Abstract
Background
A large number of research reports on vital pulp treatment (VPT) has been published over the last two decades. However, heterogeneity in reporting outcomes of VPT is a significant challenge for evidence synthesis and clinical decision‐making.
Objectives
To identify outcomes assessed in VPT studies and to evaluate how and when outcomes are measured. A subsidiary aim was to assess evidence for selective reporting bias in the included studies. The results of this review will be used to inform the development of a core outcome set (COS) for endodontic treatments.
Methods
Multiple healthcare bibliographic databases, including PubMed/MEDLINE, Ovid EMBASE, Scopus, Cochrane Database of Systematic Reviews and Web of Science were searched for systematic reviews published between 1990 and 2020, reporting on VPT. Screening, data extraction and risk of bias assessment were completed independently by two reviewers. Outcomes' information was extracted and aligned with a healthcare taxonomy into five core areas: survival, clinical/physiological changes, life impact, resource use and adverse events.
Results
Thirty‐six systematic reviews were included, 10 reporting on indirect pulp capping or selective caries removal, nine on direct pulp capping, eight on pulpotomy and nine on combined VPTs. There was considerable variation in the outcomes reported in these reviews and their included studies. Clinician‐reported outcomes were used considerably more often than patient‐reported outcomes. A range of instruments and time points were used for measuring outcomes. Several of the reviews were assessed as having low risk of selective reporting bias, but many did not specifically report this domain, whilst others did not provide risk of bias assessment at all.
Discussion
Considerable variation in selection of outcomes and how and when they are measured and reported was evident, and this heterogeneity has implications for evidence synthesis and clinical decision‐making.
Conclusions
Whilst there is a lack of consistency, several potentially important outcomes for VPT, including pulp survival, incidence of post‐operative pain and need for further intervention, have been identified which could inform the development of a COS for endodontic treatment.
Registration
Core Outcome Measures in Effectiveness Trials (COMET) (No. 1879).
Keywords: direct pulp capping, endodontics, outcomes, pulpotomy, selective caries removal, vital pulp treatment
INTRODUCTION
Vital pulp treatments (VPTs) represent a group of minimally invasive endodontic treatments intended to preserve the health of all or part of the dental pulp (Duncan, Galler, et al., 2019). These treatments include a spectrum of modalities including indirect pulp capping, direct pulp capping and pulpotomy (partial or complete). Although not novel, VPT has recently emerged as a promising biologically based treatment due, in part, to advances made in the scientific field, including the introduction of bioactive hydraulic calcium silicate cements (Nair et al., 2008; Parirokh et al., 2018) as well as advances in pulp biology that have improved clinicians' understanding of the biological and reparative processes occurring in the injured dental pulp (Duncan, Cooper, & Smith, 2019; El Karim, Cooper, et al., 2021). Consequently, a plethora of clinical studies reporting on the outcome of VPT have been published over the last two decades and have demonstrated high success rates (Asgary et al., 2017; Bjørndal et al., 2017; Taha & Abdulkhader, 2018). Many systematic reviews have also been conducted summarizing the evidence from these studies (Cushley et al., 2019, 2020; Elmsmari et al., 2019). However, these systematic reviews are limited not only by methodological shortcomings, but also by the considerable heterogeneity and lack of standardization in the reporting of outcomes within the included studies.
A treatment outcome is generally defined as a clinical measure used to judge the efficacy or effectiveness of a treatment, but it can also represent the suffering or loss of health experienced by an individual because of the disease process (Boers et al., 2014). With this background, the outcomes of all endodontic treatment, including VPT, are often evaluated through detailed history‐taking accompanied by clinical and radiographic examination. The reporting of these clinical findings, however, is heterogenous with no clear consensus amongst researchers and clinicians on the most important and relevant outcomes to be reported for each respective treatment. For instance, tooth survival is an important outcome for patients, but is generally not reported, and even when reported, different terminologies and descriptions are used. This makes evidence synthesis and meta‐analysis unnecessarily difficult, if not impossible (Saldanha et al., 2020). In addition, many of the reported outcomes tend to be clinician‐reported and not patient‐reported (Duncan, Chong, et al., 2021). There is also a lack of consensus on the methods and timing used to measure outcomes. Such heterogeneity negatively impacts evidence synthesis, pooling of primary studies, clinical guidelines development and provision of clinical care (Rosenbaum et al., 2010). Therefore, a need exists to develop a minimum core outcome set (COS) for VPT, which would be used in all future studies of these treatments.
A COS is defined as an agreed, standardized set of outcomes that should be measured and reported as a minimum in all clinical trials and clinical outcome studies in a particular field (Williamson et al., 2012). It is not intended to be a restrictive list but rather it allows researchers to also include additional outcomes that support their study aims whilst ensuring better clarity of available evidence. Adopting a COS approach in clinical research increases the likelihood that important outcomes are measured, improves evidence synthesis by reducing heterogeneity between studies and reduces outcome‐reporting bias, thereby, improving the validity of the studies (Clarke, 2008). The process of COS development as described in the Core Outcome Set‐STAnDards for Development (COS‐STAD) statement, involves identification of outcomes and how they are measured through systematic review of the literature, followed by a structured consensus process to agree the most important outcomes and how and when they should be measured (Kirkham et al., 2016; Kirkham et al., 2017).
This scoping review reports on the outcomes of existing VPT studies and serves to inform the development of a COS outcome set for endodontic treatment modalities (COSET) project (El Karim, Duncan, et al., 2021) The objectives of this scoping review are to: (1) Identify what outcome domains are assessed in studies evaluating VPT, (2) Report on how the outcomes are measured (that is, what validated or nonvalidated instruments are used) and (3) Assess any selective reporting bias in the included studies.
METHODS
This scoping review is reported in line with the PRISMA‐ScR guidance (Tricco et al., 2018). The protocol for this review and the COSET project has previously been published (El Karim, Duncan, et al., 2021). The project is registered in the Core Outcome Measures in Effectiveness Trials (COMET) database (registration No. 1879).
Selection criteria
Population: Humans undergoing VPT in a permanent tooth.
Treatment procedures carried out: direct pulp capping (DPC); indirect pulp capping (INDPC)/ selective caries removal (one and two visits); partial pulpotomy and full/complete coronal pulpotomy.
Follow up: No restriction on follow up period.
Studies: Systematic reviews published in the English language which included clinical studies reporting clinical and or radiographic outcomes of VPT.
Information sources
A comprehensive structured literature search was performed using PubMed/MEDLINE, Ovid EMBASE, Scopus, Cochrane Database of Systematic Reviews, Web of Science databases and grey literature to identify systematic reviews published in English between January 1990 and December 2020 covering the outcomes of VPT.
Search process
A detailed search strategy was developed in MEDLINE and adapted for other bibliographic databases (Table S1). An electronic library of all references was uploaded to EndNote 20 and duplicates were removed. Two reviewers (SC, IEK) independently assessed the title and abstracts of all systematic reviews identified. Any disagreement about article inclusion was resolved by arbitration from a third reviewer (HD) if required.
Outcome measures
The main outcomes of this scoping review were: (1) Identification and list all outcomes reported in the studies included in the reviews (clinician‐ and patient‐reported outcomes), (2) Methods used to measure these outcomes, and (3) Duration of follow up of the reported outcomes.
Data extraction
Data extraction from the full text of eligible reviews was completed independently by one reviewer (SC) and verified by another (IEK). A data extraction proforma was piloted based on the outcomes reported in three of the included studies. Extracted data included all clinician and patient‐reported outcomes in eligible studies. Histological and microbiological outcomes were also extracted if they were provided in conjunction with a clinical or radiographic outcome. Data were also collected on the range of instruments (radiographs, questionnaires, pulp testers, etc.) used for outcome measurement and the duration of the follow up. Instruments included pain measurement scales, unspecified pain questionnaires, radiography, cone‐beam computer tomography, histopathological as well as clinical and photographic assessments. In addition, demographic and other data to facilitate description of the included studies was collected including, country of study and the method of data synthesis.
Categorization into domains
Outcomes data collected was aligned with a healthcare taxonomy (Dodd et al., 2018). The taxonomy involves grouping outcomes into five core areas: survival, clinical/physiological changes, life impact, resource use and adverse events. Each core area has both disease and treatment‐specific domains for outcomes. The outcomes in each domain were collated and presented in table forms.
