Abstract
Aims
This study explores how women diagnosed with breast cancer may be supported by physicians and nurses during physical and existential changes related to oncoplastic breast surgery in Denmark. The following research questions were addressed: (a) how do women experience oncoplastic breast surgery, and (b) how does cancer treatment affect their body image?
Design
A descriptive qualitative study design with a six‐step thematic analysis influenced by Braun and Clarke was applied in this study. This paper has been prepared in accordance with the consolidated criteria for reporting qualitative research.
Methods
Fourteen in‐depth interviews with seven women diagnosed with breast cancer were conducted from August 2018 to March 2019. In this qualitative study, data analysis was performed concurrent with data construction, recognizing that the process of analysis and making sense of data should start during the interviews. We explicitly frame the discussion of the findings in a theory of embodiment influenced by Merleau‐Ponty, consistent with the construct of exploring human experiences to generate meaningful knowledge for applied practice.
Results
Two overall themes with related subthemes were identified: (1) 'Treatment is required for life‐threatening cancer', and (2) 'Striving for a new normal body'. Across both themes, women's experiences reflected a 'time pendulum' as they contemplated their past identity, their current rationale and their transition to a future beyond breast cancer with a changed body.
Conclusion
Participants reflected on their past, present and future when facing an altered body image caused by their breast cancer diagnosis and oncoplastic breast surgery. The participants in the study expressed broad levels of satisfaction with the results of the oncoplastic breast surgery. The reconstructed breast helped them to live normally again, in particular maintaining interpersonal relationships. Breast reconstruction supported participants' embodiment experiences and redefinition of their 'new normal'.
Impact
This study showed the dynamic changes in self‐definition from receiving a breast cancer diagnosis and cancer treatment to oncoplastic breast surgery. The main finding of self‐redefinition was from the perspective of breast cancer women who were in a period of transition between post‐diagnosis and consultation for oncoplastic breast surgery. The findings indicate that advanced nurse specialists in the field of oncoplastic breast surgery can enhance psychosocial wellbeing and support women pre‐ and post‐operatively by focusing on patient experiences of self‐image and embodiment.
Keywords: advanced nursing, breast cancer, longitudinal research, oncoplastic breast surgery, recovery, supportive care needs
1. INTRODUCTION
Women diagnosed with breast cancer in Western countries are increasingly offered oncoplastic breast surgery as part of breast cancer treatments. Formerly, the primary focus of breast cancer treatment was lumpectomy or mastectomy, with little to no focus on postsurgical aesthetics or psychosocial aspects related to the process and its result. However, the number of breast cancer survivors continues to grow due to advancements in surgical and medical treatment. Therefore, long‐term outcomes and the experiences of individuals with breast cancer, such as quality of life related to body image and satisfaction, have become increasingly important components of breast cancer treatment and rehabilitation. Moreover, the development of surgical techniques such as microsurgery offers more opportunities and solutions in oncoplastic breast surgery (Macmillan & McCulley, 2016). Contemporary, state‐of‐the‐art aesthetic goals for oncoplastic breast surgery have therefore evolved to include the retention or restoration of one or both breasts to near normal shape, appearance, symmetry and size following breast cancer surgery. Standards for oncoplastic breast surgery are now described in a European guide on best practices (Gilmour et al., 2021). In Denmark, the Danish Breast Cancer Cooperative Group and the Danish Health Authority provide guidelines on best practices for breast cancer for accelerated inquiry, diagnostics and treatment, including oncoplastic breast surgery, if relevant (The Ministry of Health, 2018).
Previous research indicates that women who undergo breast reconstruction after breast cancer treatment report the highest long‐term satisfaction with their breasts, with a lower incidence of depression, while women undergoing mastectomy without reconstruction report the lowest satisfaction (Atisha et al., 2015). This could indicate that reconstruction should be recommended for all women diagnosed with breast cancer. However, although nurses advocate for scientific evidence about care, health and illness, they also know that the standardizing tendencies of evidence‐based practice can overrule individual variation, cultural needs, preferences and rights. In nursing theory, bodily changes are not simply objective goals, they are also subjective experiences that influence the individual's experience of the body in the world and the lived life. Furthermore, individuals are challenged and confronted with the fact that bodies are individually experienced but culturally and socially produced (Hopwood & Hopwood, 2019a), meaning that women's bodily experiences might be too complex and individual a phenomenon to capture through simple satisfaction outcomes.
During clinical practice, nurses meet women recently diagnosed with breast cancer who struggle with complex decisions about whether to choose oncoplastic breast surgery or conventional breast cancer surgery. Women are usually offered one of three equally effective oncologic surgical strategies: breast‐conservation surgery, mastectomy or mastectomy with breast reconstruction (and contralateral symmetry surgery, when relevant). The care and treatment of women undergoing these surgeries require nurses to consider issues related to body image and other psychosocial aspects. This qualitative study investigated experiences of Danish women diagnosed with breast cancer who received oncoplastic breast surgery to learn how nurses can support women during such bodily and existential changes.
1.1. Background
The prognosis for breast cancer has significantly improved in recent decades: currently, over 1 million women worldwide are diagnosed with breast cancer annually, and there is a 75% survival rate in most developed countries (World Health Organization, 2021). As a result, cosmetic concerns after breast cancer treatment affect an increasing number of women, including scars, large excision volumes, breast asymmetry, breast shape change, nipple displacement, scar retraction, skin alterations and radiation boost that can negatively impact outcomes in addition to the issues previously listed (Everaars et al., 2021; Ozmen et al., 2015). Further, poor cosmetic results may negatively impact body image and self‐esteem, or result in impaired sexuality or depression (Negenborn et al., 2017). Emphasizing cosmetic results may decrease psychological distress and improve the quality of life in breast cancer survivors (Hau et al., 2013; Kim et al., 2015).
Women diagnosed with breast cancer face different options for treatment, including surgery, chemotherapy, irradiation and hormonal therapy. In Denmark, multidisciplinary tumour management conferences provide recommendations for treatment at regular meetings comprising a team of healthcare specialists, including pathologists, oncologists, breast surgeons, plastic surgeons and registered breast cancer care nurse coordinators, all of whom are involved at different stages of a patient's cancer management plan. Based on a review of individual patients, this team reaches a consensus on suggested treatment. Treatment recommendations are based on tumour pathology, cancer stage, indications of potential metastasis and patient status, to achieve positive oncological outcomes and acceptable aesthetic results (Gilmour et al., 2021; Prades et al., 2015), and may include oncoplastic breast surgery and contralateral symmetry surgery. Oncoplastic breast surgery is a fairly new technique that combines plastic surgery with surgical oncology. In a typical procedure, the tumour is removed and the remaining breast tissue is reshaped or expanders are implanted to achieve symmetry and a more natural breast appearance (Berry et al., 2010). Oncoplastic breast surgery reduces (a) the time required to adjust to a reconstructed breast and altered body image (typically, this takes 1 year or more), including potential impacts on quality of life, emotional well‐being and intimacy; and (b) the range of physical and psychological impacts of surgery (e.g., discomfort, lack of sensation, self‐consciousness, body image issues) that may contribute to dissatisfaction with outcome (Gilmour et al., 2021). Body image is a key motivation for oncoplastic breast surgery. However, the procedure is more complex than standard breast cancer surgery and requires either both a breast surgeon and a plastic surgeon to carry out the operation, or one surgeon with oncoplastic certification, which may delay the patient's cancer management plan. Significant delays to breast cancer surgery may be associated with an increased risk of mortality (Hanna et al., 2020). Furthermore, oncoplastic breast surgery often requires volume displacement or volume replacement techniques, with contralateral symmetry surgery as required (Rizki et al., 2013).
The term body image relates to the concept of body and mind and has been developed and characterized by different historical and epistemological approaches. Modern dualistic approaches can be traced back to René Descartes (1596–1650), who saw human beings as consisting of two parts, body and mind, implying a mechanical perception with no causal connection between the two parts (Cash & Pruzinsky, 2002). In contrast, in 1944, the phenomenologist Maurice Merleau‐Ponty described the concept of the mind and body as a whole (Merleau‐Ponty, 2011). In 1990, Bob Price, a nurse, developed the body image care model (Price, 1990), which focuses on how humans experience bodily changes as a result of illness, injury or disability. The model describes body image as influenced by three dimensions: body ideal, body reality and body appearance.
