Abstract
The use of cricoid pressure (CP) to prevent aspiration during rapid sequence induction (RSI) has become controversial, although CP is considered central to the practice of RSI. There is insufficient research to support its efficacy in reducing aspiration, and emerging concerns it reduces the first‐pass success (FPS) of intubation. This systematic review aims to assess the safety and efficacy of CP during RSI in EDs by investigating its effect on FPS and the incidence of complications, including gastric regurgitation and aspiration. A systematic review of four databases was performed for all primary research investigating CP during RSI in EDs. The primary outcome was FPS; secondary outcomes included complications such as gastric regurgitation, aspiration, hypoxia, hypotension and oesophageal intubation. After screening 4208 citations, three studies were included: one randomised controlled trial (n = 54) investigating the incidence of aspiration during the application of CP and two registry studies (n = 3710) comparing the rate of FPS of RSI with and without CP. The results of these individual studies are not sufficient to draw concrete conclusions but do suggest that aspiration occurs regardless of the application of CP, and that FPS is not reduced by the application of CP. There is insufficient evidence to conclude whether applying CP during RSI in EDs affects the rate of FPS or the incidence of complications such as aspiration. Further research in the ED, including introducing CP usage into other existing airway registries, is needed.
Keywords: airway management, airway maneuvers, cricoid pressure, emergency department, sellick manoeuvre
Key findings.
This systematic review of the literature explored the effectiveness and risks of applying cricoid pressure during rapid sequence induction in the ED.
There is currently limited evidence to conclude whether applying cricoid pressure during airway management in the ED affects first‐pass success at endotracheal intubation or reduces the rate of complications such as gastric regurgitation and aspiration.
Further research into the effectiveness of cricoid pressure during rapid sequence induction and the minimum effective force is needed to guide clinical practice.
Introduction
Rapid sequence induction (RSI) involves the administration of an induction agent and a muscle relaxant in rapid succession to facilitate endotracheal intubation. 1 By omitting masked ventilation, RSI enables the airway to be secured rapidly and minimises air entry into the stomach, which can increase the risk of gastric regurgitation and aspiration of stomach contents. 1
RSI in the ED is a high‐risk procedure with increased risk of complications such as oxygen desaturation, oesophageal intubation, pneumothorax, hypotension and cardiac arrest. 2 Patients presenting to the ED are often unfasted, which increases the risk of regurgitation and aspiration of gastric contents. 3 The incidence of regurgitation and aspiration has been found to be between 3 and 13% of ED intubations, and the risk increases with repeated intubation attempts and prolonged time to intubation. 4 , 5 , 6 Successful intubation on the first attempt, known as first‐pass success (FPS), is thus an important goal of RSI. 2 , 4
Cricoid pressure (CP) is a manoeuvre used during RSI to further reduce the risk of gastric regurgitation and aspiration. First described in 1961, CP involves the operator applying a downwards force to the cricoid cartilage with the aim of occluding the oesophagus between the cricoid ring and cervical vertebrae. 4 Sellick performed an observational study and reported the incidence of gastric regurgitation following the immediate release of CP in 3 out of 26 patients. Despite the limitations in the present study, CP was readily introduced into the practice of RSI and has remained central to its practice since. 5 , 6 , 7
Since its introduction, the use of CP has become controversial. 1 First, the anatomical and physiological basis of the manoeuvre has been challenged. MRI studies have shown that the oesophagus often lies laterally to the cricoid cartilage, leading to concerns that applying CP does not occlude the oesophagus. 8 This finding has since been refuted by more recent studies, which have shown that the postcricoid hypopharynx, part of the upper oesophageal sphincter, is attached to the cricoid cartilage and causes occlusion of the oesophagus during CP regardless of its position. 9 , 10 The anatomical basis for CP conflicts with the physiological evidence for the manoeuvre, which suggests that it may paradoxically favour aspiration. Balloon catheterisation of the oesophagus during CP has shown that applying pressure to the upper oesophageal sphincter reduces pressure at the lower oesophageal sphincter, increasing the likelihood of gastric regurgitation. 11 The definitive effects of CP on oesophageal anatomy and physiology are still yet to be established and remain a source of controversy for the manoeuvre.
