Abstract
Rape stigma, both external and self‐stigmatization (self‐blame), is associated with adverse health outcomes. Understanding its origins and resilience factors is critical for reducing and preventing it. We describe the prevalence of rape stigma, the characteristics of women experiencing it and the pathways to experiencing greater stigma. The Rape Impact Cohort Evaluation study enrolled 852 women aged 16–40 years who had been raped from post‐rape care centres in Durban, South Africa. We present a descriptive analysis of the baseline data, a multinomial logistic regression model of factors associated with different levels of stigma and a structural equation model (SEM). Most women reported stigmatizing thoughts or experiences, with self‐stigmatizing thoughts being more prevalent than external stigmatization. The multinomial model showed that experiences of childhood or other trauma, emotional intimate partner violence (IPV), having less gender equitable attitudes and food insecurity were significantly associated with medium or high versus low levels of stigma. Internal and external stigma were significantly associated with each other. Women who had been previously raped reported less stigma. The SEM showed a direct path between food insecurity and rape stigma, with poorer women experiencing more stigma. Indirect paths were mediated by more traditional gender attitudes and childhood trauma experience and other trauma exposure. Our findings confirm the intersectionality of rape stigma, with its structural drivers of food insecurity and gender inequality, as well as its strong association with prior trauma exposure. Rape survivors may benefit from gender‐empowering psychological support that addresses blame and shame.
Keywords: gender equality, rape, sexual violence, stigma, structural drivers, violence against women
Key Practitioner Message.
Stigma associated with rape is an important problem that has harmful health consequences.
Its structural drivers include food insecurity, and gender inequality, and it is aggravated by prior trauma exposure.
It may be possible to mitigate impact of rape stigma through including gender‐empowering psychological first aid, addressing issues of blame and stigma, as part of basic care for rape survivors.
It is imperative that professionals and other carers do not perpetuate or perpetrate stigma and blaming and judgemental attitudes.
1. BACKGROUND
Stigma can have a profound impact on people's lives. It is psychologically and socially debilitating and has been argued to both reflect social inequality and to be a vehicle of social control (Parker & Aggleton, 2003). Stigma is an important problem faced by rape survivors (Kennedy et al., 2018; Murray et al., 2018; Verelst et al., 2014). It mirrors, and replicates, prevailing gender inequalities and may be exacerbated by inequality based on socio‐economic status and race (Jackson‐Best & Edwards, 2018). It has two dimensions: external and internal (Goffman, 1963). External stigma expresses perceptions of social devaluation, or discredit, of persons with the stigmatizing condition by others. Internal stigma expresses a devaluation by oneself, through broadly self‐blame and shame. These dimensions are interrelated as externalized stigma may fuel internal stigma, although the relationship is complex (Ullman & Najdowski, 2011). Individuals may experience both internal and external stigma, and they may also find these are overlaid on other co‐occurring stigma experiences, for example, of rape and mental ill health (Jackson‐Best & Edwards, 2018).
Stigma from rape is prevalent globally, but its manifestations vary between settings. Some of the most extreme manifestations are found in settings that generally have more inequitable social norms on gender relations, often in conflict settings. For example, in the Democratic Republic of Congo (DRC), stigma after rape has been a huge problem for survivors of the widespread conflict‐related rape with many women rape survivors being rejected by their husbands, families or communities (Sandilands et al., 2017). One study conducted among women attending a hospital found that a third were rejected by their husband or community (Kelly et al., 2011). In settings where family honour is linked to control of women's bodies, such as in Afghanistan or Palestine, honour killings are an extreme manifestation of externalized stigma (Gibbs et al., 2019). In settings where the status of women is higher, reports of extreme externalized stigma are less common, but women are often still stigmatized and blamed for speaking out against the perpetrators. Most victim/survivors of rape across settings report feelings of self‐blame and shame (i.e., internal stigma).
Apart from its social impacts, stigma adversely affects rape survivors' health. Research shows that the persistence of post‐traumatic stress disorder (PTSD) and depression in the months after the rape is associated with higher levels of stigma (Hakimi et al., 2018; Kohli et al., 2014; Nöthling et al., n.d.). Further, stigma has been found to be a barrier to recovery from depression (Sirey et al., 2001). Understanding the origins of stigma, and the factors that make women more resilient to it, is critical for identifying and providing care for and support to women at risk.
In this paper, we explore the question: What factors are associated with rape stigma overall and in its two dimensions and their interrelationship. We hypothesize that the experience of rape stigma, both internal (self‐blame) and external, may be associated with previous experience of trauma (and possibly stigma), including abuse and neglect in childhood, and previous partner violence or non‐partner rape. We also hypothesize that it may be related to women's own perspectives on gender relations, the extent to which she had social support and her general resilience. Further, we hypothesize that experience of stigma after rape may be related to women's structural power, indicated by her level of education, employment and socio‐economic status.
2. METHODS
2.1. Setting, population and recruitment
A full account of the Rape Impact Cohort Evaluation (RICE) study methods are presented elsewhere (Abrahams et al., 2017). The study was conducted within the surrounds of the city of Durban in the KwaZulu‐Natal (KZN) province, and the RICE study clinic was located on a tertiary hospital premises. We recruited women from five rape service centres after permission was granted by the National and Provincial Departments of Health and the National Prosecuting Authority (NPA). Four of the recruitment sites were Thuthuzela Care Centres (TCCs) located at public health facilities, which provide one‐stop services to rape survivors. The fifth recruitment site was a Crisis Centre also located at a public health hospital and linked to the TCC network of services. All five recruitment sites operated 24 h and provided medico‐legal care, a suite of support and counselling services, as well as legal case management. The study recruiters worked closely with the TCC and Crisis Centre staff to identify potential participants. Inclusion criteria were women aged 16–40 years. Children under 16 years were excluded for ethical reasons. The upper age limit of 40 was chosen because the larger study focused on HIV incidence, which is much lower in women over the age of 40 years. We excluded participants if they were unable to understand the consent process or would have been additionally distressed by it or were more than 14 weeks pregnant. We also excluded women if the first baseline interview and sample collection would have been more than 20 days after the index rape event. We enrolled both HIV‐positive and HIV‐negative participants. Recruiters and/or rape centre staff introduced the study and interested women were invited to attend the RICE clinic where more detailed information was given, and consent procedures occurred. None of the women attended the RICE clinic on the same day as the rape. Transport arrangements were made to bring women to the clinic when they were ready within the 20‐day post‐rape period. The 20‐day post‐rape period was to ensure we captured a baseline assessment of HIV status and acute stress reactions. There was also a control group, described elsewhere (Abrahams et al., 2017). Recruitment started in October 2014 and ended in June 2019. This analysis reports on 852 women survivors of rape.