From an anthropological perspective, the body is viewed as a product of a specific historical, social and cultural context that influences how a person interacts with the surrounding world. The literature increasingly recognizes that the interface between the physical, psychological and social realms matters for body image. Patients may be affected by medical illness and treatment, leading to an altered body, changes in bodily functions and the personal and social consequences of these changes (Hopwood & Hopwood, 2019b; Rezaei et al., 2016).
The results from previous research on body image following treatment for breast cancer are diverse. Most studies concentrate on women's experiences related to body image after either mastectomy or lumpectomy (Brunet et al., 2013; Collins et al., 2011). These studies find that overall, women experience physical changes in a mostly negative way, which shapes their perceptions, thoughts, attitudes, feelings and beliefs about their bodies. Other research finds that discomfort related to body image decreases over time regardless of the type of breast surgery, if comparing breast‐conserving surgery, mastectomy alone and mastectomy with reconstruction (Collins et al., 2011). Furthermore, research also shows that mastectomy is associated with more body image issues compared with lumpectomy and mastectomy with reconstruction, and that women who have had reconstruction experience higher satisfaction with their sexual life and with the aesthetic and cosmetic result (Marinkovic et al., 2021). In addition, these women tend to experience less embarrassment related to their body and less negative attention related to the disease (Fernández‐Delgado et al., 2008). Women who choose reconstruction also tend to experience a balanced body image and expect to retain a sense of femininity, both physically and mentally (Collins et al., 2011; Crompvoets, 2006; Snöbohm et al., 2010). Other research indicates that women's experiences of body image can be subjective and dependent on multiple individual factors, such as context, culture, social relations, cancer severity, tumour size, stage and volume of excision, among others (Gilmour et al., 2021; Negenborn et al., 2017). In summary, a growing body of literature evidences that the experience of breast cancer seriously affects women and their overall sense of body image (Boquiren et al., 2013; Jabłoński et al., 2019) for years after diagnosis and treatments (Dahl et al., 2010).
In the care and treatment of women diagnosed with breast cancer, hospital nurses and physicians still tend to evidence a dualistic understanding of the body, focusing more on treatment regimens and less on the whole person (Paraskeva et al., 2019; Schmid‐Büchi et al., 2008). The complexity of body image presents an ongoing challenge to better recognize and understand the diverse issues underpinning it, including the extent and causes of, and recovery from, body image disruption (Hopwood & Hopwood, 2019b). The available research and knowledge on body image after oncoplastic breast surgery is sparse, as most research has investigated body image using scale‐based questionnaires rather than individual self‐expression. Furthermore, little is known about the information needed by women receiving oncoplastic breast surgery, or their expectations.
2. THE STUDY
2.1. Research questions and aims
This study aimed to investigate how women diagnosed with breast cancer may be supported by nurses during bodily and existential changes related to oncoplastic breast surgery. The following research questions were addressed: (a) how do women experience oncoplastic breast surgery over time, and (b) how does cancer treatment affect their body image over time?
2.2. Design
The design of this study was influenced by the authors' and their nursing colleagues' experiences in a breast surgery outpatient clinic. Nurses reported that physicians advocated for oncoplastic surgery to provide improved aesthetic results after breast cancer and thereby achieve an improved quality of life in the long term, as showed in research (Atisha et al., 2015). However, nurses noted that patients' levels of satisfaction related to their breast(s) were more associated with body image, acceptance of the oncoplastic surgery, and postoperative pathways. Therefore, the authors assumed that women's perspectives on experiences of body image over time, both during and after oncoplastic cancer treatment, could provide insights to inform future practice. To explore this, a descriptive qualitative study design with a thematic analysis influenced by Braun and Clarke was chosen for its capacity to explore women's experiences (Braun et al., 2013), and individual in‐depth interviews with key informants were collected. Individual interviews are ideally suited to explore experiential research questions and can also be useful for exploring understandings and perceptions (Braun & Clarke , 2013). The study was conducted by two experienced female nurse researchers employed at the same department. The first author is a registered nurse, Master of Science in Nursing and PhD, while the second author is a nurse specializing in clinical practice with more than 10 years of experience in applied research. An EQUATOR checklist for reports of interviews and a COREQ focus group studies checklist were applied (Tong et al., 2007); see further details in Appendix B.
2.3. Participants and settings
Participants were recruited face to face by the second author in August and September 2018 at a large breast surgery outpatient clinic at a Danish university hospital, during patient consultation appointments. At the time of the interviews, the department of plastic surgery and the department of breast surgery were separate departments located at different hospitals in the region. This was a limitation for the speciality, complicating interprofessional collaboration between the departments involved in the treatment and care of women diagnosed with breast cancer. In 2015, the departments were merged into the Department of Plastic and Breast Surgery but were not physically consolidated at the same hospital location until 2020.
In total, nine candidates for oncoplastic breast surgery were invited to participate in the interviews. Two women declined to participate. The participants were therefore seven female Danish‐speaking patients diagnosed with breast cancer or ductal carcinoma in situ who had chosen oncoplastic breast surgery. All participants had proactively requested oncoplastic breast surgery, which was not a standardized treatment at the time of the study due to limited collaboration between the specialities. Participants were purposefully sampled for maximum variation of demographic characteristics, providing variability of participant experiences with respect to the phenomenon explored. Participant demographics and other variables are presented in Table 1.
TABLE 1.
Participant variables and categories
| Variable | Categories | Frequency (f) |
|---|---|---|
| Age | 30–39 years | 1 |
| 40–49 years | 2 | |
| 50–59 years | 4 | |
| Number of children | 0 | 1 |
| 2 | 3 | |
| 3 | 3 | |
| Education | Diploma | 2 |
| Bachelors degree | 4 | |
| Relationship status | Married | 6 |
| Co‐habiting | 1 | |
| Diagnosis | Breast cancer | 6 |
| Ductal carcinoma in situ | 1 | |
| Treatment modality (>1 method is possible) | Breast conservation surgery | 1 |
| Mastectomy with breast reconstruction | 6 | |
| Contralateral balancing | 1 | |
| Bilateral breast reduction | 1 | |
| Chemotherapy | 6 | |
| Irradiation | 2 | |
| Hormonal therapy | 4 | |
| (N = 7) | ||
In Denmark, all facilities treating breast cancer are part of the multidisciplinary Danish Breast Cancer Cooperative Group, which prepares evidence‐based guidelines about diagnostic procedures, treatment and follow‐up to improve prognosis (The Danish Breast Cancer Cooperative Group [DBCG], n.d.). The healthcare system is government‐funded for all citizens, indicating that the population served by any given treatment centre represents all patients regardless of socioeconomic background.
2.4. Data collection
The interviews were conducted by the second author from August 2018 to March 2019 as in‐depth interviews following a semi‐structured interview guide (Braun & Clarke, 2013) influenced by Price's theoretical constructs of body ideal, body reality and body presentation, on the assumption that an altered body image affects women's experiences (Price, 1990). The interview guide is presented in Appendix A. Participants met individually with the second author in a conference room in the hospital and were explained the research purpose and participants' rights. Each participant was interviewed twice face‐to‐face to investigate personal development and experiences over 6 months, resulting in a total of 14 interviews. The initial interview was conducted after each participant's oncoplastic breast surgery, in 30 days of diagnosis. The second interview was conducted approximately 6 months after the first interview. Each interview lasted 30–45 min. The interviews were audio‐recorded, transcribed verbatim and uploaded to the qualitative software programme NVivo for analysis.
2.5. Data analysis and rigour
For rigorous qualitative sampling and saturation of data, Braun et al. (2013) propose that qualitative researchers require a sample that is appropriate to the research question and the theoretical aims of the study, and which can provide an adequate amount of data to fully answer the question and analyse the issue. After the 14 interviews, the authors concluded that the interview guide questions were rigorous enough for a substantial thematic analysis and sufficient to lead to relevant findings.
