Abstract
While exposure to irritant and sprayed cleaning products at home is known to have a harmful role in asthma, the potential health effect of other categories or forms has not been investigated. We studied the associations of household use of cleaning products, including green, homemade products, and disinfecting wipes, with asthma based on data from the large French population‐based CONSTANCES cohort. Participants completed standardized questionnaires on respiratory health and household use of cleaning products. Cross‐sectional associations of cleaning products with current asthma, adjusted for gender, age, smoking status, BMI, and educational level, were evaluated by logistic regressions. Analyses were conducted in 41 570 participants (mean age: 47 years, 56% women, weekly use of the six specific products/forms studied varied from 11% to 37%). Weekly use of irritants (OR = 1.23 [1.13–1.35]), scented (OR = 1.15 [1.06–1.26]), green (OR = 1.09 [1.00–1.20]), and homemade products (OR = 1.19 [1.06–1.34]), as well as sprays (OR = 1.18 [1.08–1.29]), disinfecting wipes (OR = 1.21 [1.09–1.34]) were significantly associated with asthma, with significant trends according to the frequency of use. When they were not co‐used with irritants/sprays, associations were reduced and persisted only for disinfecting wipes. Weekly use of disinfecting wipes at home was associated with current asthma, but fewer risks were observed for the use of green and homemade products.
Keywords: asthma, household cleaning, disinfecting wipes, green products, homemade cleaning products, irritants
Practical implications.
Green and home‐made products or disinfecting wipes, are increasingly attracting the interest of consumers, at the expense of conventional products, but their respiratory health risks have not been investigated
Weekly use of disinfecting wipes at home was associated with asthma, similarly to irritants and sprays, in this study of 41,570 French adults from the CONSTANCES cohort.
These associations persisted only for disinfecting wipes and were no longer observed for green and home‐made products, when considering the co‐use of irritants and sprayed products at home.
Our results suggest that using green and home‐made products may induce fewer risk for respiratory health than using conventional ones.
1. INTRODUCTION
Cleaning products are widely used, at home and in the workplace, and contribute significantly to chemical exposure in the indoor environment. 1 , 2 These products consist of a complex and diverse mixture of ingredients, with various physical and chemical properties, which can have irritant or sensitizing effects. 1 , 3 , 4 , 5 , 6 , 7 Evidence of the harmful role of these products on respiratory health, especially on asthma, comes largely from epidemiological studies carried out in populations highly exposed at work. 3 , 8 Over the past 15 years, a growing number of studies have investigated the effects of indoor exposure to household cleaning products and similar results have been observed. Most studies so far have considered the potential impact of the personal use of cleaning products containing irritant agents 9 , 10 , 11 , 12 , 13 or applied in a spray form. 9 , 11 , 13 , 14 , 15 , 16 , 17 , 18 Personal use of these two categories of cleaning products at home has been shown to be associated with the development, 13 , 18 clinical expression, 10 , 11 , 12 , 14 , 16 and poor control of asthma. 9 , 16 The clinical expression of asthma was mainly studied though the evaluation of current asthma 10 , 12 , 14 , 16 and the asthma symptom score. 11 , 12 , 14 , 16 Studies have suggested that risks for respiratory health could be even more important for women who are more involved in household tasks, and therefore also more exposed to cleaning products. 19 In addition, the female lungs might be more susceptible to the harmful damages of environmental exposures. 20 However, only few studies have assessed the associations between the use of cleaning products and asthma on mixed gender populations. 13 , 18
A wide variety of cleaning products, in several application modes and for various uses, are available to consumers. 2 More recently, “eco‐friendly” certified cleaning products are increasingly attracting the interest of consumers, manufacturers, and distributors. However, although the formulations of these products are considered to be less harmful, especially for the environment, their potential health effects have not been studied for household use. 6 , 8 , 21 An occupational study investigated for the first time the health effects of environmentally preferable products and did not show increased respiratory symptoms associated with this exposure, in contrast to exposure to traditional products. 22 More recently, an experimental study found that green products used during bathroom cleaning generated less total volatile organic compounds than other conventional products. 23 In addition, an interventional study showed a significant decrease in air concentrations of multiples volatile organic compounds when using green products, instead of using conventional ones. 24 While an increasing number of people are making their own products for home cleaning, for example, from white vinegar, 25 baking soda, soap, and sometimes essential oils, their health consequences have not yet been assessed.
Exposure to cleaning products depends on both the physicochemical characteristics of the product and its application mode. 1 , 6 , 21 , 26 Spray formulations increase the risk of inhalation and facilitates the penetration of sprayed particles into the lower respiratory tract. 19 , 27 , 28 Respiratory health risks associated with spraying application mode have been well‐established and studies found consistent associations with asthma both at home 9 , 14 , 16 , 18 and at work. 29 , 30 , 31 , 32 , 33 While a German study showed an association between a high level use of disinfectants at home, regardless of application mode, and a risk of incident asthma in young adults, 13 no study has investigated the potential impact of applying disinfectants in wipes form. Because ready‐to‐use wipes consist of towels saturated with diluted disinfectant and other chemical products, 34 with both irritant and sensitizing properties, 3 they may contain much more products compared to a product applied with a cloth and then wiped.
Thus, despite the accumulation of evidence on the adverse effects of the household use of cleaning products on asthma, evidence is lacking for some products including green and homemade products, and for some application modes, such as wipes, which are all increasingly used but their impact has never been studied to date in epidemiological surveys. We aimed to investigate the associations between household use of six large categories of cleaning products, current asthma and the asthma symptom score among French adults from the CONSTANCES cohort, after considering potential co‐exposures at home to irritants and sprays for which respiratory health effects have been shown. We hypothesized that applying disinfectants in a wipe form would have adverse effect on respiratory health and using green and homemade products would have less adverse effect on respiratory health, compared to conventional products.
2. METHODS
2.1. Population
The CONSTANCES study is a French prospective and generalist epidemiological cohort initiated in 2012, which focuses on occupational, behavioral and social factors related to chronic diseases and aging. 35 The study enrolled 214 816 adults, aged between 18 and 69 years at inclusion, randomly selected among the insured subjects of the general social security scheme of 21 departments of metropolitan France. Information on respiratory health, including asthma, was collected by self‐administered standardized questionnaires at inclusion. Follow‐up questionnaires are sent every year. Household exposure to cleaning products was estimated during the follow‐up in 2019, by a standardized questionnaire.