2.2. Data collection and study procedures
We did interview‐administered data collection at our study site using a web‐based tool (Bryant Systems). Staff were trained to provide a respectful and supportive experience for participants. Interviews were mainly conducted in isiZulu (89.94%), which is the dominant language of the area and reflects the socio‐demographic profile of the study sample.
2.3. Ethics
Ethical approval to conduct the study was obtained from the South African Medical Research Council Ethics Committee (Protocol ID: EC019‐10/2013). We followed a series of consent procedures described in the protocol publication, which included written informed consent from adults and parents of children under 18 and assent from the latter group. The study team included a trauma counsellor who provided immediate psychosocial support to participants, especially those who were identified as needing assistance during the mental health assessments. Participants were referred to counselling services at the rape centres or could choose to return to the study counsellor.
2.4. Measures
The measures included were validated scales and previously used measures. Rape stigma was assessed using a nine‐item scale, based on a modification of a South African AIDS stigma scale (Singh et al., 2011). Six items asked about self‐stigmatization, a typical item was ‘I am embarrassed and ashamed to tell other people about what happened’. Three items asked about external stigma experiences, a typical item was ‘People have avoided talking to me or spending time with me due to the incident’.
Previously used measures captured demographic data, including age, education (primary/secondary/matric and higher), living area (formal urban/informal urban/and rural), employment status and language spoken in the home. We used household food insecurity as a proxy to measure poverty and asked how often people in the home go without food and coded this as never/seldom or sometimes/often. We also asked about intimate relationships: current relationship (not in a relationship, married/cohabiting and dating [not cohabiting]).
Lifetime exposure to intimate partner violence (IPV) was assessed using behavioural specific items, following the WHO's multi‐country study on women's health and domestic violence (Garcia‐Moreno et al., 2006), and previously validated in South Africa (Machisa et al., 2017). Five items measured physical IPV, seven items measured emotional IPV, four items measured economic IPV and four items measured sexual IPV, and responses were never, once, few or many (scored 1–4). The responses were summed and used as a continuous variable in the analyses. We asked about non‐partner rape and attempted rape, and this was based on four questions: forced or persuaded to have sex against will by a non‐partner; forced to have sex by non‐partner when drunk or drugged; gang raped; and attempted rape by a non‐partner. The responses were never, once or more than once (score 1–3) and were summed to generate a score for the measure.
We used a modified version of the Life Events Checklist (LEC) to measure lifetime exposures to 10 forms of trauma (Weathers et al., 2013). We assessed childhood trauma before the age of 18 years using a modified version of the Childhood Trauma Questionnaire Short Form (CTQ‐SF) scale (Bernstein & Fink, 1998). The 14 items measure five subcategories: sexual abuse, physical abuse, emotional abuse, neglect and domestic violence, and responses were measured on a 4‐point Likert scale ranging from 1 ‘never’ to 4 ‘very often’ (Cronbach's alpha = 0.72).
Gender attitudes were measured on a 10‐item scale, with responses on a 4‐point Likert scale (Cronbach's alpha = 0.74). A typical item was ‘I think that if a wife does something wrong her husband has the right to punish her’ (Jewkes et al., 2002). Resilience was measured on a 25‐item scale, also with 4‐point Likert responses (Cronbach's alpha = 0.89), and a typical statement was ‘I feel in control of my life’ (Connor & Davidson, 2003). We used a 12‐item Social Support Appraisal Scale (Vaux et al., 1986), a typical statement was ‘There is a special person who is around when I am in need’, and responses were on a 4‐point Likert scale (Cronbach's alpha = 0.87).
2.5. Analysis
Analyses were performed using Stata 16.0 and MPlus. Some of the psychometric properties of the rape stigma scale were examined. We conducted a principal components analysis and found that the items worked well as one scale with two factors. For the overall scale, the factor loadings ranged from 0.55 to 0.76. Cronbach's alpha was 0.84. Scale items comfortably loaded on two factors, with an eigenvalue of 3.98 for factor 1 and 1.38 for factor 2. The variables corresponded to those items for internal and external stigma. With two factors, a principal components analysis showed the factor loadings for internal stigma to range from 0.55 to 0.76 and those for external to range from 0.42 to 0.58. Cronbach's alpha for the internal stigma subscale was 0.824 and that for the external stigma subscale 0.74. We derived an overall stigma score and scores for internal (six items) and external stigma (three items) by summing the items. The scale overall was also divided into tertiles, referred to as low, medium and high stigma.
We used descriptive statistics to show the distribution of responses to each item of the scale. We used descriptive statistics and bivariate analysis using multinomial logistic regression, with the low stigma category as the reference group, to describe the characteristics of the sample by stigma scale tertile. Then we conducted a multiple regression analysis. We included all the characteristics as independent variables and present the model without elimination of variables.
Using MPlus, we built a structural equation model to assess the interrelationship between the variables that were associated at p < 0.1 with rape stigma in the multinomial logistic regression model. The model outcome variable was the rape stigma as a latent variable. We first allowed the variables to freely correlate in a measurement model and retained those associations that were significantly associated with rape stigma. Then we tested associations by running a full information maximum likelihood method to deal with missing values. To assess model fit of the observed data, we used the comparative fit index (CFI) (>0.95); Tucker–Lewis Index (TLI) (>0.95) as indicative of good fit (Tucker & Lewis, 1973); and root‐mean‐square error of approximation (RMSEA) (of 0.05 or less) (Brown, 2006; Steiger, 1990).