The efficacy of CP in preventing gastric regurgitation has also come under scrutiny. While there have been attempts to determine the occurrence of aspiration with intubations involving CP, there is no standardised definition of aspiration; thus, it is difficult to compare studies in this area. 12 It is also important to note that the detection of aspiration is difficult to calibrate, and that aspiration may occur unwitnessed prior to RSI, which may impact the validity of these studies. 12 Of the available data, case series and staff surveys have reported regurgitation and aspiration of gastric contents despite the application of CP. 13 A prospective study of emergency airway management reported new or unexpected radiographic pulmonary infiltrates following 12 out of 297 intubations, nine of which involved the application of CP; however, while the use of pulmonary infiltrates has traditionally been used as a surrogate marker for aspiration, this may not be clinically valid. More recent randomised controlled trials and systematic reviews investigating CP in elective anaesthesia have demonstrated that CP does not significantly reduce the risk of gastric regurgitation and aspiration. 14 , 15 The true effect of CP on regurgitation is difficult to extrapolate from the available data and remains to be determined for populations undergoing RSI in the ED.
In addition to suggestions that CP does not effectively prevent gastric regurgitation as intended, there are concerns it may increase the difficulty of intubation and adversely affect patient outcomes. CP has been shown to worsen Cormack and Lehane's views during intubation in the operating theatre, likely because of the downward force of CP opposing the upward force of the laryngoscope and distorting the normal anatomy of the airway. 15 , 16 Poor laryngoscopic view has been associated with prolonged time to intubation and reduced FPS, which increases the risk of complications such as hypoxia, oesophageal intubation, regurgitation, aspiration, airway trauma and cardiac arrest. 14 , 16 , 17 However, it is likely that the effects of difficult intubation as a result of CP are overstated, as CP has equally been shown to not affect FPS, and in practice, it is recommended that CP is removed in the case of difficult intubation. 15 , 16
Despite the controversy surrounding the use of CP during RSI, the current literature has not been able to provide definitive insights into intubation outcomes using this manoeuvre. A 2015 Cochrane review 18 did not identify any completed randomised controlled trials addressing the use of CP during RSI, and two systematic reviews investigating CP during elective surgeries yielded conflicting results; White et al. 15 found that FPS was significantly reduced, whereas Hung et al. 14 found no significant difference in FPS when CP was applied. There have been no systematic reviews to date investigating the use of CP during RSI in the ED.
Patients requiring intubation in the ED represent a unique demographic; they are often unfasted, comorbid, may be at imminent risk of cardiovascular or respiratory compromise, and may have airway trauma or the presence of blood, secretions and vomitus in the airway. 19 As a result of these factors, intubations in the ED have a higher risk of complications, including regurgitation, hypoxia, oesophageal intubation and cardiac arrest. 20 , 21 , 22 , 23
The aim of this systematic review is to assess the safety and efficacy of CP during RSI in EDs by investigating its effect on FPS and the incidence of complications, including gastric regurgitation and aspiration.
Methods
Search strategy
The Cochrane database of systematic reviews, PubMed, Embase and MEDLINE databases were searched from 2014 to May 2021 to supplement the data search from a 2015 Cochrane review. 18 Five authors (ET, HA, NL, PS, SM) independently searched the databases using the following search strategy; (cricoid OR ‘rapid sequence’ OR Sellick OR ‘airway management’) AND intubation. Searches were limited to studies in English and involving human participants. Reference lists of included studies were reviewed for other potentially relevant studies (Fig. 1).
Figure 1.