As respiratory health and household exposures were evaluated at different time‐points, we only included participants who completed the baseline (including respiratory health) and 2019 (including household exposures) questionnaires within a timeframe of 2 years or less. Thus, the analyses focused on participants included in the cohort in 2017 and 2018 with available data on household exposure in 2019. In our study, we assume no major change in household cleaning habits in 2 years.
2.2. Current asthma and the asthma symptom score
Participants who answered positively to the question “Have you ever had asthma?” were considered as “ever asthma,” and otherwise as “never asthma.” Among participants with “ever asthma,” those who reported asthma symptoms (wheezing, woken up by a feeling of chest tightness or an attack of shortness of breath, attack of shortness of breath at rest or after exercise), asthma attacks or asthma treatment in the past 12 months were classified as “current asthma.” 10 , 12 , 14 , 16 Participants with remission asthma were excluded from these analyses (Figure 1).
FIGURE 1.
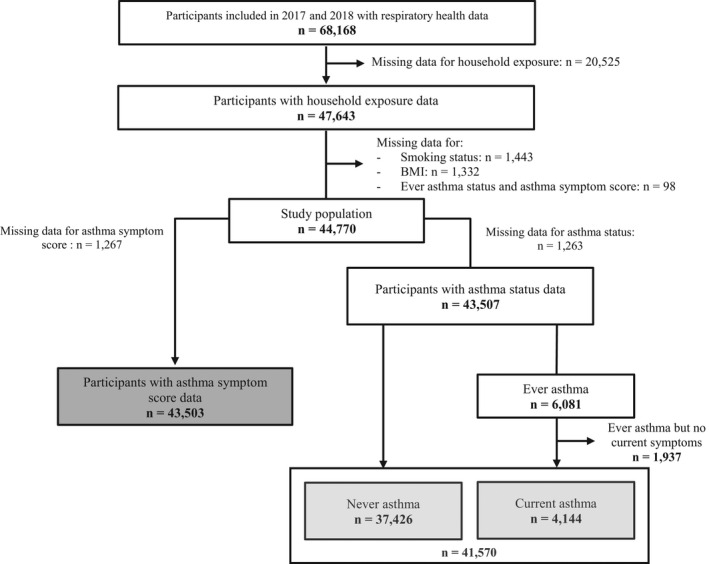
Flowchart of the study population
The asthma symptom score was calculated as described in the literature, 36 , 37 regardless of asthma status. It corresponds to the number of asthma symptoms out of five reported in the standardized questionnaire in the past 12 months (wheezing with shortness of breath, woken up by a feeling of chest tightness or an attack of shortness of breath, attack of shortness of breath at rest or after exercise). It was studied as a continuous variable (0–5).
2.3. Household use of cleaning products
The household exposure questionnaire evaluated the participants' weekly use of various products at home in the past 12 months. We studied household exposure to six large categories including four type of compounds: irritants (maximum frequency reported for bleach, ammonia, acids, and solvents), scented products (maximum frequency reported for scented cleaning products, home fragrances, scented candles, electric, or spray air freshener), green products and homemade products, and two application modes: sprays (maximum frequency reported for furniture, glass, floor, bath, oven, ironing, air freshener, insecticide, or other use) and disinfecting wipes.
The frequency of use of home cleaning products was reported according to four categories: never, less than 1 day a week, 1–3 days a week or 4–7 days a week. In the analyses, “never” and “less than one day a week” were grouped together to define the “unexposed” group, as it is commonly done. 10 , 11 , 12 , 14 , 16 , 18 For a given cleaning product, participants classified as “unexposed” but who are weekly exposed to one of the others five large categories studied were excluded from the analyses. Thus, the reference group (not weekly exposed to any of the six large categories) was the same for all analyses, as previously done. 9 , 38 Frequency of use was studied as a variable in three classes (reference, 1–3 days a week, 4–7 days a week) in the main analyses and as a binary variable (reference, ≥1 day a week) in stratified analyses.
The number of cleaning products used was calculated for irritants, sprays, and scented products (composite variables). The number of irritants used per week was assessed in three classes (reference, 1 irritant per week, ≥2 irritants per week). The number of sprays and the number of scented products were defined in four classes (reference, 1 product per week, 2 products per week, ≥3 products per week).
2.4. Statistical analysis
Associations between household exposure to cleaning products, current asthma and the asthma symptom score were evaluated by logistic and negative binomial regression models, respectively. All analyses were adjusted for gender, age (continuous), smoking status (never smoker, ex‐smoker, current smoker), Body Mass Index (BMI; <24.9, 25–29.9, >30 kg/m2), and educational level (<high school diploma, high school to 1‐level university, 2‐level university to 4‐level university, ≥5‐level university). As associations of household exposure to irritants 9 , 10 , 11 , 12 , 13 and sprays 9 , 14 , 16 , 18 with asthma were previously observed in the literature, we conducted a sensitivity analysis to examine whether the potential associations observed for newly studied products (scented products, disinfecting wipes, green and homemade products) reflect the coexposure to irritants and/or sprays. For this analysis, we defined a three‐class variable (reference, exposed to a given product without being coexposed to irritants and sprays, coexposed to irritants and/or sprays for a given product). In order to examine whether the six large categories have an influence on the age of onset of asthma, we also studied the associations between household exposure to cleaning products and the age of the onset of asthma (never asthma, current asthma developed before 18 years, current asthma developed after 18 years) by multinomial logistic regression models. In addition, analyses were stratified by sex, smoking status, educational level, and by household help (binary variable [yes/no] according to the answer to the question “Are you getting help to do home cleaning, for example, husband, household employee, family members, friends,…?”) to evaluate the robustness of the results. Finally, we performed another sensitivity analysis to consider occupational exposures to cleaning products, which could be much more important than household exposures. Therefore, we repeated the main analyses after exclusion of participants professionally exposed to cleaning products over the last 2 years, estimated after a preliminary application of the OAsJEM (Occupational asthma‐specific job‐exposure matrix 39 ) for jobs exposed to “high level chemicals disinfectants,” “indoor cleaning,” or “bleach” (49 job codes). A full transcoding (international job codes to French job codes) of the OAsJEM by experts is still in progress for future finale application in CONSTANCES.
