INTRODUCTION
Hospitalist productivity and compensation are complex topics. Hospitalist clinical work is rapidly evolving with increasingly complex patients and hospital systems, all paired with unpredictable and often high workloads. Hospitalist clinical roles have evolved, sometimes incorporating high‐value but low productivity duties (e.g., triagist) in addition to the ever‐expanding clinical reach. Hospitalist financing has also evolved with increasing direct costs to hospitals, which may incentivize hospitals to consider funding high productivity hospitalist models to help offset the costs. However, there are likely inadvertent costs to these models that can lead to deterioration in clinician wellness, patient quality and safety, and ultimately, institutional goals.
Hospitalists are charged to care for some of the healthcare industry's most complex patients as well as to lead complex institutional efforts. During the pandemic, the role of hospitalists was elevated even further as hospitalists were quickly asked to adapt to the shifting needs of health systems and lead large‐scale operational surge efforts. As hospitalists have faced unprecedented work conditions and unpredictable work demands, research is emerging that stress, anxiety, overwork, and burnout are high. 1 , 2 The stressors faced by hospitalists, further magnified during the pandemic, unfortunately, are not new. 3
As hospitalists increase their footprint in the healthcare ecosystem and have experienced unprecedented growth (with at least 75% of US hospitals utilizing hospitalists and over 50,000 practicing hospitalists 4 ), it is tempting to focus attention on the direct costs of hospitalist care models. The literature, however, suggests that this attention may be misdirected and that there exists a trade‐off where the request to “see more patients” actually increases waste and decreases quality. Hospitalists often have an intuitive sense of this via their immersion in the hospital environment, but the rigorous study of these unintended outcomes is essential. Reimagining hospitalist clinical work and goals can help optimize care models to support thriving teams, patients, and institutions and simultaneously reduce overall costs of care. We explore three ideas: (1) the current drive for productivity may be harming the workforce, patients, and institutional outcomes; (2) we must address both the measured outcomes and implicit, system‐level assumptions to better focus on determining the ideal workload, and (3) we must develop and evolve clinical staffing strategies that are evidence‐based to optimize outcomes. Recognizing that hospitalists add value to a wide array of high‐value health system efforts and scholarly pursuits, this article will focus on clinical care models.
THE TRADE‐OFFS OF PRODUCTIVITY
Hospitalist staffing models are often financially driven as most hospitalist groups across the country rely on subsidies from hospitals to support hospitalist salaries as provider fee billing does not adequately cover costs. A reflexive approach for hospitals to improve costs and efficiency may be to “squeeze more juice out of the lemon” (i.e., encourage hospitalists to see more patients more quickly). Preliminary studies suggest, however, that increasing clinical workloads negatively impact hospitalist well‐being, mental health, and hospitalist job performance, 2 , 3 , 5 while simultaneously negatively impacting hospital operational and financial outcomes. 5 , 6
Commonly cited factors for burnout in hospital medicine pertain to clinical workloads, including high patient‐to‐clinician ratios and unrealistic workloads. 2 Physician burnout has been linked to the quality of care 7 , 8 and the financial bottom line. 8 Research has shown that physicians who experience burnout are at increased risk of leaving their current position, 7 while those who do not leave may reduce their time spent taking care of patients. 9 Increasing workloads affect hospitalist job performance, such as perceived quality of care and operational outcomes (e.g., length of stay). Studies have shown that 40% of physicians stated that their typical patient load in the inpatient setting exceeded safe levels at least monthly 10 and that resources often lag behind the ever‐increasing workloads. 3 Another study by Elliott et al. 5 highlighted that when physicians saw more than 15 patients in a shift, patient length of stay increased exponentially and costs increased (i.e., hospital charges). More recently, Kamalahmadi et al. 6 highlighted that it may be beneficial for major academic medical centers (AMCs) to focus on throughput (and thus lowering hospitalist census) given AMCs typically run at high capacity as these efforts may improve hospital‐wide flow by lowering the length of stay. Similar findings were seen for community hospitals but with different rationale given different patient populations. 6 Additionally, work has suggested that quality improvement efforts may degenerate with high workloads. Kara et al. 11 reported that clinicians felt that an effort to geographically cohort patients negatively impacted patient safety, collaboration, morale, camaraderie, and efficiency with higher patient loads. This all suggests that our current measures of efficiency leave out crucial factors that have significant financial implications and that more holistic measures could simultaneously save systems money while also protecting hospitalists.