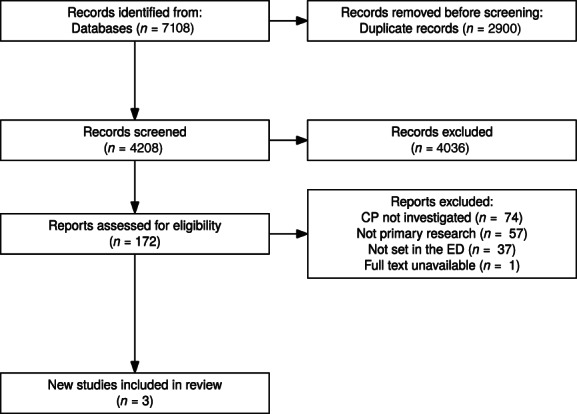
PRISMA literature search summary. CP, cricoid pressure.
Study eligibility
All primary research investigating CP during RSI in the ED was included. Studies performed on models, animals or cadavers were excluded. Included studies had to report on either FPS or complications such as aspiration (Table 1). Three reviewers (ET, HA and NL) assessed studies eligible for inclusion.
TABLE 1.
Details of the studies which met the inclusion criteria
| Study | Study design | Setting | Population | Patients | Outcomes | Results | Conclusions | Limitations |
|---|---|---|---|---|---|---|---|---|
| Alkhouri et al., 2017 5 | Registry | 43 Australian and New Zealand EDs | All patients undergoing RSI in the ED | 1112 CP: 2467 no CP |
FPS Success at three or more attempts |
FPS with CP 84.7% versus 83.3% without, P = 0.7460 Success at three or more attempts with CP 59.8% versus 55.0% without, P = 0.7387 |
CP did not significantly affect the rate of FPS or successful intubation after three or more attempts |
Potential for bias towards EDs with accredited emergency physicians Potential for underreporting of adverse events |
| Ghedina et al., 2020 27 | Registry | 30 Australian and New Zealand EDs | Paediatric patients aged 0–15 years undergoing RSI in the ED | 60 CP: 196 no CP | FPS | FPS 86.7% with CP versus FPS 78.6% without CP | Higher FPS was noted with the use of CP |
Small sample size meant statistical significance was not calculated Potential for bias towards EDs with accredited emergency physicians Potential for underreporting of adverse events |
| Trethewy et al., 2018 28 | Randomised controlled trial | 2 Australian EDs (New South Wales) | Adults >18 years old undergoing RSI in the ED | 25 measured force of CP: 29 blinded to force of CP | Gastric regurgitation |
Gastric regurgitation occurred despite the application of CP Patients were positive for oropharyngeal pepsin (11/54), tracheal pepsin (3/54) and treated with antibiotics for clinical aspiration (7/54) |
The ideal force of CP could not be maintained during intubation Applying suboptimal CP did not eliminate the risk of gastric regurgitation |
Small sample size owing to the abandonment of the study before the calculated sample size of 106 patients was reached There was no significant difference in the force of CP applied between groups, hence outcomes could not be compared between CP and a control |
CP, cricoid pressure; FPS, first‐pass success.
Data extraction
Three reviewers (ET, HA and NL) independently extracted data from eligible studies. Data from each study were entered under the following headings: study design, setting, population, patients, outcomes, results and limitations. The quality of studies was assessed by three reviewers (ET, HA and NL) using the Mixed Methods Appraisal Tool (MMAT) 24 and the Cochrane Collaboration's tool for assessing the risk of bias. 25 Disagreements were resolved by discussion of full article content with the remaining reviewers.
Outcomes
The primary outcome of this study was the rate of FPS in intubations where CP was applied compared to when it was not. Secondary outcomes involved the incidence of complications, including gastric regurgitation, aspiration, oxygen desaturation, hypotension and oesophageal intubation.
Data analysis
Because of the heterogeneity of the three studies identified, statistical analysis could not be performed on this cohort.