RESULTS
Literature search
The initial search of the data bases using the search strategy shown in Table S1 yielded 433 articles. After removal of duplicates, 367 abstracts and titles were available for screening, of which 320 were excluded for reasons summarized in Figure 1. The remaining 47 full text articles were then assessed for eligibility, and 11 that did not meet the review criteria were excluded (Table S2). Finally, 36 systematic reviews were included in this scoping review.
FIGURE 1.
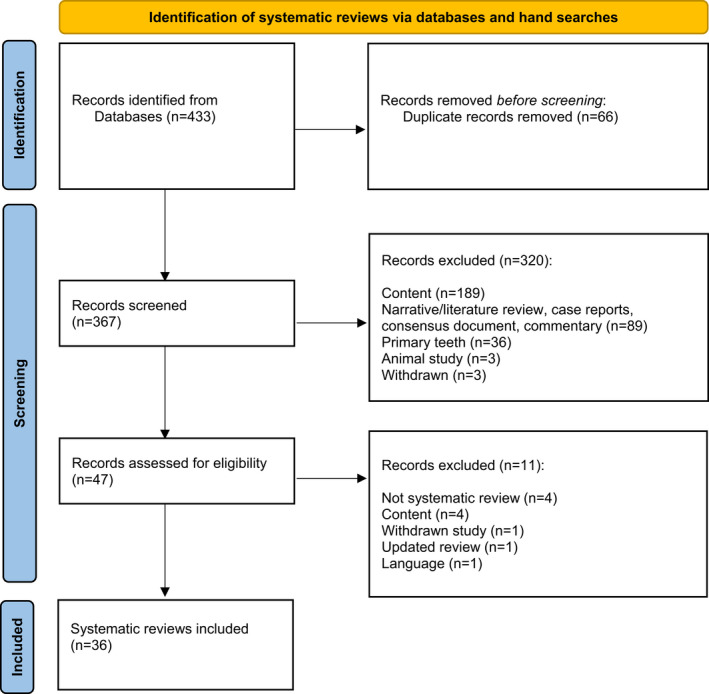
PRISMA flow diagram.
Characteristics of included studies
The characteristics of the included systematic reviews are shown in Table 1. Of these, 10 reported on INDPC/selective or stepwise caries removal (Table 1A), nine on DPC (Table 1B), eight on pulpotomy (Table 1C) and nine on a combination of VPTs (Table 1D). There was a wide geographical distribution of authors across Asia, Europe, North and South America. The number of studies included in each review varied (range: 2 to 37). The type of included studies within the reviews also varied and included randomized controlled trials (RCT) (n = 85), controlled clinical trial (CCT) (where it was not explicit that the trial was randomized) (n = 14), cohort studies (n = 47) and case series (n = 15) out of a total of 161 studies. A list of these studies and an additional 10 studies identified from the reference lists of the included systematic reviews are available in Tables S3 and S4. A meta‐analysis was conducted in 22 of the systematic reviews included in this scoping review (Table S4).
TABLE 1.
Characteristics of systematic reviews on (A) indirect pulp capping /selective caries removal (n = 10); (B) direct pulp capping (DPC) (n = 9); (C) pulptomy (n = 8); (D) combining different VPTs (n = 9)
| Author | Year | Country | Journal name | VPT modality reported | Outcomes reported in review | Number and type of eligible studies | Meta‐analysis | Follow up | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | RCT | CCT | CS | Case series | ||||||||
| (A) | ||||||||||||
| Barros et al., 2020 | 2020 | Brazil | Clinical Oral Investigations | INDPC | Maintenance of pulp health (clinically and radiographically) pulp exposure, dentin deposition, microbiological examination, quality of the restoration | 10 | 9 | 1 | Yes | 3 months–5 years | ||
| da Rosa et al., 2019 | 2019 | Brazil | International Endodontic Journal | INDPC | Dentine hardening and thickness | 2 | 2 | — | — | — | Yes b | 3–71 months |
| Hayashi et al., 2011 | 2011 | Japan | Journal of Dentistry | INDPC | Pulp exposure, postoperative pain or discomfort, amounts of cariogenic bacteria in a cavity, colour and hardness of carious dentin, remineralization of softened dentin, regeneration of tertiary dentin, and retention of sealing material, vitality | 7 | 1 | 1 | — | 5 | No | 4 months–11 years a |
| Hoefler et al., 2016 | 2016 | USA | Journal of Dentistry | INDPC | Restorative failures and loss of pulp vitality | 5 | 2 | — | — | 3 | No | 2–10 years |
| Kiranmayi et al., 2019 | 2019 | India | Journal of International Oral Health | INDPC | Success or failure of pulp capping≠ | 6 | 6 | — | — | — | Yes | 2–24 months |
| Li et al., 2018 | 2018 | China | Acta Odontologica Scandinavica | INDPC | Risk of pulp exposure, risk of pulpal symptoms. (clinical or radiological pulp symptoms such as pain, irreversible pulpitis and loss of vitality), and failure (technical or biological complications demanding intervention | 2 | 2 | — | — | — | Yes | 6–24 months |
| Ricketts et al., 2013 | 2013 | United Kingdom | Cochrane Systematic Reviews | INDPC | Pulpal exposure, signs and symptoms pulpal disease, progression caries, restoration failure, health economics, OHQoL, patient/carer and dentist perception of treatment, patient discomfort during treatment | 4 | 4 | — | — | — | Yes | 3 months–11 years a |
| Ricketts et al., 2007 | 2007 | United Kingdom | Cochrane Systematic reviews | INDPC | Exposure of the pulp during caries removal. Patient experience of symptoms of pulpal inflammation or necrosis. Progression of caries under the filling. Time until the filling is lost or replaced | 2 | 2 | — | — | — | Yes | 12 months–11 years a |
| Schwendicke, Dorfer, & Paris, 2013 | 2013 | Germany | Journal of Dental Research | INDPC | Pulpal exposure during treatment; postoperative pulpal symptoms (clinical or radiological pulp symptoms requiring treatment and failure (technical or biological complications demanding intervention) | 4 | 4 | — | — | — | Yes | 6 months–10 years |
| Schwendicke, Meyer‐Lueckel, et al., 2013 | 2013 | Germany | Journal of Dentistry | INDPC | Clinical or radiological failure. Events or conditions associated with previous treatment of deep caries, which require re‐treatment. Pulpal failures included pain, clinical or radiological signs of loss of vitality, or abscess or sinus formation leading to re‐treatment. Nonpulpal failures included fracture of the tooth or the restoration, loss of the restoration or its integrity, or secondary as well as progressing residual caries leading to re‐treatment | 14 | 7 | 1 | 6 | Yes | 6 months–10 years | |
| (B) | ||||||||||||
| Cushley et al., 2020 | 2020 | United Kingdom | International Endodontic Journal | DPC | Clinical and radiographic success of DPC | 14 | 5 | — | 9 | — | Y | 6–120 months |
| Deng et al., 2016 | 2016 | China | Journal of American Dental Association | DPC | Success or failure treatment | 5 | 5 | — | — | — | Y | 6 months–4 years |
| Edwards et al., 2020 | 2020 | United Kingdom | Endodontic Practice Today | DPC | Tooth survival, pulp survival, clinical success, cost effectiveness | 4 | 4 | — | — | N | 7 days–36 months | |
| Javed et al., 2017 | 2017 | United States of America | Lasers in Medical Science | DPC | Pulp vitality and healing response to laser therapy | 6 | 5 | — | —1 | — | Y | 0.5–54 months |
| Li et al., 2015 | 2015 | China | Journal of Endodontics | DPC | Success rate, inflammatory response, and dentin bridge formation | 9 | 4 | 2 | 3 | — | Y | 1 day–123 months a |
| Mahmoud et al., 2018 | 2018 | Egypt | Journal of Conservative Dentistry | DPC | Clinical symptoms and/or radiographic evidence | 6 | — | — | 6 | — | N | 8–540 days |
| Matsuura et al., 2019 | 2019 | Japan | Journal of Oral Science | DPC | Clinical and radiographic success | 7 | 7 | — | — | — | N | 6–36 months |
