Abstract
Background
Obesity is associated with the development of knee osteoarthritis (OA). The aim of this study was to examine the incidence of obesity in patients undergoing knee replacement (KR) for OA in Australia compared to the incidence of obesity in the general population.
Methods
A cohort study was conducted, comparing data from the Australian Bureau of Statistics (ABS) 2017–2018 National Health Survey with data from the National Joint Replacement Registry. The distribution of patients who underwent KR from July 2017 to June 2018 by BMI category was compared to the distribution of the general population, in age and gender sub‐groups.
Results
During the study period, 35.6% of Australian adults were overweight and 31.3% were obese. Of the 56 217 patients who underwent primary KR for OA, 31.9% were overweight and 57.7% were obese. The relative risk of undergoing KR for OA increased with increasing BMI category. Class 1, 2 and 3 obese females aged 55–64 years were 4.7, 8.4 and 17.3 times more likely to undergo KR than their normal weight counterparts, respectively. Males in the same age and BMI categories were 3.4, 4.5 and 5.8 times more likely to undergo KR, respectively. Class 3 obese patients underwent KR 7 years younger, on average, than normal weight individuals.
Conclusion
Obesity is associated with an increased risk of undergoing KR, and at a younger age, particularly for females. There is an urgent need for a societal level approach to address the prevalence of obesity, to reduce the burden of obesity related KR.
Keywords: knee osteoarthritis, knee replacement, obesity
Obesity markedly increases the risk of Australian adults undergoing knee replacement (KR), and is associated with the procedure being performed at a younger age. There is an urgent need for a societal level approach to address the prevalence of obesity, in order to reduce the burden of obesity related knee osteoarthritis and subsequent KR.
Introduction
Osteoarthritis (OA) is a common cause of pain and disability that places a significant psychosocial burden on patients and a large financial burden on healthcare systems. 1 Over 300 million people worldwide suffer from hip and knee OA, and both the incidence and prevalence of OA is increasing. 2 Approximately 2.2 million Australians (9.3%) are affected by OA, 3 and this figure is expected to increase to 3.1 million by 2030. 4 At a global level, OA accounts for an estimated 9.6 million years lived with disability (YLD), and this figure is increasing. 2 Knee OA is more prevalent than hip OA, and accounts for more YLD. 5
Obesity is a known risk factor for the development of knee OA and the subsequent need for knee replacement (KR). 6 , 7 , 8 The global prevalence of obesity has increased dramatically in recent decades. Estimates suggested that 6.4% of women and 3.2% of men worldwide were obese in 1975. 9 These figures had increased to 14.9% and 10.8%, respectively, by 2014. According to the World Health Organization (WHO), over 650 million adults were obese worldwide in 2016. 10 In Australia, nearly a third of adults are obese. 3
KR is a reliable and cost‐effective treatment option for patients with end‐stage knee OA where non‐operative management has failed. 11 Over 57 000 primary KR procedures were performed in Australia in 2019, representing an increase of 161% since 2003. 12 The annual incidence of KR is projected to exceed 161 000 procedures by 2030. 13
The healthcare costs associated with OA are substantial. In 2015, Australia spent over 2.1 billion dollars (AUD) managing OA, and this figure is projected to exceed 2.9 billion AUD by 2030. 4 A large proportion of these costs is associated with joint replacement. 1
The aims of this study were to examine the incidence of obesity in patients undergoing primary KR for OA in Australia compared to the incidence of obesity in the general population, and to investigate the mean age at which patients undergo KR in Australia, depending on their BMI category.
Methods
A cohort study was performed, using data from the 2017–2018 National Health Survey and the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR).
The 2017–2018 National Health Survey was conducted by the Australian Bureau of Statistics (ABS) from July 2017 to June 2018. 3 A random sample of 21 544 private dwellings were approached across urban and rural areas in all states and territories of Australia. A response rate of 76.1% was achieved, representing 21 315 persons across 16 384 households.
Height and weight measurements were collected by trained ABS interviewers, and BMI was calculated by dividing weight in kilograms by height in metres squared. Patients were classified by BMI according to the WHO classification. 14 There was a non‐response rate for these measurements of 33.8% for persons aged ≥18 years, and missing values were imputed using a hot decking method. 3
Publicly available data on the estimated number of persons in Australia in each BMI category by age and gender were obtained from the ABS website. 15 Age categories utilized in this study were 18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84 and ≥85 years.