Reporting
The present study was reported in accordance with the PRISMA guidelines. 26
Results
Literature search
The systematic literature search of four databases yielded 7108 studies, which was reduced to 4208 following the removal of duplicates. No further studies were identified through searching reference lists of relevant citations. After screening titles and abstracts, 172 studies remained for full‐text screening. Four studies were identified as meeting the inclusion criteria; however, one was excluded after the authors were contacted and confirmed there was no full‐text report available. 29 Three studies were included for data extraction; one randomised controlled trial (n = 54) investigating the incidence of aspiration during the application of CP, and two registry studies (n = 3710) comparing the rate of FPS of RSI with and without CP. The quality of these studies was assessed using the MMAT 24 and the Cochrane Collaboration's risk of bias tool 25 (Fig. 2). The registry by Alkhouri et al. 5 was identified as a high‐quality observational study, and the registry by Ghedina et al. 27 and randomised controlled trial by Trethewy et al. 28 were identified as intermediate quality studies with a moderate risk of bias.
Figure 2.
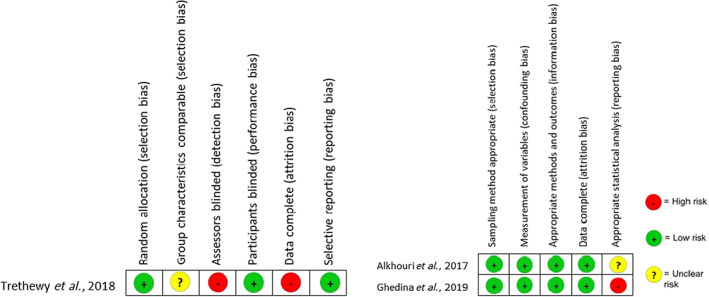
Risk of bias summary of included studies. Developed using the Mixed Methods Appraisal Tool and Cochrane risk of bias tool.
Primary outcome: FPS
Two registry studies (n = 3710) reported the rate of FPS of RSI in patients who were intubated with and without the use of CP. 5 , 27 Both studies analysed patient data collected through the Australia and New Zealand ED Airway Registry (ANZEDAR), with Alkhouri et al. 5 (n = 3710) reporting on adult and paediatric populations, and Ghedina et al. 27 (n = 256) reporting on the paediatric population only. In the combined adult and paediatric population, CP did not have a significant effect on FPS (84.7% FPS if CP used vs 83.3% FPS without CP, P = 0.7460) or successful intubation after three or more attempts (59.8% success if CP used, 55.0% without CP, P = 0.7387). The authors applied χ 2‐test or Fisher's exact test, as appropriate, to compare groups of categorical data related to CP. In the paediatric population, the rate of FPS with CP was 86.7%, compared to 78.6% without CP. Statistical significance was not reported because of the small sample size.
Secondary outcomes: complications
One randomised controlled trial (n = 54) investigated the incidence of aspiration when CP operators could measure and aim to apply the target force of CP in comparison to when operators were blinded to the force of CP they were delivering. 28 In the pilot study, only 25% of operators applied the target force of CP; hence, this was deemed an appropriate control in the ED setting. 30 The study was abandoned after 54 patients as the delivery of CP fell below the therapeutic force in both groups during laryngoscopy. In the 54 patients, 11 had evidence of gastric contents in the oropharynx, three in the trachea, and seven out of 54 were treated for clinical aspiration.
Discussion
RSI in the ED is a high‐risk procedure, posing significant risks to already critically ill patients. To date, there has not been strong evidence to conclude whether the use of CP in this population increases FPS or reduces the risks of complications, including gastric regurgitation and aspiration. This is the first systematic review investigating the outcomes of CP during RSI in the ED setting to yield results. Three studies were included in this review, consisting of two separate patient cohorts across 43 Australian and New Zealand EDs. Intubations on 3508 adults and 256 paediatric patients were available for analysis; 3710 reporting rates of FPS, and 54 investigated the incidence of gastric regurgitation and aspiration. The results of these studies suggest that CP does not affect the rate of FPS during RSI in the ED and does not prevent the occurrence of regurgitation and aspiration in this setting. However, as most of the results have arisen from observational data, reported by a multitude of health professionals and with no control over the method of CP application, this data is at a high risk of clinical bias. Additionally, it has been shown that the force of CP applied even among trained physicians varies greatly in practice and have not measured the force applied by each operator, it is unknown whether the results obtained were taken from cases where CP was appropriately applied, and what the effect of applying too little or too great force may be. 30 Therefore, the clinical significance of these results should be interpreted with caution.