Interviews and analysis were initially guided by the research questions. However, as the process of data collection and interpretation evolved, the theoretical framework was adapted. The theoretical framework for the present study was influenced by Merleau‐Ponty's phenomenology of perception and embodiment, consistent with the construct of exploring human experiences and producing meaningful knowledge for applied practice. Merleau‐Ponty argues that human understanding comes from our bodily experience of the world that we perceive (Merleau‐Ponty, 2011). He proceeds from the assumption that human existence is bodily and that we as subjects are embodied, meaning inseparable from our bodies and our world. He defines body image as 'the ways meanings, expectations, and habits are experienced and expressed in the body' (Merleau‐Ponty, 2011). Thus, illness affects the whole person and its result is not simply objective, e.g., a reconstructed breast. Rather, there is a complex relationship between meaning, body, and diagnosis and women diagnosed with breast cancer have their own perceptions of the illness. This approach enabled us to understand illness experiences from a first‐person perspective.
Analysis was conducted using the six‐step approach (illustrated in Figure 1) prescribed by Braun and Clarke (Braun & Clarke, 2006). Thematic analysis is an accessible and flexible theoretical method of qualitative analysis to construct and organize data into themes across a dataset. The analysis was conducted as an abductive analytic process, moving back and forth from data to theorizing, to unfold and create narratives about the phenomenon investigated (Braun & Clarke, 2006).
FIGURE 1.
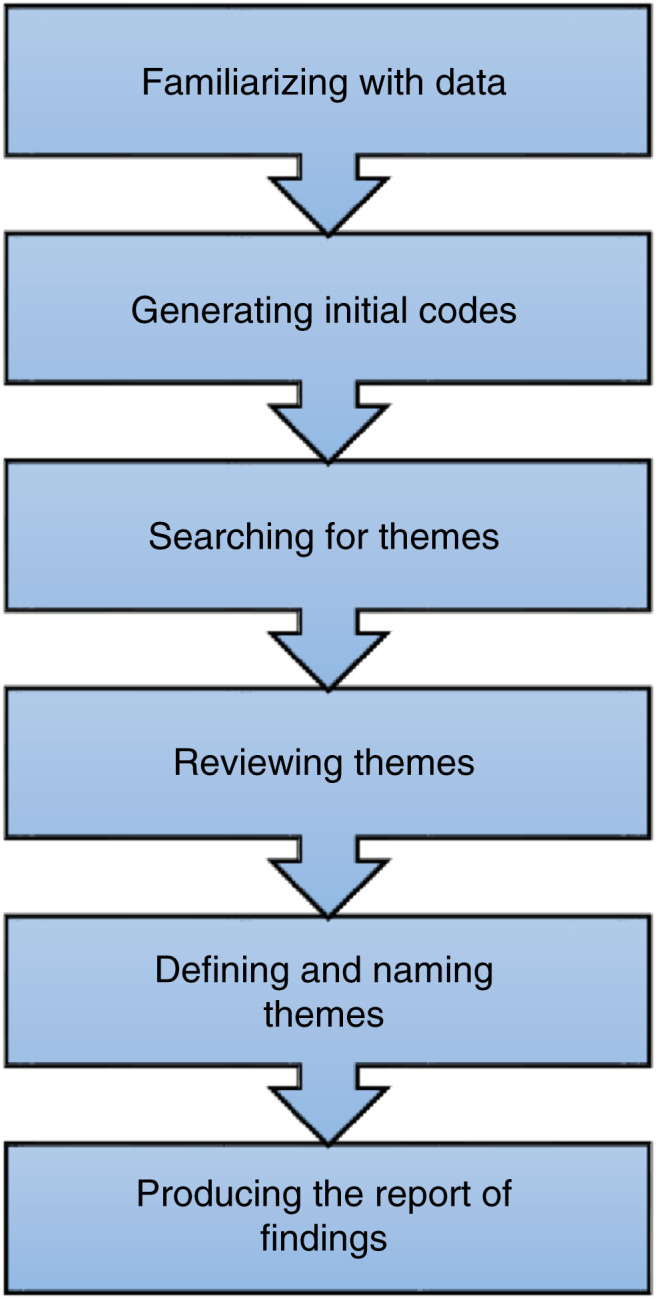
Illustration influenced by Braun and Clarke's six‐step thematic analysis (Braun & Clarke, 2006).
Analysis was conducted on the transcribed textual data. The data from the first and second interviews for each patient were combined into one analysis to explore the individual patients' personal development and experience over time. First, the authors briefly read and discussed the transcripts of the interviews, focusing on participants' experiences related to the constructs of body ideal, body reality, body presentation and preliminary interpretations. Then the first author conducted the process of coding in NVivo: first, an open coding, followed by an axial coding, looking across data to flesh out key conceptual dimensions and account for variations, leading to the construction of draft themes. NVivo supported this process by making procedures explicit and transparent. Next, the draft was discussed and interpreted by the first and second authors, leading to a novel construction and specification of themes. The analysis was undertaken in Danish, and when final themes were identified, quotes selected to illustrate the themes and subthemes were translated into English. The selected quotes were translated forward and backward by the first author according to quality assurance criteria for accuracy and correct usage of language in medical translation (Karwacka, 2014). Translations were agreed on by the authors. Participant quotes are included in the following presentation of findings to support the analysis.
2.6. Ethical considerations
Having received full information about the study aims and the data collection process, all participants provided informed written consent for their participation. Ethical clearance was obtained by the National Committee on Health Research Ethics and the Danish Data Protection Agency (REG‐104‐2021). This study was conducted in accordance with the principles of the Declaration of Helsinki ('World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects', 2013).
3. FINDINGS
The analysis resulted in two overall themes, described in detail below: (1) 'Treatment is required for life‐threatening cancer', and (2) 'Striving for a new normal body'. Common to the two themes were patients' feelings of being on a pendulum, reflecting on who they were in the past, their current rationale and transitioning to their life beyond breast cancer with a changed body. Figure 1 shows the conceptual time perspective that was an underlying mechanism throughout the identified themes.
3.1. Theme 1: Treatment is required for life‐threatening cancer
This theme encapsulates the finding that participants were confronted with life‐threatening cancer that required immediate treatment, and they were highly dependent on physicians for their treatment, and by extension, for their own future. The theme was further divided into two subthemes: 'The priority is to treat the cancer' and 'Being in the hands of the physicians'.
3.1.1. The priority is to treat the cancer
The subtheme 'The priority is to treat the cancer' was found to be a very strong underlying premise for study participants, as the life‐threatening cancer diagnosis was the overarching fact occupying their minds before thinking of oncoplastic breast surgery. Participants expressed that receiving a cancer diagnosis was like a fatal 'stamp' indicating that they could die without treatment. Living with a cancer diagnosis were described by one participant as: 'One tends to associate cancer with death, like cancer equals death' (Participant 1). Another participant described their cancer diagnosis saying, 'I was struck by lightning, but I have been lucky to survive so far' (Participant 7).
The participants experienced difficulty talking about their wishes related to their future breasts and body image. Treating the cancer in a way that would lead to the best possible outcome was their top priority. One participant said:
The only thing on my mind when I got my diagnosis was for the cancer to disappear and I did not think much about what different kinds of surgery would mean related to femininity or to the choice of surgery in general… I just wanted the breast cancer to go away as soon as possible… (Participant 3).
For the participants in the diagnosis phase, this prioritization of cancer treatment meant, quite rationally, postponing thoughts about having breasts in the future. However, the participants did express concerns related to the potential long‐term effects of an altered body image, and because of this, they proactively requested oncoplastic breast surgery.
3.1.2. Being in the hands of the physicians
This subtheme captures participants' experiences of dependency during cancer treatment and in relation to the oncoplastic breast surgery, they were offered. The participants who went through chemotherapy stated that the treatment was controlled by their oncologist and that there was a recommended course of treatment to follow to achieve the best possible outcome and recovery. The participants experienced being in the hands of different specialists—breast surgeons, oncologists and plastic surgeons, each of whom had distinct perspectives related to the oncoplastic breast surgery trajectory, which blurred the long‐term plan in participants' minds. This theme was also associated with waiting for chemotherapy to take effect, or waiting to heal from surgery, so that the physician would present the next step in the process of treatment, or 'where to go next.' For example, one participant commented: 'The physicians are in control of my cancer treatment plan… I do not know if I can get the operation while I am in chemotherapy or whether I have to wait until it is finished' (Participant 1).
Approval for oncoplastic surgery was highly dependent on a patient's condition, such as their body mass index and physical status; not all the participants were candidates for all types of breast reconstruction or correction. One participant offered nuanced insights into how she was in the hands of the physician, stating:
I do tend to get worried… The last time I got filler in my tissue expander, the physician or surgeon told me that I had three to four months to lose weight if I wanted the final operation… At the same time, that is a completely unfair battle for me because I get antihormones which impede and complicate my weight loss. (Participant 6).
