Abstract
The disposition of a drug is driven by various processes, such as drug metabolism, drug transport, glomerular filtration and body composition. These processes are subject to developmental changes reflecting growth and maturation along the paediatric continuum. However, knowledge gaps exist on these changes and their clinical impact. Filling these gaps may aid better prediction of drug disposition and creation of age‐appropriate dosing guidelines. We present innovative approaches to study these developmental changes in relation to drug metabolism and transport. First, analytical methods such as including liquid chromatography–mass spectrometry for proteomic analyses allow quantitation of the expressions of a wide variety of proteins, e.g. membrane transporters, in a small piece of organ tissue. The latter is specifically important for paediatric research, where tissues are scarcely available. Second, innovative study designs using radioactive labelled microtracers allowed study—without risk for the child—of the oral bioavailability of compounds used as markers for certain drug metabolism pathways. Third, the use of modelling and simulation to support dosing recommendations for children is supported by both the European Medicines Agency and the US Food and Drug Administration. This may even do away with the need for a paediatric trial. Physiologically based pharmacokinetics models, which include age‐specific physiological information are, therefore, increasingly being used, not only to aid paediatric drug development but also to improve existing drug therapies.
Keywords: drug metabolism, drug transport, ontogeny, paediatrics
1. INTRODUCTION
The disposition of a drug is driven by processes such as drug metabolism, drug transport and glomerular filtration. These processes are subject to age‐related changes, reflecting growth and maturation along the paediatric continuum. 1 , 2 , 3 Still, clinicians used to linearly adjust the dose for an adult to that of a child based on bodyweight. This oversimplification of paediatric physiology commonly resulted in drug plasma concentrations either below or above adult reference concentrations. A classic example is the case of toxic exposure to chloramphenicol, which resulted in fatal cardiovascular collapse (grey baby syndrome) in neonates. 4 This was ascribed to underdevelopment of drug metabolism in neonates.
Several information gaps on these developmental changes remain, bringing children at risk of subtherapeutic or toxic drug exposure. Nevertheless, paediatric studies aimed at delineating age‐related variations in drug metabolism and transport are often nontherapeutic, 5 which raises questions about ethical considerations. Studies must be designed to be of some benefit for the paediatric population and pose minimal risk to, and impose minimal burden on, the children in comparison with the standard treatment they receive. 6 A practical challenge for paediatric studies is the availability of only small blood and tissue sample volumes. Nevertheless, although paediatric drug research is considered complex and requires specific expertise, it is certainly not impossible.
The aim of this review is to show how innovative approaches have allowed filling of important gaps on the knowledge of the ontogeny of drug transport and metabolism, to illustrate the relevance of both in vitro as well as in vivo data, with the ultimate goal of improving drug therapy in children.
2. METHODS
We applied a narrative approach to identify publications concerning the ontogeny of drug metabolism and/or transport. The innovative approaches identified covered the topics (see Figure 1) presented below in this order:
In vitro data on ontogeny of transporters
In vivo paediatric microdosing and microtracer studies
Predicting paediatric pharmacokinetics (PK) by modelling and simulation
Collaboration
Promising future innovative techniques/approaches
FIGURE 1.
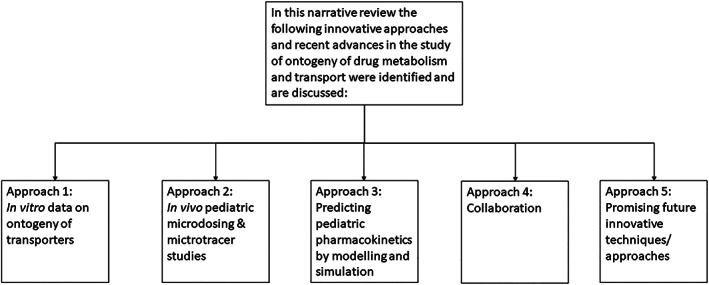
An overview of innovative approaches and recent advances in the study of ontogeny of drug metabolism and transport that are discussed in this review
The drug/molecular target nomenclature in this review conforms to the IUPHAR/BPS Guide to PHARMACOLOGY nomenclature classification. 7 Key protein targets and ligands in this article are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY.
3. APPROACH 1: IN VITRO DATA ON ONTOGENY OF TRANSPORTERS
3.1. How does membrane transporter expression change with age?
Transporters are membrane‐bound proteins present in the apical and basolateral membranes of organs such as the liver and kidney. 2 Their biological role is the bidirectional trafficking of substrates across membranes, which makes them critical determinants of tissue and cellular substrate disposition. Moreover, they act in concert with drug‐metabolizing enzymes to maintain homeostatic balance for endogenous substrates and to facilitate the detoxification and elimination of exogenous substrates, such as drugs and environmental toxins. 8
A 2015 review on the human ontogeny of drug transporters concluded that huge knowledge gaps remain for paediatrics, and that developmental patterns of transporter mRNA and protein expression needed to be elucidated to achieve safe and effective drug therapy for children. 2 At that time, mainly data from mRNA expression studies were available. Meanwhile, paediatric proteomic studies have become available through advances in liquid chromatography with tandem mass spectrometry (MS), which technique allows for quantification of the protein expressions of a variety of drug transporters in only a small amount of tissue. 9 , 10
Age‐related variations in the protein expression of clinically relevant hepatic and renal transporters (see Table 1 for an overview of these transporters) have now been studied. 11 , 12 , 13 , 14 A recent review by Cheung et al. provides a detailed overview of the reported ontogeny profiles. 15 Transporter protein expression show different developmental patterns: e.g. increasing, decreasing or stable across the paediatric age range. These developmental patterns appear to be both isoform‐ and organ‐dependent. Interestingly, for hepatic transporters, most differences in transporter expression were found between the foetal and adult age groups, and for renal transporters between infants <2 years and adults. Thus, it seems that major changes in transporter protein expression occur in early life. More specifically for hepatic transporters, the sample size and age ranges in a study from Prasad et al. 10 were complimentary to those in a study by van Groen et al. 11 Prasad et al. included 4 neonates, 19 infants, 32 children, 14 adolescents and 41 adults, whereas van Groen et al. mainly included foetuses (n = 36), preterm neonates (n = 12) and term neonates (n = 10). Both studies found that the expressions of organic cation transporter 1 (OCT1), multidrug resistance 1 (MDR1) and multidrug resistance‐associated protein 3 (MRP3) increased with age. A study by Li et al. with 43 renal samples from children, adolescents and adults did not find age‐related changes in transporter protein expression, 14 in contrast to the findings of Cheung et al. 13 This discrepancy is probably explained by the fact that the study by Li et al. had almost no samples from neonates and infants <2 years (i.e. 1 sample <1 year and 12 samples 1–<12 year). Interestingly, in addition to renal samples, Li et al. also included 26 paired hepatic samples (a subset from Prasad et al. 10 ), and confirmed that the transporter expression ontogeny was organ dependent. 14 For other major organs, such as the intestine, paediatric protein expression data are lacking. 15
TABLE 1.