An interesting conclusion made by Trethewy et al. 28 was that the recommended force of CP could not be maintained during laryngoscopy. It has been demonstrated that 30 N of force applied to the cricoid cartilage is sufficient to occlude the oesophagus at pressures above those reached in stomach of supine anaesthetised patients. 31 Trethewy et al. are the first to report the use of scales to investigate the force of CP applied during RSI in human participants. The authors found that while the target force of CP was reached during the initiation of RSI, it could not be maintained at the commencement of laryngoscopy. As this is a novel method of investigation, it is uncertain if the observed change in force applied during CP is a common occurrence and how a reduction in force applied affects the risk of aspiration. A 1992 study of 10 cadavers suggested that a force of 20 N may be sufficient to occlude the oesophagus, but this has not been investigated during laryngoscopy in clinical practice. 32
There have been previous systematic reviews investigating the outcomes of CP during endotracheal intubation in other settings. A 2015 Cochrane review investigating the outcomes of CP during RSI in any setting did not identify any completed randomised controlled trials for analysis. 18 In 2020, White et al. 15 investigated the effect of CP on the incidence of aspiration and intubating conditions. They identified 12 studies; nine involving non‐RSI intubations in the operating room, two involving RSI in the operating room and the study by Trethewy et al. 28 included in this review involving RSI performed in the ED. The results demonstrated that CP did not significantly affect the incidence of aspiration but did significantly reduce the risk of FPS. However, as subgroup analysis for RSI intubations could not be performed for FPS, the effect of CP on FPS during RSI could not be established in this review. A similar systematic review performed in 2021 by Hung et al. 14 identified five studies involving intubation performed in the operating theatre, one of which involving RSI in approximately a third of intubations. This review reported no significant effect on FPS or laryngoscopic view when CP was applied and did not investigate the risk of aspiration. The discrepancy in the results of these similar systematic reviews may be attributed to the heterogeneity of the randomised controlled trials included for analysis. Hung et al. 14 found several sources of heterogeneity in the available literature, including the intubation approach and devices used, level of operator skill, patient populations and discrepancies in the definitions of study parameters. As the available studies are so varied, it is difficult to appreciate the true effect of CP on intubation outcomes in the general population.
Limitations
There are some limitations to this review, the most notable being the lack of quality studies available for inclusion. The effect of CP on FPS was determined only from observational data; although this dataset involved a significant patient cohort and included statistical analysis, the lack of a calibrated definition of CP and method of its application in this cohort means this data has the potential for clinical bias and is best interpreted as a qualitative outcome. While the study investigating CP and the incidence of aspiration did control for the force of CP applied, it was found that in practice, this varied greatly and the proposed ideal force of CP could not be maintained during intubation; hence, the study was abandoned after 54 patients. Furthermore, as only one dataset was available for each outcome, statistical analysis was not possible for this review. The lack of studies in this area, and the absence of controlled variables and small patient cohorts of the included studies, make it difficult to determine the true effect of CP on FPS and the risk of aspiration.
A critical flaw of CP is that its practice is variable and unstandardised, making it difficult to analyse the true effect of CP in even the most robust studies. Clark et al. found that only 25% of emergency healthcare providers delivered the target force of CP, 30 and further survey responses by anaesthetic and ED staff have shown variations in the understanding of the location and force required for CP, as well as variation in the expertise of the operator. 7 , 33 , 34 , 35 The effect of these variables on the efficacy of CP in preventing aspiration and on the FPS of intubations involving CP is not controlled for in registry studies, which constitute a large portion of this systematic review, and therefore these studies have low internal validity. The true effect of CP may be over or underestimated by data that has not been calibrated for the difference in forces or placement of the manoeuvre, or for the experience of the operator; hence, the results of such data should be interpreted with discretion.