| Schwendicke et al., 2016 | 2016 | Germany | Clinical Oral Investigations | DPC | Clinical and radiographic success (no pain or signs of irreversible pulpitis or lost vitality, no abscess/sinus, no radiographic pathologies).Costs/time required for capping and subjective handling of different capping materials | 5 | 4 | 1 | — | — | Y | 3–24 months |
| Zhu et al., 2015 | 2015 | China | International Journal of Clinical Medicine | DPC | Clinical success and dentine bridge formation radiographically | 3 | 3 | — | — | — | Y | 1 week–2 years a |
| (C) | ||||||||||||
| Alqaderi et al., 2016 | 2016 | United States of America | Journal of Dentistry | CP | Success rate c | 6 | 1 | — | 5 | — | Y | 1–88 months |
| Chen et al., 2019 | 2019 | China | BMC Oral Health | CP | Clinical and radiographic success d | 5 | 5 | — | — | — | Y | 6–24 months |
| Cushley et al., 2019 | 2019 | United Kingdom | Journal of Dentistry | CP | Long‐term success of pulpotomy e | 8 | 3 | — | 5 | — | N | 12–60 months |
| Elmsmari et al., 2019 | 2019 | United Arab Emirates | Journal of Endodontics | PP | Success rate | 9 | 5 | — | — | 4 | Y | 3–154 months |
| Li et al., 2019 | 2019 | China | Journal of Dentistry | CP | Clinical or radiographic success at 12 months f | 16 | 16 | — | — | — | Y | 1–60 months |
| Taylor et al., 2020 | 2020 | United Kingdom | International Journal of Paediatric Dentistry | CP & PP | Clinical success defined as the tooth being in situ at the end of the study. Assumption that for the tooth to remain in situ it was symptom free and showed no signs of new or progressive infection | 9 | 3 | — | 5 | 1 | N | 1 day–140 months |
| Zafar et al., 2020 | 2020 | Pakistan | Journal of Conservative Dentistry | CP | Lack of clinical and radiographic signs of failure. Healing or resolution of periapical rarefaction | 6 | 2 | — | 4 | — | N | 1–10 years |
| Zanini et al., 2019 | 2019 | France | Acta Odontologica Scandinavica | CP | Clinical and histological success | 32 | 10 | 1 | 20 | 1 | N | 1 day–96 months a |
| (D) | ||||||||||||
| Aguilar & Linsuwanont, 2011 | 2011 | Thailand | Journal of Endodontics |
DPC CP |
Clinical and radiographic success of treatment | 22 | 4 | — | 5 | 1 | Y | >6 months–>3 years |
| Bergenholtz et al., 2013 | 2013 | Sweden | Singapore Dental Journal | INDPC, DPC, CP | Survival of the pulp, verified by absence of symptoms, sensibility testing, radiographic examination or closure of the roots in young teeth | 10 | 8 | 1 | — | 1 | N | 1–3.6 years |
| Brodén et al., 2016 | 2016 | Sweden | American Journal of Dentistry | DPC, CP | Treatment outcome was based on radiographic examination and/or sensitivity testing for teeth treated by pulp capping procedures and radiographic examination and the presence/absence of clinical symptoms for the root filled teeth | 10 | 2 | — | — | 8 | N | 12–140 months |
| Didilescu et al., 2018 | 2018 | Romania | Journal of American Dental Association | DPC, PP | Hard tissue formation | 18 | 7 | 11 | — | — | Y | 5–136 days |
| Fransson et al., 2016 | 2016 | Sweden | International Endodontic Journal | DPC, CP | Formation hard tissue barrier | 15 | 10 | 5 | — | — | N | 1 day–6 months |
| Mahgoub et al., 2019 | 2019 | China | Journal of International Society of Preventive & Community Dentistry | DPC, CP | Dentine bridge formation, treatment success, mineralization, and the presence of inflammatory cells | 2 | 1 | — | 1 | — | N | 3 weeks–3 years |
| Miyashita et al., 2007 | 2007 | Japan | Cochrane systematic reviews | DPC, INDPC | Clinical success, extraction, patient satisfaction, adverse events | 4 | 3 | — | 1 | — | Y | 6 months–3 years |
| Munir et al., 2020 | 2020 | Switzerland | Journal of Clinical Medicine | DPC, CP | Pulp survival after intervention | 26 | 25 | 1 | — | — | N | 1 day–5 years a |
| Paula et al., 2018 | 2018 | Portugal | Journal of Evidence Based Dental Practice | DPC, CP | Preservation of pulp vitality (success rate, absence of inflammatory response, and dentinal bridge formation) | 37 | 25 | 4 | 8 | — | Y | 30–2400 days |
Note: (A) ≠Secondary outcomes included: (1) overall, clinical, or radiographic success at longer follow up periods; and (2) root growth or apical closure (for immature permanent teeth only). Clinical success was described as devoid of clinical manifestations such as pain on percussion/palpation and spontaneous pain, and devoid of need for further root canal treatment. Radiographic success was defined as healing or resolution of radiographic periapical lesions, and devoid of need for further root canal treatment. Overall success was defined as achievement of both clinical and radiographic success.
Abbreviations: CCT, Case control studies; CP, Complete pulpotomy; CS, Cohort studies; DPC, Direct Pulp Capping; INDPC, Indirect pulp capping; OHQoL, Oral health quality of life; PP, Partial Pulpotomy; RCT, Randomized control trials; VPT, Vital pulp treatment.
Data not stated in review and collated from included studies.
The eligible studies for this review were not included in the meta‐analysis.
Success was defined as no radiographic abnormality or clinical symptoms, such as spontaneous pain, tenderness to percussion or palpation, resolution (decrease in size or elimination) of an existing radiographic periapical lesion, and no need for further pulpectomy and RCT of the treated teeth.
Success was defined as no pain, no abscess or fistulation, no excessive tooth mobility and no swelling. Radiographic success was considered if the teeth showed no evidence of apical and furcal radiolucency, internal or external root resorption, periodontal ligament widening, or periapical bone destruction.
Success was defined as; (1) radiographic success in which there was no abnormality suggestive of apical periodontitis as well as resolution (decrease in size or elimination) of an existing radiographic periapical lesion, and (2) clinical success where there were no clinical symptoms of spontaneous pain, tenderness to percussion and/or no swelling or sinus tract. Long‐term success is also defined by minimum 12‐month follow up period.
Failures were considered when there were clinical symptoms such as pain, tenderness and radiolucency in the periapical region including the widening of periodontal ligament. All the six studies evaluated the thickness of tertiary dentin formed after INDPC by tooth sensibility tests, pain evaluation by visual analogue scale, percussion test, and radiographically assessed the presence or absence of periapical radiolucency and thickness of tertiary dentin after INDPC procedure.
Synthesis of results
Outcome domains for pulpotomy, DPC and INDPC were shown in Tables 2, 3, 4, respectively, and described in detail as follows.
TABLE 2.