Full names, protein names and gene names of clinically relevant renal and hepatic transporters
| Full name | Protein name | Gene name |
|---|---|---|
| P‐glycoprotein | P‐gp | ABCB1 |
| Breast cancer resistance protein | BCRP | ABCG2 |
| Multidrug and toxin extrusion 1 | MATE1 | SLC47A1 |
| Multidrug and toxin extrusion 2‐K | MATE2‐K | SLC47A2 |
| Organic anion transporting polypeptide 1B1 | OATP1B1 | SLCO1B1 |
| Organic anion transporting polypeptide 1B3 | OATP1B3 | SLCO1B3 |
| Organic anion transporter 1 | OAT1 | SLC22A6 |
| Organic anion transporter 3 | OAT3 | SLC22A8 |
| Organic cation transporter 2 | OCT2 | SLC22A2 |
| Multidrug resistance‐associated protein 2 | MRP2 | ABCC2 |
| Multidrug resistance‐associated protein 4 | MRP4 | ABCC4 |
| Sodium/taurocholate cotransporting polypeptide | NTCP | SLC10A1 |
| Bile salt export pump | BSEP | ABCB11 |
| Glucose transporter 1 | GLUT1 | SLC2A1 |
| Glucose transporter 2 | GLUT2 | SLC2A2 |
| Monocarboxylate transporter 1 | MCT1 | SLC16A1 |
| Uric acid transporter 1 | URAT1 | SLC22A12 |
The observations described above show that the transporter substrate disposition is subject to age‐related changes. This may impact drug exposures in children and thereby potentially affect drug efficacy and safety. This supposition is supported by a study concluding that hepatic OCT1 ontogeny partly explained the lower clearance of its substrate morphine in neonates and infants than in adults. 16
Regarding renal transporters, the renal clearance in general is driven by glomerular filtration, which also changes with age. The glomerular filtration rate (GFR) reaches 50% of adult values by 2 months and 90% of adult values by age 1 year. 17 Drugs that are substrates for renal transporters may also be actively secreted or reabsorbed in the tubules by these renal transporters, on top of glomerular filtration. Thus, age‐related changes in the PK of renal transporter substrates can probably be ascribed to both maturation of transporter expression and of GFR. For instance, after hepatic metabolism, the antiviral drug valacyclovir is renally eliminated via glomerular filtration and active tubular secretion, probably by organic anion transporter (OAT)1/3. 18 The apparent clearance of valacyclovir in infants younger than 3 months was half of that in young children. 18 The GFR in infants younger than 3 months is expected to exceed 50%, 17 and therefore this lower clearance may be explained by the fact that the TM50 of OAT1 was approximately 4 months, and that of OAT3 8 months. 13 An example of an endogenous transporter substrate is uric acid (UA), which is a substrate for both the renal transporters breast cancer resistance protein and urate transporter 1. 19 , 20 The fractional excretion of UA (% of filtered UA not reabsorbed by the tubules), is 30–40% in term newborns under the age of 5 days, which decreases to 8–10% in 3‐year‐old children. 21 , 22 , 23 Apart from age‐related physiological changes in, for example, urinary acidification and concentration ability, transporter ontogeny may explain this observation. The expression of the apical efflux transporter breast cancer resistance protein decreases from birth, whereas expression of the apical uptake transporter urate transporter 1 increases from birth until childhood, resulting in a net decrease in UA excretion. 21 , 23
3.2. Potential underlying mechanisms for transporter ontogeny
Differences in maturational patterns between mRNA and protein transporter expression have been reported. 11 , 13 This interesting finding may help understand the underlying mechanisms of these patterns. Alternative splicing, a process that increases the diversity of products, i.e. splice variants, from a single gene, might be 1 of the mechanisms for maturational changes in organic anion transporting polypeptide 1B1 (OATP1B1) expression, as in a previous study the gene expressions of a fair amount of splice variants were associated with age. 24 The total gene expression quantified by quantitative reverse transcription polymerase chain reaction could be derived from a mixture of different splice variants of the targeted gene, also including splice variants that may not translate into protein. 25 Quantitative proteomics measures the actual expression of the protein of interest; hence, alternative splicing could partly explain the lack of correlation between mRNA and protein expression, especially when a correlation is found in adults but not in children, or vice versa.
More specifically, age‐related variation in the expressions of solute carrier organic anion transporter 1B1 (SLCO1B1) splice variants may have implications for children, as we have found that most of these splice variants predictably resulted in truncated isoforms of the OATP1B1 transporter. 24 The functionality of the transporter is thought to be partly dependent on the number of transmembrane regions. As the truncated isoforms have fewer transmembrane regions, the functionality of the transporter may be affected in children, and consequently the disposition of its endogenous and exogenous substrates. Furthermore, the location of a transporter is a critical determinant of activity and correct functionality, which is partly determined by post‐translational changes such as glycosylation. 26 The truncated SLCO1B1 isoforms may lack 1 or more of the N‐glycosylation sites, which may lead to an inappropriate localization as nonglycosylated OATP1B1 is retained within the endoplasmic reticulum, i.e. not being present on the cell membrane. 27
The expressions over age of several transporters, for example the renal transporters OAT1 and OAT3, have been found to be strongly correlated. 11 , 13 Still, the underlying mechanism for ontogeny may be the same. OAT1 and OAT3 are located in adjacent regions on chromosome 11. 28 Moreover, they are both positively regulated by the transcription factors hepatocyte nuclear factor (HNF) 1α and 1β. 29 We could speculate that HNF1α and 1β are also impacted by age, which then would explain the developmental patterns of OAT1 and OAT3. However, the relationship between transcription factors maintaining basal expression level, like the HNF family, and transporter expression, is still largely unknown, let alone the impact of age on transcription factors.
3.3. Methods and study design to study ontogeny of drug transport
The current lack of harmonized practices in the implementation of liquid chromatography–tandem MS‐based proteomic quantification leads to variability in reported abundances of the same proteins. 30 , 31 Using available data to simulate PK may introduce unexpected bias, especially when in vivo PK data to validate the simulations are lacking. Not only the analytical method, but also the unit in which the data are reported may differ. For example, it was found for hepatic transporters that crude membrane yield per amount of tissue was higher in foetuses than in term newborns. 11 Therefore, ontogeny patterns may not be similar when the transporter protein expression is described per gram crude membrane instead of per g of tissue. However, in literature, these units are used inconsistently, as consensus is lacking on how to report proteomic data.
More specifically regarding renal transporters, sample preparation and data interpretation are further complicated by the fact that the kidney consists of cortex and medulla. Renal transporters are primarily located in the kidney's proximal tubules, which are enriched in the cortex, whereas the medulla is enriched with distal/collecting tubules. The relative composition of cortex vs medulla in frozen tissue could vary depending on sample collection and dissection. The ontogeny data could, therefore, be confounded. Regarding renal transporters in adults, studies often apply normalization to the housekeeping protein aquaporin 1, located specifically in the proximal tubule. As the expression of aquaporin 1 in newborns is 50% of the expression in adults, 32 , 33 the use of aquaporin 1 as a housekeeping protein is limited in paediatric studies. Interestingly, Li et al. recently studied could not identify an age‐related change in aquaporin 1 protein expression in 43 human samples from age 0.5 to 35 years. 14 They first used the ratio of this protein to aquaporin 2, which is located in the distal/collecting tubules, to exclude tissues contaminated with medulla (based on the statistical Grubb's test to identify outliers). Thereafter, they normalized the renal transporter expression to aquaporin 1 to study ontogeny patterns.
3.4. Challenges, recommendations and future perspectives for the ontogeny of transporters
While the current studies significantly contributed to our understanding on age‐related changes in transporter expression, there are still future perspectives to continue this work. For 1 thing, the protein expression of renal transporters in neonates is understudied, as the 2 available studies both only included 1 neonate. 13 , 14 In addition, regarding both renal and hepatic transporters, the unexplained interindividual variability in protein expression within age groups is distinct. 11 , 12 , 13 , 14 Apart from age, comedication and the presence of inflammation, among other things, can influence the transporter expression and thereby contribute to the expression variability. 34 , 35 The impact of acute and chronic inflammation on transporter expression and activity is related to the activity of multiple proinflammatory cytokines that can activate or inhibit involved nuclear receptors or transcription factors. 36 Similarly, certain medications and environmental toxins could lead to activation of nuclear receptor pathways, and could, therefore, influence the transporter expression. 36 , 37 The underlying causes of death of tissue donors are heterogeneous—and so are the exposures to drugs and environmental toxins. Lastly, in postmortem tissue, the measure of degradation in mRNA and protein levels may vary among samples, which may impact the expression level measurements. The interplay of age with these other covariates merits further elucidation.
Furthermore, genomic variation can impact mRNA and/or protein transporter expression. Nevertheless, a study on hepatic transporters in a cohort mainly consisting of foetuses and newborns could not identify such impact, 11 although the selected genetic variants were known to affect mRNA and/or protein expression in adults or older children. This finding may be explained by the small sample size, but perhaps also by the interplay between development and genetics. For example, in a previous study, SLC22A1 181C > T in adult samples correlated with OCT1 protein expression, 38 but this was not confirmed in the paediatric cohort. 11 OCT1 expression was low in foetuses, potentially obscuring a possible effect of genetic variants. By contrast, the SLC22A1 genotype (giving rise to the OCT1 transporter) is related to tramadol disposition in preterm infants, similar to adults. 39 This suggests that, although protein levels are low, the SLC22A1 genotype can result in significant differences in protein activity in neonates. In the cohort of van Groen et al. the OATP1B1 protein expression was stable within SLCO1B1 diplotypes. 11 In contrast, Prasad et al. showed higher protein expression in neonates vs older children/adults with the SLCO1B1 *1A/*1A haplotype. 10 Thus, it remains important to include genotype when analysing developmental patterns. Furthermore, the interaction between genetic variants and age should be studied further.