There are many challenges that may be hindering the progress of research into CP. After its initial description in 1961, CP has remained standard in the practice of RSI. A common principle of medical research suggests that when an intervention is so ingrained in common practice, investigation into the intervention is not necessary. 18 This principle has likely prevented research into CP until only recently, with the first randomised controlled trial in elective surgeries published in 2001, and in RSI intubations in 2018. 28 , 36 However, because of the risks associated with CP and uncertainty surrounding its efficacy, it is important that further research is conducted to determine its safety and efficacy in current practice.
Another reason for the lack of available evidence, particularly in the setting of RSI and in the ED, is the feasibility of research in this area. While a large randomised controlled trial comparing CP to a control such as a sham CP in ED patients at risk of aspiration would be of the highest clinical value, it would be unethical to randomly allocate patients to have CP withheld when it is central to the practice of RSI.
Physician scepticism may be impeding the progression of research into CP. A survey of Australian and New Zealand anaesthetists revealed that 23% of physicians did not routinely use CP in patients at risk of aspiration for reasons including a lack of evidence proving its efficacy, research demonstrating difficulty or adverse events using CP, and personal experience of CP causing difficult intubation or adverse events. 6 Of all respondents, 39.8% believed that CP reduced the risk of aspiration, 23.8% believed it did not and 36.3% were unsure. While more robust studies into CP may alleviate these concerns, the current controversy and lack of research may deter physicians from participating in research, which presents a significant obstacle for guiding practice.
Another limitation of the present study and the available data is that outcomes in high‐risk populations were not investigated. Patients with altered airway anatomy, difficulty with jaw and/or neck mobility, obstetric patients and obese patients may be at greater risk of intubation related complications and may warrant closer investigation. 37 While these groups were not excluded from the available studies, subgroup analysis was not performed, possibly because there is a low prevalence of these patients requiring intubation in EDs.
It is possible that there are additional relevant citations in languages other than English, which were not included in this review. There is also a possibility that there are relevant citations beyond the 2014–2021 time frame searched for this review; however, a Cochrane review in 2015 yielded no relevant randomised controlled trials, and manual review of reference lists of citations did not identify any other relevant studies, the existence of additional citations is unlikely.
Future directions
Additional primary research into the outcomes of CP during RSI in EDs is needed to determine its safety and efficacy in this setting. As randomised controlled trials pose many ethical and logistical challenges, large scale observational data would be more appropriate in this population. This systematic review is a precursor to a targeted analysis including an adjusted statistical model to investigate the outcomes of CP collated through the ANZEDAR, which has over 5500 data entries of RSI performed in EDs. Many international ED airway registries were identified by this review but were excluded as they did not include CP as an investigation parameter. Inclusion of CP in these registries would easily increase the data available on the manoeuvre and its outcomes. Further considerations into the force of CP able to be maintained during intubation and the minimum force effective at reducing the risk of gastric regurgitation would also help guide clinical practice.
Conclusion
Emergency RSI is a high‐risk procedure where FPS without adverse events is essential for optimising intubation outcomes in critically ill patients. There is currently inadequate evidence to conclude whether CP during RSI in the ED affects FPS at intubation or reduces complications such as gastric regurgitation and aspiration. Further primary research into the outcomes of CP in EDs and investigation into the minimum effective force of CP are needed to guide clinical decision making in this area.
Acknowledgement
Open access publishing facilitated by University of New South Wales, as part of the Wiley – University of New South Wales agreement via the Council of Australian University Librarians.
Author contributions
All authors independently searched the databases. ET, HA and NL reviewed the full‐text articles eligible for inclusion. ET drafted the manuscript. All authors revised the manuscript and approved the final draft.
Competing interests
SM is a section editor for Emergency Medicine Australasia.
Data availability statement
Data sharing not applicable ‐ no new data generated.