ALIGNING CLINICIAN‐, PATIENT‐, AND INSTITUTIONAL‐CENTRIC MEASURES
Integrating the job demands‐resources model of burnout 12 and the conceptual model for integrated approaches to the protection and promotion of worker health and safety, 13 we propose a framework to use as a guiding principle for future studies on hospitalist work—taking into account workforce, patient, and institutional goals (Figure 1). We begin by connecting the concepts of hospitalist workload to hospitalist outcomes and job performance—as job demands and resources affect hospitalist well‐being, 2 , 3 perceptions of their work environment, and their ability to do their job (e.g., efficiency and throughput and high‐quality patient care). Importantly, research has also shown a dose–response relationship between task load and burnout. 14 In our model, we further highlight that job demands and resources also drive patient care outcomes and operational and financial outcomes to the institution. By establishing this model as our “true north,” the foundational component for our work becomes understanding and developing best work practices, targets, and models of care.
Figure 1.
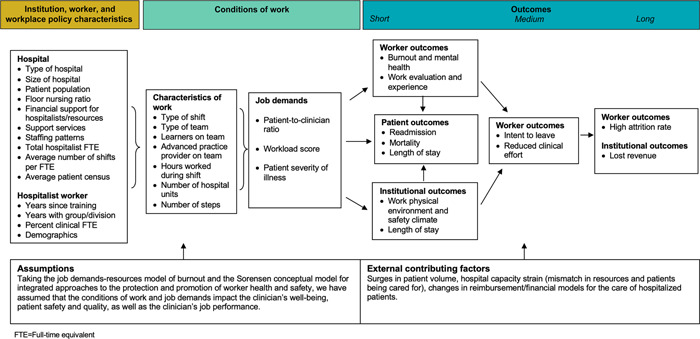
Conceptual model for hospitalist clinical work.
Current measures of workload and productivity are insufficient. As a starting place, we propose balancing measures that could signal when the drive toward ever‐greater productivity becomes counterproductive. Building off previous work that examined factors that affect hospitalist work, 15 we propose more holistic measures that capture institutional motivations and leverage the electronic health record (EHR), 16 as well as the more sensitive measures of the human aspects of care to articulate the multifaceted value that hospitalist providers bring to both patients and to the health systems that they serve (Table 1).
Table 1.
Potential measures for hospitalist clinical work
| Measure | Pros | Cons | Current or future use examples | |
|---|---|---|---|---|
| Productivity measures | wRVU/cFTE | Simple and data typically available. | May not appropriately account for true effort (i.e., effects of moonlighting, how cFTE is defined, how leave is accounted for, non‐RVU generating work). Need to account for the impact of staffing models (e.g., APP, learners). | Typical measurements for productivity and for benchmarking. |
| Encounters/cFTE | ||||
| Financial measures | Hospital support/cFTE | Simple and data typically available. | May not appropriately account for true effort (i.e., moonlighting will impact how cFTE is defined, how is leave accounted for, non‐RVU generating work). May not capture the true value of hospitalists. | Typical measures for understanding cost/hospital offset. |
| Collections/cFTE | ||||
| Workload | wRVU/cFTE | Measure quantity of work and in some cases complexity of work. | While some measures are readily available, task load would require surveying or developing some measures from EHR. Need to account for staffing models (APP, learners). Need to account for patient complexity and type of work. Other modifiers may need to be accounted for such as geography and patient population/required tasks and non‐RVU generating work. | Task load is often used in high‐risk industries (NASA), but is not utilized in daily operations in medicine. Could be utilized to periodically gauge the perception of workload in conjunction with more typical measures of workload. Patient complexity should be considered when determining the appropriate workload. No standards currently exist. |
| Encounters/cFTE | ||||
| Task load | ||||
| Patient complexity (case mix index, Charlson comorbidity) | ||||
| EHR measures (total EHR time, work outside of work, time on documentation, inbox time, distractions) | Accessible from the EHR; the potential for real‐time measures. | Hospitalists work variable hours (defining after‐hour work may be challenging). May not be efficient to extract large volumes of data. Does not capture all work. | There may be institutional reports on clinician‐specific work in the EHR. These measures could be incorporated into decision support tools. | |
| Hospitalist well‐being | Burnout/well‐being inventories | A measure of how work is affecting the hospitalist. | Requires surveying. Factors beyond work may affect individual scores. | These may be utilized in annual institutional surveys, but are not typically paired with typical measures of workload (or other measures of workload as outlined above). |
| Hospitalist outcomes (intent to stay, attrition rate, reduced clinical effort) | Measures that assess hospitalist thriving. | Requires surveying and tracking attrition rates and clinical effort changes (and understanding reasons for doing so). | ||
| Patient safety culture | Team culture and safety surveys | Gives an understanding of how work environment and staffing models support patient care and communication. | Requires surveying. | May be administered annually and paired with global questions about workload, but typically not paired with discrete measures of workload (e.g., what quantity of work leads to poor outcomes on the surveys). |