This review focuses on the kidney and liver, but transporters as well as drug‐metabolizing enzymes are also abundant in other major organs, such as the gastrointestinal tract, and sanctuary sites including the brain. 40 The developmental patterns of transporters and drug‐metabolizing enzyme isoforms appear to be organ‐dependent. 14 An understanding of the ontogeny of multiple transporters, drug‐metabolizing enzymes and tissues from different organs in parallel would provide a more holistic view on entire human development. 41
Regarding proteomic studies, a recently published white paper discussed current practices and provided recommendations towards harmonization of practices. 42 The recommendations concern specific proteomic quantification techniques, sample preparation and quality controls, as well as documenting of tissue weight and the originating organ section. For further method development, housekeeping proteins should be further validated to normalize for technical variability. Researchers are advised to follow these and future recommendations, as this would enable comparison and combining data originating from various laboratories.
Importantly, the impact of a transporter on the disposition of a substrate is determined by its functional activity. It is widely accepted to use mRNA and protein expression data as a surrogate parameter for the functional activity of a transporter. 2 However, there may be discrepancies between expression and activity, as already introduced above. Therefore, ex vivo ontogeny should preferably be validated by in vivo data. In a previous study, tazobactam PK data were used to validate the ontogeny profiles of the renal transporters OAT1/3. 15 Another approach to estimate transporter maturation is to subtract age‐specific GFR estimations from reported total renal clearance values of a specific renal tubular transporter substrate. Willmann et al. determined the renal tubular MDR1 maturation by subtracting estimated GFR from digoxin total renal clearance, a MDR1 substrate. 43 Next, plasma concentrations of the MDR1 substrate rivaroxaban were simulated over the paediatric age range. The authors assume that MDR1 transport is the rate‐limiting factor in the tubular secretion of both digoxin and rivaroxaban. These examples aid in creating confidence to incorporate the ex vivo data for predicting paediatric PK.
4. APPROACH 2: IN VIVO PAEDIATRIC MICRODOSING AND MICROTRACING STUDIES
4.1. Phenotyping drug metabolism routes subject to developmental changes
Drug metabolizing enzymes such as cytochrome P450 (CYP) enzymes, UDP‐glucuronosyltransferases and sulfotransferases are subject to developmental changes. 3 Many of these enzymes are located in both the liver and the intestine. Validated markers to phenotype a drug metabolism route can be used to study developmental changes of drug‐metabolizing enzymes in vivo. An example is midazolam, a validated marker for the developmentally regulated drug‐metabolizing enzyme CYP3A4/5, of which the PK parameters can be used as a surrogate for CYP3A4/5 maturation. As children usually are given drugs orally, 44 the drug‐metabolizing enzyme activity in both intestine and liver, captured by the oral bioavailability, is an important determinant for systemic exposure.
Traditionally, data on oral bioavailability were often obtained in a cross‐over study, in which a child receives an oral or intravenous (IV) dose of a drug twice in random order, accounting for a wash‐out period. This design is ethically and practically challenging for phenotyping purposes, as children need to be exposed twice to therapeutic doses with extensive blood sampling, without any benefit for themselves. As international ethical guidelines prohibit studies that may not provide benefit to children and that pose more than minimal risk and burden over those daily encountered, alternative approaches are needed. To overcome challenges faced with such paediatric PK studies, microdosing/microtracing studies with [14C]labelled substrates constitute an interesting alternative. A microdose is a very small, subtherapeutic dose of a drug (<1/100th of the therapeutic dose or <100 μg), which is unlikely to result in pharmacological effects or adverse events. 45 , 46 A radioactive label [14C] allows ultrasensitive quantification of extremely low plasma concentrations by accelerator MS, for which only 10–15 μL plasma is required. 47 , 48 The radiation dose associated with a [14C]microdose is safe as it is below 1 μSievert. This is much lower than the yearly background exposure (2.5 mSievert/year in the Netherlands), a computed tomography scan of the head (1,200 μSievert) or a chest x‐ray (12 μSievert). 49 Given these considerations, microdosing studies are considered as nontherapeutic trials with minimal burden that carry minimal risk. 50
A microdose concurrently administered with a therapeutic dose allows assessing the oral bioavailability, where the microdose is then called a microtracer. This elegant and innovative study design enables measurement of both IV and oral disposition, limiting the extensive blood sampling needed for a cross‐over study and avoiding the day‐to‐day variability. 51 , 52 Two paediatric studies have used this study design. In 1, age‐related changes in oral bioavailability of paracetamol (acetaminophen or AAP) as a measure of glucuronidation and sulfation were studied. An oral [14C]AAP microtracer (3.3 [2.0–3.5] ng/kg; 64 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 Bq/kg) was given to 50 stable, critically ill children (median age 6 months [range 3 days–6.9 years]) who received IV therapeutic paracetamol for clinical purposes and had an indwelling arterial catheter enabling blood sampling in place. 51 The plasma and urinary AAP‐glucuronide/AAP and AAP‐glucuronide/AAP‐sulfation ratios significantly increased by 4‐fold with increasing age, while the AAP‐sulfation/AAP ratio significantly decreased. In other words, the AAP metabolism shifted from mainly sulfation in neonates to glucuronidation in older children. 51 The mean enteral bioavailability of AAP in this population was 72% (range, 11–91%). 52
The other study used midazolam as a well‐validated CYP3A probe to unravel the ontogeny of CYP3A that is abundant in both the intestine and liver and contributes to the first‐pass metabolism of many orally administered drugs. 3 , 53 , 54 Forty‐six stable, critically ill children (median age 9.8 [range 0.3–276.4] weeks; 3/4 of the 46 subjects were 0–6 months old) received a single oral [14C]midazolam microtracer (58 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 Bq/kg). 55 The bioavailability of midazolam was 66% with a large range of 25–85% for which no explanatory covariates could be identified. These findings were in line with the expected CYP3A ontogeny, in that older children and adults have a higher CYP3A activity—and, thus, a lower oral bioavailability 54 —than the population in the microtracer study, and vice versa for preterm neonates. The median of 66% 55 is lower than the reported median value of 92% in preterm neonates 56 and higher than the reported median value of 21% in older children, aged 1–18 years. 57 Also, the reported mean ± standard deviation of 28 ± 7% in adults is lower. 58 The oral bioavailability was also highly variable in other paediatric studies. In preterm neonates, the oral bioavailability ranged from 67 to 95% 56 and from 12 to 100%, 59 and in children aged 1–18 years from 2 to 78%. 57 Factors other than age may also influence the oral bioavailability of midazolam. A study from Vet et al. found a significant impact of organ failure on the midazolam clearance, 34 with the greatest impact in children with 3 or more failing organs, and children with inflammation. 34 , 60
The oral bioavailability of both AAP and midazolam is impacted as well by drug absorption factors such as intestinal surface area, 61 permeability, 62 gastric emptying time, intestinal transit time, the production of bile fluid, 63 and organ blood flow to the intestines and liver. 64 Studies of the influences of age and disease severity on these processes should be studied to further explain the variability in oral bioavailability of AAP and midazolam.
The study design with an oral [14C]microtracer was shown successful for safely studying the oral bioavailability of AAP and midazolam in children. To ultimately improve the safety and efficacy of paediatric drug therapy, we recommend considering study designs with microdoses for minimal risk PK studies and microtracer studies to elucidate oral bioavailability.
4.2. [14C]microtracer study to create metabolite profiles of midazolam
Metabolic routes in children may be different from those in adults if a certain pathway is underdeveloped. Drug metabolism in children may even require alternative metabolic routes, in which other metabolites may be present whose action and PK are unknown. This could lead to unsafe drug therapy. Interestingly, [14C]microtracer studies permit identifying and quantifying metabolites with a radioactivity exposure of even less than 0.1 μCi. 45 , 46 Analytical advances such as these allow us to overcome ethical and analytical challenges with regard to radioactivity exposure in paediatrics. 65 , 66 A proof of concept study with a [14C]midazolam microtracer showed that in children, metabolite profiles of midazolam were safely created and the routes of excretion were safely studied. 67 This approach is promising for first‐in‐child studies to delineate age‐related variation in drug metabolite profiles.