The AOANJRR commenced data collection for KR procedures in September 1999, achieving complete national implementation by mid‐2002. The AOANJRR has collected data on almost 100% of KR procedures performed in Australia since national implementation. AOANJRR data are externally validated against patient‐level data provided by all Australian state and territory health departments. A sequential, multilevel matching process is used to identify any missing data which is subsequently retrieved by contacting the relevant hospital. Since 2015, the AOANJRR has collected BMI data for all primary KR procedures.
BMI data were obtained from the AOANJRR for primary KR (unicompartmental and total KR) procedures performed for OA from 01 July 2017 to 30 June 2018. Patellofemoral KR, which comprise 0.4% of all KR in Australia, 12 were excluded from the study. Patients were classified by gender and age into the above listed categories.
Statistical analysis was performed using SAS software version 9.4 (SAS Institute, Cary, North Carolina, USA). Relative risks were calculated using generalized linear models assuming a binomial distribution and a log link. For patient categories where small numbers were available for analysis and the estimates were imprecise, relative risks were not reported. This applied to the underweight BMI category and the 18–24, 25–34, 35–44 and ≥85 year age categories for both genders.
The AOANJRR is approved by the Commonwealth of Australia as a Federal Quality Assurance Activity under part VC of the Health Insurance Act, 1973. All AOANJRR studies are conducted in accordance with ethical principles of research (Helsinki Declaration II).
Results
The 2017–2018 National Health Survey reports BMI data for 16 370 Australian adults (aged ≥18 years). 3 Overall, 35.6% were overweight and 31.3% were obese. For those aged ≥65 years, 38.2% were overweight and 37.4% were obese.
During the study period, 58 147 patients underwent primary KR for OA in Australia. BMI was recorded for 56 217 patients, representing a capture rate of 97%. The majority of patients were female (54.2%) and the mean age was 68 years. Overall, 31.9% of patients were overweight and 57.7% were obese.
The estimated number of adult females in Australia in each BMI category, based on the 2017–2018 National Health Survey, is presented alongside the number of patients that underwent KR during the study period, in Table A1 in Appendix 1. The same data for adult males is presented in Table A2.
When comparing the distribution of the estimated Australian population and the KR population in each BMI category, by age and gender, it was noted that a higher proportion of KR patients were in the obese categories (Fig. 1). This association was particularly strong for females in the younger age categories.
Fig. 1.
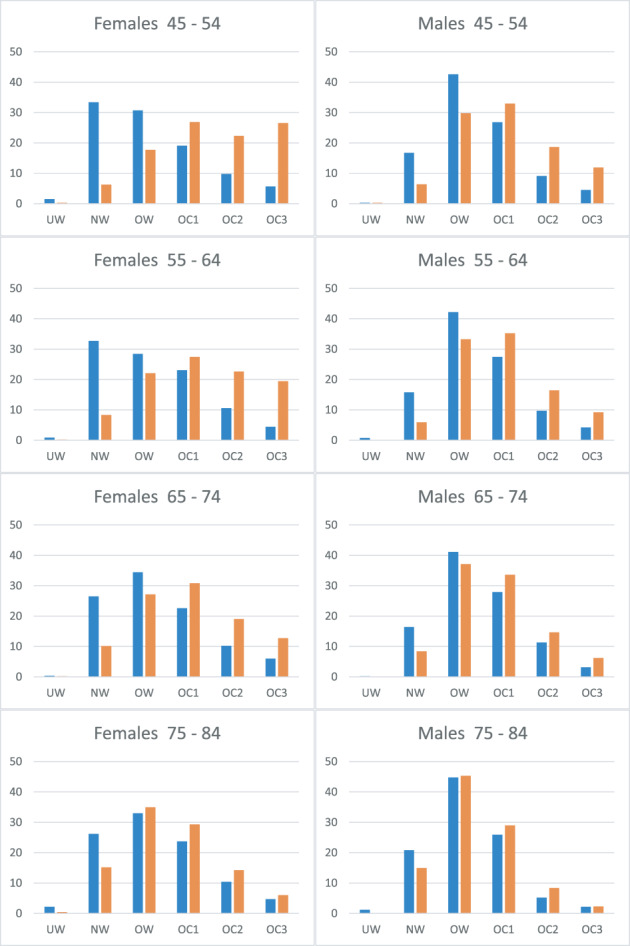
Percentage of individuals in each body mass index category, by age and gender. Blue bars, Australian Bureau of Statistics population estimate; orange bars, knee replacement patients. UW, underweight; NW, normal weight; OW, overweight; OC1, obese class 1; OC2, obese class 2; OC3, obese class 3.