The analyses were performed using the statistical analysis software SAS version 9.4 (SAS Institute).
3. RESULTS
Among the 68 168 participants included in the CONSTANCES cohort in 2017 and 2018, 47 643 had household exposure data available in 2019. Participants with missing data on smoking status (n = 1443), BMI (n = 1332) or both on ever asthma status and asthma symptom score (n = 98) were excluded. Therefore, our study population consisted of 44 770 participants (Figure 1). Participants non‐included in 2017 or 2018, slightly differed from those included in the present study: they were older, more often men and with a lower educational level, with less current asthma and symptoms (Table S1). Participants who did not complete questionnaire for household exposure differed from the studied population: they were younger, more often men, current smokers, obese, with a lower educational level, with more current asthma and symptoms. The analyses related to current asthma were carried out on 41 570 participants without missing data on asthma status, including 4144 with current asthma. Analyses related to the asthma symptom score were conducted in 43 503 participants without missing data on this outcome.
Participants were 46.8 years old on average (Table 1), 56% were women, 34% were ex‐smokers, and 15% were current smokers, 30% were overweight (BMI > 25 kg/m2), and 28% had a high educational level (≥5‐level university). Regarding exposures to cleaning products, weekly use of the six specific products/forms studied varied from 11% to 37% and 27% of participants reported no weekly use at home. Around 50% reported having help to do home cleaning and 8% had a potential occupational exposure to cleaning products. Among participants not weekly exposed to cleaning products at home, 4% reported never using any of the six categories of cleaning products studied, whereas 96% used at least of one these products <1 day per week (Table S2). Participants with current asthma were more often women, younger and current smokers, had a higher BMI and educational level, and were more exposed to cleaning products than participants without asthma (Table 1). These characteristics were also described according to the asthma symptom score (Table S3).
TABLE 1.
Population characteristics according to current asthma status
| All | Never asthma | Current asthma | p‐value | |
|---|---|---|---|---|
| n = 41 570 | n = 37 426 | n = 4144 | ||
| Gender, n (%) | ||||
| Male | 18 348 (44.1) | 16 577 (44.3) | 1771 (42.7) | 0.056 |
| Female | 23 222 (55.9) | 20 849 (55.7) | 2373 (57.3) | |
| Age (years), mean ± sd | 46.8 ± 13.2 | 47.1 ± 13.2 | 44.1 ± 13.2 | <0.0001 |
| Smoking status, n (%) | ||||
| Never smoker | 20 900 (50.3) | 18 924 (50.6) | 1976 (47.7) | <0.0001 |
| Ex‐smoker | 14 258 (34.3) | 12 891 (34.4) | 1367 (33.0) | |
| Current smoker | 6412 (15.4) | 5611 (15.0) | 801 (19.3) | |
| BMI (Body Mass Index ‐ kg/m2), n (%) | ||||
| <24.9 | 24 422 (58.7) | 22 196 (59.3) | 2226 (53.7) | <0.0001 |
| [25–29.9] | 12 345 (29.7) | 11 048 (29.5) | 1297 (31.3) | |
| ≥30 | 4803 (11.6) | 4182 (11.2) | 621 (15.0) | |
| Educational level, n (%) | ||||
| <high school diploma | 8142 (19.8) | 7413 (20.0) | 729 (17.8) | 0.0061 |
| high school to 1‐level university | 6113 (14.9) | 5513 (14.9) | 600 (14.7) | |
| 2‐level university to 4‐level university | 15 398 (37.4) | 13 836 (37.3) | 1562 (38.3) | |
| ≥5‐level university | 11 478 (27.9) | 10 284 (27.8) | 1194 (29.2) | |
| Asthma symptom score, n (%) | ||||
| 0 symptom | 28 060 (69.5) | 27 437 (75.4) | 623 (15.7) | <0.0001 |
| 1 symptom | 7736 (19.2) | 6322 (17.4) | 1411 (35.7) | |
| ≥2 symptoms | 4567 (11.3) | 2645 (7.2) | 1922 (48.6) | |
| Weekly use of cleaning products, n (%) | ||||
| <1 day/week | 10 760 (26.8) | 9790 (27.1) | 970 (24.0) | <0.0001 |
| ≥1 day/week | 29 464 (73.2) | 26 398 (72.9) | 3066 (76.0) | |
| Household help, n (%) | 21 000 (51.2) | 18 868 (51.1) | 2132 (52.1) | <0.0001 |
| Potential occupational exposure a , n (%) | 2699 (8.1) | 2394 (8.1) | 305 (9.0) | 0.0524 |
Note: Results presented in bold are significant.
To cleaning products according to a preliminary transcoding for applying the OAsJEM (Occupational asthma‐specific job‐exposure matrix 39 ) to 49 job codes in CONSTANCES.
3.1. Household use of cleaning products and asthma
Weekly use of cleaning products was significantly associated with current asthma, regardless of the categories of products used (Table 2). Indeed, we observed a significant dose‐response association between the frequency of use of irritants, sprays, scented products, disinfecting wipes, green products, homemade products, and current asthma, before and after adjustment for potential confounders. A dose‐response association was also observed for the number of irritants, sprays, scented products used, and current asthma (Figure S1).
TABLE 2.