We fitted a structural equation model using full information maximum likelihood estimation (FIML) to model all available data. The final model took into account theorized pathways and used backwards elimination to exclude endogenous variables that did not mediate any path (with significance set at the p < 0.05 level) from the exogenous variables to rape stigma in order to ensure model parsimony. The exception was previous rape, which was retained in the model as a covariate. The model fit was very good (RMSEA 0.006, CFI = 1.000 and TLI = 0.999). The model did not include any error covariances.
3. RESULTS
The cohort had 852 women exposed to rape aged 16–40 years, with a mean age of 25 years (Table 1). They were overwhelmingly isiZulu speaking, many of them had not completed school and only a quarter (26.3%) worked. Most of them were in a relationship (82.1%), but few were married or cohabiting (7.8%). The majority lived in areas of formal housing (72.0%), but 16.4% lived in urban informal settlements. Nearly 1 in 5 (18.9%) sometimes or often went without food due to lack of money.
TABLE 1.
Social and demographic characteristics of the women
| n | %/mean | |
|---|---|---|
| Age (mean) | 852 | 25.0 |
| Zulu‐speaking | 753 | 88.4 |
| Other first language | 99 | 11.6 |
| Education: matric or post‐matric | 484 | 56.8 |
| Did not complete school | 386 | 43.2 |
| Employed | 224 | 26.3 |
| Unemployed | 628 | 73.7 |
| Relationship status | ||
| No relationship | 323 | 18.0 |
| Married or cohabiting | 140 | 7.8 |
| Partner but not cohabiting | 1334 | 74.2 |
| Living area | ||
| Urban–formal | 1279 | 72.0 |
| Urban–informal | 294 | 16.6 |
| Rural | 203 | 11.4 |
| Sometimes or often goes without food | 169 | 18.9 |
| Does not go without food | 683 | 81.1 |
The responses to the items on the rape stigma scale are shown in Table 2. Of the nine questions, six were items related to self‐stigmatization and three assessed external stigma. In respect of external stigma, about half of the women had been blamed for the incident, to the extent that they were expected to have done more to prevent it (50.1%). More than 40% had experienced rude or insensitive remarks, and nearly a third said that they had experienced people avoiding talking to them or spending time with them because of the rape. Internalized stigma was much more common than external stigma, with even the most infrequently endorsed item ‘I feel personally to blame for what happened’ being expressed by more than a third of women (34.3%). All the other items were more commonly endorsed, with only about one in five women indicating that they had not had any feelings of self‐stigma.
TABLE 2.
Descriptive analysis of responses to the rape stigma questions within 20 days of the rape
| Never % (n) | Once % (n) | A few % (n) | Many times % (n) | Principal component factor loading | |
|---|---|---|---|---|---|
| I have been concerned about people respecting me less if they were to find out what happened | 16.7 (142) | 10.2 (87) | 27.9 (237) | 45.2 (384) | 0.6811 |
| I sometimes think people will blame me for what happened | 20.5 (174) | 10.4 (88) | 26.7 (227) | 42.5 (361) | 0.7472 |
| I am embarrassed and ashamed to tell other people about what happened | 19.5 (166) | 8.1 (69) | 22.0 (187) | 50.4 (428) | 0.6867 |
| I think I am now different from other women because of this experience | 35.8 (304) | 8.0 (68) | 24.7 (210) | 31.5 (268) | 0.7594 |
| I feel personally to blame for what happened | 65.7 (558) | 7.3 (62) | 14.7 (125) | 12.4 (105) | 0.5491 |
| My behaviour has changed, and I act as if I am a different person since the incident | 36.6 (311) | 8.8 (75) | 71.4 (221) | 28.6 (243) | 0.71 |
| People have avoided talking to me or spending time with me due to the incident | 69.7 (592) | 6.0 (51) | 14.9 (127) | 9.4 (80) | 0.5796 |
| I have been told that I could have done more to prevent this incident from occurring | 49.9 (424) | 10.1 (86) | 21.9 (186) | 18.1 (154) | 0.6183 |
| People make rude insensitive or inappropriate remarks about my experience | 58.7 (499) | 8.0 (68) | 17.5 (149) | 15.8 (134) | 0.6209 |
The characteristics and experiences of women by tertiles of the stigma scale are presented in Table 3. Women with lower total stigma scores were a little younger, better educated, more likely to be employed and less likely to live in formal housing than those with mid tertile or higher scores, although the differences were small and not statistically significant. Women with higher levels of total stigma were significantly more likely to be food insecure and, compared to the lowest tertile, were more likely to have low levels of social support. Women with higher exposure to stigma had been more exposed to IPV in the past. Exposure to physical, emotional, economic and sexual IPV were more common among women with the highest stigma compared to the lowest level (p < 0.05 for all except sexual IPV where p = 0.07). Exposure to more childhood neglect and abuse, and other trauma were both associated with greater levels of stigmatization. There was some evidence (p = 0.07) that having more equitable gender attitudes was protective against very high (vs. low) levels of stigma.
TABLE 3.
