthopedics. Pretreatmet Considerations: Diagnostic Records; 2017. [Google Scholar]
- 17. Han UK, Vig KW, Weintraub JA, Vig PS, Kowalski CJ. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofac Orthop. 1991;100(3):212‐219. [DOI] [PubMed] [Google Scholar]
- 18. Joffe L. Current products and practices OrthoCAD™: digital models for a digital era. J Orthod. 2004;31(4):344‐347. [DOI] [PubMed] [Google Scholar]
- 19. Bootvong K, Liu Z, McGrath C, et al. Virtual model analysis as an alternative approach to plaster model analysis: reliability and validity. Eur J Orthod. 2010;32(5):589‐595. [DOI] [PubMed] [Google Scholar]
- 20. Venkatesh V, Thong JY, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Quarterly. 2012;1:157‐178. [Google Scholar]
- 21. Yang Y, Liao C, Ho CH, Bridges S. Students’ perception of using dental e‐models in an inquiry‐based curriculum. Int J Soc Human Sci Eng. 2013;7:1267‐1271. [Google Scholar]
- 22. Gürel E, Tat M. SWOT analysis: a theoretical review. J Int Soc Res. 2017;10(51):994‐1006. [Google Scholar]
- 23. Dwivedi YK, Rana NP, Jeyaraj A, Clement M, Williams MD. Re‐examining the unified theory of acceptance and use of technology (UTAUT): towards a revised theoretical model. Inf Syst Front. 2019;21(3):719‐734. [Google Scholar]
- 24. Sweller J. Cognitive load theory. In: ELSEVIER (eds), Psychology of learning and motivation. Academic Press; 2011;55:37‐76. 10.1016/B978-0-12-387691-1.00002-8 [DOI] [Google Scholar]
- 25. Van Merrienboer JJ, Sweller J. Cognitive load theory and complex learning: recent developments and future directions. Edu Psychol Rev. 2005;17(2):147‐177. [Google Scholar]
- 26. Bickhard MH. An integration of motivation and cognition. In: BJEP Monograph Series II, Number 2‐Development and Motivation. British Psychological Society; 2003;41:56, pp. 41‐56. [Google Scholar]
- 27. Wu JH, Tennyson RD, Hsia TL. A study of student satisfaction in a blended e‐learning system environment. Comput Educ. 2010;55(1):155‐164. [Google Scholar]
- 28. Ferrari A, Punie Y, Brečko BN. DIGCOMP: a framework for developing and understanding digital competence in Europe. 2013. http://ftp.jrc.es/EURdoc/JRC83167.pdf. Accessed November 7, 2015.
- 29. Park K, Kinginger C. Writing/thinking in real time: digital video and corpus query analysis. Lang Learn Technol. 2010;14(3):31‐50. [Google Scholar]
- 30. Humes A. Research on the composing process. Rev Educ Res. 1983;53(2):201‐216. [Google Scholar]
- 31. Stallard CK. An analysis of the writing behavior of good student writers. Res Teac Engl. 1974;206‐218. [Google Scholar]
- 32. Miller KS. Second language writing research and pedagogy: a role for computer logging? Comput Compos. 2005;22(3):297‐317. [Google Scholar]
- 33. Rohsenow DJ, Marlatt GA. The balanced placebo design: methodological considerations. Addict Behav. 1981;6(2):107‐122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are not publicly available due to ethical issues but are available from the corresponding author on reasonable request.