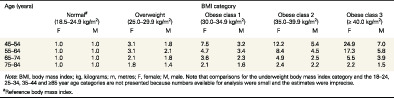
The relative risk of undergoing KR based on BMI category, compared to persons with normal BMI (18.5–24.9 kg/m2), for a given age and gender, is presented in Table 1. A positive association was noted between relative risk of undergoing KR and BMI category across all age groups and both genders. The association appears to be strongest for females and for younger patients. Females aged 55 to 64 years with Class 3 obesity are 17.3 times more likely to undergo KR than their normal weight counterparts. Males aged 55 to 64 years with Class 3 obesity are 5.8 times more likely to undergo KR than their normal weight counterparts.
Table 1.
Relative risk of undergoing knee replacement for osteoarthritis based on body mass index category, compared to persons with normal body mass index (18.5–24.9 kg/m2), by age and gender
| Age (years) | BMI category | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Normal # (18.5–24.9 kg/m2) | Overweight (25.0–29.9 kg/m2) | Obese class 1 (30.0–34.9 kg/m2) | Obese class 2 (35.0–39.9 kg/m2) | Obese class 3 (≥ 40.0 kg/m2) | ||||||
| F | M | F | M | F | M | F | M | F | M | |
| 45–54 | 1.0 | 1.0 | 3.1 | 1.8 | 7.5 | 3.2 | 12.2 | 5.4 | 24.9 | 7.0 |
| 55–64 | 1.0 | 1.0 | 3.1 | 2.1 | 4.7 | 3.4 | 8.4 | 4.5 | 17.3 | 5.8 |
| 65–74 | 1.0 | 1.0 | 2.1 | 1.8 | 3.6 | 2.3 | 4.9 | 2.5 | 5.5 | 3.9 |
| 75–84 | 1.0 | 1.0 | 1.8 | 1.4 | 2.1 | 1.6 | 2.4 | 2.2 | 2.2 | 1.5 |
Note: BMI, body mass index; kg, kilograms; m, metres; F, female; M, male. Note that comparisons for the underweight body mass index category and the 18–24, 25–34, 35–44 and ≥85 year age categories are not presented because numbers available for analysis were small and the estimates were imprecise.
Reference body mass index.
Confidence intervals and p‐values for the relative risk calculations are presented in Table A3 for females and Table A4 for males in Appendix 1.
Overweight and obese persons undergo KR in Australia at a younger age than normal weight individuals (Table 2). The mean age at which normal weight females undergo KR in Australia is 71.3 years, whereas Class 3 obese females undergo KR 7.2 years earlier, at a mean age of 64.1 years. Similarly, the mean age at which normal weight males undergo KR is 71.0 years, whereas Class 3 obese males undergo KR 7.3 years earlier, at a mean age of 63.7 years.
Table 2.
Mean age (in years) of patients undergoing knee replacement for osteoarthritis by gender and body mass index category
| Gender | BMI category | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight (< 18.50 kg/m2) | Normal weight (18.50–24.99 kg/m2) | Overweight (25.00–29.99 kg/m2) | Obese class 1 (30.00–34.99 kg/m2) | Obese class 2 (35.00–39.99 kg/m2) | Obese class 3 (≥ 40.00 kg/m2) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Female | 72 | 11 | 71.3 | 9.3 | 70.2 | 8.9 | 68.5 | 8.8 | 66.5 | 8.5 | 64.1 | 8.3 |
| Male | 69.6 | 14 | 71 | 9.6 | 68.9 | 8.9 | 67 | 8.4 | 65.4 | 8.1 | 63.7 | 7.7 |
Abbreviations: BMI, body mass index; SD, standard deviation.