Associations between the frequency of use of household cleaning products and current asthma
| All | Never asthma | Current asthma | Crude OR | Adjusted OR a | p trend | |
|---|---|---|---|---|---|---|
| n = 41 570 | n = 37 426 | n = 4144 | [95% CI] | [95% CI] | ||
| Not weekly exposed to any of the six large categories (ref) | n = 10 760 | n = 9790 | n = 970 | 1.00 | 1.00 | |
| Irritants | ||||||
| 1–3 days/week | n = 11 670 | 47.0% | 51.5% | 1.25 [1.15–1.37] | 1.22 [1.11–1.34] | <0.0001 |
| 4–7 days/week | n = 2172 | 8.7% | 9.7% | 1.27 [1.10–1.47] | 1.30 [1.11–1.52] | |
| Sprays | ||||||
| 1–3 days/week | n = 11 304 | 43.2% | 44.6% | 1.19 [1.09–1.30] | 1.13 [1.02–1.24] | <0.0001 |
| 4–7 days/week | n = 4005 | 14.9% | 19.1% | 1.47 [1.31–1.65] | 1.37 [1.22–1.55] | |
| Scented products | ||||||
| 1–3 days/week | n = 9628 | 37.9% | 40.6% | 1.23 [1.12–1.35] | 1.14 [1.03–1.25] | 0.0018 |
| 4–7 days/week | n = 4847 | 18.9% | 21.7% | 1.32 [1.18–1.47] | 1.19 [1.06–1.33] | |
| Disinfecting wipes | ||||||
| 1–3 days/week | n = 6442 | 33.3% | 37.9% | 1.32 [1.19–1.46] | 1.18 [1.06–1.31] | <0.0001 |
| 4–7 days/week | n = 1896 | 9.6% | 12.7% | 1.52 [1.31–1.76] | 1.32 [1.13–1.55] | |
| Green products | ||||||
| 1–3 days/week | n = 10 039 | 42.2% | 43.4% | 1.10 [1.00–1.21] | 1.07 [0.97–1.18] |
0.0182 |
| 4–7 days/week | n = 2939 | 12.2% | 14.0% | 1.22 [1.07–1.40] | 1.18 [1.03–1.36] | |
| Homemade products | ||||||
| 1–3 days/week | n = 3429 | 21.8% | 24.9% | 1.24 [1.09–1.41] | 1.15 [1.01–1.31] | 0.0017 |
| 4–7 days/week | n = 1303 | 8.2% | 10.6% | 1.41 [1.18–1.69] | 1.31 [1.08–1.58] | |
Adjusted Odds Ratio (OR) for gender, age, smoking status, BMI, and educational level of associations between the frequency of use of household cleaning products and current asthma, obtained by logistic regression models; results presented in bold are significant
Theses associations were slightly stronger for participants with an adult onset asthma, especially for disinfecting wipes, compared to participants with asthma onset in childhood (Figure S2). The associations between weekly use of cleaning products, studied in two classes, and current asthma were of similar magnitude after stratification by gender, smoking status, educational level, and household help, without statistically significant interactions (Table S4). In addition, after exclusion of participants with potential occupational exposure in the last 2 years (n = 2699), the same associations remained significant (Table S5).
Regarding the asthma symptom score, we observed a consistent dose‐response association with the frequency of use of the six large categories of cleaning products (Figure 2). A dose‐response association was also observed for the number of irritants (1 irritant: 1.19 [1.13–1.26]; ≥2 irritants: 1.27 [1.19–1.37]), sprays (1 spray: 1.17 [1.11–1.24]; 2 sprays: 1.22 [1.14–1.31]; ≥3 sprays: 1.27 [1.19–1.36]) and scented products used (1 perfume: 1.16 [1.09–1.22]; 2 perfumes: 1.30 [1.21–1.40]; ≥3 perfumes: 1.55 [1.42–1.69]). The associations appeared slightly stronger than those previously noticed for current asthma. These results persisted after stratification by several factors (gender, smoking status, educational level, household help, and the asthma status) and after exclusion of participants with potential occupational exposure in the last 2 years (results are not shown).
FIGURE 2.
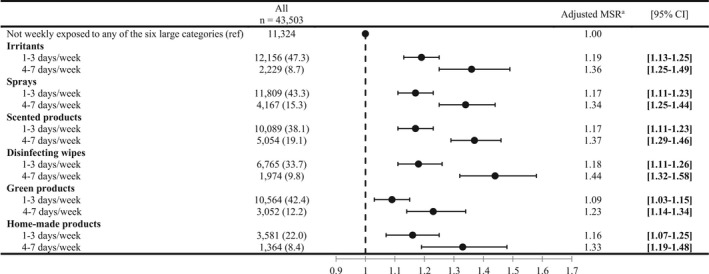
Associations between the frequency of use of cleaning products and the asthma symptom score. Mean Score Ratio (MSR) adjusted for gender, age, smoking status, BMI, and educational level of associations between the frequency of use of cleaning products and the asthma symptom score, obtained by negative binomial regression model.
3.2. Co‐exposure to irritants and sprays
The associations between a given cleaning product (disinfecting wipes, scented, green, and homemade products) used without irritants and sprays and current asthma were generally weaker and not significant, compared to the co‐use of these two products (Table 3), except for disinfecting wipes, which showed a significant association with current asthma whether used alone (OR = 1.16 [1.00–1.36]) or together with irritants or sprays (OR = 1.21 [1.09–1.35]).
TABLE 3.
Associations between weekly use of cleaning products and current asthma according to the co‐use of irritants and sprays at home
| Adjusted OR a [95% CI] | Scented products | Disinfecting wipes | Green products | Homemade products |
|---|---|---|---|---|
| Not weekly exposed to any of the six large categories (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Weekly exposed to any of the six large categories | 1.15 [1.06–1.26] | 1.21 [1.09–1.34] | 1.09 [1.00–1.20] | 1.19 [1.06–1.34] |
| Co‐exposure to risks previously identified b (irritants or sprays): | ||||
| Not co‐exposed | 0.97 [0.85–1.10] | 1.16 [1.00–1.36] | 0.94 [0.83–1.07] | 0.99 [0.83–1.19] |
| Co‐exposed | 1.23 [1.12–1.35] | 1.21 [1.09–1.35] | 1.16 [1.05–1.29] | 1.30 [1.14–1.49] |
Adjusted Odds Ratio (OR) for gender, age, smoking status, BMI, and educational level of associations between weekly use of cleaning products and current asthma according to the co‐use of irritants and sprays at home, obtained by logistic regression models; results presented in bold are significant.
Furthermore, associations between these four cleaning products used at the highest frequency (4–7 days a week), without co‐exposure to irritants/sprays and current asthma remained not significant (Table S6).
Regarding the asthma symptom score, when the co‐exposure was considered, the associations for disinfecting wipes and scented products used without irritants or sprays were weaker, but still significant (Figure 3). However, for the use of green and homemade products, the associations were weaker and no longer significant.