References
- 1. Avery P, Morton S, Raitt J, Lossius HM, Lockey D. Rapid sequence induction: Where did the consensus go? Scand. J. Trauma Resusc. Emerg. Med. 2021; 29: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad. Emerg. Med. 2013; 20: 71–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: Airway outcomes and complications. Anesthesiology 2011; 114: 42–8. [DOI] [PubMed] [Google Scholar]
- 4. Sellick B. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet 1961; 278: 404–6. [DOI] [PubMed] [Google Scholar]
- 5. Alkhouri H, Vassiliadis J, Murray M et al. Emergency airway management in Australian and New Zealand emergency departments: A multicentre descriptive study of 3710 emergency intubations. Emerg. Med. Australas. 2017; 29: 499–508. [DOI] [PubMed] [Google Scholar]
- 6. Mistry R, Frei DR, Badenhorst C, Broadbent J. A survey of self‐reported use of cricoid pressure amongst Australian and New Zealand anaesthetists: Attitudes and practice. Anaesth. Intensive Care 2021; 49: 62–9. [DOI] [PubMed] [Google Scholar]
- 7. Nafiu OO, Bradin S, Tremper KK. Knowledge, attitude, and practice regarding cricoid pressure of ED personnel at a large US teaching hospital. J. Emerg. Nurs. 2009; 35: 11–5. [DOI] [PubMed] [Google Scholar]
- 8. Smith KJ, Dobranowski J, Yip G, Dauphin A, Choi PT. Cricoid pressure displaces the esophagus: An observational study using magnetic resonance imaging. Anesthesiology 2003; 99: 60–4. [DOI] [PubMed] [Google Scholar]
- 9. Rice MJ, Mancuso AA, Gibbs C, Morey TE, Gravenstein N, Deitte LA. Cricoid pressure results in compression of the postcricoid hypopharynx: The esophageal position is irrelevant. Anesth. Analg. 2009; 109: 1546–52. [DOI] [PubMed] [Google Scholar]
- 10. Zeidan AM, Salem MR, Mazoit J‐X, Abdullah MA, Ghattas T, Crystal GJ. The effectiveness of cricoid pressure for occluding the esophageal entrance in anesthetized and paralyzed patients: An experimental and observational glidescope study. Anesth. Analg. 2014; 118: 580–6. [DOI] [PubMed] [Google Scholar]
- 11. Garrard A, Campbell A, Turley A, Hall JE. The effect of mechanically‐induced cricoid force on lower oesophageal sphincter pressure in anaesthetised patients. Anaesthesia 2004; 59: 435–9. [DOI] [PubMed] [Google Scholar]
- 12. Son YG, Shin J, Ryu HG. Pneumonitis and pneumonia after aspiration. J. Dent. Anesth. Pain Med. 2017; 17: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults: A prospective investigation of 297 tracheal intubations. Anesthesiology 1995; 82: 367–76. [DOI] [PubMed] [Google Scholar]
- 14. Hung K‐C, Hung C‐T, Poon Y‐Y et al. The effect of cricoid pressure on tracheal intubation in adult patients: A systematic review and meta‐analysis. Can. J. Anesth. 2021; 68: 137–47. [DOI] [PubMed] [Google Scholar]
- 15. White L, Thang C, Hodsdon A, Melhuish T, Vlok R. Cricoid pressure during intubation: A systematic review and meta‐analysis of randomised controlled trials. Heart Lung 2020; 49: 175–80. [DOI] [PubMed] [Google Scholar]
- 16. Birenbaum A, Hajage D, Roche S et al. Effect of cricoid pressure compared with a sham procedure in the rapid sequence induction of anesthesia: The IRIS randomized clinical trial. JAMA Surg. 2019; 154: 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mort TC. Emergency tracheal intubation: Complications associated with repeated laryngoscopic attempts. Anesth. Analg. 2004; 99: 607–13. [DOI] [PubMed] [Google Scholar]