Discussion
Like many countries worldwide, Australia has experienced a large increase in the incidence of primary KR in recent decades. 12 Potential drivers for this trend include overall population growth, an aging population, increased prevalence of obesity, increasing incidence of sport related knee injuries, improved access to specialist healthcare, and expanding indications for surgery. 1 , 16 Nearly 90% of patients undergoing primary KR in Australia are overweight or obese. 12
The results of our study suggest a strong association between increased BMI and the relative risk of undergoing KR. This association is strongest for younger females. Our findings align with those of previously published studies. Bourne et al. compared data from the 2006 Canadian Community Health Survey and the Canadian Joint Replacement Registry. 6 They found that overweight persons had a 3.2 times relative risk of undergoing KR compared to those with normal weight, and persons with Class 1, 2 and 3 obesity had relative risks of 8.5, 18.9 and 32.7, respectively. Overgaard et al. compared data from the Swedish Nationwide Health Survey and the Swedish Knee Arthroplasty Register, reporting that overweight and obese persons aged 45–64 years were 2.7 and 7.3 times more likely to undergo KR, respectively, than those with normal BMI. 7 For overweight and obese persons aged 65–84 years, the relative risks of undergoing KR were 2.1 and 4.0, respectively. Neither of these studies presented separate results by gender.
Positive associations between BMI and the risk of undergoing KR have also been noted in population studies from Great Britain, 17 , 18 Iceland, 19 Norway, 20 Singapore, 21 Spain, 22 Sweden, 23 , 24 and the United States, 25 however these studies involved linkage of participants to joint replacement registers or hospital records, rather than reviewing registry data in its entirety. Several studies noted a stronger association between increased BMI and the risk of KR in women compared to men. 20 , 21 , 24 , 25
Previous studies have linked different population cohorts to AOANJRR data to investigate the association between obesity and risk of undergoing KR. These include the AusDiab Study, 26 the Melbourne Collaborative Cohort Study, 27 , 28 and the Second Australian National Blood Pressure Study. 29 These studies have all found that obese persons have an increased risk of undergoing KR when compared to persons with a normal BMI.
We also identified that obese patients undergo KR at a younger age than non‐obese patients. In a retrospective study of 4740 KR performed in the United Kingdom (UK), Clement et al. found that overweight patients underwent KR 2.1 years younger than normal weight patients. 30 Class 1, 2 and 3 obese patients underwent KR 4.7, 6.7 and 10.5 years younger than normal weight patients, respectively.
The contribution of obesity to the development of knee OA is multifactorial. Not only does obesity cause excessive loading of joint surfaces, but dyslipidaemia and adipose tissue inflammation increase cytokine production, which also contributes to the aetiology of OA. 31 These associations may explain our finding of obese patients undergoing KR at an earlier age. The gender association we noted may be explained by differences in gait mechanics, and biochemical and metabolic factors.
While the findings of our study raise concerns about the impact of obesity on the future healthcare costs of primary KR, they also foreshadow a growing burden of revision KR. Obese patients undergoing KR have an increased risk of revision and infection, when compared to non‐obese patients. 12 , 32 Similarly, younger patients undergoing KR have a higher risk of revision than older patients. 12 Revision KR is much more expensive than primary KR, and the burden of revision KR is projected to increase dramatically. 33
Health services and policy makers must urgently intervene to reduce the prevalence of obesity at the population level, to reduce the burden of obesity related knee OA and subsequent KR. A multifaceted approach is needed, with individual and societal level interventions, including a strong focus on prevention. 34
In a recent study investigating the factors that have contributed to the increased incidence of KR in Australia from 2007 to 2017, Trieu et al. estimated that population changes in BMI have contributed to at least 6.3% of the growth in KR usage. 16 This equated to an additional 1631 KR procedures performed annually. A projection study by Ackerman et al. suggested that by reducing the population rate of overweight and obesity in Australia by 5% in 2030, 3278 KR could be avoided annually. 13
Even modest weight loss has been shown to effectively reduce the symptoms of knee OA, and the need for KR. Obese patients with symptomatic knee OA who maintain at least 10% body weight loss experience significant improvement in pain and function. 35 Overweight patients who lose over 7.5% body weight have a reduced risk of undergoing KR. 36
Our study has several strengths. As far as we are aware, this is the first study to present the relative risk of undergoing KR for different classes of obesity, by age and gender. We believe our findings will benefit healthcare professionals, health services, and policy makers alike. The datasets used in this study provide a contemporary representation of the association between BMI and the likelihood of undergoing KR in a country with a high rate of adult obesity. Our results align with those of previous studies, which used older datasets, 6 and were performed in countries with lower rates of adult obesity. 7 By utilizing AOANJRR data, we can confidently comment on the BMI for nearly 100% of patients undergoing KR in Australia. Moreover, by comparing this dataset to the 2017–2018 National Health Survey, we have avoided potential confounders involved in recruitment for previous cohort studies. 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29
We also acknowledge several limitations to our study. Firstly, the 2017–2018 National Health Survey may not provide a completely representative sample of the Australian population, and BMI data was imputed for 34% of respondents. This may affect the accuracy of our findings. Secondly, the AOANJRR calculates BMI based on the height and weight provided on data collection sheets submitted for each KR performed. The accuracy of our findings is dependent on the accuracy of the data provided; however, these data are measured at the time of the patient's preadmission to hospital and are part of the standard anaesthetic record, so we believe the data is accurate. Thirdly, using BMI to define obesity has limitations, as it does not differentiate between central and peripheral obesity.