Participants were dependent on the judgement of physicians, who acted as gatekeepers for treatment and surgical possibilities.
3.2. Theme 2: Striving for a new normal body
By their second interviews, most participants had completed their initial chemotherapy or surgical treatment; some had yet to complete certain steps, such as plastic surgery, expanders, corrections or nipple tattoos. The theme 'Striving for a new normal body' captured participants' reflections on future aspects related to their body and self. This theme also illustrated how the participants were dealing with their body at the time of the interviews, and that the process of identifying with a changed body led to different thoughts on the appearance of their breasts and their acceptance of the cosmetic result. The interpretation flowed into three subthemes: 'At least there is something in my bra,' 'Wishing for a plan for my new breasts' and 'Redefining myself after breast cancer'.
3.2.1. At least there is something in my bra
The subtheme 'At least there is something in my bra' relates to patient experiences of their breasts post‐surgery: a reconstructed breast had weight and volume even if it was no longer a natural breast. The participants in the study expressed broad levels of satisfaction with the results of the oncoplastic breast surgery. For example, one participant said:
I could wish for as many as possible to get the [oncoplastic breast] surgery…. It is a big deal that you still have breasts. They may not look very, you know, but I do think they [the surgeons] have done a good job. At least there is something to fill in the bra, so I guess people will never notice that the breast is not mine (Participant 1).
However, participants had different perspectives on the importance of physical appearance and aesthetic results from oncoplastic breast surgery. A commonality was that participants were pleased that their reconstructed breast had enough volume to fill a bra, therefore obviating a breast prosthesis. As one participant expressed:
I had to accept that it [the breast] looks very different than my own breast, but as I have now got the message that the cancer is gone, I feel now that I can expect a decent result that I can live with the rest of my life. I do feel that I am fairly young. Maybe it would be different if I was 80 years old – then it would not be so important… But the breast and shape does imply a femininity which I have always had… Therefore I think it would be much harder for me if they [the breasts] suddenly were not there… (Participant 7).
Participants also compared the surgical outcome with the alternative of having no breast(s) and reasoned that the volume of the reconstructed breast(s) was better than a flat chest due to mastectomy.
3.2.2. Wishing for a plan for my new breasts
During the second interview, the participants had completed the initial phases of treatment and were increasingly preoccupied with the construction of the new breast(s), identified in the 'Wishing for a plan for my new breasts' subtheme. The participants also expressed a wish for a concrete plan for the reconstruction of their breasts as part of returning to daily life, for example: 'I want to move on with my life now… That is also why I tend to get a bit sceptical [of the reconstruction operation plan]… When can I get the operation, because it stops my work life…?' (Participant 7). When the participants did not have a clear plan, they expressed insecurity, which could indicate uncertainty about reconstruction:
I think the plan is on standby for now, they [the physicians] have to see the result. People tell me, like, wow, those [new breasts] are so nice… That might be true, I do not know, and I do not think I can commit to this yet because I do not know if they are finished or if they [the prostheses] are here to stay (Participant 7).
Another participant also expressed frustration due to a lack of answers to specific questions they had related to their breasts:
I do not quite know how much volume I can get into the expanders. When I ask, I feel that is it not a subject of importance and that the issue is being easily bypassed because they tell me that we must wait and see how much volume the expander and skin can hold and how the breast shapes, so I listen to that, although I cannot get a concrete answer… To me, it is important if the breasts look how I want or if I just have to fit into their opinion (Participant 2).
Another participant raised the issue that plans for breast reconstruction should have been discussed at the diagnosis stage, even though participants often focused initially on treatment rather than future breast reconstruction: 'I could have used that when I got the breast cancer diagnosis and I was told that my breast should be removed; someone should have talked to me about the options [related to the breast]—what would have been good for me and what could possibly happen' (Participant 1).
3.2.3. Redefining a self after breast cancer reconstruction
During the interviews, participants elaborated on what they experienced as a unique situation: dealing with a cancer diagnosis while simultaneously being hopeful about their future. This subtheme was identified as 'Redefining a self after breast cancer reconstruction'. One participant commented on their way of coping with the situation:
My focus has been to get going after the disease, being me and keeping up the everyday life we used to have. For me it was like ‘get into the game,’ cheer up, take a walk and go to work… (Participant 5).
Another participant expressed a rather pragmatic way of redefining the body after cancer and reconstructive surgery:
Looking at my breasts is very extraordinary. Feeling them is extraordinary. I think it is comparable to giving birth, then the body is a completely different universe until it is healed. In the situation, you adjust to the condition, and you mentally retrieve the situation… It is the same with breasts (Participant 2).
Participants also elaborated on how the trajectory of treatment had not only affected their body but also their personality: ‘I felt that my personality suddenly changed…I lost my hair [due to chemotherapy] and then I had just small breasts and no hair…Now, after the [oncoplastic breast] surgery, the only one that is affected by the truth [of the previous cancer] is me and my naked body’ (Participant 2). This participant's experience in particular illustrates how individual experiences were affected by past diagnoses; how they approached defining a new self; and how they thought about their future, including integrating it with their personal history. They were experiencing a transition.
4. DISCUSSION
This study was performed to investigate women's experiences with oncoplastic breast surgery and how the cancer treatment affected their experiences of body image. Two themes were identified: (1) ‘Treatment is required for life‐threatening cancer’, and (2) ‘Striving for a new normal body’. The first theme summarizes how participants focused primarily on treating the cancer; at the same time, they were dependent on physicians for their cancer treatment and surgical plans. The second theme expresses participants' reflections on future aspects related to their body and self, including their postsurgical experiences of breast reconstruction; this theme also reflects the fact that participants actively requested a plan and were striving to redefine themselves.
The themes and subthemes extracted from the interviews with participants illustrate the complex situation women confront when diagnosed with breast cancer, a potentially life‐threatening disease. The interviews indicate that 6 months after diagnosis, participants remained in a condition of acute crisis related to their cancer diagnoses, a finding confirmed by previous research (Berterö & Chamberlain Wilmoth, 2007). Even while managing this state of crisis, participants were striving for a future, one that incorporated their new breasts. This existential situation can be compared with the movement of a pendulum, a metaphor from psychology used with regard to coping strategies in the presence of death (Sand et al., 2009). The pendulum moves between dichotomous dimensions and elicits diverse reactions depending on personal and environmental factors, a metaphor that fits our findings. Participants discussed their past, including how their breasts were before their diagnosis. They expressed the situation as a rationale underlying their life events when expressing their perspectives on the oncoplastic breast surgery. Participants also expressed uncertainty about their future related to the plan for oncoplastic surgery. This pendulum of past, present and future is illustrated in Figure 2. The pendulum effect was also seen in the transitioning, distress and repercussions for participants as they strived to identify with their altered body and self.
FIGURE 2.
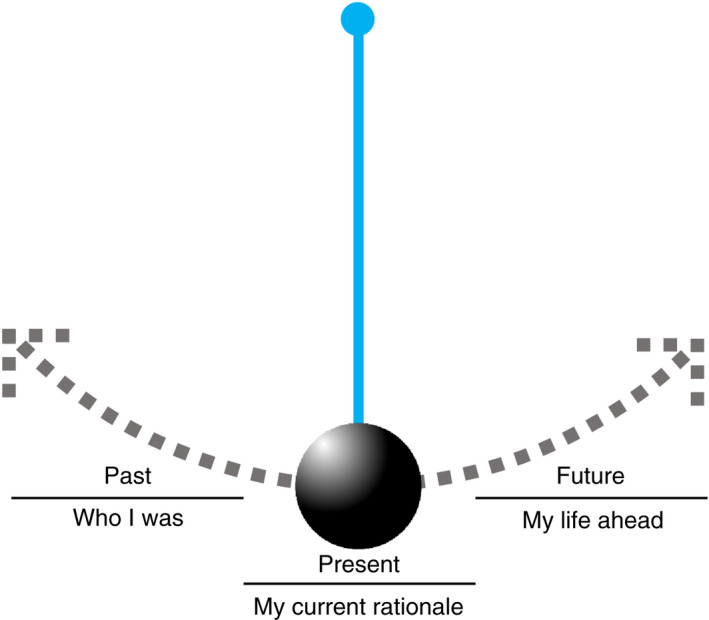
Illustration of participant experiences as a pendulum, as part of transitioning and their altered embodiment.