FIGURE 3.
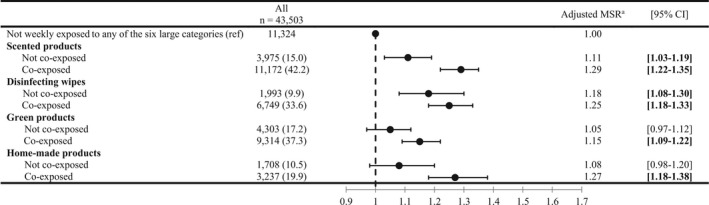
Associations between weekly use of cleaning products and the asthma symptom score, according to the co‐use of irritants and sprays at home. Mean Score Ratio (MSR) adjusted for gender, age, smoking status, BMI, and educational level of associations between weekly use of cleaning products and the asthma symptom score, according to the co‐use of irritants and sprays at home, obtained by negative binomial regression models
4. DISCUSSION
In this cross‐sectional analysis of data from the CONSTANCES cohort, consistent significant associations were found between weekly use of six large categories of cleaning products, both for current asthma and the asthma symptom score, with a dose‐response trend according to frequency of use. Moreover, we found a dose‐response association with the number of irritants, sprays and scented products used. After considering the co‐exposure to irritants or sprayed products at home, well‐established risk factors for asthma, significant associations persisted for disinfecting wipes for both outcomes, whereas no association were observed for green and homemade products.
Our findings are consistent with previous epidemiological studies on household exposure to irritants, sprays, and asthma. As in our study, a dose‐response association was recently observed between the frequency, the number of irritants used and current asthma in a large cohort of elderly French women (Étude Épidémiologique de l'Éducation Nationale – E3N). 10 Regarding sprays, our results are consistent with those of ECRHS, the first study focusing on this issue, 18 in which a dose‐response association between the frequency of use of sprays and new‐onset asthma was identified. Regarding gender, borderline significant associations were observed among men in ECRHS. 18 Given that we reported significant associations of the same magnitude in both men and women, their finding can probably be explained by the smaller number of men using at least two sprays per week. As in our study, in another French cohort (Epidemiological study on the Genetics and Environment of Asthma – EGEA), weekly use of at least two sprays was associated with current asthma and a high asthma symptom score (at least two symptoms of asthma). 16 Furthermore, current asthma was associated with the weekly use of only one spray. Also in E3N, weekly use of at least one spray was significantly associated with current asthma only among women without household help, 14 while in CONSTANCES we found significant associations for both participants with and without household help. Since the E3N cohort consists exclusively of elderly women, the help they benefit from is likely provided by a household employee, so that they are likely to do less home cleaning themselves. In the CONSTANCES cohort, as participants are younger, the household help could correspond to a family member as well as a household employee, which the questionnaire does not allow to determine. Our results for sprayed products add additional evidence on the negative impact of this application mode on respiratory health. However, the sale of products in this form has increased over the last decades and is still at high level. 18 , 40
To our knowledge, this is one of the first epidemiological studies testing the associations between the household use of scented products and asthma and the first examining disinfecting wipes, green, homemade products. For scented products, we first observed a dose‐response association between their frequency of use, current asthma and the asthma symptom score. After considering co‐exposures, the association with current asthma was no longer observed but the one with the asthma symptom score persisted. Our results are consistent with those of Lemire et al. in E3N 10 who found that weekly use of scented products identified using two exposure assessment methods (self‐questionnaire and a smartphone application linked to a product compounds database) was significantly associated with at least one symptom of asthma. Our results also suggest a deleterious effect of disinfecting wipes on asthma since we found a dose‐response association between the frequency of use of this product, current asthma and the asthma symptom score. Moreover, this association is robust because it persisted in most sensitivity analyses. For green products, our results are consistent with those of Garza et al. 22 as we found less evidence for an association with asthma. Indeed, the associations observed were lower than for other products and were no longer present after considering co‐exposures, nor among never smokers. Thus, in addition of being safer for the environment, 8 green products may be the category of cleaning products to be less harmful for respiratory health, compared to the other products studied. For homemade products, the strength of the association with asthma was close to those found in conventional products but this association disappeared after considering co‐exposures.
The underlying mechanisms involved in the respiratory effects of cleaning products are still poorly understood. 27 , 41 The assumptions are that cleaning products can have two different effects: some will have an irritating effect and others a sensitizing effect on the respiratory tract. 4 , 5 , 7 However, some products may induce both effects, depending on whether exposure occurs at a low or high concentration, as suspected for quaternary ammonium compounds, for example. 1 , 4 , 27 Furthermore, products applied in a spray form contain perfumes and may therefore have a sensitizing effect and induce asthma through allergic mechanisms. 42 , 43 In the scientific literature, associations of the same magnitude for allergic and non‐allergic asthma were once reported with the use of sprays. 16 In addition, another study reported strong association between weekly use of at least one spray and current asthma among women without allergic rhinitis, whereas no association was shown among women with allergic rhinitis. 14 The other cleaning products may rather operate by an irritating mechanism and would be more associated with non‐allergic asthma as previously shown. 12 The inhalation of irritating compounds may cause epithelial damage, increase lung permeability and oxidative stress. 4 , 7 , 8 , 42 , 44
The main strength of our study is that it is based on data from the large CONSTANCES cohort, which allowed us to assess the effect of cleaning products in a large number of participants, randomly selected among the general French population, and thus limits potential problems of statistical power. Moreover, these data also allowed us to perform analyses on a mixed gender population, with a wide range of age, whereas most epidemiological studies were only able to study the impact of the household use of cleaning products on asthma among women. 9 , 10 , 12 , 14 , 16 Secondly, we took into account the couse of products for which associations with the respiratory health were previously shown, including irritants 9 , 10 , 11 , 12 , 13 and sprays. 9 , 14 , 16 , 18 Another strength of our study is the use of the asthma symptom score, which is an alternative method recommended to assess asthma risk factors with greater statistical power. 36 , 37 By using this definition, we showed more significant associations than with the traditional dichotomous definition. Lastly, the results persisted after performing several sensitivity analyses, which underlines their robustness. In addition, results for childhood and adult onset asthma are consistent with other epidemiological studies in occupational context suggesting that the use of cleaning products can induce asthma incidence but also exacerbate a pre‐existing asthma. 21