In conclusion, obesity markedly increases the risk of Australian adults undergoing KR and is associated with the procedure being performed at a younger age. There is an urgent need for a societal level approach to address the prevalence of obesity, to reduce the burden of obesity related knee OA and subsequent KR.
Author contributions
Christopher J. Wall: Investigation; methodology; writing – original draft. Richard N. de Steiger: Supervision; writing – review and editing. Christopher J. Vertullo: Supervision; writing – review and editing. James D. Stoney: Conceptualization; writing – review and editing. Stephen E. Graves: Conceptualization; writing – review and editing. Michelle F. Lorimer: Data curation; formal analysis. Srinivas Kondalsamy‐Chennakesavan: Supervision; writing – review and editing.
Conflict of interest
None declared.
Supporting information
Appendix 1
Table A1. Number of females undergoing knee replacement for osteoarthritis by age group and body mass index category, compared with estimates for the general population. National data obtained from the Australian Bureau of Statistics website. 14 ABS, Australian Bureau of Statistics population estimate; KR, knee replacement; BMI, body mass index. * Estimate has a relative standard error of 25–50% and should be used with caution. ** Estimate has a relative standard error greater than 50% and is considered too unreliable for general use.
Table A2. Number of males undergoing knee replacement for osteoarthritis by age group and body mass index category, compared with estimates for the general population. National data obtained from the Australian Bureau of Statistics website. 14 ABS, Australian Bureau of Statistics population estimate; KR, knee replacement; BMI, body mass index. * Estimate has a relative standard error of 25–50% and should be used with caution. ** Estimate has a relative standard error greater than 50% and is considered too unreliable for general use.
Table A3. Statistical analysis for female data. F, female; RR, relative risk; CI, 95% confidence interval; Pr > ChiSq, p‐value.
Table A4. Statistical analysis for male data. M, male; RR, relative risk; CI, 95% confidence interval; Pr > ChiSq, p‐value.
Acknowledgements
Christopher Wall is a consultant for Stryker and has delivered paid presentations for Stryker, unrelated to this project. Richard de Steiger, James Stoney, and Stephen Graves are Directors for the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Christopher Vertullo is a Director for Knee Research Australia and the Australian Orthopaedic Association (AOA). Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
C. J. Wall MBBS, FRACS; R. N. de Steiger PhD, FRACS; C. J. Vertullo PhD, FRACS; J. D. Stoney MBBS, FRACS; S. E. Graves DPhil, FRACS; M. F. Lorimer BSc (Hons); S. Kondalsamy‐Chennakesavan MBBS, FRSPH.
The corresponding author is not a recipient of a research scholarship. This article was presented at the 81st Australian Orthopaedic Association (AOA) Virtual Annual Scientific Meeting, in November 2021.
References
- 1. Hunter DJ, Bierma‐Zeinstra S. Osteoarthritis. Lancet. 2019; 393: 1745–59. [DOI] [PubMed] [Google Scholar]
- 2. Safiri S, Kolahi AA, Smith E et al. Global, regional and national burden of osteoarthritis 1990‐2017: a systematic analysis of the global burden of disease study 2017. Ann. Rheum. Dis. 2020; 79: 819–28. [DOI] [PubMed] [Google Scholar]
- 3. Australian Bureau of Statistics . National Health Survey: First Results, 2017–18 Canberra: ABS; 2018. Available from URL: https://www.abs.gov.au/ausstats/abs@.nsf/PrimaryMainFeatures/4364.0.55.001?OpenDocument.