In Merleau‐Ponty's phenomenology of perception, changing or replacing parts of the physical body leads to embodiment alterations (Merleau‐Ponty, 2011). The altered body is an integral part of the subjective being, wherein the body influences the mind, and time and transition are required before the altered body is part of the individual's embodiment (Merleau‐Ponty, 2011). Oncoplastic breast surgery affects the whole person: there is a complex relationship between meaning, body and the situation, in which women have their own perceptions of the illness and treatment (Thomas, 2005). Participants in our study experienced that adapting to embodied alterations could be hindered by uncertainty related to future surgical plans and results. Embodiment issues also manifested in how the participants related their self‐image and bodily awareness to embodied normalization; striving to redefine the self was linked to the process of breast reconstruction, having ‘something to put in the bra’.
This perspective of women's embodiment is supported by the embodied body framework by Hopwood and Hopwood, who introduced this framework as an aspect of psycho‐oncology. The authors suggest a multidimensional approach to better recognize and understand the extent, causes and recovery related to altered embodiment; they state that humans cannot untether themselves from the past and that the past will always intrude on the present (Hopwood & Hopwood, 2019b).
Our findings support existing knowledge, affirming that coping with breast reconstruction surgery is complex, with multiple influencing factors. Furthermore, our study demonstrates the embodiment phenomenon among women who are interested in receiving breast cancer reconstruction surgery. The impact of breast reconstruction on participants' embodiment was to support them in redefining their 'new normal'. An interview study by Gershfeld Litvin and Jacoby explored women's experiences when electing to undergo breast reconstruction: women experienced mastectomy as a disability, and their expectations that breast reconstruction would restore their sense of normalcy were not fulfilled. Most women perceived the reconstructed breast mainly as a visual replacement (Gershfeld Litvin & Jacoby, 2017). These findings are consistent with our findings, as participants focused on ‘something to put into the bra’.
In our study, participants requested more information about oncoplastic breast surgery. Access to information was difficult due to varying departmental organizations at different locations in the region and a lack of a standardized care plan or collaboration specifically for oncoplastic surgery. In a 2019 study exploring women's decision‐making on breast reconstruction as a surgical option post‐mastectomy, the authors showed that the choice was negatively influenced by poor acceptance of this surgical procedure among the women. This was possibly due to variation in how physicians communicated treatment options to patients: patients offered breast reconstruction by their primary oncologist were more likely to consider integrating it in their breast cancer treatment plan (Retrouvey et al., 2019). Furthermore, acceptance of breast reconstruction was a complex process that took time, as from the moment of diagnosis to breast reconstruction consideration, survival was prioritized over reconstruction. However, as women realized that breast reconstruction was a way to regain normalcy, this surgical procedure gained acceptance. These findings support our hypothesis that women were initially interested in and focused on the removal of the cancer, potentially because of poor information on surgical procedures from physicians, but also because consideration of oncoplastic surgery might be overwhelming at the time of diagnosis. Another qualitative study by Retrouvey et al. identified that health care professionals do not consistently integrate oncoplastic breast surgery as an option when discussing treatments for breast cancer, affecting delivery between patients (Retrouvey et al., 2020). Likewise, the participants in our study expressed that information on oncoplastic breast surgery was absent at the time of the diagnosis, but at the same time, the participants' focus at that time was mainly on cancer treatment; this is slightly contradictory, with ambiguous implications for what information nurses and physicians should introduce to patients, how and when.
In a survey from 2019, Herring et al. showed considerable variability in women's experiences of their appearance after mastectomy and/or breast reconstruction (Herring et al., 2019). Some felt prepared and emotionally supported while others felt that elements of supportive care were missing. Proposed areas for improvement were preoperative discussions and increased preparation and support for patients, which could potentially contribute to better patient outcomes overall (Herring et al., 2019). A retrospective study from 2019 investigated women's experience of breast reconstruction and their ability to cope (Carr et al., 2019). The authors concluded that as nurses play a pivotal role in providing information to women recovering from breast reconstruction, improving communication channels between nurses and patients is likely to improve patients' experiences of support. Another study showed that nurses can assess women's specific support needs and partner with families to help them understand how best to support women during recovery (Carr et al., 2019), while other studies suggest psychosocial interventions to reduce body image–related distress in women with breast cancer (Brunet et al., 2021; Sebri et al., 2021; Sherman et al., 2018).
Our findings, together with the existing research on women's experiences with oncoplastic reconstruction, indicate doubts concerning the early benefits of reconstruction in general and oncoplastic breast surgery in particular. In some of the literature, oncoplastic breast surgery is presented to women as a procedure that 'cancels out' the mastectomy and facilitates a return to normalcy (Berry et al., 2010; Gilmour et al., 2021; Liu et al., 2018; Macmillan & McCulley, 2016; Riis, 2020; Weber et al., 2020), but this tends to underestimate the range of repercussions reported by women who have undergone the procedure.
Our findings show that women's experiences of oncoplastic breast surgery are complex on the individual level and that the repercussions of the surgery indicate the need for individualized and continuous support from nurses and physicians to support women throughout oncoplastic breast surgery and recovery. Some existing recommendations include increasing interprofessional collaboration at hospitals (Campbell‐Enns et al., 2017; Retrouvey et al., 2020) or deploying advanced nurse specialists in the field of oncoplastic breast surgery specifically to enhance the focus on psychosocial aspects and support women pre‐ and post‐operatively (Spector et al., 2010; Wilson et al., 2013). Furthermore, existing evidence suggests that hope mediates the relationship between self‐compassion about well‐being and distress outcomes in patients (Arambasic et al., 2019; Todorov et al., 2019), indicating that this should be part of specialist breast cancer nurses' psychosocial follow‐up care to help women cope with the impact of breast cancer on their quality of life. This finding is supported by a recent Cochrane systematic review on nurses' support of women with breast cancer which suggests that psychosocial interventions delivered by specialist breast cancer care nurses may improve supportive interventions during diagnosis, treatment and survivorship for women with primary breast cancer (Brown et al., 2021). This evidence clearly suggests that nurse specialists in the field of oncoplastic surgery have an essential role in supporting breast cancer survivors.
The contribution of the present study is that women experience a variety of emotions, sometimes moving from distress to hope for the future, during the process of oncoplastic breast surgery and transitioning to an altered body image. One implication for future practice is that nurses and physicians should carefully inform women about oncoplastic breast surgery, including providing information about the strict guidelines for candidates for oncoplastic breast surgery (Gilmour et al., 2021) and how the treatment is delivered by healthcare professionals from different departments. If women choose oncoplastic breast surgery, nurses and physicians can engage with the women's lived experiences of embodiment and recognize the importance of these experiences concerning the personal recovery process, for instance, through narratives in nursing (Damsgaard et al., 2021).
5. STRENGTHS AND LIMITATIONS
To our knowledge, this is the first study to qualitatively investigate the experiences of women undergoing oncoplastic breast surgery influenced by a longitudinal perspective, defined as 'a study design in which data are collected at more than one point in time' (Polit & Beck, 2018). Additional research on embodied perspectives may help to improve nurses' and physicians' understanding of how individuals manage problems or phenomena in illness, leading to better ways of supporting women in oncology settings (Thomas, 2005). Qualitative research of this kind on the oncoplastic breast surgery population can provide additional evidence for developing supportive practices. The current study did not focus on the fact that oncoplastic breast surgery often involves benign contralateral symmetry surgery, which is complex itself and the implications of which should be discussed with patients (Rizki et al., 2013).
The small sample of seven participants providing 14 interviews may be considered a weakness of the study; however, the sampling rationale aimed to engage a small number of individuals experientially familiar with the phenomenon and willing to share their experiences (Braun & Clarke, 2013). The sample size was appropriate to explore the specific research questions on human experiences in oncoplastic breast surgery treatment and the underlying subjective, experiential nature of related phenomena (Braun & Clarke, 2013).