| Job performance | Patient outcomes (LOS, mortality, readmissions, ICU transfers) | Simple and data typically available. | Many factors may influence these outcomes. | Readily available in EHR; could be paired with workloads to understand how workload impacts these outcomes. When paired with workload, begins to link work models to clinician/institutional performance. |
| Communication (HCAHPS) | Simple and data typically available. | Many factors may influence these outcomes. | ||
| Institutional outcomes | Patient and safety outcomes as outlined above, LOS and throughput | Simple and data typically available. | Many factors may influence these outcomes. | Must assess the trade‐offs between direct costs and outcomes. When paired with workload, begins to link work models to institutional performance. |
| Financial outcomes | Must be financially viable and also must look beyond direct costs. | Assessing direct costs only may miss indirect costs/benefits. |
Abbreviations: APP, advanced practice provider; cFTE, clinical fraction full‐time equivalent; EHR, electronic health record; HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems; ICU, intensive care unit; LOS, length of stay; NASA, National Aeronautics and Space Administration; wRVU, work relative value unit.
In high‐risk industries, both within and outside of medicine, attention and cognitive load are increasingly areas of focus as research shows fractured attention leads to increased processing time on complex tasks, impaired working memory, and bias. 17 A better understanding of these clinician‐centric measures and how they intersect with staffing models, patient outcomes, and institutional goals would help us design work environments and staffing models that are more humane while assessing the value to which our current measures of productivity are insensitive. Importantly, tracking these measures in real‐time and eventually integrating predictive analytics will be key to understanding how changing workloads may impact vital outcomes and could offer the opportunity to proactively course‐correct as models evolve.
DEVELOP STAFFING STRATEGIES THAT ARE DATA‐ AND EVIDENCE‐BASED
Integrated information systems must be coupled with workflows and business process management, which would allow for an iterative improvement process informed by data 18 and aligned with hospital priorities. 19 These data may come from the EHR and from real‐time assessments of clinician workload, task load, and biosensor technology to understand the true impact of work on the workforce and how staffing models affect a hospitalist's ability to do their job. Easy‐to‐use workforce assessments must be implemented in addition to or in place of the once‐a‐year wellness surveys and paired with operational decision support tools. We must also understand operational inefficiencies and recognize that staffing models and needs will evolve over time and these information systems and decision tools must evolve with them.
Ensuring the return‐on‐investment will be a central focus for any hospital. Kamalahmadi et al. 6 showed that reducing hospitalists' census could lead to ~$1.5 million in annual savings— solely by implementing optimal staffing strategies that include lowering hospitalist census (although models vary based upon whether the institution is academic or community and patient complexity). Presumably, in addition to cost savings, busy AMCs that run at capacity could then focus on bringing in more profit‐generating admissions such as surgeries. Lastly, the cost of burnout and attrition is high. While on face value, some may believe that turnover is cost‐effective (e.g., more junior hospitalists may have lower salaries), the literature would suggest that much of that savings may be negated by additional recruitment costs, costs from burnout‐driven full‐time equivalent reduction, and worse outcomes including increased mortality 20 from an inexperienced workforce.
LOOKING FORWARD
We must realign the outcomes to which hospitalists and healthcare systems subscribe. As a starting point, all measures of workload should have balancing measures. Understanding what constitutes total work and developing robust mechanisms to seamlessly measure this global measure must be undertaken. The field of hospital medicine has an incredible opportunity before it. With nearly unlimited access to data, agile staffing models, and diverse models of care implemented across the United States, hospitalists can again serve as the forerunners of American healthcare reform. As part of these efforts, we have a responsibility to develop measurements of total work, understand the effects on clinicians, patients, and institutional outcomes, and begin to aim toward thriving.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Burden M, Patel M, Kissler M, Harry E, Keniston A. Measuring and driving hospitalist value: Expanding beyond wRVUs. J Hosp Med. 2022;17:760‐764. 10.1002/jhm.12849
Marisha Burden and Moksha Patel are co‐first authors.