Characteristics and experiences of the women by tertiles of the stigma scale
| Bivariable multinomial logistic regression, base = low | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Low | Mid | High | Mid vs. low | High vs. low | |||||
| Mean/% | Mean/% | Mean/% | RRR | 95% CI | p value | RRR | 95% CI | p value | |
| Age (mean) | 24.8 | 25.1 | 25.1 | 0.008 | −0.022, 0.038 | 0.583 | 0.008 | −0.025, 0.042 | 0.629 |
| Education: matric or post‐matric | 59.9 | 57.7 | 51.8 | 0.92 | 0.66, 1.27 | 0.595 | 0.72 | 0.50, 1.04 | 0.077 |
| Employed | 28.2 | 26.6 | 23.9 | 0.92 | 0.65, 1.32 | 0.652 | 0.80 | 0.53, 1.20 | 0.284 |
| Living area | |||||||||
| Urban–formal | 60.9 | 68.0 | 65.0 | 1.00 | 1.00 | ||||
| Urban–informal | 21.9 | 19.5 | 19.4 | 0.80 | 0.53, 1.19 | 0.272 | 0.83 | 0.52, 1.31 | 0.427 |
| Rural | 17.2 | 12.6 | 15.7 | 0.66 | 0.42, 1.04 | 0.074 | 0.85 | 0.52, 1.41 | 0.541 |
| Sometimes or often goes without food | 14.7 | 18.2 | 29.0 | 1.29 | 0.84, 1.99 | 0.25 | 2.37 | 1.51, 3.72 | <0.0001 |
| Relationship status | |||||||||
| No relationship | 21.6 | 19.0 | 24.3 | 1.00 | 1.00 | ||||
| Married or cohabiting | 6.6 | 8.7 | 8.1 | 1.51 | 0.76, 2.99 | 0.242 | 1.10 | 0.51, 2.35 | 0.81 |
| Partner but not cohabiting | 71.8 | 72.4 | 67.6 | 1.15 | 0.77, 1.71 | 0.496 | 0.84 | 0.54, 1.29 | 0.417 |
| Low social support scale | 24.7 | 25.7 | 26.0 | 1.04 | 1.01, 1.07 | 0.015 | 1.050 | 1.01, 1.09 | 0.006 |
| IPV | |||||||||
| Emotional IPV score | 9.8 | 10.7 | 40.2 | 1.04 | 1.00, 1.07 | 0.037 | 1.07 | 1.03, 1.11 | <0.0001 |
| Economic IPV score | 4.6 | 4.8 | 19.4 | 1.05 | 0.962, 1.15 | 0.261 | 1.13 | 1.03, 1.24 | 0.008 |
| Physical IPV score | 7.4 | 7.7 | 27.4 | 1.02 | 0.97, 1.06 | 0.456 | 1.06 | 1.01, 1.10 | 0.013 |
| Sexual IPV score | 4.8 | 4.8 | 19.4 | 1.000 | −0.086, 0.077 | 0.911 | 1.08 | 0.99, 1.17 | 0.07 |
| Child abuse | 15.6 | 16.9 | 17.7 | 1.160 | 1.09, 1.24 | <0.0001 | 1.210 | 1.14, 1.30 | <0.0001 |
| Prior exposure to trauma | 1.7 | 2.2 | 2.2 | 1.160 | 1.06, 1.28 | 0.002 | 1.180 | 1.06, 1.31 | 0.002 |
| Non‐partner sexual violence score | 4.5 | 4.5 | 4.7 | 0.990 | 0.85, 1.17 | 0.926 | 1.120 | 0.95, 1.32 | 0.173 |
| Gender attitudes (high = progressive) | 29.6 | 29.1 | 29 | 0.970 | 0.93, 1.01 | 0.133 | 0.95 | 0.91, 1.00 | 0.069 |
The multiple regression model of factors associated with rape stigma is presented in Table 4. It shows that the risk of stigma (internal and external) associated with rape was elevated among women with food insecurity (proxy for poverty) and childhood trauma exposure. The risk was lower among those with more equitable gender attitudes, and there was a suggestion that it may have been lower among women who had experienced sexual IPV (p = 0.08).
TABLE 4.
Multiple regression model of factors associated with rape stigma
| Full stigma scale | Internal stigma subscale | External stigma subscale | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95% CI | p value | Coef. | 95% CI | p value | Coef. | 95% CI | p value | |
| Age | −0.019 | −0.115, 0.077 | 0.701 | 0.036 | −0.068, 0.074 | 0.929 | −0.022 | −0.061, 0.017 | 0.266 |
| No relationship | 0.000 | 0.000 | 0.000 | ||||||
| Married or cohabiting | −0.435 | −2.437, 1.566 | 0.669 | 0.582 | −0.903, 2.067 | 0.442 | −1.018 | −1.826, −0.209 | 0.014 |
| Partner but not cohabiting | −0.295 | −1.521, 0.930 | 0.636 | 0.122 | −0.787, 1.031 | 0.792 | −0.417 | −0.912, 0.078 | 0.098 |
| Educated to matric or beyond | −0.304 | −1.307, 0.700 | 0.552 | 0.091 | −0.654, 0.835 | 0.811 | −0.395 | −0.800, 0.011 | 0.056 |
| Employed | −0.096 | −1.200, 1.008 | 0.865 | −0.139 | −0.958, 0.680 | 0.739 | 0.043 | −0.403, 0.490 | 0.849 |
| Lives in formal area | 0.000 | 0.000 | 0.000 | ||||||
| Informal settlement | −0.744 | −1.932, 0.443 | 0.219 | −0.660 | −1.541, 0.221 | 0.142 | −0.084 | −0.564, 0.396 | 0.73 |
| Rural area | −0.401 | −1.746, 0.944 | 0.558 | −0.560 | −1.558, 0.438 | 0.271 | 0.159 | −0.384, 0.702 | 0.566 |
| Often or sometimes has no food | 1.972 | 0.780, 3.164 | 0.001 | 1.240 | 0.355, 2.124 | 0.006 | 0.732 | 0.250, 1.213 | 0.003 |
| Social support score (high = low support) | 0.064 | −0.031, 0.160 | 0.185 | 0.061 | −0.010, 0.132 | 0.09 | 0.003 | −0.035, 0.042 | 0.869 |
| Emotional IPV score | 0.091 | −0.056, 0.238 | 0.226 | 0.055 | −0.054, 0.164 | 0.324 | 0.036 | −0.023, 0.096 | 0.235 |
| Economic IPV score | −0.014 | −0.269, 0.241 | 0.914 | −0.038 | −0.227, 0.151 | 0.694 | 0.024 | −0.079, 0.127 | 0.650 |
| Physical IPV score | 0.042 | −0.132, 0.217 | 0.634 | 0.047 | −0.083, 0.177 | 0.476 | −0.005 | −0.075, 0.066 | 0.895 |
| Sexual IPV score | −0.222 | −0.472, 0.029 | 0.083 | −0.134 | −0.319, 0.052 | 0.158 | −0.088 | −0.189, 0.013 | 0.089 |
| Childhood trauma score | 0.332 | 0.198, 0.466 | <0.0001 | 0.260 | 0.160, 0.359 | <0.0001 | 0.072 | 0.018, 0.126 | 0.009 |
| Trauma score | 0.201 | −0.074, 0.475 | 0.152 | 0.191 | −0.013, 0.395 | 0.066 | 0.010 | −0.101, 0.121 | 0.863 |
| Non‐partner rape score | −0.069 | −0.546, 0.409 | 0.778 | −0.264 | −0.618, 0.091 | 0.145 | 0.195 | 0.002, 0.388 | 0.048 |
| Gender attitudes (high = more progressive) | −0.217 | −0.352, −0.081 | 0.002 | −0.135 | −0.235, −0.034 | 0.009 | −0.082 | −0.137, −0.027 | 0.003 |
The factors associated with internal stigma are also presented. Internal stigma was positively associated with food insecurity and childhood trauma and negatively associated with having gender equitable attitudes. External stigma was positively associated with exposure to childhood trauma, food insecurity and having previously experienced non‐partner rape. There was a lower likelihood of it among those who were married or cohabiting, better educated and with more equitable ideas about gender.