In terms of the quality criteria of validity and generalizability (Braun & Clarke, 2013), the findings in this study are dependent on the specific hospital department from which the participants were recruited, which influences external validity. However, the findings are highly relatable to existing research, which strengthens the trustworthiness of the results (Braun & Clarke, 2013). The findings provide nuanced perspectives from individuals undergoing oncoplastic breast surgery; however, the findings could have been more comprehensive if the study had proceeded as a multi‐centre study. The study findings might also differ if the study was conducted today, as the department has since developed more advanced trajectories for breast cancer treatment, consolidating the departments of plastic and breast surgery.
6. CONCLUSION
The contribution of this study is the finding that participants' rationales related to their past, present and future can be compared with a pendulum, transitioning to an altered body image due to the diagnosis of breast cancer and the subsequent oncoplastic breast surgery. At the time of diagnosis, the participating women concentrated on treating cancer, confident in the treatment prescribed by their physicians, and they expressed little interest in the long‐term oncoplastic breast surgery plan. As participants proceeded through treatment and towards surgery, they requested more information about the oncoplastic breast surgery procedures to clarify their future embodied self‐image; they also suggested that this information could have been provided at the time of diagnosis, a suggestion that was at odds with the finding that treatment, rather than reconstruction, was the initial focus.
An implication for future practice is that nurses and physicians caring for women with breast cancer who are candidates for oncoplastic breast surgery need to provide person‐centred care and information throughout the treatment process, from diagnosis and surgery to medical treatment and recovery, to engage with the women's lived experiences of embodiment and body image and to recognize the importance of these experiences in their transitions.
AUTHOR CONTRIBUTIONS
STH, LWR: Made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; STH, LWR: Involved in drafting the manuscript or revising it critically for important intellectual content; STH, LWR: Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; STH, LWR: Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
CLINICAL TRIAL REGISTRATION
Ethical clearance was obtained by the National Committee on Health Research Ethics and the Danish Data Protection Agency (REG‐104‐2021).
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15309.
ACKNOWLEDGEMENTS
The study team would like to acknowledge the contribution of the patients who are participating in this study.
APPENDIX A.
INTERVIEW GUIDES
Interview 1—The time of diagnosis
| Themes | Interview questions |
|---|---|
|
Body reality Attention to: Satisfaction with breast size/shape, appearance, pain, physical condition, issues with physical activities, sexuality. Bodily reality immediately after the breast cancer operation. The physical body in the acute disease phase. |
1. How did you experience your health condition and physical body before you got your breast cancer diagnosis? How do you experience your body at this stage after the surgery? Supportive questions
2. What are your thoughts about your breast cancer diagnosis? Supportive questions
3. Can you describe what you were thinking when you were offered oncoplastic surgery as part of your cancer treatment? Supportive questions
|
|
Body ideal Attention to: Female body ideals, the influence of nutrition, societal norms. |
4. Can you tell me about your ideal body? What is important to you? Supportive questions
|
|
Patient body presentation Attention to: Satisfaction with reflection in the mirror, physical condition, clothing, comfort in social contexts, equal with other women, attractive (with and without clothing). |
5. Tell me about how you think you present yourself. What perception do you think others have of you? Supportive questions
|
Interview 2—Post surgery
| Themes | Interview questions |
|---|---|
|
The patient's body reality Attention to: Satisfaction with size and shape of breasts, appearance, pain, physical condition, problems with physical activity, sexuality The surgeon's ability to inform. Confidence in the situation |
1. How do you consider your health status and your body in physical terms now, six months after the operation? Supportive questions
2. What thoughts do you have on your treated breast cancer? Supportive questions:
3. Describe your reflections on the offer of plastic surgery you were given. Supportive questions:
|
|
The patient's body ideal Attention to: female ideal, nutritional impact, societal norms. |
4. Tell me about your body ideal after your surgery. What do you consider important? Supportive questions:
|
|
The patient's body presentation Attention to: Satisfaction with reflection in the mirror, physical condition, clothing. Feeling comfortable in social contexts, feeling equal to other women and feeling attractive (with and without clothes). |
5. Tell me what you think about your apperance now, six months after your surgery? Supportive questions:
|
APPENDIX B.
CONSOLIDATED CRITERIA FOR REPORTING QUALITATIVE STUDIES (COREQ): 32‐ITEM CHECKLIST
Checklist of items that should be included in reports of interviews and focus groups according to Tong et al., 2007
| Section/topic | # Item | Guide questions/description | Reported on page # |
|---|---|---|---|
| Domain 1: Research team and reflexivity | Personal Characteristics | ||
|
Which author/s conducted the interview or focus group? | 9 | |
|
What were the researcher's credentials? E.g. PhD, MD | 8 | |
|
What was their occupation at the time of the study? | 8, 9 | |
|
Was the researcher male or female? | 8 | |
|
What experience or training did the researcher have? | 8 | |
|
Was a relationship established prior to study commencement? | 8 | |
|
What did the participants know about the researcher? e.g. personal goals, reasons for doing the research | 12 | |
|
What characteristics were reported about the interviewer/facilitator? e.g. Bias, assumptions, reasons and interests in the research topic | 8 | |
|
Domain 2: Study design |
Theoretical framework | ||
|
What methodological orientation was stated to underpin the study? e.g. grounded theory, discourse analysis, ethnography, phenomenology, content analysis | 8, 10, 11 | |
| Participant selection | |||
|
How were participants selected? e.g. purposive, convenience, consecutive, snowball | 9 | |
|
How were participants approached? e.g. face‐to‐face, telephone, mail, email | 9 | |
|
How many participants were in the study? | 9 | |
|
How many people refused to participate or dropped out? Reasons? | 9 | |
| Setting | |||
|
Where was the data collected? e.g. home, clinic, workplace | 9–10 | |
|
Was anyone else present besides the participants and researchers? | 10 | |
|
What are the important characteristics of the sample? e.g. demographic data, date | Table 1 | |
| Data collection | |||
|
Were questions, prompts, guides provided by the authors? Was it pilot tested? | Appendix A | |
|
Were repeat interviews carried out? If yes, how many? | 10 | |
|
Did the research use audio or visual recording to collect the data? | 10 | |
|
Were field notes made during and/or after the interview or focus group? | ‐ | |
|
What was the duration of the interviews or focus group? | 10 | |
|
Was data saturation discussed? | 10 | |
|
Were transcripts returned to participants for comment and/or correction? | ‐ | |
|
Domain 3: Analysis and findings |
Data analysis | ||
|
How many data coders coded the data? | 11–12 | |
|
Did authors provide a description of the coding tree? | ‐ | |
|
Were themes identified in advance or derived from the data? | 11–12 | |
|
What software, if applicable, was used to manage the data? | 11–12 | |
|
Did participants provide feedback on the findings? | ‐ | |
| Reporting | |||
|
Were participant quotations presented to illustrate the themes/findings? Was each quotation identified? e.g. participant number | 13‐19 | |
|
Was there consistency between the data presented and the findings? | ‐ | |
|
Were major themes clearly presented in the findings? | ‐ | |
|
Is there a description of diverse cases or discussion of minor themes? | ‐ | |
Hansen, S. T. , & Willemoes Rasmussen, L. A. (2022). 'At least there is something in my bra': A qualitative study of women's experiences with oncoplastic breast surgery. Journal of Advanced Nursing, 78, 3304–3319. 10.1111/jan.15309
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions.