REFERENCES
- 1. Dugani SB, Geyer HL, Maniaci MJ, Fischer KM, Croghan IT, Burton C. Psychological wellness of internal medicine hospitalists during the COVID‐19 pandemic. Hosp Pract. 2021;49(1):47‐55. [DOI] [PubMed] [Google Scholar]
- 2. Glisch C, Yadav S, Bhandari S, Jha P. Perceptions of burnout among academic hospitalists. WMJ. 2021;120(4):268‐272. [PubMed] [Google Scholar]
- 3. Arogyaswamy S, Vukovic N, Keniston A, et al. The impact of hospital capacity strain: a qualitative analysis of experience and solutions at 13 academic medical centers. J Gen Intern Med. 2021;37:1463‐1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wachter RM, Goldman L. Zero to 50,000—the 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009‐1011. [DOI] [PubMed] [Google Scholar]
- 5. Elliott DJ, Young RS, Brice J, Aguiar R, Kolm P. Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786‐793. [DOI] [PubMed] [Google Scholar]
- 6. Kamalahmadi M, Bretthauer K, Helm J, et al. Mixing it up: Operational impact of hospitalist caseload and case‐mix. Accessed May 30, 2021. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3456882.
- 7. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. [DOI] [PubMed] [Google Scholar]
- 8. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well‐being. JAMA Intern Med. 2017;177(12):1826‐1832. [DOI] [PubMed] [Google Scholar]
- 9. Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91(4):422‐431. [DOI] [PubMed] [Google Scholar]
- 10. Michtalik HJ, Yeh HC, Pronovost PJ, Brotman DJ. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375‐377. [DOI] [PubMed] [Google Scholar]
- 11. Kara A, Johnson CS, Hui SL, Kashiwagi D. Hospital‐based clinicians' perceptions of geographic cohorting: identifying opportunities for improvement. Am J Med Qual. 2018;33(3):303‐312. [DOI] [PubMed] [Google Scholar]
- 12. Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands‐resources model of burnout. J Appl Psychol. 2001;86(3):499‐512. [PubMed] [Google Scholar]
- 13. Sorensen G, McLellan DL, Sabbath EL, et al. Integrating worksite health protection and health promotion: a conceptual model for intervention and research. Prev Med. 2016;91:188‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harry E, Sinsky C, Dyrbye LN, et al. Physician task load and the risk of burnout among US physicians in a national survey. Jt Comm J Qual Patient Saf. 2021;47(2):76‐85. [DOI] [PubMed] [Google Scholar]
- 15. Michtalik HJ, Pronovost PJ, Marsteller JA, Spetz J, Brotman DJ. Developing a model for attending physician workload and outcomes. JAMA Intern Med. 2013;173(11):1026‐1028. [DOI] [PubMed] [Google Scholar]
- 16. Sinsky CA, Rule A, Cohen G, et al. Metrics for assessing physician activity using electronic health record log data. J Am Med Inform Assoc. 2020;27(4):639‐643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kissler MJ, Kissler K, Burden M. Toward a medical "Ecology of Attention". N Engl J Med. 2021;384(4):299‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ryan J, Doster B, Daily S, Lewis C, Ryan R. Perioperative workflow and patient care documentation perpetuated through electronic medical records via integrated hospital information systems. 2015. Accessed March 19, 2022. AMCIS 2015 Proceedings. 27. https://aisel.aisnet.org/amcis2015/HealthIS/GeneralPresentations/27 [Google Scholar]
- 19. White AA, McIlraith T, Chivu AM, et al. Collaboration, not calculation: a qualitative study of how hospital executives value hospital medicine groups. J Hosp Med. 2019;14(11):662‐667. [DOI] [PubMed] [Google Scholar]
- 20. Goodwin JS, Salameh H, Zhou J, Singh S, Kuo YF, Nattinger AB. Association of hospitalist years of experience with mortality in the hospitalized medicare population. JAMA Intern Med. 2018;178(2):196‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]