In a further analysis, we considered whether external stigma may be a driver of internal stigma and vice versa. We found these to be very strongly associated. With internal stigma as the outcome and external stigma as an independent variable, the coefficient for the association was 0.41 (95% CI 0.35, 0.47), p < 0.0001. With external stigma as the outcome and internal stigma as an independent variable, the coefficient was 0.43 (95% CI 0.37, 0.50), p < 0.0001. In the latter analysis, there was no evidence of confounding between internal stigma and the other variables associated with external stigma. However, in the model with internal stigma as the outcome, there was significant confounding between external stigma and other independent variables. Only two variables, experience of childhood trauma (a risk) and experience of prior non‐partner rape (a protective factor), in addition to external stigma, were statistically significantly associated with internal stigma.
The results for the structural equation model of pathways to stigma are presented in Figure 1 and Table 5. There was a direct path to rape stigma from food insecurity, such that having greater food insecurity elevated the risk of rape stigma. There was an indirect path from food insecurity to rape stigma mediated by gender attitudes, with the direction of effect indicating that when mediated by less traditional gender attitudes, levels of stigma were likely to be lower. There was also an indirect path from food insecurity to rape stigma mediated by childhood trauma, with the direction of effect increasing rape stigma risk with elevated childhood trauma exposure. There was also a path from food insecurity to rape stigma mediated by both childhood trauma and gender attitudes. The direction of the effect indicates that more food insecure women had more childhood trauma and more gender inequitable attitudes, and this increased the likelihood of having more rape stigma. There was also a pathway from other trauma to rape stigma mediated by childhood trauma and exposure to other trauma, with the direction of effect indicating that greater trauma exposure was associated with more rape stigma. During model building, we examined the variable for previous non‐partner rape, but the path to rape stigma was not statistically significant and the model fit less good than the one we present.
FIGURE 1.
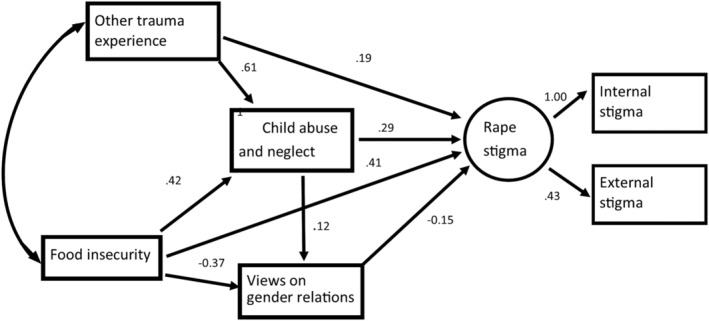
Final structural model of paths to rape stigma
TABLE 5.
Rape stigma SEM: Direct effects and equation‐level goodness of fit
| Unstandardized coef. (95% CI) | Standardized coef. (95% CI) | p value | |
|---|---|---|---|
| Paths | |||
| Childhood abuse and neglect → rape stigma | 0.19 (0.29, 0.38) | 0.19 (0.27, 0.35) | <0.001 |
| Food insecurity → rape stigma | 0.04 (0.41, 0.78) | 0.01 (0.09, 0.16) | 0.03 |
| Equitable gender attitudes → rape stigma | −0.24 (−0.15, 0.06) | −0.21 (−0.14, 0.06) | 0.001 |
| Other traumatic experiences → rape stigma | 0.02 (0.19, 0.37) | 0.01 (0.09, 0.17) | 0.033 |
| Food insecurity → childhood abuse and neglect | 0.10 (0.49, 0.87) | 0.03 (0.11, 0.19) | 0.014 |
| Childhood abuse and neglect → other traumatic experiences | 0.10 (0.14, 0.18) | 0.22 (0.29, 0.37) | <0.001 |
| Childhood abuse and neglect → equitable gender attitudes | 0.05 (0.12, 0.18) | 0.05 (0.12, 0.2) | 0.001 |
| Food insecurity → equitable gender attitudes | −0.65 (−0.37, 0.09) | −0.15 (−0.09, 0.02) | 0.009 |
| Variances | |||
| Other traumatic experiences | 2.68 (3.02, 3.35) | 0.87 (0.91, 0.96) | <0.001 |
| Equitable gender attitudes | 11.38 (12.65, 13.92) | 0.96 (0.98, 1) | <0.001 |
| Childhood abuse and neglect | 10.97 (14.62, 18.27) | 0.97 (0.99, 1.01) | <0.001 |
| Internal rape stigma | 5.26 (10.09, 14.92) | 0.2 (0.38, 0.56) | <0.001 |
| External rape stigma | 3.75 (4.72, 5.68) | 0.48 (0.61, 0.73) | <0.001 |
| Rape stigma | 9.67 (14.45, 19.23) | 0.83 (0.88, 0.93) | <0.001 |
| Equation‐level goodness of fit | R 2 | ||
| Other traumatic experiences | 0.086 | ||
| Equitable gender attitudes | 0.021 | ||
| Childhood abuse and neglect | 0.012 | ||
| Internal rape stigma | 0.619 | ||
| External rape stigma | 0.393 | ||
| Rape stigma | 0.118 | ||
4. DISCUSSION
We have shown that stigma post‐rape is most often experienced by poorer women and is integrally linked to their views on gender relations as well as their previous experience of trauma, particularly trauma experienced in childhood. It is also associated with experience of IPV. This provides further evidence to support the argument that stigma reflects social inequalities (Parker & Aggleton, 2003). We have also shown that internal and external stigma are distinct but overlapping and appear to drive each other.