Outcomes of INDPC/selective/stepwise caries removal
| Core area | Outcome domain | How it is measured | Number of articles reporting outcome | Minimum/maximum follow up |
|---|---|---|---|---|
| Survival | Tooth survival | Tooth present | 2 | 1.5–10 years |
| NS | 4 | 6–62 months | ||
| Physiological/clinical changes | Pain | Patient report | 19 | 1 week–5 years |
| VAS | 2 | |||
| Symptoms | Patient report | 9 | 1 day–62 month | |
| Infection‐swelling, sinus, fistula or abscess | Clinical assessment | 6 | 3 months–3 years | |
| Radiographic evidence disease progression | Radiographic assessment | 19 | 2–62 months | |
| Vitality/sensibility | Cold test only | 15 | 1 week–10 years | |
| Heat and cold test | 1 | |||
| Cold test and EPT | 6 | |||
| Heat and cold test and EPT | 1 | |||
| Cold test or EPT | 2 | |||
| Thermal unspecified and EPT | 1 | |||
| NS | 2 | |||
| Tenderness to percussion /palpation | Clinical assessment | 4 | 1 week–5 years | |
| TTP and palpation | 6 | |||
| TTP only | — | |||
| Palpation only | — | |||
| Mobility | NS | 6 | 3 months–3 years | |
| Continued root development or apexogenesis | Radiographic assessment | 2 | 2 months–11 years | |
| Remineralisation/ hard tissue/dentine barrier formation | Radiographic assessment | 10 | 3 months–10 years | |
| Clinical assessment | 11 | |||
| Radiographic and CBCT | 1 | |||
| Histological assessment | 2 | |||
| Histological evidence of carious process in dentine | Microbiology | 10 | 3–12 months | |
| Integrity /quality of restoration | NS | 5 | 2 months–10 years | |
| Exposure during caries excavation or temporary restoration removal | Clinical assessment | 12 | Baseline–6 months | |
| Life impact | Success | Clinical and radiographic assessment | 12 | 1 week–11 years |
| Clinical assessment | — | — | ||
| Radiographic assessment | — | — | ||
| NS | 4 | 6–62 months | ||
| Aesthetics‐ discolouration | Clinical assessment‐ photographic comparison | 1 | 6 months | |
| Resources use | Need for further intervention | Clinical and radiographic assessment | 13 | 1 week–10 years |
| Time to complete procedure | CROM‐ timed procedure | 1 | 18 months | |
| Use of analgesics after procedure | Patient report | 1 | 1 week–1 year | |
| Adverse effects | Resorption | Radiographic assessment | 3 | 2 months–3 years |
| Change in lesion depth/ secondary caries | Radiographic assessment | 7 | 3 months–10 years | |
| NS | 5 | |||
| Radiographic and CBCT | 1 |
Abbreviations: CBCT, Cone‐beam computed tomography; CROM, Clinician reported outcome measures; EPT, Electric pulp test; NS, not specified; TTP, tender to percussion; VAS, visual analogue scale.
TABLE 3.
Outcomes for DPC
| Core area | Outcome domain | How it is measured | Number of articles reporting outcome | Min/max follow up (day; week; month; year) |
|---|---|---|---|---|
| Survival | Tooth survival | Pulp | 5 | 6 months–9 years |
| Tooth | 4 | 0.4–22 years | ||
| NS | 7 | 1–3 years | ||
| Physiological/Clinical changes | Pain | VAS | 4 | 1–7 days |
| Questionnaire | 1 | 8–30 days | ||
| Patient report | 39 | 1 day–16.6 years | ||
| Verbal pain scale | 1 | 1–6 weeks | ||
| Symptoms | Patient report | 36 | 1 week–7.4 years | |
| Infection‐swelling, sinus, fistula or abscess | Clinical examination | 16 | 1 week–123 months | |
| Radiographic evidence of disease progression | Radiographic assessment | 44 | 3 weeks–22 years | |
| Vitality/sensibility | Cold test only | 16 | 1 week–22 years | |
| EPT only | 7 | |||
| Cold test and EPT | 4 | |||
| Cold test or EPT | 3 | |||
| Thermal unspecified and EPT | 3 | |||
| Heat and cold test and EPT | 2 | |||
| EPT &/or heat or cold | 1 | |||
| Thermal unspecified and Doppler flowmetry | 1 | |||
| Cold test and Doppler flowmetry | 1 | |||
| NS | 10 | |||
| Tenderness to percussion/palpation | TTP and palpation | 8 | 1 week–16.6 years | |
| TTP only | 14 | |||
| Palpation only | 1 | |||
| Mobility | Clinical examination/NS | 7 | 3–123 months | |
| Periodontal probing depths/attachment loss | Clinical examination | 5 | 1–22 years | |
| Continued root development or apexogenesis | Radiographic assessment | 4 | 6 months–22 years | |
| Evidence of inflammatory response | Histology | 28 | 1–300 days | |
| Clinical | 2 | |||
| Hard tissue/dentine barrier formation/remineralisation | Radiographic assessment | 8 | 30 days–22 years | |
| Radiographic and clinical | 1 | 2 months | ||
| Histological assessment | 24 | 7 days–6 months | ||
| Histological and CBCT | 2 | 2 weeks | ||
| Integrity /quality of restoration | Clinical and radiographic | 4 | 12–123 months | |
| Clinical only | 5 | 1 week–8 months | ||
| Life impact | Presence of a functional tooth | NS | 2 | 12–123 months |
| Success | Clinical/ radiographic assessment | 18 | 1 week–6 years | |
| Clinical only | 4 | 0.4–16.6 years | ||
| Radiographic only | 1 | 3 years | ||
| NS | 7 | 1 month–5 years | ||
| Aesthetics‐ discolouration | Clinical assessment | 9 | 1 month–7 years | |
| Visual comparison, photographs | ||||
| Satisfaction with treatment | History and questionnaire | 1 | 8–30 days | |
| Resource use | Need for further intervention | Clinical or radiographic assessment | 22 | 1 month–22.2 years |
| Time to complete procedure | Timed by clinician | 1 | Baseline | |
| Patient comfort | Questionnaire | 1 | Baseline | |
| Emergency attendance for any treatment related to tooth | CROM | 1 | 6–36 months | |
| Need for analgesic medication in postop period | History | 4 | 1 week–1 year | |
| Adverse effects | Calcification | Radiographic assessment | 10 | 6–72 months |
| Resorption | Radiographic assessment | 10 | 6 month–22 years | |
| Histological assessment | 1 | 7–65 days | ||
| Pathological narrowing pulp chamber or canals/ obliteration | Radiographic assessment | 3 | 6 months–3 years | |
| Secondary caries | Clinical and radiographic assessment | 3 | 1–123 months |
Abbreviations: CBCT, Cone‐beam computed tomography; CROM, Clinician reported outcome measure; EPT, electric pulp test; NS, Not specified; TTP, tender to percussion; VAS, Visual analogue Scale.
TABLE 4.
Outcomes of pulpotomy
| Core area | Outcome domain | How it is measured | Number of articles reporting outcome | Min/max follow up (day; week; month; year) |
|---|---|---|---|---|
| Survival | Tooth survival | Tooth present | 1 | 1–29 years |
| NS | 4 | 1–2 years | ||
| Physiological/Clinical changes | Pain | Standardized questionnaire | 1 | 1 day–29 years |
| VAS | 5 | |||
| Numeric rating scale | 3 | |||
| Patient report | 36 | |||
| Symptoms | Patient report | 20 | 1 day–88 months | |
| Infection‐ swelling, sinus, fistula or abscess | Clinical examination | 35 | 1 day–96 months | |
| Radiographic evidence of disease progression | Radiographic assessment | 47 | 1 month–29 years | |
| Vitality/sensibility | Probing dentine barrier to elicit pain | 1 | 6 months | |
| NS | 9 | 2 days–29 years | ||
| Cold test only | 2 | 6–154 months | ||
| Heat and cold test | 1 | 45–60 days | ||
| EPT only | 5 | 1–140 months | ||
| Thermal unspecified | 1 | 3–53 months | ||
| Cold test or EPT | 2 | 12–60 months | ||
| Cold test and EPT | 2 | 3–24 months | ||
| Periapical tests‐ (tenderness to percussion, palpation) | Clinical examination | 8 | 1 month–29 years | |
| TTP and palpation | 24 | |||
| TTP only | — | |||
| Palpation only | — | |||
| Mobility | Clinical examination | 18 | 1–154 months | |
| Periodontal probing depths/attachment loss | Clinical examination | 6 | 2 weeks–88 months | |
| Continued root development or apexogenesis | Radiographic assessment | 17 | 3–154 months | |
| Physiological narrowing of chamber/canals | Radiographic assessment | 2 | 3–48 months | |
| Hard tissue/dentine barrier formation | Radiographic assessment | 31 | 1 month–29 years | |
| Clinical assessment‐ probing | 5 | 45 days–9 months | ||
| Histological assessment | 9 | 5 weeks–20 months | ||
| Histological and radiographic assessment | 1 | 5–24 weeks | ||
| Integrity /quality of restoration | Clinical assessment (2/12 use USPHS criteria) | 12 | 1–88 months | |
| Radiographic assessment | 2 | 2 weeks–62 months | ||
| Histological evidence of pulpal inflammation | Histopathology | 5 | 4 weeks–6 months | |
| Life impact | Functional tooth | NS | 4 | 6–12 months |
| Success | Clinical and radiographic assessment | 23 | 6 weeks–73.6 months | |
| Radiographic and histological assessment | 1 | 6 months | ||
| Aesthetics‐ discolouration | Clinical assessment Visual comparison, photographs | 5 | 6 months–3 years | |
| Resource use | Need for further intervention | Clinical or radiographic assessment | 14 | 1–96 months |
| Time to complete procedure | CROM | 1 | Baseline | |
| Analgesic use in postoperative period | Patient report | 7 | 1 day–3 months | |
| Cost‐effectiveness | Questionnaires | 1 | 2 years | |
| Adverse effects | Calcification | Radiographic assessment | 9 | 3–154 months |
| Resorption | Radiographic assessment | 20 | 1 month–29 years | |
| Pathological narrowing pulp chamber or canals/ obliteration | Radiographic assessment | 11 | 5 weeks–154 months |
Abbreviations: CBCT, Cone‐beam computed tomography systems; CROM, Clinician reported outcome measures; EPT, Electric pulp test; NS, Not specified; TTP, tender to percussion; USPHS, United States Public Health Service; VAS, Visual analogue Scale.