- 18. Algie CM, Mahar RK, Tan HB, Wilson G, Mahar PD, Wasiak J. Effectiveness and risks of cricoid pressure during rapid sequence induction for endotracheal intubation. Cochrane Database Syst. Rev. 2015; 11: CD011656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bernhard M, Becker TK, Gries A, Knapp J, Wenzel V. The first shot is often the best shot: First‐pass intubation success in emergency airway management. Anesth. Analg. 2015; 121: 1389–93. [DOI] [PubMed] [Google Scholar]
- 20. Bair AE, Filbin MR, Kulkarni RG, Walls RM. The failed intubation attempt in the emergency department: Analysis of prevalence, rescue techniques, and personnel. J. Emerg. Med. 2002; 23: 131–40. [DOI] [PubMed] [Google Scholar]
- 21. Graham C, Beard D, Oglesby A et al. Rapid sequence intubation in Scottish urban emergency departments. Emerg. Med. J. 2003; 20: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: A closed claims analysis. Anesthesiology 2005; 103: 33–9. [DOI] [PubMed] [Google Scholar]
- 23. Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department: A one‐year study of 610 tracheal intubations. Ann. Emerg. Med. 1998; 31: 325–32. [DOI] [PubMed] [Google Scholar]
- 24. Hong QN, Fàbregues S, Bartlett G et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inform. 2018; 34: 285–91. [Google Scholar]
- 25. Higgins JP, Altman DG, Gøtzsche PC et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009; 62: e1–34. [DOI] [PubMed] [Google Scholar]
- 27. Ghedina N, Alkhouri H, Badge H, Fogg T, McCarthy S. Paediatric intubation in Australasian emergency departments: Ass report from the ANZEDAR. Emerg. Med. Australas. 2020; 32: 401–8. [DOI] [PubMed] [Google Scholar]
- 28. Trethewy CE, Doherty SR, Burrows JM, Clausen D. Ideal cricoid pressure is biomechanically impossible during laryngoscopy. Acad. Emerg. Med. 2018; 25: 94–8. [DOI] [PubMed] [Google Scholar]
- 29. Kojima T, Owen E, Shenoi A et al. 1020: clinical impact of cricoid pressure in the ICU/ED: A retrospective multicenter observational study. Crit. Care Med. 2016; 44: 331. [Google Scholar]
- 30. Clark RK, Trethewy CE. Assessment of cricoid pressure application by emergency department staff. Emerg. Med. Australas. 2005; 17: 376–81. [DOI] [PubMed] [Google Scholar]
- 31. Vanner R, Asai T. Safe use of cricoid pressure. Anaesthesia 1999; 54: 1–3. [DOI] [PubMed] [Google Scholar]
- 32. Vanner R, Pryle B. Regurgitation and oesophageal rupture with cricoid pressure: A cadaver study. Anaesthesia 1992; 47: 732–5. [DOI] [PubMed] [Google Scholar]
- 33. Meek T, Gittins N, Duggan J. Cricoid pressure: Knowledge and performance amongst anaesthetic assistants. Anaesthesia 1999; 54: 59–62. [DOI] [PubMed] [Google Scholar]
- 34. Morris J, Cook T. Rapid sequence induction: A national survey of practice. Anaesthesia 2001; 56: 1090–115. [DOI] [PubMed] [Google Scholar]
- 35. Quigley P, Jeffrey P. Cricoid pressure: Assessment of performance and effect of training in emergency department staff. Emerg. Med. Australas. 2007; 19: 218–22. [DOI] [PubMed] [Google Scholar]
- 36. Hodgson RE, Gopalan PD, Burrows RC, Zuma K. Effect of cricoid pressure on the success of endotracheal intubation with a lightwand. Anesthesiology 2001; 94: 259–62. [DOI] [PubMed] [Google Scholar]
- 37. Cook T, Woodall N, Frerk C, FNA P. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Br. J. Anaesth. 2011; 106: 617–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable ‐ no new data generated.