Poorer women report higher levels of childhood trauma exposure (Gibbs et al., 2018). The long‐term consequences of childhood trauma include low self‐esteem, depression and low self‐compassion, otherwise a greater likelihood of internalizing self‐blame and shame (i.e., self‐stigmatize) in the face of rape (Boyraz et al., 2019). Women who had previously experienced rape were more vulnerable to external stigma, which may be due to prior experiences from the first rape, or fear of compassion fatigue in their social network. However, they were less vulnerable to internal stigma, and this was particularly visible in the final model of internal stigma adjusting for experience of external stigma. Our findings show that external experiences of stigma impact on how a survivor sees herself (self‐blame), a more surprising finding was that internalized stigma was associated with reporting more external stigma. It may be that survivors who blame themselves expect others to do so too, potentially altering how they perceive others behave towards them.
The strong association between both forms of stigma and women having more gender inequitable ideas highlights the intersectionality of rape stigma and gender inequality as well as women's internalization of societal views that they are responsible for the rape. They may perceive their social network to hold the same unequal gender views and therefore fear external stigma. Women who were married and better educated perceived less external stigma. These two attributes (education and marriage) are often regarded as indicators of higher social status and power, particularly in South Africa (Jewkes & Morrell, 2010). Therefore, this finding, together with the evidence pointing to vulnerability among women with low socio‐economic status and levels of social support, suggests that the social position of women is strongly associated with vulnerability to external stigma.
These findings have important implications for service provision. Whilst we recognize that all survivors need support after rape, our findings have shown that some women are more vulnerable to stigma after rape and so may need more support. People who are tasked with providing services to rape survivors such as health workers, police and actors in the legal system may enact external stigma against survivors, for example, by implying they were to blame for the rape. We need to eradicate this from our services. Although changing gender attitudes can be a long‐term process, the evidence of a protective effect of holding more progressive gender attitudes warrants attention. This supports a view that part of the psychological assistance women require after rape involves specifically addressing ideas around gender equality and a shift from self‐blame to appropriate blame of the perpetrator. There are questions about how this might be delivered, apart from being incorporated into the messages and discussions with rape survivors in the initial stages of interaction with health or social care.
Although some survivors are more resilient and seem not to need further treatment, many survivors need interventions to reduce stigma and treat PTSD and depression, as stigma drives PTSD and depression, hinders healing and recovery, and exacerbates feelings of self‐blame and shame (Nöthling et al., n.d.). Although interventions focused on reducing internalized stigma are nascent, there is promising evidence in support of psychoeducation (such as addressing gender equity and rape myths in post‐rape counselling) and cognitive–behavioural interventions to modify self‐stigmatizing beliefs (Alonso et al., 2019). Apart from the potential impact on internalized stigma, cognitive interventions may also address the underlying factors that increase risk of rape stigma, namely, childhood trauma (Thomas et al., 2020). Apart from reducing stigma, there is also good evidence to support the use of cognitive–behavioural therapy/cognitive processing therapy (CBT/CPT) interventions in rape survivors, and trauma‐focused CBT interventions (CBT/CPT) have been shown to accelerate recovery in rape survivors who have acute stress disorder (ASD) (Lomax & Meyrick, 2020). Reduced rape stigma has been described as an outcome of CPT provided to rape survivors with ASD in high‐income countries (Resick et al., 2002). Research in the DRC shows promise in addressing rape stigma through group CPT administered by lay workers (Murray et al., 2018). There is also evidence of self‐help plus and a growing range of other therapies being useful in reducing mental distress among rape survivors, and these could be potentially adapted to low‐ and middle‐income settings. These therapies are not very accessible to rape survivors in the public sector in most low‐ and middle‐income countries, but given the global nature of the problem of rape, this is a challenge for health sector development that must be addressed.
4.1. Strengths and limitations
RICE is the first study of a large sample of women that focused on the health burden associated with rape in a low‐ or middle‐income country. Its strengths are that the cohort had a large sample of women survivors of rape who were recruited and interviewed within 3 weeks of the rape. Women were interviewed under standardized, private, supportive conditions at the research site. Measures had been previously used and validated with other populations. Although this paper presents cross‐sectional data of the cohort of rape survivors, other analyses from the study have shown the predictive power of the measure of rape stigma at baseline.
Our study has limitations. It was a volunteer sample and not necessarily representative of the total population of women experiencing rape in the age group in the metropolitan recruitment area or other parts of the country. We did not include non‐vaginal forms of rape (anal/oral), male victims or children under the age of 16 years. The stigma measure was relatively short (nine items), and six of these measured self‐stigmatization. Further, the stigma questions analysed were reports within 20 days of the rape, and it is possible that some women may have experienced stigma after this time. All trauma reports may be subject to under‐reporting.