4.3. Dose linearity of a microdose
A prerequisite of extrapolating the PK of microdose directly to a therapeutic dose is that the PK of a microdose of a certain drug or compound is linear to the PK of a therapeutic dose. 68 , 69 Lack of linearity may occur, for example, when a therapeutic dose saturates drug metabolism pathways, plasma protein binding and/or active transporters. 69 , 70 Because of the maturational differences in drug metabolism and transport, one should be careful with extrapolating the results from adults directly to the paediatric population. A very elegant approach was taken to study the dose linearity of a [14C]midazolam microdose in children 71 by comparing the PK parameters of an isolated [14C]microdose with the PK parameters of a [14C]microtracer administered concurrently or even mixed with a therapeutic drug dose. This study supported dose linearity of the PK of the isolated [14C]midazolam microdose to that of the [14C]midazolam microtracer.
4.4. Feasibility
Earlier studies have shown that it is feasible to use a [14C]labelled substrate to phenotype a certain drug metabolism pathway 51 , 52 , 67 , 72 , 73 , 74 ; not only were the PK findings in line with expectations, but importantly, parents allowed their children to participate in these studies with a consent rate of around 50%. This informed consent rate is in agreement with the consent rates of other nontherapeutic studies in paediatric intensive care. 75 Most often, professionals express ethical concerns regarding the radioactive exposure, including the expectation that parents will not allow their children to participate in such studies. The authors of that study had noted that parents not necessarily refused consent for reasons of the radioactivity exposure, as they had well been informed of the negligible exposure compared with the yearly background exposure. The reason for refusing consent was more often the burden of additional procedures. This is not surprising, as for clinical reasons a child may have to undergo a number of painful and stressful procedures (median 11 [interquartile range = 5–23] per day established in a previous study 76 ), which also has impact on the parents.
4.5. Challenges, recommendations and perspectives for paediatric microdosing and microtracing studies
One of the opportunities of these paediatric microtracer studies, is that findings can be extrapolated to drugs metabolized by the same drug‐metabolizing enzymes. For instance, the PK of midazolam served as a marker for CYP3A4/5 activity. As many drugs are metabolized by the CYP3A family, 77 it would be helpful to extrapolate the results to other CYP3A‐substrates, especially to define a first‐in‐child dose during development of a new drug that is a CYP3A‐substrate. Recently, a framework was published for between‐drug extrapolation of covariate models. 78 The authors recommended to take into account relevant drug properties such as the extraction ratio, the plasma protein to which the drug is binding, and the fraction unbound. Brussee et al. applied this framework to study whether scaling with a paediatric covariate function from midazolam will lead to accurate clearance values of other CYP3A‐substrates, such as atorvastatin, sirolimus and vincristine. 79 Clearances were accurately scaled of drugs mainly eliminated by CYP3A‐mediated metabolism with, for example, high protein binding to HSA (>90%) and a low‐to‐intermediate extraction ratio of <0.55 in adults.
Over the past decade, regulatory legislations for drug development in children have been passed worldwide. Accordingly, the number of drugs tested in children has dramatically increased. In 2014–2015, the US Food and Drug Administration (FDA) reviewed 274 paediatric study plans, whereas in 2012–2013 the number was only 20. 80 This trend was also seen in the EU, with 31 new drugs/indications authorized for use in children in 2004–2006, vs 86 in 2012–2016. 81 Nevertheless, still many drugs enter the market without being licensed for paediatric use. Since the EU Paediatric Regulation came into force in 2007 and up to 31 December 2015, only 26% out of all 352 new medicines were centrally authorized for paediatric use. 81 One of the reasons for this low proportion is that many paediatric studies failed. 82 Another reason is a specific condition of this regulation: if the prediction of the risk of toxicity of a new compound is not adequate, the European Medicines Agency and the US FDA may waive the studies in the youngest children. 83 However, a drug which has not been authorized may still be prescribed off‐label. 84 Although off‐label is not off‐evidence, as paediatric PK data for existing drugs are increasingly available in literature, there are still huge knowledge gaps on possible risks. A microdosing study could be of benefit by studying the PK and the metabolite profile of a drug under development in children without risk of toxicity. These studies are considered as nontherapeutic trials with minimal burden that carry minimal risk, which is echoed by the Dutch legislation, EU regulation and the U.S. FDA regulations. 85
Despite positive experiences with microdose studies, 1 may still be reluctant to use this approach in studies with children or other vulnerable populations. Doses are rather derived from physiologically based PK (PBPK) models (see paragraph ‘Using PBPK models to predict paediatric drug exposure and its challenges’) or allometric scaling with the use of adult data. These approaches are relevant, for example, for drugs that are not substrates for drug‐metabolizing enzymes or transporters, or drugs that are substrate for enzymes and transporters of which we have thorough understanding on their ontogeny. But for many drugs this approach is suboptimal as there are still large knowledge gaps for the biological data underlying the PBPK models for special populations. 86 The knowledge gaps regarding transporters are discussed in paragraph ‘Challenges, recommendations and future perspectives for the ontogeny of transporters’. Other knowledge gaps include the influence of age on intestinal surface area, 61 permeability, 62 gastric emptying time, intestinal transit time, the production of bile fluid 63 and organ blood flow to the intestines and liver. 64 This leaves these special populations at a higher risk of toxicity or therapeutic failure. Also, regarding specific paediatric indications, for example congenital diseases, the first‐in‐human dose will be given to children and not to adults. Good understanding of the paediatric PK is then key to safety. Therefore, microdosing studies may be of great value in paediatric drug development and are now suggested in the 2019 FDA (draft) Guidance: General Clinical Pharmacology Considerations for Neonatal Studies for Drugs and Biological Products Guidance for Industry. 87 Lastly, these approaches would also allow studying the PK or metabolite profiles in other vulnerable populations, such as pregnant women, critically ill or elderly.
5. APPROACH 3: PREDICTING PAEDIATRIC DRUG EXPOSURE AND DOSING RECOMMENDATIONS
5.1. Using PBPK models to predict paediatric drug exposure and its challenges
Protein and gene expression data on drug metabolism and drug transport may be leveraged in PBPK models alongside paediatric physiology. These models are complex multicompartment kinetic models that allow prediction of drug exposure in a specific target population. They rely on in vitro data and physiological parameters, and can subsequently be explored based on in vivo data. PBPK models are also increasingly used to optimize clinical drug trial design and doses, also for paediatric trials. 88 Fifteen percent of all new drug application submissions to the FDA between 2008 and 2017 that included PBPK analyses supported the evaluation of paediatric‐related issues such as initial dose recommendation for clinical trials. 89 Several paediatric clinical studies have been replaced with or informed by PBPK modelling. 90 , 91 For example, models have been used to set a starting dose in a clinical trial with eribulin in children and adolescents aged 6–18 years, and to bridge from immediate to extended release quetiapine formulations in children and adolescents aged 10–17 years. 90 , 92
PBPK modelling could also be helpful to evaluate drug–drug interactions (DDIs). Hospitalized children may be exposed to up to 10 different drugs. 93 With that, DDIs are inevitable, for which recommendations from adult DDI studies are often extrapolated to the paediatric population. In a systematic literature review, the numbers of interactions for 24 drug pairs were compared between 31 paediatric studies and 33 adult studies. The number of DDIs differed: in 15 of the 33 cases, the number of DDIs was >1.25‐fold higher for children than for adults, and in 8 of the 33 cases, the number of DDIs was <0.8‐fold lower in children than in adults. For example, digoxin plus amiodarone and lamotrigine plus valproate resulted in a 2.18‐fold higher and a 0.58‐fold lower exposure, respectively, in children compared with adults. This could be ascribed to the underlying maturation of processes involved in drug disposition. These findings warn us that simple extrapolation of adult DDI data to the paediatric population can under‐ or overpredict the impact of a DDI—with subtherapeutic or toxic exposure to a drug as a result. PBPK modelling is a powerful tool to explore and quantitatively predict DDIs, also in a paediatric population. 90
The use of PBPK models to predict paediatric drug exposure comes with important limitations, however. For some genes, the gene expression, protein expression and/or activity involved in drug disposition are correlated, and in these cases the expression data are used in PBPK models as a surrogate for determining activity. So far, however, such correlations have been most often shown in adult populations. A previous study found that the fraction of highly glycosylated OATP1B3 increased with age. 94 Because post‐transcriptional and post‐translational modifications of transporters, such as glycosylation, 94 may be subject to age‐related changes, it could well be that gene and protein expression are correlated in adults but not in children. Hence, these correlations should not be extrapolated directly from adults to children, as this could lead to inaccurate predictions of drug disposition. This also accounts for the fraction of a parent drug that is metabolized or transported by a certain protein, 95 which often is assumed to be the same for children and adults. However, the maturation of enzymes and transporters may change their relative contributions in the disposition. 95 , 96
The success of PBPK simulation in children depends highly on knowledge of the drug disposition pathways and the availability of ex vivo/in vitro data. As knowledge gaps remain next to newly available data, routine use of PBPK modelling in prediction of paediatric drug disposition should be done carefully until these knowledge gaps are filled. Nevertheless, PBPK modelling currently helps us understand drug metabolism and transport pathways, and the impact of changes, such as maturation.