Our study also has some limitations. First, household exposure to cleaning products was only assessed by questionnaire, thus relying on participant statement, which could induce differential and non‐differential misclassification biases. Eight epidemiological studies have discussed this type of bias, some of them estimated household exposure to cleaning products by different methods (Principal Component Analysis – PCA, 14 , 16 composite score, 14 scanning cleaning products barcodes by a smartphone application linked to a product compounds database, 11 …) and observed similar results for irritants and sprays to those obtained by crude questionnaire‐based assessments. In addition, it was recently highlighted that almost all cleaning products contain perfumes. 11 It is then possible that, when assessing exposure to scented products by questionnaire, participants may not be aware that some contain perfumes and may underestimate their exposure. In general, it would be important to develop more objective methods to estimate household exposure to cleaning products. A recently developed smartphone application 11 may allow to identify the chemical compounds specifically causing the health effect to better understand the mechanisms by which they can induce or exacerbate asthma. Secondly, the use of green and homemade cleaning products could be influenced by participants' lifestyle and socioeconomic level. Indeed, participants with a healthier lifestyle may perceive such products to cause the least adverse effects on the environment and the health and rather use them than conventional ones. In addition, these products can be less affordable than conventional ones. However, to consider this possibility, associations were adjusted on major lifestyle risk factors known for asthma. Finally, because of the cross‐sectional design of our study and the assessment of respiratory health and household exposures 2 years apart, we were not able to consider the temporal relationship between the use of cleaning products and asthma. A possible reverse causation phenomenon, that is, participants with current asthma using more frequently cleaning products at home than non‐asthmatic participants in order to eliminate dust or molds, which may cause symptoms, might partly explain our results. However, significant associations were observed for sprays and irritants, but not for green and homemade products when used alone, and it seems unlikely that participants with current asthma use specifically more irritants and sprays than green and homemade products. In addition, our results are consistent with literature in occupational settings 45 , 46 where workers do not choose the frequency of cleaning tasks, and with associations observed between household use of sprays or disinfectants and new‐onset asthma in longitudinal studies. 13 , 18 Therefore, a reverse causation phenomenon is unlikely to explain associations assessed in our manuscript.
5. CONCLUSIONS
In conclusion, household use of cleaning products with various application modes, was associated with asthma among French adults. Based on our results, it seems less harmful to use liquid products than sprays or ready‐to‐use disinfecting wipes and to use green products than conventional ones. Further research is needed on this issue, in particular to clarify the impact of green and homemade products on respiratory health. This will eventually allow the development of preventive measures targeting the use of certain products with the final goal to reduce the world's asthma‐related morbidity.
AUTHOR CONTRIBUTION
E.P.D.S contributed to the analysis and interpretation of the data, and primary manuscript preparation. M.G., C.R., and M.Z. contributed to acquisition and interpretation of the data and critical revision of the manuscript. G.S, B.L., R.N., N.R., and R.V. were involved in the data interpretation and critical revision of the manuscript. N.L.M. and O.D. developed the study hypotheses, and contributed to data interpretation, primary manuscript preparation and critical revision of the manuscript. All authors approved the final version of the manuscript. All authors have read and agreed to the published version of the manuscript.
FUNDING INFORMATION
The CONSTANCES Cohort Study was funded by the Caisse nationale d'assurance maladie des travailleurs salariés (CNAMTS), and benefits from a grant from the French Commissariat général à l'investissement (ANR‐11‐INBS‐0002). CONSTANCES also receives funding from MSD, AstraZeneca, Lundbeck and l'Oréal managed by INSERM‐Transfert. Emilie PACHECO DA SILVA's internship was funded by the DIM Qi2 Île‐de‐France and she has benefited from a PhD scholarship by the University of Paris‐Saclay, France.
CONFLICT OF INTEREST
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supporting information
Appendix S1
ACKNOWLEDGEMENT
The authors thank the “Caisse nationale d'assurance maladie des travailleurs salariés” (CNAMTS), the “Centres d'examens de santé” of the French Social Security where cohort participants were included and the CONSTANCES respiratory group.
Pacheco Da Silva E, Sit G, Goldberg M, et al. Household use of green and homemade cleaning products, wipe application mode, and asthma among French adults from the CONSTANCES cohort. Indoor Air. 2022;32:e13078. doi: 10.1111/ina.13078
Contributor Information
Emilie Pacheco Da Silva, Email: emilie.pacheco-da-silva@inserm.fr.
Guillaume Sit, Email: guillaume.sit@inserm.fr.
Marcel Goldberg, Email: marcel.goldberg@inserm.fr.
Bénédicte Leynaert, Email: benedicte.leynaert@inserm.fr.
Rachel Nadif, Email: rachel.nadif@inserm.fr.
Céline Ribet, Email: celine.ribet@inserm.fr.
Nicolas Roche, Email: nicolas.roche@aphp.fr.
Marie Zins, Email: marie.zins@inserm.fr.
Raphaëlle Varraso, Email: raphaelle.varraso@inserm.fr.
Orianne Dumas, Email: orianne.dumas@inserm.fr.
Nicole Le Moual, Email: nicole.lemoual@inserm.fr.
DATA AVAILABILITY STATEMENTS
Data were obtained from the CONSTANCES group. It can be provided upon reasonable request after approval by the CONSTANCES scientific committee.
The CONSTANCES cohort received ethical approval from the French National Data Protection Authority (authorization no. 910486) and the Institutional Review Board of the National Institute for Medical Research (authorization no. 01–011). All participants gave informed consent to participate.
The participants provided their written consent to participate in this study.