Survival
In the survival core area, the outcome domain was ‘tooth survival’ and ‘pulp survival’. Tooth survival was reported in 2 INDPC studies, 4 DPC studies and 1 pulpotomy study. Pulp survival was reported only in DPC studies (n = 5). Several studies (4 INDPC, 7 DPC, 4 pulpotomy) did not define the type of ‘survival’ being measured.
Clinical and physiological changes
Most of the outcome domains were reported in this core area. Whilst there was some commonality with the reported outcomes, slight differences existed between different VPT modalities (Tables 2, 3, 4). ‘Pain’, maintenance of ‘tooth vitality’ and ‘radiographic assessment’ were frequently reported outcomes across all three VPT methods. ‘Pain’ was reported in 21 INDPC studies, 45 DPC studies and 45 pulpotomy studies. The ‘tooth vitality’ domain was reported in 28 INDPC, 48 DPC and 23 pulpotomy studies. Radiographic assessment was also reported for all three treatments. This assessment was carried out for a variety of indications including radiographic evidence of apical periodontitis in 19 INDPC, 44 DPC and 47 pulpotomy studies. ‘Continued root development’ in cases of immature teeth was reported for 2 INDPC, 4 DPC and 17 pulpotomy studies. Other outcome domains within this core area reported across all treatment types include ‘evidence of infection’, ‘tertiary dentine formation’, ‘tooth mobility’ and ‘integrity or quality of the tooth restoration’. Treatment‐specific outcomes included ‘pulp exposure during caries excavation’, which was reported only in the INDPC studies, and ‘change in carious lesion depth’ which was reported in both the DPC and INDPC studies.
Life impact
The most commonly reported outcome domain in this area across all treatment types was success/healing following the intervention assessed clinically and radiographically (n = 16, 30, 24) for INDPC, DPC and pulpotomy studies, respectively. The definition of success differed between studies and between treatment modalities. ‘Presence of a functional tooth’ was occasionally reported as was ‘discolouration’, and ‘satisfaction with treatment’ (Tables 2, 3, 4).
Use of resources
The ‘need for further intervention’ was the most commonly reported outcome being reported in 13 IDPC, 22 DPC and 14 pulpotomy studies. ‘Use of analgesics’ during the postoperative period and ‘time to complete the procedure’ were also reported across all treatment types, whilst ‘cost‐effectiveness’ was reported in one pulpotomy study only.
Adverse effects
Outcomes were rarely reported in this core area but included, ‘intra‐chamber or pulpal calcification’ (n = 10, 9) and ‘pathological narrowing of the pulp chamber’ (n = 3, 11) reported in DPC and pulpotomy, respectively. Resorption was reported across all three treatment types (n = 3, 11, 20), whilst development of the carious lesion was reported only in INDPC and DPC studies (n = 13, 3).
How were the outcomes measured?
Different methods have been used to measure the reported outcomes. Pain for example, was measured using VAS (n = 11) and NRS (n = 3). Some studies used unspecified questionnaires (n = 2), but in most of the studies (n = 94) pain was reported from patient history using no measurement instrument. Several studies reported presence of symptoms that were not specified (n = 9, 36, 20) for IDPC, DPC and pulpotomy, respectively. Clinical examination was used in most studies to assess outcomes such as pain on percussion and palpation, and presence of signs of infection such as swelling and sinus tract. Radiographic assessment was carried out for various indications but mainly for evidence of periapical changes indicative of disease or healing (n = 110). Other studies reported on root resorption, pathological and physiological narrowing of the pulp chamber, pulpal calcifications, and root development. Assessment of pulpal status was measured using multiple methods including singular or combinations of thermal, electric and Doppler flowmetry tests. Cold only tests were employed in 33 studies, hot and cold tests combined (n = 2), electric only (n = 12), cold and heat tests combined with electric (n = 3). Doppler flowmetry was employed in two studies. In many studies the type of thermal test used was not specified (n = 6) whereas in others the method used for assessing vitality/sensibility was not specified (n = 21). One pulpotomy study involved probing the calcific barrier for evidence of vitality whilst a further 21 studies did not specify the method of measurement in reporting this outcome. Although the level of pulpal inflammation can be assessed objectively by measurement of selected biomarker levels, none of the included studies reported adoption of this measure. Outcomes related to life impact such as functionality of the tooth were reported from the patient history. No study reported global quality‐of‐life measures.
When are the outcomes measured?
The minimum and maximum follow up time for outcomes depended largely on the nature of the outcome and treatment modality. Pain and symptoms of pulpal disease were usually reported for short‐, as well as long‐term (range: 1 day to 29 years). Histological outcomes were frequently reported in the short‐ to medium‐term (range: 1 week to 20 months) whilst evidence of tissue healing usually requires a long‐term follow up. There is inconsistency in the timing of reporting, even within the early and late outcome categories.
Outcome reporting bias
An assessment of selective reporting bias within the included reviews is outlined in Tables 5. The outcomes reported in this review covered all the five core healthcare areas, albeit with a high level of heterogeneity (Tables 2, 3, 4). All the reviews assessing risk of selective reporting bias for RCT followed by Cochrane's Risk of Bias tool. Several reporting methodologies were used for other study designs including Newcastle‐Ottawa Scale (n = 4), modified Downs & Black (n = 3), Methodological Index for Non‐Randomized Studies MINORS (n = 2), Risk of Bias in Non‐Randomized Studies‐of Interventions ROBINS‐I (n = 3) and Critical Appraisal Skills Programme CASP (n = 1).
TABLE 5.
Selective reporting bias in (A) indirect pulp capping studies; (B) direct pulp capping studies; (C) pulpotomy studies; (D) combined vital pulp treatment studies
| Systematic review | Method for assessing risk of bias (RCT/CCT) | Selective reporting bias risk |
|---|---|---|
| (A) | ||
| Barros 2020 | Cochrane RoB and NOS | All low |
| da Rosa 2019 | Cochrane's Collaboration | All low |
| Hayashi 2011 | Not reported | |
| Hoefler 2016 | Cochrane's Collaboration & NOS | 1 high, 1 low |
| Kiranmayi 2019 | Cochrane RoB | 5 low, 1 not specified |
| Li 2018 | Cochrane RoB | All low |
| Ricketts 2013 | Cochrane RoB | All low |
| Ricketts 2006 | Cochrane guidelines | Not reported |
| Schwendicke 2013 | Cochrane RoB | 2 Low, 9 unclear, 3 high |
| Schwendicke 2013 | Cochrane RoB | 1 Low, 3 unclear |
| (B) | ||
| Cushley 2020 | Cochrane RoB, Modified Downs & Black | All low for RCT |
| Deng 2016 | Cochrane RoB | All low |
| Edwards 2020 | Cochrane RoB | All low |
| Javed 2017 | CASP | Not specified |
| Li 2015 | Cochrane RoB | All low |
| Mahmoud 2018 | Cochrane's Collaboration a | Not specified |
| Matsuura 2019 | Cochrane RoB | All low |
| Schwendicke 2016 | Cochrane RoB | 1 unclear, 4 low |
| Zhu 2015 | Not reported | |
| (C) | ||
| Alqaderi 2016 | Cochrane RoB and NOS | All low |
| Chen 2019 | Cochrane RoB | All low |
| Cushley 2019 | Cochrane RoB | Unclear |
| Elmsmari 2019 | Cochrane RoB NOS | All low |
| Li 2019 | Cochrane RoB | All low |
| Taylor 2020 | Cochrane RoB | All high |
| Zafar 2020 | Cochrane RoB | All low |
| Zanini 2019 | Not reported | |
| (D) | ||
| Aguilar 2011 | Not reported | |
| Bergenholtz 2013 | Not reported | |
| Broden 2016 | Not reported | |
| Didilescu 2018 | Cochrane RoB | All low b |
| Fransson 2016 | Not reported | |
| Maghoub 2019 | Modified Downs & Black | Not specified |
| Miyashita 2007 | Not reported | |
| Munir 2020 | Cochrane RoB‐2 | All low |
| Paula 2018 | Cochrane RoB | 28 low, 1 high |
Abbreviations: CASP, Critical Appraisal Skills Programme; CCT, controlled clinical trial; NOS, Newcastle Ottawa Scale; RCT, randomized controlled trials; RoB, Risk of bias.