REFERENCES
- Arambasic, J. , Sherman, K. A. , & Elder, E. (2019). Attachment styles, self‐compassion, and psychological adjustment in long‐term breast cancer survivors. Psycho‐Oncology, 28(5), 1134–1141. 10.1002/pon.5068 [DOI] [PubMed] [Google Scholar]
- Atisha, D. M. , Rushing, C. N. , Samsa, G. P. , Locklear, T. D. , Cox, C. E. , Shelley Hwang, E. , Zenn, M. R. , Pusic, A. L. , & Abernethy, A. P. (2015). A National Snapshot of satisfaction with breast cancer procedures. Annals of Surgical Oncology, 22(2), 361–369. 10.1245/s10434-014-4246-9 [DOI] [PubMed] [Google Scholar]
- Berry, M. G. , Fitoussi, A. D. , Curnier, A. , Couturaud, B. , & Salmon, R. J. (2010). Oncoplastic breast surgery: A review and systematic approach. Journal of Plastic, Reconstructive and Aesthetic Surgery, 63(8), 1233–1243. 10.1016/j.bjps.2009.05.006 [DOI] [PubMed] [Google Scholar]
- Berterö C., & Chamberlain Wilmoth M. (2007). Breast cancer diagnosis and its treatment affecting the self. Cancer Nursing, 30(3), 194–202. 10.1097/01.ncc.0000270707.80037.4c [DOI] [PubMed] [Google Scholar]
- Boquiren, V. M. , Esplen, M. J. , Wong, J. , Toner, B. , & Warner, E. (2013). Exploring the influence of gender‐role socialization and objectified body consciousness on body image disturbance in breast cancer survivors. Psycho‐Oncology, 22(10), 2177–2185. 10.1002/pon.3271 [DOI] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Braun, V. , & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners (1st ed.). SAGE Publications Ltd. [Google Scholar]
- Brown T., Cruickshank S., & Noblet M. (2021). Specialist breast care nurses for support of women with breast cancer. Cochrane Database of Systematic Reviews, 2021(2). 10.1002/14651858.cd005634.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet, J. , Price, J. , & Harris, C. (2021). Women's preferences for body image programming: A qualitative study to inform future programs targeting women diagnosed with breast cancer. Frontiers in Psychology, 12, 4559. 10.3389/fpsyg.2021.720178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet J., Sabiston C. M., Burke S. (2013). Surviving breast cancer: Women's experiences with their changed bodies. Body Image, 10(3), 344–351. 10.1016/j.bodyim.2013.02.002 [DOI] [PubMed] [Google Scholar]
- Campbell‐Enns, H. J. , Woodgate, R. L. , & Chochinov, H. M. (2017). Barriers to information provision regarding breast cancer and its treatment. Supportive Care in Cancer, 25(10), 3209–3216. 10.1007/s00520-017-3730-8 [DOI] [PubMed] [Google Scholar]
- Carr, T. L. , Groot, G. , Cochran, D. , Vancoughnett, M. , & Holtslander, L. (2019). Exploring Women's support needs after breast reconstruction surgery: A qualitative study. Cancer Nursing, 42(2), E1–E9. 10.1097/NCC.0000000000000600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash, T. F. & Pruzinsky, T. (Eds.) (2022) Body image: A handbook of theory, research, and clinical practice (1st ed.). The Guilford Press. [Google Scholar]
- Collins, K. K. , Liu, Y. , Schootman, M. , Aft, R. , Yan, Y. , Dean, G. , Eilers, M. , & Jeffe, D. B. (2011). Effects of breast cancer surgery and surgical side effects on body image over time. Breast Cancer Research and Treatment, 126(1), 167–176. 10.1007/s10549-010-1077-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crompvoets, S. (2006). Comfort, control, or conformity: Women who choose breast reconstruction following mastectomy. Health Care for Women International, 27(1), 75–93. 10.1080/07399330500377531 [DOI] [PubMed] [Google Scholar]
- Dahl, C. A. F. , Reinertsen, K. V. , Nesvold, I. L. , Fosså, S. D. , & Dahl, A. A. (2010). A study of body image in long‐term breast cancer survivors. Cancer, 116(15), 3549–3557. 10.1002/cncr.25251 [DOI] [PubMed] [Google Scholar]
- Damsgaard, J. B. , Simonÿ, C. , Missel, M. , Beck, M. , & Birkelund, R. (2021). Can patients' narratives in nursing enhance the healing process? Nursing Philosophy, 22(3), e12356. 10.1111/nup.12356 [DOI] [PubMed] [Google Scholar]
- Everaars, K. E. , Welbie, M. , Hummelink, S. , Tjin, E. P. M. , de Laat, E. H. , & Ulrich, D. J. O. (2021). The impact of scars on health‐related quality of life after breast surgery: A qualitative exploration. Journal of Cancer Survivorship: Research and Practice, 15(2), 224–233. 10.1007/s11764-020-00926-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández‐Delgado, J. , López‐Pedraza, M. J. , Blasco, J. A. , Andradas‐Aragones, E. , Sánchez‐Méndez, J. I. , Sordo‐Miralles, G. , & Reza, M. M. (2008). Satisfaction with and psychological impact of immediate and deferred breast reconstruction. Annals of Oncology, 19(8), 1430–1434. 10.1093/annonc/mdn153 [DOI] [PubMed] [Google Scholar]
- Gershfeld Litvin, A. , & Jacoby, R. (2017). Immediate breast reconstruction: Does it restore what was lost? A qualitative study. Illness, Crisis & Loss, 28(2), 141–157. 10.1177/1054137317705876 [DOI] [Google Scholar]
- Gilmour, A. , Cutress, R. , Gandhi, A. , Harcourt, D. , Little, K. , Mansell, J. , Pennery, E. , Tillett, R. , Vidya, R. , & Martin, L. (2021). Oncoplastic breast surgery: A guide to good practice. European Journal of Surgical Oncology, 47, 2272–2285. 10.1016/j.ejso.2021.05.006 [DOI] [PubMed] [Google Scholar]
- Hanna, T. P. , King, W. D. , Thibodeau, S. , Jalink, M. , Paulin, G. A. , Harvey‐Jones, E. , O'Sullivan, D. E. , Booth, C. M. , Sullivan, R. , & Aggarwal, A. (2020). Mortality due to cancer treatment delay: Systematic review and meta‐analysis. BMJ, 371, m4087. 10.1136/bmj.m4087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hau, E. , Browne, L. , Capp, A. , Delaney, G. P. , Fox, C. , Kearsley, J. H. , Millar, E. , Nasser, E. H. , Papadatos, G. , & Graham, P. H. (2013). The impact of breast cosmetic and functional outcomes on quality of life: Long‐term results from the St. George and Wollongong randomized breast boost trial. Breast Cancer Research and Treatment, 139(1), 115–123. 10.1007/s10549-013-2508-z [DOI] [PubMed] [Google Scholar]
- Herring, B. , Paraskeva, N. , Tollow, P. , & Harcourt, D. (2019). Women's initial experiences of their appearance after mastectomy and/or breast reconstruction: A qualitative study. Psycho‐Oncology, 28(10), 2076–2082. 10.1002/pon.5196 [DOI] [PubMed] [Google Scholar]
- Hopwood, P. , & Hopwood, N. (2019a). New challenges in psycho‐oncology: An embodied approach to body image. Psycho‐Oncology, 28(2), 211–218. 10.1002/pon.4936 [DOI] [PubMed] [Google Scholar]
- Jabłoński, M. J. , Mirucka, B. , Streb, J. , Słowik, A. J. , & Jach, R. (2019). Exploring the relationship between the body self and the sense of coherence in women after surgical treatment for breast cancer. Psycho‐Oncology, 28(1), 54–60. 10.1002/pon.4909 [DOI] [PubMed] [Google Scholar]
- Karwacka, W. (2014). Quality assurance in medical translation. The Journal of Specialised Translation, (21), 19–34. [Google Scholar]
- Kim, M. K. , Kim, T. , Moon, H. G. , Jin, U. S. , Kim, K. , Kim, J. , Lee, E. , Yoo, T. K. , Noh, D.‐Y. , Minn, K. W. , & Han, W. (2015). Effect of cosmetic outcome on quality of life after breast cancer surgery. European Journal of Surgical Oncology, 41(3), 426–432. 10.1016/j.ejso.2014.12.002 [DOI] [PubMed] [Google Scholar]
- Liu, L. Q. , Branford, O. A. , & Mehigan, S. (2018). BREAST‐Q measurement of the patient perspective in oncoplastic breast surgery: A systematic review. Plastic and Reconstructive Surgery ‐ Global Open, 6(8), 1–8. 10.1097/GOX.0000000000001904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmillan, R. D. , & McCulley, S. J. (2016). Oncoplastic breast surgery: What, when and for whom? Current Breast Cancer Reports, 8(2), 112–117. 10.1007/s12609-016-0212-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinkovic, M. , Djordjevic, N. , Djordjevic, L. , Ignjatovic, N. , Djordjevic, M. , & Karanikolic, V. (2021). Assessment of the quality of life in breast cancer depending on the surgical treatment. Supportive Care in Cancer, 29(6), 3257–3266. 10.1007/s00520-020-05838-7 [DOI] [PubMed] [Google Scholar]