REFERENCES
- 1. Quirce S, Barranco P. Cleaning agents and asthma. J Investig Allergol Clin Immunol. 2010;20(7):542‐550. quiz 2p following 550. [PubMed] [Google Scholar]
- 2. Dumas O, Le Moual N. Damaging effects of household cleaning products on the lungs. Expert Rev Respir Med. 2020;14(1):1‐4. doi: 10.1080/17476348.2020.1689123 [DOI] [PubMed] [Google Scholar]
- 3. Dumas O, Le Moual N. Do chronic workplace irritant exposures cause asthma? Curr Opin Allergy Clin Immunol. 2016;16(2):75‐85. doi: 10.1097/ACI.0000000000000247 [DOI] [PubMed] [Google Scholar]
- 4. Folletti I, Siracusa A, Paolocci G. Update on asthma and cleaning agents. Curr Opin Allergy Clin Immunol. 2017;17(2):90‐95. doi: 10.1097/ACI.0000000000000349 [DOI] [PubMed] [Google Scholar]
- 5. Le Moual N, Jacquemin B, Varraso R, Dumas O, Kauffmann F, Nadif R. Environment and asthma in adults. La Presse Médicale. 2013;42(9, Part 2):e317‐e333. doi: 10.1016/j.lpm.2013.06.010 [DOI] [PubMed] [Google Scholar]
- 6. Quinn MM, Henneberger PK, Braun B, et al. Cleaning and disinfecting environmental surfaces in health care: toward an integrated framework for infection and occupational illness prevention. Am J Infect Control. 2015;43(5):424‐434. doi: 10.1016/j.ajic.2015.01.029 [DOI] [PubMed] [Google Scholar]
- 7. Vandenplas O, Wiszniewska M, Raulf M, et al. EAACI position paper: irritant‐induced asthma. Allergy. 2014;69(9):1141‐1153. doi: 10.1111/all.12448 [DOI] [PubMed] [Google Scholar]
- 8. Siracusa A, Blay FD, Folletti I, et al. Asthma and exposure to cleaning products – a European academy of allergy and clinical immunology task force consensus statement. Allergy. 2013;68(12):1532‐1545. doi: 10.1111/all.12279 [DOI] [PubMed] [Google Scholar]
- 9. Dumas O, Bédard A, Marbac M, et al. Household cleaning and poor asthma control among elderly women. J Allergy Clin Immunol In Pract. 2021;9(6):2358‐2365.e4. doi: 10.1016/j.jaip.2021.02.022 [DOI] [PubMed] [Google Scholar]
- 10. Lemire P, Dumas O, Chanoine S, et al. Domestic exposure to irritant cleaning agents and asthma in women. Environ Int. 2020;144:106017. doi: 10.1016/j.envint.2020.106017 [DOI] [PubMed] [Google Scholar]
- 11. Lemire P, Temam S, Lyon‐Caen S, et al. Comparison of a barcode‐based smartphone application to a questionnaire to assess the use of cleaning products at home and their association with asthma symptoms. Int J Environ Res Public Health. 2021;18(7):3366. doi: 10.3390/ijerph18073366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Matulonga B, Rava M, Siroux V, et al. Women using bleach for home cleaning are at increased risk of non‐allergic asthma. Respir Med. 2016;117:264‐271. doi: 10.1016/j.rmed.2016.06.019 [DOI] [PubMed] [Google Scholar]
- 13. Weinmann T, Gerlich J, Heinrich S, et al. Association of household cleaning agents and disinfectants with asthma in young German adults. Occup Environ Med. 2017;74(9):684‐690. doi: 10.1136/oemed-2016-104086 [DOI] [PubMed] [Google Scholar]
- 14. Bédard A, Varraso R, Sanchez M, et al. Cleaning sprays, household help and asthma among elderly women. Respir Med. 2014;108(1):171‐180. doi: 10.1016/j.rmed.2013.10.018 [DOI] [PubMed] [Google Scholar]
- 15. Mehta AJ, Adam M, Schaffner E, et al. Heart rate variability in association with frequent use of household sprays and scented products in SAPALDIA. Environ Health Perspect. 2012;120(7):958‐964. doi: 10.1289/ehp.1104567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Le Moual N, Varraso R, Siroux V, et al. Domestic use of cleaning sprays and asthma activity in females. Eur Respir J. 2012;40(6):1381‐1389. doi: 10.1183/09031936.00197611 [DOI] [PubMed] [Google Scholar]
- 17. Svanes Ø, Bertelsen RJ, Lygre SHL, et al. Cleaning at home and at work in relation to lung function decline and airway obstruction. Am J Respir Crit Care Med. 2018;197(9):1157‐1163. doi: 10.1164/rccm.201706-1311OC [DOI] [PubMed] [Google Scholar]
- 18. Zock J‐P, Plana E, Jarvis D, et al. The use of household cleaning sprays and adult asthma. Am J Respir Crit Care Med. 2007;176(8):735‐741. doi: 10.1164/rccm.200612-1793OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Leynaert B, Le Moual N, Neukirch C, Siroux V, Varraso R. Facteurs environnementaux favorisant le développement d'un asthme. Presse Med. 2019;48(3):262‐273. doi: 10.1016/j.lpm.2019.02.022 [DOI] [PubMed] [Google Scholar]
- 20. Townsend E, Miller V, Prakash YS. Sex differences and sex steroids in lung health and disease. Endocr Rev. 2012;33:1‐47. doi: 10.1210/er.2010-0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med. 2014;370:640‐649. doi: 10.1056/NEJMra1301758 [DOI] [PubMed] [Google Scholar]
- 22. Garza JL, Cavallari JM, Wakai S, et al. Traditional and environmentally preferable cleaning product exposure and health symptoms in custodians. Am J Ind Med. 2015;58(9):988‐995. doi: 10.1002/ajim.22484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lindberg JE, Quinn MM, Gore RJ, et al. Assessment of home care aides' respiratory exposure to total volatile organic compounds and chlorine during simulated bathroom cleaning: an experimental design with conventional and “green” products. J Occup Environ Hyg. 2021;18(6):276‐287. doi: 10.1080/15459624.2021.1910280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harley KG, Calderon L, Nolan JES, et al. Changes in Latina Women's exposure to cleaning chemicals associated with switching from conventional to “green” household cleaning products: the LUCIR intervention study. Environ Health Perspect. 2021;129(9):97001. doi: 10.1289/EHP8831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Benjamin M, Arnold S, Rao M, Davis K, Maier A, Virkutyte J. Ventilation and posture effects on inhalation exposures to volatile cleaning ingredients in a simulated domestic worker cleaning environment. Indoor Air. 2020;31:128‐140. doi: 10.1111/ina.12715 [DOI] [PubMed] [Google Scholar]