5.2. Dosing recommendations in clinical practice
The increase in paediatric research has helped enormously in understanding how PK of a variety of drugs is different in various age groups, giving rise to paediatric‐specific dosing recommendations. To implement this knowledge in clinical practice, however, comes with challenges. First, prescribers may remain unaware of the rationale of certain dosing recommendations published in scientific literature or lack understanding of and trust in PK studies and their subsequent dosing simulations. The Netherlands Knowledge Centre on Pharmacotherapy in Children hereby serves as an example on how this knowledge translation gap can be bridged, as it has developed a paediatric drug formulary based on best available evidence from registration data, investigator‐initiated research, professional guidelines and clinical experience. 97 That this approach is valuable is shown by the recent extension of the formulary to country‐specific editions for Germany, Austria and Norway have been prepared. Second, the current paediatric dosing recommendations are often only based on PK data, on the assumption that the target concentration for effect is the same in children and adults. However, these target concentrations may well be different in children, as the pharmacodynamics (PD) could also be subject to age‐related changes. 98 These dosing recommendations should therefore preferably be validated prospectively, especially when only based on PK data. Validation can be performed in clinical practice with opportunistic PK sampling or with clinical data collection of PD parameters of specific interest. In the case of low confidence on the dosing recommendation, a paediatric trial is recommended, in which the former dosing regimen is compared to the new dosing regimen based on PK and PD parameters.
Using population PK and PBPK models to simulate and predict the optimal drug exposure may lead to complex dosing regimens and consequently logistical problems in clinical practice. In hospitals, for example, nurses are used to administering drugs to patients at fixed times. Home drug therapy compliance may be negatively affected if medication must be taken at varying times. Moreover, some doses are not feasible to administer, for example 1/8 of a tablet is hard to prepare, and paediatric formulations are not available. 99 Furthermore, the electronic health care systems may not be equipped to integrate complex models. 100 , 101 Lastly, clinical staff may have little understanding of complex population PK models, and may lack trust in these dosing regimens. Nevertheless, efforts are being made to accelerate implementation. For example, the calculator that comes with the Dutch paediatric formulary allows inclusion of covariates that will lead to the optimal dose. Furthermore, start‐ups are creating electronic systems to integrate complex dosing regimens for use in clinical care parallel to the electronic health care system. 101
6. APPROACH 4: COLLABORATION
As tissues for ex vivo paediatric studies are scarce, and sample sizes for in vivo studies are small, establishing collaborations with other research groups is the way to go. Pooling samples beforehand will avoid lab‐to‐lab variability and lead to more reliable and complete results. Furthermore, setting up international biobanks would help overcome the scarcity of paediatric tissue.
Similar collaborative efforts should be taken to overcome challenges in recruitment of patients for in vivo studies due to low number of eligible patients, and optimal paediatric trial design and infrastructure. Examples of existing collaborative efforts are the IMI2 project to develop a Europe‐wide Paediatric Clinical Trial Network, Conect4Children for Europe and the Paediatric Clinical Trials Network and iACT both in the US existing government‐supported research infrastructures in Europe, such as BBMRI (biobanking), ELIXIR (data), EATRIS (drug development) and ECRIN (clinical trials), which have traditionally focused on adults, should collaborate to integrate paediatrics, with the ethical and practical specificities outlined throughout this review. An important side note: these paediatric trial networks and infrastructures may create new challenges, such as accounting for differences in clinical practice between countries and hospitals, and the efforts needed to reach consensus about study designs. Pharmaceutical companies, academia and regulatory institutes work together in these initiatives, but their scientific goals and procedures for paediatric trials may differ.
In terms of data availability, initiatives for data sharing platforms 31 are encouraged in which all raw data of published articles are made freely available. Several scientific journals have already made it mandatory for authors to submit the raw dataset along with the manuscript, 102 which is a positive advancement.
7. APPROACH 5: PROMISING FUTURE INNOVATIVE TECHNIQUES/APPROACHES
Regarding ex vivo studies, opportunities exist for unravelling the ontogeny of drug disposition on the level of protein/mRNA expression in fresh tissue instead of postmortem tissue. The options include the use of organoids that represent 3‐dimensional culture systems in which stem cells grow and represent the native physiology of the cells in vivo. 103 When using tissue‐derived hepatic, renal or intestinal stem cells from children, the organoid may reflect the paediatric native physiology and allow to study the expression of transporters or drug‐metabolizing enzymes. Organoids can also be used to unravel regulatory pathways. Two‐dimensional models of e.g. intestinal organoids may permit studying drug metabolism and transporter activity in a situation that even closer resembles the in vivo situation. Another innovative approach is the use of exosomes. 104 These are extracellular vesicles secreted by organs, which circulate in the blood. They contain proteins, mRNA and microRNA derived from the originating organ, and, therefore, can be used to measure transporter and drug‐metabolizing enzyme expression. 104 It is not known, however, whether organoids and exosomes keep their age‐specific properties outside a human body, which is a prerequisite for studying age‐related changes in expression/activity of transport and metabolism.
Another approach involves in vivo assessment of drug‐metabolizing enzyme or transporter activity through endogenous substrates as biomarkers, for example 6b‐hydroxycortisol or 4b‐hydroxycholesterol for assessment of CYP3A activity. 105 Interestingly, studies in adults have identified endogenous substrates as potential markers to phenotype the activity of transporters in vivo, for example thiamine for OCT1 and dehydroepiandrosterone sulfate for OATP1B1/3. 105 This approach does not require administration of an external marker, and only a single blood draw is needed. This approach has been little used so far, as reference values of endogenous substrate levels in children are lacking. These values cannot be simply extrapolated from values in adults, as homeostatic levels in children may differ from those in adults. For example, dehydroepiandrosterone sulfate levels at birth are high and decrease drastically over the first month of life, followed by a more progressive decrease until age 6 months. 106 Hence, specific reference values for these endogenous substrates for various age groups should be gained first.
Global metabolomics studies can help identify biomarkers for enzymes and transporters, also in a paediatric population. This approach was taken by Tay‐Sontheimer et al. who identified a urinary biomarker to phenotype CYP2D6 activity. 107 Although that specific biomarker was not structurally identified, this example shows that metabolomic studies may identify new biomarkers in children.
8. CONCLUSION
Our understanding of the ontogeny of drug metabolism and transport in children has increased, notably the ontogeny of transporters, especially those in the liver and kidney. This increased knowledge has significant implications for understanding drug disposition of substrates in the younger age groups. Paediatric [14C]labelled microdosing and microtracing studies provide an opportunity to study the PK of drugs used in children, such as AAP and midazolam. Moreover, PBPK modelling helps us understand drug metabolism and transport pathways, and the impact of a change in a certain pathway. This approach should be used with some restraint until knowledge gaps on the ontogeny of drug disposition have been filled. The results of this review are of importance for paediatric drug development and current practice—with the ultimate aim of improving paediatric drug therapy.
COMPETING INTERESTS
There are no competing interests to declare.
ACKNOWLEDGEMENTS
The authors thank J. Hagoort for editorial assistance.
van Groen BD, Allegaert K, Tibboel D, de Wildt SN. Innovative approaches and recent advances in the study of ontogeny of drug metabolism and transport. Br J Clin Pharmacol. 2022;88(10):4285–4296. 10.1111/bcp.14534
REFERENCES
- 1. van den Anker J, Reed MD, Allegaert K, Kearns GL. Developmental changes in pharmacokinetics and pharmacodynamics. J Clin Pharmacol. 2018;58(Suppl 10):S10‐S25. [DOI] [PubMed] [Google Scholar]
- 2. Brouwer KL, Aleksunes LM, Brandys B, et al. Human ontogeny of drug transporters: review and recommendations of the pediatric transporter working group. Clin Pharmacol Ther. 2015;98(3):266‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kearns GL, Abdel‐Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE. Developmental pharmacology‐drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349(12):1157‐1167. [DOI] [PubMed] [Google Scholar]
- 4. Weiss CF, Glazko AJ, Weston JK. Chloramphenicol in the newborn infant. A physiologic explanation of its toxicity when given in excessive doses. N Engl J Med. 1960;262(16):787‐794. [DOI] [PubMed] [Google Scholar]
- 5. European Commission . Ethical considerations for clinical trials on medicinal products conducted with minors. In [DOI] [PubMed]
- 6. European Parliament and of the Council. Regulation (EU) . no 536/2014: Clinical trials on medicinal products for human use, and repealing Directive 2001/20/EC. In.