This study only focused on stigma associated with rape, but it is recognized that individuals may experience various types of intersecting stigma. In this sample, for example, many of the women had HIV, mental ill health and were particularly poor. We did not measure the stigma associated with these factors, but it is likely that this population would also be experiencing some or all of these. We have shown in this analysis that limited power and experience of inequality were potent drivers of stigma for rape, and this points to the intersection of stigma with disempowerment. We did consider whether pre‐existing experiences of stigma might inform the degree to which the women anticipated stigma from others and in the absence of other measures tested an association with HIV status, but we did not show an association or that HIV status was a confounder (data not shown) (Jackson‐Best & Edwards, 2018).
5. CONCLUSION
Stigma associated with rape is an important problem, with internal and external elements, that has been shown to be associated with harmful health consequences. We have shown its associations with structural drivers of food insecurity, and gender inequality, and that it is aggravated by prior trauma exposure, including in childhood. Our findings suggest that it may be possible to mitigate some of the severe impact of rape stigma through including gender‐empowering psychological first aid, addressing issues of blame and stigma, as part of basic care for rape survivors. It is imperative that healthcare providers and others dealing with rape survivors do not perpetuate or perpetrate stigma and blaming and judgemental attitudes.
CONFLICT OF INTERESTS
None.
AUTHOR CONTRIBUTIONS
R. J. conceptualized the paper, analysed the data and wrote the first draft; N. A. was the principal investigator of the RICE study and co‐wrote the paper; S. M. and E. C. were the main RICE statisticians and confirmed the data analysis and its description; and B. M., N. P., S. S., C. G.‐M. and K. D. contributed to manuscript drafts. C. G.‐M. is a staff member of the World Health Organization. The views expressed are her own and do not necessarily reflect the views or policies of the WHO.
ACKNOWLEDGEMENTS
This research and the publication thereof is the result of funding provided by the South African Medical Research Council in terms of the SAMRC's Flagships Awards Project ‘SAMRC‐RFA‐IFSP‐01‐2013/RAPE COHORT’. We are very grateful to the participants in the RICE study for sharing their time and intimate experiences with the study team. We thank all the staff who worked to make the study possible. We also thank Pierre Smith from the National Prosecuting Authority SOCA Unit for giving us access to the TCCs for recruitment.
Jewkes, R. , Mhlongo, S. , Chirwa, E. , Seedat, S. , Myers, B. , Peer, N. , Garcia‐Moreno, C. , Dunkle, K. , & Abrahams, N. (2022). Pathways to and factors associated with rape stigma experienced by rape survivors in South Africa: Analysis of baseline data from a rape cohort. Clinical Psychology & Psychotherapy, 29(1), 328–338. 10.1002/cpp.2637
Funding information South African Medical Research Council
DATA AVAILABILITY STATEMENT
The data used in this paper are available on request to the corresponding author. Data are available on request only as it is a longitudinal data set that has not been fully analysed by investigators.
REFERENCES
- Abrahams, N. , Seedat, S. , Lombard, C. , Kengne, A. P. , Myers, B. , Sewnath, A. , Mhlongo, S. , Ramjee, G. , Peer, N. , Garcia‐Moreno, C. , & Jewkes, R. (2017). Study protocol for a longitudinal study evaluating the impact of rape on women's health and their use of health services in South Africa. BMJ Open, 7(9), e017296. 10.1136/bmjopen-2017-017296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso M, Guillén AI, & Muñoz, M . (2019). Interventions to reduce internalized stigma in individuals with mental illness: A systematic review. The Spanish Journal of Psychology, 22, E27. 10.1017/sjp.2019.9. PMID: 31084665. [DOI] [PubMed] [Google Scholar]
- Bernstein, D. P. , & Fink, L. (1998). Childhood trauma questionnaire: A retrospective self‐report: Manual. Psychological Corporation. [Google Scholar]
- Boyraz, G. , Ferguson, A. N. , Zaken, M. D. , Baptiste, B. L. , & Kassin, C. (2019). Do dialectical self‐beliefs moderate the indirect effect of betrayal traumas on posttraumatic stress through self‐compassion? Child Abuse & Neglect, 96, 104075. 10.1016/j.chiabu.2019.104075 [DOI] [PubMed] [Google Scholar]
- Brown, T. (2006). Confirmatory factor analysis for applied research. New York: Guilford Press. [Google Scholar]
- Connor, K. M. , & Davidson, J. (2003). Development of a new resilience scale: The Connor‐Davidson Resilience Scale (Cd‐Risc). Depression and Anxiety, 18, 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Garcia‐Moreno, C. , Jansen, H. A. , Ellsberg, M. , Heise, L. , & Watts, C. H. (2006). Prevalence of intimate partner violence: Findings from the WHO multi‐country study on women's health and domestic violence. Lancet, 368(9543), 1260–1269. 10.1016/s0140-6736(06)69523-8 [DOI] [PubMed] [Google Scholar]
- Gibbs, A. , Jewkes, R. , Willan, S. , & Washington, L. (2018). Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18‐30) women and men in urban informal settlements in South Africa: A cross‐sectional study and structural equation model. PLoS ONE, 13(10), e0204956. 10.1371/journal.pone.0204956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs, A. , Said, N. , Corboz, J. , & Jewkes, R. (2019). Factors associated with ‘honour killing’ in Afghanistan and the occupied Palestinian Territories: Two cross‐sectional studies. PLoS ONE, 14(8), e0219125. 10.1136/bmjgh-2019-001946, e001946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster Inc. [Google Scholar]