No RCT was included.
RoB not completed for all included RCT and CCTs.
Of the included reviews, 10 failed to completely report on the risk of selective reporting bias. Due to the measurement scale adopted, selective reporting bias was not specified in four reviews. Lack of reporting of selective reporting bias seemed to be a problem with the systematic reviews that reported on a combination of VPTs (Table 5D).
DISCUSSION
Summary of evidence
This scoping review has identified outcomes of VPT reported in clinical studies and how and when these outcomes were measured. A large number of systemic reviews representing a variable number of clinical studies were eligible for inclusion. The outcomes reported in these studies fell within the five core areas defined in the taxonomy developed for health interventions (Dodd et al., 2018). There is evidence of heterogeneity in the outcome definitions and reporting across the three VPT modalities investigated. The same was also noted for the instruments and timing used for measuring the reported outcomes.
The results of the current review will be used to identify outcomes for the development of a COS for endodontic treatments (El Karim, Duncan, et al., 2021). The findings of the review demonstrated clear lack of consensus and standardization in outcomes reporting in the included studies, highlighting the need for a COS for VPT. The review has also shown that the majority of the outcomes reported are clinician‐reported outcomes with fewer reports focussing on patient‐reported outcomes. For instance, tooth survival is one of the most important patient‐reported outcomes (Ng et al., 2011), but was reported by few studies. In some studies where “survival” was mentioned, there was no specific reference to whether it was tooth or pulp survival. The most important patient‐reported outcome is oral health‐related quality of life (OHRQoL), which is a significant contributor to overall health‐related quality of life (John, 2020). Surprisingly, none of the clinical studies assessed the global quality of life of patients after undergoing VPT whilst a small number did report on tooth function, tooth discolouration and treatment satisfaction postintervention.
A range of different instruments have been used for the measurement of outcomes. In most of the studies, pain experience was only obtained through patient history. Some studies used a numerical rating scale (NRS) and nonspecified questionnaires, whilst the visual analogue scale (VAS), which is more sensitive than other pain scales (Price et al., 1994), was used in few studies. This lack of standardization in reporting pain is a major problem for meta‐analysis in systematic reviews reporting on endodontic pain (Vishwanathaiah et al., 2021). There are many other patient‐reported outcomes such as cost effectiveness of treatment and satisfaction with treatment which are not reported in most of the studies. It is also not clear whether all outcomes are accounted for in these studies because assessment for selective reporting bias revealed many of the reviews did not report this and many others found high selective reporting bias.
The optimal time for measuring a specific outcome or end point is important for patient‐reported outcomes (Browne et al., 2013), but it is evident from this review that a range of timings and follow ups have been used in research. Whilst there is no clear indication of the optimal time to measure long‐term vs short‐term outcomes, a recent publication has identified time points appropriate for VPT follow up (Duncan, Nagendrababu, et al., 2021).
Although a recent scoping review reported on the outcomes of endodontic treatments (Azarpazhooh et al., 2022), the review reported here is the first to adopt the health intervention taxonomy to summarize outcomes into a format compatible with COS development covering the breadth of VPTs.
Strengths of review
The review design was appropriately based on the need to conduct a preliminary assessment of the available literature and capture data from a wide range of study designs, adopting a range of methodologies. A robust, transparent and reproducible methodology was employed throughout the review process. Thorough database searches combined with the screening of the reference lists of the 36 included reviews and use of an electronic library minimized the risk of missing studies. Finally, including the full range of study designs more closely mimics clinical practice optimizing the likelihood of inclusion of any study which reported clinical and/or radiographic outcomes as a minimum.
Limitations of review
Whilst systematic reviews bring together the findings of primary research, the applicability and reliability of their conclusions is only as accurate as the included studies. Having based our search strategy on existing systematic reviews, the accuracy of this review is reliant on the original review authors' development of a focussed and comprehensive search strategy. However, these authors did employ inclusive and appropriate search terms across the breadth of health‐related databases minimizing the likelihood of missing literature. Language restrictions were applied in several of the systematic reviews, and in this review, which was limited to reviews published in English. Although often done for practical reasons, this does exclude research in this area that was published in other languages. Restricting inclusion to published reviews only also risks the introduction of publication bias. Heterogeneity in the terminology used within studies to describe seemingly similar constructs was apparent. Criteria of success of treatment for example, when reported, differed across studies and between mature and immature teeth. Finally, one author extracted the data which increases the risk of misclassification within the taxonomy. This was mitigated by having a second author verify the results, and repeated checks during the piloting of the extraction form and the classification process.
Future directions
This review clearly demonstrates large heterogeneity and a lack of standardization in reporting outcome of VPTs. The number of included studies in the included reviews highlights the increasing interest in VPTs. Therefore, improvements in the reporting of future clinical studies and evidence synthesis and the quality of clinical decision making, will require the development of an agreed set of patient‐ and clinician‐reported outcomes for VPT.
CONCLUSION
The evidence in this review suggests that there is considerable heterogeneity in the outcomes reported in VPT research, with only minimal commonality across methods and timing of measurement. Moreover, aside from pain measurement, there is a general paucity of patient‐reported outcomes reflecting the need to ensure the valuable addition of patient experience is not missed when designing, conducting and reporting clinical trials. Within the limitations of this review, however, there is the opportunity to seek consensus and develop a COS to improve healthcare provision in VPT and the wider discipline of endodontics.
AUTHOR CONTRIBUTIONS
All the authors have made relevant contributions to the manuscript. All the authors have read and approved the final version of the manuscript.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ETHICAL STATEMENT
Ethical approval was not necessary as this article is secondary research involving review of the literature.