- 4. Ackerman IN, Bohensky MA, Pratt C, Gorelik A, Liew D. Counting the Cost: The Current and Future Burden of Arthritis. Part 1: Healthcare Costs. Sydney, Australia: Arthritis Australia, 2016. [Google Scholar]
- 5. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1545–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bourne R, Mukhi S, Zhu N, Keresteci M, Marin M. Role of obesity on the risk for total hip or knee arthroplasty. Clin. Orthop. Relat. Res. 2007; 465: 185–8. [DOI] [PubMed] [Google Scholar]
- 7. Overgaard A, Frederiksen P, Kristensen LE, Robertsson O. The implications of an aging population and increased obesity for knee arthroplasty rates in Sweden: A register‐based study. Acta Orthop. 2020; 91: 738–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Y, Wluka AE, Simpson JA et al. Body weight at early and middle adulthood, weight gain and persistent overweight from early adulthood are predictors of the risk of total knee and hip replacement for osteoarthritis. Rheumatology (Oxford) 2013; 52: 1033–41. [DOI] [PubMed] [Google Scholar]
- 9. Trends in adult body‐mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population‐based measurement studies with 19·2 million participants. Lancet 2016; 387: 1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization . Obesity and Overweight. Geneva, Switzerland: WHO. 2021. Available from URL: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- 11. Daigle ME, Weinstein AM, Katz JN, Losina E. The cost‐effectiveness of total joint arthroplasty: A systematic review of published literature. Best Pract. Res. Clin. Rheumatol. 2012; 26: 649–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) . Hip, Knee & Shoulder Arthroplasty: 2020 Annual Report. Adelaide: AOA, 2020. [Google Scholar]
- 13. Ackerman IN, Bohensky MA, Zomer E et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet. Disord. 2019; 20: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . Body Mass Index – BMI. Copenhagen, Denmark: WHO. 2022. Available from URL: https://www.euro.who.int/en/health‐topics/disease‐prevention/nutrition/a‐healthy‐lifestyle/body‐mass‐index‐bmi. [Google Scholar]
- 15. Australian Bureau of Statistics . Overweight and Obesity. Canberra, Australia: ABS, 2018. Available from URL:. https://www.abs.gov.au/statistics/health/health‐conditions‐and‐risks/overweight‐and‐obesity/latest‐release. [Google Scholar]
- 16. Trieu J, Dowsey MM, Schilling C, Spelman T, Choong PF. Population growth, ageing and obesity do not sufficiently explain the increased utilization of total knee replacement in Australia. ANZ J. Surg. 2020; 90: 1283–8. [DOI] [PubMed] [Google Scholar]
- 17. Liu B, Balkwill A, Banks E, Cooper C, Green J, Beral V. Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle‐aged women. Rheumatology (Oxford) 2007; 46: 861–7. [DOI] [PubMed] [Google Scholar]
- 18. Liu B, Balkwill A, Green J, Beral V. Body size from birth to middle age and the risk of hip and knee replacement. BMC Musculoskelet. Disord. 2016; 17: 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jonsson H, Helgadottir GP, Aspelund T et al. Hand osteoarthritis severity is associated with total knee joint replacements independently of BMI The Ages‐Reykjavik Study. Open Rheumatol. J. 2011; 5: 7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Apold H, Meyer HE, Nordsletten L, Furnes O, Baste V, Flugsrud GB. Risk factors for knee replacement due to primary osteoarthritis, a population based, prospective cohort study of 315,495 individuals. BMC Musculoskelet. Disord. 2014; 15: 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leung YY, Allen JC Jr, Noviani M et al. Association between body mass index and risk of total knee replacement, the Singapore Chinese health study. Osteoarthr. Cartil. 2015; 23: 41–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leyland KM, Judge A, Javaid MK et al. Obesity and the relative risk of knee replacement surgery in patients with knee osteoarthritis: A prospective cohort study. Arthritis Rheumatol. (Hoboken, NJ). 2016; 68: 817–25. [DOI] [PubMed] [Google Scholar]
- 23. Järvholm B, Lewold S, Malchau H, Vingård E. Age, bodyweight, smoking habits and the risk of severe osteoarthritis in the hip and knee in men. Eur. J. Epidemiol. 2005; 20: 537–42. [DOI] [PubMed] [Google Scholar]