- Hakimi, D. , Bryant‐Davis, T. , Ullman, S. E. , & Gobin, R. (2018). Relationship between negative social reactions to sexual assault disclosure and mental health outcomes of ethnically diverse female survivors. Psychological Trauma, 10, 270–275. 10.1037/tra0000245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson‐Best, F. , & Edwards, N. (2018). Stigma and intersectionality: A systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health, 18, 919. 10.1186/s12889-018-5861-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes, R. , Levin, J. , & Penn‐Kekana, L. (2002). Risk factors for domestic violence: Findings from a South African cross‐sectional study. Social Science & Medicine, 55(9), 1603–1617. 10.1016/S0277-9536(01)00294-5 [DOI] [PubMed] [Google Scholar]
- Jewkes, R. , & Morrell, R. (2010). Gender and sexuality: Emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. Journal of the International AIDS Society, 13(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, J. T. , Betancourt, T. S. , Mukwege, D. , Lipton, R. I. , & Vanrooyen, M. (2011). Experiences of female survivors of sexual violence in eastern Democratic Republic of the Congo: A mixed‐methods study. Conflict and Health, 5, 25. 10.1186/1752-1505-5-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy, A. C. , Prock, K. A. , Albutt, K. , Kelly, J. , Kabanga, J. , & VanRooyen, M. (2018). “I still feel like I am not normal”: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence stigmatisation and rejection of survivors of sexual violence in eastern Democratic Republic of the Congo. Trauma Violence Abuse, 19(5), 512–527. 10.3389/fpsyg.2017.00192 [DOI] [PubMed] [Google Scholar]
- Kohli, A. , Perrin, N. A. , Mpanano, R. M. , Mullany, L. C. , Murhula, C. M. , Binkurhorhwa, A. K. , Mirindi, A. B. , Banywesize, J. H. , Bufole, N. M. , Ntwali, E. M. , & Glass, N. (2014). Risk for family rejection and associated mental health outcomes among conflict‐affected adult women living in rural eastern Democratic Republic of the Congo. Health Care for Women International, 35, 789–807. 10.1080/07399332.2014.903953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lomax, J. , & Meyrick, J. (2020). Systematic review: Effectiveness of psychosocial interventions on wellbeing outcomes for adolescent or adult victim/survivors of recent rape or sexual assault. Journal of Health Psychology, 1359105320950799, 135910532095079. 10.1177/1359105320950799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machisa, M. T. , Christofides, N. , & Jewkes, R. (2017). Mental ill health in structural pathways to women's experiences of intimate partner violence. PLoS ONE, 12(4), e0175240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, S. M. , Augustinavicius, J. , Kaysen, D. , Rao, D. , Murray, L. K. , Wachter, K. , … Bass, J. K. (2018). The impact of cognitive processing therapy on stigma among survivors of sexual violence in eastern Democratic Republic of Congo: Results from a cluster randomized controlled trial. Conflict and Health, 12, 1. 10.1136/bmjopen-2017-016560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nöthling J, Abrahams N, Jewkes R, Mhlongo S, Lombard C, Hemmings S, & Seedat, S (n.d.). Risk and protective factors affecting the symptom trajectory of PTSD post‐rape. [DOI] [PubMed]
- Parker, R. , & Aggleton, P. (2003). HIV‐ and AIDS‐related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine, 57, 13–24. 10.1016/S0277-9536(02)00304-0 [DOI] [PubMed] [Google Scholar]
- Resick, P. A. , Nishith, P. , Weaver, T. L. , Astin, M. C. , & Feuer, C. (2002). A comparison of cognitive‐processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70, 867–879. 10.1037/0022-006X.70.4.867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandilands M, Jewkes R, Baguma Lele U, & Scott, N . (2017). Faith engagement, gender norms and violence against women and girls in conflict‐affected communities: Baseline research in Ituri Province, Democratic Republic of Congo. What Works to Prevent Violence Against Women and Girls Project. Retrieved from London.
- Singh, D. , Chaudoir, S. R. , Escobar, M. C. , & Kalichman, S. (2011). Stigma, burden, social support, and willingness to care among caregivers of PLWHA in home‐based care in South Africa. AIDS Care, 23(7), 839–845. 10.1080/09540121.2010.542122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirey, J. A. , Bruce, M. L. , Alexopoulos, G. S. , Perlick, D. A. , Friedman, S. J. , & Meyers, B. (2001). Stigma as a barrier to recovery: Perceived stigma and patient‐rated severity of illness as predictors of antidepressant drug adherence. Psychiatric Services, 52, 1615–1620. 10.1176/appi.ps.52.12.1615 [DOI] [PubMed] [Google Scholar]
- Steiger, J. (1990). Structural model equation and modification: An interval estimation approach. Multivariate Behavioral Research, 25(173–80), 173–180. 10.1207/s15327906mbr2502_4 [DOI] [PubMed] [Google Scholar]
- Thomas, F. C. , Puente‐Duran, S. , Mutschler, C. , & Monson, C. (2020). Trauma‐focused cognitive behavioral therapy for children and youth in low and middle‐income countries: A systematic review. Child and Adolescent Mental Health. 10.1111/camh.12435 [DOI] [PubMed] [Google Scholar]
- Tucker, L. R. , & Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1–10. 10.1007/BF02291170 [DOI] [Google Scholar]
- Ullman, S. E. , & Najdowski, C. J. (2011). Prospective changes in attributions of self‐blame and social reactions to women's disclosures of adult sexual assault. Journal of Interpersonal Violence, 26, 1934–1962. 10.1177/0886260510372940 [DOI] [PubMed] [Google Scholar]
- Vaux, A. , Phillips, J. , Holly, L. , Thomson, B. , Williams, D. , & Stewart, D. (1986). The social support appraisals (SS‐A) scale: Studies of reliability and validity. American Journal of Community Psychiatry, 14(2), 195–219. 10.1007/BF00911821 [DOI] [Google Scholar]
- Verelst, A. , De Schryver, M. , De Haene, L. , Broekaert, E. , & Derluyn, I. (2014). The mediating role of stigmatization in the mental health of adolescent victims of sexual violence in Eastern Congo. Child Abuse & Neglect, 38(7), 1139–1146. 10.1016/j.chiabu.2014.04.003 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane, T . (2013). The Life Events Checklist for DSM‐5 (LEC‐5)—Interview [measurement instrument]. https://www.ptsd.va.gov
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this paper are available on request to the corresponding author. Data are available on request only as it is a longitudinal data set that has not been fully analysed by investigators.