Supporting information
Table S1
Table S2
Table S3
Table S4
Cushley, S. , Duncan, H.F. , Lundy, F.T. , Nagendrababu, V. , Clarke, M. & El Karim, I. (2022) Outcomes reporting in systematic reviews on vital pulp treatment: A scoping review for the development of a core outcome set. International Endodontic Journal, 55, 891–909. Available from: 10.1111/iej.13785
Funding information
This work was supported by HSC R&D Division, Public Health Agency [EAT/5579/19]
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study
REFERENCES
- Aguilar, P. & Linsuwanont, P. (2011) Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. Journal of Endodontics, 37, 581–587. [DOI] [PubMed] [Google Scholar]
- Alqaderi, H. , Lee, C.T. , Borzangy, S. & Pagonis, T.C. (2016) Coronal pulpotomy for carious;y exposed permanent posterior teeth with closed apices: a systematic review and meta‐analysis. Journal of Dentistry, 44, 1–7. [DOI] [PubMed] [Google Scholar]
- Asgary, S. , Eghbal, M.J. & Bagheban, A.A. (2017) Long‐term outcomes of pulpotomy in permanent teeth with irreversible pulpitis: a multi‐center randomized controlled trial. American Journal of Dentistry, 30, 151–155. [PubMed] [Google Scholar]
- Azarpazhooh, A. , Sgro, A. , Cardoso, E. , Elbarbary, M. , Laghapour Lighvan, N. , Badewy, R. et al. (2022) A scoping review of 4 decades of outcomes in nonsurgical root canal treatment, nonsurgical retreatment, and apexification studies‐part 2: outcome measures. Journal of Endodontics, 48, 29–39. [DOI] [PubMed] [Google Scholar]
- Barros, M.M.A.F. , De Queiroz Rodrigues, M.I. , Muniz, F.W.M.G. & Rodrigues, L.K.A. (2020) Selective, stepwise, or nonselective removal of carious tissue: which technique offers lower risk for the treatment of dental caries in permanent teeth? A systematic review and meta‐analysis. Clinical Oral Investigations, 24, 521–532. [DOI] [PubMed] [Google Scholar]
- Bergenholtz, G. , Axelsson, S. , Davidson, T. , Frisk, F. , Hakeberg, M. , Kvist, T. et al. (2013) Treatment of pulps in teeth affected by deep caries – a systematic review of the literature. [review]. Singapore Dental Journal, 34, 1–12. [DOI] [PubMed] [Google Scholar]
- Bjørndal, L. , Fransson, H. , Bruun, G. , Markvart, M. , Kjældgaard, M. , Näsman, P. et al. (2017) Randomized clinical trials on deep carious lesions: 5‐year follow‐up. Journal of Dental Research, 96, 747–753. [DOI] [PubMed] [Google Scholar]
- Boers, M. , Kirwan, J.R. , Wells, G. , Beaton, D. , Gossec, L. , D'Agostino, M.A. et al. (2014) Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. Journal of Clinical Epidemiology, 67, 745–753. [DOI] [PubMed] [Google Scholar]
- Brodén, J. , Heimdal, H. , Josephsson, O. & Fransson, H. (2016) Direct pulp capping versus root canal treatment in young permanent vital teeth with pulp exposure due to caries. A systematic review. American Journal of Dentistry, 29, 201–207. [PubMed] [Google Scholar]
- Browne, J. , Bastaki, H. & Dawson, J. (2013) What is the optimal time point to assess patient‐reported recovery after hip and knee replacement? A systematic review and analysis of routinely reported outcome data from the English patient‐reported outcome measures programme. Health and Quality of Life Outcomes, 11, 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y. , Chen, X. , Zhang, Y. , Zhou, F. , Deng, J. , Zou, J. et al. (2019) Materials for pulpotomy in immature permanent teeth: a systematic review and meta‐analysis. BMC Oral Health, 19, 227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, M. (2008) Standardising outcomes in Paediatric clinical trials. PLoS Medicine, 5, e102. [Google Scholar]
- Cushley, S. , Duncan, H.F. , Lappin, M.J. , Chua, P. , Elamin, A.D. , Clarke, M. et al. (2019) Pulpotomy for mature carious teeth with symptoms of irreversible pulpitis: a systematic review. Journal of Dentistry, 88, 103158. [DOI] [PubMed] [Google Scholar]
- Cushley, S. , Duncan, H.F. , Lappin, M.J. , Chua, P. , Elamin, A.D. , Clarke, M. et al. (2020) Efficacy of direct pulp capping for management of cariously exposed pulps in permanent teeth: a systematic review and meta‐analysis. International Endodontic Journal, 54, 556–571. [DOI] [PubMed] [Google Scholar]
- Da Rosa, W.L.O. , Lima, V.P. , Moraes, R.R. , Piva, E. & Da Silva, A.F. (2019) Is a calcium hydroxide liner necessary in the treatment of deep caries lesions? A systematic review and meta‐analysis. International Endodontic Journal, 52, 588–603. [DOI] [PubMed] [Google Scholar]
- Deng, Y. , Zhu, X. , Zheng, D. , Yan, P. & Jiang, H. (2016) Laser use in direct pulp capping: a meta‐analysis. Journal of the American Dental Association, 147, 935–942. [DOI] [PubMed] [Google Scholar]
- Didilescu, A.C. , Cristache, C.M. , Andrei, M. , Voicu, G. & Perlea, P. (2018) The effect of dental pulp‐capping materials on hard‐tissue barrier formation: a systematic review and meta‐analysis. Journal of the American Dental Association, 149, 903–917.e4. [DOI] [PubMed] [Google Scholar]
- Dodd, S. , Clarke, M. , Becker, L. , Mavergames, C. , Fish, R. & Williamson, P.R. (2018) A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. Journal of Clinical Epidemiology, 96, 84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan, H.F. , Chong, B.S. , Del Fabbro, M. , El‐Karim, I. , Galler, K. , Kirkevang, L.L. et al. (2021) The development of European society of endodontology S3‐level guidelines for the treatment of pulpal and apical disease. International Endodontic Journal, 54, 643–645. [DOI] [PubMed] [Google Scholar]
- Duncan, H.F. , Cooper, P.R. & Smith, A.J. (2019) Dissecting dentine‐pulp injury and wound healing responses: consequences for regenerative endodontics. International Endodontic Journal, 52, 261–266. [DOI] [PubMed] [Google Scholar]
- Duncan, H.F. , Galler, K.M. , Tomson, P.L. , Simon, S. , El‐Karim, I. , Kundzina, R. et al. (2019) European Society of Endodontology position statement: management of deep caries and the exposed pulp. International Endodontic Journal, 52, 923–934. [DOI] [PubMed] [Google Scholar]
- Duncan, H.F. , Nagendrababu, V. , El‐Karim, I. & Dummer, P.M.H. (2021) Outcome measures to assess the effectiveness of endodontic treatment for pulpitis and apical periodontitis for use in the development of European society of endodontology S3‐level clinical practice guidelines: a consensus‐based development. International Endodontic Journal, 54, 2184–2194. [DOI] [PubMed] [Google Scholar]
- Edwards, D.C. , Burns, L. , Witton, R. & Tredwin, C. (2020) MTA or calcium hydroxide for direct pulp capping in fully developed permanent teeth: a systematic review. Endo‐Endodontic Practice Today, 14, 91–102. [Google Scholar]
- El Karim, I.A. , Cooper, P.R. , About, I. , Tomson, P.L. , Lundy, F.T. & Duncan, H.F. (2021) Deciphering reparative processes in the inflamed dental pulp. Frontiers in Dental Medicine, 2, 1–10. [Google Scholar]
- El Karim, I.A. , Duncan, H.F. , Cushley, S. , Nagendrababu, V. , Kirkevang, L.L. , Kruse, C. et al. (2021) A protocol for the development of Core outcome sets for endodontic treatment modalities (COSET): an international consensus process. Trials, 22, 812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmsmari, F. , Ruiz, X.F. , Miro, Q. , Feijoo‐Pato, N. , Duran‐Sindreu, F. & Olivieri, J.G. (2019) Outcome of partial pulpotomy in cariously exposed posterior permanent teeth: a systematic review and meta‐analysis. Journal of Endodontics, 45, 1296–1306. [DOI] [PubMed] [Google Scholar]
- Fransson, H. , Wolf, E. & Petersson, K. (2016) Formation of a hard tissue barrier after experimental pulp capping or partial pulpotomy in humans: an updated systematic review. International Endodontic Journal, 49, 533–542. [DOI] [PubMed] [Google Scholar]
- Hayashi, M. , Fujitani, M. , Yamaki, C. & Momoi, Y. (2011) Ways of enhancing pulp preservation by stepwise excavation‐‐a systematic review. Journal of Dentistry, 39, 95–107. [DOI] [PubMed] [Google Scholar]
- Hoefler, V. , Nagaoka, H. & Miller, C.S. (2016) Long‐term survival and vitality outcomes of permanent teeth following deep caries treatment with step‐wise and partial‐caries‐removal: a systematic review. Journal of Dentistry, 54, 25–32. [DOI] [PubMed] [Google Scholar]