- 26. Shin HM, McKone TE, Bennett DH. Model framework for integrating multiple exposure pathways to chemicals in household cleaning products. Indoor Air. 2017;27(4):829‐839. doi: 10.1111/ina.12356 [DOI] [PubMed] [Google Scholar]
- 27. Clausen PA, Frederiksen M, Sejbæk CS, et al. Chemicals inhaled from spray cleaning and disinfection products and their respiratory effects. A comprehensive review. Int J Hyg Environ Health. 2020;229:113592. doi: 10.1016/j.ijheh.2020.113592 [DOI] [PubMed] [Google Scholar]
- 28. Lovén K, Isaxon C, Wierzbicka A, Gudmundsson A. Characterization of airborne particles from cleaning sprays and their corresponding respiratory deposition fractions. J Occup Environ Hyg. 2019;16(9):656‐667. doi: 10.1080/15459624.2019.1643466 [DOI] [PubMed] [Google Scholar]
- 29. Dumas O, Wiley AS, Quinot C, et al. Occupational exposure to disinfectants and asthma control in US nurses. Eur Respir J. 2017;50(4):1700237. doi: 10.1183/13993003.00237-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mirabelli MC, Zock J, Plana E, et al. Occupational risk factors for asthma among nurses and related healthcare professionals in an international study. Occup Environ Med. 2007;64(7):474‐479. doi: 10.1136/oem.2006.031203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zock J‐P, Kogevinas M, Sunyer J, et al. Asthma risk, cleaning activities and use of specific cleaning products among Spanish indoor cleaners. Scand J Work Environ Health. 2001;27(1):76‐81. doi: 10.5271/sjweh.590 [DOI] [PubMed] [Google Scholar]
- 32. Archangelidi O, Sathiyajit S, Consonni D, Jarvis D, Matteis SD. Cleaning products and respiratory health outcomes in occupational cleaners: a systematic review and meta‐analysis. Occup Environ Med. 2020;24:604‐617. doi: 10.1136/oemed-2020-106776 [DOI] [PubMed] [Google Scholar]
- 33. Medina‐Ramón M, Zock JP, Kogevinas M, et al. Asthma, chronic bronchitis, and exposure to irritant agents in occupational domestic cleaning: a nested case‐control study. Occup Environ Med. 2005;62(9):598‐606. doi: 10.1136/oem.2004.017640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Song X, Vossebein L, Zille A. Efficacy of disinfectant‐impregnated wipes used for surface disinfection in hospitals: a review. Antimicrob Resist Infect Control. 2019;8:139. doi: 10.1186/s13756-019-0595-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zins M, Goldberg M, CONSTANCES team . The French CONSTANCES population‐based cohort: design, inclusion and follow‐up. Eur J Epidemiol. 2015;30(12):1317‐1328. doi: 10.1007/s10654-015-0096-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sunyer J, Pekkanen J, Garcia‐Esteban R, et al. Asthma score: predictive ability and risk factors. Allergy. 2007;62(2):142‐148. doi: 10.1111/j.1398-9995.2006.01184.x [DOI] [PubMed] [Google Scholar]
- 37. Pekkanen J, Sunyer J, Anto JM, Burney P. Operational definitions of asthma in studies on its aetiology. Eur Respir J. 2005;26(1):28‐35. doi: 10.1183/09031936.05.00120104 [DOI] [PubMed] [Google Scholar]
- 38. Zock J‐P, Cavallé N, Kromhout H, et al. Evaluation of specific occupational asthma risks in a community‐based study with special reference to single and multiple exposures. J Expo Anal Environ Epidemiol. 2004;14(5):397‐403. doi: 10.1038/sj.jea.7500337 [DOI] [PubMed] [Google Scholar]
- 39. Le Moual N, Zock JP, Dumas O, et al. Update of an occupational asthma‐specific job exposure matrix to assess exposure to 30 specific agents. Occup Environ Med. 2018;75(7):507‐514. doi: 10.1136/oemed-2017-104866 [DOI] [PubMed] [Google Scholar]
- 40. European Aerosol Federation . European aerosol federation . Published 2021. Accessed December 2, 2021. https://www.aerosol.org/
- 41. 2020 GINA Main Report . Global initiative for asthma ‐ Gina . Accessed April 23, 2020. https://ginasthma.org/gina‐reports/
- 42. Maestrelli P, Boschetto P, Fabbri LM, Mapp CE. Mechanisms of occupational asthma. J Allergy Clin Immunol. 2009;123(3):531‐542. doi: 10.1016/j.jaci.2009.01.057 [DOI] [PubMed] [Google Scholar]
- 43. Wolkoff P, Nielsen GD. Effects by inhalation of abundant fragrances in indoor air ‐ an overview. Environ Int. 2017;101:96‐107. doi: 10.1016/j.envint.2017.01.013 [DOI] [PubMed] [Google Scholar]
- 44. Dumas O. Cleaners and airway diseases. Curr Opin Allergy Clin Immunol. 2021;21(2):101‐109. doi: 10.1097/ACI.0000000000000710 [DOI] [PubMed] [Google Scholar]
- 45. Dumas O, Siroux V, Luu F, et al. Cleaning and asthma characteristics in women. Am J Ind Med. 2014;57(3):303‐311. doi: 10.1002/ajim.22244 [DOI] [PubMed] [Google Scholar]
- 46. Le Moual N, Carsin AE, Siroux V, et al. Occupational exposures and uncontrolled adult‐onset asthma in the European Community respiratory health survey II. Eur Respir J. 2014;43(2):374‐386. doi: 10.1183/09031936.00034913 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
Data were obtained from the CONSTANCES group. It can be provided upon reasonable request after approval by the CONSTANCES scientific committee.
The CONSTANCES cohort received ethical approval from the French National Data Protection Authority (authorization no. 910486) and the Institutional Review Board of the National Institute for Medical Research (authorization no. 01–011). All participants gave informed consent to participate.
The participants provided their written consent to participate in this study.