- 7. Alexander SP, Kelly E, Marrion NV, et al. THE CONCISE GUIDE TO PHARMACOLOGY 2017/18: overview. Br J Pharmacol. 2017;174(Suppl 1):S1‐S16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nigam SK. What do drug transporters really do? Nat Rev Drug Discov. 2015;14(1):29‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mooij MG, van de Steeg E, van Rosmalen J, et al. Proteomic analysis of the developmental trajectory of human hepatic membrane transporter proteins in the first three months of life. Drug Metab Dispos. 2016;44(7):1005‐1013. [DOI] [PubMed] [Google Scholar]
- 10. Prasad B, Gaedigk A, Vrana M, et al. Ontogeny of hepatic drug transporters as quantified by LC‐MS/MS proteomics. Clin Pharmacol Ther. 2016;100(4):362‐370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Groen BD, van de Steeg E, Mooij MG, et al. Proteomics of human liver membrane transporters: a focus on fetuses and newborn infants. Eur J Pharm Sci. 2018;124:217‐227. [DOI] [PubMed] [Google Scholar]
- 12. Prasad B, Johnson K, Billington S, et al. Abundance of drug transporters in the human kidney cortex as quantified by quantitative targeted proteomics. Drug Metab Dispos. 2016;44(12):1920‐1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wun Kathy Cheung K, van Groen BD, Spaans E, et al. A comprehensive analysis of ontogeny of renal drug transporters: mRNA analyses, quantitative proteomics and localization. Clin Pharmacol Ther. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li CY, Hosey‐Cojocari C, Basit A, Unadkat JD, Leeder JS, Prasad B. Optimized renal Transporter quantification by using aquaporin 1 and aquaporin 2 as anatomical markers: application in characterizing the ontogeny of renal transporters and its correlation with hepatic transporters in paired human samples. AAPS j. 2019;21(5):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cheung KWK, van Groen BD, Burckart GJ, Zhang L, de Wildt SN, Huang SM. Incorporating ontogeny in physiologically based pharmacokinetic modeling to improve Pediatric drug development: what we know about developmental changes in membrane transporters. J Clin Pharmacol. 2019;59(Suppl 1):S56‐S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Emoto C, Johnson TN, Neuhoff S, Hahn D, Vinks AA, Fukuda T. PBPK model of morphine incorporating developmental changes in hepatic OCT1 and UGT2B7 proteins to explain the variability in clearances in neonates and small infants. CPT Pharmacometrics Syst Pharmacol. 2018;7(7):464‐473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rhodin MM, Anderson BJ, Peters AM, et al. Human renal function maturation: a quantitative description using weight and postmenstrual age. Pediatr Nephrol. 2009;24(1):67‐76. [DOI] [PubMed] [Google Scholar]
- 18. Mooij MG, Nies AT, Knibbe CA, et al. Development of human membrane transporters: drug disposition and pharmacogenetics. Clin Pharmacokinet. 2016;55(5):507‐524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brackman DJ, Giacomini KM. Reverse translational research of ABCG2 (BCRP) in human disease and drug response. Clin Pharmacol Ther. 2018;103(2):233‐242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xu L, Shi Y, Zhuang S, Liu N. Recent advances on uric acid transporters. Oncotarget. 2017;8(59):100852‐100862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Passwell JH, Modan M, Brish M, Orda S, Boichis H. Fractional excretion of uric acid in infancy and childhood. Index of tubular maturation. Arch Dis Child. 1974;49(11):878‐882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baldree LA, Stapleton FB. Uric acid metabolism in children. Pediatr Clin North am. 1990;37(2):391‐418. [DOI] [PubMed] [Google Scholar]
- 23. Stiburkova B, Bleyer AJ. Changes in serum urate and urate excretion with age. Adv Chronic Kidney Dis. 2012;19(6):372‐376. [DOI] [PubMed] [Google Scholar]
- 24. van Groen BD, Bi C, Gaedigk R, et al. Alternative splicing of the SLCO1B1 gene: an exploratory analysis of isoform diversity in Pediatric liver. Clin Transl Sci. 2020;13(3):509‐519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhang M, Liu YH, Chang CS, et al. Quantification of gene expression while taking into account RNA alternative splicing. Genomics. 2018;111(6):1517‐1528. 10.1016/j.ygeno.2018.10.009 [DOI] [PubMed] [Google Scholar]
- 26. Klaassen CD, Aleksunes LM. Xenobiotic, bile acid, and cholesterol transporters: function and regulation. Pharmacol Rev. 2010;62(1):1‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yao J, Hong W, Huang J, Zhan K, Huang H, Hong M. N‐glycosylation dictates proper processing of organic anion transporting polypeptide 1B1. PLoS ONE. 2012;7(12):e52563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kent WJ, Sugnet CW, Furey TS, et al. The human genome browser at UCSC. Genome Res. 2002;12(6):996‐1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang L, Sweet DH. Renal organic anion transporters (SLC22 family): expression, regulation, roles in toxicity, and impact on injury and disease. AAPS j. 2013;15(1):53‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wegler C, Gaugaz FZ, Andersson TB, et al. Variability in mass spectrometry‐based quantification of clinically relevant drug transporters and drug metabolizing enzymes. Mol Pharm. 2017. [DOI] [PubMed] [Google Scholar]
- 31. Ladumor MK, Thakur A, Sharma S, et al. A repository of protein abundance data of drug metabolizing enzymes and transporters for applications in physiologically based pharmacokinetic (PBPK) modelling and simulation. Sci Rep. 2019;9(1):9709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Devuyst O, Burrow CR, Smith BL, Agre P, Knepper MA, Wilson PD. Expression of aquaporins‐1 and ‐2 during nephrogenesis and in autosomal dominant polycystic kidney disease. Am J Physiol. 1996;271(1 Pt 2):F169‐F183. [DOI] [PubMed] [Google Scholar]
- 33. Liu H, Wintour EM. Aquaporins in development ‐ a review. Reprod Biol Endocrinol. 2005;3(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vet NJ, Brussee JM, de Hoog M, et al. SkicInflammation and organ failure severely affect midazolam clearance in critically ill children. Am J Respir Crit Care Med. 2016;194(1):58‐66. [DOI] [PubMed] [Google Scholar]
- 35. le Vee M, Jouan E, Moreau A, Fardel O. Regulation of drug transporter mRNA expression by interferon‐gamma in primary human hepatocytes. Fundam Clin Pharmacol. 2011;25(1):99‐103. [DOI] [PubMed] [Google Scholar]
- 36. Evers R, Piquette‐Miller M, Polli JW, et al. Disease‐associated changes in drug transporters may impact the pharmacokinetics and/or toxicity of drugs: a white paper from the international Transporter consortium. Clin Pharmacol Ther. 2018;104(5):900‐915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Prakash C, Zuniga B, Song CS, et al. Nuclear receptors in drug metabolism. Drug Response and Drug Interact Nuclear Receptor Res. 2015;2:101178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nies AT, Koepsell H, Winter S, et al. Expression of organic cation transporters OCT1 (SLC22A1) and OCT3 (SLC22A3) is affected by genetic factors and cholestasis in human liver. Hepatology. 2009;50(4):1227‐1240. [DOI] [PubMed] [Google Scholar]
- 39. Matic M, de Wildt SN, Elens L, et al. SLC22A1/OCT1 genotype affects O‐desmethyltramadol exposure in newborn infants. Ther Drug Monit. 2016;38(4):487‐492. [DOI] [PubMed] [Google Scholar]
- 40. DeGorter MK, Xia CQ, Yang JJ, Kim RB. Drug transporters in drug efficacy and toxicity. Annu Rev Pharmacol Toxicol. 2012;52(1):249‐273. [DOI] [PubMed] [Google Scholar]
- 41. Smits A, Annaert P, Allegaert K. Drug disposition and clinical practice in neonates: cross talk between developmental physiology and pharmacology. Int J Pharm. 2013;452(1‐2):8‐13. [DOI] [PubMed] [Google Scholar]
- 42. Prasad B, Achour B, Artursson P, et al. Toward a consensus on applying quantitative liquid chromatography‐tandem mass spectrometry proteomics in translational pharmacology research: a white paper. Clin Pharmacol Ther. 2019;106(3):525‐543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Willmann S, Becker C, Burghaus R, et al. Development of a paediatric population‐based model of the pharmacokinetics of rivaroxaban. Clin Pharmacokinet. 2014;53(1):89‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schirm E, Tobi H, de Vries TW, Choonara I, de Jong‐van den Berg LT. Lack of appropriate formulations of medicines for children in the community. Acta Paediatr. 2003;92(12):1486‐1489. [DOI] [PubMed] [Google Scholar]
- 45. European Medicines Agency . ICH Topic M3 (R2) Non‐Clinical Safety Studies for the Conduct of Human Clinical Trials and Marketing Authorization for Pharmaceuticals. 2008.