- 24. Lohmander LS, Gerhardsson de Verdier M, Rollof J, Nilsson PM, Engström G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population‐based prospective cohort study. Ann. Rheum. Dis. 2009; 68: 490–6. [DOI] [PubMed] [Google Scholar]
- 25. Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am. J. Prev. Med. 2004; 27: 385–90. [DOI] [PubMed] [Google Scholar]
- 26. Hussain SM, Wang Y, Shaw JE et al. Relationship of weight and obesity with the risk of knee and hip arthroplasty for osteoarthritis across different levels of physical performance: a prospective cohort study. Scand. J. Rheumatol. 2019; 48: 64–71. [DOI] [PubMed] [Google Scholar]
- 27. Lim YZ, Wang Y, Cicuttini FM et al. Obesity defined by body mass index and waist circumference and risk of total knee arthroplasty for osteoarthritis: a prospective cohort study. PLoS One 2021; 16: e0245002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang Y, Simpson JA, Wluka AE et al. Relationship between body adiposity measures and risk of primary knee and hip replacement for osteoarthritis: a prospective cohort study. Arthritis Res. Therapy 2009; 11: R31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mnatzaganian G, Ryan P, Reid CM, Davidson DC, Hiller JE. Smoking and primary total hip or knee replacement due to osteoarthritis in 54,288 elderly men and women. BMC Musculoskelet. Disord. 2013; 14: 262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Clement ND, Deehan DJ. Overweight and obese patients require total hip and total knee arthroplasty at a younger age. J. Orthop. Res. 2020; 38: 348–55. [DOI] [PubMed] [Google Scholar]
- 31. Thijssen E, van Caam A, van der Kraan PM. Obesity and osteoarthritis, more than just wear and tear: pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity‐induced osteoarthritis. Rheumatology (Oxford) 2015; 54: 588–600. [DOI] [PubMed] [Google Scholar]
- 32. Kerkhoffs GM, Servien E, Dunn W, Dahm D, Bramer JA, Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta‐analysis and systematic literature review. J. Bone Joint Surg. Am. 2012; 94: 1839–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 2007; 89: 780–5. [DOI] [PubMed] [Google Scholar]
- 34. Blüher M. Obesity: global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019; 15: 288–98. [DOI] [PubMed] [Google Scholar]
- 35. Messier SP, Resnik AE, Beavers DP et al. Intentional weight loss in overweight and obese patients with knee osteoarthritis: is more better? Arthritis Care Res. 2018; 70: 1569–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jin X, Gibson AA, Gale J et al. Does weight loss reduce the incidence of total knee and hip replacement for osteoarthritis? A prospective cohort study among middle‐aged and older adults with overweight or obesity. Int. J. Obes. (Lond) 2021; 45: 1696–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1
Table A1. Number of females undergoing knee replacement for osteoarthritis by age group and body mass index category, compared with estimates for the general population. National data obtained from the Australian Bureau of Statistics website. 14 ABS, Australian Bureau of Statistics population estimate; KR, knee replacement; BMI, body mass index. * Estimate has a relative standard error of 25–50% and should be used with caution. ** Estimate has a relative standard error greater than 50% and is considered too unreliable for general use.
Table A2. Number of males undergoing knee replacement for osteoarthritis by age group and body mass index category, compared with estimates for the general population. National data obtained from the Australian Bureau of Statistics website. 14 ABS, Australian Bureau of Statistics population estimate; KR, knee replacement; BMI, body mass index. * Estimate has a relative standard error of 25–50% and should be used with caution. ** Estimate has a relative standard error greater than 50% and is considered too unreliable for general use.
Table A3. Statistical analysis for female data. F, female; RR, relative risk; CI, 95% confidence interval; Pr > ChiSq, p‐value.
Table A4. Statistical analysis for male data. M, male; RR, relative risk; CI, 95% confidence interval; Pr > ChiSq, p‐value.