- Merleau‐Ponty, M. (2011). Phenomenology of perception (1st ed.). Routledge. 10.4324/9780203720714 [DOI] [Google Scholar]
- Negenborn, V. L. , Volders, J. H. , Krekel, N. M. A. , Haloua, M. H. , Bouman, M. B. , Buncamper, M. E. , Niessen, F. B. , Winters, H. A. H. , Terwee, C. B. , Meijer, S. , & van den Tol, M. P. (2017). Breast‐conserving therapy for breast cancer: Cosmetic results and options for delayed reconstruction. Journal of Plastic, Reconstructive and Aesthetic Surgery, 70(10), 1336–1344. 10.1016/j.bjps.2017.05.005 [DOI] [PubMed] [Google Scholar]
- Ozmen, T. , Polat, A. V. , Polat, A. K. , Bonaventura, M. , Johnson, R. , & Soran, A. (2015). Factors affecting cosmesis after breast conserving surgery without oncoplastic techniques in an experienced comprehensive breast center. The Surgeon, 13(3), 139–144. 10.1016/j.surge.2013.12.005 [DOI] [PubMed] [Google Scholar]
- Paraskeva, N. , Herring, B. , Tollow, P. , & Harcourt, D. (2019). First look: A mixed‐methods study exploring women's initial experiences of their appearance after mastectomy and/or breast reconstruction. Journal of Plastic, Reconstructive & Aesthetic Surgery, 72(4), 539–547. 10.1016/j.bjps.2019.01.012 [DOI] [PubMed] [Google Scholar]
- Polit, D. F. , & Beck, C. T. (2018). Essentials of nursing research: Appraising evidence for nursing practice. In Part 3: Designs and methods for quantitative and qualitative nursing research (9th ed.). Lippincott, Williams & Wilkins. [Google Scholar]
- Prades, J. , Remue, E. , van Hoof, E. , & Borras, J. M. (2015). Is it worth reorganising cancer services on the basis of multidisciplinary teams (MDTs)? A systematic review of the objectives and organisation of MDTs and their impact on patient outcomes. Health Policy, 119(4), 464–474. 10.1016/j.healthpol.2014.09.006 [DOI] [PubMed] [Google Scholar]
- Price, B. (1990). Body image: Nursing concepts and care (1st ed.). Prentice Hall. [Google Scholar]
- Retrouvey, H. , Zhong, T. , Gagliardi, A. R. , Baxter, N. N. , & Webster, F. (2019). How patient acceptability affects access to breast reconstruction: A qualitative study. BMJ Open, 9(9), e029048. 10.1136/bmjopen-2019-029048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retrouvey, H. , Zhong, T. , Gagliardi, A. R. , Baxter, N. N. , & Webster, F. (2020). How ineffective Interprofessional collaboration affects delivery of breast reconstruction to breast cancer patients: A qualitative study. Annals of Surgical Oncology, 27(7), 2299–2310. 10.1245/s10434-020-08463-0 [DOI] [PubMed] [Google Scholar]
- Rezaei, M. , Elyasi, F. , Janbabai, G. , Moosazadeh, M. , & Hamzehgardeshi, Z. (2016). Factors influencing body image in women with breast cancer: A comprehensive literature review. Iranian Red Crescent Medical Journal, 18(10), e39465. 10.5812/ircmj.39465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riis, M. (2020). Modern surgical treatment of breast cancer. Annals of Medicine and Surgery, 56(June), 95–107. 10.1016/j.amsu.2020.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizki, H. , Nkonde, C. , Ching, R. C. , Kumiponjera, D. , & Malata, C. M. (2013). Plastic surgical management of the contralateral breast in post‐mastectomy breast reconstruction. International Journal of Surgery, 11(9), 767–772. 10.1016/j.ijsu.2013.06.844 [DOI] [PubMed] [Google Scholar]
- Sand, L. , Olsson, M. , & Strang, P. (2009). Coping strategies in the presence of One's own impending death from cancer. Journal of Pain and Symptom Management, 37(1), 13–22. 10.1016/j.jpainsymman.2008.01.013 [DOI] [PubMed] [Google Scholar]
- Schmid‐Büchi, S. , Halfens, R. J. G. , Dassen, T. , & Van Den Borne, B. (2008). A review of psychosocial needs of breast‐cancer patients and their relatives. Journal of Clinical Nursing, 17(21), 2895–2909. 10.1111/j.1365-2702.2008.02490.x [DOI] [PubMed] [Google Scholar]
- Sebri, V. , Durosini, I. , Triberti, S. , & Pravettoni, G. (2021). The efficacy of psychological intervention on body image in breast cancer patients and survivors: A systematic‐review and meta‐analysis. Frontiers in Psychology, 12, 1–15. 10.3389/fpsyg.2021.611954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman, K. A. , Przezdziecki, A. , Alcorso, J. , Kilby, C. J. , Elder, E. , Boyages, J. , Koelmeyer, L. , & Mackie, H. (2018). Reducing body image‐related distress in women with breast cancer using a structured online writing exercise: Results from the my changed body randomized controlled trial. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 36(19), 1930–1940. 10.1200/JCO.2017.76.3318 [DOI] [PubMed] [Google Scholar]
- Snöbohm, C. , Friedrichsen, M. , & Heiwe, S. (2010). Experiencing one's body after a diagnosis of cancer—A phenomenological study of young adults. Psycho‐Oncology, 19(8), 863–869. 10.1002/pon.1632 [DOI] [PubMed] [Google Scholar]
- Spector, D. , Mayer, D. K. , Knafll, K. , & Pusic, A. (2010). Not what I expected: Informational needs of women undergoing breast surgery. Plastic Surgical Nursing, 30(2), 70–74. 10.1097/PSN.0b013e3181dee9a4 [DOI] [PubMed] [Google Scholar]
- The Danish Breast Cancer Cooperative Group (DBCG) About DBCG. Retrieved November 1, 2021, from https://www.dbcg.dk/about‐dbcg/
- The Ministry of Health [Sundhedsstyrelsen] (2018). Guidelines in Breast Cancer [Pakkeforløb for brystkræft]. Retrived July 5, 2022, from https://www.sst.dk/‐/media/Udgivelser/2018/Brystkraeft/Pakkeforl%C3%B8b‐for‐brystkr%C3%A6ft‐2018.ashx?sc_lang=da&hash=6D281953554BD4472CA64588D45935FD
- Thomas, S. P. (2005). Through the lens of Merleau‐Ponty: Advancing the phenomenological approach to nursing research. Nursing Philosophy, 6(1), 63–76. 10.1111/j.1466-769X.2004.00185.x [DOI] [PubMed] [Google Scholar]
- Todorov, N. , Sherman, K. A. , & Kilby, C. J. (2019). Self‐compassion and hope in the context of body image disturbance and distress in breast cancer survivors. Psycho‐Oncology, 28(10), 2025–2032. 10.1002/pon.5187 [DOI] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Weber, W. P. , Morrow, M. , de Boniface, J. , Pusic, A. , Montagna, G. , Kappos, E. A. , Ritter, M. , Haug, M. , Kurzeder, C. , Saccilotto, R. , Schulz, A. , Benson, J. , Fitzal, F. , Matrai, Z. , Shaw, J. , Peeters, M.‐J. V. , Potter, S. , Heil, J. , & Oncoplastic Breast Consortium Collaborators . (2020). Knowledge gaps in oncoplastic breast surgery. The Lancet Oncology, 21(8), e375–e385. 10.1016/S1470-2045(20)30084-X [DOI] [PubMed] [Google Scholar]
- Wilson, A. R. M. , Marotti, L. , Bianchi, S. , Biganzoli, L. , Claassen, S. , Decker, T. , Frigerio, A. , Goldhirsch, A. , Gustafsson, E. G. , Mansel, R. E. , Orecchia, R. , Ponti, A. , Poortmans, P. , Regitnig, P. , Del Turco, M. R. , Rutgers, E. J. T. , van Asperen, C. , Wells, C. A. , Wengström, Y. , … EUSOMA (European Society of Breast Cancer Specialists . (2013). The requirements of a specialist breast Centre. European Journal of Cancer, 49(17), 3579–3587. 10.1016/j.ejca.2013.07.017 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2021). Breast cancer . Retrieved November 11, 2021, from https://www.who.int/news‐room/fact‐sheets/detail/breast‐cancer
- World Medical Association . (2013). World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