- 46. Food and Drug Administration US Department of Health and Human Services Guidance for Industry Investigators and Reviewers . Exploratory IND Studies. 2006.
- 47. Salehpour M, Possnert G, Bryhni H. Subattomole sensitivity in biological accelerator mass spectrometry. Anal Chem. 2008;80(10):3515‐3521. [DOI] [PubMed] [Google Scholar]
- 48. Vuong LT, Blood AB, Vogel JS, Anderson ME, Goldstein B. Applications of accelerator MS in pediatric drug evaluation. Bioanalysis. 2012;4(15):1871‐1882. [DOI] [PubMed] [Google Scholar]
- 49. Turner MA, Mooij MG, Vaes WH, et al. Pediatric microdose and microtracer studies using 14C in Europe. Clin Pharmacol Ther. 2015;98(3):234‐237. [DOI] [PubMed] [Google Scholar]
- 50. Ethical Considerations For Clinical Trials On Medicinal Products Conducted With The Paediatric Population . ‐ Recommendations of the ad hoc group for the development of implementing guidelines for Directive 2001/20/EC relating to good clinical practice in the conduct of clinical trials on medicinal products for human use 2008.
- 51. Mooij MG, van Duijn E, Knibbe CA, et al. Successful use of [14C]paracetamol microdosing to elucidate developmental changes in drug metabolism. Clin Pharmacokinet. 2017;56(10):1185‐1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kleiber N, Calvier E, Mooij MG, et al. Enteral acetaminophen bioavailability in Pediatric intensive Care patients determined with an Oral microtracer and pharmacokinetic modeling to optimize dosing. Crit Care Med. 2019. [DOI] [PubMed] [Google Scholar]
- 53. Hines RN. The ontogeny of drug metabolism enzymes and implications for adverse drug events. Pharmacol Ther. 2008;118(2):250‐267. [DOI] [PubMed] [Google Scholar]
- 54. de Wildt SN, Kearns GL, Leeder JS, van den Anker JN. Cytochrome P450 3A: ontogeny and drug disposition. Clin Pharmacokinet. 1999;37(6):485‐505. [DOI] [PubMed] [Google Scholar]
- 55. van Groen BD, Krekels EHJ, Mooij MG, et al. The oral bioavailability and metabolism of midazolam in stable critically ill children: a pharmacokinetic microtracing study. Accepted for Publication in Clin Pharmacol Ther. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Brussee JM, Yu H, Krekels EHJ, et al. First‐pass CYP3A‐mediated metabolism of midazolam in the Gut Wall and liver in preterm neonates. CPT Pharmacometrics Syst Pharmacol. 2018;7(6):374‐383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Brussee JM, Yu H, Krekels EHJ, et al. Characterization of intestinal and hepatic CYP3A‐mediated metabolism of midazolam in children using a physiological population pharmacokinetic modelling approach. Pharm Res. 2018;35(9):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brill MJ, van Rongen A, Houwink AP, et al. Midazolam pharmacokinetics in morbidly obese patients following semi‐simultaneous oral and intravenous administration: a comparison with healthy volunteers. Clin Pharmacokinet. 2014;53(10):931‐941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. de Wildt SN, Kearns GL, Hop WC, Murry DJ, Abdel‐Rahman SM, van den Anker JN. Pharmacokinetics and metabolism of oral midazolam in preterm infants. Br J Clin Pharmacol. 2002;53(4):390‐392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ince I, de Wildt SN, Peeters MY, et al. Critical illness is a major determinant of midazolam clearance in children aged 1 month to 17 years. Ther Drug Monit. 2012;34(4):381‐389. [DOI] [PubMed] [Google Scholar]
- 61. Bai JPF, Burckart GJ, Mulberg AE. Literature review of gastrointestinal physiology in the elderly, in Pediatric patients, and in patients with gastrointestinal diseases. J Pharm Sci. 2016;105(2):476‐483. [DOI] [PubMed] [Google Scholar]
- 62. Debotton N, Dahan A. A mechanistic approach to understanding oral drug absorption in pediatrics: an overview of fundamentals. Drug Discov Today. 2014;19(9):1322‐1336. [DOI] [PubMed] [Google Scholar]
- 63. Mooij MG, de Koning BA, Huijsman ML, de Wildt SN. Ontogeny of oral drug absorption processes in children. Expert Opin Drug Metab Toxicol. 2012;8(10):1293‐1303. [DOI] [PubMed] [Google Scholar]
- 64. Bjorkman S. Prediction of drug disposition in infants and children by means of physiologically based pharmacokinetic (PBPK) modelling: theophylline and midazolam as model drugs. Br J Clin Pharmacol. 2005;59(6):691‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Schadt S, Bister B, Chowdhury SK, et al. A decade in the MIST: learnings from investigations of drug metabolites in drug development under the "metabolites in safety testing" regulatory Guidances. Drug Metab Dispos. 2018;46(6):865‐878. [DOI] [PubMed] [Google Scholar]
- 66. Yu H, Bischoff D, Tweedie D. Challenges and solutions to metabolites in safety testing: impact of the international conference on harmonization M3(R2) guidance. Expert Opin Drug Metab Toxicol. 2010;6(12):1539‐1549. [DOI] [PubMed] [Google Scholar]
- 67. van Groen BD, van Duijn E, de Vries A, et al. Proof of concept: first pediatric [14C]microtracer study to create metabolite profiles of midazolam. Accepted for Publication in Clin Pharmacol Ther. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lappin G, Kuhnz W, Jochemsen R, et al. Use of microdosing to predict pharmacokinetics at the therapeutic dose: experience with 5 drugs. Clin Pharmacol Ther. 2006;80(3):203‐215. [DOI] [PubMed] [Google Scholar]
- 69. Bosgra S, Vlaming ML, Vaes WH. To apply microdosing or not? Recommendations to single out compounds with non‐linear pharmacokinetics. Clin Pharmacokinet. 2016;55(1):1‐15. [DOI] [PubMed] [Google Scholar]
- 70. van Nuland M, Rosing H, Huitema ADR, Beijnen JH. Predictive value of microdose pharmacokinetics. Clin Pharmacokinet. 2019. [DOI] [PubMed] [Google Scholar]
- 71. van Groen BD, Vaes WH, Park BK, et al. Dose‐linearity of the pharmacokinetics of an intravenous [(14) C]midazolam microdose in children. Br J Clin Pharmacol. 2019;85(10):2332‐2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Mooij MG, van Duijn E, Knibbe CA, et al. Pediatric microdose study of [(14)C]paracetamol to study drug metabolism using accelerated mass spectrometry: proof of concept. Clin Pharmacokinet. 2014;53(11):1045‐1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gordi T, Baillie R, Vuong Le T, et al. Pharmacokinetic analysis of 14C‐ursodiol in newborn infants using accelerator mass spectrometry. J Clin Pharmacol. 2014;54(9):1031‐1037. [DOI] [PubMed] [Google Scholar]
- 74. Garner CR, Park KB, French NS, et al. Observational infant exploratory [(14)C]‐paracetamol pharmacokinetic microdose/therapeutic dose study with accelerator mass spectrometry bioanalysis. Br J Clin Pharmacol. 2015;80(1):157‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Menon K, Ward R, Canadian Critical Care Trials G . A study of consent for participation in a non‐therapeutic study in the pediatric intensive care population. J Med Ethics. 2014;40(2):123‐126. [DOI] [PubMed] [Google Scholar]
- 76. Baarslag MA, Jhingoer S, Ista E, Allegaert K, Tibboel D, van Dijk M. How often do we perform painful and stressful procedures in the paediatric intensive care unit? A prospective observational study. Aust Crit Care. 2019;32(1):4‐10. [DOI] [PubMed] [Google Scholar]
- 77. Ince I, Knibbe CA, Danhof M, de Wildt SN. Developmental changes in the expression and function of cytochrome P450 3A isoforms: evidence from in vitro and in vivo investigations. Clin Pharmacokinet. 2013;52(5):333‐345. [DOI] [PubMed] [Google Scholar]
- 78. Calvier EAM, Krekels EHJ, Yu H, et al. Drugs being eliminated via the same pathway will not always require similar Pediatric dose adjustments. CPT Pharmacometrics Syst Pharmacol. 2018;7(3):175‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Brussee JM, Krekels EHJ, Calvier EAM, et al. A Pediatric covariate function for CYP3A‐mediated midazolam clearance can scale clearance of selected CYP3A substrates in children. AAPS j. 2019;21(5):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Department of Health and Human Services, Food and Drug Administration . Best Pharmaceuticals for Children Act and Pediatric Research Equity Act ‐ Status Report to Congress. 2016.