- Javed, F. , Kellesarian, S.V. , Abduljabbar, T. , Gholamiazizi, E. , Feng, C. , Aldosary, K. et al. (2017) Role of laser irradiation in direct pulp capping procedures: a systematic review and meta‐analysis. Lasers in Medical Science, 32, 439–448. [DOI] [PubMed] [Google Scholar]
- John, M.T. (2020) Foundations of oral health‐related quality of life. Journal of Oral Rehabilitation, 48, 355–359. [DOI] [PubMed] [Google Scholar]
- Kiranmayi, G. , Hussainy, N. , Lavanya, A. & Swapna, S. (2019) Clinical performance of mineral trioxide aggregate versus calcium hydroxide as indirect pulp‐capping agents in permanent teeth: a systematic review and meta‐analysis. Journal of International Oral Health, 11, 235–243. [Google Scholar]
- Kirkham, J.J. , Davis, K. , Altman, D.G. , Blazeby, J.M. , Clarke, M. , Tunis, S. et al. (2017) Core outcome set‐STAndards for development: the COS‐STAD recommendations. PLoS Medicine, 14, e1002447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham, J.J. , Gorst, S. , Altman, D.G. , Blazeby, J.M. , Clarke, M. , Devane, D. et al. (2016) Core outcome set–STAndards for reporting: the COS‐STAR statement. PLoS Medicine, 13, e1002148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Z.F. , Cao, L.H. , Fan, M.W. & Xu, Q.G. (2015) Direct pulp capping with calcium hydroxide or mineral trioxide aggregate: a meta‐analysis. Journal of Endodontics, 41, 1412–1417. [DOI] [PubMed] [Google Scholar]
- Li, Y.Y. , Sui, B.D. , Dahl, C. , Bergeron, B. , Shipman, P. , Niu, L. et al. (2019) Pulpotomy for carious pulp exposures in permanent teeth: a systematic review and meta‐analysis. Journal of Dentistry, 84, 1–8. [DOI] [PubMed] [Google Scholar]
- Li, T. , Zhai, X. , Song, F. & Zhu, H. (2018) Selective versus non‐selective removal for dental caries: a systematic review and meta‐analysis. [review]. Acta Odontologica Scandinavica, 76, 135–140. [DOI] [PubMed] [Google Scholar]
- Mahgoub, N. , Alqadasi, B. , Aldhorae, K. , Assiry, A. , Altawili, Z.M. & Hong, T. (2019) Comparison between iRoot BP plus (EndoSequence root repair material) and mineral trioxide aggregate as pulp‐capping agents: a systematic review. Journal of International Society of Preventive and Community Dentistry, 9, 542–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoud, S.H. , El‐Negoly, S.A. , Zaen El‐Din, A.M. , El‐Zekrid, M.H. , Grawish, L.M. , Grawish, H.M. et al. (2018) Biodentine versus mineral trioxide aggregate as a direct pulp capping material for human mature permanent teeth – a systematic review. Journal of Conservative Dentistry, 21, 466–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuura, T. , Kawata‐Matsuura, V.K.S. & Yamada, S. (2019) Long‐term clinical and radiographic evaluation of the effectiveness of direct pulp‐capping materials. Journal of Oral Science, 61, 1–12. [DOI] [PubMed] [Google Scholar]
- Miyashita, H. , Worthington, H.V. , Qualtrough, A. & Plasschaert, A. (2007) Pulp management for caries in adults: maintaining pulp vitality. Cochrane Database of Systematic Reviews, 11, CD004484. [DOI] [PubMed] [Google Scholar]
- Munir, A. , Zehnder, M. & Rechenberg, D.K. (2020) Wound lavage in studies on vital pulp therapy of permanent teeth with carious exposures: a qualitative systematic review. Journal of Clinical Medicine, 9, 989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair, P.N. , Duncan, H.F. , Pitt Ford, T.R. & Luder, H.U. (2008) Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: a randomized controlled trial. International Endodontic Journal, 41, 128–150. [DOI] [PubMed] [Google Scholar]
- Ng, Y.L. , Mann, V. & Gulabivala, K. (2011) A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. International Endodontic Journal, 44, 583–609. [DOI] [PubMed] [Google Scholar]
- Parirokh, M. , Torabinejad, M. & Dummer, P.M.H. (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview ‐ part I: vital pulp therapy. International Endodontic Journal, 51, 177–205. [DOI] [PubMed] [Google Scholar]
- Paula, A.B. , Laranjo, M. , Marto, C.M. , Paulo, S. , Abrantes, A.M. , Casalta‐Lopes, J. et al. (2018) Direct pulp capping: what is the MOST effective therapy?‐Systematic review and META‐analysis. The Journal of Evidence‐Based Dental Practice, 18, 298–314. [DOI] [PubMed] [Google Scholar]
- Price, D.D. , Bush, F.M. , Long, S. & Harkins, S.W. (1994) A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain, 56, 217–226. [DOI] [PubMed] [Google Scholar]
- Ricketts, D.N. , Kidd, E.A. , Innes, N. & Clarkson, J. (2007) Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database of Systematic Reviews, 3, CD003808. [DOI] [PubMed] [Google Scholar]
- Ricketts, D. , Lamont, T. , Innes, N.P.T. , Kidd, E. & Clarkson, J.E. (2013) Operative caries management in adults and children. Cochrane Database of Systematic Reviews, 3, CD003808. [DOI] [PubMed] [Google Scholar]
- Rosenbaum, S.E. , Glenton, C. & Oxman, A.D. (2010) Summary‐of‐findings tables in Cochrane reviews improved understanding and rapid retrieval of key information. Journal of Clinical Epidemiology, 63, 620–626. [DOI] [PubMed] [Google Scholar]
- Saldanha, I.J. , Lindsley, K.B. , Money, S. , Kimmel, H.J. , Smith, B.T. & Dickersin, K. (2020) Outcome choice and definition in systematic reviews leads to few eligible studies included in meta‐analyses: a case study. BMC Medical Research Methodology, 20, 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwendicke, F. , Brouwer, F. , Schwendicke, A. & Paris, S. (2016) Different materials for direct pulp capping: systematic review and meta‐analysis and trial sequential analysis. Clinical Oral Investigations, 20, 1121–1132. [DOI] [PubMed] [Google Scholar]
- Schwendicke, F. , Dorfer, C.E. & Paris, S. (2013) Incomplete caries removal: a systematic review and meta‐analysis. Journal of Dental Research, 92, 306–314. [DOI] [PubMed] [Google Scholar]
- Schwendicke, F. , Meyer‐Lueckel, H. , Dorfer, C. & Paris, S. (2013) Failure of incompletely excavated teeth‐A systematic review. Journal of Dentistry, 41, 569–580. [DOI] [PubMed] [Google Scholar]
- Taha, N.A. & Abdulkhader, S.Z. (2018) Full pulpotomy with biodentine in symptomatic young permanent teeth with carious exposure. Journal of Endodontics, 44, 932–937. [DOI] [PubMed] [Google Scholar]
- Taylor, G.D. , Vernazza, C.R. & Abdulmohsen, B. (2020) Success of endodontic management of compromised first permanent molars in children: a systematic review. International Journal of Paediatric Dentistry, 30, 370–380. [DOI] [PubMed] [Google Scholar]
- Tricco, A.C. , Lillie, E. , Zarin, W. , O'Brien, K.K. , Colquhoun, H. , Levac, D. et al. (2018) PRISMA extension for scoping reviews (PRISMA‐ScR): checklist and explanation. Annals of Internal Medicine, 169, 467–473. [DOI] [PubMed] [Google Scholar]
- Vishwanathaiah, S. , Maganur, P.C. , Khanagar, S.B. , Chohan, H. , Testarelli, L. , Mazzoni, A. et al. (2021) The incidence and intensity of Postendodontic pain and flareup in single and multiple visit root canal treatments: a systematic review and meta‐analysis. Applied Sciences, 11, 3358. [Google Scholar]
- Williamson, P.R. , Altman, D.G. , Blazeby, J.M. , Clarke, M. , Devane, D. , Gargon, E. et al. (2012) Developing core outcome sets for clinical trials: issues to consider. Trials, 13, 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zafar, K. , Nazeer, M.R. , Ghafoor, R. & Khan, F.R. (2020) Success of pulpotomy in mature permanent teeth with irreversible pulpitis: a systematic review. Journal of Conservative Dentistry, 23, 121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanini, M. , Hennequin, M. & Cousson, P.Y. (2019) Which procedures and materials could be applied for full pulpotomy in permanent mature teeth? A systematic review. Acta Odontologica Scandinavica, 77, 541–551. [DOI] [PubMed] [Google Scholar]
- Zhu, C.X. , Ju, B. & Ni, R. (2015) Clinical outcome of direct pulp capping with MTA or calcium hydroxide: a systematic review and meta‐analysis. International Journal of Clinical and Experimental Medicine, 8, 17055–17060. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Table S2
Table S3
Table S4
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study