- 81. European Medicines Agency . 10‐year Report to the European Commission: General report on the experience acquired as a result of the application of the Paediatric Regulation (EMA/231225/2015). 2016.
- 82. Stiers JL, Ward RM. Newborns, one of the last therapeutic orphans to be adopted. JAMA Pediatr. 2014;168(2):106‐108. [DOI] [PubMed] [Google Scholar]
- 83. Food and Drug Administration . Guidance for Industry: How to Comply with the Pediatric Research Equity Act 2005.
- 84. Schrier L, Hadjipanayis A, Stiris T, et al. Off‐label use of medicines in neonates, infants, children, and adolescents: a joint policy statement by the European academy of Paediatrics and the European society for developmental perinatal and Pediatric pharmacology. Eur J Pediatr. 2020;179(5):839‐847. [DOI] [PubMed] [Google Scholar]
- 85. Roth‐Cline M, Nelson RM. Microdosing studies in children: a US regulatory perspective. Clin Pharmacol Ther. 2015;98(3):232‐233. [DOI] [PubMed] [Google Scholar]
- 86. Verscheijden LFM, Koenderink JB, Johnson TN, de Wildt SN, Russel FGM. Physiologically‐based pharmacokinetic models for children: starting to reach maturation? Pharmacol Ther. 2020;211:107541. [DOI] [PubMed] [Google Scholar]
- 87. Food and Drug Administration . General Clinical Pharmacology Considerations for Neonatal Studies for Drugs and Biological Products Guidance for Industry ‐ DRAFT. 2019.
- 88. Wang Y, Zhu H, Madabushi R, Liu Q, Huang SM, Zineh I. Model‐informed drug development: current US regulatory practice and future considerations. Clin Pharmacol Ther. 2019;105(4):899‐911. [DOI] [PubMed] [Google Scholar]
- 89. Grimstein M, Yang Y, Zhang X, Grillo J, Huang SM, Zineh I, Wang Y. Physiologically Based Pharmacokinetic Modeling in Regulatory Science: An Update From the U.S. Food and Drug Administration's Office of Clinical Pharmacology. In: Journal of Pharmaceutical Sciences, 2019. 108(1);21‐25. [DOI] [PubMed] [Google Scholar]
- 90. Shebley M, Sandhu P, Emami Riedmaier A, et al. Physiologically based pharmacokinetic model qualification and reporting procedures for regulatory submissions: a consortium perspective. Clin Pharmacol Ther. 2018;104:88‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Wagner C, Zhao P, Pan Y, et al. Application of physiologically based pharmacokinetic (PBPK) modeling to support dose selection: report of an FDA public workshop on PBPK. CPT Pharmacometrics Syst Pharmacol. 2015;4(4):226‐230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Johnson TN, Zhou D, Bui KH. Development of physiologically based pharmacokinetic model to evaluate the relative systemic exposure to quetiapine after administration of IR and XR formulations to adults, children and adolescents. Biopharm Drug Dispos. 2014;35(6):341‐352. [DOI] [PubMed] [Google Scholar]
- 93. Dai D, Feinstein JA, Morrison W, Zuppa AF, Feudtner C. Epidemiology of polypharmacy and potential drug‐drug interactions among Pediatric patients in ICUs of U.S. Children's hospitals. Pediatr Crit Care Med. 2016;17(5):e218‐e228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Thomson MM, Hines RN, Schuetz EG, Meibohm B. Expression patterns of organic anion transporting polypeptides 1B1 and 1B3 protein in human Pediatric liver. Drug Metab Dispos. 2016;44(7):999‐1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Salem F, Johnson TN, Barter ZE, Leeder JS, Rostami‐Hodjegan A. Age related changes in fractional elimination pathways for drugs: assessing the impact of variable ontogeny on metabolic drug‐drug interactions. J Clin Pharmacol. 2013;53(8):857‐865. [DOI] [PubMed] [Google Scholar]
- 96. Elmorsi Y, Barber J, Rostami‐Hodjegan A. Ontogeny of hepatic drug transporters and relevance to drugs used in pediatrics. Drug Metab Dispos. 2016;44(7):992‐998. [DOI] [PubMed] [Google Scholar]
- 97. van der Zanden TM, de Wildt SN, Liem Y, Offringa M, de Hoog M, Dutch Paediatric Pharmacotherapy Expertise Network N. Developing a paediatric drug formulary for the Netherlands. Arch Dis Child. 2017;102(4):357‐361. [DOI] [PubMed] [Google Scholar]
- 98. Anderson BJ, Holford NH. Understanding dosing: children are small adults, neonates are immature children. Arch Dis Child. 2013;98(9):737‐744. [DOI] [PubMed] [Google Scholar]
- 99. Gerrard SE, Walsh J, Bowers N, Salunke S, Hershenson S. Innovations in Pediatric drug formulations and Administration Technologies for low Resource Settings. Pharmaceutics. 2019;11(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Darwich AS, Ogungbenro K, Vinks AA, et al. Why has model‐informed precision dosing not yet become common clinical reality? Lessons from the past and a roadmap for the future. Clin Pharmacol Ther. 2017;101(5):646‐656. [DOI] [PubMed] [Google Scholar]
- 101. Keizer RJ, ter Heine R, Frymoyer A, Lesko LJ, Mangat R, Goswami S. Model‐informed precision dosing at the bedside: scientific challenges and opportunities. CPT Pharmacometrics Syst Pharmacol. 2018;7:785‐787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wilkinson MD, Dumontier M, Aalbersberg IJ, et al. The FAIR guiding principles for scientific data management and stewardship. Sci Data. 2016;3(1):160018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Nantasanti S, de Bruin A, Rothuizen J, Penning LC, Schotanus BA. Concise review: organoids are a powerful tool for the study of liver disease and personalized treatment design in humans and animals. Stem Cells Transl Med. 2016;5(3):325‐330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Rodrigues D, Rowland A. From endogenous compounds as biomarkers to plasma‐derived Nanovesicles as liquid biopsy; has the Golden age of translational pharmacokinetics‐absorption, distribution, metabolism, excretion‐drug‐drug interaction science finally arrived? Clin Pharmacol Ther. 2019;105(6):1407‐1420. [DOI] [PubMed] [Google Scholar]
- 105. Muller F, Sharma A, Konig J, Fromm MF. Biomarkers for in vivo assessment of Transporter function. Pharmacol Rev. 2018;70(2):246‐277. [DOI] [PubMed] [Google Scholar]
- 106. de Peretti E, Forest MG. Pattern of plasma dehydroepiandrosterone sulfate levels in humans from birth to adulthood: evidence for testicular production. J Clin Endocrinol Metab. 1978;47(3):572‐577. [DOI] [PubMed] [Google Scholar]
- 107. Tay‐Sontheimer J, Shireman LM, Beyer RP, et al. Detection of an endogenous urinary biomarker associated with CYP2D6 activity using global metabolomics. Pharmacogenomics. 2014;15(16):1947‐1962. [DOI] [PMC free article] [PubMed] [Google Scholar]


